Abstract
Several sequential passages are involved in the pre-analytical handling of surgical specimens from resection in the surgical theater to paraffin-embedding and storage. Each passage is highly critical and can significantly affect the preservation of morphology, antigens, and nucleic acids. Some key points in this process are still undefined and are subject to high variability among hospitals. High quality and standardization are demanded and pathologists should therefore work to comply with all novel clinical requests (such as genomic and antigenic testing for targeted molecular therapies). Under-vacuum sealing of surgical pieces can be a safe and reliable alternative to storage in large formalin-filled boxes; it prevents dehydration and favors cooling by removing air. Moreover, it implements tissue banking and preservation of nucleic acids. After transport of specimens to pathological anatomy laboratories, the next passage, fixation, has been the object of several attempt to find alternatives to formalin. However, none of the substitutes proved successful, and formalin fixation is still considered the gold standard for preservation of morphology and antigens. RNA has instead been found to be heavily affected by degradation and fragmentation in formalin-fixed tissues. Based on the hypothesis that RNA degradation would be inhibited by maintaining a low temperature, a protocol based on processing tissues with formalin at low temperature (cold fixation) was evaluated and proved useful in obtaining a reduction in RNA fragmentation. Finally, the problem of storage is discussed, in order to find ways to guarantee feasibility of molecular analyses even years after the original diagnosis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Preparation of surgical specimens for histopathological examination requires a sequence of step-wise passages, leading from the biopsy removal up to the paraffin block (Fig. 1).
Sequence of the pre-analytical steps. From the surgical theaters, tissue specimens are transferred to Pathological Anatomy. Grossing is immediately followed by fixation and paraffin embedding. After sectioning of the tissue blocks, sections are appropriately stained. So far, only paraffin embedding and staining are standardized being run with dedicated apparatuses, while for the other steps ample variations of modalities, times, and protocols are used in different laboratories
Local variations in the practice of these steps are common in pathology laboratories worldwide and depend on type of tissue, traditional habits, requests by clinicians and patients and on specific investigations. Moreover, the goal of shortening the turn-around time (TAT) has to be considered.
In common practice, diagnostic and TAT requirements, hence processing, are different for “small” biopsies (<2 cm in size) and large, surgical resection specimens. A fast and reliable pre-surgical diagnosis is requested for the former and, accordingly, these biopsies are best collected directly in fixative-filled vials and soon transferred to the laboratory for paraffin embedding and routine diagnosis.
The processing of “large” surgical specimens is instead more critical, variable, and problematic, involving steps significantly affecting the preservation of antigens and nucleic acids.
This implies that fixation and processing of “small”, pre-surgical biopsies, which starts immediately after procurement, is relatively standardized. At variance, the handling of surgical specimens is more critical and undefined. This will be the topic of the present analysis.
The present interest on the analytical definition of the steps involved in the preparation of surgical specimens is linked to novel clinical requests, demanding genomic and antigenic testing for targeted molecular therapies. Indeed, requests for exploitation of archival formalin-fixed paraffin embedded (FFPE) tissues from surgical resections of breast, lung and colon cancers are exponentially increasing and Pathologists should get ready to play an important role in sample standardization in the years ahead. As a result, guidelines will have to be adopted by laboratories and hospitals on a global scale. Standardization of the pre-analytical phase of surgical specimens’ preparation would be the right answer.
2 The Ischemia Time
The time interval between surgical intervention and proper fixation of the removed specimen is defined as “ischemia time” and is crucial, since ischemia allows activation of tissue enzymes, autolysis, and degradation of proteins and nucleic acids [1, 2]. Substantial RNA degradation may occur during this time interval [3].
The “ischemia time” is currently subdivided into the “warm ischemia time” which occurs during operation, after ligation of blood supply till removal of the specimen from the body, and the “cold ischemia time,” afterwards. The former varies considerably (from a few minutes up to hours), depending on the complexity of the surgical procedure, ability of the surgeon, modality of intervention. The tissue remains alive and reactive, but will undergo progressive metabolic stress due to hypoxia. In an experimental study on colon cancer, Bray et al. [4] emphasized the need of protocols for tissue procurement and showed that significant variation in the level of expression (either increased or decreased) of transcripts was detectable already after 15 min, and by 120 min there was a fourfold increase in a number of genes with a more than twofold change in the level of expression. Indeed, this is bound to heavily influence the interpretation on the involvement of specific genes in the pathogenesis of diseases. For example, it is suggested that reduced expression of KLF6 may be implicated in the early stages of the molecular pathogenesis of approximately one-third of colorectal carcinoma cases, but the study by Bray et al. [4] shows that expression of KLF6 mRNA is significantly increased by delay in sample procurement.
The “cold ischemia time” is instead defined as the time interval between tissue removal from the patient and arrival in the pathology laboratory for grossing. During this interval it is mandatory to avoid autolysis and drying of the surface, which might damage tissue structure and components. The temperature of the specimen gradually reaches external temperature (either room temperature or 4 °C for tissues left in fridge), but this process is rather lengthy, as can be tested by using a needle thermometer (Fig. 2).
Methods of transfer of surgical specimens vary according to the architectural layout and distance between surgical theaters and pathology laboratories. The ideal situation is when physical location and hospital protocols allow for the immediate transfer of “fresh” tissue specimens for prompt grossing and fixation. Accordingly, it has been recommended the “cold ischemia time” to remain below 1 h so as to allow a proper processing of breast cancer specimens and permit a correct evaluation of both morphological and therapeutic-prognostic parameters [5, 6]. Preservation of HER2 reactivity seems less critical than that of Estrogen (ER) and Progesterone Receptors (PgR), since optimal results are still attainable after a 3 h delay [7]. Problems arise when the “cold ischemia time” cannot be kept into properly defined limits: depending on the hospital structure the transport of surgical specimens from the surgical theater to the pathology lab may prolong the ischemia time. In addition, transfer is currently performed wordwide using the most variable types of boxes, transport media, and at different temperatures. It is common practice in many hospitals to immerse surgical resection specimens and organs into large formalin-filled containers, which are then transferred to the pathology laboratory in due time, usually once everyday. This practice carries problems, since:
-
1.
Plastic containers are large and relatively heavy; spilling may occur.
-
2.
Immersion of the whole specimen into formalin prevents the collection of fresh material for tissue banking. In addition, fixation does begin, but only at the periphery. A delay in the transfer to pathology is somehow justified by the fact that “the tissue is already in formalin".
-
3.
Surgical nurses are becoming increasingly concerned about potential toxicity and carcinogenicity of formalin, since the fluid has to be handled outside the hood.
-
4.
When the container does arrive at the pathology lab, opening of the boxes, and handling of the specimen is major cause of diffusion of formaldehyde fumes.
Toxicity of formaldehyde is a matter of concern. This reagent demands caution since it is a skin allergen and produces irritating vapors that can cause asthma. Moreover, the International Agency for Cancer Research [8] has classified formaldehyde as a Class 1 carcinogenic agent. A positive relationship between formalin and respiratory symptoms has been reported not only in workers in match factories [9], but also in hospital staff members professionally exposed to this substance [10]. Statistical evidence has been presented for a possible link between formaldehyde exposure and lympho-hematopoietic malignancies [11], an observation that might fit with data reporting an excess of deaths due to cancer of the lymphatic and hematopoietic systems among British pathologists [12]. Still, the major concern for formaldehyde use is linked to the production of toxic, irritating, and allergenic vapors.
To ride over these problems, we adopted procedures designed to avoid the transfer of formalin-filled boxes in the hospital premises. We accordingly proposed to seal fresh surgical specimens under-vacuum in plastic bags in the surgical theaters, immediately after removal, and to keep them cooled at 4 °C until transfer to the pathology labs, where they are routinely processed [13]. Sealing of tissues in plastic bags is a quick procedure, taking approximately 15 s and is easily performed by nurses [14].
3 Under Vacuum Sealing
Under-vacuum sealing (UVS), per se, does not guarantee preservation, as experienced by Kristensen et al. [15]. Vacuum sealing, by removing air, prevents dehydration and favors cooling, the latter being the main preserving factor by blocking enzymatic autolysis. In fact, we experimentally demonstrated that cooling down at 4 °C is quicker in UVS-treated tissues [16]. Moreover, cooling down of under-vacuum sealed specimens can be speeded up by using a properly devised procedure (Fig. 3).
Variations of the inner temperature in a surgical specimen (approximately 7 cm in diameter) in different conditions. From the body temperature, on surgical removal, if left at room temperature (A), it takes approximately 3 h for the specimen to stabilize at the external temperature. When the specimen is left, free, in a fridge (B), the inner temperature will gradually go down. The cooling process in Under-Vacuum Sealed (UVS) specimens (C) is facilitated by the lack of insulating air. By using cooling (-20°C) elements (D), the cooling of the UVS specimens is very rapid
Additional benefits are linked to the possibility of standardizing fixation times and of implementing tissue banking. In fact, we can now determine the starting time of fixation in formalin, thus avoiding over-fixation, which can affect immune-phenotyping of the specimen, an issue that is presently regarded as mandatory for breast cancer processing. A bonus of this under-vacuum Sealing and Cooling (UVSC) procedure is the preservation of RNA, which is permitted by the storage at 4 °C [17, 18], thus favoring tissue banking and gene expression profiling. Moreover, the UVSC procedure proved valuable for the preservation of hypoxia resistant cells, such as human stem/progenitor cells, which were successfully isolated and cultured from kidneys stored UVSC up to 48 h after surgery [19]. It derives that this procedure can be exploited to render the extraction of stem cells from human samples more practical and feasible. UVSC could also represent a reliable source for creation of primary cell cultures. The environmentally safe UVSC collection, preservation, and storage of surgical specimens may represent a strategy to bridge diagnostic and experimental pathology thus offering a new tool for bio-banking and for creation of clinically relevant models of neoplastic lesions (primary cultures) [16].
The UVSC procedure has extensively been adopted at the Azienda Ospedaliera Città della Salute e della Scienza di Torino (Italy), a large regional “pavilion” hospital where the distance between surgical theaters and pathology laboratories prevents an immediate transfer of fresh specimens. The transfer of surgical specimens across the Hospital in large formalin-filled boxes was a time-honored habit, but since 2009 the procedure of under-vacuum sealing and cooling has been adopted as the sole and routine procedure for the transfer of surgical specimens (larger than 2 cm). The experience accrued has been duly analyzed and reported [14]. The survey on the feasibility, compliance, and quality assurance of this new procedure for transferring surgical specimens was definitely positive. Dedicated apparatuses (TissueSafe®, Milestone srl, Sorisole, BG, Italy) were located in the premises of each of the six surgical theaters of the Hospital. The UVSC procedure was favorably accepted by the staff and did not present special problems of practical or diagnostic interest and was therefore adopted as the standard in the Hospital.
Moreover, the environmental goal of a progressive reduction of the exposure for nurses, pathologists, and technical personnel to formaldehyde vapors was met. The use of formalin has been reduced and restricted to dedicated areas in the pathology laboratory, and transfer of large boxes filled with fixative throughout the hospital ceased. The flowchart presented in Fig. 4 illustrates the procedures currently practiced in our Institution for tissue transfer and preservation.
Outline of the procedure for handling of the large (>2 cm) surgical specimens, as practiced in the Azienda Ospedaliera Città della Salute e della Scienza di Torino since year 2008. Under-Vacuum Sealed specimens are kept cool (in a fridge) in the surgical premises for a time variable from 1 up to 72 h (during weekends). Grossing, fixation, and histological processing follow. In alternative, material for tissue banking or culturing can be obtained from fresh tissues (PB phosphate buffered)
In conclusion, the simple UVSC processing offered advantages in terms of staff satisfaction, tissue preservation and cost.
4 Tissue Fixation
Fixation is the process whereby cell and tissue structures, as well as chemical components, are preserved in their integrity. This process is most commonly accomplished by immersion into a fluid, which gradually penetrates and acts chemically on the tissue components.
Several fixatives have been proposed, but those presently practiced are either of the aldehyde cross-linking category or alcohol-based, the latter producing coagulation by water subtraction. Alcohol-based fixatives have the advantage of lack of toxicity and of a good preservation of nucleic acids, but show a poor penetration and reportedly result in an unsatisfactory preservation of morphological details [20]. Moreover, in our [21] and in others’ [20, 22] experience, the performance of some immunohistochemical tests is impaired. The alcohol-based substitutes which have been proposed are generally non-cross-linking [21, 23–25] and allow a better preservation of RNA sequences. However, they are inferior as far as morphological (and immunohistochemical) preservation is concerned, and we have to conclude that substitution of formalin with alternative fixatives cannot be foreseen at present.
A 4 % formaldehyde solution in 0.1 M phosphate buffer pH 7.2 (phosphate buffered formalin, PBF) has been adopted as the fixative of choice in histopathology being (relatively) cheap, easy to use, and reliable (it does not over-fix). It guarantees, in appropriate conditions, an optimal morphological preservation. Still, the finality of formalin fixation has evolved over time. Originally, optimal morphological preservation was the sole requirement, but in more recent times, with the advent of immuno-histochemical typing, reliable antigenic preservation is also required [26, 27]. As a consequence, the protocols of formalin fixation have become stricter.
This issue is particularly relevant in onco-pathology for the evaluation of factors predicting responsiveness to therapeutic treatments, and thus, fixation in PBF of breast cancer tissue blocks for no less than 6 and no more than 48 h is now required in order to guarantee an optimal evaluation of ER, PgR, and HER2 expression by immunohistochemistry [28].
In more recent times, a crucial request in cancer pathology has been nucleic acid preservation for gene expression profiling, with the goal of generating new and reliable diagnostic and prognostic parameters [2, 29]. Indeed, evaluation of proliferation activity and clinical evolution prospects in breast cancer are already attainable with molecular tests, and evidence has been presented that evaluation of predictive biomarkers (ER, PgR, HER2) by RNA analysis is fully matching that obtained by immunohistochemistry [2, 29].
The process of formalin fixation involves two separate and interrelated phenomena: (1) penetration into tissues by diffusion and (2) proper fixation by establishment of cross-links between different reactive groups. This latter phenomenon is slow (it takes hours or even days to be completed) and was extensively described and analyzed in numerous studies conducted on the reaction of formaldehyde with different tissue components [30, 31]. The main effect of formaldehyde on tissues is linked to the formation of methylol groups on amino groups first, followed by the establishment of cross-linking methylene groups that lead to proper fixation [32]. These links are partly reversible by the action of peptidases and heating [33], which seems to explain the extensively practiced procedures leading to “antigen retrieval”, that is the restitution of immuno-histochemical reactivity in (FFPE) tissue sections.
The “penetration” step that is represented by the diffusion of the formaldehyde solution into tissues is instead poorly known in its analytical essence and reactions involved. It is only stated that it is “rapid”, at a speed of approximately 1 mm/h [30] (see Fig. 5). The experience in surgical pathology testifies that the speed varies with tissues (being lower in fat tissues), that it is influenced by temperature, relative quantity of the fixative and agitation and that it can be enhanced by application of ultrasounds [34]. As a general rule, we can state that in a 3–4 mm thick tissue section (the tissue blocks produced by grossing) the center of the block is reached in 2 h while, on the contrary, in whole organs immersed in formalin overnight diffusion does not proceed over 1 cm depth. The above statement is referred to PBF which is the solution currently employed [30, 35]. The addition of a minute amount of mercaptoethanol [36] significantly speeds the penetration. As for the relative amount of fluid, common practice dictates that the quantity of formalin should be at least 10 times that of the tissue to be fixed. Experimental tests proved however that fixing tissues with a ratio of PBF volume to tissue volume of 2:1 for 48 h at 20–22 °C was enough to assure a proper fixation and infiltration of the tested tissues [37], fixation being improved by pressure and agitation.
Evaluation of the penetration of formalin in a square block of liver. After 1 h (a) or 2 h (b) of immersion in the fluid, the block is split, frozen, and sections are cut in a cryostat. The formalin-free area appears transparent, while a rough appearance marks the depth of penetration of the fixative (b). In b, the depth of formalin penetration after 2 h of immersion is indicated
The experimental measure of formalin penetration has not been pursued so far. As a test we exploited the phenomenon whereby frozen sections of fresh tissues are transparent, while instead those of formalin-fixed tissues are not and show a rough appearance. This experimental approach, when tested on 1 cm3 liver tissue blocks, shows that indeed at room temperature the penetration is 1 mm in the first hour and approximately 2 mm after 2 h (Fig. 5).
Studies conducted on the preservation status of nucleic acids in FFPE tissues generally agree on the relatively good (though not optimal) preservation of DNA [3]. On the contrary, RNA has been found to be heavily degraded and fragmented so that only short sequences (approximately 100–200 nucleotides) can be recognized and amplified [32, 38–41]. The reasons for this effect are presently unknown, but the cross-linking properties of formaldehyde should be considered. Bases of nucleic acids are involved in this cross-linking process, resulting in the establishment of bonds with side-chain amino groups of proteins. However, this linkage is at least partly reversible following extensive treatment of FFPE tissue sections with peptidases and high temperature [32, 33, 35, 38]. We may conclude that cross-linking of nucleic acid bases cannot be the sole responsible for nucleic acid fragmentation and degradation. The RNA degradation process may well continue during fixation. In fact, while formalin penetration is a rather fast process, tissue fixation is known to be a slow process that requires long time exposure [31, 33].
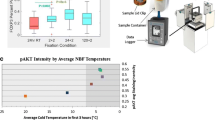
Based on these hypotheses, we have further considered that RNA degradation would be inhibited by maintaining low temperature through all the process of fixation. We have evaluated whether a protocol based on processing tissues with formalin at low temperature, a cold fixation (CF) process, would better preserve nucleic acid integrity, while preserving morphological and antigenic features as well.
The CF process [42] is based on a fixation process in PBF at 4 °C for 20–24 h, followed by dehydration in cold ethanol for 2 h. This was then followed by routine dehydration and paraffin embedding. Using this procedure, we succeeded in obtaining a substantial reduction in RNA fragmentation in FFPE tissue blocks, as assessed by RT-PCR and gene array analysis, while at the same time preserving the morphological and immuno-histochemical properties which make formalin the fixative of choice in histopathology. These data were further confirmed by investigations using whole genome arrays (Agilent Technologies, Inc. Santa Clara, CA). We investigated in parallel RNA extracted from fresh-frozen and Cold Formalin Fixed Paraffin Embedded (CFFPE) material from the same cases of breast cancer. The number of genes detected in RNA extracted from fresh tissues closely matches that of RNA extracted from cold formalin-fixed material from the same cases, the former being only 4.12 % higher [17, 18].
The improvement offered by the CF procedure is therefore linked to a definitely lower degree of nucleic acid fragmentation, especially of mRNA, while keeping the basic advantages that make formalin the fixative of choice in diagnostic histopathology.
The ensuing step of embedding in paraffin wax following dehydration through a sequence of passages in ethanol is well standardized and generally processed with dedicated apparatuses. It has recently been demonstrated that even this process might involve variables affecting tissues and the performance of analytical tests. It is in fact well known that paraffin blocks stored for long times (years) undergo alteration affecting antigenicity as well as RNA preservation (personal experience). Xie and coworkers [43] revealed that inadequate tissue processing, resulting in retention of endogenous water in tissues, leads to antigen degradation and even tissues embedded in paraffin (a non-reactive medium) can undergo a slow degradation process.
Variables which so far attracted little interest, but in the experience of von Ahlfen et al. [44] might influence the status of RNA in the FFPE tissue blocks, are temperature and storage conditions. These authors showed that storage at different temperatures has a profound influence on the extent of RNA fragmentation. After 1 year storage at 4 °C, RIN values around 5–6 could be obtained while in contrast, RNA from blocks stored at room temperature (20–25 °C) or 37 °C, did not show clearly distinct rRNA bands anymore, and the mean fragment length was well below 100 nucleotides. Indeed a demanding topic of future interest would be to standardize the conditions of embedding and storage of FFPE tissue blocks, in order to guarantee feasibility of molecular analyses even years after the original diagnosis.
5 Conclusions
Morphological diagnoses are no longer the sole analyses requested to pathologists. Novel clinical demands, which require the evaluation of prognostic and predictive factors for targeted molecular therapies through genomic and antigenic testing, are pushing for the necessity to standardize handling of surgical specimens, so as to obtain high quality, reliable and reproducible results.
Technologies such as under-vacuum sealing and cold fixation will be implemented in future years, in an attempt to optimize and standardize on a global scale pathological diagnoses and analyses.
References
Ruijter E, van de Kaa C, Aalders T et al (1998) Heterogeneous expression of E-cadherin and p53 in prostate cancer: clinical implications. BIOMED-II markers for prostate cancer study group. Mod Pathol 11(3):276–281
Medeiros F, Rigl CT, Anderson GG et al (2007) Tissue handling for genome-wide expression analysis: a review of the issues, evidence, and opportunities. Arch Pathol Lab Med 131(12):1805–1816
Chung JY, Braunschweig T, Williams R et al (2008) Factors in tissue handling and processing that impact RNA obtained from formalin-fixed, paraffin-embedded tissue. J Histochem Cytochem 56:1033–1042
Bray SE, Paulin FE, Fong SC et al (2010) Gene expression in colorectal neoplasia: modifications induced by tissue ischaemic time and tissue handling protocol. Histopathology 56:240–250
Hammond ME, Hayes DF, Dowsett M et al (2010) American Society of Clinical Oncology and College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Clin Oncol 28(16):2784–2795
Wolff AC, Hammond ME, Hicks DG et al (2013) American Society of Clinical Oncology; College of American Pathologists. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology and College of American Pathologists clinical practice guideline update. J Clin Oncol 31(31):3997–4013
Portier BP, Wang Z, Downs-Kelly E et al (2013) Delay to formalin fixation ‘cold ischemia time’: effect on ERBB2 detection by in-situ hybridization and immunohistochemistry. Mod Pathol 26(1):1–9
Cancer IARC (2006) Monographs on the evaluation of carcinogenic risk to humans. IARC, Lyon
Vaughan WTBH (1939) The practice of allergy. Maryland CV Mosby, Rockville, p 677
Hendrick DJ, Lane DJ (1975) Formalin asthma in hospital staff. Br Med J 1(5958):607–608
Beane Freeman LE, Blair A, Lubin JH et al (2009) Mortality from lymphohematopoietic malignancies among workers in formaldehyde industries: the National Cancer Institute Cohort. J Natl Cancer Inst 101:751–761
Hall A, Harrington JM, Aw TC (1991) Mortality study of British pathologists. Am J Ind Med 20(1):83–89
Bussolati G, Chiusa L, Cimino A et al (2008) Tissue transfer to pathology labs: under vacuum is the safe alternative to formalin. Virchows Arch 452:229–231
Di Novi C, Minniti D, Barbaro S et al (2010) Vacuum-based preservation of surgical specimens: an environmentally-safe step towards a formalin-free hospital. Sci Total Environ 408:3092–3095
Kristensen T, Engvad B, Nielsen O et al (2011) Vacuum sealing and cooling as methods to preserve surgical specimens. Appl Immunohistochem Mol Morphol 19:460–469
Annaratone L, Marchiò C, Russo R et al (2013) A collection of primary tissue cultures of tumors from vacuum packed and cooled surgical specimens: a feasibility study. PLoS ONE 8:e75193
Comanescu M, Annaratone L, D’Armento G et al (2012) Critical steps in tissue processing in histopathology. Recent Pat DNA Gene Sequences 6:22–32
Comanescu M, Arsene D, Ardeleanu C et al (2012) The mandate for a proper preservation in histopathological tissues. Rom J Morphol Embryol 53:233–242
Moggio A, D’Armiento G, Bussolati B (2012) Efficient stem cell isolation from under vacuum preserved tissue samples. Organogenesis 8(3):71–75
Groenen PJ, Blokx WA, Diepenbroek C et al (2011) Preparing pathology for personalized medicine: possibilities for improvement of the pre-analytical phase. Histopathology 59(1):1–7
Stanta G, Mucelli SP, Petrera F et al (2006) A novel fixative improves opportunities of nucleic acids and proteomic analysis in human archive’s tissues. Diagn Mol Pathol 15(2):115–123
Nietner T, Jarutat T, Mertens A (2012) Systematic comparison of tissue fixation with alternative fixatives to conventional tissue fixation with buffered formalin in a xenograft-based model. Virchows Arch 461(3):259–269
Moelans CB, Oostenrijk D, Moons MJ et al (2011) Formaldehyde substitute fixatives: effects on nucleic acid preservation. J Clin Pathol 64:960–967
Arzt L, Kothmaier H, Quehenberger F et al (2011) Evaluation of formalin-free tissue fixation for RNA and microRNA studies. Exp Mol Pathol 91:490–495
Denouel A, Boissiere-Michot F, Rochaix P et al (2011) An alternative fixative to formalin fixation for molecular applications: the RCL2((R))-CS100 approach. Methods Mol Biol 724:297–307
Goldstein NS, Hewitt SM, Taylor CR et al (2007) Recommendations for improved standardization of immunohistochemistry. Appl Immunohistochem Mol Morphol 15:124–133
Dabbs DJ (2008) Immunohistochemical protocols: back to the future. Am J Clin Pathol 129:355–356
Goldstein NS, Ferkowicz M, Odish E et al (2003) Minimum formalin fixation time for consistent estrogen receptor immunohistochemical staining of invasive breast carcinoma. Am J Clin Pathol 120(1):86–92
Lewis F, Maughan NJ, Smith V et al (2001) Unlocking the archive–gene expression in paraffin-embedded tissue. J Pathol 195:66–71
Fox CH, Johnson FB, Whiting J et al (1985) Formaldehyde fixation. J Histochem Cytochem 33(8):845–853
Stanta G, Schneider C (1991) RNA extracted from paraffin-embedded human tissues is amenable to analysis by PCR amplification. Biotechniques 11:304, 306, 308
Helander KG (1994) Kinetic studies of formaldehyde binding in tissue. Biotech Histochem 69:177–179
Sompuram SR, Vani K, Bogen SA (2006) A molecular model of antigen retrieval using a peptide array. Am J Clin Pathol 125:91–98
Zou N, Liang Q, He H et al (2011) Ultrasound-facilitated formalin fixation of biological specimens. Biotech Histochem 86(6):413–420
Hewitt SM, Lewis FA, Cao Y et al (2008) Tissue handling and specimen preparation in surgical pathology: issues concerning the recovery of nucleic acids from formalin-fixed, paraffin-embedded tissue. Arch Pathol Lab Med 132(12):1929–1935
Durgun-Yücel B, Hopwood D, Yücel AH (1996) The effects of mercaptoethanol-formaldehyde on tissue fixation and protein retention. Histochem J 28(5):375–383
Buesa RJ, Peshkov MV (2012) How much formalin is enough to fix tissues? Ann Diagn Pathol 16:202–209
Dotti I, Bonin S, Basili G et al (2010) Effects of formalin, methacarn, and fineFIX fixatives on RNA preservation. Diagn Mol Pathol 19:112–122
van Maldegem F, de Wit M, Morsink F et al (2008) Effects of processing delay, formalin fixation, and immunohistochemistry on RNA recovery from formalin-fixed paraffin-embedded tissue sections. Diagn Mol Pathol 17:51–58
Paska C, Bogi K, Szilak L et al (2004) Effect of formalin, acetone, and RNAlater fixatives on tissue preservation and different size amplicons by real-time PCR from paraffin-embedded tissue. Diagn Mol Pathol 13:234–240
Masuda N, Ohnishi T, Kawamoto S et al (1999) Analysis of chemical modification of RNA from formalin-fixed samples and optimization of molecular biology applications for such samples. Nucleic Acid Res 27:4436–4443
Bussolati G, Annaratone L, Medico E et al (2011) Formalin fixation at low temperature better preserves nucleic Acid integrity. PLoS ONE 6:e21043-e
Xie R, Chung JY, Ylaya K et al (2011) Factors influencing the degradation of archival formalin-fixed paraffin-embedded tissue sections. J Histochem Cytochem 59(4):356–365
von Ahlfen S, Missel A, Bendrat K et al (2007) Determinants of RNA quality from FFPE samples. PLoS ONE 2(12):e1261
Acknowledgments
This work was supported by Ricerca Sanitaria Finalizzata RF-2010-2310674.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Bussolati, G., Annaratone, L., Maletta, F. (2015). The Pre-analytical Phase in Surgical Pathology. In: Dietel, M., Wittekind, C., Bussolati, G., von Winterfeld, M. (eds) Pre-Analytics of Pathological Specimens in Oncology. Recent Results in Cancer Research, vol 199. Springer, Cham. https://doi.org/10.1007/978-3-319-13957-9_1
Download citation
DOI: https://doi.org/10.1007/978-3-319-13957-9_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-13956-2
Online ISBN: 978-3-319-13957-9
eBook Packages: MedicineMedicine (R0)