Abstract
Listeria monocytogenes is a food-borne pathogen of great concern for the food-producing companies. This Gram-positive bacterium is the causative agent of listeriosis, a highly fatal opportunistic food-borne infection. L. monocytogenes causes listeriosis in humans characterised by invasive and noninvasive illness, associated with high mortality (20–30 %) and has a propensity to cause severe problems, especially in pregnant women, neonates, the elderly and immuno-suppressed individuals. Thus, the presence of this pathogen in food is a major concern to the food industry and public health regulators. L. monocytogenes has been involved in numerous outbreaks of listeriosis occurring through consumption of milk and milk products. Hence, there is an urgent need from the dairy industry to understand the introduction of emerging food-borne pathogens in milk, and thus, in turn control and prevention of milk-borne epidemics and outbreaks.
A total of 767 milk samples from dairy cows were taken at different levels of collection and processing and were utilized for the isolation of Listeria. Overall, 10.56 % of the samples were positive for Listeria species and 37 isolates were designated as L. monocytogenes. Pulse-field gel electrophoresis (PFGE) was used to discriminate the L. monocytogenes isolates into 5 ApaI and 4 AscI PFGE patterns (pulsotypes). The ability to carry out epidemiological investigations to determine the primary sources of bacterial contamination is therefore important to improve public health.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
15.1 Introduction
Food safety is at the centre of one’s health as food is an excellent vehicle by which many pathogens can reach an appropriate colonization site in a new host. Many, if not most, of all important zoonoses relate in some way to animals in the food production chain. One of the major issues in food safety over the latest decennial has been the lack of cross-sectoral collaboration across this chain (Wielinga and Schlundt 2012) .
Dairying plays a dynamic role in agro-based economy and milk is a high value source of nutrients for the urban and rural population. Milk as it is secreted by the gland of the mammals is free of microorganisms but can get contaminated with bacteria during or after milking. Mastitis is one of the most economically important diseases affecting the dairy industry and reduces milk production and alters milk composition (Bansal and Gupta 2009). Although many studies are reported on the analysis of milk collected at different stages of processing, data are lacking on the analysis of milk in production chain, i.e. from farm to table (Anon 2011). Hence, there is an urgent need from the dairy industry to understand the introduction of emerging food-borne pathogens in milk and thus in turn control and prevent milk-borne epidemics and outbreaks.
Human illness from milk-borne pathogens is usually associated with consumption of raw milk or products made from raw milk. Occasionally, this has also been linked to pasteurised milk products but these cases usually have been a result of contamination of the product after pasteurisation or improper pasteurisation (Oliver et al. 2005). In the past 20 years, food-borne illnesses from dairy product consumption have been predominantly associated with Salmonella enterica, Campylobacter jejuni, Escherichia coli O157:H7 and Listeria monocytogenes .
The microbiological safety of food remains a dynamic situation heavily influenced by multiple factors. Given the recent spate of food-borne illness outbreaks, Listeria monocytogenes is once again in the spotlight as an important bacterial pathogen (Newell et al. 2011) . Although the number of people infected by food-borne Listeria is comparatively small, this bacterium is one of the leading causes of death from food-borne illness due to its toxin listeriolysin O which is rightly referred to the Swiss army knife of Listeria (Hamon et al. 2012) .
15.2 Listeria spp. and Listeria monocytogenes
Listeria spp. are ubiquitous bacteria widely distributed in the environment (Liu et al. 2006). They are Gram-positive, nonsporulating, facultatively anaerobic rods that measure 1–2 µm in length and 0.5 µm width. Growth occurs between 3 and 50 °C but the optimum temperature is 30–37 °C and they show typical tumbling motility at 20–25 °C (Topley and Wilson 1990) which is a characteristic feature of the organism .
The genus Listeria includes various species such as L. monocytogenes, Listeria ivanovii, Listeria innocua, Listeria welshmeri, Listeria seeligeri, Listeria grayi, Listeria marthii (Graves et al. 2010) , Listeria rocourtiae (Leclercq et al. 2010), Listeria weihenstephanensis (Lang et al. 2013), Listeria fleischmannii (Bertsch et al. 2013) , Listeria floridensis, Listeria aquatica, L. cornellensis, L. riparia and L. grandensis. (Bakker et al. 2014) . Among the 15 species of Listeria,only L. monocytogenes is pathogenic for humans whereas L. ivanovii mainly affects ruminants.
L. monocytogenes is a food-borne opportunistic pathogen of great concern for the food industry and milk-producing companies. Due to its physiological characteristics, such as resistance to acidic and sodium chloride stress, ability to grow at low temperature and possibility to form biofilms (Harvey et al. 2007), it can persist and/or recontaminate food products, thereby representing an important risk for the safety of the consumers (Gardan et al. 2003; Liu et al. 2002; Olesen et al. 2009; Pan et al. 2006) . The term “Listeria hysteria” was coined towards the end of 1980s following a series of listeriosis outbreaks due to the consumption of soft cheese and ready-to-eat (RTE) meats in the UK. Recently, this emerged again in the large outbreaks in Canada caused by deli meats (Warriner and Namvar 2009) and also in USA (Anon 2011). Although human listeriosisoccurs only sporadically (Farber and Peterkin 1991; Schuchat et al. 1991) several outbreakshave been observed during the last two decades (McLauchlin et al. 2004).It is established that food-borne transmission constitutesthe main route of acquisition of listeriosis (Farber and Peterkin 1991). Although the incidence of the first human case of listeriosis was reported by Nyfeldt (1929), it is only since 1981, after the three well investigated listeriosis epidemics, first caused by coleslaw (Schlech et al. 1983), second caused by whole and 2 % fat milk (Fleming et al. 1985) and third caused by consumption of soft Mexican-style cheese (Linnan et al. 1988) that this organism came to be considered as a food-borne pathogen. Multinational outbreak from dairy products was reported by Fretz et al. (2010). L. monocytogenes is composed of at least 12 serovars, i.e. 1/2a, 1/2b, 1/2c, 3a, 3b, 3c, 4a, 4b, 4c, 4d, 4e and 7 (Liu 2006); All 12 serovars of the pathogen are known to cause human listeriosis, but serovars 1/2a, 1/2b and 4b are associated with most of the cases.
15.3 Listeriosis
Listeriosis is a serious invasive bacterial zoonotic disease characterised by neural, visceral and reproductive disorders. It is usually manifested as septicaemia, abortion, stillbirth, meningitis, and meningo-encephalitis in a variety of animals including humans; especially in immunocompromised individuals and persons in contact with animals. It is an important food-borne bacterial disease and a nagging public health hazard caused by ingestion of contaminated food and water. To manage the problem of food-borne listeriosis, it requires an understanding of the burden of the disease on a worldwide scale as food that are prone to contamination are eaten widely domestically and many are traded globally (Todd and Notermans 2011). Listeria spp. including L. monocytogenes are isolated from diverse environmental sources including soil, water, sewage, vegetation (e.g. grass, meadows, forests, silage), wild animal faeces, as well as on the farm and in food-processing facilities (Barbuddhe and Chakraborty 2009; Doijad et al. 2011; Sauders and Wiedmann 2007) .
Listeriosis was first recognized as a disease in 1926 during a spontaneous outbreak of infection among laboratory rabbits and guinea pigs in Cambridge characterised by mononuclear leucocytosis (monocytosis) and the isolated organism was named as “Bacterium monocytogenes” (Murray et al. 1926). Subsequently, in 1927, Pirie isolated a similar bacillus from the liver of infected gerbils and named it Listerella hepatolytica in honour of Lord Lister (Gray and Killinger 1966) . Finally, the genus was named as Listeria in 1940 for taxonomic reasons (McLauchlin 1987).
Although Listeriosis was first recognized as a disease of animals and the link between silage feeding and infection in farm animals has been known for decades, it was the recognition in the 1980s of listeriosis as a food-borne human disease that promised intense research activity (Low and Donachie 1997).
Human listeriosis is a public health problem of low incidence but high mortality, requiring prompt diagnosis and adequate antibiotic therapy. Antibiotic resistance and inefficient empirical treatment of Listeria infections could be responsible for this increased mortality (Rodas-Suárez et al. 2006).
Milk-Borne Listeriosis
The food-borne pathogens in raw milk originate from the farm environment and direct excretion from animals’ infected udder and poor silage quality, whereas, in dairy plants the pathogens may enter via contaminated raw milk, colonize the dairy plant environment and consequently contaminate dairy products. Important sources of contamination during the handling and processing might be the workers as well (Bemrah et al. 1998; Kousta et al. 2010), with Listeria also being shed in the faeces (Van Kessel et al. 2004) . The prolonged excretion of the organism in milk, the apparently normal appearance of the milk in majority cases and the consumption of raw milk, especially on farms, could be important factors in the transmission and epidemiology of Listeria infection. The sources of contamination of Listeria spp. in raw milk are probably insufficient hygiene during milking, storage and transport of milk. L. monocytogenes may directly contaminate milk as a consequence of listerial mastitis, encephalitis or Listeria-related abortion in cattle. Rawool et al. (2007) reported overall occurrence of L. monocytogenes in 0.55 % of 243 cattle and buffaloes with subclinical mastitis in India. The contamination of food by L. monocytogenes occurs along the food chain from farm-to-fork (Farber and Peterkin 1991). The ability of L. monocytogenes to grow at low temperatures is important in the bacterium’s persistence in food-processing environments. Further, biofilm-forming abilities (Di Bonaventura et al. 2008) and sanitizer resistance (Lundén et al. 2003) also contribute to the persistence of L. monocytogenes.
Globally, cases of human listeriosis are on the increase which is evident from the major outbreaks recorded in various countries. The first proof that milk products could be responsible for listeriosis outbreaks was corroborated by Fleming et al.in 1985which involved 49 cases, seven of them in the fetus and 42 in immunocompromised adults. Listeriosis outbreaks have mostly been linked to consumption of raw milk or cheese made of unpasteurized milk (Fleming et al. 1985; Linnan et al. 1988; Lyytikäinen et al. 2000; Rebagliati et al. 2009).
When cattle are infected with L. monocytogenes, the organism is excreted in the milk. L. monocytogenes is quite resistant to heat and milk’s postpasteurisation storage at a refrigeration temperature might allow the selective growth of the remaining organisms (Dalton et al. 1997). Extensive work has been ongoing in many countries during the last decade to prevent outbreaks and decrease the incidence of listeriosis (Rossi et al. 2008).
The occurrence of listeric infections in the Indian subcontinent has been extensively reviewed by Malik et al. (2002). In Indian context, few studies have been carried out to study the incidence of Listeria in food. L. monocytogenes was isolated from 8.1 % of raw milk samples (Bhilegaonkar et al. 1997) . L. monocytogenes could not be isolated from pasteurised bulk milk tanks. Isolation of pathogenic L. monocytogenes strains was reported from milk of 1.56 % goats (Barbuddhe et al. 2000) and 6.25 % buffaloes (Barbuddhe et al. 2002). In an extensive study involving central India, Listeria spp. were isolated from 139 (6.75 %) samples out of 2060 samples collected from dairy cows; 105 (5.1 %) were positive for L. monocytogenes (Kalorey et al. 2008). Aurora et al. (2008) analysed milk (471) and RTE indigenous milk products (627) and detected L. monocytogenes isolates. L. monocytogenes has been isolated from cases of mastitis, reproductive disorders and septicaemia in animals (Shakuntala et al. 2006; Rawool et al. 2007).
15.3.1 Symptoms of Listeriosis
L. monocytogenes causes two forms of listeriosis : noninvasive gastrointestinal listeriosis and invasive listeriosis (Allerberger and Wagner 2010) . L. monocytogenes infects normally sterile parts of the body such as liver, spleen, cerebro-spinal fluid and blood, and most cases end up being hospitalized (Todd and Notermans 2011). Persons with a predisposed condition, linked to decreased level of cell-mediated immunity such as individuals with cancer malignancies, organ transplant, liver disease, HIV/AIDS and diabetes are more prone to infection and can develop sepsis, meningitis and serious infections affecting the nervous system (Allerberger and Wagner 2010) .
In healthy adults, disease is mainly diarrhoea and fever. In pregnant women fever, diarrhoea, abortion or stillbirth are common; newborns get sepsis, pneumonia or meningitis (Todd and Notermans 2011). Most cases of confirmed listeriosis fall into the ageing category, especially over 65 years old. Case-fatality rates can be high (20–30 %). It is estimated that 10 % of the population in the developed world carry the bacterium in their gastrointestinal tract (Swaminathan and Gerner-Smidt 2007) .
15.4 Isolation of Listeria Species
Meat, poultry and dairy products have been most frequently implicated as vehicles of transmission. Large outbreaks are usually linked to errors in food-processing plants, such as contaminated slicing machines, followed by opportunities for growth of the pathogen (Todd and Notermans 2011). A number of methods and media currently exist for the detection and enumeration of L. monocytogenes. For the isolation of L. monocytogenes from foods, animals/human clinical samples and environmental samples, the use of enrichment cultures followed by selective plating is required (Curtis and Lee 1995) . The Food and Drug Administration (FDA) Bacteriological and Analytical Method (BAM), and the International Organization for Standardization (ISO) 11290 method (Barbuddhe et al. 2008) are the most widely used culture reference methods for detection of Listeria in all foods. Other methods, like the United States Department of Agriculture (USDA) and the Association of Analytical Chemists (AOAC) are also used.
15.4.1 Enrichment Procedure/Media
Isolation of Listeria from complex samples, such as food, environmental and stool samples, containing abundant background flora and a low number of Listeria, requires enrichment. The earliest method available was the cold enrichment technique (Gray et al. 1948). This required inoculation of the sample into a nutrient broth lacking selective agents, followed by incubation at 4 °C for long periods. However, the method was time consuming and has subsequently been replaced by methods involving selective enrichment and selective plating based on the inhibition of the growth of background flora by adding inhibitory agents such as lithium chloride, nalidixic acid, acriflavine, cefotetan, ceftazidime, colistin, cycloheximide, fosfomycin and polymyxin B (Gasanov et al. 2005).
A number of media such as polymixin acriflavin lithium chloride ceftazidime aesculin mannitol egg yolk (L-PALCAMY; Van Netten et al. 1989) , Lovett (FDA; Lovett et al. 1987), University of Vermont Medium (UVM; Donnelly and Baigent 1986) and Fraser broth (Fraser and Sperber 1988) were developed.
The ISO 11290 method employs a two-stage enrichment process: the first enrichment in half Fraser broth (Fraser and Sperber 1988) for 24 h, followed by transfer of an aliquot to full-strength Fraser broth for further enrichment. In the FDA BAM method, the sample (25 g) is enriched for 48 h at 30 °C in Listeria enrichment broth (LEB; Lovett et al. 1987) containing the selective agents acriflavin and nalidixic acid, and the antifungal agent cycloheximide. The USDA and the AOAC/International Dairy Federation (IDF) methods use a modification of UVM (Donnely and Baigent 1986) containing acriflavin and nalidixic acid for primary enrichment. The USDA method was designed and has been officially recommended primarily for meat and poultry products and the FDA method was designed for processing dairy products (Brackett and Beuchat 1989) .
15.4.1.1 Selective or Differential Plating Media
A number of media have been developed which include Oxford agar (Curtis et al. 1989) ; lithium chloride–ceftazidime agar (LCAM; Lachica 1990); polymixin–acriflavin–lithium chloride–ceftazidime–asculin–mannitol (PALCAM) agar (Van Netten et al. 1989); Dominguez-Rodriguez isolation agar (DRIA; Dominguez-Rodriguez et al. 1984); Dominguez-Rodriguez Listeria selective agar medium, modified (LSAMm agar; Blanco et al. 1989) ; modified Vogel Johnson agar (MVJ; Buchanan et al. 1989) and MVJ modified further (MVJM; Smith and Buchanan 1990) . L. monocytogenes blood agar (LMBA) is a a very useful tool to detect L. monocytogenes.
15.4.1.2 Chromogenic Media
The chromogenic media commercially available include Agar Listeria according to Ottaviani and Agosti (ALOA), the BCM L. monocytogenes detection system, CHROM agar, and rapid L. monocytogenes. Chromogenic media are simple, cost effective and easy to interpret (Gasanov et al. 2005). ALOA is both a selective and differential medium for the isolation of Listeria spp. and presumptive identification of L. monocytogenes (Ottaviani et al. 1997). ALOA was found to be superior to Oxford and PALCAM when samples containing both L. monocytogenes and L. innocua were examined (Vlaemynck et al. 2000) .
15.4.2 Differentiation of Listeria Species
Conventionally, the identification of Listeria spp. have relied on the results of fermentation of sugars and haemolytic reactions (Seeliger and Jones 1986), and the commercially available API Listeria identification kit (Bille et al. 1992) .
Differentiation of innocua and monocytogenes (DIM), a test based on the detection of acrylamidase present in L. innocua strains and in majority of other non- L. monocytogenes listerial strains but absent in L. monocytogenes can easily and clearly differentiate L. innocua and other Listeria strains from L. monocytogenes (Bille et al. 1992) . All species of Listeria except L. monocytogenes produce amino acid peptidase activity on alanine substituted substrates (Kämpfer 1992). This reaction has been modified by using DL-alanine ß-napthylamide (DLABN) as the substrate and has successfully been carried out for identification of Listeria within 5 h (Clark and McLaughlin 1997; McLauchlin 1997) . However, despite the availability of alternative identification techniques, conventional and haemolytic reactions are most commonly used (McLauchlin 1997).
15.4.3 Detection of Listeria Species
L. monocytogenes and other Listeria species closely resemble morphologically and biochemically and the clinical manifestations of listeriosis are nonspecific (Vázquez-Boland et al. 2001). Therefore, rapid, specific and sensitive diagnostic tests capable of distinguishing L. monocytogenes from other Listeria species are essential for the effective control of the disease (Liu 2006).
Detection and enumeration of L. monocytogenes from environments such as food, which can be heavily contaminated with other organisms, are often difficult (Golden et al. 1988) . The L. monocytogenes demonstrates strain variations in virulence and pathogenicity (Liu et al. 2003; Roche et al. 2003). Therefore, the ability to determine accurately and rapidly the pathogenic potential of L. monocytogenes isolates is essential to limit the spread of listeriosis and reduce unnecessary recalls of food products. The pathogenic potential of Listeria isolates can be assessed by in vitro pathogenicity tests like β-haemolysis on sheep or horse blood agar (Schonberg 1989), phosphatidylinositol-specific phospholipase C (PI-PLC) assay (Notermans et al. 1991b) and by the use of chromogenic media (Greenwood et al. 2005), and by in vivo methods namely, chick embryo and mouse inoculation (Menudier et al. 1991). The in vivo methods remain objectionable from an ethical point of view and need skilled personnel to perform. Therefore, the application of molecular techniques has facilitated the identification and characterisation of L. monocytogenes (Liu 2006). Among the several approaches to nucleic acid amplification, The polymerase chain reaction (PCR) was the first and remains the most widely applied technique in both research and clinical laboratories (Liu 2006).
A number of factors have been shown to be associated with the virulence of L. monocytogenes (Portnoy et al. 1992) . The haemolysin gene, hly, was the first virulence determinant to be identified and sequenced in Listeria spp. Subsequently, the virulencegene cluster in which most of the genetic determinants requiredfor the intracellular life cycle of pathogenic Listeria spp. residewas discovered(Vázquez-Boland et al. 2001). The listeriolysin O(LLO)-encoding gene (hlyA) is present only in virulent strains of the species and is required for virulence. LLO is a secreted protein toxin that can be detected easily with the use of blood agar or haemolysis assays, and it is well characterised and understood (Churchill et al. 2005) . A strong correlation between haemolytic activity and pathogenicity in the genus Listeria has been demonstrated (Seeliger and Jones 1986; Skalka et al. 1982).
Differentiation of L. ivanovii from L. monocytogenes and other Listeria species can be achieved by its production of a wide, clear or double zone of haemolysis on sheep or horse blood agar, a positive Christie–Atkins–Munch-Petersen (CAMP) reaction with Rhodococcus equi but not with haemolytic Staphylococcus aureus (Rocourt and Catimel 1985) . A positive CAMP reaction or fermentation of rhamnose and nonfermentation of xylose can be used to identify pathogenic Listeria spp. with the exception of L. seeligeri which is haemolytic but nonpathogenic (Seeliger and Jones 1986).
Pathogenic Listeria spp. exhibit three different enzymes with phospholipase C (PLC) activity, PlcA and PlcB activities are shown by L. monocytogenes and SmcL is specific to L. ivanovii (Vázquez-Boland et al. 2001). The activity of virulence factor called phosphatidylinositol-specific phospholipase C (PI-PLC), encoded by the plcA gene, has been reported to be expressed by the pathogenic species of Listeria (Notermans et al. 1991b) . The plcA-deficient strains have been reported to be less virulent in mice (Camilli et al. 1991) .
A chromogenic medium (ALOA) has been developed based on PI-PLC activity (Ottaviani et al. 1997). ALOA medium has proven to be a useful and significantly better assay than other media for the differentiation of L. monocytogenes from nonpathogenic Listeria species (Vlaemynck et al. 2000; Beumer and Hazeleger 2003) . All the Listeria species form bluish green colonies due to the presence of a chromogenic compound X-glucosidase which detects β-glucosidase. Further, pathogenic Listeria spp. can be distinguished from other Listeria species through the production of opaque halo around the colonies (Ottaviani et al. 1997).
Virulence of L. monocytogenes for humans has been correlated with pathogenicity in mice (Mainou-Fowler et al. 1988), particularly in immuno-compromised mice (Stelma et al. 1987). Mice inoculation is capable of providing an in vivo measurement of all virulent determinants; therefore, it is regarded as the gold standard for any newly developed tests for L. monocytogenes virulence (Liu et al. 2003; Roche et al. 2001). The mouse virulence assay is conducted by inoculating mice with various doses of L. monocytogenes via the oral, nasal, intraperitoneal, intravenous or subcutaneous routes. The virulence of a given L. monocytogenes strain is determined by the mouse mortality resulting from infection, or by the number of L. monocytogenes bacteria that reach the spleen following experimental infection (Liu 2006).
Inoculation of chick embryos with pathogenic Listeria species through chorioallantoic (CAM) route may cause death of embryo within 72 h while nonpathogenic species fail to do so (Terplan and Steinmeyer 1989), and the test has been reported to agree with mouse bioassay (Notermans et al. 1991a) . Because of nonspecific deaths, yolk sac route inoculation has been found to be less suitable than the CAM challenge for assessing virulence (Notermans et al. 1991a) .
An array of virulence-associated genes associated with the pathogenicity of Listeria spp., include plcA encoding phosphatidylinositol phospholipase-C (PI-PLC), plcB encoding phosphatidycholine phospholipase-C, hlyA encoding a haemolysin, mpl encoding a metalloprotease and actA encoding the surface actin polymerisation protein ActA. All these genes are physically linked in a 9 kb chromosomal island referred to as Listeria pathogenicity island-1 (LIPI-1; Vázquez-Boland et al. 2001).
One of the biggest problems associated with the detection of L. monocytogenes is the low numbers at which the bacteria are normally found in contaminated food samples (Hoffman and Weidmann 2001). DNA-based methods of detection employ ways of amplifying the specific genetic signals from a few cells. PCR is the basis of many nucleic acid-based detection systems (Churchill et al. 2005) . Among the target genes for PCR detection of L. monocytogenes are the hlyA gene (Norton et al. 2001; Thimothe et al. 2004) , the iap gene (Cocolin et al. 2002) , inlB (encoding internalin B; Lunge et al. 2002) and 16S rRNA (Call et al. 2003). Among these genes, the hlyA gene has been most commonly used (Aznar and Alarcón 2002) .
Multiplex PCR is a variation of the traditional PCR. This method makes use of multiple sets of primers to amplify a number of genes or gene fragments simultaneously (Churchill et al. 2005) . An mPCR assay employing four genes, the hlyA, plcA, iap and actA for the detection of L. monocytogenes from clinical samples has been developed (Kaur et al. 2007). Rawool et al. (2007) detected multiple virulence-associated genes (the plcA, prfA, hlyA, actA and iap) in L. monocytogenes isolated from bovine mastitis cases. The development of PCR-based serotyping procedures, such as the use of group-specific PCR primers, has provided additional tools for the identification and grouping of L. monocytogenes (Borucki and Call 2003; Doumith et al. 2004) .
Use of real-time PCR in a 96-well PCR format eliminates the need for agarose gel electrophoresis. In this method, a fluorescent dye, such as SYBR Green I is used to follow the PCR amplification in real-time and can be used to detect the amplified products from a number of genes at the same time (Bhagwat 2003) . Primers for real-time PCR can be designed to simultaneously detect both Listeria spp. and L. monocytogenes by amplifying the 23S rRNA gene (conserved in all Listeria spp.) at the same time as the hlyA gene (Rodríguez-Lázaro et al. 2004). Real-time PCR can be used with the proper primers to quantify the number of pathogens present in a sample by measuring the level of fluorescence as compared to a standard. The adaptation of conventional PCR to the reverse transcription PCR (RT-PCR) format also permits the detection of viable L. monocytogenes organisms in specimens (Liu 2006).
The development of a 10-min assay based on matrix-assisted laser desorption/ionisation-time of flight (MALDI-TOF) spectroscopy directly from colonies on agar plates has been reported. The method allows not only discrimination between pathogenic and nonpathogenic Listeria spp. but also permits resolution up to the level of the PCR serotype analysis (Barbuddhe et al. 2008) . Nevertheless, high cost of the capital equipment involved, despite being offset by cheap running costs of the assay, puts this method beyond the means of smaller diagnostic laboratories.
15.5 Subtyping of Listeria Species
L. monocytogenes is a ubiquitous organism and exhibits diversity of strains. The subtyping procedures are used to track individual strains involved in listeriosis outbreaks, and to examine the epidemiology and population genetics of L. monocytogenes. The subtyping is integral to control and prevention programmes aimed at listeriosis. Two major subtyping approaches are in common use: phenotypic and genotypic (molecular or DNA subtyping).
The choice of a method depends most on the performance criteria of the method, such as typeability, discriminatory power, reproducibility, rapidity and ease of use and the purpose of subtyping, e.g. phylogenetic analysis, epidemiological surveillance, outbreak investigations or food-processing contamination analysis (Struelens et al. 1996) .
L. monocytogenes can be classified into four lineages: lineage I encompasses serotypes 1/2b, 3b, 4b and 3c; lineage II includes serotypes 1/2a, 1/2c, 3a, lineage III comprises serotypes 4a, 4b and 4c and lineage IV comprises 4a, 4b, 4c (Orsi et al. 2011). Several subtyping procedures including serotyping, multilocus enzyme electrophoresis (MLEE), DNA restriction endonuclease analysis, ribotyping, DNA sequencing-based subtyping techniques, e.g. multilocus sequence typing (MLST) and PFGE have been developed for L. monocytogenes (Borucki and Call 2003; Liu 2006) . Serotyping may potentially be useful for tracking L. monocytogenes strains involved in disease outbreaks. Indeed, it has been observed that L. monocytogenes serotypes 1/2a, 1/2b and 4b are responsible for 98 % of documented human listeriosis cases, whereas serotypes 4a and 4c are rarely associated with outbreaks of the disease (Wiedmann et al. 1996; Jacquet et al. 2002) . The development of PCR-based serotyping procedures has provided additional tools for the identification and grouping of L. monocytogenes (Borucki and Call 2003; Doumith et al. 2004).
15.5.1 Phenotypic Methods
Phenotypic methods often have a low power of discrimination in strains, suffer from biologic variability (e.g. phage typing), and may not be applicable to all strains (Graves et al. 1999) . Serotyping has been a classical tool in subtyping of L. monocytogenes. Based on somatic (O) and flagellar (H) antigens, L. monocytogenes strains are divided into 12 serotypes: 1/2a, 1/2b, 1/2c, 3a, 3b, 3c, 4a, 4b, 4c, 4d, 4e and 7 (Seeliger and Höhne 1979). The major drawbacks of serotyping include cost, availability and standardization of reagents, as well as the technical expertise needed to perform the assay (Borucki and Call 2003) . The usefulness of serotyping in epidemiological investigations is limited as more than 95 % of strains isolated from human cases and foods belong to serotypes 1/2a, 1/2b and 4b (Liu 2006). The enzyme-linked immunosorbent assay (ELISA) method of serotyping described by Palumbo et al. (2003) is a cost-effective method. The reduced variability of the antiserum quality by using a commercially available antisera and also the reduction of inconsistencies in judgement associated with weakly agglutinating antigen–antiserum combinations are overcome by this method (Palumbo et al. 2003). Studies have found that serotype 1⁄2a was the predominant serotype of L. monocytogenes food and environmental isolates (Corcoran et al. 2006; Gilbreth et al. 2005; Lukinmaa et al. 2003) .
Phage typing has been shown to be an efficient method for large-scale subtyping of L. monocytogenes (Audurier and Martin 1989) , and a standard phage set with a standardized method has been described (McLauchlin et al. 1996). Even though phage typing shows high discrimination power, the high number of strains remains nontypeable (Rocourt and Catimel 1985) .
Multi locus enzyme electrophoresis (MLEE) is a protein-based, isoenzyme typing method that correlates specific protein band patterns with genotypes (Liu 2006).
15.5.2 Genotypic Methods
PFGE is a molecular subtyping method that has been successfully used to characterise L. monocytogenes isolates (Kerouanton et al. 2010; Mammina et al. 2009) and is considered to be the gold standard subtyping method because of the documented reproducibility in previous epidemiological studies and its high discriminatory power (Autio et al. 2002; Graves and Swaminathan 2001) . Ribotyping is based on the use of nucleic acid probes targeting ribosomal genes after restriction enzyme analysis of chromosomal DNA (Grimont and Grimont 1986) . Automated ribotyping was previously used for rapid subtyping L. monocytogenes for source tracking, population genetics-based studies, and epidemiological investigations (Wiedmann 2002) ; however, it is expensive and not as discriminatory as PFGE (Inglis et al. 2003). PFGE provides sensitive subtype discrimination and is often considered the standard subtyping method for L. monocytogenes (Graves and Swaminathan 2001). However, this method is not automated and is labour intensive. Even recently developed rapid protocols take approximately 30 h to perform (Graves and Swaminathan 2001) . Computer-assisted data analysis of large and diverse PFGE type databases can improve the correct interpretation of subtyping data in epidemiological studies and in tracing routes and sources of contamination in the food industry (Neves et al. 2008) .
The application of PFGE in the characterisation of L. monocytogenes isolated from the food can provide a significant insight into the presence of endemic strains and valuable information on potential sites of cross-contamination. Epidemiological tracking of strains over a period of time is required to enable more precise identification of sites of cross-contamination, or critical control points, and to enable to take some measures to avoid the persistence of individual strains within the processing environment.
Several typing methods involving PCR have been developed. The methods employ either just PCR amplification or random amplified polymorphic DNA-PCR (RAPD-PCR) amplification is performed either before polymerase chain reaction-restriction enzyme analysis (PCR-REA) or after amplified fragment length polymorphism (AFLP) restriction enzyme analysis. RAPD is more economical and faster than other typing methods and is particularly suitable for testing fewer than 50 strains (Liu 2006). It employs short (9–10 bp) primers with sequences chosen at random, thus prior sequence knowledge of template DNA is not needed. A total of 30 L. monocytogenes isolates from human patients and food originated from two different geographic locations without any epidemiological relations showed 92–99 % genetic homogeneity and contained virulence genes, inlA, inlB, actA, hlyA, plcA and plcB (Jaradat et al. 2002) .
A rapid multiplex PCR serotyping assay has been developed which separated the four major L. monocytogenes serovars (1/2a, 1/2b, 1/2c and 4b) into distinct groups (Doumith et al. 2004, 2005). Serotyping of 145 L. monocytogenes isolates revealed serovar 1/2a to be the most frequent (57.4 %) followed by 4b (14.1 %, 1⁄2b (9.7 %) and 4c (4.4 % and 1⁄2c (6.7 %).
15.6 Studies on Listeria spp. from Milk Samples in Goa
15.6.1 Isolation and Characterisation
A total of 767 milk samples from dairy cows were taken at different levels of collection and processing (udder, from milking utensils/cans, dairy cooperative society, receiving dock and market) and were processed for the isolation of Listeria as per the USDA method described by McClain and Lee (1988) after making necessary modifications. Double enrichment of the samples was carried out using UVM medium. The enriched inoculum from UVM-2 was streaked on PALCAM agar (Himedia Labs, Mumbai, India). The inoculated plates were incubated at 37 °C for 24–48 h. From the isolation media, suspected colonies of Listeria were subcultured on 5 % sheep blood agar. Morphologically typical colonies were verified by Gram’s staining, catalase and oxidase reaction, tumbling motility at 25 °C, methyl red-Voges Proskauer (MR-VP) reactions, fermentation of sugars (rhamnose, xylose, mannitol and α-methyl- D-mannopyranoside), hemolysis and Christie-Atkins Munch Petersen (CAMP) test with S. aureus and Rhodococcus equi.
The grey green colonies with black sunken centres from PALCAM (Fig. 15.1), Gram-positive, coccobacillary forms (Fig. 15.2) with characteristic tumbling motility at 20–25 °C were considered as to be of Listeria. Overall, 10.56 % of the samples (81 of 767) were positive for Listeria species. The catalase positivity and oxidase negativity was observed in all the 81 isolates. On further testing, 37 isolates produced acid from rhamnose and Α-methyl D-mannopyranoside but not from xylose, and therefore were tentatively designated as L. monocytogenes.
On streaking of 81 confirmed Listeria isolates onto 5 % sheep blood agar, a varying degree of haemolysis was observed (Fig. 15.3) and a total of 38 isolates showed haemolysis. Unlike a typical β-haemolysis with broad and clear zones exhibited by the isolate of L. ivanovii, the degree of haemolysis shown by L. monocytogenes isolates was moderate.
The 81 Listeria isolates from milk were then analysed by CAMP test. 37 isolates showed characteristic enhancement of haemolytic zone with S. aureus indicating the presence of L. monocytogenes while one isolate showed enhanced haemolytic zone typically with R. equi confirming the presence of L. ivanovii (Fig. 15.4).
Agar Listeria according to Ottaviani and Agosti (ALOA) assay, an alternative way to assess phophatidyl inositol phospho lipase C activity (PI-PLC) was carried out using chromogenic ALOA (Himedia, Mumbai, India) medium which helps to differentiate pathogenic Listeria spp. From nonpathogenic ones. (Ottaviani et al. 1997). Out of the 81 isolates of Listeria, 38 isolates exhibited halo formation on ALOA (Fig. 15.5). The enzymatic activity expressed by L. monocytogenes isolates on ALOA agar was reckoned as high (with 8–9 mm zones), moderate (with 5–6 mm zones) and low (with > 4 mm zone) in case of 11, 18 and 8 isolates, respectively. The only isolate of L. ivanovii showed a low enzymatic activity.
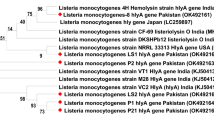
Among the virulence genes of Listeria, hemolysin gene (hlyA) of L. monocytogenes has been used most commonly for confirmation of the isolates (Aznar and Alarcón 2002) . All the isolates were subjected to PCR assay for amplification of the hlyA gene as per the method described by Paziak-Domańska et al. (1999) and Notermans et al. (1991b). Out of 81 Listeria isolates, the hlyA gene was detected in 37 isolates while all the other Listeria spp. were negative in PCR analysis. Amplification of the hlyA gene of L. monocytogenes to its respective 456 bp product represented by a single band in the corresponding region of the DNA marker ladder is as presented in Fig. 15.6.
15.6.2 Serotyping by Multiplex PCR
Typing of L. monocytogenes is important in epidemiological studies for investigation of food-borne outbreaks and in the food-processing environment, to identify the sources of contamination and routes of dissemination. Serotyping by multiplex PCR (mPCR) has been developed which separates the four major L. monocytogenes serovars into distinct groups (Doumith et al. 2004, 2005). This assay was employed in the present investigation to serotype L. monocytogenes isolates recovered from milk. The genomic DNA of all the isolates was extracted using bacterial DNA extraction kit (Chromous Biotech, Bangalore, India) and were subjected to mPCR- based serotyping. The five primer sets for target fragments from genes lmo0737, lmo1118, ORF2819, ORF2110 and prs were synthesized by Sigma Aldrich, USA (Table 15.1).
Out of 37 L. monocytogenes isolates, a larger proportion of isolates (26) belonged to the group corresponding to serovars 1/2a, 1/2c, 3a, and 3c. Serogroup corresponding to serovars 4b, 4d and 4e was detected in two strains while serogroup 1/2b, 3b, 4b, 4d, and 4e was detected in nine strains (D’Costa et al. 2012). The profiles of multiplex PCR serotyping of standard Listeria strains and L. monocytogenes isolates recovered from milk are as depicted in Fig. 15.7. Our data showed that most of the isolates belonged to 1/2a, which was considered as a sporadic cause for human listeriosis (Liu 2006). Studies have also found that serotype 1⁄2a was the predominant serotype of L. monocytogenes food and environmental isolates (Corcoran et al. 2006; Gilbreth et al. 2005; Lukinmaa et al. 2003) . Our earlier studies indicated predominance of L. monocytogenes serotype 4b in human clinical isolates (Kalekar et al. 2011) and 1/2a in isolates from milk-processing environments (Doijad et al. 2011). The observation indicates the potential of milk and milk products to serve as vehicles of transmission of virulent L. monocytogenes.
15.6.3 Pulsed-Field Gel Electrophoresis (PFGE)
PFGE is considered the gold standard method for subtyping food-borne pathogens, because of its high discriminatory power and reproducibility and is currently used by several public and private laboratories for subtyping and serogrouping L. monocytogenes. A total of 36 Listeria isolates were subjected to PFGE analysis to cover different sampling areas and different species. PFGE was performed according to the CDC PulseNet standardized procedure (Graves and Swaminathan 2001) used for typing L. monocytogenes by using the CHEF-DRII apparatus (Bio-Rad Laboratories, Hercules, USA).
PFGE discriminated the L. monocytogenes isolates into 5 ApaI and 4 AscI PFGE patterns (pulsotypes) at 80 % similarity, but could differentiate serovars within multiplex PCR (MPCR) serogroups, in which isolates from different serovars displaying the same pulsotype were found.
Dendrogram analysis showed that PFGE yielded a good binary division into genetic lineages I (serotypes 1/2b, 3b, 4b, and 4e) and II (serotypes 1/2a, 1/2c, 3a and 3c) a result that is consistent with previous studies (Gilbreth et al. 2005; Nadon et al. 2001) and further confirm that these two lineages represent distinct subgroups. Our data also showed that there was a nearly complete correlation between pulsotypes and serotypes with identical PFGE patterns belonging to the same serotype.
15.7 Conclusions and Future Prospects
Based on the results, it can be concluded that enzymatic assays like CAMP and ALOA tests simultaneously with PCR targeting hlyA gene, serotyping by multiplex PCR and PFGE dendrograms can be used for confirming and comparing the pathogenic strains of L. monocytogenes.
Farm animals can be asymptomatic or suffer from encephalitis, septicaemia and abortions and thus may be a source of L. monocytogenes in the farm environment. Managing the problem of milk-borne listeriosis requires an understanding of the burden of the disease on a worldwide scale as milk that is prone to contamination is consumed widely domestically and traded globally. Surveillance of the disease, caused by L. monocytogenes, is typically restricted to developed countries, but many of these do not consider listeriosis as a notifiable disease and estimate the numbers by other means.
Studies on microbiological surveillance of milk and milk products at farm level may help in management and stamping of herds as clean. Human illness attribution has been recently recognized as an important tool to better inform food safety decisions. All dairy farmers, suppliers to dairy farmers, milk carriers, dairy product and food manufacturers, distributors and retailers should be part of an integrated food safety and quality assurance management system. Good farming practices underpin the marketing of safe, quality-assured milk-based products. Good dairy-farming practices should contribute to ensuring that milk and milk products are safe and suitable for their intended use.
References
Allerberger, F., & Wagner, M. (2010). Listeriosis: A resurgent foodborne infection. Clinical Microbiology and Infection, 16, 16–23.
Anon. (2011). Deadliest U.S. foodborne illness outbreaks. Food saftey news. Accessed 8 Nov 2011.
Audurier, A., & Martin, C. (1989). Phage typing of Listeria monocytogenes. International Journal of Food Microbiology, 8, 251–257.
Aurora, R., Prakash, A., Prakash, S., Rawool, D. B., & Barbuddhe, S. B. (2008). Comparison of PIPLC based assays and PCR alongwith in-vivo pathogenicity tests for rapid detection of pathogenic Listeria monocytogenes. Food Control, 19, 641–647.
Autio, T., Lundén, J., Fredriksson-Ahomaa, M., Björkroth, J., Sjöberg, A. M., & Korkeala, H. (2002). Similar Listeria monocytogenes pulsotypes detected in several foods originating from different sources. International Journal of Food Microbiology, 77, 83–90.
Aznar, R., & Alarcón, B. (2002). On the specificity of PCR detection of Listeria monocytogenes in food: A comparison of published primers. Systematic and Applied Microbiology, 25, 109–119.
Bakker, H., Warchocki, S., Wright, E., Allred, A., Ahlstrom, C., Manuel, C., Stasiewicz, M., Burrell, A., Roof, S., Strawn, L., Fortes, E., Nightingale, K., Kephart, D., & Wiedmann, M. (2014). Five new species of Listeria (L. floridensis sp. nov, L. aquatica sp. nov., L. cornellensis sp. nov. L. riparia sp. nov., and L. grandensissp. nov.) from agricultural and natural environments in the United States. International Journal of Systems Evolutionary Microbiology, 64(Pt 6), 1882–1889.
Bansal, B. K., & Gupta, D. K. (2009). Economic analysis of Bovine Mastitis in India and Punjab – A Review. Ind. J. Dairy Sci., 62, 337–344.
Barbuddhe, S. B., & Chakraborty, T. (2009). Listeria as an enteroinvasive gastrointestinal pathogen. Current Topics in Microbiology and Immunology, 337, 173–195.
Barbuddhe, S. B., Malik, S. V. S., Bhilegaonkar, K. N., Prahlad, K., & Gupta, L. K. (2000). Isolation of Listeria monocytogenes and anti-listeriolysin O detection in sheep and goats. Small Ruminant Research, 38, 151–155.
Barbuddhe, S. B., Chaudhari, S. P., & Malik, S. V. S. (2002). The occurrence of pathogenic Listeria monocytogenes and antibodies against listeriolysin O in buffaloes. Journal of Veterinary Medicine, 49, 181–184.
Barbuddhe, S. B., Maier, T., Schwarz, G., Kostrzewa, M., Domann, E., Chakraborty, T., & Hain, T. (2008). Rapid identification and typing of Listeria species using matrix assisted laser desorption ionisation-time of flight mass spectrometry. Applied and Environmental Microbiology, 74, 5402–5407.
Bemrah, N., Sanaa, M., Cassin, M. H., Griffiths, M. W., & Cerf, O. (1998). Quantitative risk assessment of human listeriosis from consumption of soft cheese made from raw milk. Preventive Veterinary Medicine, 37, 129–145.
Bertsch, D., Rau, J., Eugster, M. R., Haug, M. C., Lawson, P. A., Lacroix, C., & Meile, L. (2013). Listeria fleischmannii sp. nov., isolated from cheese. International Journal of Systematic and Evolutionary Microbiology, 63, 526–532.
Beumer, R. R., & Hazeleger, W. C. (2003). Listeria monocytogenes: Diagnostic problems. FEMS Immunology and Medical Microbiology, 35, 191–197.
Bhagwat, A. A. (2003). Simultaneous detection of Escherichia coli O157:H7, Listeria monocytogenes and Salmonella strains by real-time PCR. Internatioanl Journal of Food Microbiology, 84, 217–224.
Bhilegaonkar, K. N., Kulshreshtha, S. B., Kapoor, K. N., Kumar, A., Agarwal, R. K., & Singh, B. R. (1997). Isolation of Listeria monocytogenes from milk. Journal of Food Science and Technology, 34, 248–250.
Bille, J., Catimel, B., Bannerman, E., Jacquet, C., Yersin, M. N., Caniaux, I., Monget, D., & Rocourt, J. (1992). API Listeria, a new and promising one-day system to identify Listeria isolates. Applied Environmental Microbiology, 58, 1857–1860.
Blanco, M. B., FernandezGarayzabal, J. F., Dominguez, L., Briones, V., VazquezBoland, J. A., Blanco, J. L., Garcia, J. A., & Suarez, G. (1989). A technique for the direct identification of haemolytic pathogenic Listeria on selective plating media. Letters in Applied Microbiology, 9, 125128.
Borucki, M. K., & Call, D. R. (2003). Listeria monocytogenes Serotype Identification by PCR. Journal of Clinical Microbiology, 41, 5537–5540.
Brackett, R. E., & Beuchat, L. R. (1989). Methods and media for the isolation and cultivation of Listeria monocytogenes from various foods. International Journal of Food Microbiology, 8, 219–223.
Buchanan, R. L., Stahl, H. G., Bencivingo, M. M., & Corral, F. D. (1989). Comparison of lithium chloridepheny lethanolmoxalactum and modified Vogel Johnson agars for detection of Listeria spp. in retail level meats, poultry and sea food. Applied and Environmental Microbiology, 55, 599603.
Call, D. R., Borucki, M. K., & Loge, F. J. (2003). Detection of bacterial pathogens in environmental samples using DNA microarrays. Journal of Microbiological Methods, 53, 235–243.
Camilli, A., Goldfine, H., & Portnoy, D. A. (1991). Listeria monocytogenes mutants lacking phosphatidylinositol specific phospholipase-C are avirulent. Journal of Experimental Medicine, 173, 751–754.
Churchill, R. L., Lee, H., & Hall, J. C. (2005). Detection of Listeria monocytogenes and the toxin listeriolysin O in food. Journal of Microbiological Methods, 64, 141–170.
Clark, A. G., & McLaughlin, J. (1997). Simple color tests based on an alanyl peptidase reaction which differentiate Listeria monocytogenes from other Listeria species. Journal of Clinical Microbiology, 35, 2155–2156.
Cocolin, L., Rantsiou, K., Iacumin, L., Cantoni, C., & Comi, G. (2002). Direct identification in food samples of Listeria spp. and Listeria monocytogenes by molecular methods. Applied and Environmental Microbiology, 68, 6273–6282.
Corcoran, D., Clancy, D., O'Mahony, M., Grant, K., Hyland, E., Shanaghy, N., Whyte, P., McLauchlin, J., Moloney, A., & Fanning, S. (2006). Comparison of Listeria monocytogenes strain types in Irish smoked salmon and other foods. International Journal of Hygiene and Environmental Health, 209, 527–534.
Curtis, G. D. W., & Lee, W. H. (1995). Culture media and methods for isolation of Listeria monocytogenes. International Journal of Food Microbiology, 26, 1–13.
Curtis, G. D. W., Nichols, W. W., & Falla, T. J. (1989). Selective agents for Listeria can inhibit their growth. Letters in Applied Microbiology, 8, 169172.
Dalton, C. B., Austin, C. C., Sobel, J., Hayes, P. S., Bibb, W. F., Graves, L. M., Swaminathan, B., Proctor, M. E., & Griffin, P. M. (1997). An outbreak of gastroenteritis and fever due to Listeria monocytogenes in milk. The New England Journal of Medicine, 336, 100–106.
D’Costa, D., Bhosle, S. N., Dhuri R.B. Kalekar, S., Rodrigues, J., Doijad, S. P., & Barbuddhe, S. B. (2012). The occurrence and characterization of Listeria species isolated from milk production chain. Milchwissenchaft, 67, 43–46.
Di Bonaventura, G., Piccolomini, R., Paludi, D., D’Orio, V., Vergara, A., Conter, M., & Ianieri, A. (2008). Influence of temperature on biofilm formation by Listeria monocytogenes on various food-contact surfaces: Relationship with motility and cell surface hydrophobicity. Journal of Applied Microbiology, 104, 1552–1561.
Doijad, S. P., Barbuddhe, S. B., Garg, S., Kalekar, S., Rodrigues, J., D’Costa, D., Bhosle, S., & Chakraborty, T. (2011). Incidence and genetic variability of Listeria species from three milk processing plants. Food Control, 22, 1900–1904.
Dominguez-Rodriguez, L., Suarez-Fernandez, G., Fernandez-Garayzobal, J., & Rodriguez-Ferri, E. (1984). New methodology for the isolation of Listeria monocytogenes from heavily contaminated environments. Applied and Environmental Microbiology, 47, 1188–1190.
Donnelly, C. W., & Baigent, G. J. (1986). Method for flow cytometric detection of Listeria monocytogenes in milk. Applied and Environmental Microbiology, 52, 689–695.
Doumith, M., Buchrieser, C., Glaser, P., Jacquet, C., & Martin, P. (2004). Differentiation of the major Listeria monocytogenes serovars by multiplex PCR. Journal of Clinical Microbiology, 42, 3819–3822.
Doumith, M., Jacquet, C., Gerner-Smidt, P., Graves, L. M., Loncarevic, S., Mathisen, T., Morvan, A., Salcedo, C., Torpdahl, M., Vazquez, J. A., & Martin, P. (2005). Multicenter validation of a multiplex PCR assay for differentiating the major Listeria monocytogenes serovars 1/2a, 1/2b, 1/2c, and 4b: Toward an international standard. Journal of Food Protection, 68, 2648–2650.
Farber, J. M., & Peterkin, P. I. (1991). Listeria monocytogenes, a food-borne pathogen. Microbiology Reviews, 55, 476–511.
Fleming, D. W., Cochi, S. L., Mackonald, K. L., Brondum, J., Hayes, P. S., Plikaytis, B. D., Holmes, M. B., Audurier, A., Broome, C. V., & Reingold, A. L. (1985). Pasteurised milk as a vehicle of infection in an outbreak of listeriosis. The New England Journal of Medicine , 312, 404407.
Fraser, J. A., & Sperber, W. H. (1988). Rapid detection of Listeria spp. in food and environmental samples by esculin hydrolysis. Journal of Food Protection, 51, 762765.
Fretz, R., Pichler, J., Sagel, U., Much, P., Ruppitsch, W., Pietzka, A. T., Stöger, A., Huhulescu, S., Heuberger, S., Appl, G., Werber, D., Stark, K., Prager, R., Flieger, A., Karpísková, R., Pfaff, G., & Allerberger, F. (2010). Update: Multinational listeriosis outbreak due to ‘Quargel’, a sour milk curd cheese, caused by two different L. monocytogenes serotype 1/2a strains, 2009–2010. Eurosurveillance, 15, 19543.
Gardan, R., Cossart, P., & Labadie, J. (2003). Identification of Listeria monocytogenes genes involved in salt and alkaline-pH tolerance. Applied and Environmental Microbiology, 69, 3137–3143.
Gasanov, U., Hughes, D., & Hansbro, P. M. (2005). Methods for the isolation and identification of Listeria spp. and Listeria monocytogenes: A review. FEMS Microbiology Reviews, 29, 851–875.
Gilbreth, S. E., Call, J. E., Wallace, F. M., Scott, V. N., Chen, Y., & Luchansky, J. B. (2005). Relatedness of Listeria monocytogenes isolates recovered from selected ready-to-eat foods and listeriosis patients in the United States. Applied Environmental Microbiology, 71, 8115–8122.
Golden, D. A., Beuchat, L. R., & Brackett, R. E. (1988). Evaluation of selective direct plating media for their suitability to recover uninjured, heat-injured, and freeze-injured Listeria monocytogenes from foods. Applied Environmental Microbiology, 54, 1451–1456.
Graves, L. M., & Swaminathan, B. (2001). PulseNet standardized protocol for subtyping Listeria monocytogenes by macrorestriction and pulsed-field gel electrophoresis. International Journal of Food Microbiology, 65, 55–62.
Graves, L. M., Swaminathan, B., & Hunter, S. B. (1999). Subtyping Listeria monocytogenes. In E. Ryser & E. Marth (Eds.), Listeria, listeriosis, and food safety (p. 279). New York: Marcel Dekker.
Graves, L. M., Helsel, L. O., Steigerwalt, A. G., Morey, R. E., Daneshvar, M. I., Roof, S. E., Orsi, R. H., Fortes, E. D., Milillo, S. R., Den Bakker, H. C., Wiedmann, M., Swaminathan, B., & Sauders, B. D. (2010). Listeria marthii sp. nov., isolated from the natural environment, Finger Lakes National Forest. International Journal of Systematic and Evolutinary Microbiology, 60, 1280–1288.
Gray, M. L., & Killinger, A. H. (1966). Listeria monocytogenes and listeric infections. Bacteriological. Reviews, 30, 309–382.
Gray, M. L., Stafseth, H. J., Thorp, F. Jr., Sholl, L. B., & Riley, W. F. Jr. (1948). A new technique for isolating Listeria from the bovine brain. Journal of Bacteriology, 55, 471476.
Greenwood, M., Willis, C., Doswell, P., Allen, G., & Pathak, K. (2005). Evaluation of chromogenic media for the detection of Listeria species in food. Journal of Applied Microbiology, 99, 1340–1345.
Grimont, F., & Grimont, P. A. (1986). Ribosomal ribonucleic acid gene restriction patterns as potential taxonomic tools. Annales de l’Institut Pasteur Microbiologie, 137B, 165–175.
Hamon, M. A., Ribet, D., Stavru, F., & Cossart, P. (2012). Listeriolysin O: The Swiss army knife of Listeria. Trends in Microbiology, 20, 360–368.
Harvey, J., Keenan, K. P., & Gilmour, A. (2007). Assessing biofilm formation by Listeria monocytogenes strains. Food Microbiology, 24, 380–392.
Hoffman, A. D., & Wiedmann, M. (2001). Comparative evaluation of culture- and BAX polymerase chain reaction-based detection methods for Listeria spp. and Listeria monocytogenes in environmental and raw fish samples. Journal of Food Protection, 64, 1521–1526.
Inglis, T. J., Clair, A., Sampson, J., O’Reilly, L., Vandenberg, S., Leighton, K., & Watson, A. (2003). Real-time application of automated ribotyping and DNA macrorestriction analysis in the setting of a listeriosis outbreak. Epidemiology and Infection, 131, 637–645.
Jacquet, C., Gouin, E., Jeannel, D., Cossart, P., & Rocourt, J. (2002). Expression of ActA, Ami, InlB, and Listeriolysin O in Listeria monocytogenes of Human and Food Origin. Applied and Environmental Microbiology, 68, 616–622.
Jaradat, Z. W., Schutze, G. E., & Bhunia, A. K. (2002). Genetic homogeneity among Listeria monocytogenes strains from infected patients and meat products from two geographic locations determined by phenotyping, ribotyping and PCR analysis of virulence genes. International Journal of Food Microbiology, 76, 1–10.
Kalekar, S., Rodrigues, J., D’Costa, D., Doijad, S., Ashok Kumar, J., Malik, S. V. S., Kalorey, D. R., Rawool, D. B., Hain, T., Chakraborty, T., & Barbuddhe, S. B. (2011). Genotypic characterization of Listeria monocytogenes isolated from humans in India. Annals of Tropical Medicine and Parasitology, 105, 351–358.
Kalorey, D. R., Kurkure, N. V., Warke, S. R., Rawool, D. B., & Barbuddhe, S. B. (2008). Listeria species in bovine raw milk: A large survey of Central India. Food Control., 19, 109–112.
Kämpfer, P. (1992). Differentiation of Corynebacterium spp., Listeria spp. and related organisms by using fluorogenic substrates. Journal of Clinical Microbiology, 30(5), 1067–1071.
Kaur, S., Malik, S. V. S., Vaidya, V. M., & Barbuddhe, S. B. (2007). Listeria monocytogenes in spontaneous abortions in humans and its detection by multiplex PCR. Journal of Applied Microbiology, 103, 1889–1896.
Kerouanton, A., Roche, S. M., Marault, M., Velge, P., Pourcher, A. M., Brisabois, A., Federighi, M., & Garrec, N. (2010). Characterization of isolates of Listeria monocytogenes from sludge using pulsed-field gel electrophoresis and virulence assays. Journal of Applied Microbiology, 108, 1380–1388.
Kousta, M., Mataragas, M., Skandamis, P., & Drosinos, E. H. (2010). Prevalence and sources of cheese contamination with pathogens at farm and processing levels. Food Control, 21, 805–815.
Lachica, R. V. (1990). Selective plating medium for quantitative recovery of food-borne Listeria monocytogenes. Applied and Environmental Microbiology, 56, 167–169.
Lang, H. E., Neuhaus, K., & Scherer, S. (2013). Listeria weihenstephanensis sp. nov., isolated from the water plant Lemna trisulca taken from a freshwater pond. International Journal of Systematic and Evolutionary Microbiology, 63, 641–647.
Leclercq, A., Clermont, D., Bizet, C., Grimont, P. A., Le Flèche-Matéos, A., Roche, S. M., Buchrieser, C., Cadet-Daniel, V., Le Monnier, A., Lecuit, M., & Allerberger, F. (2010). Listeria rocourtiae sp. nov. International Journal of Systematic and Evolutionary Microbiology, 60, 2210–2214.
Linnan, M. J., Nascola, L., Lou, X. D., Goulet, V., May, S., Salminen, C., Hird, D. W., Yonekura, M. L., Hayes, P., Weaver, R., Audurier, A., Plikaytis, B. D., Fannin, S. L., Kleks, A., & Broome, C. V. (1988). Epidemic listeriosis associated with Mexican style cheese. The New England Journal of Medicine, 319, 823–828.
Liu, D. (2006). Identification, subtyping and virulence determination of an important foodborne pathogen. Journal of Medical Microbiology, 55, 645–659.
Liu, S., Graham, J. E., Bigelow, L., Morse, P. D., & Wilkinson, B. J. (2002). Identification of Listeria monocytogenes genes expressed in response to growth at low temperature. Applied and Environmental Microbiology, 68, 1697–1700.
Liu, D., Ainsworth, A. J., Austin, F. W., & Lawrence, M. L. (2003). Characterization of virulent and avirulent Listeria monocytogenes strains by PCR amplification of putative transcriptional regulator and internalin genes. Journal of Medical Microbiology, 52, 1065–1070.
Liu, D., Lawrence, M., Gorski, L., Mandrell, R. E., Austin, F. W., & Ainsworth, A. J. (2006). Listeria monocytogenes serotype 4b strains belonging to lineages I and III possess distinct molecular features. Journal of Clinical Microbiology, 44, 204–207.
Lovett, J., Francis, D. W., & Hunt, J. M. (1987). Listeria monocytogenes in raw milk: Detection, incidence and pathogenicity. Journal of Food Protection, 50, 185192.
Low, J. C., & Donachie, W. (1997). A review of Listeria monocytogenes and listeriosis. The Veterinary Journal, 153, 9–29.
Lukinmaa, S., Miettinen, M., Nakari, U. M., Korkeala, H., & Siitonen, A. (2003). Listeria monocytogenes isolates from invasive infections: Variation of sero- and genotypes during an 11-year period in Finland. Journal of Clinical Microbiology, 41, 1694–1700.
Lundén, J. M., Autio, T. J., Sjöberg, A. M., & Korkeala, H. J. (2003). Persistent and nonpersistent Listeria monocytogenes contamination in meat and poultry processing plants. Journal of Food Protection, 66, 2062–2069.
Lunge, V. R., Miller, B. J., Livak, K. J., & Batt, C. A. (2002). Factors affecting the performance of 5’ nuclease PCR assays for Listeria monocytogenes detection. Journal of Microbiological Methods, 51(3), 361–368.
Lyytikäinen, O., Autio, T., Maijala, R., Ruutu, P., Honkanen-Buzalski, T., Miettinen, M., Hatakka, M., Mikkola, J., Anttila, V. J., Johansson, T., Rantala, L., Aalto, T., Korkeala, H., & Siitonen, A. (2000). An outbreak of Listeria monocytogenes serotype 3a infections from butter in Finland. Journal of Infectious Diseases, 181, 1838–1841.
Mainou-Fowler, T., MacGowan, A. P., & Postehwaite, R. (1988). Virulence of Listeria spp. Course of infection in resistant and susceptible mice. Journal of Medical Microbiology, 27, 131–140.
Malik, S. V. S., Barbuddhe, S. B., & Chaudhari, S. P. (2002). Listeric infections in humans and animals in Indian subcontinent: A review. Tropical Animal Health and Production, 34, 359–381.
Mammina, C., Aleo, A., Romani, C., Pellissier, N., Nicoletti, P., Pecile, P., Nastasi, A., & Pontello, M. M. (2009). Characterization of Listeria monocytogenes isolates from human listeriosis cases in Italy. Journal Clinical Microbiology, 47, 2925–2930.
McClain, D., & Lee, W. H. (1988). Development of USDA-FSIS method for isolation of Listeria monocytogenes from raw meat and poultry. Journal of the Association of Official Analytical Chemists, 71, 660–664.
McLauchlin, J. (1987). Listeria monocytogenes, recent advances in the taxonomy and epidemiology of listeriosis in humans. Journal of Applied Bacteriology, 63, 1–11.
McLauchlin, J. (1997). The identification of Listeria species. International Journal of Food Microbiology, 38, 77–81.
McLauchlin, J., Audurier, A., Frommelt, A., Gerner-Smidt, P., Jacquet, C., Loessner, M. J., van-der Mee-Marquet, N., Rocourt, J., Shah, S., & Wilhelms, D. (1996). WHO study on subtyping Listeria monocytogenes: Results of phage-typing. International Journal of Food Microbiology, 32, 289–299.
McLauchlin, J., Mitchell, R. T., Smerdon, W. J., & Jewell, K. (2004). Listeria monocytogenes and listeriosis: A review of hazard characterisation for use in microbiological risk assessment of foods. International Journal of Food Microbiology, 92, 15–33.
Menudier, A., Bosiraud, C., & Nicolas, J. A. (1991). Virulence of Listeria monocytogenes serovars and Listeria s. in experimental infection in mice. Journal of Food Protection, 54, 917921.
Murray, E. G. D., Webb, R. A., & Swann, M. B. R. (1926). A disease of rabbits characterised by a large mononuclear leucocytosis caused by a hitherto underscribed bacillus Bacterium monocytogenes (N.Sp.). Journal of Pathology and Bacteriology, 29, 407–409.
Nadon, C. A., Woodward, D. L., Young, C., Rodgers, F. G., & Wiedmann, M. (2001). Correlations between molecular subtyping and serotyping of Listeria monocytogenes. Journal of Clinical Microbiology, 39, 2704–2707.
Neves, E., Silva, A. C., Roche, S. M., Velge, P., & Brito, L. (2008). Virulence of Listeria monocytogenes isolated from the cheese dairy environment, other foods and clinical cases. Journal of Medical Microbiology, 57, 411–415.
Newell, D. G., Koopmans, M., Verhoef, L., Duizer, E., Aidara-Kane, A., Sprong, H., Opsteegh, M., Langelaar, M., Threfall, J., Scheutz, F., van der Giessen, J., & Kruse, H. (2011). Food-borne diseases-the challenges of 20 years ago still persist while new ones continue to emerge. International Journal of Food Microbiology, 145, 493.
Norton, D. M., Scarlett, J. M., Horton, K., Sue, D., Thimothe, J., Boor, K. J., & Wiedmann, M. (2001). Characterization and pathogenic potential of Listeria monocytogenes isolates from the smoked fish industry. Applied and Environmental Microbiology, 67, 646–653.
Notermans, S. H. W., Dufrenne, J., LeimeisterWachter, M., Domann, E., & Chakraborty, T. (1991a). Phosphatidylinositol-specific phospholipase C activity as a marker to distinguish between pathogenic and non pathogenic Listeria species. Applied Environmental Microbiology, 57, 26662670.
Notermans, S., Dufrenne, J., Chakraborty, T., Steinmeyer, S., & Terplant, G. (1991b). The chick embryo test agrees with the mouse bioassay for assessment of the pathogenicity of Listeria species. Letters in Applied Microbiology, 13, 161164.
Nyfeldt, A. (1929). Etiologie de la mononucleose infectieuse. Compt Rend Soc Biol, 101, 590–591.
Olesen, I., Vogensen, F. V., & Jespersen, L. (2009). Gene tanscription and virulence potential of Listeria monocytogenes strains after exposure to acidic and NaCl stress. Foodborne Pathogens and Disease, 6, 669–680.
Oliver, S. P., Jayarao, B. M., & Almeida, R. A. (2005). Foodborne pathogens in milk and the dairy farm environment: Food safety and public health implications. Foodborne Pathogens and Disease, 2, 115–129.
Orsi, R. H., den Bakker, H. C., Wiedmann, M. (2011). Listeria monocytogenes lineages: Genomics, evolution, ecology, and phenotypic characteristics. International Journal of Medical Microbiology, 301, 79–96.
Ottaviani, F., Ottaviani, M., & Agosti, M. (1997). Esperienza su um agar selettivo e differentiale per Listeria monocytogenes. Industrie Alimentari, 36, 1–3.
Palumbo, J. D., Borucki, M. K., Mandrell, R. E., & Gorski, L. (2003). Serotyping of Listeria monocytogenes by enzyme-linked immunosorbent assay and identification of mixed-serotype cultures by colony immunoblotting. Journal of Clinical Microbiology, 41, 564–571.
Pan, Y., Breidt, F. Jr., & Kathariou, S. (2006). Resistance of Listeria monocytogenes biofilms to sanitizing agents in a simulated food-processing environment. Applied and Environmental Microbiology, 72, 7711–7717.
Paziak-Domańska, B., Bogusławska, E., Wieckowska-Szakiel, M., Kotłowski, R., Rózalska, B., Chmiela, M., Kur, J., Dabrowski, W., & Rudnicka, W. (1999). Evaluation of the API test, phosphatidylinositol-specific phospholipase C activity and PCR method in identification of Listeria monocytogenes in meat foods. FEMS Microbiology Letters, 171, 209–214.
Portnoy, D. A., Chakraborty, T., Goebel, W., & Cassart, P. (1992). Molecular determinants of Listeria monocytogenes pathogenesis. Infection and Immunity, 60, 12631267.
Rawool, D. B., Malik, S. V., Shakuntala, I., Sahare, A. M., & Barbuddhe, S. B. (2007). Detection of multiple virulence associated genes in Listeria monocytogenes from bovine mastitis cases. International Journal of Food Microbiology, 113, 201–207.
Rebagliati, V., Philippi, R., Rossi, M., & Troncoso, A. (2009). Prevention of foodborne listeriosis. Indian Journal of Pathology & Microbiology, 52(2), 145–149.
Roche, S. M., Velge, P., Bottreau, E., Durier, C., Marquet-van-der Mee, N., Pardon, P. (2001). Assessment of the virulence of Listeria monocytogenes: Agreement between a plaque-forming assay with HT-29 cells and infection of immunocompetent mice. International Journal of Food Microbiology, 68, 33–44.
Roche, S. M., Gracieux, P., Albert. I., Gouali, M., Jacquet, C., Martin, P. M., & Velge, P. (2003). Experimental validation of low virulence in field strains of Listeria monocytogenes. Infection and Immunity, 71, 3429–3436.
Rocourt, J., & Catimel, B. (1985). Biochemical characterization of species in the genus Listeria. Zentralblatt für Bakteriologie, Mikrobiologie, und Hygiene. Series A, Medical microbiology, infectious diseases, virology, parasitology, 260(2), 221–231.
Rodas-Suárez, O. R., Flores-Pedroche, J. F., Betancourt-Rule, J. M., Quiñones-Ramírez, E. I., & Vázquez-Salinas, C. (2006). Occurrence and Antibiotic Sensitivity of Listeria monocytogenes Strains Isolated from Oysters, Fish, and Estuarine Water. Applied and Environmental Microbiology, 72, 7410–7412.
Rodríguez-Lázaro, D., Fernández, M., & Pla, M. (2004). Simultaneous quantitative detection of Listeria spp. and Listeria monocytogenes using a duplex real-time PCR-based assay. FEMS Microbiology Letters, 233, 257–267.
Rossi, M. L., Paiva, A., Tornese, M., Chianelli, S., & Troncoso, A. (2008). Listeria monocytogenes outbreaks: A review of the routes that favor bacterial presence. Revista. Chilena de Infectologia, 25, 328–335.
Sauders, B. D., & Wiedmann, M. (2007). Ecology of Listeria species and L. monocytogenes in the natural environment. In E. T. Ryser & E. H. Marth (Eds.), Listeria, listeriosis, and food safety (pp. 21e53). New York: Marcel Dekker.
Schlech, W. F. 3rd, Lavigne, P. M., Bortolussi, R. A., Allen, A. C., Haldane, E. V., Wort, A. J., Hightower, A. W., Johnson, S. E., King, S. H., Nicholls, E. S., Broome, C. V. (1983). Epidemic listeriosis-evidence for transmission by food. The New England Journal of Medicine, 308, 203–206.
Schonberg, A. (1989). Method to determine virulence of Listeria strains. International Journal of Food Microbiology, 8, 281284.
Schuchat, A., Swaminathan, B., & Broome, C. V. (1991). Epidemiology of human listeriosis. Clinical Microbiology Reviews, 4, 169–183.
Seeliger, H. P. R., & Höhne, K. (1979). Serotyping of Listeria monocytogenes and related species. Methods in Microbiology, 13, 31–49.
Seeliger, H. P. R., & Jones, D. (1986). Genus Listeria Pirie, 1940, 383AL. In: P. M. A. Sneath, N. S. Nair, M. E. Sharpe & J. G. Holt (Eds.), Bergey’s manual of systematic bacteriology (Vol. 2, pp. 1235–1245). Baltimore: The Williams and Wilkins Co.
Shakuntala, I., Malik, S. V. S., Barbuddhe, S. B., & Rawool, D. B. (2006). Isolation of Listeria monocytogenes from buffaloes with reproductive disorders and its confirmation by polymerase chain reaction. Veterinary Microbiology, 117, 229–234.
Skalka, B., Smola, J., & Elischerova, K. (1982). Routine test for in vitro differentiation of pathogenic and apathogenic Listeria monocytogenes strains. Journal of Clinical Microbiology, 15, 503507.
Smith, J. L., & Buchanan, R. L. (1990). Identification of supplements that enhance the recovery of Listeria monocytogenes on modified Vogel-Johnson agar. Journal of Food Safety, 10, 155–163.
Stelma, G. N., Reyes, A. L., Peeler, J. T., Francis, D. W., Hunt, J. M., Spaulding, P. L., Johnson, C. H., & Lovett, J. (1987). Pathogenicity test for testing Listeria monocytogenes using immunocompromised mice. Journal of Clinical Microbiology, 25, 2085–2089.
Struelens, M. J., & the Members of the European Study Group on Epidemiological Markers (ESGEM), of the European Society for Clinical Microbiology and Infectious Diseases (ESCMID). (1996). Consensus guidelines for appropriate use and evaluation of microbial epidemiologic typing systems. Clinical Microbiology and Infection, 2, 2–11.
Swaminathan, B., & Gerner-Smidt, P. (2007). The epidemiology of human listeriosis. Microbes and Infection, 9, 1236–1243.
Terplan, G., & Steinmeyer, S. (1989). Investigations on the pathogenicity of Listeria spp. by experimental infection of the chick embryo. International Journal of Food Microbiology, 8, 277280.
Thimothe, J., Nightingale, K. K., Gall, K., Scott, V. N., & Wiedmann, M. (2004). Tracking of Listeria monocytogenes in smoked fish processing plants. Journal of Food Protection, 67, 328–341.
Todd, E. C. D., & Notermans, S. (2011). Surveillance of listeriosis and its causative pathogen, Listeria monocytogenes. Food Control, 22, 1484–1490.
Topley, W. W. C., & Wilson, G. S. (1990). Principles of bacteriology, virology and immunity. In M. T. Parker & B. I. Duerden (Eds.), Systemic bacteriology (pp. 63–71). London: Edward Amold.
Van Kessel, J. S., Karns, J. S., Gorski, L., McCluskey, B. J., & Perdue, M. L. (2004). Prevalence of Salmonellae, Listeria monocytogenes, and fecal coliforms in bulk tank milk on US dairies. Journal of Dairy Science, 87, 2822–2830.
Van Netten, P., Perales, I., Curtis, G. D. W., & Mossel, D. A. A. (1989). Liquid and solid selective differential media for the detection and enumeration of Listeria monocytogenes and other Listeria spp. International Journal of Food Microbiology, 8, 224316.
Vázquez-Boland, J. A., Kuhn, M., Berche, P., Chakraborty, T., Domínguez-Bernal, G., Goebel, W., González-Zorn, B., Wehland, J., & Kreft, J. (2001). Listeria pathogenesis and molecular virulence determinants. Clinical Microbiology Reviews, 14, 584–640.
Vlaemynck, G., Lafarge, V., & Scotter, S. (2000). Improvement of the detection of Listeria monocytogenes by the application of ALOA, a diagnostic, chromogenic isolation medium. Journal of Applied Microbiology, 88, 430–441.
Warriner, K., & Namvar, A. (2009). What is the hysteria with Listeria? Trends in Food Science and Technology, 20, 245–254.
Wiedmann, M. (2002). Molecular subtyping methods for Listeria monocytogenes. Journal of AOAC International, 85(2), 524–531.
Wiedmann, M., Bruce, J. L., Knorr, R., Bodis, M., Cole, E. M., McDowell, C. I., McDonough, P. L., & Batt, C. A. (1996). Ribotype diversity of Listeria monocytogenes strains associated with outbreaks of listeriosis in ruminants. Journal of Clinical Microbiology, 34, 1086–1090.
Wielinga, P. R., & Schlundt, J. (2012). Food safety: At the center of a one health approach for combating zoonoses. In P. R. Wielinga & J. Schlundt (Eds.), Current topics in microbiology and immunology (pp. 3–17). Berlin: Springer.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
D’Costa, D. (2015). Prevalence of Listeria in Milk from Farm to Table. In: Borkar, S. (eds) Bioprospects of Coastal Eubacteria. Springer, Cham. https://doi.org/10.1007/978-3-319-12910-5_15
Download citation
DOI: https://doi.org/10.1007/978-3-319-12910-5_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-12909-9
Online ISBN: 978-3-319-12910-5
eBook Packages: Earth and Environmental ScienceEarth and Environmental Science (R0)