Abstract
Worldwide, L. monocytogenes bacteria are frequently associated with illness in humans, where immunocompromised individuals and pregnant women are at high risk of contracting listeriosis. The pathogen most often spreads through food consumption, so it is a major concern in most food-processing environments. In Africa, however, research on L. monocytogenes is scarce, making data on listeriosis limited. This is problematic because in Africa, traditionally produced foods have poor microbial quality. On average, 5.1 % of dairy and ready-to-eat foods are contaminated with L. monocytogenes. The pathogen has been isolated from milk, local cheese (“wara”), yogurt, ice cream, “kunu,” and ready-to-eat meat products during and after processing. Furthermore, it is resistant to one or more antibiotics and can also form biofilms on various surfaces that contact food. So, while L. monocytogenes is persistent in food-processing environments in Africa, the serotypes of its circulating strains are largely unknown. This study therefore expounds the characteristics of L. monocytogenes and listeriosis associated with consuming contaminated diary and ready-to-eat foods in Africa. We also present the prevalence and persistence of the pathogen in most food environments as well as the safety measures that can limit its ability to contaminate foods/surfaces and spread.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
L. monocytogenes, a bacterium that causes listeriosis, is continuously viewed as a threat to global public health and is gaining important attention among stakeholders in food safety. Listeriosis affects all species of domestic animals and humans. The human infection is usually severe, resulting in high hospitalization rates and mortality, especially for “at-risk” populations, and causes abortions, meningitis, meningoencephalitis, spontaneous peritonitis, septicemia, etc. (Farber and Peterkin 1991; Rocourt 1996; Mead et al. 1999; Acha and Szyfres 2003). At-risk individuals are those with low immunity, such as HIV/AIDS patients, children under 5 years old, pregnant women, and elderly people (Farber and Peterkin 1991; Acha and Szyfres 2003; Borucki and Call 2003; McLauchlin et al. 2004; Liu 2006; Kuhn et al. 2008). L. monocytogenes is ubiquitous in nature and can survive harsh environmental conditions such as low pH, water activity (Nolan et al. 1992; Buchanan et al. 2000; Duffy et al. 1994), and a wide temperature range (including refrigeration temperature) (HPA 2009). Food contamination is a major way that L. monocytogenes infections are acquired (Taormina and Beauchat 2002). As such, the pathogen has been isolated from various ready-to-eat, dairy, and other minimally processed foods in many countries and has caused various documented foodborne disease outbreaks (Piffaretti et al. 1989; Mahmood et al. 2003; Vitas et al. 2004; Aurora et al. 2009; Rahimi et al. 2010; Rivoal et al. 2010). Its virulence and persistence in the environment is further potentiated by its ability to form fimbriae, cellulose, and biofilms (Hood and Zottola 1995; Abu-lail and Camesano 2003; Gulsun et al. 2005; Adetunji 2010). Furthermore, the pathogen is now more resistant to many commercially available antibiotics and sanitizers (Poyart-Salmeron et al. 1992).
Listeriosis is frequently reported in developed countries, but its representation in Africa is still unclear. Research on L. monocytogenes in Africa is scarce, so data on listeriosis is limited. However, the prevalence, virulence, and serotypes of L. monocytogenes in ready-to-eat foods have been reported in Ethiopia, Uganda, Morocco, Egypt, Nigeria, Botswana, and Lesotho (Molla et al. 2004; Ennaji et al. 2008; Salihu et al. 2008; Morobe et al. 2009, 2012; Abd El Malek et al. 2010; Mugampoza et al. 2011; Abeer et al. 2012; Moshoeshoe and Olivier 2012; Yakubu et al. 2012), but the serotypes and virulence of the circulating strains remain largely unknown. The objectives of this review are to expound the characteristics of L. monocytogenes and listeriosis associated with consumption of contaminated diary and ready-to-eat foods in Africa and to briefly discuss the prevalence and persistence of the pathogen in foods and food environments. We also highlight the safety measures that can be applied to limit its contamination, spread, and persistence.
2 Characteristics of L. monocytogenes
Listeria are facultative anaerobes that are gram-positive, non-acid-fast, non-spore-forming, acapsular rod-shaped bacteria, and they measure 0.5–2 μm by 0.4–0.5 μm (Walker 2005). The history of Listeria is traced to 1926 when Murray, Web, and Swann demonstrated that it was the causative organism of listeriosis (Parihar 2008). In 1940, Pirie suggested the name L. monocytogenes. Other species in the genus Listeria include Listeria ivanovii, Listeria seeligeri, Listeria innocua, Listeria welshimeri, and Listeria grayi. Of these, only Listeria ivanovii and Listeria monocytogenes are pathogenic.
L. monocytogenes is a facultative intracellular, anaerobic, psychotropic bacterium with low G+C (36–42 %) content (Vazquez-Boland et al. 2001; Monk et al. 2008; Parihar 2008; Sukhadeo and Trinad 2009), and it moves in a distinctive way called “tumbling motility,” propelled by its peritrichous flagellum (Ferreira et al. 2003; Adetunji and Adegoke 2008). L. monocytogenes has a high motility (Mead et al. 1999) and grows within a wide temperature range (<0 –45 °C) (HPA 2009), with an optimum at 30–37 °C (Swaminathan et al. 1995). However, the pathogen can be destroyed when kept at high temperatures (e.g., pasteurization) for short durations (Walker 2005). This microorganism is oxidase negative and catalase positive, it ferments glucose and produces acid without gas, and it survives in vacuum-packaged products at refrigeration temperatures (Duffy et al. 1994). Furthermore, it has low water activity and a low pH (Nolan et al. 1992; Buchanan et al. 1993) and produces a narrow zone of hemolysis on sheep blood agar (Varnam and Evans 1991). The bacterial particles usually occur singly, in short chains, or in diploforms, producing V-shape arrangements (Parihar 2008). Furthermore, it is genetically heterogeneous (Piffaretti et al. 1989; Wiedmann et al. 1997; Kathariou 2002) and displays great biodiversity and serological cross-reactivity with various bacteria strains in other genera (Parihar 2008). L. monocytogenes is ubiquitous and can be isolated anywhere in the environment, making it a very dangerous organism. In 2008, the Office International des Epizooties (OIE) documented many molecular and cellular determinants of virulence for this intracellular pathogen, and although there is evidence that polymorphisms influence virulence in some of the different L. monocytogenes strains, this heterogeneity cannot be correlated with the organism’s ability or inability to produce disease. Therefore, all L. monocytogenes strains are considered to be potentially pathogenic.
3 L. monocytogenes Infections
L. monocytogenes causes a severe zoonotic illness known as listeriosis, which is associated with morbidity and mortality in humans and livestock (Borucki and Call 2003). Animals usually affected include both large and small ruminants, pigs, rabbits, mice, birds, and fish (Ireton 2006). Listeriosis commonly affects people with compromised immunity (e.g., HIV/AIDS patients), pregnant women, neonates, and elderly people (Farber and Peterkin 1991; Borucki and Call 2003; McLauchlin et al. 2004; Liu 2006; Kuhn et al. 2008), resulting in meningitis, meningoencephalitis, spontaneous peritonitis, abortion, septicemia, arthritis, pelvic infection, or arthritis (Khelef et al. 2006; Sukhadeo and Trinad 2009; Adetunji and Isola 2011a). Infections often have high risks of hospitalization, and human mortality is also high, ranging between 20 % and 30 % (Farber and Peterkin 1991; Rocourt 1996; Mead et al. 1999) and up to 80–99 % in the vulnerable groups (Farber and Peterkin 1991; Gray and Killinger 1966; Rocourt 1996; Sauders et al. 2003; Chenal-Francisque et al. 2011). Several listeriosis outbreaks have been reported throughout the world, including many multistate outbreaks in the United States. In 2003, mortality from listeriosis was about 500 people from a reported ~2500 illnesses (Mead et al. 1999). However, listeriosis is underreported in Africa (Boukadidda et al. 1994) because food-processing industries are still evolving. In Nigeria, L. monocytogenes was isolated from some patients that showed clinical signs of listeriosis, and the infection produced a mortality rate of 27 % (Onyemelukwe et al. 1983). But in Morocco, human listeriosis is uncommon (Benomar et al. 2000). Chintu and Bathirunathan (1975) reported 85 cases of listeriosis in Zambia, while Hohne et al. (1975) reported that the outbreak serotypes (1/2a and 4b) of L. monocytogenes were isolated in slaughtered cattle in Togo.
Contamination of ready-to-eat foods—as well as other minimally processed foods—is widely documented as the main source of Listeria outbreaks. Consequently, it is a great public health concern. Outbreaks are often linked with the consumption of several contaminated food products, including ready-to-eat dairy and meat products, such as coleslaw, pasteurized milk, milk from lactating ruminants, soft cheeses, raw and pasteurized eggs, poultry meat, cooked meats, cured meats, and smoked salmon (Piffaretti et al. 1989; Mahmood et al. 2003; Vitas et al. 2004; Aurora et al. 2009; Rahimi et al. 2010; Rivoal et al. 2010).
4 Traditional Foods and L. monocytogenes: Isolation, Prevalence, and Persistence
4.1 Isolation and Prevalence of L. monocytogenes in Ready-to-Eat Foods in Africa
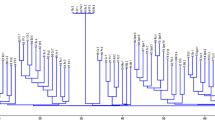
In Africa, roughly 5.1 % of dairy and ready-to-eat food sample are contaminated with L. monocytogenes, as shown in some of the few available prevalence studies. While Africa comprises over 50 countries, there are reports on L. monocytogenes incidence and prevalence from ready-to-eat foods from only a few countries (Fig. 1). In North Africa, Egypt has a prevalence of 5 % (Abd El Malek et al. 2010) and Morocco is at 2.4 % (Ennaji et al. 2008). In these two countries, L. monocytogenes isolates were obtained from meats, luncheon, and frozen chicken legs using multiplex polymerase chain reaction (PCR). However, in a study by Abeer et al. (2012), L. monocytogenes was not detected in camel milk from Egypt. Camel milk contains lysozyme and lactoferrin (El Agamy et al. 1992; Wernery 2003; Al-Majali et al. 2007; Al-Haj and Al-Kanhal 2010), which prevent the pathogen’s growth.
Countries in Africa with known prevalence, serotypes, and virulence of circulating Listeria monocytogenes strains. Virulence genes: (A) prfA (Egypt); (B) actA (Egypt); (C) hly (Morocco). Circulating serotypes: (1) 1/2b, 3b, 7, 4b, 4d, 4e (Morocco); (2) 1/2b, 4b, 4e (Ethiopia); (3) 1/2b, 3b, 4a, 4b, 4c, 4d, 4e (Botswana). (asterisk) Countries with known prevalence (Botswana, Egypt, Ethiopia, Lesotho, Morocco, Nigeria, Uganda). The outline map of Africa was sourced from http://www.worldatlas.com/webimage/countrys/africa/afoutl.htm
Ethiopia and Uganda represent the only countries in East Africa where studies on the prevalence of L. monocytogenes were carried out. Using both conventional and molecular methods, L. monocytogenes was isolated from ice cream, pork samples, minced beef, fish, and chicken samples, amounting to a prevalence of 5.1 % in Ethiopia (Molla et al. 2004). In Uganda, L. monocytogenes contaminated 3 % and 13 % of locally processed yogurt and bulk raw milk, respectively (Mugampoza et al. 2011). Currently, there is no clear evidence on its prevalence in central Africa. In Southern Africa, recorded prevalences ranged from 2.5 % in Lesotho (Moshoeshoe and Olivier 2012) to 4.3 % in Botswana (Morobe et al. 2009). In this region, the contaminated ready-to-eat foods were unpasteurized bovine milk, cheese, meat, frozen cabbage, and salads. In South Africa, researchers work more on Listeria ivanovii (Nyenje et al. 2012a, 2012b, 2012c) rather than Listeria monocytogenes so data on this pathogen are limited. Like other parts of the continent, few reports exist regarding the prevalence of L. monocytogenes in West Africa. Using agar-based techniques, some studies carried out in northern Nigeria by Yakubu et al. (2012) and Salihu et al. (2008) obtained prevalences of 5.3 % and 25 % in bovine milk and smoked fish, respectively.
4.2 Virulence and Serotypes of Circulating Listeria monocytogenes Strains
L. monocytogenes strains are diverse (Kathariou 2002), having dissimilar virulence characteristics. Usually, the pathogen’s virulence genes inhabit a 9.6-kb chromosomal region (Gouin et al. 1994), where the prfA gene regulates these clustered genes on the chromosome (Chakraborty et al. 1992). In every successful infection of a host, L. monocytogenes makes use of several virulence factors (Doyle 2001; Vazquez-Boland et al. 2001; Liu 2006). These include internalins (inlA and inlB), surface protein p104, listeriolysin O (LLO: encoded by hly), ActA protein, phospholipases (phosphatidylinositol-specific phospholipase C (PI-PLC, encoded by plcA) and a broad-range or phosphatidylcholine-specific phospholipase C (PCPLC, plcB)), zinc-dependent metalloprotease, Clp proteases and ATPases, protein p60, and stress response genes (opuCA, lmo1421, and bsh). Only very few of the virulent genes expressed by L. monocytogenes have been determined in the existing circulating strains, and they are mostly from North Africa (Fig. 1). Abd El-Malek et al. (2010) and Abeer et al. (2012) determined the presence of prfA and actA genes in L. monocytogenes in some ready-to-eat foods in Egypt; in camel milk, the prevalence of actA in L. monocytogenes is 2.16 % (Abd El-Malek et al. 2010). Also, Ennaji et al. (2008) confirmed the presence of virulent hly genes in some foods sourced from Morocco. However, there are very few additional reports on other virulence factors responsible for Listeria pathogenesis in L. monocytogenes isolates from other parts of Africa.
Based on the specific O and H surface antigen of Listeria species, 12 or more serotypes of L. monocytogenes have been typed using serological detection (Liu 2006; Arun 2008). These serotypes include: 1/2a, 1/2b, 1/2c, 3a, 3b, 3c, 4a, 4b, 4c, 4d, 4e, 4ab, and 7. Serotypes 1/2a, 1/2b, and 4b are the most virulent causing up to 98 % of human listeriosis. This nomenclature has also been used to define three existing L. monocytogenes lineages: Lineage I (highly pathogenic with epidemic clones, 1/2b, 3b, 4b, 4d, 4e), Lineage II (medium pathogenic, 1/2a, 1/2c, 3c, 3a), and Lineage III (not very pathogenic, 4a, 4c). Lineages I, II, and III are responsible for most, rare, and small outbreaks, respectively (Wiedmann et al. 1996, 1997; Jacquet et al. 2002; Arun 2008). In ready-to-eat foods in Africa, circulating L. monocytogenes strains have been serotyped into 1/2a, 1/2b, 3b, 4b, 4d, 4e, and 7 (Molla et al. 2004; Ennaji et al. 2008; Morobe et al. 2009, 2012), indicating that more of the highly pathogenic lineages with epidemic clones are circulating in Africa. Also, because these identified serotypes are from only three countries (Fig. 1), studies on serological typing L. monocytogenes in African foods are needed.
5 Resistance of Listeria monocytogenes to Antimicrobials
Antimicrobial susceptibility test have shown that L. monocytogenes isolates in Africa were sensitive to a wide range of antibiotics. However, since the first documented report of multidrug-resistant L. monocytogenes in France in 1988 (Poyart-Salmeron et al. 1992), several studies in all parts of the world, including Africa, have isolated pathogens that are resistant to one or more antibiotics. Antimicrobial resistance is also common in the African food industry. L. monocytogenes is confirmed to be resistant to over 13 commonly used antibiotics (Table 1), especially isolates from ready-to-eat foods in Botswana, Morocco, and Nigeria, but L. monocytogenes isolates usually have dissimilar resistance patterns. Also, other studies have shown that L. monocytogenes strains isolated from various food sources are resistant to tetracycline (Morobe et al. 2009; Adetunji and Adegoke 2008; Adetunji and Isola 2011a, 2011b) more than other commonly used antibiotics, which corroborates findings from other places (Charpentier et al. 1995; Charpentier and Courvalin 1999). One reason for this resistance may be because tetracycline is one of the most commonly used antibiotics in both animal and human therapeutics (Morobe et al. 2009). Of the six classes of tetracycline-resistance genes—tet(K), tet(L), tet(M), tet(O), tet(P), and tet(S)—that confer the reduced susceptibility of bacterial pathogens to tetracycline (Charpentier et al. 1995), tet(L) and tet(S) are present in L. monocytogenes (Poyart-Salmeron et al. 1992; Charpentier and Courvalin 1999). Other commonly resistant antibiotics include ampicillin, gentamicin, nitrofurantoin, and streptomycin.
6 Biofilm, Cellulose, and Fimbriae Virulence Characteristics in L. monocytogenes
Factors such as biofilm, cellulose, and fimbriae formation in L. monocytogenes are responsible for its virulence and persistence. The level of production of these characteristics has been described to influence virulence in bacterial isolates (Hood and Zottola 1995; Gulsun et al. 2005; Adetunji 2010) and also has major implications in food-processing environments. Fimbria and cellulose formation help pathogens adhere to food contact surfaces (Abu-lail and Camesano 2003; Adetunji 2010). Furthermore, isolates’ level of biofilm production influences the virulence characteristics of such isolates (Hood and Zottola 1995; Gulsun et al. 2005). Biofilms are aggregation of microbial cells organized within a glycocalyx (exopolysaccharide material made up of cellulose). Biofilms facilitate resistance of pathogens to antimicrobials, increase access to nutrients, protect bacteria from external assaults, and promote plasmid and gene transfer through quorum sensing (Jefferson 2004). These characteristics enhance persistence of pathogens in food-processing environments. Furthermore, hydrophobicity, nature and type of incubating surface/medium, pH, surface charge, and temperature all affect biofilm formation by pathogenic Listeria spp. (Wong 1998; Sinde and Carballo 2000; Donlan 2002). Some studies have investigated biofilm formation by L. monocytogenes strains in Nigeria (Adetunji and Adegoke 2008; Adetunji 2010; Adetunji and Isola 2011b; Adetunji and Odetokun 2012), finding that L. monocytogenes can form biofilms on cement, glass, wood, and steel food contact surfaces. These biofilms increase with higher incubation temperature and time, but the degree of biofilm formation varied across the different surfaces. Reports on biofilms from other countries are scarce. Researchers in developing countries should investigate ways of mitigating biofilms in food-processing facilities since Listeria can persist for years (Unnerstand et al. 1996).
7 Controlling the Contamination, Spread, and Persistence of L. monocytogenes
Success in controlling L. monocytogenes contamination of ready-to-eat foods and dairy products depends largely on the level of sanitation and hygiene present during food processing. Various international food safety authorities have recommended that L. monocytogenes should not be detected in 25 g of ready-to-eat foods (HPA 2009). If detected at levels greater than 102 cfu/g in foods, this indicates problems in various control points during food handling and processing, and it poses significant hazards for the at-risk populations. L. monocytogenes contamination usually arises because of poor-quality raw materials, inadequate cooking of foods, cross-contamination, poor cleaning and sanitation, and inappropriate temperature and time controls (HPA 2009).
Since L. monocytogenes is ubiquitous, environmental contamination should be avoided. Processing facilities and equipment should always be kept clean, before and after use. Cleaning must be thorough and strategic. Cleaning and sanitation schedules should be carefully formulated and strictly adhered to in every processing facility to achieve an appreciable level of effectiveness. All areas of the facility should be cleaned, including floors, roofs, walls, drains, pipes, etc. During cleaning, detergents and chemical sanitizers sensitive to L. monocytogenes should be used. Suggested sanitizers are formulations of iodoform, quarter ammonium compounds, peracetic/peroctanoic acids, and chlorinated solutions. Hot water should also be used during sanitation because it has been shown to be effective in pathogen removal. Processing facilities should be properly designed and suitable food contact surfaces should be carefully selected. Food contact surfaces that have lesser affinity for L. monocytogenes adhesion should be used in processing facilities. This will reduce the rate of biofilm formation and forestall dispersal of organisms that facilitate the spread of disease.
Furthermore, clean and dirty operations should be separated. Wastes generated during processing must be treated and properly disposed of. Local processing of ready-to-eat and dairy foods should also be standardized and employ new technologies. Good manufacturing practices are encouraged. L. monocytogenes colonization and infection must be treated as a bacterial hazard, and thus, the principles of hazard analysis critical control points (HACCP) must be applied. A good HACCP plan should be designed for all processing lines and the critical control points carefully identified. The HACCP plan should be well monitored to ensure that the system is working. Also, effective pathogen detection procedures must be utilized. These steps will reduce L. monocytogenes colonization, transmission, and cross-contamination in processing facilities. Personnel and workers handling ready-to-eat and dairy foods should be educated and encouraged to observe maximum cleanliness during processing, packaging, transportation, and display. Protective clothing including neat aprons, hand gloves, head caps, face masks, etc. must be worn at all times. Personnel should maintain regular cleanliness. They should not observe any contacts between raw and finished products. Products must be well packaged and any source of possible L. monocytogenes contamination must be avoided. Strict operation measures must also be applied when products are displayed for sale. It is imperative that all African countries establish food safety authorities that will set the required microbiological standards for ready-to-eat and dairy products consumed in these countries. Measures to enforce these set standards must also be instituted.
8 Conclusion
L. monocytogenes is a pathogen that is a public health concern in food-processing environments. Its wide environmental distribution pattern, persistence through biofilm formation, and ability to cause illnesses in humans, especially through consumption of contaminated ready-to-eat foods, are of serious concerns. Mostly, ready-to-eat foods including dairy products are poorly processed, making L. monocytogenes infections and outbreaks common in Africa, but they are clearly underreported. To improve the microbial quality and control contamination of ready-to-eat foods, especially by L. monocytogenes, the processing lines of these foods should be standardized with modern technologies that would limit pathogen contamination, colonization, spread, and persistence in processing plants. Surveillance of L. monocytogenes and its associated infections especially in at-risk populations is appropriate. More studies are required to highlight the current prevalence of listeriosis in all African regions and countries. The virulence and serotypes of circulating L. monocytogenes in ready-to-eat foods across the continent need to be unraveled, particularly using current molecular isolation and serotyping techniques. This will allow for an important differentiation of all the circulating L. monocytogenes strains. Finally, with the increasing resistance of L. monocytogenes to most currently used antibiotics, authorities should also consider shifting to the use of natural medical plants as antimicrobials and biopreservatives.
References
Abd El-Malek AM, Ali SFH, Hassanein R, Mohamed MA, Elsayh KI (2010) Occurrence of Listeria species in meat, chicken products and human stools in Assiut city, Egypt with PCR use for rapid identification of Listeria monocytogenes. Vet World 3:353–359
Abeer AA, Gouda ASA, Dardir HA, Ibrahim AK (2012) Prevalence of some milk borne bacterial pathogens threatening camel milk consumers in Egypt. Global Vet 8:76–82
Abu-lail NI, Camesano TA (2003) Role of lipopolysaccharides in the adhesion, retention, and transport of Escherichia coli JM109. Environ Sci Tech 37:2173–2183
Acha PN, Szyfres B (2003) Zoonoses and communicable diseases common to man and animals. In Bacterioses and mycoses, 3rd edn. Pan American Health Organization (PAHO), Scientific and Technical Publication, Washington DC, pp 168–179
Adetunji VO (2010) Virulence characteristics of food processing relevance in isolates of Listeria monocytogenes and Escherichia coli O157: H7 strains isolated from ‘wara’ a West African soft cheese. Afr J Microbiol Res 4:249–254
Adetunji VO, Adegoke GO (2008) Formation of biofilm by strains of Listeria monocytogenes isolated from soft cheese ‘wara’ and its processing environment. Afr J Biotechnol 7:2893–2897
Adetunji VO, Isola TO (2011a) Antibiotic resistance of Escherichia coli, Listeria and Salmonella isolates from retail meat tables in Ibadan municipal abattoir, Nigeria. Afr J Biotechnol 10:5795–5799
Adetunji VO, Isola TO (2011b) Crystal violet binding assay for assessment of biofilm formation by Listeria monocytogenes and Listeria spp on wood, steel and glass surfaces. Glob Veterinaria 6:06–10
Adetunji VO, Odetokun IA (2012) Biofilm formation in human and tropical foodborne isolates of Listeria strains. Am J Food Technol 7:517–531
Al-Haj OA, Al-Kanhal HA (2010) Compositional, technological and nutritional aspect of dromedary camel milk. Int Dairy J 20:811–821
Al-Majali AM, Ismail ZB, Al-Hami Y, Nour AY (2007) Lactoferrin concentration in milk from camels (Camelus dromedarius) with and without sub-clinical mastitis. Int J Appl Res Vet Med 5:120–124
Arun KB (2008) Food-borne microbial pathogens mechanisms and pathogenesis. Springer, New York, pp 165–182
Aurora R, Prakash A, Prakash S (2009) Genotypic characterization of Listeria monocytogenes isolated from milk and ready-to-eat indigenous milk products. Food Control 20:835–839
Benomar S, Nejjari N, Lahbabi MS (2000) Listeriose neonatale: une infection exceptionnelle au Maroc. Arch Pediatr 7:428
Borucki MK, Call DR (2003) Listeria monocytogenes serotype identification by PCR. J Clin Microbiol 41:5537–5540
Boukadidda J, Sboui H, Monastiri H et al (1994) La listeriose humaine en Tunisie: deux nouveaux cas chez le nouveau- ne. Med Mal Infect 24:117–118
Buchanan RL, Smith JL, Long W (2000) Microbial risk assessment: dose-response relations and risk characterization. Int J Food Microbiol 58:159–172
Chakraborty T, Leimeister-Wachter M, Domann E, Hartl M, Goebel W, Nichterlein T, Notermans S (1992) Coordinate regulation of virulence genes in Listeria monocytogenes requires the product of the prfA gene. J Bacteriol 174:568–574
Charpentier E, Courvalin P (1999) Antibiotic resistance in Listeria species. Antimicrob Agents Chemother 43:2103–2108
Charpentier E, Gerbaud G, Jacquet C, Rocourt J, Courvalin P (1995) Incidence of antibiotic resistance in Listeria species. J Infect Dis 172:277–281
Chenal-Francisque V, Lopez J, Cantinelli T, Caro V, Tran C, Leclercq A, Lecuit M, Brisse S (2011) Worldwide distribution of major clones of Listeria monocytogenes. Emerg Infect Dis 17:1110–1112
Chintu C, Bathirunathan N (1975) Bacterial meningitis in infancy and childhood in Lusaka (One year prospective study). Med J Zambia 9:150–157
Donlan RM (2002) Biofilms: microbial life on surfaces. Emerg Infect Dis 8:881–890
Doyle ME (2001) Virulence characteristics of Listeria monocytogenes. FRI Briefings. Food Research Institute, University of Wisconsin-Madison. http://fri.wisc.edu/docs/pdf/virulencelmono.pdf. Cited 15 Jan 2014
Duffy LL, Vanderlinde PB, Grau FH (1994) Growth of Listeria monocytogenes on vacuum-packed cooked meats; effects of low pH, aw, nitrite and ascorbate. Int J Food Microbiol 23:377–390
El Agamy EI, Ruppanner R, Ismail A, Champagene CP, Assaf R (1992) Antimicrobial and antiviral activity of camel milk protective proteins. J Dairy Res 59:169–175
Ennaji H, Timinouni M, Ennaji MM, Hassar M, Cohen N (2008) Characterization and antibiotic susceptibility of Listeria monocytogenes isolated from poultry and red meat in Morocco. Infect Drug Resist 1:45–50
Farber JM, Peterkin PI (1991) Listeria monocytogenes: a food-borne pathogen. Microbiol Rev 55:476–511
Ferreira A, Sue D, O’Byrne CP, Boor KJ (2003) Role of Listeria monocytogenes in survival of lethal acidic conditions and in the acquired acid tolerance response. Appl Environ Microbiol 69:2692–2698
Gouin E, Mengaud J, Cossart P (1994) The virulence gene cluster of Listeria monocytogenes is also present in Listeria ivanovii, an animal pathogen, and Listeria seeliger, a nonpathogenic species. Infect Immun 62:3550
Gray ML, Killinger KH (1966) Listeria monocytogenes and listeric infections. Bacteriol Rev 30:309–382
Gulsun S, Oguzoglu N, Inan A, Ceran N (2005) The virulence factors and antibiotic sensitivities of Escherichia coli isolated from recurrent urinary tract infections. Saudi Med J 26:1755–1758
Health Protection Agency (2009) Guidelines for assessing the microbiological safety of ready-to-eat foods placed on the market. Health Protection Agency, London. http://www.hpa.org.uk/webc/hpawebfile/hpaweb_c/1259151921557. Cited 16 2014
Hohne K, Loose B, Seeliger HP (1975) Isolation of Listeria monocytogenes in slaughter animals and bats of Togo (West Africa). Annu Microbiol Paris 126A:501–507
Hood SK, Zottola EA (1995) Biofilm in food processing. Food Control 1:9–18
Ireton K (2006) Listeria monocytogenes. In: Chan VL, Sherman PM, Bourke B (eds) Bacterial genomes and infectious diseases. Humana Press, Totowa, NJ, pp 125–149
Jacquet C, Gouin E, Jeannel D, Cossart P, Rocourt J (2002) Expression of ActA, Ami, InlB, and listeriolysin O in Listeria monocytogenes of human and food origin. Appl Environ Microbiol 68:616–622
Jefferson KK (2004) What drives bacteria to produce a biofilm? FEMS Microbiol Lett 236:163–173
Kathariou S (2002) Listeria monocytogenes virulence and pathogenicity, a food safety perspective. J Food Prot 65:1811–1829
Khelef N, Lecuit M, Buchrieser C, Cabanes D, Dussurget O, Cossart P (2006) The Listeria monocytogenes and the genus Listeria. Prokaryotes 4:404–476
Kuhn M, Scortti M, Vázquez-Boland JA (2008) Pathogenesis. In: Liu D (ed) Handbook of Listeria monocytogenes. CRC Press, New York, pp 99–102
Liu D (2006) Identification, subtyping and virulence determination of Listeria monocytogenes, an important foodborne pathogen. J Med Microbiol 55:645–659
Mahmood MS, Ahmed AN, Hussain I (2003) Prevalence of Listeria monocytogenes in poultry meat, poultry meat products and other related in animates at Faisalabad. Pak J Nutr 2:346–349
McLauchlin J, Mitchel RT, Smerdon WJ, Jewell K (2004) Listeria monocytogenes and listeriosis. A review of hazard characterization for use in microbial risk assessment of foods. Int J Food Microbiol 92:15–33
Mead PS, Slutsker L, Dietz V, McCraig LF, Breese JS, Shapiro C, Griffin PM, Tauxe RV (1999) Food-related illness and death in the United States. Emerg Infect Dis 5:607–623
Molla B, Yilma R, Alemayehu D (2004) Listeria monocytogenes and other Listeria species in retail meat and milk products in Addis Ababa, Ethiopia. Ethiop J Health Dev 18:208–212
Monk IR, Gahan CGM, Hill C (2008) Tools for functional postgenomic analysis of Listeria monocytogenes. Appl Environ Microbiol 74:3921–3934
Morobe IC, Obi CL, Nyila MA, Gashe BA, Matsheka MI (2009) Prevalence, antimicrobial resistance profiles of Listeria monocytogenes from various foods in Gaborone, Botswana. Afr J Biotechnol 8:6383–6387
Morobe IC, Obi CL, Nyila MA, Matsheka MI, Gashe BA (2012) Molecular characterization and serotyping of Listeria monocytogenes with a focus on food safety and disease prevention, Biochemical testing. In Jimenez-Lopez JC (ed) InTech. http://www.intechopen.com/books/biochemical-testing/molecular-characterization-and-serotyping-of-listeriamonocytogenes -isolates-from-various-foods-in-g. Cited 15 Jan 2014
Moshoeshoe SL, Olivier D (2012) Incidence of aerobic spoilage- and psychrotrophic bacteria in non-pasteurised and pasteurised bovine milk from Maseru. Med Technol SA 26:22–27
Mugampoza D, Muyanja CMBK, Ogwok P, Serunjogi ML, Nasinyama GW (2011) Occurrence of Listeria monocytogenes in bulked raw milk and traditionally fermented dairy products in Uganda. Afr J Food Nutr Dev 11:4610–4622
Nolan DA, Chamblin DC, Troller JA (1992) Minimal water activity levels for Listeria monocytogenes and Listeria innocua. Int J Food Microbiol 16:323–335
Nwachukwu NC, Orji FA, Amaike JI (2009) Isolation and characterization of Listeria monocytogenes from Kunu, a locally produced beverage marketed in different markets in Abia State of Nigeria. Aust J Basic Appl Sci 3:4432–4436
Nyenje ME, Green E, Ndip RN (2012a) Biofilm formation and adherence characteristics of Listeria ivanovii strains isolated from ready-to-eat foods in alice, South Africa. Sci World J 2012, 873909. doi:10.1100/2012/873909
Nyenje ME, Tanih NF, Green E, Ndip RN (2012b) Current status of antibiograms of Listeria ivanovii and Enterobacter cloacae isolated from ready-to-eat foods in Alice, South Africa. Int J Environ Res Public Health 9:3101–3114
Nyenje ME, Odjadjare CE, Tanih NF, Green E, Ndip RN (2012c) Foodborne pathogens recovered from ready-to-eat foods from roadside cafeterias and retail outlets in Alice, Eastern Cape Province, South Africa: public health implications. Int J Environ Res Public Health 9:2608–2619
Onyemelukwe GC, Lawande RV, Egler LJ, Mohammed I (1983) Listeria monocytogenes in Northern Nigeria. J Infect Dis 6:141–145
Parihar VS (2008) Human Listeriosis- sources and routes. In: Alsbjer M (ed) Orebro studies in medicine 19. Örebro University, Sweden, 90pp
Pirie JHH (1940) Listeria: change of name for a genus of bacteria. Nature 145:145–264
Piffaretti JC, Kressebuch H, Aeschbacher M (1989) Genetic characterization of clones of bacterium Listeria monocytogenes causing epidemic disease. Proc Natl Acad Sci USA 86:3818–3822
Poyart-Salmeron C, Trieu-Cuot P, Carlier C, MacGowan A, McLauchlin J, Courvalin P (1992) Genetic basis of tetracycline resistance in clinical isolates of Listeria monocytogenes. Antimicrob Agents Chem 36:463–466
Rahimi E, Ameri M, Momtaz H (2010) Prevalence and antimicrobial resistance of Listeria species isolated from milk and dairy products in Iran. Food Control 21:1448–1452
Rivoal K, Quéguiner S, Boscher E, Bougeard S, Ermel G, Salvat G, Federighi M, Jugiau F, Protais J (2010) Detection of Listeria monocytogenes in raw and pasteurized liquid whole eggs and characterization by PFGE. Int J Food Microbiol 138:56–62
Rocourt J (1996) Risk factors for listeriosis. Food Control 7:195–202
Salihu MD, Junaidu AU, Manga SB, Gulumbe ML, Magaji AA, Ahmed A, Adamu AY, Shittu A, Balarabe I (2008) Occurrence of Listeria monocytogenes in smoked fish in Sokoto, Nigeria. Afr J Biotechnol 7:3082–3084
Sauders BD, Fortes ED, Morse DL, Dumas N, Kiehlbauch JA, Schukken Y, Hibbs JR, Wiedmann M (2003) Molecular subtyping to detect human Listeriosis clusters. Emerg Infect Dis 9:672–680
Sinde E, Carballo J (2000) Attachment of Salmonella spp and Listeria monocytogenes to stainless steel, rubber and polytetrafluorethylene: the influence of free energy and the effect of commercial sanitizers. Food Microbiol 17:439–447
Sukhadeo BB, Trinad C (2009) Molecular mechanisms of bacterial infection via the gut. Curr Top Microbiol Immunol 337:173–195
Swaminathan B, Rocourt J, Bille J (1995) Listeria. In: Murray PR, Baron EJ, Pfaller MA, Ternover FC, Yolken RH (eds) Manual of clinical microbiology. ASM Press, Washington, DC, pp 341–348
Taormina PJ, Beauchat LR (2002) Survival of Listeria monocytogenes in commercial food processing equipment cleaning solutions and subsequent sensitivity to sanitizers and heat. J Appl Microbial 92:71–80
Unnerstand H, Bannerman E, Bille J, DanielssonTham ML, Waak E, Tham W (1996) Prolonged contamination of a dairy with Listeria monocytogenes. Neth Milk Dairy J 50:493–499
Varnam AH, Evans MG (1991) Foodborne pathogens: an illustrated text. Mosby, London
Vazquez-Boland JA, Kuhn M, Berche P, Chakraborty T, Domínguez-Bernal G, Goebel W, González-Zorn B, Wehland J, Kreft J (2001) Listeria pathogenesis and molecular virulence determinants. Clin Microbiol Rev 14:584–640
Vitas AI, Aguado V, Garcia-Jalon EL (2004) Occurrence of Listeria monocytogenes in fresh and processed foods in Navarra (Spain). Int J Food Microbiol 90:349–356
Walker RL (2005) Listeria. In: Hirsh DC, MacLachlan NJ, Walker RL (eds) Veterinary microbiology. Blackwell Publishing, Ames, IA, USA
Wernery U (2003) New observations on camels and their milk. Dar Al Fajr, Abu Dhabi, UAE, pp 41–42
Wiedmann M, Bruce JL, Knorr R, Bodis M, Cole EM, McDowell CI, McDonough PL, Batt CA (1996) Ribotype diversity of Listeria monocytogenes strains associated with outbreaks of listeriosis in ruminants. J Clin Microbiol 34:086–1090
Wiedmann M, Bruce JL, Keating C, Johnson AE, McDonough PL, Batt CA (1997) Ribotypes and virulence gene polymorphisms suggest three distinct Listeria monocytogenes lineages with differences in pathogenic potential. Infect Immun 65:2707–2716
Wong AC (1998) Biofilms in food processing environment. J Dairy Sci 81:2765–2770
Yakubu Y, Salihu MD, Faleke OO, Abubakar MB, Junaidu AU, Magaji AA, Gulumbe ML, Aliyu RM (2012) Prevalence and antibiotic susceptibility of Listeria monocytogenes in raw milk from cattle herds within Sokoto Metropolis, Nigeria. Sok J Vet Sci 10:13–17
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Odetokun, I.A., Adetunji, V.O. (2016). Prevalence and Persistence of Listeria monocytogenes in Dairy and Other Ready-to-Eat Food Products in Africa. In: Garg, N., Abdel-Aziz, S., Aeron, A. (eds) Microbes in Food and Health. Springer, Cham. https://doi.org/10.1007/978-3-319-25277-3_18
Download citation
DOI: https://doi.org/10.1007/978-3-319-25277-3_18
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-25275-9
Online ISBN: 978-3-319-25277-3
eBook Packages: Chemistry and Materials ScienceChemistry and Material Science (R0)