Abstract
Distal humerus fractures present with either intra-articular involvement or they are pure extra-articular fractures. Initial clinical evaluation must assess the neurovascular status of the affected extremity and associated injuries to the ipsilateral shoulder and wrist joints. A computed tomography (CT) scan must be obtained when extension of the fracture is suspected in the articular surface or when there is intra-articular involvement with comminution. Bic-column fixation usually provides optimum stability allowing early range of motion of the elbow joint reducing the risk of joint stiffness. We present a case that failed following fixation, analyse the aetiology of failure and discuss the treatment that was successfully implemented.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
History of Previous Primary Failed Treatment
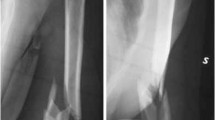
A 61-year-old female patient was admitted to the local hospital after falling two steps landing onto her left elbow. Her medical history was unremarkable. She was a nonsmoker and had not taken any medication for bone protection. On admission, trauma primary and secondary surveys revealed an isolated left distal humerus fracture with comminution over the medial and lateral columns and intra-articular extension (Fig. 10.1).
The fracture was closed and there was no distal neurovascular deficit. An above-elbow splint was applied in the emergency department for temporarily stabilisation and pain relief. She was admitted to the orthopaedic ward for definitive reconstruction. A computed tomography (CT) scan of the left elbow was not obtained. The following day she was taken to the operating room and through a medial and a lateral approach she had the fracture stabilised with a lateral and medial plate. Two days later, postoperative radiographs revealed a compromised fixation (lateral column: unreduced fracture stabilised with a short plate having one screw in each bone fragment; the medial plate last screw was not in bone), Fig. 10.2.
The drain was removed 2 days after surgery and the patient was discharged home the third day. She was seen at 2 weeks in the outpatient clinic. New radiographs taken showed the fixation to have become loose and the medial distal plate screw to have been backed out (Fig. 10.3).
The surgical team decided to proceed with revision of the fixation, and 2 weeks later after the wound had settled down using the same approaches the plates were removed. However, difficulties were encountered with the reconstruction and it was decided to stabilise the fracture with two medial and two lateral K-wires (Fig. 10.4).
Subsequently, the fixation became loose and one of the medial wires backed out through the skin and it was removed.
At 10 weeks following surgery, she was referred to our institution with failed fixation and healthy looking medial and lateral wounds (Fig. 10.5).
Evaluation of the Aetiology of Failure of Fixation
The initial left elbow postoperative radiographs (Fig. 10.2) demonstrate that the fracture was not reduced anatomically and there was a residual valgus deformity. In addition, both columns of the elbow were stabilised with poor fixation as there were only two screws on the lateral column (one on each fragment) and two screws to each proximal and distal fragment on the medial column. Following the revision of the fixation made, the stability of the fixation was further weakened as two K-wires were inserted on each of the medial and lateral columns of the elbow (Fig. 10.3). Both attempts of stabilisation were associated with suboptimal fixation leading to the subsequent failure. The surgical team failed to obey to the principles of intra-articular fracture fixation being restoration of the mechanical axis, anatomical reduction of the articular surface, stable fixation of the articular segment, stable connection of the articular segment to the metaphysis of the affected bone (humerus in this case) and early mobilisation for preservation of cartilage and restoration of the arc of joint movement.
Clinical Examination
At the 10-week follow-up, the wounds were healthy (Fig. 10.5). There was no evidence of infection. There was no redness or erythema. No distal neurovascular deficit was present. Left elbow movements were limited due to pain and the presence of instability. The medial wires were palpable through the skin but not visible.
Diagnostic-Biochemical and Radiological Investigations
In this case it was important to exclude the presence of low-grade infection. Haematological and biochemical investigations were requested, which revealed a normal white blood count, erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). From the clinical examination, biochemical and haematological investigations were caried out and there was no evidence of infection.
The plain radiographs taken (Fig. 10.5) were complemented with a left elbow computed tomography scan to allow a more detailed evaluation of the local environment (Fig. 10.6).
Preoperative Planning
Following the analysis of failure of the fixation, the preoperative plan implemented included:
-
1.
Utilisation of a posterior approach to the distal humerus through an olecranon osteotomy for removal of K-wires and removal of the subchondral screw.
-
2.
Visualisation and protection of the ulnar nerve throughout the procedure.
-
3.
Cleaning the previous fracture planes for reduction of the intra-articular component of the fracture and insertion of lag screws.
-
4.
Sending tissue samples to microbiology to exclude low-grade infection.
-
5.
Anatomical reattachment of the articular segment to the metaphysis with K-wires prior to definitive fixation.
-
6.
Osteosynthesis of the lateral column with application a posterior lateral plate.
-
7.
Osteosynthesis of the medial column with a medial plate.
-
8.
Reduction of the osteotomised olecranon fragment and stabilisation with tension band wiring and a one-third semitubular plate to prevent backing out of the K-wiring.
The Depuy-Synthes anatomical distal humerus combi-hole plates were selected for fracture fixation. They have the options of either locking or nonlocking screw insertion.
In case that following reduction and fixation of the left elbow fragments bone voids were present, autologous iliac crest bone graft would be harvested from the left iliac crest supporting the process of osteogenesis and bone repair. For this reason, small osteotomes were also requested in case that bone grafting would be necessary.
Revision Surgery
Under general anaesthesia, the patient was placed in the lateral decubitus position on a standard table with the left elbow hanging overusing a supporting device attached to the table in a flexed position. The patient was administered one dose of intravenous prophylactic antibiotics (flucloxacillin and gentamycin). We prefer to use a tourniquet. Following prepping and draping of both the left iliac crest and the left elbow, a posterior incision over the distal humerus was made down to the triceps, which curves around the tip of the olecranon, thus minimising the exertion of skin pressure at the incision after wound closure. Then the ulnar nerve was identified by dissection on the medial side and was isolated with a sling.
A chevron olecranon osteotomy is performed with its apex being made at the bare area of the olecranon fossa. Then the triceps fascia is incised and mobilised both medially and laterally while protecting the ulnar and radial nerves. The tip of the olecranon was then held and isolated with a wet swab, proximally allowing good visualisation of the distal humerus articular surface (Fig. 10.7).
Intraoperative picture showing: (a) ulnar nerve being retracted with a blue vascular sling; blue arrow: osteotomised olecranon fragment held with reduction forceps and being retracted proximally; green arrow: intra-articular extension of the fracture; and (b) white arrow: the screw previously used for fixation of the intra-articular component prior to its removal
The previous lag screw was removed. The articular fragments were mobilised, and the articular surface was cleaned and reduced with pointed reduction forceps. Tissue samples were sent to microbiology.
Two 3.5-mm lag screws were inserted for fixation of the intercondylar fracture. Subsequently, using two K-wires the articular block was reduced and was connected to the metaphysis (Fig. 10.8).
Initially a posterolateral six-hole anatomical combi plate was applied for fixation of the lateral column. The medial column was stabilised with an eight-hole medial combi anatomical plate. During the reconstruction process, a defect area was apparent on the medial distal metaphyseal region (Fig. 10.9).
(a) Intraoperative picture showing stabilisation of the fracture with a posterolateral and medial column plate. The white arrow shows the bone defect area on the medial metaphyseal area. (b) AP and (c) lateral fluoroscopic images of the left distal humerus showing fixation of the fracture with the plates
Iliac crest bone graft was harvested from the left iliac crest and was inserted in the area of the bone defect (Fig. 10.10).
(a) AP fluoroscopic image of left distal humerus showing fixation of the fracture with the plates and the reconstruction of the medial column bone defect area with iliac crest bone graft. (b) Intraoperative picture showing the presence of the bone graft in the previous medial bone defect area (white arrow). (c) Intraoperative image of the autologous iliac crest bone graft harvested from the left pelvic iliac crest
Reduction of the fracture and implant positioning and appropriate screw length were checked with the image intensifier prior to fixation of the olecranon osteotomy. The olecranon osteotomy was then reduced with a pointed reduction forceps and was stabilised with tension band wiring. A six-hole one-third semitubular plate was applied with its proximal end siting at the top of K-wires to minimise the risk of wires backing out (Fig. 10.11).
The ulnar nerve was not anteriorly transposed but was left in its natural place. After a drain was inserted, the wound was closed in layers, 1/0; 2/0 PDS and 3/0 S/C stich for the skin. The pelvic iliac wound was closed with 1/0; 2/0 PDS and 3/0 nylon for the skin. A wound dressing was applied. The tourniquet was released (tourniquet time: 1 h 50 min) and a dressing was applied to the wound. The arm was rested in a collar and cuff.
The patient has a good postoperative course without the development of any complications. Neurovascularly, she remained intact. The drain was removed at the second postoperative day. The following day she had postoperative radiographs and a CT scan and was discharged home (Fig. 10.12).
She was seen in the outpatient clinic at 12 days for wound check and removal of stiches. The microbiology samples were all negative for any pathogens. She then started gentle mobilisation of the elbow joint. She was sent to physiotherapy at 4 weeks. She was seen at regular intervals in the outpatient clinic. The fracture united at 12 weeks following surgery. At the final follow-up, 10 months after surgery, she had an excellent range of elbow motion (she lacked only 15° of full elbow extension; flexion and supination/pronation were full and pain-free) and radiographs showed union without radiological features of ectopic bone formation or implant loosening (Fig. 10.13).
Summary: Lesson Learned
Management of distal humerus fractures, particularly intra-articular with comminution, continues to be challenging injuries to reconstruct.
The goal of fracture treatment is the same like any other intra-articular fracture focusing on restoring rotation and the mechanical axis, anatomical joint reduction and fixation and early range of motion to minimise the development of joint stiffness and functional impairment. Acquisition of computed tomography is of paramount importance for accurate evaluation of the fracture lines and position of the metalwork.
When there exists comminution of the articular surfaces, angular, stable plate fixation (bridging plates) should be considered particularly in elderly patients with compromised bone stock. Plate configuration in 90° or 180° positioning as long as they are placed according to the principles of fracture fixation of periarticular fractures can be both successful. In comminuted fractures, or when revision surgery is required, an olecranon osteotomy approach can provide good exposure of the articular surface, facilitating anatomic reduction and easy placement of subchondral lag screws.
Overall, in this case the principles of fixation of intra-articular fractures were not followed leading to mal-reduction and inappropriate selection of implants for fixation inhibiting stable fixation and early range of motion. The subsequent revision performed addressed all the issues that were overlooked (fracture reduction, stable fixation) and loss of bone continuity by the implantation of autologous bone grafting. The revision of fixation strategy that was applied in this case should be considered when surgeons are dealing with analogous situations of failure of fixation of distal humerus fractures.
Further Reading
Lauder A, Richard MJ. Management of distal humerus fractures. Eur J Orthop Surg Traumatol. 2020;30(5):745–62. https://doi.org/10.1007/s00590-020-02626-1. Epub 2020 Jan 21.
Moursy M, Wegmann K, Wichlas F, Tauber M. Distal humerus fracture in patients over 70 years of age: results of open reduction and internal fixation. Arch Orthop Trauma Surg. 2022;142(1):157–64. https://doi.org/10.1007/s00402-020-03664-4.
O’Driscoll SW. The triceps-reflecting anconeus pedicle (TRAP) approach for distal humeral fractures and nonunions. Orthop Clin North Am. 2000;31(1):91–101.
O’Driscoll SW, Sanchez-Sotelo J, Torchia ME. Management of the smashed distal humerus. Orthop Clin North Am. 2002;33(1):19–33, vii 2. Shin SJ, Sohn HS, Do NH. A clinical comparison of two different double plating methods for intraarticular distal humerus fractures. J Shoulder Elb Surg. 2010;19(1):2–9.
Schneider MM, Nowak TE, Bastian L, et al. Tension band wiring in olecranon fractures: the myth of technical simplicity and osteosynthetical perfection. Int Orthop. 2014;38(4):847–55.
Yetter TR, Weatherby PJ, Somerson JS. Complications of articular distal humeral fracture fixation: a systematic review and meta-analysis. J Shoulder Elbow Surg. 2021;30(8):1957–67. https://doi.org/10.1016/j.jse.2021.02.017.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2024 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Oh, CW., Giannoudis, P.V. (2024). Distal Humerus Failed Plate Fracture Fixation. In: Giannoudis, P.V., Tornetta III, P. (eds) Failed Fracture Fixation. Springer, Cham. https://doi.org/10.1007/978-3-031-39692-2_10
Download citation
DOI: https://doi.org/10.1007/978-3-031-39692-2_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-39691-5
Online ISBN: 978-3-031-39692-2
eBook Packages: MedicineMedicine (R0)