Abstract
Purpose
The tension band wiring (TBW) technique is a common treatment for the fixation of olecranon fractures with up to three fragments. The literature and surgeons describe TBW as an uncomplicated, always available and convenient operation producing excellent results. The purpose of this study was to determine whether TBW is more ambitious than believed or the procedure provides an increased level of tolerance concerning the surgical technique.
Methods
This study reviewed 239 TBW cases in patients with olecranon fractures or osteotomies. We reviewed a total of 2,252 X-rays for ten operative imperfections: (1) nonparallel K-wires, (2) long K-wires, (3) K-wires extending radially outwards, (4) insufficient fixation of the proximal ends of the K-wires, (5) intramedullary K-wires, (6) perforation of the joint surface, (7) single wire knot, (8) jutting wire knot(s), (9) loose figure-of-eight configuration, and (10) incorrect repositioning.
Results
On average, there were 4.24 imperfections per intervention in the cases reviewed. A total of 1,014 of 2,390 possible imperfections were detected. The most frequent imperfections were insufficient fixation of the proximal ends of the K-wires (91 % of all cases), the use of a single wire knot (78 %) and nonparallel K-wires (72 %). Mayo IIa (n = 188) was the most common fracture type.
Conclusions
Our results and the number of complications described by the literature together support the conclusion that TBW is not as easy as surgeons and the literature suggest. Although bone healing and the functional results of TBW are excellent in most cases, the challenges associated with this operation are underestimated.
Level of Evidence: IV, treatment study
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fractures of the olecranon account for up to 40 % of all fractures around the elbow joint. An uncomplicated fracture of the olecranon is considered to be a common injury. The main goal of tension band wiring (TBW) is the exact repositioning of the articular surface and the re-establishment of stability in the humero-ulnar joint. The literature and surgeons refer to TBW as a simple, always available and convenient technique that can be performed by residents early in their training. In contrast to the widespread belief that TBW is an easy-to-learn and easy-to-use operative technique, the complication rate reaches up to 80 % [1–3]. The most common complications in patients undergoing TBW are pain and the need for hardware removal due to migration of the K-wires and prominence of the hardware [2–6]. Other complications have been reported in different studies, including the loss of range of motion [7–10], degenerative changes of the elbow joint [11], nerve and vascular injuries [12–14], nonunions [15], heterotopic ossification [16, 17] and infection [18, 19]. The number of complications, including the high incidence of necessary hardware removals, and recurrently suggested surgical improvements in TBW raise the question of whether the current method is up to date or a critical review of the technique is required. In this retrospective study, we want to determine if TBW is an easy-to-use technique in patients with olecranon fractures. The purpose of this study was to point out that the difficulty of TBW is underestimated because of its good outcomes. Therefore, we examined pre-, intra- and postoperative radiographs for fracture classification and imperfections in the TBW in order to prove that the technique should be used more precisely.
Materials and methods
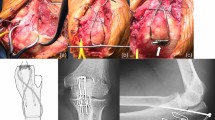
This retrospective study reviewed 233 patients (239 cases; 153 female and 86 male cases) with olecranon fractures (n = 231) or olecranon osteotomies (n = 8) undergoing tension band wiring (TBW) at five different institutions. The mean age of the patients at the time of surgery was 58 years (64.9 years for females and 45.7 years for males). This work was based on 2,252 pre-, intra- and postoperative radiographs in the anteroposterior and lateral projections (Fig. 1a and b).
Intraoperative radiographs of the elbow joint in anteroposterior and lateral projection (example for adequate, but not ‘perfect’, tension band wiring after olecranon fracture because of the use of a single wire knot, an insufficient fixation of one K-wire end and a loose figure-of-eight configuration)
Every X-ray image was reviewed and discussed with an elbow trauma specialist. The pre-operative radiographs helped to classify the fractures. We used the Mayo Clinic classification [20] as this is the most common gradation used in the clinic and allows for reliable predictions concerning the morphology and outcome of the fracture. The study included every patient diagnosed with an olecranon fracture with intraoperative or early postoperative radiographs after tension band wiring.
Mayo Clinic classification
The Mayo Clinic classification is a useful system that describes olecranon fractures based on their displacement and stability (I = stable, undisplaced; II = stable, but displaced; III = unstable due to accompanying lesions) and comminution (a = non comminuted, b = comminuted).
Intraoperative imaging provided the most precise illustration of the elbow joint and, if available, was primarily used to determine the imperfections in the TBW (for examples, see Figs. 6a,b, 7a,b, 8a,b, 9a,b and 10a, b). Intra-operative imaging allowed for an evaluation of the surgical technique immediately after the intervention when secondary complications, such as migration of K-wires, were non-existent. In cases in which intra-operative documentation was missing, we utilized early postoperative radiographs, usually taken one or two days after the operation. We identified a total of ten imperfections based on the literature and clinical knowledge (Fig. 2).
Possible imperfections of tension band wiring (modified from [21])
-
(1)
Nonparallel K-wires
Parallelism of the inserted K-wires was verified through examination of both the anteroposterior and lateral radiographs of the elbow joint. K-wires were considered nonparallel when the angle between them was greater than 5°. Parallel K-wires deliver the best force transmission [21].
-
(2)
Long K-wires
Although Prayson et al. described a maximal tolerable protrusion of 10 mm, we classified an excess length as when one of the K-wires surmounted the far cortex by twice the length of the K-wire tip. Long K-wires may cause several complications such as vascular or nerve lesions and limited mobility [13, 14, 22].
-
(3)
K-wires extending radially outwards
K-wires extending radially outwards were easily visualized in the anteroposterior projection.
-
(4)
Insufficient fixation of proximal ends of the K-wires
The proximal ends of the K-wires should be bent into a U-shape (180°) in order to fix the bent ends into the bone. The intraosseous fixation decreases complications such as wire prominence under the skin and wire migration [3].
-
(5)
Intramedullar K-wires
In the past, intramedullary placement of K-wires was a common technique in TBW. Several studies found that a transcortical fixation results in higher stability and a lower rate of wire migration [10, 23, 24]. Therefore, transcortical fixation is recommended.
-
(6)
Perforation of the joint surface
Exact repositioning without affecting the joint surface is crucial to ensure bone healing and recovery of the patient’s full range of motion. Intra-articular K-wires contribute to early revision surgery because they restrict mobility and cause possible long-term damage, including osteoarthritis.
-
(7)
Single wire knot
The AO Manual of Fracture Management states that tying the wire cerclage with one knot is sufficient. Several authors recommend the use of two wire knots to guarantee equal compression. These studies demonstrated that two wire knots provided greater stability than a single knot [25–27].
-
(8)
Jutting wire knot(s)
We classified twist ends as distant when they were not in direct contact with the bone. Jutting wire knots may lead to complications, such as pain, and necessitate hardware removal [28, 29].
-
(9)
Loose figure-of-eight configuration
The TBW technique relies on the conversion of the traction forces of the triceps muscle to compressive forces on the fracture gap to promote bone healing. Loose configurations were noted when the wire cerclage was distant from the bone or exhibited a rippled course.
-
(10)
Incorrect repositioning
Correct repositioning of the joint surface is essential in olecranon fractures. Incorrect repositioning results in complications including pain, restrictions in the range of motion and a higher rate of osteoarthritis [2, 5, 30]. We classified the repositioning as incorrect when remarkable step-offs were present or fragments were missing.
Results
The average number of observed imperfections per operation was 4.24, and no case was considered to be a flawless treatment. Surgeries with four imperfections were the most common. Five of the 239 cases had one imperfection. A total of 87.44 % (n = 209) of the reviewed cases showed three or more imperfections (Fig. 3).
Across all 239 cases, a total of 2,390 possible insufficiencies were reviewed. The total number of imperfections found was 1,014 (42.4 %). The most common imperfection was the missing proximal fixation of the K-wires, which occurred in 218 operations (91.21 %). The second most common imperfection were non-parallel K-wires (n = 171, 71.55 %). K-wires surmounting the contralateral cortex too far were observed in 153 cases (64.01 %). While a perforation of the joint surface was found in five cases, an incorrect repositioning with loose or ill-fitting fragments and joint incongruity was detected in 39.74 % of all surgeries (n = 95) (Fig. 4).
The most common fracture was the “Mayo IIa” fracture, observed in 188 cases (78.66 %). In type IIa fractures, 41.22 % of all possible imperfections were observed, corresponding to an average of 4.12 imperfections per TBW. The case with the most imperfections in a single TBW was a case of type IIa fracture that demonstrated eight of ten possible imperfections. A type IIb fracture (comminuted, dislocated and stable) occurred in 18 cases (7.53 %) and showed a total of 84 out of a possible 180 imperfections (46.67 %). Type IIa and Ib fractures had the lowest imperfection rates with 775/1880 (41.22 %) and 8/20 possible imperfections (40 %), respectively.
Displaced and unstable fractures (type IIIa: n = 5, 2.09 % and IIIb: n = 2, 0.84 % of all cases) had the highest imperfection rates, which were 27/50 (54 %) and 12/20 (60 %), respectively (Figs. 5, 6a,b, 7a,b, 8a,b, 9a,b and 10a,b).
In the group of olecranon osteotomies (n = 8, 3.34 % of all cases), we observed 42 of 80 possible imperfections (52.5 %).
Discussion
The literature and surgeons refer to TBW as a simple, cost-efficient and easily performed procedure. After reviewing 2,252 digital radiographs of patients with olecranon fractures, we conclude that this treatment is not nearly as elementary as described. Over the years, minor changes have been applied to optimize the technique of TBW, and the intra- and postoperative complications appear to be low in both frequency and severity. In contrast to the prevailing opinion, several case reports highlight major risks, such as damage to the median and anterior interosseous nerves, vascular lesions in the ulnar artery, Volkmann’s contracture, radio-ulnar synostosis, heterotopic ossification and restriction in mobility [13, 14, 17, 22, 31–33]. Most of these complications occur when the K-wires surmount the far cortex of the ulna. In our study this imperfection was present in 64.02 % (n = 153) of the cases. Attaining a minimal perforation of the contralateral bone seems to be a demanding step during the procedure. Prayson et al. stated that major complications may occur when the K-wires extend by more than 10 mm. Wu et al. developed a technique using long K-wires placed intramedullary to avoid these complications. Despite good results, this technique has not been widely applied in clinical practice [24].
The angle of the implanted K-wires is also important. K-wires that extend radially outward may impair motion during pronation and supination. K-wires that extended radially outwards were observed in 10.45 % (n = 25) of the cases. Candal-Couto et al. evaluated two patients who suffered rotational impairment after TBW. The group analyzed different forearm positions and ulnar angulations during K-wire insertion into artificially created olecranon fractures. The results showed that the rotational position plays an important role in TBW. The forearm should be maximally supinated at 30° ulnar angulation when K-wires are inserted to prevent impingement of the radius and of soft tissues, such as the biceps tendon or the supinator muscle [22].
The main postoperative patient complaints were the prominence of the K-wires under the skin, secondary dislocation and the proximal migration of the K-wires causing pain, perforation of the skin and local inflammation. These complications are influenced by the proximal intraosseous fixation of the K-wires into the bone and the missing transcortical fixation [1, 3, 5, 23, 34]. An insufficient scuttling was detected in 218 of 239 cases (91.21 %) making it the most common imperfection in our study. K-wires that are not buried can cause painful complications and enhance the risk for a secondary dislocation. Macko et al. described symptoms caused by the implants before union of the fracture in 17 of 20 cases (85 %). Fifteen of the 20 patients complained of prominent K-wires under the skin, and perforation appeared in four patients [3].
Villanueva et al. performed hardware removal in 17 of 37 cases (46 %). Skin perforation at the time of hardware removal was present in three patients (8 %) [35]. In a study by Hume et al., 42 % of the patients suffered from local discomfort due to K-wires. Migration could be detected in only one case. The authors assumed that improper coverage of the proximal ends of the K-wires might be veiled by the swollen local tissues [30].
Chalidis et al. recorded a hardware removal rate of 82.3 % (n = 51/62). Thirty four of the 51 patients (66 % of all hardware removals) complained of mild pain in daily life, and nonetheless 50 % of all 62 patients were completely satisfied with a satisfaction rate of 10 out of 10. The mean satisfaction rate was 9.3 out of 10 in all 62 patients who underwent surgery. The Mayo Elbow Performance Score (MEPS) showed excellent results in 85.5 % of the cases (n = 52) [1].
Other studies also demonstrated excellent results, although the rate of required material removal reached up to 87 % [1, 4, 7, 10, 36]. The high rate of material removal represents a second operation with additional stress on the patient, and discomfort remains in up to 66 % of patients after removal [1]. In contrast, the removal of material may diminish discomfort and increase the range of motion [9, 10]. Van der Linden et al. compared humero-ulnar mobility before (116° ± 21°) and after hardware removal (135° ± 11°) and found a significant increase in the range of motion in the patients’ elbows with hardware removal without capsulectomy. The AO modified tension band wiring technique provides superb clinical and patient satisfaction results and, therefore, has been a common method for the treatment of olecranon fractures. In our study, a comparison of the clinical outcomes to the radiographical results revealed a mean of 4.24 imperfections per operation. These imperfections were determined by highly qualified clinicians using available guidance from the literature concerning the surgical technique of TBW. None of the 239 cases could be described as flawless. TBW seems to be a sophisticated procedure that leaves a large margin for error. Nineteen years ago, Karlsson et al. stated that 96 % of the patients who were treated with different techniques after suffering olecranon fractures (conservative, TBW, figure-of-eight wire and Rush pins techniques) had excellent or good clinical results despite a reduced range of motion and degenerative changes observed in follow-up radiographs. About 50 % of the patients showed degenerative changes, but only four patients had symptoms [4]. This raises the question of whether not only TBW but olecranon fractures themselves have a tendency to yield good clinical results regardless of the chosen therapy.
Brink et al. scrutinized the tension band principle in 2012 and suggested that the fixation functions as a static compression device rather than a dynamic system. They used six fresh frozen cadaveric upper limbs treated with tension band wiring and applied various loading protocols. None of the six fractures showed secondary dislocation, but the dynamic compression of the principle tension band was only achieved when the elbow was actively extended against gravity at between 30° and 120° [37].
The main goal of a surgical intervention in patients with olecranon fractures is the correct repositioning of the joint surface. In our study, incorrect reduction was detected in 95 cases (39.7 %). A perforation of the joint surface occurred five times. Overall, joint congruity was disrupted in 100 of 239 surgical interventions.
In a study published by Hume et al., a good reduction (less than 1 mm) was achieved in only 12 of 19 patients (63 %) treated with TBW after olecranon fractures. A loss of reduction was observed in follow-up radiographs in ten of these cases [30].
Compared to the clinical outcomes of TBW reported in various publications, the results of our study suggest that olecranon fractures treated with tension band wiring require a thorough approach to minimize imperfections and to help to enhance the surgical outcome. Because of the multicenter design of this study we can exclude surgeon and surgeon’s experience bias. Despite the detected imperfections, TBW appears to be an effective procedure in various studies. Furthermore, fractures of the olecranon seem to have a tendency to heal well and produce good clinical results [4].
A limitation of this study is that it contains an evaluation of radiographs only. It is not possible to relate the imperfections observed intra-operatively to postoperative outcomes. Therefore, we cannot distinguish whether the frequency of imperfections and fracture morphology correlate with functional outcomes or if the tension band wiring technique is simply a procedure that withstands operative imperfections or probably even failures. Another limitation of this study is the method of measurement. The different manufacturers and the miscellaneous diameters of the K-wires as well as the non-standardized radiographs made it hard to evaluate the exact lengths and angles of K-wires.
The principles of the tension band wiring technique as described by the AO foundation represent a guideline for the treatment of olecranon fractures. Many surgeons intentionally use different approaches that produce similar results. Therefore, another limitation of this study is that the recommendations made by the AO foundation allow for different strategies in the treatment of olecranon fractures with TBW without being seen as incorrect.
Conclusion
With more than 40 % of all possible imperfections, our study shows that the TBW technique is not as simple as described by many clinicians. The frequent necessity of material removal due to patient discomfort and subsequent patient restrictions require a thorough approach when using TBW. Although this technique seems to tolerate imperfections and produce excellent results, further enhancements must be devised to improve the quality of patient treatment and the outcomes after tension band wiring. Applying an optimal technique may reduce both the postoperative complications and the need for secondary surgery, especially metal removal, and increase patient satisfaction.
References
Chalidis BE, Sachinis NC, Samoladas EP et al (2008) Is tension band wiring technique the “gold standard” for the treatment of olecranon fractures? A long term functional outcome study. J Orthop Surg Res 22:3–9
Helm RH, Hornby R, Miller SWM (1987) The complications of surgical treatment of displaced fractures of the olecranon. Injury 18(1):48–50. doi:10.1016/0020-1383(87)90386-X
Macko D, Szabo RM (1985) Complications of tension-band wiring of olecranon fractures. J Bone Joint Surg Am 67(9):1396–1401
Karlsson MK, Hasserius R, Karlsson C et al (2002) Fractures of the olecranon: a 15- to 25-year followup of 73 patients. Clin Orthop Relat Res 403:205–212. doi:10.1097/00003086-200210000-00030
Murphy DF, Greene WB, Gilbert JA et al (1987) Displaced olecranon fractures in adults. Biomechanical analysis of fixation methods. Clin Orthop Relat Res 224:210–214
Karlsson MK, Hasserius R, Besjakov J et al (2002) Comparison of tension-band and figure-of-eight wiring techniques for treatment of olecranon fractures. J Shoulder Elbow Surg 11(4):377–382. doi:10.1067/mse.2002.124548
Holdsworth BJ, Mossad MM (1984) Elbow function following tension band fixation of displaced fractures of the olecranon. Injury 16(3):182–187. doi:10.1016/0020-1383(84)90156-6
Horne JG, Tanzer TL (1981) Olecranon fractures: a review of 100 cases. J Trauma 21(6):469–472
Rommens PM, Küchle R, Schneider RU et al (2004) Olecranon fractures in adults: factors influencing outcome. Injury 35(11):1149–1157. doi:10.1016/j.injury.2003.12.002
Van der Linden SC, Van Kampen A, Jaarsma RL (2012) K-wire position in tension-band wiring technique affects stability of wires and long-term outcome in surgical treatment of olecranon fractures. J Shoulder Elbow Surg 21(3):405–411. doi:10.1016/j.jse.2011.07.022
Guitton TG, Zurakowski D, van Dijk NC et al (2010) Incidence and risk factors for the development of radiographic arthrosis after traumatic elbow injuries. J Hand Surg [Am] 35(12):1976–1980
Lee SH, Han SB, Jeong WK et al (2010) Ulnar artery pseudoaneurysm after tension band wiring of an olecranon fracture resulting in Volkmann’s ischemic contracture: a case report. J Shoulder Elbow Surg 19(2):e6–8. doi:10.1016/j.jse.2009.06.007
Parker JR, Conroy J, Campbell DA (2005) Anterior interosseus nerve injury following tension band wiring of the olecranon. Injury 36(10):1252–1253. doi:10.1016/j.injury.2004.12.028
Thumroj E, Jianmongkol S, Thammaroj J (2005) Median nerve palsy after operative treatment of olecranon fracture. J Med Assoc Thai 88(10):1434–1437
Korner J, Josten C, Lill H (2001) Kapitel 10: Olekranonfrakturen. In: Josten C, Lill H (eds) Ellenbogenverletzungen, vol 1, Auflage. Steinkopff-Verlag, Darmstadt, pp 151–161
Ilahi OA, Strausser DW, Gabel GT (1998) Post-traumatic heterotopic ossification about the elbow. Orthopedics 21(3):265–268
Velkes S, Tytiun Y, Salai M (2005) Proximal radio-ulnar synostosis complicating tension band wiring of the fractured olecranon. Injury 36(10):1254–1256. doi:10.1016/j.injury.2004.12.034
Gartsman GM, Sculco TP, Otis JC (1981) Operative treatment of olecranon fractures. Excision or open reduction with internal fixation. J Bone Joint Surg Am 63(5):718–721. doi:10.1016/j.jhsa.2010.08.010
Papagelopoulos PJ, Morrey BF (1994) Treatment of nonunion of olecranon fractures. J Bone Joint Surg Br 76(4):627–635
Morrey BF (1995) Current concepts in the treatment of fractures of the radial head, the olecranon, and the coronoid. J Bone Join Surg Am 77(2):316–327
Hak DJ, Stewart RL (2008) Prinzip der Zuggurtung. In: Rüedi TP, Buckley RE, Moran CG (eds) AO-Prinzipien des Frakturmanagements, vol 2, Auflage. Georg Thieme Verlag KG, Stuttgart, pp 249–254
Candal-Couto JJ, Williams JR, Sanderson PL (2005) Impaired forearm rotation after tension-band-wiring fixation of olecranon fractures: evaluation of the transcortical K-wire technique. J Orthop Trauma 19(7):480–482. doi:10.1097/01.bot.0000164338.79013.10
Mullett JH, Shannon F, Nöel J et al (2000) K-wire position in tension band wiring of the olecranon—a comparison of two techniques. Injury 31(6):427–431. doi:10.1016/S0020-1383(00)00014-0
Wu C-C, Tai C-L, Shih C-H (2000) Biomechanical comparison for different configurations of tension band wiring techniques in treating an olecranon fracture. J Trauma 48(6):1063–1067. doi:10.1097/00005373-200006000-00011
Deliyannis SN (1973) Comminuted fractures of the olecranon treated by the Weber-Vasey technique. Injury 5(1):19–24. doi:10.1016/S0020-1383(73)80004-X
Fyfe IS, Mossad MM, Holdsworth BJ (1985) Methods of fixation of olecranon fractures. An experimental mechanical study. J Bone Joint Surg Br 67(3):367–372
Mauffrey C, Krikler S (2009) Surgical techniques: how I do it? Open reduction and tension band wiring of olecranon fractures. Injury 40(4):461–465. doi:10.1016/j.injury.2008.09.026
Jensen CM, Olsen BB (1986) Drawbacks of traction-absorbing wiring (TAW) in displaced fractures of the olecranon. Injury 17(3):174–175. doi:10.1016/0020-1383(86)90326-8
Netz P, Strömberg L (1982) Non-sliding pins in traction absorbing wiring of fractures: a modified technique. Acta Orthop Scand 53(3):355–360. doi:10.3109/17453678208992228
Hume MC, Wiss DA (1992) Olecranon fractures. A clinical and radiographic comparison of tension band wiring and plate fixation. Clin Orthop Relat Res 285:229–235
Catalano LW III, Crivello K, Lafer MP et al (2011) Potential dangers of tension band wiring of olecranon fractures: an anatomic study. J Hand Surg [Am] 36(10):1659–1662. doi:10.1016/j.jhsa.2011.07.001
De Carli P, Gallucci GL, Donndorff AG et al (2009) Proximal radio-ulnar synostosis and nonunion after olecranon fracture tension-band wiring: a case report. J Shoulder Elbow Surg 18(3):e40–44. doi:10.1016/j.jse.2009.02.005
Rompen JC, Vos GA, Verheyen CC (2010) Acute ischemia of the hand seven months after tension-band wiring of the olecranon. J Shoulder Elbow Surg 19(3):e9–11. doi:10.1016/j.jse.2009.10.009
Wolfgang G, Burke F, Bush D et al (1987) Surgical treatment of displaced olecranon fractures by tension band wiring technique. Clin Orthop Relat Res 224:192–204
Villanueva P, Osorio F, Commessatti M et al (2006) Tension-band wiring for olecranon fractures: analysis of risk factors for failure. J Shoulder Elbow Surg 15(3):351–356. doi:10.1016/j.jse.2005.08.002
Romero JM, Miran A, Jensen CH (2000) Complications and re-operation rate after tension-band wiring of olecranon fractures. J Orthop Sci 5(4):318–320. doi:10.1007/s007760070036
Brink PR, Windolf M, de Boer P et al (2013) Tension band wiring of the olecranon: is it really a dynamic principle of osteosynthesis? Injury 44(4):518–522. doi:10.1016/j.injury.2012.08.052
Author information
Authors and Affiliations
Corresponding author
Additional information
Marco M. Schneider and Tobias E. Nowak contributed equally as co-first authors.
Rights and permissions
About this article
Cite this article
Schneider, M.M., Nowak, T.E., Bastian, L. et al. Tension band wiring in olecranon fractures: the myth of technical simplicity and osteosynthetical perfection. International Orthopaedics (SICOT) 38, 847–855 (2014). https://doi.org/10.1007/s00264-013-2208-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-013-2208-7