Abstract
Approximately 30% of COVID-19 cases may experience chronic symptoms, known as post-COVID-19 syndrome (PCS). Common PCS symptoms can include fatigue, cognitive impairment, and persistent physical, neurological, and neuropsychiatric complaints. To improve healthcare and management of the current and future pandemics, we highlight the need for establishing interdisciplinary post-viral outpatient clinics comprised of specialists in fields such as psychiatry, psychotherapy, neurology, cardiology, pneumology, and immunology. In this way, PCS patients with a high health burden can receive modern diagnostics and targeted therapeutic recommendations. A key objective is to distinguish the “sick recovered” from the “healthy recovered.” Our hypothesis is that there is a PCS subgroup with autoimmune-mediated systemic and brain-vascular dysregulation, which may lead to circulatory disorders, fatigue, cognitive impairment, depression, and anxiety. This can be clarified using a combination of specific antibody diagnostics and precise clinical, psychological, and apparative testing.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Although there have been over 600 million confirmed cases of coronavirus 2019 (COVID-19) worldwide [1], estimates indicate that the actual proportion is considerably higher. From March 2020 to the appearance of the omicron variant (B.1.1.529) towards the end of 2021, a statistical analysis of 190 countries and territories indicated that approximately 3.4 billion people (almost 44% of the world population) had been infected at least once by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), the pathogen responsible for COVID-19 disease [2]. A later figure was produced using the Institute for Health Metrics and Evaluation Model, which showed that the infection rate had increased to approximately 4.5 billion people (approximately 57% of the world population) by the end of January 2022 [3]. There has also been a high proportion of the population who were re-infected, particularly during the recent omicron waves [4,5,6,7]. This is likely to be due to the increased infectivity and enhanced ability of the omicron variant to evade the immune system.
Approximately one-third of COVID-19 cases may experience chronic symptoms, known as post-COVID-19 syndrome (PCS) [8, 9]. According to National Institute for Health and Care Excellence (NICE) definition, this syndrome is characterized as “signs and symptoms that develop during or after an infection consistent with COVID-19, continue for more than 12 weeks and are not explained by an alternative diagnosis” [10]. A similar clinical case definition was also put forward by the World Health Organization (WHO) [11]. However, the clinical characterization is not uniform, and the time criteria may be misleading as PCS may present with a variety of overlapping symptoms, which can fluctuate and have negative impact on many parts of the body. Common symptoms of PCS can include fatigue, cognitive impairment, as well as lasting physical and neurological or neuropsychiatric complaints [12, 13]. A meta-analysis of 68 studies comprising over 25,000 cases found that the percentage of people experiencing fatigue for 12 or more weeks after a COVID-19 diagnosis was 32% [14]. The same investigation also used a narrative synthesis of 43 studies encompassing more than 13,000 individuals, which found that 22% of these individuals exhibited cognitive impairment, as determined by a validated tool for performance-based cognitive function, clinical diagnostics, or self-report.
Although the precise cause of PCS is still not clear, many cases are associated with persistence of a proinflammatory state that may lead to an autoimmune response [15,16,17]. In the most severe cases of PCS, the latency in the effects on various organ systems resembles the course of post-infectious autoimmune diseases. As with other viral diseases, various auto-antibody-mediated syndromes such as N-methyl-D-aspartate receptor/contactin-associated protein-like 2 (NMDAR/Caspr2)-associated brain inflammation, Guillain-Barré syndrome, myasthenia, vasculitis, or postural tachycardia syndrome have been observed after SARS-COV-2 infections [18, 19].
In this paper, we review the mechanisms underlying PCS as it relates to a pro-inflammatory, autoimmune phenotype, and we describe potential treatment avenues based on these observations. We believe that surveillance gained from clinical experience during rehabilitation of PCS patients might allow identification of subgroups with similar disease mechanisms, which could inform treatment options. Finally, we highlight the need for dedicated interdisciplinary post-viral outpatient clinics so that PCS patients with a high health burden can receive modern diagnostics and targeted therapeutics.
2 The SARS-CoV-2 Structure and Molecular Mimicry
The SARS-CoV-2 structure is shown in Fig. 5.1. The key features include an encapsulated positive-sense RNA genome consisting of approximately 30 kilobases, an enveloped structure containing a nucleocapsid (N) protein which stabilizes the genomic RNA, envelope (E) and membrane (M) proteins, and exterior projections of multiple spike (S) proteins that drive the attachment and infection process of host cells [20,21,22]. The first 70% of the genome encodes two macro polypeptides termed 1a and 1b. These undergo auto-proteolysis resulting in the production of the 16 non-structural proteins (NSPs) with various functions involved in the infection and replication processes [23, 24]. The remaining 30% of the genome encodes the major structural proteins S, E, M, and N, as well as the accessory proteins encoding by ORFs 3a, 6, 7a, 7b, 8, 9b, and 10 (Table 5.1) [25, 26].
As with many other environmental factors, viruses such as Epstein-Barr virus (EBV), cytomegalovirus (CMV), human immunodeficiency virus (HIV), and SARS-CoV-2 can contribute to production of an autoimmune response in the host [18]. Yapici-Eser et al. described how some of the neuropsychiatric and other symptoms of COVID-19 disease may be explained by SARS-CoV-2 protein mimicry of multiple host protein interactions, including those involved in neuronal functions. These can include targets such as G protein-coupled receptor (GPCR; e.g., β-adrenergic, serotonin and dopamine receptors) and ion channel receptor (e.g., NMDARs) signaling pathways (Fig. 5.2a) [27]. This means that the SARS-CoV-2 antigens share similarities with endogenous host antigens. Many of these SARS-CoV-2 proteins are also capable of mimicking interactions for synaptic, mitochondrial, and inflammatory functions (Table 5.2) [27]. Another computational study identified molecular mimicry hotspots in the S protein which shared antibody binding motifs with thrombopoietin, linked with blood coagulation, and tropomyosin, associated with cardiac health, and multiple other proteins involved in platelet activation and calcium regulation (Fig. 5.2b) [28]. In line with this, several studies have detected circulating autoantibodies in serum from COVID-19 patients with prothrombotic [29, 30] and hemolytic [31] activities, as well as those suspected of having damaging effects against the vascular endothelium [32] and smooth muscle [33, 34].
(a) Possible pathophysiology of autoimmune response against host GPCR and ion channel receptors in the brain induced by SARS-CoV-2 infection. Viral particles in the bloodstream are recognized by T cells, leading to B-cell activation and sequential production of IgM and IgG antibodies Fig. 5.2 (continued) against the SARS-CoV-2 NSPs, as well as the S, E, M, and N proteins. The SARS-CoV-2-mediated endothelitis and production of IL-17 by activated T cells disrupt the blood-brain barrier, allowing these antibodies to enter the CNS. The release of IL-6 alters glial cell activity, leading to neutrophil migration, inflammation, and further BBB damage. Antibodies produced against the SARS-CoV-2 proteins produced by plasma cells in the central nervous system can cross-react as auto-antibodies with the brain receptors indicated in Table 5.2, leading to neurological and neuropsychiatric manifestations. BBB: blood-brain barrier; CNS: central nervous system; NSP: non-structural proteins. (b) Possible pathophysiological autoimmune response following SARS-CoV-2 infection against smooth muscle, endothelial proteins, phospholipids, membrane receptors and components of inflammatory pathways via mimicry of viral proteins, leading to thrombus formation in blood vessels in the brain and disruption of blood supply. RBC = red blood cell
We recently proposed that mimicry of SARS-CoV-2 NSP8 and NSP9 with NMDAR NR1 and NR2A subunit epitopes may lead to autoimmune responses against these receptors in the brain as a potential cause of anti-NMDAR encephalitis [19]. This condition is an autoimmune disorder characterized by neurological and psychosis-like symptoms [35]. In our study, we identified eight SARS-CoV-2 cases with signs of anti-NMDAR encephalitis [19]. All of these patients had antibodies against the NMDAR in their cerebrospinal fluid (CSF) and showed a recent onset of deficits in working memory, mental status, or neuropsychiatric symptoms such as confusion, agitation, hallucination, or catatonia. Interestingly, all patients showed improvement after receiving steroid-based and immunoglobulin treatments. This suggested that there is considerable scope for effective treatments that can reduce PCS neurological symptoms.
There has now been a number of reports of neurological and neuropsychiatric conditions resulting from COVID-19 infections. One study showed that 39 out of 125 COVID-19 cases with such symptoms presented with altered mental status and 23 of these fit the definitions for either recent-onset psychosis, neurocognitive decline, or an affective disorder [36]. In a study on the effects of COVID-19 infection on brain pathology, Donaud et al. investigated brain changes in 401 individuals who were scanned by magnetic resonance imaging (MRI) before and after testing positive for a COVID-19 infection [37]. This revealed a significant reduction in gray matter thickness and tissue contrast in the orbitofrontal cortex and parahippocampal gyrus, as well as changes in biomarkers of tissue damage in olfactory regions. The researchers also found a reduction in global brain size in COVID-19 cases compared to controls, and PCS patients showed a cognitive decline between the two scans.
3 Autoantibodies in PCS
In order to increase our understanding of neuropsychiatric conditions in PCS, analyses of autoimmune disorders of vascular regulation and the autonomic nervous system may be required. Although autoantibodies against GPCRs and ion channel receptors have been detected in COVID-19 disease, these have not been systematically studied in PCS. The presence of antibodies against α- and β-adrenergic, M1, M2, M3, M4, and M5 muscarinic acetylcholine, angiotensin II, and endothelin-A receptors could explain many of the symptoms such as peripheral and cerebral blood flow disturbances, cardiac arrhythmias, consequent chronic fatigue, as well as cognitive, depressive, and anxiety disorders [18, 38, 39]. To characterize such PCS cases, differential diagnosis at the clinical level is crucial to differentiate these from non-COVID-19 related mental disorders, intensive care unit (ICU) complications, reduced general conditions, or cardiac, respiratory, or renal insufficiencies.
Wallukat et al. investigated the association of neurological or cardiac symptoms with the presence of functionally active autoantibodies against GPCRs, following the acute phase of COVID-19 infection in 31 patients [40]. They found that 29 of the patients showed a spectrum of neurological symptoms such as fatigue, alopecia, and attention deficits, and 17 patients showed a combination of neurological and cardiovascular symptoms. Screening in rat neonatal cardiomyocytes revealed the presence of two to seven different GPCR autoantibodies, some of which either increased (angiotensin II type 1 receptor, α1-adrenoceptor, β2-adrenoceptor, nociceptin-like opioid receptor) or decreased (muscarinic M2-receptor, MAS-receptor, endothelin type A receptor) the heart rate. In each case, the antibodies targeted the extracellular domains of the receptors.
A recent study investigated the association of autoantibodies against GPCRs with impaired retinal microcirculation in PCS [41]. All 42 PCS patients showed seropositivity for different autoantibodies against GPCRs, while none of the controls (n = 6) did. Furthermore, a decrease in retinal vessel density was associated with autoantibodies targeting the adrenergic β2, MAS, angiotensin-II-type-1, and α1 adrenergic receptors. This suggests the possibility that techniques such as optical coherence tomography (OCT) may be useful clinical tools to search for such vascular dysregulations in the retina of PCS patients [42]. Furthermore, analyses of the blood vessels of the retina and optic nerve using OCT may lead to useful insights into the vascularization of the brain since many neurological diseases have early retinal manifestations [43, 44].
4 Autoantibody Screening and Treatment Options for PCS
Our investigation of anti-NMDAR encephalitis patients described above demonstrated the importance of early detection using antibody diagnostic screening in severe cases of COVID-19 infection [19]. We also suggest the use of electroencephalography (EEG) and CSF testing for detection of autoimmune encephalitis. Confirmed positive cases could be treated with immunotherapeutics to prevent severe neurological impairments. However, this will first require testing in large randomized trials to show that these therapies help in PCS. There are available screening panels for PCS patients to test for the presence of autoantibodies. This includes assays from CellTrend (Berlin, Germany) which test for antibodies against the M1, M2, and M5 muscarinic acetylcholine receptors, the α1- and α2- adrenergic receptors, as well as the angiotensin-II-receptor-1(AT1R) and the endothelin A receptor [45]. In addition, EUROIMMUN (Lübeck, Germany) offers tests for autoantibodies against other neurological/neuropsychiatric-related markers such as the NMDAR as well as for components of myelin and the α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) and gamma-aminobutyric acid (GABAB) receptors [46].
A case report from the eye clinic of the University Hospital of Friedrich-Alexander-Universität (FAU) gave cause for optimism that there may soon be an effective therapeutic intervention for PCS [47]. This study showed that a 59-year-old man who had been suffering from PCS was discharged symptom-free after treatment with the active substance BC 007. This compound acts to bind autoantibodies against GPCRs, including the α1-, β1-, and β2-adrenergic receptors, as well as the endothelin-A receptor, which have been implicated cardiomyopathies [48, 49]. The treatment led to an improvement in this patient in symptoms such as concentration and sense of smell, as well as blood flow in the eyes. Since this time, two further patients treated with this compound have shown improvements in their PCS symptoms [50]. Other potential treatments which have shown successful outcomes in autoimmune conditions include intravenous immunoglobulin infusion, which provides passive immune protection against multiple pathogens [51, 52] and extracorporeal apheresis [53].
5 The Case for More Studies on PCS
To improve outcomes in patients with PCS, we propose that there is an urgent need for establishment of interdisciplinary outpatient clinics dedicated to this purpose. This platform will also enable carrying out research to determine the frequency of autonomic and vascular dysregulation mediated by autoantibodies in patients with post-COVID syndrome compared to those without. For example, we propose such a clinic should perform accurate neuropsychiatric and autonomic phenotyping to increase our understanding of autoimmunity associated with the clinical presentation and complaint patterns.
5.1 The Need for Dedicated PCS Outpatient Clinics: Using Saxony-Anhalt as an Example
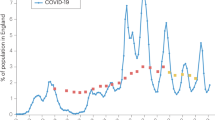
As of April 6, 2022, more than 625 thousand COVID-19 infections were detected in Saxony-Anhalt, Germany, out of approximately 2.2 million inhabitants (around 30% of the population) [54]. From this number, it is expected that 30% of the infected group will experience late and long-term health effects, based on data from the REACT-2 study in England [55]. As with many other regions in Germany and other countries, rehabilitation clinics in Saxony-Anhalt have been stretched to their capacity, and there is only one PCS outpatient clinic at Klinikum Bergmannstrost Halle [56]. Furthermore, only a small proportion of rehabilitation clinics with PCS experience and university research hospitals have shown effective interactions. The specific aims of a proposed clinic are indicated in Table 5.3. Using this interdisciplinary approach, we aim to test the hypothesis that there is a PCS subgroup with antibody-mediated vascular dysregulation that differs from other PCS cases and healthy recovered patients.
5.2 Proposed Methodology for Interdisciplinary PCS Outpatient Clinic
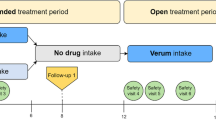
In our case, patient recruitment will occur via university hospital and rehabilitation clinics at Bad Salzelmen and Bad Suderode, Germany. Recruitment of controls will occur via the Internet. As shown in Fig. 5.3, the following information will be obtained for all patients who had been infected with COVID-19 to guide the most appropriate treatment options:
-
1.
Medical history, psychiatric, physical neurological-internal examination
-
2.
Psychological and cognitive testing
-
Current well-being/cognition: Hospital Anxiety and Depression Scale (HADS), Fatigue Scale (FS), Symptom Checklist-90-Revised (SCL-90), mini-mental state examination, Consortium to Establish a Registry for Alzheimer’s Disease (CERAD), Brief Neuropsychological Cognitive Examination (BNCE)
-
Risk/stress factors: Childhood Trauma Questionnaire (CTQ), prolonged standing strain index (PSSI)
-
-
3.
Routine laboratory blood analysis
-
4.
Autoantibody screening:
-
Screening for circulating neuronal antibodies: NMDA receptor, LGI1 (leucine-rich glioma inactivated 1), Caspr2, AMPA1/2 (α-amino-3-hydroxy-5-methyl-4-isoxazolepropionicacid 1/2) receptor, DPPX (dipeptidyl-peptidase-like protein-6), GABA-B receptor, mGluR5 (metabotropic glutamate receptor 5) and GlyR (glycine receptor)
-
Determination of circulating GPCR-antibodies: α1, α2, β1, β2-adrenergic, M1, M2, M3, M4, M5-acetylcholine, angiotensin-II and endothelin A
-
Screening for antibody-associated brain inflammation: Lumbar puncture/CSF analysis (lymphocytic pleocytosis: cell count >5/μL, CSF-specific oligoclonal bands or blood–CSF barrier impairment) and EEG (epileptic or slow-wave activity, possibly with temporal focus, “extreme delta brush”) have the highest sensitivity. Magnetic resonance imaging (MRI) is abnormal in only about 50% of patients with definite autoimmune encephalitis
-
-
5.
Cardiovascular and pulmonary diagnostics
-
ECG, heart rate variability (HRV), and echocardiography
-
In case of exertional dyspnea, chest pain, and exercise-induced tachycardia, apply spiroergometry and exercise stress test
-
In case of abnormal findings, test vascular stiffness using pulse wave velocity and microvascular changes, OCT ocular fundus to assess cerebrovascular regulation, autonomic nervous system (orthostasis test with tilt table if necessary) and sleep diagnostics (Pittsburgh Sleep Quality Questionaire [PSQI]), use of wearables devices
-
-
6.
Review of findings, differential diagnostic assessment, and therapeutic recommendation by interdisciplinary team if necessary
-
Application of machine and deep learning for selection of discriminating variables for PCS endophenotypes with GPCR-antibodies and vascular dysregulation
-
Data analysis to determine variance, correlation, factor analyses, logistic regression, cluster analyses for group comparisons regarding GPCR and other autoantibodies, their correlation with clinical-apparative findings, and identification of PCS subtypes
-
-
7.
Development of a diagnostic and treatment scheme based on clinical experience and data
Diagnostic algorithm to test for an autoimmune origin of neurological/neuropsychiatric symptoms. Since some symptoms cannot be excluded by negative findings from EEG, MRI, or CSF profile, screening should be carried out for the presence of autoantibodies to aid in stratification of the most appropriate treatment options on a case-by-case basis. Those who test positive for the presence of neuronal (left), vascular (middle), thrombotic (right), or other relevant autoantibodies can be treated with immunotherapies and other drugs as appropriate. EEG: electroencephalography; MRI: magnetic resonance imaging; CSF: cerebrospinal fluid; NMDA: N-methyl-D-aspartate, CASPR2: contactin-associated protein 2, AMPA: α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid, LGI1: leucine-rich glioma-inactivated protein 1, DPPX: dipeptidyl aminopeptidase-like protein 6, GABAB: γ-aminobutyric acid B; OCT: optical coherence tomographya
Patients found to have new onset neurological or neuropsychiatric symptoms persisting for 12 or more weeks following a COVID-19 diagnosis will be tested as above and screened for the presence of antineuronal antibodies (Fig. 5.3). Those found to be positive for neuronal or vascular-related autoantibodies can be treated as appropriate with immunotherapies and anti-inflammatory compounds to minimize neurological damage, given positive results from clinical trials.
5.3 Methodologies for Autoimmune-Associated Neuronal, Vascular, or Thrombotic Dysregulation
For patients with confirmed autoimmune encephalitis and neuropsychiatric symptoms (Fig. 5.3), the following therapeutic procedure can be followed as described previously [19, 57, 58]. Firstly, assessment and screening should be performed as described above. If anti-neuronal antibodies are detected, immunosuppression can be attempted using corticosteroid therapy (1 g methyl-prednisolone/day for 5 days), intravenous human immunoglobulin administration (0.4 g/kg/day for 5 days), or immunoadsorption or plasmapheresis for rapid removal of pathogenic autoantibodies. If there is no improvement, treatment can be extended with rituximab administration (2 × 1000 mg i.v. or s.c. 2–4 week intervals). In refractory cases, combination treatment can be performed with cyclophosphamide (750 mg/m2 body surface area every 4 weeks) and mycophenolate mofetil or methotrexate. Bortezomib may be applied (1–6 cycles of 1.3 mg/m2 body surface area, 21 days/cycle) to eliminate plasma cells in the case of patients who require artificial ventilation and do not respond adequately to the above treatments. Normalization can be assessed by clinical improvement in symptoms, and pathological cardiac MRI and EEG findings can be used to monitor treatment response. Finally, antineuronal serum and CSF antibody titres should be measured after a few weeks of treatment to determine if these have normalized.
In case of neuropsychiatric symptoms associated with clinical or apparative warning signs for autoimmune-triggered vascular dysregulation [59] or other conditions such as postural orthostatic tachycardia syndrome (POTS) [60], patients should be screened for heart rate variability (HRV), using electrocardiography (ECG), echocardiography, and spiroergometry for differentiation between cardiac, pulmonary or peripheral limitations (Fig. 5.3). If abnormalities are detected, OCT can be measured as marker for microvascular dysfunction. Screening should then be performed for GPCR autoantibody levels (α1, α2, β1, β2-adrenergic, M1, M2, M3, M4, M5-acetylcholine, angiotensin-II, endothelin A). Given the presence of autoantibodies, treatment can be performed with BC 007 to scavenge GPCR-autoantibodies with and other immunotherapies as described above.
For neuropsychiatric manifestations associated with autoimmune-associated pro-thrombotic syndromes or dyspnea [61, 62], it is recommended that patients are tested for troponin/NT-pro-BNP levels and by echocardiography, chest-X-ray, pulmonary function, and, depending on the results, MRI (Fig. 5.3). Screening should then be carried out for anti-phospholipid antibodies and other antibodies associated with thrombopoietin, tropomyosin, platelet activation, and calcium regulation. If autoantibodies are detected, immunotherapies can be performed as described above.
6 Conclusions and Future Perspectives
Given the high proportion of COVID-19 cases that result in PCS, urgent steps are required to identify those patients most at risk and to develop routine screening procedures at the clinical and molecular levels. This will enable identification of the underlying causes to facilitate the most appropriate therapeutic treatments. The consensus now appears to indicate that a high proportion of PCS cases result from inappropriate hyper-inflammatory and autoimmune states resulting from SARS-CoV-2 infection. In order to improve care of PCS patients, we aim to open an interdisciplinary PCS outpatient clinic encompassing clinical and technical teams from the fields of psychiatry, psychotherapy, neurology, immunology, cardiology, angiology, and pneumology at Otto von Guericke-University in Magdeburg, Germany. This will enable patients with a high health burden to receive modern diagnostic and competent therapeutic recommendations. The main aim is to test our hypothesis that there is a PCS subgroup with autoimmune-mediated systemic and brain-vascular dysregulation, which may lead to conditions such as circulatory disorders, fatigue, cognitive impairment, depression and anxiety. This will be assessed using a combination of specific autoantibody screening diagnostics and precise clinical, psychological, and apparative testing. This system could be used as a model for identifying those individuals most at risk of developing PCS for prevention, or for treatment-focussed clinical trials, and for planning education and rehabilitation services in the event of a continuing COVID-19 pandemic and/or the emergence of future coronavirus outbreaks.
References
COVID-19 Coronavirus Pandemic. https://www.worldometers.info/coronavirus/. Accessed August 26, 2022
COVID-19 Cumulative Infection Collaborators (2022) Estimating global, regional, and national daily and cumulative infections with SARS-CoV-2 through Nov 14, 2021: a statistical analysis. Lancet 399(10344):2351–2380
Davis A (2022) COVID Evaluation Model Estimates 57 Percent of World Population Infected at Least Once. https://www.newsweek.com/covid-evaluation-model-estimates-57-percent-world-population-infected-least-once-1672440. Accessed August 26, 2022
Pulliam JRC, van Schalkwyk C, Govender N, et al (2022) Increased risk of SARS-CoV-2 reinfection associated with emergence of Omicron in South Africa. Science 376(6593):eabn4947. https://doi.org/10.1126/science.abn4947
Phan TT, Nguyen TB, Phung QT, et al (2022) Incidence of SARS-CoV-2 Infection during the Omicron Variant Emergence in Southern Vietnam: Prior Infection versus Third-Dose Vaccination. Microbiol Spectr; Aug 24:e0117522. https://doi.org/10.1128/spectrum.01175-22
Achenbach J (2022) As the BA.5 variant spreads, the risk of coronavirus reinfection grows. https://www.washingtonpost.com/health/2022/07/10/omicron-variant-ba5-covid-reinfection/
Keane D (2022) How likely am I to be reinfected with Covid and do Omicron BA.4 and BA.5 have different symptoms? Evening Standard; July 11. https://www.standard.co.uk/news/uk/covid-how-likely-reinfected-ba4-ba5-omicron-variant-symptoms-b1011555.html
Tenforde MW, Kim SS, Lindsell CJ, et al (2020) Symptom Duration and Risk Factors for Delayed Return to Usual Health Among Outpatients with COVID-19 in a Multistate Health Care Systems Network – United States, March-June 2020. MMWR Morb Mortal Wkly Rep 69(30):993–998
Huang Y, Pinto MD, Borelli JL, et al (2021) COVID Symptoms, Symptom Clusters, and Predictors for Becoming a Long-Hauler: Looking for Clarity in the Haze of the Pandemic. medRxiv 2021.03.03.21252086. https://doi.org/10.1101/2021.03.03.21252086
National Institute for Health and Care Excellence (NICE), Scottish Intercollegiate Guidelines Network (SIGN) and Royal College of General Practitioners (RCGP) (2022) March 01; COVID-19 rapid guideline: managing the long-term effects of COVID-19. https://www.nice.org.uk/guidance/ng188/resources/covid19-rapid-guideline-managing-the-longterm-effects-of-covid19-pdf-51035515742. Accessed August 26, 2022
A clinical case definition of post COVID-19 condition by a Delphi consensus, 6 October 2021. World Health Organization. https://www.who.int/publications/i/item/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1. Accessed April 06, 2022
Renaud-Charest O, Lui LMW, Eskander S, et al (2021) Onset and frequency of depression in post-COVID-19 syndrome: A systematic review. J Psychiatr Res 144:129–137
Nalbandian A, Sehgal K, Gupta A, et al (2021) Post-acute COVID-19 syndrome. Nat Med 27(4):601–615
Ceban F, Ling S, Lui LMW, et al (2022) Fatigue and cognitive impairment in Post-COVID-19 Syndrome: A systematic review and meta-analysis. Brain Behav Immun 101:93–135
Sacchi MC, Tamiazzo S, Stobbione P, et al (2021) SARS-CoV-2 infection as a trigger of autoimmune response. Clin Transl Sci 14(3):898–907
Acosta-Ampudia Y, Monsalve DM, et al (2022) Persistent Autoimmune Activation and Proinflammatory State in Post-Coronavirus Disease 2019 Syndrome. J Infect Dis 225(12):2155–2162
Seeßle J, Waterboer T, Hippchen T, et al (2022) Persistent Symptoms in Adult Patients 1 Year After Coronavirus Disease 2019 (COVID-19): A Prospective Cohort Study. Clin Infect Dis 74(7):1191–1198
Dotan A, Muller S, Kanduc D, et al (2021) The SARS-CoV-2 as an instrumental trigger of autoimmunity. Autoimmun Rev 20(4):102792. https://doi.org/10.1016/j.autrev.2021.102792
Vasilevska V, Guest PC, Bernstein HG, et al (2021) Molecular mimicry of NMDA receptors may contribute to neuropsychiatric symptoms in severe COVID-19 cases. J Neuroinflammation 18(1):245. https://doi.org/10.1186/s12974-021-02293-x
Kim D, Lee JY, Yang JS, et al (2020) The Architecture of SARS-CoV-2 Transcriptome. Cell 181(4):914–921.e10. https://doi.org/10.1016/j.cell.2020.04.011
Jamison DA Jr, Anand Narayanan S, Trovão NS, et al (2022) A comprehensive SARS-CoV-2 and COVID-19 review, Part 1: Intracellular overdrive for SARS-CoV-2 infection. Eur J Hum Genet 30(8):889–898
Rashid F, Xie Z, Suleman M, et al (2022) Roles and functions of SARS-CoV-2 proteins in host immune evasion. Front Immunol 13:940756. https://doi.org/10.3389/fimmu.2022.940756
Rohaim MA, El Naggar RF, Clayton E, Munir M (2021) Structural and functional insights into non-structural proteins of coronaviruses. Microb Pathog 150:104641. https://doi.org/10.1016/j.micpath.2020.104641
Sun G, Xue L, He Q, et al (2021) Structural insights into SARS-CoV-2 infection and therapeutics development. Stem Cell Res 52:102219. https://doi.org/10.1016/j.scr.2021.102219
Gordon DE, Jang GM, Bouhaddou M, et al (2020) A SARS-CoV-2 protein interaction map reveals targets for drug repurposing. Nature 583(7816):459–468
Alexandersen S, Chamings A, Bhatta TR (2020) SARS-CoV-2 genomic and subgenomic RNAs in diagnostic samples are not an indicator of active replication. Nat Commun 11(1):6059. https://doi.org/10.1038/s41467-020-19883-7
Yapici-Eser H, Koroglu YE, Oztop-Cakmak O, et al (2021) Neuropsychiatric Symptoms of COVID-19 Explained by SARS-CoV-2 Proteins’ Mimicry of Human Protein Interactions. Front Hum Neurosci 15:656313. https://doi.org/10.3389/fnhum.2021.656313
Nunez-Castilla J, Stebliankin V, Baral P, et al (2022) Potential Autoimmunity Resulting from Molecular Mimicry between SARS-CoV-2 Spike and Human Proteins. Viruses 14(7):1415. https://doi.org/10.3390/v14071415
Zuo Y, Estes SK, Ali RA, et al (2020) Prothrombotic autoantibodies in serum from patients hospitalized with COVID-19. Sci Transl Med 12(570):eabd3876. https://doi.org/10.1126/scitranslmed.abd3876
Emmenegger M, Kumar SS, Emmenegger V, et al (2021) Anti-prothrombin autoantibodies enriched after infection with SARS-CoV-2 and influenced by strength of antibody response against SARS-CoV-2 proteins. PLoS Pathog 17(12):e1010118. https://doi.org/10.1371/journal.ppat.1010118
Narula S, Winkle S, Brand K, et al (2021) Hyperhemolysis in the Setting of Mixed-Autoimmune Hemolytic Anemia: A Rare Complication of COVID-19. Cureus 13(12):e20356. https://doi.org/10.7759/cureus.20356
Shi H, Zuo Y, Navaz S, Harbaugh A, et al (2022) Endothelial Cell-Activating Antibodies in COVID-19. Arthritis Rheumatol 74(7):1132–1138
Singh B, Kaur P, Maroules M (2021) Autoimmune Hepatitis-Primary Biliary Cholangitis Overlap Syndrome Triggered by COVID-19. Eur J Case Rep Intern Med 8(3):002264. https://doi.org/10.12890/2021_002264
de Vries MP, Mohammadnia N, Simsek S, Schoorl M (2022) Eosinopenia and increased markers of endothelial damage are characteristic of COVID-19 infection at time of hospital admission. Scand J Clin Lab Invest 82(4):290–295
Kayser MS, Dalmau J (2016) Anti-NMDA receptor encephalitis, autoimmunity, and psychosis. Schizophr Res 176(1):36–40
Varatharaj A, Thomas N, Ellul MA, et al (2020) Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiatry 7(10):875–882
Douaud G, Lee S, Alfaro-Almagro F, et al (2022) SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature 604(7907):697–707
Miedema J, Schreurs M, van der Sar-van der Brugge S, et al (2021) Antibodies Against Angiotensin II Receptor Type 1 and Endothelin A Receptor Are Associated With an Unfavorable COVID19 Disease Course. Front Immunol 12:684142. https://doi.org/10.3389/fimmu.2021.684142
Cabral-Marques O, Halpert G, Schimke LF, et al (2022) Autoantibodies targeting GPCRs and RAS-related molecules associate with COVID-19 severity. Nat Commun 13(1):1220. https://doi.org/10.1038/s41467-022-28905-5
Wallukat G, Hohberger B, Wenzel K, et al (2021) Functional autoantibodies against G-protein coupled receptors in patients with persistent Long-COVID-19 symptoms. J Transl Autoimmun 4:100100. https://doi.org/10.1016/j.jtauto.2021.100100
Szewczykowski C, Mardin C, Lucio M, et al (2022) Long COVID: Association of Functional Autoantibodies against G-Protein-Coupled Receptors with an Impaired Retinal Microcirculation. Int J Mol Sci 23(13):7209. https://doi.org/10.3390/ijms23137209
Bayram N, Gundogan M, Ozsaygılı C, Adelman RA (2022) Posterior ocular structural and vascular alterations in severe COVID-19 patients. Graefes Arch Clin Exp Ophthalmol 260(3):993–1004
Tsokolas G, Tsaousis KT, Diakonis VF, et al (2020) Optical Coherence Tomography Angiography in Neurodegenerative Diseases: A Review. Eye Brain 12:73–87
Augustin AJ, Atorf J (2022) The Value of Optical Coherence Tomography Angiography (OCT-A) in Neurological Diseases. Diagnostics (Basel) 12(2):468. https://doi.org/10.3390/diagnostics12020468
POTS/Long Covid-diagnostics; CellTrend; https://www.celltrend.de/en/pots-cfs-me-sfn/. Accessed September 4, 2022
EUROIMMUN Autoantibodies in neurological diseases. https://www.euroimmun.com/documents/Indications/Autoimmunity/Neurology/MAG_myelin_GAD/FA_1111_I_UK_A.pdf
Dingerman T (2022) Is an active substance against Long Covid in sight? https://www.pharmazeutische-zeitung.de/ist-ein-wirkstoff-gegen-long-covid-in-sicht-128192/#:~:text=Vier%20Long%20Covid%2DPatienten%20konnten,klinische%20Studie%20steht%20noch%20aus
Brodde OE, Hillemann S, Kunde K, et al (1992) Receptor systems affecting force of contraction in the human heart and their alterations in chronic heart failure. J Heart Lung Transplant 11(4 Pt 2):S164–74
Salazar NC, Chen J, Rockman HA (2007) Cardiac GPCRs: GPCR signaling in healthy and failing hearts. Biochim Biophys Acta 1768(4):1006–1018
Hohberger B (2021) Results of first successful treatment confirmed with two other Long COVID patients. https://www.fau.eu/2021/08/27/news/research/further-patients-benefit-from-drug-against-long-covid/
Tzilas V, Manali E, Papiris S, Bouros D (2020) Intravenous Immunoglobulin for the Treatment of COVID-19: A Promising Tool. Respiration 99(12):1087–1089
Danieli MG, Piga MA, Paladini A, et al (2021) Intravenous immunoglobulin as an important adjunct in the prevention and therapy of coronavirus 2019 disease. Scand J Immunol 94(5):e13101. https://doi.org/10.1111/sji.13101
Bornstein SR, Voit-Bak K, Donate T, et al (2022) Chronic post-COVID-19 syndrome and chronic fatigue syndrome: Is there a role for extracorporeal apheresis? Mol Psychiatry 27(1):34–37
Robert Koch-Institut: COVID-19-Dashboard. Evaluations based on the reporting data transmitted from the health authorities in accordance with IfSG. https://experience.arcgis.com/experience/478220a4c454480e823b17327b2bf1d4. Accessed April 06, 2022
Whitaker M, Elliott J, Chadeau-Hyam M, et al (2022) Persistent COVID-19 symptoms in a community study of 606,434 people in England. Nat Commun 13(1):1957. https://doi.org/10.1038/s41467-022-29521-z
Post-COVID-19 Ambulances; LONG COVID GERMANY. https://longcoviddeutschland.org/ambulanzen/. Accessed April 06, 2022
Steiner J, Prüss H, Köhler S, et al (2020) Autoimmune encephalitis with psychosis: Warning signs, step-by-step diagnostics and treatment. World J Biol Psychiatry 21(4):241–254
Pollak TA, Lennox BR, Müller S, et al (2020) Autoimmune psychosis: an international consensus on an approach to the diagnosis and management of psychosis of suspected autoimmune origin. Lancet Psychiatry 7(1):93–108
Kayser MS, Dalmau J (2011) The emerging link between autoimmune disorders and neuropsychiatric disease. J Neuropsychiatry Clin Neurosci 23(1):90–97
Zhao S, Tran VH (2022) Postural Orthostatic Tachycardia Syndrome. [Updated 2021 Aug 11]. In: StatPearls [Internet]. Treasure Island, FL, USA. https://www.ncbi.nlm.nih.gov/books/NBK541074/ (accessed October 10, 2022)
Arnson Y, Shoenfeld Y, Alon E, Amital H (2010) The antiphospholipid syndrome as a neurological disease. Semin Arthritis Rheum 40(2):97–108
Man YL, Sanna G (2022) Neuropsychiatric Manifestations of Antiphospholipid Syndrome-A Narrative Review. Brain Sci 12(1):91. https://doi.org/10.3390/brainsci12010091
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Guest, P.C. et al. (2023). A Molecular Biomarker-Based Triage Approach for Targeted Treatment of Post-COVID-19 Syndrome Patients with Persistent Neurological or Neuropsychiatric Symptoms. In: Guest , P.C. (eds) Application of Omic Techniques to Identify New Biomarkers and Drug Targets for COVID-19. Advances in Experimental Medicine and Biology(), vol 1412. Springer, Cham. https://doi.org/10.1007/978-3-031-28012-2_5
Download citation
DOI: https://doi.org/10.1007/978-3-031-28012-2_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-28011-5
Online ISBN: 978-3-031-28012-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)