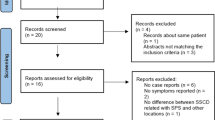
Abstract
The concept of the third mobile labyrinthine window (TMW) was for the first time used by Cawthorne to describe the principle of semicircular canal (SC) fenestration in patients with advanced otosclerosis [1]. Minor et al. [2] and Smullen et al. [3] described the first clinical observations of superior semicircular canal dehiscence (SSCD) as a distinctive clinical form of spontaneous (or primary) third window abnormality. Merchant et al. further issued the hypothesis regarding the mechanism of this type of conductive hearing loss of the inner ear [4]. Since the 2000s, we have witnessed the progressive appearance of TMW variants with similar clinical and audiological features [5]. The broader concept of otic capsule dehiscence syndrome proposed by Wackym et al. refers to all pathologies of the TMW spectrum whose symptoms, clinical signs, and audiometric aspects correspond to bony defects of the otic capsule confirmed by tomodensitometry [6]. On an anatomical-radiological basis, a classification of TMW subtypes based on anatomical and radiological aspects has recently been proposed [7]. It also includes some intralabyrinthine pathologies that mimic the clinical presentation of a “classical” TMW.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Endovascular treatment
- Third mobile window syndrome
- Otic capsule dehiscence
- Vascular dehiscence
- High riding jugular bulb
- Superior petrosal sinus
Introduction
The concept of the third mobile labyrinthine window (TMW) was for the first time used by Cawthorne to describe the principle of semicircular canal (SC) fenestration in patients with advanced otosclerosis [1]. Minor et al. [2] and Smullen et al. [3] described the first clinical observations of superior semicircular canal dehiscence (SSCD) as a distinctive clinical form of spontaneous (or primary) third window abnormality. Merchant et al. further issued the hypothesis regarding the mechanism of this type of conductive hearing loss of the inner ear [4]. Since the 2000s, we have witnessed the progressive appearance of TMW variants with similar clinical and audiological features [5]. The broader concept of otic capsule dehiscence syndrome proposed by Wackym et al. refers to all pathologies of the TMW spectrum whose symptoms, clinical signs, and audiometric aspects correspond to bony defects of the otic capsule confirmed by tomodensitometry [6]. On an anatomical-radiological basis, a classification of TMW subtypes based on anatomical and radiological aspects has recently been proposed [7]. It also includes some intralabyrinthine pathologies that mimic the clinical presentation of a “classical” TMW.
In the classification mentioned above, type II otic capsule dehiscence corresponds to an abnormal contact between the membranous labyrinth and a vascular structure (venous or, less frequently, arterial structure) facilitated by the lack of bony otic capsule. In these TMW variants, the pathomechanism is not yet fully understood. Nonetheless, it can be assumed that non-physiological audio-vestibular stimulation is mainly produced by the pulsating energy of the vascular wall transmitted through the TMW interface to the membranous labyrinth. Obviously, this stimulation would be greater in the case of moderate or intense physical effort as the acceleration of the heart rate and increased cardiac output promotes the appearance of vertigo and tinnitus. This also explains the recurrent presence of pulsatile tinnitus in these variants [8]. When in contact with the perilymphatic space, the vibrations generated by the vascular wall can generate symptoms of different intensities, which depend on the location, surface, and the importance of any mass effect exerted by the vessel on the labyrinthine structure [9]. Other symptoms, including hearing loss, are due to the acoustic energy shunt carried by the vibrating perilymphatic fluid to the zone of minimal resistance generated by the dehiscence, as seen in the classic description of the TMW mechanism.
Three subvariants of labyrinthine-vascular dehiscence will be considered here, as they are accessible for endovascular management.
-
The most common symptomatic labyrinthine-vascular TMW subvariant found in our practice involves the vestibular aqueduct (VA) and a high-riding jugular bulb (HRJB). HRJB is an irregular outpouching or protrusion of the vessel that may project into the middle ear cavity, mastoid cavity, or medially toward the petrous apex. The jugular bulb is localized in the upper part of the internal jugular vein and is in close relation with anatomic structures such as the inner ear, carotid artery, and the cranial nerves that pass through the jugular foramen. Jugular bulb abnormalities (JBAs) affect up to 15% of the general population [10] but only very few of these patients are symptomatic. JBAs include high-riding jugular bulb (HRJB), located higher than the basal turn of the cochlea or more than 2 mm from the floor of the internal auditory canal [11], and jugular bulb diverticulum defined as an irregular outpouching issued from the bulb [12]. Venous hypertension and/or turbulent venous flow in the Internal Jugular Vein (IJV) has been suggested as a possible etiologic factor for venous diverticulum with erosion of the overlying bone causing dehiscence through the otic capsule and adjacent structures [13]. Based on various anatomic observations, Couloigner et al. postulated that high jugular bulbs could induce Ménière’s disease by a direct or indirect effect on the endolymphatic duct and/or sac, producing a decrease in endolymph resorption [14].
-
The second most frequent symptomatic labyrinthine-vascular dehiscence variant involves a HRJB and the posterior semicircular canal (PSC). It should be noted that symptomatic JBAs could be underdiagnosed, and no consensual management has been established. When the symptoms are well tolerated, a “wait-and-see” policy can be adopted [10]. Otherwise, some invasive surgical techniques have been used, such as ligation [15], embolization of the IJV, or surgical lowering of the HRJB [14]. This carries out a high risk of facial palsy, sensorineural hearing loss, jugular hemorrhage, or thrombosis [16]. Alternatively, an endovascular stent-assisted coil implantation has recently been described [17]. The endovascular stent-assisted coil placement technique has been recognized as a safe and effective technique for many years in the treatment of unruptured wide-neck intracranial aneurysms [18]. A similar endovascular technique has been used in the jugular bulb to treat pulsatile tinnitus [19, 20].
-
The less frequent labyrinthine-vascular dehiscence (or type II TMW) involves the SSC and the superior petrous sinus (SPS). SSCD by the SPS accounts for 4% to 9% of ears in symptomatic SSCD [21]. Until recently, a surgical procedure like the one proposed in SSCD described by Minor was considered as the only effective method for disabling SPS [22, 23]. Middle cranial fossa or transmastoid approaches are used [24, 25] to reach the dehiscence, and techniques such as plugging, capping or both methods combined can be used to treat this variant. Resurfacing and/or plugging via a middle fossa craniotomy in patients with SSCD by SPS implies mobilizing the SPS which may cause bleeding, thrombosis or complications related to the surgical approach [22, 25, 26]. Recently, an innovative endovascular treatment was proposed [27]. Its principle is to reinforce the vascular wall in contact with the membranous SSC by placing a stent at that level. This procedure aims at reducing the minimal resistance at the dehiscence level, the hypothesis being that the stent rigidifies the SPS walls, minimizing the venous pulsation transmission to the inner ear end organs.
Preliminary Otoneurological and Radiological Investigations
Otoneurological assessment of SSCD classically includes pure tone audiometry showing low-frequency negative bone conduction thresholds on the dehiscent side, and enhanced vestibular-evoked myogenic potentials (VEMPs) responses in air conduction [28]. For other TMWs such as dehiscence related to an IJV interface and labyrinthine structures, there are no recommendations although a similar assessment seems well advised.
Commonly, a CT scan of the temporal bone in infra millimetric sections is the gold standard to detect the bony defect [29, 30]. In case of dehiscence involving the jugular bulb, axial slice images are performed, centered on the IJV often associated with a HRJB position (Fig. 16.1a, b). This variant is often observed on the right side, for hemodynamic reasons [31].
In case of dehiscence involving the SPS, a “classic” SSCD image is detected in the plane of this canal (Pöschl plane). However, this image is often more medially located than in a SSCD of the labyrinthine-meningeal interface and has the shape of a “cookie bite” [21] (Fig. 16.2a). We observe the SPS opacification after injection, in the venous phase. MRI of the petrosal bone and inner ear structures has the advantage of being able to improve the diagnosis, and to identify the vascular structure causing the dehiscence [9]. Particularly, 3D T1 weighted sequences can show SPS opacification, and high-resolution labyrinthine sequence 3D T2 could help show the membranous labyrinth morphology and patency [9].
(a) high-resolution computed tomography (HRCT) Pöschl plane. “Cookie bite” aspect, SSCD by SPS (length measured at 1.7 mm). (b) Fusion between HRCT and 3D T1 weighted enhanced sequence. (c) Fusion between 3D T1 weighted enhanced and T2 HR sequences. Compression effect on the SSC (arrow). SSCD superior semicircular canal dehiscence, SPS superior petrosal sinus
Fusion imaging between HRCT Pöschl plane or 3D T2 and 3D T1 weighted enhanced sequence could help in visualizing the TW’s interface (dimensions of the SPS, interface surface, or contact surfaces between vestibular membrane (s) and the walls of the SPS, and an eventual compression effect on the membranous SSC) [9] (Fig. 16.2b, c).
The importance of combining the standard HRCT with 3T MRI to allow a better visualization of the membranous SSC, and an eventual mass-effect by the adjacent SPS at the dehiscence level, has already been described [9].
Before any endovascular procedure, it is essential to check the neuro-vascular anatomy as well as the risk of bleeding. If an endovascular management is chosen to treat a dehiscence between an HRBJ and the VA or between the HRBJ and a PSC, an evaluation of the IJV in the venous phase of an arteriography carried out by selective catheterization of the ipsilateral internal carotid artery is systematically performed, generally one week before the treatment.
In the case of an SSCD by SPS, the shape and size of the cavernous sinus and the inferior petrosal sinus are assessed to assure retrograde access to the SPS. To avoid possible negative hemodynamic consequences in the venous cerebral circulation in case of SPS thrombosis, alternative accessible retrograde drainage of the SPV through the IJV should be checked beforehand. In addition, if significant anatomic variations of the petrosal venous system (inferior or superior petrosal sinus narrowing or hypoplasia) are found during the preliminary evaluation, stenting of the SPS is not recommended.
Obviously, as for any invasive procedure, the patient must take the decision after being informed of the risks and benefits of the procedure.
Standardized quality of life questionnaires should be used to assess the daily discomfort. The Dizziness Handicap Inventory (DHI) scale in three functional stages proposed by Jacobson and Newman [32] and the Tinnitus Handicap Inventory (THI) scale, classifying tinnitus according to the impact on daily life, [33] seem useful in SSCD [9, 34].
Surgical Treatment
Invasive surgical techniques have been properly described previously. These techniques include ligation, embolization of the jugular vein, or surgical lowering of the HRBJ [18]. The later latter technique requires a deep mastoidectomy with drilling close to the facial nerve, inner ear, and jugular bulb to lower the vein and reconstruct the bony labyrinth with bone dust or cartilage [14, 16].
Endovascular Management
The aim of endovascular management consists in limiting the transmission of vibrations from the vascular wall to the labyrinthine end organs. The TW variants mentioned above can benefit nowadays from alternative endovascular options. These appear to be more conservative than classical surgery, which in some cases may involve sacrificing the venous structures at the origin of possible disturbances of the normal venous return to the base of the skull. In addition, endovascular treatment techniques appear to have an advantage over “classical” surgical techniques because these techniques do not involve manipulating the membranous labyrinth during endovascular procedures. Thus, the risk of hearing or vestibular impairment is estimated to be lower. In fact, the very principle of the endovascular procedure, which aims only to strengthen the vascular resistance at the interface of the dehiscence of the otic capsule, guarantees the preservation of the vestibular function. Thus, in principle, the endovascular procedure is completely opposite to the plugging surgical treatment techniques that propose the anatomical exclusion of SSC involved in non-physiological vestibular stimulation.
Vestibular Aqueduct: Jugular Bulb Dehiscence
The decision to perform endovascular treatment is mutually agreed upon by head and neck surgeons and the neuro-interventional team and is suggested to the patient as an alternative to surgery. Clinicians need to look for signs of Ménière’s-like syndrome due to VA compression by JBA [35] as Ménière’s syndrome may require a specific treatment, including surgical endolymphatic sac surgery [36].
In case of symptoms due to TW, stent-assisted coil implantation of the JBAs is minimally invasive, preserves venous cerebral blood flow, and gives immediate positive results for pulsatile tinnitus and vertigo [17].
The treatment itself takes place under general anesthesia in a neuro-angiographic suite, after a bolus of heparin. A venous access is performed uni or bilaterally, after femoral venous puncture or direct jugular approach for microcatheter insertion. The guiding catheter is slipped in the jugular vein and two microcatheters are used, one guided in the transverse sinus upstream to the dehiscence to introduce the stent and the other in the outpouching to block it with coils (“jailing technique”).
Technically the dehiscence is managed as an aneurysm supplanting the vein, whose treatment is obstruction by placing coils within it, under the protection of a stent forcing the coils to remain in place. The venous sinus thus remains permeable. A stent is deployed to cover the outpouching from top to bottom (Fig. 16.3a, b). If stent deployment is incomplete, it is expanded by stent angioplasty with the use of the same guidewire and a monorail dilation balloon. It is important to perform these stent angioplasties over the jugular foramen to avoid possible compression of the cranial nerves contained in the pars nervosa. Finally, the outpouching is packed with detachable bare coils or hydrocoils through the microcatheter (Fig. 16.3a, b). The number of coils depends on the size and filling of the JBA.
Endovascular procedure for dehiscence of the jugular gulf with the VA. (a) Radiography. Coils and stents in place in the right IJV. (b) Schematic representation of the jailing technique. IJV internal jugular vein. Endolymphatic sac and duct (vestibular aqueduct - VA) are displayed in green and brown respectively
At the end of the procedure, the microcatheter is gently removed from the outpouching without disturbing the stent position.
The management of antiplatelet therapy varies; frequently, one antiplatelet drug (clopidogrel) is given for one week before the implantation and is maintained for several months (usually for six months). Some prefer to prescribe two antiplatelet drugs, such as clopidogrel and aspirin.
An immediate postprocedural angiogram can show the placement of the material, with neither coil migration nor interruption of normal venous flow. When performed, postoperative CT scan allows the opportunity to see the coils (metallic artifact) in contact with the dehiscence (see Fig. 16.4 for pre-(a, b) and post-endovascular procedure aspects (c)).
(a) right axial petrosal bone high-resolution computed tomography (HRCT). VA in contact with HRJB (black arrow). (b) Fusion between HRCT and 3D T1 weighted enhanced sequence of the right petrosal bone—coronal. (c) CT—control post treatment: metallic artifact image due to the coils in contact with the right bony labyrinthine structure
Posterior Semicircular Canal: Jugular Bulb Dehiscence
Although the authors have not yet had any case of this type of dehiscence under clinical observation for which such a treatment could be chosen, we estimate that a similar technique as described above can be successfully applied in this variant.
Dehiscence of the SSCD Involving the Superior Petrous Sinus (SPS)
The first endovascular treatment reported for this variant consisted in stenting the SPS [27]. A standard femoral vein puncture was made under general anesthesia and 500 mg of IV aspirin was injected per procedure. A six French guiding catheter with guide wire was moved forward into the right inferior petrosal sinus, guided by digital subtraction imaging. After accessing the right cavernous sinus, a venogram with retrograde opacification confirmed the presence of a complete petrosal venous system (Fig. 16.5a) Alternatively, the access to the SPS could be made homolaterally to the pathology by catheterization of the SPS abutment in the transverse sinus if the obtuse angle between the two venous structures is sufficiently accessible for navigation. Therefore, the angle formed by SPS with the transverse sinus should be evaluated before choosing the access via the inferior petrosal sinus and cavernous sinus. A single catheter in the SPS will allow the introduction of a stent which has a metal cover and sufficient rigidity to isolate the third window; the stent is placed distally to the cavernous sinus avoiding the obstruction of the superior petrosal vein (SPV) junction to the SPS (Fig. 16.5b). Its size must be chosen with caution, in order to avoid migration or, on the contrary, to avoid labyrinth compression. At the end of the procedure, a venogram showed the patency of both SPS and SPV (Fig. 16.5c). Then, the guidewire and microcatheter are gently withdrawn.
Another case of endovascularly treated SSCD by SPS has been reported in the literature, using a technique inspired by the one described above. The authors preferred a coiled SPS thrombosis, a method justified by the presence of a large arachnoid granulation, visualized by angio-MRI. This endovascular procedure was facilitated by the configuration of the deep petrosal venous system. The preoperative anatomic workup had estimated that sacrificing the SPS would leave sufficient alternative venous routes to drain the cavernous sinus and jugular bulb [37].
Post-Treatment Findings
Postoperative clinical assessment often reveals immediate relief of the pulsatile tinnitus. Despite the good results we have obtained and although we have no complications in our small series, these techniques still present a theoretical risk of coil migration and stent thrombosis. The risk of stent thrombosis extrapolated from larger series of venous stents in the transverse sinus seems to be limited. Ahmed et al. reported 52 cases of bilateral transverse sinus stent placement for idiopathic intracranial hypertension without any stent thrombosis or thromboembolic complications [38]. Apart from this, it is known that the peripetrosal sinuses are created by the reflections of the meningeal and periosteal layers of the dura mater, being relatively tense, lined with endothelial cells, which would theoretically limit the risk of thrombosis [39].
A short hospitalization of two days is preferable for anticoagulant treatment surveillance. As the technique uses coils, the same antiplatelet management as described above is recommended after embolization. The rationale for double anti-aggregation in the case of venous stents is not always justified in the absence of a personal history of venous thrombosis. Follow-up angiography at one year may be performed to evaluate the permeability of the stent with stable exclusion of the JBA.
Conclusion
In selected patients, first-line endovascular treatment for vestibular-vascular dehiscence emerges as a new, elegant, and apparently safe alternative to existing surgical techniques. Its principle relies on strengthening the endovascular of the third mobile interface to avoid the transfer of acoustic and/or vibratory energy from the vascular structure to the sensory organs of the inner ear. In addition to classical audiological, vestibular and radiological examinations to diagnose a TMW, additional angio-MRI should be performed in these variants to verify the integrity of the peripetrosal venous circulation.
Obviously our series is still small, our experience being limited to not more than 20 endovascularly treated patients. Therefore, before concluding on the effectiveness and especially the safety of this method, more patients with disabling symptoms should first benefit from it and be followed up enough to assess the real benefit/risk ratio.
References
Cawthorne T. Otosclerosis. J Laryngol Otol. 1955;69:437–56. https://doi.org/10.1017/S0022215100050933.
Minor LB, Solomon D, Zinreich JS, Zee DS. Sound- and/or pressure-induced vertigo due to bone dehiscence of the superior semicircular canal. Arch Otolaryngol Head Neck Surg. 1998;124(3):249–58. https://doi.org/10.1001/archotol.124.3.249.
Smullen JL, Andrist EC, Gianoli GJ. Superior semicircular canal dehiscence: a new cause of vertigo. J Louisiana State Med Soc. 1999;151:397–400.
Merchant SN, Rosowski JJ, McKenna MJ. Superior semicircular canal dehiscence mimicking otosclerotic hearing loss. Adv Otorhinolaryngol. 2007;65:137–45. https://doi.org/10.1159/000098790.
Ho ML, Moonis G, Halpin CF, Curtin HD. Spectrum of third window abnormalities: semicircular canal dehiscence and beyond. AJNR Am J Neuroradiol. 2017;38(1):2–9. https://doi.org/10.3174/ajnr.A4922.
Wackym PA, Wood SJ, Siker DA, Carter DM. Otic capsule dehiscence syndrome: superior semicircular canal dehiscence syndrome with no radiographically visible dehiscence. Ear Nose Throat J. 2015;94:E8–24. https://doi.org/10.1177/014556131509400802.
Reynard P, Idriss S, Ltaief-Boudrigua A, Bertholon P, Pirvan A, Truy E, Thai-Van H, Ionescu EC. Proposal for a unitary anatomo-clinical and radiological classification of third mobile window abnormalities. Front Neurol. 2022;12:792545. https://doi.org/10.3389/fneur.2021.792545.
Liu Z, Bi W, Li J, Li Q, Dong C, Zhao P, et al. Superior semicircular canal dehiscence in relation to the superior petrosal sinus: a potential cause of pulsatile tinnitus. Clin Radiol. 2015;70:943–7. https://doi.org/10.1016/j.crad.2015.04.017.
Ionescu E, Reynard P, Coudert A, Roiban L, Boudrigua AL, Thai-Van H. Superior semicircular canal dehiscence by superior petrosal sinus: proposal for classification. J Int Adv Otol. 2021;17:35–41. https://doi.org/10.5152/iao.2020.9384.
Friedmann DR, Eubig J, Winata LS, Pramanik BK, Merchant SN, Lalwani AK. A clinical and histopathologic study of jugular bulb abnormalities. Arch Otolaryngol Head Neck Surg. 2012a;138(1):66–71. https://doi.org/10.1001/archoto.2011.231.
Friedmann DR, Le BT, Pramanik BK, Lalwani AK. Clinical spectrum of patients with erosion of the inner ear by jugular bulb abnormalities. Laryngoscope. 2010;120(2):365–72. https://doi.org/10.1002/lary.20699.
Friedmann DR, Eubig J, Winata LS, Pramanik BK, Merchant SN, Lalwani AK. Prevalence of jugular bulb abnormalities and resultant inner ear dehiscence: a histopathologic and radiologic study. Otolaryngol Head Neck Surg. 2012b;147(4):750–6. https://doi.org/10.1177/0194599812448615.
Otto KJ, Hudgins PA, Abdelkafy W, Mattox DE. Sigmoid sinus diverticulum: a new surgical approach to the correction of pulsatile tinnitus. Otol Neurotol. 2006;28:48–53.
Couloigner V, Grayeli AB, Bouccara D, Julien N, Sterkers O. Surgical treatment of the high jugular bulb in patients with Meniere’s disease and pulsatile tinnitus. Eur Arch Otorhinolaryngol. 1999;256(5):224–9. https://doi.org/10.1007/s004050050146.
Berguer R, Nowak P. Treatment of venous pulsatile tinnitus in younger women. Ann Vasc Surg. 2015;29(4):650–3.
El-Begermy MA, Rabie AN. A novel surgical technique for management of tinnitus due to high dehiscent jugular bulb. Otolaryngol Head Neck Surg. 2010;142(4):576–81. https://doi.org/10.1016/j.otohns.2009.12.007.
Hitier M, Barbier C, Marie-Aude T, Moreau S, Courtheoux P, Patron V. New treatment of vertigo caused by jugular bulb abnormalities. Surg Innov. 2014a;21(4):365–71. https://doi.org/10.1177/1553350613505918.
Thénint MA, Barbier C, Hitier M, Patron V, Saleme S, Courthéoux P. Endovascular treatment of symptomatic vestibular aqueduct dehiscence as a result of jugular bulb abnormalities. J Vasc Interv Radiol. 2014;25:1816–20. https://doi.org/10.1016/j.jvir.2014.07.013.
Gard AP, Klopper HB, Thorell WE. Successful endovascular treatment of pulsatile tinnitus caused by a sigmoid sinus aneurysm. A case report and review of the literature. Interv Neuroradiol. 2009;15(4):425–8. https://doi.org/10.1177/159101990901500409.
Signorelli F, Mahla K, Turjman F. Endovascular treatment of two concomitant causes of pulsatile tinnitus: sigmoid sinus stenosis and ipsilateral jugular bulb diverticulum. Case report and literature review. Acta Neurochir. 2012;154(1):89–92. https://doi.org/10.1007/s00701-011-1202-3.
Schneiders SMD, Rainsbury JW, Hensen EF, Irving RM. Superior petrosal sinus causing superior canal dehiscence syndrome. J Laryngol Otol. 2017;131:593–647. https://doi.org/10.1017/S0022215117001013.
Koo JW, Hong SK, Kim DK, Kim JS. Superior semicircular canal dehiscence syndrome by the superior petrosal sinus. J Neurol Neurosurg Psychiatry. 2010;81:465–7. https://doi.org/10.1136/jnnp.2008.155564.
Lookabaugh S, Kelly HR, Carter MS, Niesten ME, McKenna MJ, Curtin H, Lee DJ. Radiologic classification of superior canal dehiscence: implications for surgical repair. Otol Neurotol. 2015;36(1):118–25. https://doi.org/10.1097/MAO.0000000000000523.
Ziylan F, Kinaci A, Beynon AJ, Kunst HP. A comparison of surgical treatments for superior semicircular canal dehiscence: a systematic review. Otol Neurotol. 2017;38:1–10. https://doi.org/10.1097/MAO.0000000000001277.
Ward BK, Agrawal Y, Nguyen E, Della Santina CC, Limb CJ, Francis HW, et al. Hearing outcomes after surgical plugging of the superior semicircular canal by a middle cranial fossa approach. Otol Neurotol. 2012;33:1386–91. https://doi.org/10.1097/MAO.0b013e318268d20d.
McCall AA, McKenna MJ, Merchant SN, Curtin HD, Lee DJ. Superior canal dehiscence syndrome associated with the superior petrosal sinus in pediatric and adult patients. Otol Neurotol. 2011;32:1312–9. https://doi.org/10.1097/MAO.0b013e31822e5b0a.
Ionescu EC, Coudert A, Reynard P, Truy E, Thai-Van H, Ltaief-Boudrigua A, Turjman F. Stenting the superior petrosal sinus in a patient with symptomatic superior semicircular canal dehiscence. Front Neurol. 2018;9:689. https://doi.org/10.3389/fneur.2018.00689.
Ward BK, van de Berg R, van Rompaey V, Bisdorff A, Hullar TE, Welgampola MS, Carey JP. Superior semicircular canal dehiscence syndrome: Diagnostic criteria consensus document of the committee for the classification of vestibular disorders of the Bárány Society. J Vestib Res. 2021;31(3):131–41. https://doi.org/10.3233/VES-200004.
Belden CJ, Weg N, Minor LB, Zinreich SJ. CT evaluation of bone dehiscence of the superior semicircular canal as a cause of sound and/or pressure-induced vertigo. Radiology. 2003;226:337–43. https://doi.org/10.1148/radiol.2262010897.
Ward BK, Carey JP, Minor LB. Superior Canal dehiscence syndrome: lessons from the first 20 years. Front Neurol. 2017;8:177. https://doi.org/10.3389/fneur.2017.00177.
Friedmann DR, Eubig J, McGill M, Babb JS, Pramanik BK, Lalwani AK. Development of the jugular bulb: a radiologic study. Otol Neurotol. 2011;32(8):1389–95. https://doi.org/10.1097/MAO.0b013e31822e5b8d.
Jacobson GP, Newman CW. The development of the dizziness handicap inventory. Arch Otolaryngol Head Neck Surg. 1990;116:424–7. https://doi.org/10.1001/archotol.1990.01870040046011.
Newman CW, Jacobson GP, Spitzer JB. Development of the Tinnitus Handicap Inventory. Arch Otolaryngol Head Neck Surg. 1996;122(2):143–8. https://doi.org/10.1001/archotol.1996.01890140029007.
Crane BT, Minor LB, Carey JP. Superior canal dehiscence plugging reduces dizziness handicap. Laryngoscope. 2008;118(10):1809–13. https://doi.org/10.1097/MLG.0b013e31817f18fa.
Hitier M, Roger V, Moreau S, Patron V. High jugular bulb in a cohort of patients with definite Ménière’s disease. J Laryngol Otol. 2014b;128(12):1125.
Gendre A, Bourget-Aguilar K, Calais C, Espitalier F, Bordure P, Michel G. Evaluation of vestibular function following endolymphatic sac surgery. Eur Arch Otorhinolaryngol. 2022;279(3):1193–201. https://doi.org/10.1007/s00405-021-06743-3.
Aw GE, Parker GD, Halmagyi GM, Saxby AJ. Pulsatile tinnitus in superior semicircular canal dehiscence cured by endovascular coil occlusion of the superior petrosal sinus. Otol Neurotol. 2021;42(5):e629–30. https://doi.org/10.1097/MAO.0000000000003012.
Ahmed RM, Wilkinson M, Parker GD, Thurtell MJ, Macdonald J, McCluskey PJ, Allan R, Dunne V, Hanlon M, Owler BK, Halmagyi GM. Transverse sinus stenting for idiopathic intracranial hypertension: a review of 52 patients and of model predictions. AJNR Am J Neuroradiol. 2011;32(8):1408–14. https://doi.org/10.3174/ajnr.A2575.
Miyawaki EK. Encyclopedia of the neurological sciences. 2nd ed. Cambridge, MA: Academic Press; 2014.
Acknowledgment
The authors thank Ruxandra C. Ionescu for checking the accuracy of translation in English for this chapter.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Reynard, P., Ionescu, E., Hitier, M., Barbier, C., Turjman, F. (2022). Endovascular Therapy for Third Mobile Window Syndrome. In: Gianoli, G.J., Thomson, P. (eds) Third Mobile Window Syndrome of the Inner Ear. Springer, Cham. https://doi.org/10.1007/978-3-031-16586-3_16
Download citation
DOI: https://doi.org/10.1007/978-3-031-16586-3_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-16585-6
Online ISBN: 978-3-031-16586-3
eBook Packages: MedicineMedicine (R0)