Abstract
Purpose
To evaluate objective vestibular function after endolymphatic sac surgery (ELSS) for Menière’s disease (MD), using comparative vestibular function tests: videonystagmography (VNG), vestibular evoked myogenic potentials (VEMP) and video head-impulse test (VHIT)
Methods
Patients with definite MD using the American Academy of Otolaryngology—Head and Neck Surgery (AAO-HNS) of 1995 criteria modified in 2015 and treated with ELSS (sac decompression or sac opening) were included. The primary outcome was the preservation of vestibular function, comparing pre- and postoperative vestibular function tests: VNG, VEMP, VHIT. Secondary outcomes were control of episodes of vertigo, hearing outcome using AAO-HNS criteria, and QoL using the Menière’s disease outcome questionnaire.
Results
73 patients were included in the study. We found a significant preservation of vestibular function as measured by VNG and VHIT. There was no statistical difference in the presence or absence of cervical and ocular (P13/N23 and N1/P1) waves on VEMP pre- and postoperatively. 67% of patients had good control of episodes of vertigo post-operatively, with significantly better results in the sac opening group (75%). There was no significant change in hearing postoperatively, and QoL scores were significantly improved after surgery (p < 0.0001).
Conclusion
Endolymphatic sac surgery (ELSS) is a conservative surgical treatment, which does not negatively impact vestibular function. It was associated with improved control of episodes of vertigo, preservation of hearing, and a clear improvement in QoL scores. Despite its pathophysiology not being fully understood, it remains a first-line procedure preserving vestibular function, for MD refractory to medical management.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Objective
Endolymphatic sac surgery (ELSS) is recognized as third-line treatment for Menière’s disease (MD) for patients who do not respond to medical treatment [1]. The rationale for ELSS is based on the pathophysiology of MD relating to endolymphatic hydrops.
The effects of this surgery have long been criticized after two Danish comparative studies were published [2, 3]. More recently, a Cochrane meta-analysis and an International Consensus (ICON) have given a grade B recommendation in favor of ELSS. They concluded that it should be considered as the next option after failure of conservative medical treatment, especially if hearing is preserved [1, 4]. In contrast to chemical labyrinthectomy and vestibular neurotomy, ELSS is considered a conservative surgical treatment.
The main objective of this study was to demonstrate the non-destructive nature of ELSS on vestibular function, using objective vestibular function tests: videonystagmography (VNG), vestibular evoked myogenic potentials (VEMP) and video head impulse test (VHIT). Secondary outcomes were episodes of vertigo, auditory outcome and quality of life (QoL) using the Menière's disease outcome questionnaire (MDOQ) [5].
Materials and methods
Cases from a tertiary referral center were retrospectively reviewed.
Inclusion criteria were as follows:
-
patients with a definite MD, according to guidelines from the American Academy of Otolaryngology—Head & Neck Surgery (AAO-HNS) of 1995, modified in 2015 [6,7,8
-
debilitating vertigo spells despite medical treatment,
-
treated with ELSS using two techniques: “sac decompression” or “sac opening with mastoid shunt” [9].
Exclusion criteria were as follows:
-
lost to follow-up (follow-up of less than 2 months after surgery),
-
lack of patient consent.
This study was approved by the local ethics committee (GNEDS).
Patients’ characteristics and symptoms were evaluated. We reviewed radiological investigations and previous medical treatments. We also reviewed any prior conservative treatments such as grommet insertion, intratympanic injection of steroids (ITS).
Vestibular function was assessed before and after surgery using vestibular function tests: VNG, VEMP, VHIT.
In VNG, caloric testing was performed, and several measures were evaluated: canal paresis (negative if paresis on the operated side, positive if on the contralateral side), vestibular excitability and directional preponderance.
Cervical and ocular VEMP (cVEMP and oVEMP) were performed. Presence or absence of P13/N23 waves for cVEMP was recorded, as well as their latency, amplitude, and asymmetry ratio (AR) with the following formula:
-
(peak to peak amplitude of P13/N23 of the operated side – non-operated side),
-
(peak to peak amplitude of P13/N23 of the operated side + non-operated side).
The same measurements were calculated for oVEMP with N1/P1.
VHIT gain was measured on the superior, lateral and posterior semi-circular canals.
Our hypothesis was that there would be no deterioration in vestibular function postoperatively. Consequently, a non-inferiority study was performed and non-inferiority margins had to be determined (delta).
The non-inferiority margins were chosen based on clinical judgment using normal standard values and pathological limits [10, 11]. The margins were as follows:
-
VNG canal paresis: − 20%
-
VNG vestibular excitability: − 10°/s
-
VNG directional preponderance: + 2°/s
-
VEMP latency: + 2 ms
-
VEMP amplitude: − 50 μV (saccular)/− 5 μV (utricular)
-
VEMP asymmetry ratio: + 35%
-
VHIT gain: − 0.25
Secondary outcomes were control of episodes of vertigo, auditory outcome (both using AAO-HNS guidelines) and QoL after surgery.
To assess episodes of vertigo we calculated VN = (X/Y)/100 (X = average number of episodes of vertigo per month evaluated 18–24 months after surgery, and Y = average number of defined episodes of vertigo per month during the 6 months before surgery). There were six levels of vertigo control ranging from A; complete resolution of episodes of vertigo, to F; intractable episodes of vertigo requiring further operative treatment.
The worst audiograms obtained before and after surgery were evaluated using pure tone average (PTA) defined as the mean of hearing thresholds at 500, 1000, 2000, 3000 Hz. The patient’s hearing was then classified: stage 1 (PTA < 26 dB), stage 2 (PTA 26–40 dB), stage 3 (PTA 41–70 dB) or stage 4 (PTA > 70 dB). Hearing was considered to have deteriorated if PTA decreased by a minimum of 10 dB.
QoL was assessed postoperatively using the Retrospective-MDOQ questionnaire (Table 1). It uses 19 paired multiple-choice questions assessing pre and postoperative health, each with values ranging from 0 (poorest QoL) to 4 [5, 12].
The procedures were performed by a single experienced surgeon, using either the technique of simple sac decompression or by opening the endolymphatic sac. The technique was chosen by the surgeon based on preoperative audiometry. The main steps of ELSS included canal wall-up mastoidectomy with identification of the sigmoid sinus and 3rd portion of the facial nerve, thinning of the bone covering the dura mater of the posterior fossa between the posterior semi-circular canal and the sigmoid sinus, finishing with deep infralabyrinthine drilling to expose the body of the endolymphatic sac and the endolymphatic duct [13]. Endolymphatic sac opening could be performed with rigid ear endoscope.
In terms of data analysis, a two-tailed Student’s t test was used to compare means of the primary and secondary outcomes. McNemar’s Chi-square test was used to compare paired nominal data. A p value ≤ 0.05 was assigned for significance.
Results
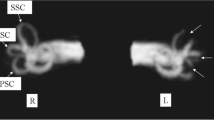
We analysed a total of 73 patients between 2011 and 2018; 39 males (53%) and 34 females (47%), with a mean age of 54 ± 12.6 years. Apart from episodes of vertigo, the main presenting symptoms were hearing loss (79%) and tinnitus (67%). The mean duration of disease before surgery was 6.8 ± 4.76 years. Most patients had a CT scan (52%) and an MRI (82%) performed before the operation.
A 3-T MRI (with IV Gadolinium and late FLAIR sequence at + 4 h) was performed in 19 patients with signs of endolymphatic hydrops seen in 58%.
All patients had failed long-term medical treatment, defined by persistent debilitating vertigo spells. 21% had a history of grommet insertion and 8% received ITS before surgery.
Two types of surgical procedures were performed: sac decompression in 30% and opening of the sac in 70%. The mean operative time was 90.5 ± 29 min, with no statistical difference between the two procedures (p = 0.92). The surgeon used endoscopy in 85% of the cases. There were no postoperative complications (i.e. facial paralysis, cerebrospinal fluid leak or meningitis).
The mean follow-up time was 20.5 months.
Primary outcome
Descriptive results of pre- and postoperative vestibular function tests are shown in Table 2.
25 VNG were compared. Results of the non-inferiority statistical analysis are shown in Fig. 1. Canal paresis was reduced to an average of − 3.65 (CI 90% − 15.95 to 8.65). There was no statistically significant change in canal paresis (CP) as the lower end of the confidence interval was superior to the non-inferiority margin (− 20%). Vestibular excitability (VE) was raised in an average of + 7.57°/s (CI 90%; 0.52–14.61) and directional preponderance (DP) was reduced in an average of − 1.47°/s (CI 90%; − 3.01 to 0.01). There was no statistically significant change in VE or DP as the lower and the upper ends of the confidence interval were superior and inferior to the delta, respectively.
16 cervical and ocular VEMP were analysed. Results of the non-inferiority statistical analysis are shown in Fig. 2a (cVEMP) and 2b (oVEMP).
There was no statistical difference in the presence or absence of P13/N23 waves pre- and postoperatively (p = 0.71).
Mean variations for cervical VEMP were.
-
P13 latency: + 4.10 ms (CI 90% − 0.79 to 8.99),
-
N23 latency: + 4.82 ms (CI 90% − 1.62 to 11.25),
-
P13N23 amplitude: − 40.78 µV (CI 90% − 87.78 to 6.23),
-
Asymmetry ratio: + 0.056 (CI 90% − 0.312 to 0.424).
Deltas were included in the confidence interval for the above values; thus, we could not determine non-inferiority for changes in latencies, amplitude and AR.
For oVEMP, there was no statistical difference in the presence or absence of N1/P1 waves pre- and postoperatively (p = 0.18).
Mean variations for ocular VEMP were.
-
N1 latency: + 1.32 ms (CI 90% − 4.26 to 6.90),
-
P1 latency: + 1.28 ms (CI 90% − 6.47 to 9.03),
-
N1P1 amplitude: − 3.27 µV (CI 90% − 13.05 to 6.51),
-
Asymmetry ratio: + 0.22 (CI 90% − 0.35 to 0.79).
Deltas were included in the confidence interval for the above values; thus, we could not determine non-inferiority for changes in latencies, amplitude and AR.
7 VHIT were compared. Results of the non-inferiority statistical analysis are shown in Fig. 3. Mean variations of VHIT gain were.
-
Superior canal: + 0.12 (CI 90% − 0.18 to 0.42),
-
Posterior canal: + 0.14 (CI 90% − 0.23 to 0.51),
-
Lateral canal: + 0.043 (CI 90% − 0.005 to 0.090).
Non-inferiority was demonstrated for VHIT gain as all lower ends of the confidence intervals were higher than the delta.
Secondary outcomes
ELSS was associated with a reduction in the number of episodes of vertigo in 67% of the patients (51% and 16% in class A and class B, respectively). 13 patients required further surgical treatment due to persistent episodes of vertigo (class F 18%).
Improvement in vertigo was significantly better when sac opening was performed (75% of class A and B combined) compared with 50% in the simple decompression group (odds ratio 3.16; p = 0.04).
A non-statistically significant decrease in postoperative mean PTA was noted, on average − 4 dB ± 18 (− 0.2 to 8.4) (p = 0.06).
Preoperative PTA was higher in the sac decompression group 30 dB ± 19 (5–61), versus 56 dB ± 14 (19–78) in the sac opening group. Postoperative decrease in PTA was higher in the sac opening group (− 6 dB ± 23.4) versus (− 2.29 dB ± 6.09) in the decompression group but this difference was not statistically significant (p = 0.62).
We collected 38 MDOQ QoL questionnaires (52% response rate), with an average time between surgery and evaluation of 56 months ± 28. Mean response to MDOQ was 22 ± 9.9 (7–56) preoperatively. Mean postoperative response was 43 ± 16 (11–69).
There was a statistically significant improvement in QoL after surgery (p < 0.0001), with a mean improvement of + 21 ± 15 (−6 to 57).
Discussion
ELSS was first described by Portmann in 1927 [13] and has since been widely used for intractable Menière’s disease. Despite experimental and animal studies, the role of the endolymphatic sac in hydrops remains unclear. Numerous hypotheses have been proposed including accumulation of osmotically active proteins in the sac, insufficient reabsorption of endolymphatic fluid [14, 15].
Population
The population of our study was largely representative of the MD population found in the literature [16], with a similar proportion of male and female, and most patients in their 5th or 6th decades. Not many patients previously underwent ITS, as this procedure was not performed routinely in the center at the time of this study. It is now recommended by the ICON consensus as the second line in case of failure of medical treatment [1]. This was not felt to compromise the result as several studies show that ITS only offers short-term benefit [17, 18].
Controversy on ELSS
ELSS has been criticized since the publication of two Danish studies in 1981 and 1998 which contested the effectiveness of the procedure. Thomsen et al. conducted a prospective study comparing a group of patients who underwent ELSS with another group who underwent simple mastoidectomy [2]. Functional results were compared, and the authors did not find any statistical differences between the two groups and consequently referred to ELSS as “placebo surgery”. This study has been heavily criticised from an ethical perspective by several other authors, not only for controversially performing an alleged “placebo surgery” on patients for the purpose of the study, but also from a methodological point of view. In that regard, Welling et al. reanalyzed Thomsen’s results and found a statistically significant improvement in episodes of vertigo and tinnitus in the group ELSS vs the mastoidectomy group [19].
Thomsen et al. published another comparative study in 1998, this time comparing ELSS with grommet insertion [3]. There was an improvement in episodes of vertigo in both groups with no statistical difference. Several biases in this study were outlined in a Cochrane analysis [4]; there was no description of the randomization protocol, there were no precise numerical results, follow-up was less than a year, double-blinding was not possible.
A more recent meta-analysis by Lim et al. in 2015 found 8 studies with level 3 evidence showing short- and long-term efficacy in terms of vertigo control for more than 80% who underwent ELSS. None of these studies included an analysis of vestibular function.
Primary outcome
Previous studies had demonstrated the beneficial effect of surgery on endolymphatic hydrops measured by electrocochleography, but did not include other vestibular function tests [20, 21].
Our study demonstrates the conservation of vestibular function as measured by the caloric test of VNG. Therefore, we demonstrate that functional improvement associated with ELSS is not related to the destruction of the vestibular apparatus, in contrast to other non-conservative interventions such as chemical labyrinthectomy (CL) or vestibular neurotomy (VN). Vestibular excitability on the operated side seemed to increase postoperatively which can be a sign of a better vestibular function.
This result supports the use of ELSS especially in patients with bilateral disease, as the preservation of vestibular function could be useful to avoid postural instability after surgery. ELSS could also be considered in the elderly, who may be more prone to vestibular instability related to presbyvestibulia, where a destructive procedure could have negative consequences in terms of postural stability [22]. In comparison, the residual instability rate is reported to be as high as 30% following VN [23].
Regarding VEMP, there was no significant change in the presence or absence of P13/N23 or N1/P1 waves. Conversely, we did not succeed in demonstrating non-inferiority for other VEMP criteria. This result could be explained by a lack of power due to the relatively small sample size for VEMP. Also, we intentionally chose small non-inferiority margins to obtain a clinically significant result for the primary outcome. A great variability in normal VEMP norms is found in the literature which can also explain that our predetermined delta was included in the confidence interval.
VEMP abnormalities in MD are quite inconsistent as VEMP variations are found in 30–69% of patients in the majority of studies [16].
There was in our study no significant deterioration of VHIT gain. This result was predictable. Gain changes are rarely seen in MD [24, 25]. In a study by Jerin et al., VHIT gains were always normal in MD and not correlated with canal paresis on caloric response or with VEMP asymmetry ratio [24]. We demonstrated that ELSS did not alter the high-frequency vestibulo-ocular reflex.
Secondary outcomes
Reduction in episodes of vertigo in our study was approximately 70%, which is close to the rate reported in similar studies [26, 27]. We found that the sac opening technique was associated with a higher rate of improvement in control of vertigo. This result is not found in other studies that demonstrated no particular advantage in using one technique over another. The rate of improvement in episodes of vertigo is usually greater than 90% for VN and between 85 and 90% for CL [28, 29]. These success rates are slightly better than the one in ours (75% for the sac opening technique). However, the adverse effects and potential complications of such destructive procedures should be taken into consideration. For example, VN is associated with a significant rate of postoperative complications. In their study of 58 patients treated with VN, Schmerber et al. described complications including infection or delayed healing (12%), CSF leak (7%), and also a risk of meningitis and other neurological complications [30]. There were no such adverse effects or postoperative complications reported in our ELSS patient cohort.
Regarding hearing outcomes, rates of preservation of hearing function (improved or deteriorated by no more than 10 dB) are usually around 70% [31]. A similar rate was found in our study, with a non-statistically significant decrease in PTA of − 4 dB. Hearing decreased slightly more in the sac opening group, but that difference was not statistically significant. This finding is consistent with most studies [31]. This trend probably influenced the surgeon as he generally chose a simple decompression in the group of patients with a normal preoperative PTA. In comparison, the hearing preservation rate is usually approximately 85% with VN [32]. With CL, hearing deteriorates in as many as 25 to 45% of patients, with great variability depending on the treatment protocol used [33]. In summary, ELSS is associated with a high rate of hearing preservation.
The QoL questionnaire we used was presented by Kato et al. to assess the impact of ELSS on the physical, emotional and social aspects of health [5]. Convert et al. used the same questionnaire to evaluate ELSS, demonstrating an 81.4% increase in the QoL score with a mean follow-up time of 57 months [12]. We found very similar results with an 87% improvement in QoL scores after surgery, with a mean follow-up of 56 months. Compared with other interventions, a meta-analysis by Ballard et al. reported a mean improvement of + 25 to + 42 points in the MDOQ score for ELSS [34]. With CL, the improvement was on average between + 7 and + 33. There were no studies using the MDOQ score to evaluate VN. The more heterogenous results in QoL in CL could be related to residual postural instability which is often described as a complication of this destructive method. This highlights the advantage of using conservative techniques such as ELSS whenever possible [23].
Future scope for research
The pathophysiology of ELSS and its relationship to symptom improvement still have to be clarified. Although they had a small number of patients, Liu et al. demonstrated that endolymphatic fluid volume measured on 3 T MRI had decreased after ELSS.
A better understanding of the role of the endolymphatic sac is needed. Some authors recently described a new technique of endolymphatic duct blockage, showing promising results [35]. The hypothesis is that the sac plays a role in both endolymphatic fluid absorption and secretion and that hydrops actually occurs due to excess secretion within the sac. As such, blocking the duct would help limit the accumulation of fluid. These results do not contradict the techniques described in our study as many hypotheses have been formulated to explain the effect of surgery on the endolymphatic sac: altering osmotic pressures, altering blood supply, and modifying immune factors [36].
Although ethical issues would need to be addressed, further studies are needed including a controlled comparative group.
Conclusion
We have demonstrated preservation of vestibular function with ELSS, as measured with the main vestibular function tests (VNG, VHIT), which had not been demonstrated in previous studies. There was no modification of the presence of P13/N23 or N1/P1 waves postoperatively in cervical and ocular VEMP. This result highlights the main advantage of this conservative technique over destructive procedures, as preserved vestibular function will cause less postural instability and will not impede vestibular rehabilitation.
We have also shown the beneficial effects of the surgery in reducing episodes of vertigo with 70% reporting improved control, and with no significant reduction in hearing. The sac opening technique was associated with a better improvement in vertigo. The vast majority of patients had a significantly improved QoL after surgery.
The pathophysiology of MD and the role of the endolymphatic sac has yet to be clearly established. New imaging techniques including 3-T-FLAIR MRI will be useful in the future to diagnose and quantify endolymphatic hydrops. Despite more widely used techniques like ITS, ELSS remains an effective and low-risk surgical option in the treatment of MD.
References
Nevoux J, Barbara M, Dornhoffer J, Gibson W, Kitahara T, Darrouzet V (2018) International consensus (ICON) on treatment of Ménière’s disease. Eur Ann Otorhinolaryngol Head Neck Dis 135(1S):S29-32
Thomsen J, Bretlau P, Tos M, Johnsen NJ (1981) Placebo effect in surgery for Ménière’s disease. A double-blind, placebo-controlled study on endolymphatic sac shunt surgery. Arch Otolaryngol Chic Ill 1960. 107(5):271–277
Hellström S, Thomsen J et al (1998) The non-specific effect of endolymphatic sac surgery in treatment of Meniere’s disease: a prospective, randomized controlled study comparing “classic” endolymphatic sac surgery with the insertion of a ventilating tube in tympanic membrane. Acta Oto-Laryngol 118:769–773 (Acta Otolaryngol (Stockh). 2018 Mar 4;138(3):304–9)
Pullens B, Verschuur HP, van Benthem PP (2013) Surgery for Ménière’s disease. Cochrane Database Syst Rev 2:CD005395
Kato BM, LaRouere MJ, Bojrab DI, Michaelides EM (2004) Evaluating quality of life after endolymphatic sac surgery: the Ménière’s Disease Outcomes Questionnaire. Otol Neurotol 25(3):339
(1995) Committee on Hearing and Equilibrium guidelines for the diagnosis and evaluation of therapy in Menière’s disease. American Academy of Otolaryngology-Head and Neck Foundation, Inc. Otolaryngol Head Neck Surg 113(3):181–5
Lopez-Escamez JA, Carey J, Chung W-H, Goebel JA, Magnusson M, Mandalà M et al (2015) Diagnostic criteria for Menière’s disease. J Vestib Res Equilib Orientat 25(1):1–7
Claes J (2000) A review of medical treatment for Ménière’s disease. Acta Otolaryngol (Stockh) 120(544):34–39
Flores García ML, de la Llata SC, Cisneros Lesser JC, Pane PC (2017) Endolymphatic sac surgery for Ménière’s disease—current opinion and literature review. Int Arch Otorhinolaryngol. 21(2):179–183
Young Y-H, Huang T-W, Cheng P-W (2003) Assessing the stage of Meniere’s disease using vestibular evoked myogenic potentials. Arch Otolaryngol Head Neck Surg 129(8):815–818
Rubin F, Simon F, Verillaud B, Herman P, Kania R, Hautefort C (2018) Comparison of video head impulse test and caloric reflex test in advanced unilateral definite Menière’s disease. Eur Ann Otorhinolaryngol Head Neck Dis 135(3):167–169
Convert C, Franco-Vidal V, Bebear J-P, Darrouzet V (2006) Outcome-based assessment of endolymphatic sac decompression for Ménière’s disease using the Ménière’s disease outcome questionnaire: a review of 90 patients. Otol Neurotol 27(5):687–696
Portmann G (1927) Vertigo: surgical treatment by opening the saccus endolymphaticus. Arch Otolaryngol 6(4):309–319
Couloigner V, Sterkers O, Rask-Andersen H, Teixeira M, Ferrary E (2004) Le sac endolymphatique : ses fonctions au sein de l’oreille interne. Med Sci Paris 20(3):304–310
Paparella MM, Djalilian HR (2002) Etiology, pathophysiology of symptoms, and pathogenesis of Meniere’s disease. Otolaryngol Clin N Am. 35(3):529–45, vi
Kim M-B, Choi J, Park GY, Cho Y-S, Hong SH, Chung W-H (2013) Clinical value of vestibular evoked myogenic potential in assessing the stage and predicting the hearing results in Ménière’s disease. Clin Exp Otorhinolaryngol 6(2):57
Barrs DM (2004) Intratympanic injections of dexamethasone for long-term control of vertigo. Laryngoscope 114(11):1910–1914
Martin-Sanz E, Esteban-Sanchez J, Rodrigañez-Riesco L, Sanz-Fernández R (2015) Transitory effect on endolymphatic hydrops of the intratympanic steroids for Ménière’s disease. Laryngoscope 125(5):1183–1188
Welling DB, Nagaraja HN (2000) Endolymphatic mastoid shunt: a reevaluation of efficacy. Otolaryngol-Head Neck Surg 122(3):340–345
Radeloff A, Hamad M, Helms J, Hagen R, Shehata-Dieler W (2009) Short and long term results of endolymphatic sac surgery: a patient-questionnaire based study. Laryngorhinootologie 88(10):653–659
Schwager K, Baier G, El-Din M, Shehata-Dieler W, Carducci F, Helms J (2002) Revision surgery after saccotomy for Meniere’s disease: does it make sense? Eur Arch Oto-Rhino-Laryngol 259(5):239–242
Ionescu E, Dubreuil C, Ferber-Viart CC (2005) Physiological changes in balance control of adults aged 20 to 60 years assessed with Equitest. Ann Oto-Laryngol Chir Cervico Faciale Bull Soc Oto-Laryngol Hopitaux Paris 122(5):231–235
Lacombe H (2009) Surgery for vertigo. Neurochirurgie 55(2):268–271
Jerin C, Maxwell R, Gürkov R (2019) High-frequency horizontal semicircular canal function in certain Menière’s disease. Ear Hear 40(1):128–134
Fukushima M, Oya R, Nozaki K, Eguchi H, Akahani S, Inohara H et al (2019) Vertical head impulse and caloric are complementary but react opposite to Meniere’s disease hydrops. Laryngoscope 129(7):1660–1666
Lim MY, Zhang M, Yuen HW, Leong J-L (2015) Current evidence for endolymphatic sac surgery in the treatment of Meniere’s disease: a systematic review. Singapore Med J 56(11):593–598
Brinson GM, Chen DA, Arriaga MA (2007) Endolymphatic mastoid shunt versus endolymphatic sac decompression for Ménière’s disease. Otolaryngol-Head Neck Surg 136(3):415–421
Morel N, Dumas G, Nguyen D-Q, Mohr E, Hitter A, Schmerber S (2005) Vestibular neurotomy versus chemical labyrinthectomy for disabling Menière disease. Ann Oto-Laryngol Chir Cervico Faciale Bull Soc Oto-Laryngol Hopitaux Paris 122(6):271–280
Pullens B, van Benthem PP (2011) Intratympanic gentamicin for Ménière’s disease or syndrome. Cochrane Database Syst Rev. 3:CD008234
Schmerber S, Dumas G, Morel N, Chahine K, Karkas A (2009) Vestibular neurectomy vs. chemical labyrinthectomy in the treatment of disabling Menière’s disease: a long-term comparative study. Auris Nasus Larynx 36(4):400–405
Sood AJ, Lambert PR, Nguyen SA, Meyer TA (2014) Endolymphatic sac surgery for Ménière’s disease: a systematic review and meta-analysis. Otol Neurotol 35(6):1033–1045
Nevoux J, Franco V, Bouccara D, Parietti-Winkler C, Uziel A, Chays A et al (2017) Recommandations de la SFORL (version courte) sur la stratégie diagnostique et thérapeutique dans la maladie de Menière. Ann Fr Oto-Rhino-Laryngol Pathol Cervico-Faciale 1(134):422–426
Yetişer S (2018) Intratympanic gentamicin for intractable Ménière’s disease—a review and analysis of audiovestibular impact. Int Arch Otorhinolaryngol 22(2):190–194
Ballard DP, Sukato DC, Timashpolsky A, Babu SC, Rosenfeld RM, Hanson M (2019) Quality-of-life outcomes following surgical treatment of Ménière’s disease: a systematic review and meta-analysis. Otolaryngol-Head Neck Surg 160(2):232–238
Gabra N, Asmar MH, Berbiche D, Saliba I (2016) Endolymphatic duct blockage: quality of life assessment of a novel surgical technique for Ménière disease. Eur Arch Otorhinolaryngol 273(10):2965–2973
Zhang Y, Fu J, Lin H, Shen C, Wang X, Wu J (2019) The clinical outcomes after intratympanic gentamicin injection to treat Menière’s disease: a meta-analysis. Otol Neurotol 40(4):419–429
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that they have no competing interest.
Ethics approval
This study was approved by the local ethics committee (GNEDS—Groupe Nantais d’Ethique dans le Domaine de la Santé).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gendre, A., Bourget-Aguilar, K., Calais, C. et al. Evaluation of vestibular function following endolymphatic sac surgery. Eur Arch Otorhinolaryngol 279, 1193–1201 (2022). https://doi.org/10.1007/s00405-021-06743-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-06743-3