Abstract
Bulk fill resin composite materials are now popular with clinicians as they offer faster restorative treatments options for vital and non-vital posterior teeth. It is important for the clinician to understand the material’s critical physical and mechanical properties and apply this information to deliver safe and top-quality clinical dentistry for their patients. Additionally, a good knowledge of the various types of bulk fill materials available (full body, flowable, and fiber reinforced) and how they might be applied in various clinical situations. The aim of this chapter is to outline the most important mechanical and biological characteristics as well as the advantages and limits of those materials.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Bulk fill
- Mechanical properties
- Flexural strength
- Microhardness
- Wear
- Diametral tensile strength
- Cytotoxicity
6.1 Introduction
Resin-based composites (RBCs) have advanced significantly in the past few years. Filler type, resin matrix, and initiator systems have frequently been updated to improve the mechanical properties and to decrease polymerization shrinkage stress. The purpose of these improvements is intended to enhance the clinical longevity of RBC restorations, to reduce the complexity of the restorative procedure, and to decrease chairside time. The recent introduction of bulk fill RBCs represents a revolution in restorative dentistry and provides the clinician considerably shorter chairside time. Since their introduction these materials are now used by clinicians as an alternative to conventional resin composite for posterior restorations and for core build-ups [1].
Full body bulk fill resins require a shorter restorative time in posterior teeth than conventional resins. Flowable bulk fill resin composites provide faster treatment options with time when considering capping [2]. Clinically, a reduction in operative time has been considered a positive reason for selecting bulk fill products [3]. For light-cured bulk fill RBCs, insufficient polymerization at increasing depths has been reported in some studies. This limitation might compromise the clinical success of the restorations with the possibility of increased cytotoxicity [4], susceptibility to marginal defects [5, 6], and reduced hardness [7,8,9].
There is scientific evidence that the degree of conversion of a resin-based material may influence various mechanical properties, such as BFS (biaxial flexural strength) and KHN (Knoop hardness) [10,11,12,13].
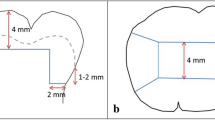
Data on curing efficiency has also been inconclusive, with some studies reporting depths of cure of more than 4 mm and others describing insufficient curing at 4-mm layers [14,15,16,17,18].
Differences in mechanical properties and depth of cure may be attributed to differences in resin compositions, material translucency, viscosity, filler type, and content [19].
The mechanical properties of bulk fill RBCs have been, in fact, the subject of some debate. While some authors have reported lower mechanical properties than conventional highly filled RBCs, others have reported values close to conventional materials [20,21,22].
The type of organic matrix, filler size and morphology, monomer type and ratio, and photoinitiation chemistries vary greatly between products [23]. This makes a comparison of the mechanical properties very difficult [23].
6.2 Flexural Strength
Flexural testing is widely used in characterizing RBCs since it determines both flexural (elastic) modulus and strength and is an important property for restorative materials used in high-stress-bearing areas [24, 25]. Flexural modulus describes the stiffness of RBCs, whereas flexural strength represents the maximum stress that RBCs can be subjected to prior to failure. Elastic modulus is an indicator of stiffness and an important factor affecting shrinkage stress of resin-based composites [26]. Significant relationships between the modulus and stress have been reported by several researchers [27,28,29,30].
A lower Young’s modulus may allow stress dissipation during the polymerization process, thus reducing the stress when bigger increments are used [10, 31,32,33,34].
Certain low-viscosity bulk fill RBCs (flowable) have a modulus of elasticity (and hardness) considerably below the mean values measured for regular nano-hybrid and micro-hybrid RBCs. For this reason, manufacturers recommend covering flowable bulk fill RBC restoration with a capping layer made of regular RBCs [21].
The variation between the flexural properties of various RBCs is useful for different clinical situations [35, 36]. For example, in class I, II, III, and IV cavities, RBCs with high flexural properties are usually selected to minimize fracture or deformation under the high occlusal forces, while in class V cavities, RBCs having low flexural modulus are preferred, as they can flex with the teeth during function and parafunction, which in turn reduces the stresses at the adhesive interface and decreases the chances of debonding [35, 37]. In fact, with their greater flexibility, bulk fill flowable RBCs are preferred over full body bulk fill restorative or conventional materials in deep class V cavities, as they appear to offer better marginal adaptation [38].
The flexural modulus of the bulk fill flowable RBCs is lower than for full body bulk fill restorative or conventional resin composites [33, 39]. A material with a low modulus of elasticity, particularly when placed in load-bearing areas, will result in higher deformability under masticatory stresses and a reduction of wear resistance. Over time this will cause catastrophic failure of the restoration [21, 40]. Testing of the flexural properties of the different categories of bulk fill materials and those from the different manufacturers are both material and specimen conditioning dependent as confirmed by several authors [39, 41].
The decrease in BFS (biaxial flexural strength) of bulk fill materials with depth was seen to be highly product-dependent [42].
The flexural strength of full body/high-viscosity bulk fill is higher than the limit of 80 MPa established in ISO 4049/2009 for polymer-based restorative materials indicated for restorations involving occlusal surfaces [43, 44]. Bulk fill restorative RBCs (full body) are generally stiffer than bulk fill flowable and conventional counterparts. This may be attributed to the similar or higher filler content of the bulk fill restoratives in comparison to the other RBCs [45,46,47]. Some authors have reported no correlation between the elastic modulus and filler content for high-viscosity composites, but a strong correlation is generally noted for low-viscosity resins. The low correlation between high-viscosity composites may occur because they present a relatively lower elastic modulus when compared to their filler content [48, 49]. Some flowable and packable resin composites have demonstrated an increase in the elastic modulus 12 h after irradiation due to post-irradiation polymerization [27, 50]. Furthermore, there is an increase in the polymerization stress and the elastic modulus for many bulk fill resin composites after irradiation as they develop a major part of their stiffness within 1 h [51]. The correlation between the degree of conversion and elastic modulus for bulk fill composites is controversial. Some authors have reported that there is no correlation between the degree of conversion and elastic modulus [16].
6.3 Microhardness and Wear of Bulk Fill RBCs
Assessment of a material’s hardness is often used by RBCs researchers. Microhardness allows an understanding of the mechanical properties of the composite surfaces [52]. Furthermore, there is a strong relationship between microhardness and elastic modulus values, depth of cure, and polymerization shrinkage [53]. Microhardness is used, in fact, as an indirect measurement of the extent of polymerization of a specific composite material [54, 55], due to its proven correlation with the degree of conversion [56, 57].
According to Watts and others, an acceptable curing depth is achieved if the bottom hardness corresponds to at least 80% of the top surface hardness [58]. The decrease in microhardness of bulk fill materials with depth was also seen to be highly product-dependent, with some materials demonstrating similar hardness values at 1 and 4 mm depth levels [42]. Alrahlah et al. [17], using Vickers hardness profiles, determined that the depth of cure of various bulk fill composite materials ranged from 4.14 to 5.03 mm, which confirms the claims of the manufacturers for the tested materials. An increase in microhardness values is generally expected as the filler content increases. This assumption has been confirmed by several authors [14, 20, 59,60,61,62,63,64].
Flowable Bulk fill resins have lower microhardness because of the low percentage values for load particles. It is therefore always necessary to apply a conventional resin over them [65, 66].
Papadogiannis et al. reported that the use of a capping layer is mandatory to achieve higher creep resistance [67]. High-viscosity (full body) bulk fill RBCs generally have higher filler content and can be used to cover the softer flowable RBCs or they can be used to fill the entire restorations as they have better wear resistance and improved mechanical properties [44, 68]. Besides the filler size and shape, the hardness of the fillers, the strength of the bond between the inorganic content and polymer matrix, and the light-curing of the RBC can also affect wear resistance [69].
Melo et al. compared conventional resin composites using incremental fill technique and bulk fill RBCs. The conventional composites presented good physical properties, but the bulk fill composites showed better results for surface hardness and solubility at the bottom surface [70].
High variability in the results could be detected for the microhardness test, even among high-viscosity bulk fill resin composites. This may be explained by the lower elastic modulus observed for some of the bulk fill RBCs, generally associated with a differences in filler contents and matrix [21, 61, 62, 71].
Camassari et al. evaluated the physical–mechanical properties of several bulk fill materials submitted to biodegradation by oral biofilm (S. Mutans). Increased roughness and reduced hardness and gloss of all the evaluated composites were reported. The biodegradation induced by S. mutans negatively affected mechanical and surface properties. It is therefore mandatory to select the proper restorative material and to advice the patient about the importance of good oral hygiene techniques to maintain the esthetics and longevity of RBC restorations [72].
6.4 Diametral Tensile Strength (DTS)
The diametral compression test may also be used to measure strength [73]. However, the results of such test should be consciously judged, as sometimes shear and tensile stresses may occur at the same time, determining a different fracture pattern,. Moreover, this test is not defined by standards for dental materials. Al Sunbul et al. reported different DTS values for several bulk fill materials (SDR, Venus bulk Fill, Tetric Evoceram Bulk fill, Ever X Posterior) [74]. They reported that the differences at baseline were also confirmed after aging in water and in food simulating solvents: ethanol and methyl ethyl ketone. The authors did not report a correlation between filler loading and mechanical properties. They did not report a correlation between DTS and hardness. Conversely Medeiros et al. reported a strong correlation among these two properties [75].
6.5 Water Sorption
Water sorption is crucial in determining clinical success. Although resin composite is considered in general as a stable material that can accomplish several years of clinical service, the presence of polymer networks determines a certain degree of moisture sorption. Water sorption has a negative effect on the restorative material by contributing to lower/weaken mechanical properties, reduce wear resistance, and affect discoloration.
The effect of water sorption on the resin composite behavior is influenced by several factors, such as the composition of the polymer matrix, the type and content of the filler, and the size and shape of filler particles [76].
Janda et al. [77] investigated water sorption and solubility differences between various types of dental resin composites and reported that the correlation between water sorption and filler load was significant. The lowest water sorption values were found in the composite with the highest filler load. Sorption into a polymer can be explained by two theories: the free volume theory, and the interaction theory [78]. The free volume theory involves solvent absorption through voids in the polymer, while in the interaction theory, water binds to specific ionic groups of the polymer chain depending on their water affinity [79]. Water sorption may decrease the longevity of a RBC resin by expanding and plasticizing its components, causing the hydrolysis of the silane coupling agents. The expansion is undesirable because of the potential stress inducing microcracks or even macrocracks in restored teeth [80]. Bis-GMA-based resin matrix presents higher water sorption because of its hydrophilicity in respect to other methacrylate monomers, such as UDMA [81]. When Bis-GMA resins are combined with TEGDMA to manage viscosity, water uptake can even increase more [82]. Kalachandra et al. supported this finding reporting that partial substitution of TEGDMA with UDMA comonomer in Bis-GMA/TEGDMA RBCs resulted in decreased water absorption [83].
Alshali et al. reported higher sorption values for a conventional flowable (X-Flow, Dentsply Sirona, Kostanz, Germany) compared to a flowable bulk fill (X-tra base, Voco GmbH, Cuxhaven, Germany), the latter showing the lowest values when compared to other bulk fill or conventional nano-hybrid composites [59].
Apart from matrix, fillers play a role in staining susceptibility of RBCs. They are added to increase mechanical properties, to reduce the volume of resin matrix, thus reducing shrinkage and water sorption [84]. Glass fillers do not contribute to the water sorption process but water may get adsorbed onto their surface. The hydrolytic degradation of resin–filler interface bonds can in fact induce the release of unreacted monomers [85], compromising the material biocompatibility [78].
Water sorption depends therefore on material’s filler load, with flowable, and low-viscosity bulk fill showing a higher degree, rather than on the polymerization extent characteristic of bulk fill materials. In other words, it is not the fact of being a bulk fill that determines the level of water sorption, rather the viscosity.
6.6 Differences in Mechanical Properties Between Flowable, Full Body, and Fiber-Reinforced Bulk Fill Composites
Differences in mechanical properties have been reported between flowable, full body, and fiber-reinforced bulk fill materials. Because of their poor mechanical properties the use of low-viscosity bulk fill composite is not recommended in situations where high mechanical stress is present, such as in direct contact with occlusal loads [86, 87]. Previous findings showed that Young modulus, Vickers hardness, and Indentation modulus classify some bulk fill materials (SureFil SDR, Venus Bulk Fill, and Filtek Bulk Fill) as between hybrid and flowable composites [18]. The poor mechanical properties of flowable bulk fill composites highlights the need of coverage with a conventional RBC. This capping procedure should be performed to overcome poor surface properties, low esthetics and material degradation [20]. Attik et al. reported that fiber-reinforced bulk fill show lower flexural modulus and hardness than full body bulk fills [88]. The authors reported similar flexural strength between these two types of bulk fill materials. This leads to the conclusion that fiber-reinforced bulk fill materials may endure higher strain before being damaged.
Fiber-reinforced materials have significantly higher fracture toughness results, showing the higher toughness established by the fiber reinforcement. These materials may prevent fracture propagation inside the material and are indicated for the restoration of endodontically treated teeth [89]. Fiber-reinforced materials undergo higher stress during polymerization [90].
The mechanical properties of flowable bulk fill composites are generally lower compared with the full body high-viscosity materials, and, at best are comparable to the conventional flowable composite [20, 91] as given in Table 6.1.
6.7 Cytotoxicity
While their physico-mechanical properties, handling characteristics and wear performance have been extensively tested [14, 17, 20, 92,93,94], scientific data on the biocompatibility of bulk fill composite materials is very limited [95]. Biocompatibility is the ability of materials to coexist with living tissues without causing harm. Non-biocompatible or cytotoxic (i.e., toxic to cells) restorative materials can cause short-term and long-term adverse tissue reactions ranging from postoperative sensitivity to irreversible pulp damage [96]. It has been reported that RBCs alone may contribute to more than 12% of adverse reactions of dental materials [97]. In addition to the leaching of unreacted monomers, cytotoxicity can also be caused by the release of initiators and other additives from the organic resin as well as metal ions from the inorganic fillers. Proper curing of RBCs is important to ensure adequate mechanical properties and biocompatibility [98, 99]. This materials’ cytotoxicity has been related to the released residual monomer quantity and type; some studies reported a correlation between this aspect and loss of mass and/or lower conversion degree [100]. Bulk fill RBCs placed with a 4 mm single increment present lower shrinkage stress and higher DOC at this depth; this can be related to the increased translucency and to polymerization modulators [3, 101]. However, a common concern about bulk fill materials is whether the degree of conversion at 4 mm depth is sufficient, which would increase the cytotoxic potential, especially in the case of bulk fill flowable resins with a higher organic matter content [102, 103].
Some authors have concluded that the placement of bulk fill composite materials in contrast to conventional resin composite, in a 4-mm layer thickness could be recommended in terms of both mechanical stability and biocompatibility [104].
Alshali et al. [59] reported that despite the increased increment thickness of bulk fill composites, monomer elution from these materials can be comparable to that of conventional composites, with the rate of elution being dependent on monomer molecular weight and the cross-link density of the polymer [105,106,107]. While highly cross-linked polymers are more resistant to solvent uptake and swelling, linear polymers provide more space and pathways for diffusion of solvent molecules within the structure [82, 108].
The fact that RBCs are biologically accepted, allergic effects on oral soft tissues have been reported [109]. These are generally due to the dissolution of methacrylate and leaching of its components [110], resulting from masticatory forces and chemical degradation [104]. Conversely, Gonçalves et al. reported no toxic response to gingival fibroblasts for bulk fill RBCs placed at the thickness of 4 mm [31].
Others have investigated potential genotoxic effects emanating from resin-based bulk fill materials. They concluded that none of the tested bulk fill resin composites caused primary DNA damage. The finding that eluates obtained from both the top and bottom composite surface of the tested bulk fill materials did not induce genotoxic effects might be explained by an adequate extent of polymerization of the bulk fill resin composites, even when applied in 4-mm thickness.
An irradiation time of 20 s (at an irradiance of ≈1200 mW/cm2) might suffice for the bulk fill resin composites to not induce relevant genotoxic effects [104].
6.8 Clinical Significance
According to the properties described above, some clinical considerations can be drawn:
-
Flowable bulk fill materials must be capped with a conventional RBC.
-
In patients with parafunctional habits, restorative materials with higher mechanical properties should be selected.
-
Fiber-reinforced BF could be selected to restore ETT as they reduce fracture propagation.
-
Adequate curing of bulk fill materials is mandatory to ensure a correct conversion, increase mechanical properties and to reduce cytotoxicity.
6.9 Conclusions
Bulk fill materials can be inserted and polymerized in large increments, in posterior teeth. Although this is a clinical advantage, clinicians should always be aware of the limitations of the mechanical properties of these materials.
A number of bulk fill materials show lower mechanical properties when compared to highly filled nano-hybrid composites. The use of flowable bulk fill materials for restorations under high occlusal load is subject to caution. It is a critical requirement that flowable materials be veneered or capped with a conventional or full body bulk fill material not only to improve esthetics but to reduce the impact of degradation.
Suitably designed clinical studies are required to avoid the biases observed in in vitro studies to better understand clinical performances of these materials.
References
Warangkulkasemkit S, Pumpaluk P. Comparison of physical properties of three commercial composite core build-up materials. Dent Mater J. 2019;38(2):177–81.
Bellinaso MD, Soares FZM, de Olivera RR. Do bulk-fill resins decrease the restorative time in posterior teeth? A systematic review and meta-analysis of in vitro studies. J Investig Clin Dent. 2019;10(4):e12463.
Benetti AR, Havndrup-Pedersen C, Honoré D, Pedersen MK, Pallesen U. Bulk-fill resin composites: polymerization contraction, depth of cure, and gap formation. Oper Dent. 2015;40(2):190–200.
Price RB, Shortall AC, Palin WM. Contemporary issues in light curing. Oper Dent. 2014;39(1):4–14.
Frassetto A, Breschi L, Turco G, Marchesi G, Di Lenarda R, Tay FR, et al. Mechanisms of degradation of the hybrid layer in adhesive dentistry and therapeutic agents to improve bond durability—a literature review. Dent Mater. 2016;32(2):e41–53.
Ferracane JL, Mitchem JC, Condon JR, Todd R. Wear and marginal breakdown of composites with various degrees of cure. J Dent Res. 1997;76(8):1508–16.
Soto-Montero J, Nima G, Rueggeberg FA, Dias C, Giannini M. Influence of multiple peak light-emitting-diode curing unit beam homogenization tips on microhardness of resin composites. Oper Dent. 2020;45(3):327–38.
Price RBT, Labrie D, Rueggeberg FA, Sullivan B, Kostylev I, Fahey J. Correlation between the beam profile from a curing light and the microhardness of four resins. Dent Mater. 2014;30(12):1345–57.
Uhl A, Mills RW, Jandt KD. Photoinitiator dependent composite depth of cure and Knoop hardness with halogen and LED light curing units. Biomaterials. 2003;24(10):1787–95.
Fronza BM, Rueggeberg FA, Braga RR, Mogilevych B, Soares LES, Martin AA, et al. Monomer conversion, microhardness, internal marginal adaptation, and shrinkage stress of bulk-fill resin composites. Dent Mater. 2015;31(12):1542–51.
Fronza BM, Ayres A, Pacheco RR, Rueggeberg FA, Dias C, Giannini M. Characterization of inorganic filler content, mechanical properties, and light transmission of bulk-fill resin composites. Oper Dent. 2017;42(4):445–55.
Rueggeberg FA, Cole MA, Looney SW, Vickers A, Swift EJ. Comparison of manufacturer-recommended exposure durations with those determined using biaxial flexure strength and scraped composite thickness among a variety of light-curing units. J Esthet Restor Dent. 2009;21(1):43–61.
Bouschlicher MR, Rueggeberg FA, Wilson BM. Correlation of bottom-to-top surface microhardness and conversion ratios for a variety of resin composite compositions. Oper Dent. 2004;29(6):698–704.
Bucuta S, Ilie N. Light transmittance and micro-mechanical properties of bulk fill vs. conventional resin based composites. Clin Oral Investig. 2014;18(8):1991–2000.
Garcia D, Yaman P, Dennison J, Neiva G. Polymerization shrinkage and depth of cure of bulk fill flowable composite resins. Oper Dent. 2014 Aug;39(4):441–8.
Czasch P, Ilie N. In vitro comparison of mechanical properties and degree of cure of bulk fill composites. Clin Oral Investig. 2013;17(1):227–35.
Alrahlah A, Silikas N, Watts DC. Post-cure depth of cure of bulk fill dental resin-composites. Dent Mater. 2014;30(2):149–54.
Ilie N, Keßler A, Durner J. Influence of various irradiation processes on the mechanical properties and polymerisation kinetics of bulk-fill resin based composites. J Dent. 2013;41(8):695–702.
Jang J-H, Park S-H, Hwang I-N. Polymerization shrinkage and depth of cure of bulk-fill resin composites and highly filled flowable resin. Oper Dent. 2015;40(2):172–80.
Leprince JG, Palin WM, Vanacker J, Sabbagh J, Devaux J, Leloup G. Physico-mechanical characteristics of commercially available bulk-fill composites. J Dent. 2014;42(8):993–1000.
Ilie N, Bucuta S, Draenert M. Bulk-fill resin-based composites: an in vitro assessment of their mechanical performance. Oper Dent. 2013;38(6):618–25.
El Gezawi M, Kaisarly D, Al-Saleh H, ArRejaie A, Al-Harbi F, Kunzelmann KH. Degradation potential of bulk versus incrementally applied and indirect composites: color, microhardness, and surface deterioration. Oper Dent. 2016;41(6):e195–208.
Leprince J, Palin WM, Mullier T, Devaux J, Vreven J, Leloup G. Investigating filler morphology and mechanical properties of new low-shrinkage resin composite types. J Oral Rehabil. 2010;37(5):364–76.
Paolone MG, Kaitsas R, Paolone G, Kaitsas V. Lingual orthodontics and forced eruption: a means for osseous and tissue regeneration. Prog Orthod. 2008;9(2):46–57.
Heintze SD, Zimmerli B. Relevance of in vitro tests of adhesive and composite dental materials, a review in 3 parts. Part 1: approval requirements and standardized testing of composite materials according to ISO specifications. Schweiz Monatsschr Zahnmed. 2011;121(9):804–16.
Braga RR, Ballester RY, Ferracane JL. Factors involved in the development of polymerization shrinkage stress in resin-composites: a systematic review. Dent Mater. 2005;21(10):962–70.
Yamamoto T, Hanabusa M, Momoi Y, Sakaguchi RL. Polymerization stress of dental resin composite continues to develop 12 hours after irradiation. J Esthet Restor Dent. 2015;27(1):44–54.
Condon JR, Ferracane JL. Assessing the effect of composite formulation on polymerization stress. J Am Dent Assoc. 2000;131(4):497–503.
Calheiros FC, Braga RR, Kawano Y, Ballester RY. Relationship between contraction stress and degree of conversion in restorative composites. Dent Mater. 2004;20(10):939–46.
Feng L, Suh BI. A mechanism on why slower polymerization of a dental composite produces lower contraction stress. J Biomed Mater Res B Appl Biomater. 2006;78(1):63–9.
Gonçalves F, de Paiva CLM, Rodrigues-Júnior EC, Costa FV, Marques PA, Francci CE, et al. A comparative study of bulk-fill composites: degree of conversion, post-gel shrinkage and cytotoxicity. Braz Oral Res. 2018;32:e17.
Ferracane JL. Resin-based composite performance: are there some things we can’t predict? Dent Mater. 2013;29(1):51–8.
Jung JH, Park SH. Comparison of polymerization shrinkage, physical properties, and marginal adaptation of Flowable and restorative bulk fill resin-based composites. Oper Dent. 2017;42(4):375–86.
Prager M, Pierce M, Atria PJ, Sampaio C, Cáceres E, Wolff M, et al. Assessment of cuspal deflection and volumetric shrinkage of different bulk fill composites using non-contact phase microscopy and micro-computed tomography. Dent Mater J. 2018;37(3):393–9.
Yap AUJ, Chandra SP, Chung SM, Lim CT. Changes in flexural properties of composite restoratives after aging in water. Oper Dent. 2002;27(5):468–74.
Rodrigues Junior SA, Zanchi CH, de Carvalho RV, Demarco FF. Flexural strength and modulus of elasticity of different types of resin-based composites. Braz Oral Res. 2007;21(1):16–21.
Pontes LF, Alves EB, Alves BP, Ballester RY, Dias CGBT, Silva CM. Mechanical properties of nanofilled and microhybrid composites cured by different light polymerization modes. Gen Dent. 2013;61(3):30–3.
Szesz A, Parreiras S, Martini E, Reis A, Loguercio A. Effect of flowable composites on the clinical performance of non-carious cervical lesions: a systematic review and meta-analysis. J Dent. 2017;65:11–21.
Eweis AH, Yap AU, Yahya NA. Comparison of flexural properties of bulk-fill restorative/flowable composites and their conventional counterparts. Oper Dent. 2020;45(1):41–51.
Ferracane JL. Resin composite—state of the art. Dent Mater. 2011;27(1):29.
Shibasaki S, Takamizawa T, Nojiri K, Imai A, Tsujimoto A, Endo H, et al. Polymerization behavior and mechanical properties of high-viscosity bulk fill and low shrinkage resin composites. Oper Dent. 2017;42(6):E177–87.
de Mendonça BC, Soto-Montero JR, de Castro EF, Pecorari VGA, Rueggeberg FA, Giannini M. Flexural strength and microhardness of bulk-fill restorative materials. J Esthet Restor Dent. 2021;33(4):628–35.
Paolone G, Breschi L. Restauri diretti in composito: Le potenzialità di un sistema composito universale. Dent Cadmos. 2017;85(5):306–10.
Goracci C, Cadenaro M, Fontanive L, Giangrosso G, Juloski J, Vichi A, et al. Polymerization efficiency and flexural strength of low-stress restorative composites. Dent Mater. 2014;30(6):688–94.
Ilie N, Rencz A, Hickel R. Investigations towards nano-hybrid resin-based composites. Clin Oral Investig. 2013;17(1):185–93.
Ilie N, Hickel R. Investigations on mechanical behaviour of dental composites. Clin Oral Investig. 2009;13(4):427–38.
Masouras K, Silikas N, Watts DC. Correlation of filler content and elastic properties of resin-composites. Dent Mater. 2008;24(7):932–9.
Kalliecharan D, Germscheid W, Price RB, Stansbury J, Labrie D. Shrinkage stress kinetics of bulk fill resin-based composites at tooth temperature and long time. Dent Mater. 2016;32(11):1322–31.
Al Sunbul H, Silikas N, Watts DC. Polymerization shrinkage kinetics and shrinkage-stress in dental resin-composites. Dent Mater. 2016;32(8):998–1006.
Helvatjoglu-Antoniades M, Papadogiannis Y, Lakes RS, Dionysopoulos P, Papadogiannis D. Dynamic and static elastic moduli of packable and flowable composite resins and their development after initial photo curing. Dent Mater. 2006;22(5):450–9.
Yamamoto T, Hanabusa M, Kimura S, Momoi Y, Hayakawa T. Changes in polymerization stress and elastic modulus of bulk-fill resin composites for 24 hours after irradiation. Dent Mater J. 2018;37(1):87–94.
Pieniak D, Niewczas AM, Walczak M, Zamościńska J. Influence of photopolymerization parameters on the mechanical properties of polymer-ceramic composites applied in the conservative dentistry. Acta Bioeng Biomech. 2014;16(3):29–35.
Li J, Li H, Fok ASL, Watts DC. Multiple correlations of material parameters of light-cured dental composites. Dent Mater. 2009;25(7):829–36.
Tauböck TT, Oberlin H, Buchalla W, Roos M, Attin T. Comparing the effectiveness of self-curing and light curing in polymerization of dual-cured core buildup materials. J Am Dent Assoc. 2011;142(8):950–6.
Tauböck TT, Buchalla W, Hiltebrand U, Roos M, Krejci I, Attin T. Influence of the interaction of light- and self-polymerization on subsurface hardening of a dual-cured core build-up resin composite. Acta Odontol Scand. 2011;69(1):41–7.
Rueggeberg FA, Craig RG. Correlation of parameters used to estimate monomer conversion in a light-cured composite. J Dent Res. 1988;67(6):932–7.
Price RB, Whalen JM, Price TB, Felix CM, Fahey J. The effect of specimen temperature on the polymerization of a resin-composite. Dent Mater. 2011;27(10):983–9.
Watts DC, Amer O, Combe EC. Characteristics of visible-light-activated composite systems. Br Dent J. 1984;156(6):209–15.
Alshali RZ, Salim NA, Sung R, Satterthwaite JD, Silikas N. Analysis of long-term monomer elution from bulk-fill and conventional resin-composites using high performance liquid chromatography. Dent Mater. 2015;31(12):1587–98.
Rodriguez A, Yaman P, Dennison J, Garcia D. Effect of light-curing exposure time, shade, and thickness on the depth of cure of bulk fill composites. Oper Dent. 2017;42(5):505–13.
Tekin TH, Kantürk Figen A, Yılmaz Atalı P, Coşkuner Filiz B, Pişkin MB. Full in-vitro analyses of new-generation bulk fill dental composites cured by halogen light. Mater Sci Eng C Mater Biol Appl. 2017;77:436–45.
Son S-A, Park J-K, Seo D-G, Ko C-C, Kwon YH. How light attenuation and filler content affect the microhardness and polymerization shrinkage and translucency of bulk-fill composites? Clin Oral Investig. 2017;21(2):559–65.
Miletic V, Pongprueksa P, De Munck J, Brooks NR, Van Meerbeek B. Curing characteristics of flowable and sculptable bulk-fill composites. Clin Oral Investig. 2017;21(4):1201–12.
Chung KH, Greener EH. Correlation between degree of conversion, filler concentration and mechanical properties of posterior composite resins. J Oral Rehabil. 1990;17(5):487–94.
Garoushi S, Vallittu P, Shinya A, Lassila L. Influence of increment thickness on light transmission, degree of conversion and micro hardness of bulk fill composites. Odontology. 2016;104(3):291–7.
Flury S, Peutzfeldt A, Lussi A. Influence of increment thickness on microhardness and dentin bond strength of bulk fill resin composites. Dent Mater. 2014;30(10):1104–12.
Papadogiannis D, Tolidis K, Gerasimou P, Lakes R, Papadogiannis Y. Viscoelastic properties, creep behavior and degree of conversion of bulk fill composite resins. Dent Mater. 2015;31(12):1533–41.
Van Ende A, De Munck J, Lise DP, Van Meerbeek B. Bulk-fill composites: a review of the current literature. J Adhes Dent. 2017;19(2):95–109.
Ilie N, Hilton TJ, Heintze SD, Hickel R, Watts DC, Silikas N, et al. Academy of dental materials guidance-resin composites: part I-mechanical properties. Dent Mater. 2017;33(8):880–94.
Melo RA, SL BAD, GAS B, Galvão MR, de Assunção IV, Souza RO, et al. Morphochemical characterization, microhardness, water sorption, and solubility of regular viscosity bulk fill and traditional composite resins. Microsc Res Tech. 2019;82(9):1500–6.
Ilie N, Stark K. Effect of different curing protocols on the mechanical properties of low-viscosity bulk-fill composites. Clin Oral Investig. 2015;19(2):271–9.
Camassari JR, Correr-Sobrinho L, Correr AB, Puppin-Rontani J, Stipp RN, Puppin-Rontani RM, et al. Physical-mechanical properties of bulk fill composites submitted to biodegradation by Streptococcus mutans. Braz Dent J. 2020;31(4):431–9.
Carneiro FLLB, Barcellos A. Concrete tensile strength, Bulletin no. 13, Union of testing and research laboratories for materials and structures, Paris, France; 1953. pp. 97–123.
Sunbul HA, Silikas N, Watts DC. Surface and bulk properties of dental resin-composites after solvent storage. Dent Mater. 2016;32(8):987–97.
Medeiros IS, Gomes MN, Loguercio AD, Filho LER. Diametral tensile strength and Vickers hardness of a composite after storage in different solutions. J Oral Sci. 2007;49(1):61–6.
Alshali RZ, Salim NA, Satterthwaite JD, Silikas N. Long-term sorption and solubility of bulk-fill and conventional resin-composites in water and artificial saliva. J Dent. 2015;43(12):1511–8.
Janda R, Roulet J-F, Latta M, Rüttermann S. Water sorption and solubility of contemporary resin-based filling materials. J Biomed Mater Res B Appl Biomater. 2007;82(2):545–51.
Wei Y, Silikas N, Zhang Z, Watts DC. Diffusion and concurrent solubility of self-adhering and new resin-matrix composites during water sorption/desorption cycles. Dent Mater. 2011;27(2):197–205.
Chaves LP, Graciano FMO, Bim Júnior O, do Vale Pedreira APR, Manso AP, Wang L. Water interaction with dental luting cements by means of sorption and solubility. Braz Dent Sci. 2012;15:29–35.
Sideridou ID, Vouvoudi EC, Adamidou EA. Dynamic mechanical thermal properties of the dental light-cured nanohybrid composite Kalore, GC: effect of various food/oral simulating liquids. Dent Mater. 2015;31(2):154–61.
Bagheri R, Burrow MF, Tyas M. Influence of food-simulating solutions and surface finish on susceptibility to staining of aesthetic restorative materials. J Dent. 2005;33(5):389–98.
Ferracane JL. Hygroscopic and hydrolytic effects in dental polymer networks. Dent Mater. 2006;22(3):211.
Kalachandra S, Turner DT. Water sorption of polymethacrylate networks: bis-GMA/TEGDM copolymers. J Biomed Mater Res. 1987;21(3):329–38.
Bociong K, Szczesio A, Sokolowski K, Domarecka M, Sokolowski J, Krasowski M, et al. The influence of water sorption of dental light-cured composites on shrinkage stress. Materials (Basel). 2017;10(10):E1142.
Yiu CKY, King NM, Pashley DH, Suh BI, Carvalho RM, Carrilho MRO, et al. Effect of resin hydrophilicity and water storage on resin strength. Biomaterials. 2004;25(26):5789–96.
El-Safty S, Akhtar R, Silikas N, Watts DC. Nanomechanical properties of dental resin-composites. Dent Mater. 2012;28(12):1292–300.
Ilie N, Hickel R. Investigations on a methacrylate-based flowable composite based on the SDR™ technology. Dent Mater. 2011;27(4):348–55.
Attik N, Colon P, Gauthier R, Chevalier C, Grosgogeat B, Abouelleil H. Comparison of physical and biological properties of a flowable fiber reinforced and bulk filling composites. Dent Mater. 2022;38(2):e19–30.
Eapen AM, Amirtharaj LV, Sanjeev K, Mahalaxmi S. Fracture resistance of endodontically treated teeth restored with 2 different fiber-reinforced composite and 2 conventional composite resin core buildup materials: an in vitro study. J Endod. 2017;43(9):1499–504.
Shouha PSR, Ellakwa AE. Effect of short glass fibers on the polymerization shrinkage stress of dental composite. J Biomed Mater Res B Appl Biomater. 2017;105(7):1930–7.
Osiewicz MA, Werner A, Roeters FJM, Kleverlaan CJ. Wear of bulk-fill resin composites. Dent Mater. 2021;S0109-5641(21):00473–5.
Petrovic LM, Zorica DM, Stojanac IL, Krstonosic VS, Hadnadjev MS, Atanackovic TM. A model of the viscoelastic behavior of flowable resin composites prior to setting. Dent Mater. 2013;29(9):929–34.
Barkmeier WW, Takamizawa T, Erickson RL, Tsujimoto A, Latta M, Miyazaki M. Localized and generalized simulated wear of resin composites. Oper Dent. 2015;40(3):322–35.
Tauböck TT, Tarle Z, Marovic D, Attin T. Pre-heating of high-viscosity bulk-fill resin composites: effects on shrinkage force and monomer conversion. J Dent. 2015;43(11):1358–64.
Toh WS, Yap AUJ, Lim SY. In vitro biocompatibility of contemporary bulk-fill composites. Oper Dent. 2015;40(6):644–52.
Geurtsen W. Biocompatibility of resin-modified filling materials. Crit Rev Oral Biol Med. 2000;11(3):333–55.
Scott A, Egner W, Gawkrodger DJ, Hatton PV, Sherriff M, van Noort R, et al. The national survey of adverse reactions to dental materials in the UK: a preliminary study by the UK adverse reactions reporting project. Br Dent J. 2004;196(8):471–7; discussion 465.
Baharav H, Brosh T, Pilo R, Cardash H. Effect of irradiation time on tensile properties of stiffness and strength of composites. J Prosthet Dent. 1997;77(5):471–4.
Caughman WF, Caughman GB, Shiflett RA, Rueggeberg F, Schuster GS. Correlation of cytotoxicity, filler loading and curing time of dental composites. Biomaterials. 1991;12(8):737–40.
Salehi S, Gwinner F, Mitchell JC, Pfeifer C, Ferracane JL. Cytotoxicity of resin composites containing bioactive glass fillers. Dent Mater. 2015;31(2):195–203.
Marovic D, Tauböck TT, Attin T, Panduric V, Tarle Z. Monomer conversion and shrinkage force kinetics of low-viscosity bulk-fill resin composites. Acta Odontol Scand. 2015;73(6):474–80.
Furness A, Tadros MY, Looney SW, Rueggeberg FA. Effect of bulk/incremental fill on internal gap formation of bulk-fill composites. J Dent. 2014;42(4):439–49.
Jan Y-D, Lee B-S, Lin C-P, Tseng W-Y. Biocompatibility and cytotoxicity of two novel low-shrinkage dental resin matrices. J Formos Med Assoc. 2014;113(6):349–55.
Tauböck TT, Marovic D, Zeljezic D, Steingruber AD, Attin T, Tarle Z. Genotoxic potential of dental bulk-fill resin composites. Dent Mater. 2017;33(7):788–95.
Ferracane JL. Elution of leachable components from composites. J Oral Rehabil. 1994;21(4):441–52.
Durner J, Obermaier J, Draenert M, Ilie N. Correlation of the degree of conversion with the amount of elutable substances in nano-hybrid dental composites. Dent Mater. 2012;28(11):1146–53.
Benetti AR, Asmussen E, Munksgaard EC, Dewaele M, Peutzfeldt A, Leloup G, et al. Softening and elution of monomers in ethanol. Dent Mater. 2009;25(8):1007–13.
Cavalcante LM, Schneider LFJ, Silikas N, Watts DC. Surface integrity of solvent-challenged ormocer-matrix composite. Dent Mater. 2011;27(2):173–9.
Sevkusic M, Schuster L, Rothmund L, Dettinger K, Maier M, Hickel R, et al. The elution and breakdown behavior of constituents from various light-cured composites. Dent Mater. 2014;30(6):619–31.
Darmani H, Al-Hiyasat AS, Milhem MM. Cytotoxicity of dental composites and their leached components. Quintessence Int. 2007;38(9):789–95.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Paolone, G., Vichi, A. (2023). Physical and Mechanical Properties of BFC’s. In: Sabbagh, J., McConnell, R. (eds) Bulk Fill Resin Composites in Dentistry. Springer, Cham. https://doi.org/10.1007/978-3-031-16388-3_6
Download citation
DOI: https://doi.org/10.1007/978-3-031-16388-3_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-16387-6
Online ISBN: 978-3-031-16388-3
eBook Packages: MedicineMedicine (R0)