Abstract
Vestibular schwannoma (VS) represents a challenging intracranial tumor to treat. Almost a century ago, the most prominent neurosurgeons in Europe reported operative mortality rates greater than 70% [1–3]. Harvey Cushing, in the US, advocated for a wide bilateral posterior fossa decompression and intracapsular internal decompression of the tumor to achieve a safe subtotal resection (STR) and reduced the operative mortality to ~20% [4, 5]. Walter Dandy, on the other hand, described a unilateral craniectomy and complete tumor removal with the necessary sacrifice of cranial nerves VII and VIII but obviating the risk of tumor regrowth and need for additional treatment [6–9]. Over the next several decades, the integration of the operating microscope, improvement in neuroanesthetic techniques, and development of intraoperative electromyographic (EMG) monitoring have markedly improved the outcome from microsurgical resection of VS.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Introduction
Vestibular schwannoma (VS) represents a challenging intracranial tumor to treat. Almost a century ago, the most prominent neurosurgeons in Europe reported operative mortality rates greater than 70% [1,2,3]. Harvey Cushing, in the US, advocated for a wide bilateral posterior fossa decompression and intracapsular internal decompression of the tumor to achieve a safe subtotal resection (STR) and reduced the operative mortality to ~20% [4, 5]. Walter Dandy, on the other hand, described a unilateral craniectomy and complete tumor removal with the necessary sacrifice of cranial nerves VII and VIII but obviating the risk of tumor regrowth and need for additional treatment [6,7,8,9]. Over the next several decades, the integration of the operating microscope, improvement in neuroanesthetic techniques, and development of intraoperative electromyographic (EMG) monitoring have markedly improved the outcome from microsurgical resection of VS.
Lars Leksell from Sweden, internationally recognized as the father of stereotactic radiosurgery, treated his first patient with VS at the Karolinska Hospital in 1969 [10]. He reported 81% tumor control rate at a median follow-up of 3.7 years. The first Gamma Knife center in the United States was established at the University of Pittsburgh, which reported their 4-year data with 134 treated patients in 1993 [11]. The 4-year actuarial tumor control rate was 89.2% using a median marginal radiation dose of 17 Gy.
Currently, no prospective randomized controlled trials exist to directly compare the outcomes following radiosurgical and microneurosurgical options for acoustic neuromas; in the absence of class I evidence, three management strategies are available to this patient population: observation, stereotactic radiotherapy/radiosurgery, and microsurgical resection. This chapter provides an overview of the outcomes of each approach with respect to tumor control and preservation of cranial nerve function; particular emphasis is provided regarding stereotactic radiosurgery and fractionated radiotherapy.
Observation
There is a wealth of data in the medical literature to support the rationale for careful observation. Two systematic reviews based on 21 and 26 studies, respectively, with more than 1300 patients found the average annual growth rate of acoustic neuromas to be 1.2–1.9 mm, with 43–46% of tumors showing some degree of growth and only 18–20% requiring intervention at a mean follow-up of approximately 3 years [12, 13]. Tumor size at diagnosis, presence of disequilibrium, and cerebellopontine angle location rather than pure intracanalicular tumors have been reported to be associated with a higher risk of progression, thereby necessitating intervention [14, 15]. It should also be noted that some studies have reported that 3–11% of tumors will spontaneously regress without any form of intervention [13, 16, 17]. As such, elderly patients with small tumors represent the ideal population to be observed, especially on the grounds of increasing mean age at the time of diagnosis, that is, from 49 years in 1976 to 58 years in 2008 [18].
Patients who opt for watchful waiting are followed up with serial magnetic resonance imaging (MRI) and audiograms, typically every 6 months for the first year, then annually until year 5, and then biennially indefinitely. While the initial MRI scan should include gadolinium (Gd) to make sure there are not additional intracranial tumors, the follow-up scans can be thin-slice, heavily T2-weighted, steady state images without Gd as some recent reports suggest that Gd may accumulate in the brain—an increasing concern for some patients [19]. Evidence of tumor growth, that is, >2.5 mm/year, regardless of tumor size, is usually an indication for therapeutic intervention. If the patient cannot tolerate MRI, high-resolution computed tomography scanning with and without contrast is an option. Additionally, recently published guidelines suggest that, for intracanalicular or small tumors (<2 cm in the posterior fossa) without tinnitus, observation does not have a negative impact on tumor growth or hearing preservation compared to treatment [20]. However, according to data from the Acoustic Neuroma Association observation is associated with worsening of symptomatic tinnitus, whereas tinnitus severity is reduced with microsurgical resection or radiosurgery [21].
In an important observational study by Stangerup and colleagues, 932 patients were allocated with “wait and scan” with annual imaging and audiological examination over a follow-up period exceeding 10 years [22]. The authors found that the level of hearing preservation during follow-up correlated with speech discrimination (according to the American Academy of Otolaryngology-Head and Neck Surgery classification [AAO-HNS] [23]) at the time of diagnosis: 87% chance of maintaining good hearing (speech discrimination over 70%) for patients with perfect speech discrimination compared to 54% for patients with minor (1–10%) and 33% for those with moderate (21–30%) speech discrimination loss at the time of diagnosis [22, 23].
The same group recently showed that, in 156 patients with intracanalicular VS, tumor growth had occurred in 37% and growth into the cerebellopontine angle in 23% of patients after a mean follow-up of 9.5 years, while the proportion of patients with good hearing decreased from 52% to 22% [24]. Our institutional experience revealed a volumetric increase >20% from baseline AAO-HNS tumor size >2 mm at a median radiographic follow-up of 4.1 years. In addition, almost 70% of patients exhibited some degree of volumetric growth after a median of 1.1 years.
Finally, another important consideration is how tumor progression during the observation period may affect future treatment options. Two studies by Flint and colleagues and Shin and colleagues found that approximately 11–33% of observed patients will lose eligibility for hearing preservation surgery [17, 25]. In addition, Hajioff and colleagues reviewed the 10-year outcome data from 72 patients with unilateral VS that were managed conservatively, 25 of which required surgical intervention during the study period [14]. Interestingly, they demonstrated similar outcomes in patients who failed conservative management and those who underwent primary treatment without a period of observation [14].
In summary, observation is preferred for elderly patients, patients with small tumors and good hearing function, those who are poor surgical candidates, and those who refuse treatment. Based on a review by Telian and colleagues, the following factors should be taken into account when observation is recommended: patient’s life expectancy, tumor size and growth rate, neurofibromatosis type 2 status, preoperative hearing in both ears, and risk of complications, particularly hearing loss and facial nerve paralysis as a result of surgery [26].
Stereotactic Radiation and Radiosurgery
Radiation can be delivered to VS using either stereotactic radiosurgery (SRS) (≤5 fractions) or stereotactic radiotherapy (>5 fractions) (Table 10.1). Considerable contention exists in the literature regarding the comparative effectiveness of the two modalities for the management of patients with small to medium-sized tumors. Shared decision making should be based on patient preference between a minimally invasive 1-day procedure and up to 5–6 weeks of daily treatment, technology availability, and tumor size [27].
Stereotactic Radiosurgery
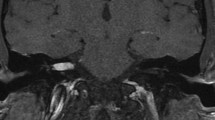
Stereotactic radiosurgery can be performed using either Leksell Gamma Knife® (Elekta Instruments, Norcross, GA, USA) or Linear Accelerator (LINAC) systems, such as X-knife (Radionics Inc., Burlington, MA, USA), Novalis® (BrainLAB, Heimstetten, Germany), Versa HD™ (Elekta Instruments, Norcross, GA, USA) and Cyberknife® (Accuray Inc., Sunnyvale, CA, USA). Gamma Knife uses a fixed number of cobalt radiation sources to deliver very focused radiation with steep fall-off beyond the target volume (Fig. 10.1). A stereotactic headframe is placed under local anesthesia that serves as both reference fiducials for stereotactic imaging and fixation in the device during treatment [28]. More recently, thanks to advances in computer software and machine hardware, “face masks” have been used to immobilize the patient thereby eliminating the need for a rigid frame (frameless stereotactic radiosurgery) while achieving a similar degree of precision. LINAC systems also make use of a stereotactic head frame; however, instead of relying on multiple fixed radiation sources, the arc radiation delivery system moves (Figs. 10.2 and 10.3). In newer systems, the patient’s bed moves along with the arcs in order to shape target volume and improve dose conformality. With respect to ionized particles emitted, these can either be photons, protons, or carbon ions.
The Cyberknife® (Accuray Inc., Sunnyvale, CA, USA) is a linear accelerator mounted on a six-axis robot that delivers radiation at the target from different positions. The system allows for the detection of patient movement and correction of dose delivery in real time. (Image courtesy of Accuray Incorporated—©2018 Accuray Incorporated. All Rights Reserved)
A landmark paper by the Pittsburgh group in 1998 demonstrated the excellent long-term (5–10 years) tumor control rates (i.e., 95%) that can be achieved with stereotactic radiosurgery [29]. In addition, function was noted to be preserved in 84% and 85% of patients with intact trigeminal and facial nerves at presentation, respectively, with 63% actuarial recovery rate of facial nerve deficit at 8 years. Subsequently, stereotactic radiosurgery and radiotherapy have become a very viable alternative to microsurgical removal of small to medium-sized VS.
Tumor Control Rates
Although there is an established body of literature on the effectiveness of radiosurgery for VS, the optimal parameters, including appropriate time of treatment, treatment modality (Gamma Knife vs. LINAC vs. proton beam) as well as dose and dosing scheme are still a matter of contention. A comprehensive review of the literature, including both retrospective and prospective studies, shows similar favorable radiosurgical failure rates ranging from 1.4% to 10.8% [30,31,32,33,34,35,36,37,38,39].
Following stereotactic radiosurgery, patients should be followed up with MRI scans and audiograms every 6 months for the first year, then annually for the next 2 years, then every other year for 4 years, then every 3 years for 6 years, and continuing in a similar pattern for the next few decades. Patients should also be informed that a transient increase in tumor volume after radiosurgery is an expected phenomenon (mean interval 13.4 months); therefore, additional treatments should not be hastily recommended [20, 40]. Median time to salvage microsurgery has been reported at 30–37 months (range 3–153 months) [31, 41, 42].
Hearing Preservation
Published hearing results following stereotactic radiosurgery have been highly variable among institutional series ranging from 23% to 74%, depending on the length of follow-up [30,31,32,33,34,35,36,37,38,39]. Most studies use the Gardner-Robertson classification scale (I–V, from good hearing to deaf), where hearing is considered preserved when it is class I (0–30 dB pure tone average and 70–100% speech discrimination) or class II (31–50 dB pure tone average and 50–69% speech discrimination). The American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS) scale uses the same criteria for defining useful hearing [23].
A pooled analysis by Coughlin and colleagues with almost 2200 patients showed a 58% crude hearing preservation rate after an average follow-up of 46.6 months [43]. Regarding longer-term outcomes, according to our experience, only 23% of patients maintained useful hearing (AAO-HNS Class A/B) at 10 years [39]. Similarly, Hasegawa and colleagues observed that hearing function remain unchanged in 68% of patients, while the useful hearing was preserved in 37% of cases [44].
Excellent pretreatment hearing remains the most predictive factor of preserved serviceable hearing irrespective of the cochlear dose. Proposed strategies suggest reducing the radiation dose to the cochlea with the rationale of improving hearing outcomes; however, this strategy may require that we reduce the marginal dose, thereby intentionally undertreating the lateral portion of the tumor and compromising long-term tumor control [45]. Several studies have identified a cochlear dose between 3.0 and 5.3 Gy as the optimal threshold, beyond which risk of losing serviceable hearing increases significantly [36, 37, 46, 47].
Cranial Nerve Function
Besides the vestibulocochlear nerves, the cranial nerves mostly at risk following stereotactic radiosurgery are the trigeminal and the facial nerves. Several reviews have identified tumor size and the delivered marginal dose to be important prognostic factors for subsequent risk of cranial neuropathy [31, 48,49,50]. Evidence has consistently shown that a marginal tumor dose of 12–13 Gy is associated with excellent trigeminal and facial nerve preservation rates, which range from 92% to 100% [30, 31, 48, 51,52,53,54,55,56,57,58]. These rates are lower, though, in patients who have undergone microsurgical resection prior to radiosurgery [50].
Linskey and colleagues hypothesized that it is the CN length, rather than tumor volume and dose that determines the risk of cranial neuropathy following SRS [59]. Specifically, they found the pons-petrous distance and the mid-porous transverse tumor diameter to independently correlate with the risk of neuropathy. Consequently, the maximal diameter allowable for radiosurgery is generally accepted as 3 cm; however, some centers may still treat larger lesions by administering a dose lower than 12 Gy or employing fractionation. Data regarding the function of the vestibular nerve are more limited. A detailed examination of vestibular function by Fukuoka and colleagues showed that almost 90% of patients had some degree of vestibular dysfunction before radiosurgery and that treatment did not significantly affect vestibular function [52]. In addition, persistent dizziness was observed in 2% of patients. Similarly, Combs and colleagues reported that patients presenting with dizziness noticed no improvement following treatment [60]. In a series of 117 patients by Murphy and colleagues, 4% of patients reported new vertigo and 18% had new gait imbalance [61]. Finally, Badakhshi and colleagues conducted a retrospective analysis of 190 patients treated with a LINAC-based, image-guided system and found that 14% of patients had worse symptoms compared to baseline, while 29% had symptom relief.
Fractionated Radiotherapy
Fractionated radiotherapy refers to radiation delivered in multiple fractions. When it is delivered in a small number of fractions (i.e., 2–5) it is referred to as hypofractionated. Wallner and colleagues were the first to report the use of fractionated radiotherapy as an adjunct treatment to STR and biopsy [62]. Local tumor recurrence decreased from 46% to 6% when doses greater than 45 Gy were delivered to the postoperative bed, with an actuarial 15-year tumor control rate equal to 94% [62]. Accordingly, the first report with 20-year data noted a tumor control rate of 88% at 5 years and 85% at 15 years; the mean radiation dosage was 51 Gy with an average of 1.8 Gy per fraction and a 1–2 mm margin on the contrast-enhanced tumor image on MRI [27, 63,64,65,66,67].
With the popularization of stereotactic techniques, advanced radiotherapy technologies have allowed for more conformal dose distributions. Stereotactic radiotherapy emerged as an attractive option after reports of high rates of cranial neuropathy following initially high single-fraction doses (i.e., 16 Gy) [30]. Tumors with a pons-petrous distance >1 cm and mid-porous transverse diameter >2 cm were the first ones to be treated [59, 68]. Several stereotactic radiotherapy schemes have been reported in the literature for the treatment of VS [28, 41, 60, 64, 69,70,71]. Current dosing schemes typically range from 1.8 to 2.0 Gy per fraction for a total maximum dose of 40.0–57.6 Gy.
Reported local tumor control rates are estimated at 94–100% [41, 61]. Similarly, trigeminal and facial nerve preservation rates range from 84–100% and 96–100%, respectively [72]. Fractionating the total radiation dosage into a series of smaller doses aims to minimize injury to adjacent cranial nerves, particularly the cochlear nerve. Though inconsistently measured, hearing preservation rates are estimated at 61–98%, based on a systematic review by Jian and colleagues of modern series (843 patients with a median follow-up ranging from 1.6 to 9 years) [72].
It is worth mentioning that in the largest contemporary series by Aoyama and colleagues and by Litre and colleagues, with a total 356 patients who underwent fractionated stereotactic radiotherapy (median total dose of 50 Gy in sessions of 1.8–2 Gy), tumor growth necessitating new intervention was noted in 4.8% at a median follow-up of 60–72 months [73, 74]. Hearing deterioration (Gardner-Robertson class I–II to III–V) was observed in 45%, facial nerve deterioration in 2.5–2.7%, and trigeminal nerve deterioration in 2–3.6% of patients.
Data on hypofractionated radiotherapy (five sessions) is more limited. According to a systematic review by Nguyen and colleagues of 228 patients treated with LINAC-based systems (total dose of 20–25 Gy), estimated pooled tumor control rates average 95%, while hearing, facial nerve, and trigeminal nerve preservation rates were 37%, 97%, and 98%, respectively [75]. Lastly, with regard to the number of sessions and outcomes, Meijer and colleagues treated 80 patients with a fractionated schedule (20–25 Gy in five fractions) and 49 patients in a single fraction (10 or 12.5 Gy) [65]. Tumor control, facial nerve preservation, and hearing preservation rates at 5 years were similar for the two groups. Interestingly, patients receiving the hypofractionated regimen had a significantly higher trigeminal nerve preservation rate (98% vs. 92%).
Comparing Radiosurgery and Radiotherapy
Currently, data from prospective, randomized studies directly comparing the outcomes following the two methods do not exist, which is partly attributed to physician bias or patient expectations that influence treatment decision, thereby rendering enrollment very challenging [60, 76]. Comparisons across different studies are even more difficult given the wide variety of definitions of tumor control and hearing preservation (the Gardner-Robertson hearing classification scale is less often used by fractionated groups). Though each technique has distinct technical properties and radiobiologic benefits, there is little evidence on the superiority of one technique over the other (Table 10.1).
Andrews and colleagues retrospectively compared 125 patients and found equivalent tumor control (98% vs. 97%) and preservation of CN V (95% vs. 93%) and VII (98% vs. 98%) function between radiosurgery (12 Gy) and fractionated radiotherapy (50 Gy) [76]. Hearing preservation was significantly lower in the radiosurgery group (33% vs. 81% at a median follow-up of 41 and 38 weeks, respectively). In a similar fashion, Combs and colleagues compared 191 patients who were treated with LINAC-based single-dose radiosurgery (≤13 Gy) versus fractionated stereotactic radiotherapy (57.6 Gy) and observed comparable tumor control (96% vs. 96%) and hearing preservation (78% vs. 78%) rates at a median follow-up of 75 months [60].
In regard to hearing preservation, the most satisfactory results have been achieved with stereotactic fractionated radiotherapy, with the majority of studies reporting 61–98% hearing preservation rate after a total dose of 40–57.6 Gy at a median follow-up ranging from 1.6 to 9 years [72]. However, more long-term follow-up data are needed before conclusions are made. Thomas and colleagues reported a delay in sensorineural hearing loss following fractionated radiotherapy occurring with a latency of 1.5–5 years [71]. Interestingly, in the study by Combs and colleagues, the majority of hearing detriment was observed at 6–10 months after treatment [60].
Proton Beam Therapy
Proton beam therapy has been employed for the treatment of VS as well. Its highly conformal properties and rapid dose fall-off in combination with minimal exit dose offer an appealing advantage over photon-based systems, which is particularly beneficial in the treatment of intracranial targets surrounded by sensitive critical structures, including the cochlea.
Proton beam therapy has been utilized in several delivery schemes, including single-fraction, hypofractionated, and fractionated approaches. For example, Bush and colleagues administered 54 and 60 cobalt-Gy equivalents (cGye) in 30–33 fractions for patients with and without useful hearing (Gardner-Robertson class I–II vs. III–V), respectively [77]. Tumor control rates have been reported to range from 84% to 100% at a mean follow-up of 34–60 months [77,78,79,80]. Cranial nerve function rates were excellent as well; studies have reported trigeminal and facial nerve preservation rates of 89–100% and 91–100%, respectively. Finally, hearing results are less satisfactory. Based on these early experiences, hearing preservation rates were 31–42%, which might be attributed to the small proportion of patients presenting with useful hearing.
In summary, the theoretical advantages of proton beam therapy should be weighed against its much higher cost; until firmer evidence is established, its application for the treatment of patients with VS will be fairly limited.
Risk of Secondary Malignancy
Risk of malignant transformation is exceedingly rare, and only case reports exist in the literature after an interval of 5–30-years of follow-up [81,82,83]. According to an institutional review by Rowe and colleagues of 5000 patients treated with SRS over 30,000 patient-years of follow-up, a single new brain astrocytoma was detected, which is lower than the anticipated number of 2.47 cases based on population statistics. Given that SRS typically delivers radiation in a single fraction to a small target and regional tissue volume, which is more likely to lead to cell death than cell transmutation, the risk of delayed malignancy is very small [84]. The risk theoretically might be higher with fractionated external beam radiotherapy as radiation is delivered in more sessions but still remains extremely small.
Summary
The guideline panel of the Congress of Neurological Surgeons recently released its recommendations on the management of acoustic neuromas with radiation [20]. According to the guideline panel, it is recommended that doses less than 13 Gy should be used in single-fraction stereotactic radiosurgery schemes to facilitate hearing preservation and minimize new onset or worsening of preexisting cranial nerve deficits [20]. Additionally, the report highlighted that follow-up imaging should be obtained at regular intervals after SRS based on “clinical indications, a patient’s personal circumstances, or institutional protocols” [20]. Currently, there is not sufficient evidence to support the superiority of radiosurgery over radiotherapy with respect to tumor control rates. Therefore, future prospective trials are needed to provide firm evidence on the optimal use of the various radiation modalities, ideally leading to an appropriate individualized management algorithm for patients with VS.
Microsurgery
Microsurgical resection combined with sophisticated cranial nerve monitoring has been a widely accepted option for the treatment of VS with varying degrees of hearing loss. Microsurgical approaches to acoustic tumors can be grouped into three broad categories: retrosigmoid, translabyrinthine, and middle fossa approaches, each with its own advantages and disadvantages. Some surgeons prefer a single technique to remove all types of tumors regardless of size and related symptoms. Others tailor their approach based on tumor characteristics, patient’s preference/expectations, and audiologic parameters [85,86,87].
One of the earliest documentations of VS resection is attributed to Annandale in 1895, who attempted a unilateral suboccipital approach [88, 89]. In 1904, Parry described a middle fossa approach to the vestibulocochlear complex for the surgical management of a patient with tinnitus and vertigo [90]. In 1912, Franciscus H. Quix published the first translabyrinthine resection as part of a two-stage procedure [91]; the approach was later popularized by William House [92]. As previously detailed, Harvey Cushing and Walter Dandy contributed greatly to the advancement of the surgical treatment of VS [4, 89, 93, 94].
As Gonzalez and Spetzler highlight, the internal auditory canal (IAC) may be accessed through different approaches that are based on distinct trajectories [95]. The retrosigmoid is the most common one, as it is the approach that most neurosurgeons are familiar with, allowing for exposure of the IAC in an angle parallel to the petrous surface. On the other hand, the translabyrinthine approach is ideal for tumors confined to the IAC or when they extend laterally beyond the “accessible” region, after the posterior lip of the IAC has been drilled [95]. It is generally preferred when hearing is severely compromised (Gardner-Robertson class III or IV) or is not an issue because of tumor size (usually larger than 2 cm) [95, 96]. Finally, compared to the other two, the middle fossa approach offers satisfactory exposure of the IAC and its contents, including the facial (all segments) and superior vestibular nerves, through a superior trajectory. It is primarily employed for small lesions confined to the IAC, or less than 1 cm in posterior fossa diameter, particularly when preservation of hearing is desired.
Complete surgical removal is the best answer for long-term recurrence-free outcomes. Nakatomi and colleagues also showed the extent of resection to be the strongest predictor of recurrence, with patients treated with STR having a nearly 11-fold greater risk of recurrence compared to those who underwent gross total resection (GTR) [97]. Specifically, recurrence-free survival rates at 10 and 15 years were estimated to be 82% and 73% for GTR compared to 17% and 8% for STR, respectively [97]. Comparably, a study by Jacob and colleagues revealed a 13-fold higher risk of recurrence for STR than near total resection (NTR), with the median to recurrence following NTR being 124 months compared to 32 months after STR [98]. The authors concluded that complete resection should be the primary goal of microsurgery and less than complete resection should be based on intraoperative impression, on the grounds of potential neurological deficit due to “continued dissection of adherent disease” [98]. In addition, a review of the literature by Yamakami and colleagues demonstrated 0–2% recurrence with long-term follow-up when the majority of tumors were completely removed [99]. Significantly higher rate was observed in only one small study with 33 patients in which 69% had a subtotal removal and 20% had a recurrence. More recently, a preliminary report of the Acoustic Neuroma Subtotal Resection Study (prospective, multicenter, nonrandomized cohort study) revealed three-times higher risk of recurrence in patients with vestibular schwannoma ≥2.5 cm who had STR compared to GTR and NTR [100].
Hearing Results
Often, the most important factor determining the surgical approach is preoperative hearing status. Reported rates of hearing preservation after retrosigmoid or middle fossa approaches range from 17% to 88% [101, 102]. Generally, the average risk of serviceable hearing loss correlates with tumor size, with the risk increasing with increasing tumor size. Additionally, the extension of the tumor to the fundus of the IAC and cochlear aperture is a negative predictor of ability to remove the tumor and preserve useful hearing. The considerable variety in audiologic criteria used renders the comparability of hearing outcomes across studies difficult [23, 102, 103]. At a minimum, useful hearing requires speech discrimination scores greater than 50% and a pure tone average sufficient for amplification (typically >50 dB).
Facial Nerve Outcomes
Preservation of facial nerve function is one of the important drivers of surgical success from the patient’s perspective. Although not directly life-threatening, facial nerve palsy can be life-altering, particularly in cases of minimal postoperative recovery of function. Excellent rates of facial nerve function preservation can be achieved with all three surgical approaches [101, 102, 104,105,106]. The middle fossa approach is associated with worse facial nerve outcomes than the retrosigmoid approach based on directly comparative studies [102, 105]. It should be noted that facial nerve outcomes worsen as tumor size increases [107]. For tumors larger than 2.5 cm, the rates for both translabyrinthine and retrosigmoid approaches range from 50% to 94%, with functional “good” results from 20% to 80% [108].
In an attempt to preserve facial nerve function, many surgeons will opt for STR or NTR followed by radiosurgery either primarily or because of tumor remnant growth. According to recently published guidelines, more than 90% of patients maintain normal or near normal facial function, rates better than those reported for GTR (31.4–92.8%) [109]. In the Acoustic Neuroma Subtotal Resection Study, good facial nerve function (House-Brackmann grade I and II) was achieved in 67% immediately and 81% at 1 year [100]. Furthermore, immediate facial nerve function (House-Brackmann grade I/II) was associated with smaller preoperative tumor diameter and volume as well as a larger percentage of the tumor left behind [100].
Cerebrospinal Fluid Leakage
Cerebrospinal fluid (CSF) leakage is the most common complication associated with VS surgery [32]. Reported rates are highly variable in the literature, ranging from more than 20% to as low as 0%, depending on the approach, surgeons’ experience, operative time, and patient’s body mass index [110,111,112]. In the largest study to date, Alattar and colleagues queried a statewide administrative database and found an incidence of readmission with CSF leak of 3.5% among 6820 patients with VS treated between 1995 and 2010 [113]. Significant factors found to be independently associated with readmission for CSF leak were male sex, obesity, teaching-hospital status, and hospital case volume. Regardless of the approach, the meticulous surgical technique is critical in reducing the risk of CSF leakage. Careful application of bone wax to exposed air cells and packing autologous fat or muscle is now standard [114]. More recently, hydroxyapatite bony replacement and tissue glues have been proposed as well; however, their effectiveness is not well established, and they may present a higher risk of infection [87, 115].
Patient Reported Quality of Life
Given the increasingly important role of patient reported outcomes in healthcare quality measurement, there have been a rising number of publications investigating patient’s health-related quality of life (QOL), symptom-associated disability, and treatment satisfaction using subjective instruments [116,117,118,119]. This increase is particularly relevant to the study of VS because the focus of treatment has shifted from survival to improvement in patient functionality, symptoms, and well-being. To date, the only validated instrument specifically designed for patients with sporadic VS is the Penn Acoustic Neuroma QOL (PANQOL) questionnaire [120].
To date, only four prospective observational studies have been published looking at patients’ QOL following different treatment modalities [121,122,123,124]. Pollock and colleagues as well as Myrseth and colleagues demonstrated more favorable outcomes for radiosurgery compared to surgical resection, whereas Di Maio observed similar trends in QOL following observation, radiation therapy, or surgery after a mean follow-up period of 31.8 months [121, 123, 124]. Finally, Breivik and colleagues reported a statistically significant, albeit small, improvement in vertigo and balance but no change in tinnitus comparing radiosurgery to microsurgery and observation after a median observation period of 43 months [122].
Carlson and colleagues investigated long-term QOL in VS patients managed with microsurgery, stereotactic radiosurgery, and observation in two tertiary academic referral centers in the United States and Western Europe. Mean interval between treatment and survey was 7.7 years. Interestingly, microsurgical management was found to be associated with the greatest decrease in health-related QOL measurements. Furthermore, patients who underwent microsurgery had significantly lower PANQOL total score by 8–11% compared with those managed with stereotactic radiosurgery or observation, respectively. The questionnaire domains in which the largest differences were observed included facial function (13–14%), balance (10–19%), and pain (19–30%) [125]. In another large-scale study by Soulier and colleagues, patients with tumors ≤10 mm in size under observation reported significantly higher total PANQOL score compared to the radiosurgical and microsurgical groups at a mean follow-up of 4 years [126].
In addition, we recently analyzed QOL data from 143 patients enrolled in a prospective, international study [127]. GTR was achieved in 122 patients while the remaining had STR. Interestingly, we found GTR to be associated with better QOL at a mean follow-up of 7.7 years after surgery across all three measures used (i.e., Short Form-36, PROMIS-10, and PANQOL, even after adjusting for baseline and outcome differences thereby indicating that there is a psychological advantage to patient reported well-being when the entire tumor is removed).
Yet, it should be noted that several of the reported differences in QOL might not represent significant changes from the patient’s perspective. Carlson and colleagues published the minimum clinically important thresholds for the PANQOL domain and total scores and found that they exceeded the differences reported in prior studies, which based conclusions on QOL benefit among VS treatment modalities on statistical significance alone [128].
Conclusions
Significant advances have been made in the past three decades in the management of VS. Currently, three options exist: observation, stereotactic radiosurgery/radiotherapy, and microsurgical resection. Observation may be offered to patients with small lesions and minor symptoms while stereotactic radiation/radiosurgery is a good option for tumors up to 3 cm in size. Comparable tumor control rates have been demonstrated using the different radiation modalities. Contemporary single-session radiosurgery schemes allow for hearing preservation rates greater than 60% in short-term follow-up and a risk of facial weakness of approximately 1%. Surgery remains a commonly employed treatment, particularly in patients with large tumors causing brainstem compression or progressive neurological symptoms.
References
Ballance SCA. Some points in the surgery of the brain and its membranes. London: Macmillan; 1908.
Koerbel A, Gharabaghi A, Safavi-Abbasi S, Tatagiba M, Samii M. Evolution of vestibular schwannoma surgery: the long journey to current success. Neurosurg Focus. 2005;18:e10.
Krause F. Discussion of von Eiselsberg’s paper. Tr Int Cong Med Lond VII. 1913;214.
Cushing H. Tumors of the nervus acusticus and the syndrome of the cerebellopontile angle. Philadelphia: W.B. Saunders; 1917.
Cushing H. Further concerning the acoustic neuromas. Laryngoscope. 1921;31:209–28.
Dandy WE. An operation for the total extirpation of tumors in the cerebello-pontine angle. A preliminary report. Bull Johns Hopkins Hosp. 1922;33:344–5.
Dandy WE, Others. An operation for the total removal of cerebellopontine (acoustic) tumors. Surg Gynecol Obstet. 1925;41:129–48.
Dandy WE. Removal of cerebellopontile (acoustic) tumors through a unilateral approach. Arch Surg. 1934;29:337–44.
Dandy WE. Results of removal of acoustic tumors by the unilateral approach. Arch Surg. 1941;42:1026–33.
Leksell L. A note on the treatment of acoustic tumours. Acta Chir Scand. 1971;137:763–5.
Flickinger JC, Lunsford LD, Linskey ME, Duma CM, Kondziolka D. Gamma knife radiosurgery for acoustic tumors: multivariate analysis of four year results. Radiother Oncol. 1993;27:91–8.
Smouha EE, Yoo M, Mohr K, Davis RP. Conservative management of acoustic neuroma: a meta-analysis and proposed treatment algorithm. Laryngoscope. 2005;115:450–4.
Yoshimoto Y. Systematic review of the natural history of vestibular schwannoma. J Neurosurg. 2005;103:59–63.
Hajioff D, Raut VV, Walsh RM, et al. Conservative management of vestibular schwannomas: third review of a 10-year prospective study. Clin Otolaryngol. 2008;33:255–9.
Malhotra PS, Sharma P, Fishman MA, et al. Clinical, radiographic, and audiometric predictors in conservative management of vestibular schwannoma. Otol Neurotol. 2009;30:507–14.
Hoistad DL, Melnik G, Mamikoglu B, Battista R, O’Connor CA, Wiet RJ. Update on conservative management of acoustic neuroma. Otol Neurotol. 2001;22:682–5.
Shin YJ, Fraysse B, Cognard C, et al. Effectiveness of conservative management of acoustic neuromas. Am J Otol. 2000;21:857–62.
Stangerup S-E, Caye-Thomasen P. Epidemiology and natural history of vestibular schwannomas. Otolaryngol Clin N Am. 2012;45:257–68.
Pullicino R, Radon M, Biswas S, Bhojak M, Das K. A review of the current evidence on gadolinium deposition in the brain. Clin Neuroradiol. 2018;28:159–69. https://doi.org/10.1007/s00062-018-0678-0.
Olson JJ, Kalkanis SN, Ryken TC. Congress of neurological surgeons systematic review and evidence-based guidelines on the treatment of adults with vestibular schwannomas: executive summary. Neurosurgery. 2018;82:129–34.
Van Gompel JJ, Patel J, Danner C, et al. Acoustic neuroma observation associated with an increase in symptomatic tinnitus: results of the 2007–2008 Acoustic Neuroma Association survey. Collections. 2013;118:864–8.
Stangerup S-E, Thomsen J, Tos M, Cayé-Thomasen P. Long-term hearing preservation in vestibular schwannoma. Otol Neurotol. 2010;31:271–5.
Balkany TA, Gates GA, Goldenberg RA, et al. Committee on Hearing and Equilibrium guidelines for the evaluation of hearing preservation in acoustic neuroma (vestibular schwannoma). Otolaryngol Head Neck Surg. 1995;113:179–80.
Kirchmann M, Karnov K, Hansen S, Dethloff T, Stangerup S-E, Caye-Thomasen P. Ten-year follow-up on tumor growth and hearing in patients observed with an intracanalicular vestibular schwannoma. Neurosurgery. 2017;80:49–56.
Flint D, Fagan P, Panarese A. Conservative management of sporadic unilateral acoustic neuromas. J Laryngol Otol. 2005;119:424–8.
Telian SA. Management of the small acoustic neuroma: a decision analysis. Am J Otol. 1994;15:358–65.
Murphy ES, Suh JH. Radiotherapy for vestibular schwannomas: a critical review. Int J Radiat Oncol Biol Phys. 2011;79:985–97.
Link MJ, Driscoll CLW, Foote RL, Pollock BE. Radiation therapy and radiosurgery for vestibular schwannomas: indications, techniques, and results. Otolaryngol Clin N Am. 2012;45:353–66.
Kondziolka D, Lunsford LD, McLaughlin MR, Flickinger JC. Long-term outcomes after radiosurgery for acoustic neuromas. N Engl J Med. 1998;339:1426–33.
Chopra R, Kondziolka D, Niranjan A, Lunsford LD, Flickinger JC. Long-term follow-up of acoustic schwannoma radiosurgery with marginal tumor doses of 12 to 13 Gy. Int J Radiat Oncol Biol Phys. 2007;68:845–51.
Hasegawa T, Fujitani S, Katsumata S, Kida Y, Yoshimoto M, Koike J. Stereotactic radiosurgery for vestibular schwannomas: analysis of 317 patients followed more than 5 years. Neurosurgery. 2005;57:257–65.
Pollock BE, Lunsford LD, Kondziolka D, et al. Outcome analysis of acoustic neuroma management: a comparison of microsurgery and stereotactic radiosurgery. Neurosurgery. 1995;36:215–24.
Friedman RA, Kesser B, Brackmann DE, Fisher LM, Slattery WH, Hitselberger WE. Long-term hearing preservation after middle fossa removal of vestibular schwannoma. Otolaryngol Head Neck Surg. 2003;129:660–5.
Régis J, Pellet W, Delsanti C, et al. Functional outcome after gamma knife surgery or microsurgery for vestibular schwannomas. J Neurosurg. 2013;119:1091–100.
Yang I, Sughrue ME, Han SJ, et al. A comprehensive analysis of hearing preservation after radiosurgery for vestibular schwannoma. J Neurosurg. 2010;112:851–9.
Kano H, Kondziolka D, Khan A, Flickinger JC, Lunsford LD. Predictors of hearing preservation after stereotactic radiosurgery for acoustic neuroma. J Neurosurg. 2009;111:863–73.
Hasegawa T, Kida Y, Kato T, Iizuka H, Yamamoto T. Factors associated with hearing preservation after Gamma Knife surgery for vestibular schwannomas in patients who retain serviceable hearing. J Neurosurg. 2011;115:1078–86.
Hasegawa T, Kida Y, Kato T, Iizuka H, Kuramitsu S, Yamamoto T. Long-term safety and efficacy of stereotactic radiosurgery for vestibular schwannomas: evaluation of 440 patients more than 10 years after treatment with Gamma Knife surgery. J Neurosurg. 2013;118:557–65.
Carlson ML, Jacob JT, Pollock BE, et al. Long-term hearing outcomes following stereotactic radiosurgery for vestibular schwannoma: patterns of hearing loss and variables influencing audiometric decline. J Neurosurg. 2013;118:579–87.
Williams BJ, Xu Z, Salvetti DJ, McNeill IT, Larner J, Sheehan JP. Gamma Knife surgery for large vestibular schwannomas: a single-center retrospective case-matched comparison assessing the effect of lesion size. J Neurosurg. 2013;119:463–71.
Chan AW, Black P, Ojemann RG, et al. Stereotactic radiotherapy for vestibular schwannomas: favorable outcome with minimal toxicity. Neurosurgery. 2005;57:60–70.
Wise SC, Carlson ML, Tveiten ØV, et al. Surgical salvage of recurrent vestibular schwannoma following prior stereotactic radiosurgery. Laryngoscope. 2016;126:2580–6.
Coughlin AR, Willman TJ, Gubbels SP. Systematic review of hearing preservation after radiotherapy for vestibular schwannoma. Otol Neurotol. 2018;39:273–83.
Hasegawa T, Kida Y, Kobayashi T, Yoshimoto M, Mori Y, Yoshida J. Long-term outcomes in patients with vestibular schwannomas treated using gamma knife surgery: 10-year follow up. J Neurosurg. 2005;102:10–6.
Jacob JT, Pollock BE, Carlson ML, Driscoll CLW, Link MJ. Stereotactic radiosurgery in the management of vestibular schwannoma and glomus jugulare: indications, techniques, and results. Otolaryngol Clin N Am. 2015;48:515–26.
Jacob JT, Carlson ML, Schiefer TK, Pollock BE, Driscoll CL, Link MJ. Significance of cochlear dose in the radiosurgical treatment of vestibular schwannoma: controversies and unanswered questions. Neurosurgery. 2014;74:466–74.
Massager N, Nissim O, Delbrouck C, et al. Irradiation of cochlear structures during vestibular schwannoma radiosurgery and associated hearing outcome. J Neurosurg. 2007;107:733–9.
Friedman WA, Bradshaw P, Myers A, Bova FJ. Linear accelerator radiosurgery for vestibular schwannomas. J Neurosurg. 2006;105:657–61.
Foote KD, Friedman WA, Buatti JM, Meeks SL, Bova FJ, Kubilis PS. Analysis of risk factors associated with radiosurgery for vestibular schwannoma. J Neurosurg. 2001;95:440–9.
Spiegelmann R, Lidar Z, Gofman J, Alezra D, Hadani M, Pfeffer R. Linear accelerator radiosurgery for vestibular schwannoma. J Neurosurg. 2001;94:7–13.
Combs SE, Thilmann C, Debus J, Schulz-Ertner D. Long-term outcome of stereotactic radiosurgery (SRS) in patients with acoustic neuromas. Int J Radiat Oncol Biol Phys. 2006;64:1341–7.
Fukuoka S, Takanashi M, Hojyo A, Konishi M, Tanaka C, Nakamura H. Gamma knife radiosurgery for vestibular schwannomas. Prog Neurol Surg. 2009;22:45–62.
Iwai Y, Yamanaka K, Kubo T, Aiba T. Gamma knife radiosurgery for intracanalicular acoustic neuromas. J Clin Neurosci. 2008;15:993–7.
Kalogeridi M-A, Georgolopoulou P, Kouloulias V, Kouvaris J, Pissakas G. Long-term results of LINAC-based stereotactic radiosurgery for acoustic neuroma: the Greek experience. J Cancer Res Ther. 2009;5:8–13.
Kim K-M, Park C-K, Chung H-T, Paek SH, Jung H-W, Kim DG. Long-term outcomes of gamma knife stereotactic radiosurgery of vestibular schwannomas. J Korean Neurosurg Soc. 2007;42:286–92.
Myrseth E, Moller P, Pedersen P-H, Vassbotn FS, Wentzel-Larsen T, Lund-Johansen M. Vestibular schwannomas: clinical results and quality of life after microsurgery or gamma knife radiosurgery. Neurosurgery. 2005;56:927–35.
Prasad D, Steiner M, Steiner L. Gamma surgery for vestibular schwannoma. J Neurosurg. 2000;92:745–59.
Unger F, Walch C, Schröttner O, Eustacchio S, Sutter B, Pendl G. Cranial nerve preservation after radiosurgery of vestibular schwannomas. Acta Neurochir Suppl. 2002;84:77–83.
Linskey ME, Flickinger JC, Lunsford LD. Cranial nerve length predicts the risk of delayed facial and trigeminal neuropathies after acoustic tumor stereotactic radiosurgery. Int J Radiat Oncol Biol Phys. 1993;25:227–33.
Combs SE, Welzel T, Schulz-Ertner D, Huber PE, Debus J. Differences in clinical results after LINAC-based single-dose radiosurgery versus fractionated stereotactic radiotherapy for patients with vestibular schwannomas. Int J Radiat Oncol Biol Phys. 2010;76:193–200.
Murphy ES, Barnett GH, Vogelbaum MA, et al. Long-term outcomes of Gamma Knife radiosurgery in patients with vestibular schwannomas. J Neurosurg. 2011;114:432–40.
Wallner KE, Sheline GE, Pitts LH, Wara WM, Davis RL, Boldrey EB. Efficacy of irradiation for incompletely excised acoustic neurilemomas. J Neurosurg. 1987;67:858–63.
Maire J-P, Huchet A, Milbeo Y, et al. Twenty years’ experience in the treatment of acoustic neuromas with fractionated radiotherapy: a review of 45 cases. Int J Radiat Oncol Biol Phys. 2006;66:170–8.
Fuss M, Debus J, Lohr F, et al. Conventionally fractionated stereotactic radiotherapy (FSRT) for acoustic neuromas. Int J Radiat Oncol Biol Phys. 2000;48:1381–7.
Meijer OWM, Vandertop WP, Baayen JC, Slotman BJ. Single-fraction vs. fractionated linac-based stereotactic radiosurgery for vestibular schwannoma: a single-institution study. Int J Radiat Oncol Biol Phys. 2003;56:1390–6.
Selch MT, Pedroso A, Lee SP, et al. Stereotactic radiotherapy for the treatment of acoustic neuromas. J Neurosurg. 2004;101:362–72.
Combs SE, Volk S, Schulz-Ertner D, Huber PE, Thilmann C, Debus J. Management of acoustic neuromas with fractionated stereotactic radiotherapy (FSRT): long-term results in 106 patients treated in a single institution. Int J Radiat Oncol Biol Phys. 2005;63:75–81.
Kalapurakal JA, Silverman CL, Akhtar N, Andrews DW, Downes B, Thomas PR. Improved trigeminal and facial nerve tolerance following fractionated stereotactic radiotherapy for large acoustic neuromas. Br J Radiol. 1999;72:1202–7.
Andrews DW, Werner-Wasik M, Den RB, et al. Toward dose optimization for fractionated stereotactic radiotherapy for acoustic neuromas: comparison of two dose cohorts. Int J Radiat Oncol Biol Phys. 2009;74:419–26.
Koh E-S, Millar B-A, Menard C, et al. Fractionated stereotactic radiotherapy for vestibular schwannoma: single institutional experience at the Princess Margaret Hospital. Radiother Oncol. 2005;76:S29.
Thomas C, Di Maio S, Ma R, et al. Hearing preservation following fractionated stereotactic radiotherapy for vestibular schwannomas: prognostic implications of cochlear dose. J Neurosurg. 2007;107:917–26.
Jian BJ, Kaur G, Sayegh ET, Bloch O, Parsa AT, Barani IJ. Fractionated radiation therapy for vestibular schwannoma. J Clin Neurosci. 2014;21:1083–8.
Litre F, Rousseaux P, Jovenin N, et al. Fractionated stereotactic radiotherapy for acoustic neuromas: a prospective monocenter study of about 158 cases. Radiother Oncol. 2013;106:169–74.
Aoyama H, Onodera S, Takeichi N, et al. Symptomatic outcomes in relation to tumor expansion after fractionated stereotactic radiation therapy for vestibular schwannomas: single-institutional long-term experience. Int J Radiat Oncol Biol Phys. 2013;85:329–34.
Nguyen T, Duong C, Sheppard JP, et al. Hypo-fractionated stereotactic radiotherapy of five fractions with linear accelerator for vestibular schwannomas: a systematic review and meta-analysis. Clin Neurol Neurosurg. 2018;166:116–23.
Andrews DW, Suarez O, Goldman HW, et al. Stereotactic radiosurgery and fractionated stereotactic radiotherapy for the treatment of acoustic schwannomas: comparative observations of 125 patients treated at one institution. Int J Radiat Oncol Biol Phys. 2001;50:1265–78.
Bush DA, Mcallister CJ, Loredo LN, Johnson WD, Slater JM, Slater JD. Fractionated proton beam radiotherapy for acoustic neuroma. Neurosurgery. 2002;50:270–5.
Harsh GR, Thornton AF, Chapman PH, Bussiere MR, Rabinov JD, Loeffler JS. Proton beam stereotactic radiosurgery of vestibular schwannomas. Int J Radiat Oncol Biol Phys. 2002;54:35–44.
Vernimmen FJAI, Mohamed Z, Slabbert JP, Wilson J. Long-term results of stereotactic proton beam radiotherapy for acoustic neuromas. Radiother Oncol. 2009;90:208–12.
Weber DC, Chan AW, Bussiere MR, et al. Proton beam radiosurgery for vestibular schwannoma: tumor control and cranial nerve toxicity. Neurosurgery. 2003;53:577–88.
Tanbouzi Husseini S, Piccirillo E, Taibah A, Paties CT, Rizzoli R, Sanna M. Malignancy in vestibular schwannoma after stereotactic radiotherapy: a case report and review of the literature. Laryngoscope. 2011;121:923–8.
Fusco DJ, Williamson R, Yanamadala V, Eschbacher J, Porter R, Weisskopf P. Malignant transformation of a vestibular schwannoma following gamma knife radiosurgery: case report and review of the literature. J Neurol Surg B Skull Base. 2012;73:A293.
Niranjan A, Kondziolka D, Lunsford LD. Neoplastic transformation after radiosurgery or radiotherapy: risk and realities. Otolaryngol Clin N Am. 2009;42:717–29.
Kondziolka D, Mousavi SH, Kano H, Flickinger JC, Lunsford LD. The newly diagnosed vestibular schwannoma: radiosurgery, resection, or observation? Neurosurg Focus. 2012;33:E8.
Wiet RJ, Mamikoglu B, Odom L, Hoistad DL. Long-term results of the first 500 cases of acoustic neuroma surgery. Otolaryngol Head Neck Surg. 2001;124:645–51.
Sanna M, Taibah A, Russo A, Falcioni M, Agarwal M. Perioperative complications in acoustic neuroma (vestibular schwannoma) surgery. Otol Neurotol. 2004;25:379–86.
Bambakidis NC, Megerian CA, Spetzler RF. Surgery of the cerebellopontine angle. Shelton, CT: PMPH-USA; 2009.
Ramsden RT. A brilliant surgical result, the first recorded: Annandale’s case, 3 May 1895. J Laryngol Otol. 1995;109:369–73.
Olson JJ, Kalkanis SN, Ryken TC. Congress of neurological surgeons systematic review and evidence-based guidelines on the treatment of adults with vestibular schwannomas: introduction and methods. Neurosurgery. 2018;82:135.
Parry RH. A case of tinnitus and vertigo treated by division of the auditory nerve. J Laryngol Otol. 1904;19:402–6.
Quix FH. Ein Fall von translabyrintharisch operiertem Tumor acusticus. Verh Dtsch Otol Ges. 1912;21:245–55.
House WF. Transtemporal bone microsurgical removal of acoustic neuromas. Report of cases. Arch Otolaryngol. 1964;80:617–67.
Dandy WE, et al. An operation for the total removal of cerebellopontine (acoustic) tumors. Surg Gynecol Obstet. 1925;41:129–48.
Dandy WE. Removal of cerebellontine (acoustic) tumors through a unilateral approach. Arch Surg. 1934;29:337–44.
Gonzalez LF, Lekovic GP, Porter RW, Syms MJ, Daspit CP, Spetzler RF. Surgical approaches for resection of acoustic neuromas. Barrow Q. 2004;20:1–11.
Day JD, Chen DA, Arriaga M. Translabyrinthine approach for acoustic neuroma. Neurosurgery. 2004;54:391–6.
Nakatomi H, Jacob JT, Carlson ML, et al. Long-term risk of recurrence and regrowth after gross-total and subtotal resection of sporadic vestibular schwannoma. J Neurosurg. 2017;19:1–7.
Jacob JT, Carlson ML, Driscoll CL, Link MJ. Volumetric analysis of tumor control following subtotal and near-total resection of vestibular schwannoma. Laryngoscope. 2016;126:1877–82.
Yamakami I, Uchino Y, Kobayashi E, Yamaura A. Conservative management, gamma-knife radiosurgery, and microsurgery for acoustic neurinomas: a systematic review of outcome and risk of three therapeutic options. Neurol Res. 2003;25:682–90.
Monfared A, Corrales CE, Theodosopoulos PV, et al. Facial nerve outcome and tumor control rate as a function of degree of resection in treatment of large acoustic neuromas: preliminary report of the acoustic neuroma subtotal resection study (ANSRS). Neurosurgery. 2016;79:194–203.
Mangham CA Jr. Retrosigmoid versus middle fossa surgery for small vestibular schwannomas. Laryngoscope. 2004;114:1455–61.
Sanna M, Khrais T, Russo A, Piccirillo E, Augurio A. Hearing preservation surgery in vestibular schwannoma: the hidden truth. Ann Otol Rhinol Laryngol. 2004;113:156–63.
Samii M, Matthies C. Management of 1000 vestibular schwannomas (acoustic neuromas): hearing function in 1000 tumor resections. Neurosurgery. 1997;40:248–62.
McElveen JT Jr, Belmonte RG, Fukushima T, Bullard DE. A review of facial nerve outcome in 100 consecutive cases of acoustic tumor surgery. Laryngoscope. 2000;110:1667–72.
Colletti V, Fiorino F. Middle fossa versus retrosigmoid-transmeatal approach in vestibular schwannoma surgery: a prospective study. Otol Neurotol. 2003;24:927–34.
Arts HA, Telian SA, El-Kashlan H, Thompson BG. Hearing preservation and facial nerve outcomes in vestibular schwannoma surgery: results using the middle cranial fossa approach. Otol Neurotol. 2006;27:234–41.
Fenton JE, Chin RY, Fagan PA, Sterkers O, Sterkers JM. Predictive factors of long-term facial nerve function after vestibular schwannoma surgery. Otol Neurotol. 2002;23:388–92.
Lanman TH, Brackmann DE, Hitselberger WE, Subin B. Report of 190 consecutive cases of large acoustic tumors (vestibular schwannoma) removed via the translabyrinthine approach. J Neurosurg. 1999;90:617–23.
Hadjipanayis CG, Carlson ML, Link MJ, et al. Congress of neurological surgeons systematic review and evidence-based guidelines on surgical resection for the treatment of patients with vestibular schwannomas. Neurosurgery. 2018;82:E40–3.
Copeland WR, Mallory GW, Neff BA, Driscoll CLW, Link MJ. Are there modifiable risk factors to prevent a cerebrospinal fluid leak following vestibular schwannoma surgery? J Neurosurg. 2015;122:312–6.
Murphy ME, McCutcheon BA, Kerezoudis P, et al. Morbid obesity increases risk of morbidity and reoperation in resection of benign cranial nerve neoplasms. Clin Neurol Neurosurg. 2016;148:105–9.
Selesnick SH, Liu JC, Jen A, Carew JF. Management options for cerebrospinal fluid leak after vestibular schwannoma surgery and introduction of an innovative treatment. Otol Neurotol. 2004;25:580–6.
Alattar AA, Hirshman BR, McCutcheon BA, et al. Risk factors for readmission with cerebrospinal fluid leakage within 30 d of vestibular schwannoma surgery. Neurosurgery. 2018;82:630–7. https://doi.org/10.1093/neuros/nyx197.
Isaacson JE. Radiologic follow-up after vestibular schwannoma surgery. Otol Neurotol. 2005;26:552.
Costantino PD, Hiltzik DH, Sen C, et al. Sphenoethmoid cerebrospinal fluid leak repair with hydroxyapatite cement. Arch Otolaryngol Head Neck Surg. 2001;127:588–93.
Gauden A, Weir P, Hawthorne G, Kaye A. Systematic review of quality of life in the management of vestibular schwannoma. J Clin Neurosci. 2011;18:1573–84.
Gouveris HT, Mann WJ. Quality of life in sporadic vestibular schwannoma: a review. ORL J Otorhinolaryngol Relat Spec. 2010;72:69–74.
Martin HC, Sethi J, Lang D, Neil-Dwyer G, Lutman ME, Yardley L. Patient-assessed outcomes after excision of acoustic neuroma: postoperative symptoms and quality of life. J Neurosurg. 2001;94:211–6.
Nicoucar K, Momjian S, Vader J-P, De Tribolet N. Surgery for large vestibular schwannomas: how patients and surgeons perceive quality of life. J Neurosurg. 2006;105:205–12.
Shaffer BT, Cohen MS, Bigelow DC, Ruckenstein MJ. Validation of a disease-specific quality-of-life instrument for acoustic neuroma: the Penn Acoustic Neuroma Quality-of-Life Scale. Laryngoscope. 2010;120:1646–54.
Di Maio S, Akagami R. Prospective comparison of quality of life before and after observation, radiation, or surgery for vestibular schwannomas. J Neurosurg. 2009;111:855–62.
Breivik CN, Varughese JK, Wentzel-Larsen T, Vassbotn F, Lund-Johansen M. Conservative management of vestibular schwannoma—a prospective cohort study: treatment, symptoms, and quality of life. Neurosurgery. 2012;70:1072–80.
Myrseth E, Møller P, Pedersen P-H, Lund-Johansen M. Vestibular schwannoma: surgery or gamma knife radiosurgery? A prospective, nonrandomized study. Neurosurgery. 2009;64:654–63.
Pollock BE, Driscoll CLW, Foote RL, et al. Patient outcomes after vestibular schwannoma management: a prospective comparison of microsurgical resection and stereotactic radiosurgery. Neurosurgery. 2006;59:77–85.
Carlson ML, Tveiten OV, Driscoll CL, Goplen FK. Long-term quality of life in patients with vestibular schwannoma: an international multicenter cross-sectional study comparing microsurgery, stereotactic radiosurgery. J Neurosurg. 2015;122:833–42.
Soulier G, van Leeuwen BM, Putter H, et al. Quality of life in 807 patients with vestibular schwannoma: comparing treatment modalities. Otolaryngol Head Neck Surg. 2017;157:92–8.
Link MJ, Lund-Johansen M, Lohse CM, et al. Quality of life in patients with vestibular schwannomas following gross total or less than gross total microsurgical resection: should we be taking the entire tumor out? Neurosurgery. 2018;82:541–7.
Carlson ML, Tveiten ØV, Yost KJ, Lohse CM, Lund-Johansen M, Link MJ. The minimal clinically important difference in vestibular schwannoma quality-of-life assessment: an important step beyond P < .05. Otolaryngol Head Neck Surg. 2015;153:202–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Kerezoudis, P., Weisskopf, P.A., Driscoll, C.L.W., Link, M.J. (2022). Treatment Options for Acoustic Neuroma, Including Stereotactic Radiosurgery. In: Bambakidis, N.C., Megerian, C.A., Spetzler, R.F. (eds) Surgery of the Cerebellopontine Angle. Springer, Cham. https://doi.org/10.1007/978-3-031-12507-2_10
Download citation
DOI: https://doi.org/10.1007/978-3-031-12507-2_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-12506-5
Online ISBN: 978-3-031-12507-2
eBook Packages: MedicineMedicine (R0)