Abstract
Brain code is a term used to describe acute, unstable intracranial hypertension or elevated intracranial pressure. Anesthesiologists often become involved in the management of brain codes if the patient requires neurosurgical intervention or if they require advanced airway management due to decompensating neurologic and respiratory status. The following chapter discusses the anesthetic management of stroke codes, signs and symptoms of elevated intracranial pressure, and the acute management of intracranial hypertension.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Brain code
- Intracranial hypertension
- Intracranial pressure
- Neurosurgery
- Stroke code
- Neurocritical care
- Altered mental status
Case Outline
Learning Objectives
-
1.
Discuss anesthetic management of stroke code.
-
2.
Describe signs and symptoms of elevated intracranial pressure.
-
3.
Discuss acute management of elevated intracranial pressure.
Simulator Environment
-
1.
Location: interventional radiology suite of an adult hospital.
-
2.
Manikin setup:
-
(a)
Age: adult
-
(b)
Lines: 1 x 20 Gauge (G) peripheral intravenous (PIV) line, radial arterial line, foley catheter
-
(c)
Monitors: non-invasive blood pressure (NIBP) cuff, 5-lead electrocardiogram (EKG), pulse oximeter
-
(a)
-
3.
Medications available: normal saline, propofol, etomidate, succinylcholine, rocuronium, epinephrine, albuterol, fentanyl, midazolam, calcium chloride, hypertonic saline, mannitol.
-
4.
Equipment available
-
(a)
Airway equipment: ventilator, face mask, laryngoscope and cuffed and uncuffed endotracheal tubes (ETTs) of various sizes, stylet, oral airway, nasal trumpet, laryngeal mask airway (LMA), suction, fiberoptic bronchoscope, video laryngoscope.
-
(b)
Monitors: pulse oximeter, blood pressure cuff, 5-lead EKG.
-
(c)
Lines: arterial line kit, central line kit, PIV kits
-
(d)
Crash cart with defibrillator
-
(e)
Paperwork: pre-operative anesthesia history and physical
-
(a)
Actors
-
1.
Scrub tech
-
(a)
The scrub tech is busy opening trays.
-
(a)
-
2.
Circulator nurse
-
(a)
The nurse is busy charting.
-
(a)
-
3.
Neuro-interventional radiologist
-
(a)
The neuro-interventional radiology (Neuro-IR) team is focused on locating and removing the clot.
-
(a)
Case Narrative
-
1.
Scenario background given to participants:
-
(a)
You are the anesthesiologist taking care of a 70-year-old man with poorly controlled type 2 diabetes mellitus (T2DM) and severe gastroesophageal reflux disease (GERD). He was found down in the parking lot of a grocery store and on exam was found to have dysarthria, dysphagia, facial droop, and hemiparesis. Computed tomography (CT) scan of the head confirmed acute ischemic middle cerebral artery (MCA) stroke.
-
(b)
He is currently in the interventional radiology suite undergoing diagnostic cerebral angiogram and clot removal under monitored anesthesia care (MAC)/sedation with propofol infusion for maintenance of anesthesia.
-
(c)
Medications: insulin, metformin, gabapentin.
-
(d)
Preoperative labs: potassium (K) 4.9, hemoglobin (Hb) 11.5, bicarbonate (HCO3) 30.
-
(a)
-
2.
Phase 1: coughing, vomiting and nonresponsiveness
-
(a)
The patient is initially doing well, calm, breathing spontaneously on simple face mask. The surgeons are advancing their catheter towards the clot when suddenly the patient starts coughing and moving. The patient is unable to remain still despite verbal instructions from the staff. He then turns his head and throws up. He becomes nonresponsive, hypoventilating, and is no longer following commands.
-
(b)
The learner should move to the head of the bed and recognize the hypoventilation and acute change in neurologic status. The learner should move to intubate as soon as possible to protect against aspiration.
-
(a)
-
3.
Phase 2: intracranial bleed leading to elevated intracranial pressure
-
(a)
The blood pressure will acutely increase to systolic blood pressure (SBP) 190 s and the heart rate will slow down to the 40s–50s. The surgeon will now report that on angiogram, there was an accidental rupture of a major cerebral artery that must have occurred while the patient was coughing.
-
(b)
The learner should recognize an acute intracranial bleed now resulting in elevated intracranial pressure, and should activate a brain code. They should recommend the following steps:
-
(i)
The surgeon will remove the catheter and hold pressure at the groin site.
-
(ii)
Brain code will be activated to alert pharmacy and neurology.
-
(iii)
Administer mannitol or hypertonic saline loading dose/infusion.
-
(iv)
Hyperventilate the patient.
-
(v)
Alert the operating room and prepare for possible surgical decompression – Burr holes, craniotomy for clot evacuation.
-
(vi)
Ask the surgeons to consider emergent external ventricular drain (EVD) placement for intracranial pressure (ICP) treatment and monitoring.
-
(vii)
Elevate head of bed.
-
(viii)
Manage hemodynamics: maintain goal cerebral perfusion pressure (CPP) >60 while also controlling hypertension to avoid hematoma expansion.
-
(i)
-
(a)
Scoring Rubric
Summary of Clinical Teaching Points
What are the pros and cons of doing a diagnostic cerebral angiogram and intervention under general anesthesia with an endotracheal tube (GETA) versus monitored anesthesia care (MAC)/sedation?
What are the signs and symptoms of intracranial hypertension? [1,2,3,4]
-
Presentation
-
Headache
-
Decreased consciousness
-
Vomiting
-
Cushing triad: hypertension, bradycardia, respiratory arrest
-
Dilated pupil on ipsilateral side of hemorrhage
-
Cranial nerve palsies III, IV, VI – double vision, ptosis
-
-
When to call a brain code
-
Signs of herniation
-
Intracranial pressure >20 cm H2O for >3 minutes
-
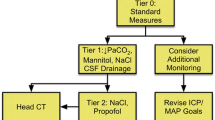
How do you manage intracranial hypertension? [1,2,3,4]
-
Activate hospital Brain Code to alert Pharmacy and Neurology
-
Administer mannitol or hypertonic saline loading dose or infusion.
-
Hyperventilate the patient.
-
Operative management
-
Alert the operating room and prepare for possible surgical decompression – Burr holes, craniotomy for clot evacuation.
-
Ask the surgeons to consider emergent external ventricular drain (EVD) placement for intracranial pressure (ICP) treatment and monitoring.
-
-
Elevated head of bed.
-
Manage hemodynamics: goal cerebral perfusion pressure (CPP) >60 mmHg, intracranial pressure (ICP) <20 mmHg.
-
If someone is herniating, do not use antihypertensives to lower blood pressure – generally need a higher mean arterial pressure (MAP) in the setting of higher ICP to maintain CPP.
-
Also avoid overshooting MAP, which will skyrocket cerebral blood flow (CBF) and exacerbate ICP.
-
-
Ensure adequate oxygenation.
-
Consider antiepileptics.
-
Consider antipyretics.
-
Avoid hyperglycemia.
How do you manage intracranial hemorrhage? [1,2,3,4]
-
Immediate control of blood pressure within 10 minutes
-
Goal is to prevent hematoma from expanding
-
Goal systolic blood pressure (SPB) <150 mmHg
-
Antihypertensives: nicardipine, labetalol, hydralazine
-
-
Immediate reversal of coagulopathy
How do you decide whether to use hypertonic saline or mannitol to treat intracranial hypertension? [1,2,3,4]
References
Curry P, Viernes D, Sharma D. Perioperative management of traumatic brain injury. Int J Crit Illn Inj Sci. 2011;1(1):27–35.
Abraham P, Rennert RC, Gabel BC, Sack JA, Karanjia N, Warnke P, Chen CC. ICP management in patients suffering from traumatic brain injury: a systematic review of randomized controlled trials. Acta Neurochir. 2017;159(12):2279–87.
Stevens RD, Shoykhet M, Cadena R. Emergency neurological life support: intracranial hypertension and herniation. Neurocrit Care. 2015;23(Suppl 2):S76–82.
Kalanuria AA, Geocadin RG, Püttgen HA. Brain code and coma recovery: aggressive management of cerebral herniation. Semin Neurol. 2013 Apr;33(2):133–41.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Sampankanpanich Soria, C. (2022). Brain Code (Adult). In: Sampankanpanich Soria, C., Trivedi, S. (eds) Pediatric and Adult Anesthesiology Simulation Education. Springer, Cham. https://doi.org/10.1007/978-3-030-95338-6_7
Download citation
DOI: https://doi.org/10.1007/978-3-030-95338-6_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-95337-9
Online ISBN: 978-3-030-95338-6
eBook Packages: MedicineMedicine (R0)