Abstract
The goals of orthodontic treatment are to correct the malocclusion and position the dentition in its most harmonious position in relation to the craniofacial structures. Traditional diagnostic data gathering approaches relied heavily on analyzing two-dimensional and static three-dimensional data such as radiographs and dental casts to obtain the most appropriate diagnosis for a given malocclusion and suggest the applicable treatment options accordingly. Digital three-dimensional data can be obtained, analyzed and measured using various three-dimensional imaging processes. These processes can also be merged into specialized software to allow the practitioner to visualize the craniofacial structures and dentition simultaneously, thus significantly increasing the accuracy of the diagnosis and treatment planning process. This chapter describes the digital three-dimensional imaging procedures and compares them to the conventional two-dimensional acquisition processes. The advantages of these technologies and the best practice of implementation are also described.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 The Objectives of an Orthodontic Diagnosis
Capturing diagnostic information to analyze the craniofacial complex is a demanding process in modern orthodontics. The craniofacial structures are highly organized with many vital functions and dynamic interactions. Breathing, mastication, swallowing, speech, and facial expressions are controlled by complex neuromuscular functions that must be in balance [1]. These interactions play a large role in the development of malocclusions but are still not well understood. They are also difficult to correlate with our current diagnostic methods [2, 3]. The temporomandibular joints are the most complex joints in our body. They are potentially associated with craniofacial dysfunctions but their imaging is currently not a routine part of a conventional orthodontic diagnosis [4], although dental models are sometimes mounted on a semi-adjustable articulator to give better 3D orientation of the dentition in relation to condylar position. All clinical information needed to obtain an accurate orthodontic diagnosis are not readily available with conventional records since malocclusions develop in three planes of space and may involve the entire craniofacial complex [5]. 3D imaging and advances in digital technologies have significantly increased the potential for integrating different formats of orthodontic records to enhance the accuracy of the orthodontic diagnosis process [6] (Fig. 1.1).
The goals for accurate orthodontic diagnoses are to record and analyze interactions between the dentition and surrounding craniofacial structures, and to obtain a problem list to formulate a treatment plan [7]. A large quantity of information is gathered from an orthodontic clinical examination, analyses of 2D radiographs and orthodontic study models, as well as other relevant records of a patient. These orthodontic records are usually taken in a static state [8, 9]. Consequently, these records only partially reflect the intricacies of craniofacial and dentoalveolar structures, and therefore limit their diagnostic power [10]. As traditional diagnosis and treatment planning procedures are usually performed without a patient being present, orthodontic records are aimed to faithfully replicate clinical presentations of a patient in order to facilitate these procedures [11]. To obtain an orthodontic diagnosis, most orthodontists still rely mainly on 2D radiographs such as a cephalogram [12] and a panoramic radiograph [13, 14], in addition to plaster dental casts which have been in use since the eighteenth century. Each element of these records provides orthodontists with a different type of information. Orthodontists combine all these data from clinical experiences and derive a differential diagnosis of the observed malocclusions. The process of recording a 3D structure on 2D radiograph causes a significant loss of data [15]. This is due to the fact that a conventional 2D radiograph is a mere “shadow” of a 3D object and provide only a partial or incomplete detail of projected structures. As a result, clinicians must always use their considerable skill and experience to “interpret” radiographs in a “forward propagation” method [16] in an attempt to arrive at an accurate diagnosis as each element of these conventional orthodontic records is variably formatted. They cannot be digitally integrated to recreate a virtual patient for the purpose of diagnosis and treatment planning. The inability of these conventional diagnostic tools to accurately portray malocclusion and its associated craniofacial structures in three dimensions may result in an incomplete diagnosis or a misdiagnosis [17, 18]. An integrable set of 3D orthodontic records recreating a real patient’s anatomy and function is therefore desirable to increase diagnostic accuracy, and to ensure that a treatment option selected can be effectively implemented [19, 20] (Fig. 1.2).
For the past 15 years, significant changes have taken place in the field of orthodontic diagnosis. These changes include uses of digital photography, digital examination forms, cone beam radiography [21], digital dental models [22], and intraoral scanning. They have allowed for a large amount of clinical information to be gathered. The additional diagnostic information has opened new possibilities for orthodontists. Sequential records easily obtained with intraoral scanning, digital photography and radiography facilitate various treatment simulations and may further customize orthodontic treatment approaches, and even perform in-house 3D printing [23]. Despite these advances, there is still a significant paucity of knowledge required to optimize the use of 3D digital technologies for orthodontic records [24]. A recent data mining technology offers new possibilities to improve on orthodontic diagnostic process [25]. The goals of gathering and computing digital orthodontic data are:
-
1.
To obtain the most accurate depiction of the patient’s unique occlusal and craniofacial structures
-
2.
To store the data efficiently
-
3.
To simulate different treatment options
-
4.
To formulate a final treatment plan
-
5.
To compare the findings to other types of malocclusions
-
6.
To facilitate an analysis of treatment progress
-
7.
To plan for orthognathic surgery
-
8.
To produce individualized and customized appliances
- 9.
2 Evolution of the Orthodontic Record Overtime
2.1 Examination Form
Paper-based forms have been widely used to gather relevant patient information. They include a questionnaire, a medical history, recording of extra- and intraoral examination, and patient’s chief complaints. These collected data are rarely reviewed during treatment and almost never incorporated into any database.
2.1.1 Dental Photographs
Dental photographs were introduced several decades ago [26]. Extraoral photographs provide valuable information on a patient’s facial features while intraoral photographs record conditions and positions of teeth in relation to each other and to surrounding soft tissues [27]. Dental photographs are not quantifiable, unless properly calibrated. They mostly provide qualitative data used by most clinicians to validate their physical observation of patients [28] (Fig. 1.5).
2.1.2 Panoramic Radiographs
A panoramic radiograph is based on the concept of focal plane tomography as described by Pickens et al. [29]. Widely used in orthodontics, it enables clinicians to visualize all teeth present, temporomandibular joints, the alveolus, and other orofacial structures in a single radiograph [14]. For a routine diagnostic process, a panoramic radiograph offers several advantages including low costs and easy access. It dispenses low amount of radiation. It is considered more like a screening radiograph and does not allow for consistent and reliable measurements. Despite its benefits, the radiograph provides an incomplete rendering of the anatomy or pathology presented by a patient. Both false positive and negative interpretations occur frequently [30]. As an example, the following panoramic radiograph (Fig. 1.6) shows impacted canines but does not provide any spatial information or their relationship to the rest of the dentition [31]. The condition of the lateral incisor roots is also very challenging to assess. The use of Cone Beam Computed Tomography (CBCT) allows clinicians to accurately assess the condition of the lateral incisor roots (Fig. 1.7).
2.1.3 Cephalometric Radiograph
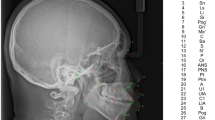
The lateral cephalogram depicts a projection of the entire craniofacial structures onto a sagittal 2D plane [32]. It is mainly used to perform cephalometric analyses to compare a patient’s measurements to standard norms [33]. Cephalometric radiographs are very valuable in orthodontics as they provide a measurable assessment of maxilla, mandible, dentition, and their spatial relationships in the anteroposterior and vertical dimensions [34]. Anatomical structures such as the condyles, temporal fossa, and auditory meatus are sometimes more challenging to identify as they are not located on the mid-sagittal plane [35]. The 2D posteroanterior cephalogram is not commonly employed as a part of routine orthodontic records despite its usefulness in transverse analyses. This could be due to the fact that landmarks used in the aforementioned analyses are difficult to identify and reproduce [36] (Fig. 1.8).
2.1.4 Orthodontic Study Models
Orthodontic study models are usually composed of free-posteriorly standing maxillary and mandibular dental casts trimmed in a trimmed in centric occlusion relationship. They are traditionally made of plaster of Paris. They provide invaluable information on multiple parameters that influences orthodontic diagnosis and treatment planning [37]. The models are not three-dimensionally oriented to the surrounding craniofacial complex, particularly regarding the condylar position. They are useful to obtain information on relative spatial relationship of the dentition and allow for measurements of teeth and dentoalveolar structures. However, it is impossible using orthodontic study models to determine accurate root positions and their relations to surrounding dentoalveolar bones using orthodontic study models. It is also very tedious to perform a simulation of an orthodontic treatment plan on plaster models. Each simulation requires a considerable effort and time to achieve. In general, they have less diagnostic capabilities when compared to their digital counterparts [38] (Fig. 1.9).
In conclusion, the conventional diagnostic process has allowed orthodontists to obtain a reasonably accurate diagnosis in the past [39]. However, validity of the process with fragmented 2D records has often been challenged in this current digital era. The conventional orthodontic records do not significantly improve a diagnostic power despite a carefully conducted clinical examination [16, 39]. This could be explained by the fact that there may be a significant loss of clinical information from these disintegrated formats of records [40].
3 The Rationale for 3D Digital Orthodontic Records: A More Accurate Method to Analyze the Craniofacial Complex
The digital technology with its inherent characteristics of accuracy, speed, and reproducibility is fast gaining acceptance by the orthodontic community [41]. In a digital orthodontic office, a patient file is created by a practice management software prior to patient’s initial visit. During the diagnostic phase of an orthodontic treatment, an electronic orthodontic screening form, 3D radiographic records (e.g., CBCT in DICOM file format), intraoral photographs, and intraoral dental scan (in STL file format) can all be merged into a single digital patient dataset [42]. This dataset is then transferred to a Computer-Assisted Design (CAD) software to create an individualized and interactive 3D rendering of an orthodontic patient. One of the most promising application of this digitally integrated patient data is the ability to analyze multiple variables of a malocclusion and its surrounding craniofacial structures. This also allows orthodontists to fully customize a treatment plan to address the specific needs of a patient [43, 44]. With this technology, 3D analyses of craniofacial structures, occlusion, and dentoalveolar support measurements can be simultaneously performed to formulate the most appropriate treatment plan and alternatives. After patients agree and consent to a treatment plan, this integrated digital data set can also be used to create individualized appliances with Computer-Aided-Design (CAD) software and Computer-Assisted Manufacturing (CAM) technology. Customization and individualization of the entire treatment process are some of the major advantages of digital technology [45]. Currently both clear aligners and orthodontic fixed appliances can be fabricated in-house as a result of these technologies [46].
Once an electronic patient’s file is created, any forms, charts, communications, and digital records can be digitally added. These files can be kept in local servers or by using cloud storage. The stored data may be used for treatment planning and communication with the patient and other clinicians in any location with a secure internet connection [47]. Data backups can also be performed automatically on a regular basis. The digital charts are patient-centered and other clinicians can add their entries to a shared file while maintaining their original data sets [10]. Major advantages of these digital files include shareability, retrievability, and storability. The main disadvantage of these cloud- or server-based files is that the files can be hacked [48]. Companies usually charge annual fees for storage and/or security for the files. And these fees can amount to significant expenses for orthodontic offices (Fig. 1.10).
3.1 Digital Photography
Digital photography became popular around the early 2000s [28]. The digital format allows clinicians to store and use images from multiple locations. Photographic software such as Photoshop™ (San Jose, California, USA) and DigitalSmileDesign™ (Madrid, Spain), if specifically designed for orthodontic purpose, can enhance the quality and edit these images. They allow for the digital photographs to be easily integrated into a digital data set [49]. Even though most of the commercially available software use 2D images, the digital rendering of these clinical photographs still offers significant advantages over their analog counterparts especially when combined with CBCT and intraoral dental scans [50]. Chapter 2 will cover in detail the role of photography as a contributing diagnostic tool when combined with intraoral scans and CBCT (Fig. 1.11).
3D photograph technology such as the one developed by 3DMD™ (Atlanta, Georgia, USA) uses a special setup consisting of two cameras placed at a strategic angle to each other to create a 3D image. They use complex algorithms capable of digitally reconstructing a patient’s facial features from 3D data captured from both cameras. This technology is more commonly used in research and not widely adopted in clinical orthodontics due to its high cost and fairly narrow range of application [51] (Fig. 1.12 and Table 1.1).
3.1.1 Cone Beam Radiography
As 2D radiography proved to have limited accuracy in depicting craniofacial structures, the development of a 3D radiographic imaging system became highly desirable in orthodontic diagnosis [52]. The cone beam computerized tomography (CBCT) was first introduced by Sir Godfrey N. Hounsfield in 1967. It was initially used for general medical imaging [53]. The first successful craniofacial cone beam machine was introduced in 1996 by QR s.r.l™ (NewTom 9000). The 3D rendering gives orthodontists an ability to visualize the craniofacial complex from different angles focusing on different structures (teeth, bone, and soft tissue) just by changing filters provided in a software. The tomography in different planes provides significantly more details in comparison to traditional 2D radiographs. A CBCT may replace the need for most other radiographic images commonly used in orthodontics including a panoramic x-ray, and a lateral cephalogram. Significant technological progress has decreased the amount of radiation and the exposure time required for obtaining a diagnostically valid CBCT, while the image quality has considerably increased. CBCT technology and its indications will be further discussed in subsequent chapters (Fig. 1.13).
Bone density can only be approximated as a Hounsfield scale which is not reliable in CBCT radiography [54]. A CBCT offers orthodontists the following advantages over a conventional 2D radiograph [55, 56].
-
1.
More accurate representation of the craniofacial structures.
-
2.
More precise radiographic data.
-
3.
Structures are visible in their exact positions with their exact shapes.
-
4.
No radiographic projection errors.
-
5.
No enlargement or distortion of structures.
-
6.
Ease of landmark identification.
-
7.
Superimposition with 3D facial photograph.
-
8.
Ability of accurately comparing several CBCTs of the same patient [57] (Figs. 1.14 and 1.15).
3.1.1.1 Reformatted Panoramic and Cephalometric Radiographs
CBCT software presents many useful functions for orthodontic diagnosis procedures including an ability to digitally reconstruct a panoramic (not totally containing all the informations that a traditional panoramic x-ray contains) and a cephalometric radiograph from a CBCT data set [58]. A central cut of the CBCT allows practitioners to precisely visualize the cranial base angle, an essential measurement in patients affected by craniofacial disorders, a measurement more difficult to obtain with a conventional cephalometric radiograph [59] (Fig. 1.16).
(a) A panoramic radiograph reconstructed from CBCT data. (b) A conventional 2D cephalometric radiograph showing superimposition of different craniofacial structures. (c) A 3D rendering of a CBCT illustrating the 3D relationship of craniofacial structures. (d) A mid-sagittal cut of a CBCT showing the cranial base clearly
3.1.1.2 3D Cephalometric Analysis
At the moment, 3D cephalometric analyses are not widely adopted in clinical orthodontics and orthognathic surgery as their advantages over the 2D analyses are not yet evident to the clinician [60, 61]. Artificial intelligence may have a potential to easily integrate the CBCT data into 3D cephalometric analyses using automatic voxel recognition [62]. This will allow 3D cephalometric analyses to become a routine part of an orthodontic diagnosis, and increase the accuracy of superimpositions. It will also provide invaluable assistance to clinicians to recognize and quantify craniofacial asymmetries as well as growth deficiencies [63] (Fig. 1.17 and Table 1.2).
3.1.2 Intraoral Scanner and Digital Model
Prior to the advent of intraoral scanners, digital dental models were made either by tabletop scanners or by a CT scan. A digital stereolithographic file (also known as Standard Tessellation Language or STL) was produced [64]. Cerec™ introduced the first intraoral scanner in the 1980s for restorative dentistry [65]. Itero™ followed with the introduction of full-arch intraoral scanners in the 1990s. Multiple intraoral scanners are now commercially available. All employ STL or PLY files to reproduce dental anatomy and related structures. The digital orthodontic models were shown to be as reliable as plaster casts in orthodontic diagnosis and treatment planning [66].
3.1.2.1 STL 3D Digital Orthodontic Models and Software Programs to Analyze the Dentition
3D digital orthodontic models have replaced plaster models in many orthodontic practices. Currently these digital models are stored as STL files. Importing these files into a software to analyze the dentition is the next step in the diagnostic process. These software programs provide a visualization of occlusal contacts, overjet, overbite, molar and canine relationships. One major advantage of an STL virtual model is its versatility. A single STL file can be used for record keeping, simulations, superimpositions, and comparisons of different treatment options [67]. The software also allows common orthodontic analyses such as tooth/arch size analysis, Bolton analysis, intercanine, and intermolar measurements to be performed with more efficiency and accuracy [68] (Fig. 1.18).
In an STL virtual file , the upper and lower digital models are individual “solid” entities. Segmentation of the dentition is required for treatment simulation or virtual orthodontic movements. The process of segmentation is carried out by a tooth recognition in some softwares artificial intelligence is used as an segmentation-assistant [69]. Following segmentation, each tooth becomes disconnected from the adjacent teeth and gingival base. It becomes movable in three planes of space [70]. These software programs create realistic and accurate movements of the dentition. They allow for orthodontic simulations and planning of tooth movements [71]. 3 Shape™ (Copenhagen, Denmark), Onyxceph™ (Chemnitz, Germany), Maestro™ (New Age, Piza, Italy), Suresmile™ (Orametrix,Richardson, USA), Deltaface (Limoges, France) and Align™ (San Jose, California, USA) are some of the commercially available software programs [72] (Fig. 1.19).
For clear aligners fabrication, orthodontists now have the ability to simulate an orthodontic treatment plan using a CAD software once the teeth are segmented [73]. The clinical crowns of teeth are moved by different algorithms into the desired position. The amount and direction of these movements are recorded in three planes of space [74]. However, an STL orthodontic model file does not contain data on root positioning. Therefore, the software calculates an approximate position of the roots. Once these orthodontic movements are accepted, the software will then analyze these movements, apply proprietary biomechanical manipulations to the movements prescribed, add interproximal reduction, attachments and other relevant auxiliaries. The sequence will then be divided into multiple stages and transferred to a CAM software for the fabrication of programmed STL files. The staging of aligners being established, the production of individualized aligners can be initiated [75, 76]. It is noteworthy that STL files allow for segmentation of dental arches and make treatment simulation possible but this is done without relating the dentition to surrounding craniofacial structures. These software do not have the capacity to accurately predict the biological response to conduct totally accurate tooth movement [77] (Figs. 1.20 and 1.21).
Currently, the most popular appliances produced by CAD/CAM technologies are clear aligners and programmed indirect bonding trays. Recently, CAD-CAM customized brackets have been introduced to take an advantage of this unique interaction between a treatment simulation and production of an individualized bracketing system [78]. Lingual orthodontics has adopted part of this system [79]. Robotically created archwires as advocated by Suresmile™ (Orametrix, Richardson, USA) is another example of a technology that employs an individualization of orthodontic treatment approach [80] (Fig. 1.22).
3.2 Integration of 3D Files: A Fusion of STL-DICOM
The ultimate goal of obtaining CBCT, intraoral scans, and digital photographs is to accurately reproduce a patient’s dentofacial morphology by accurate 3D orientation [81]. Software such as Anatomage(TM) (Santa Clara, USA) can now integrate a DICOM data set from CBCT with an STL file from an intraoral scan. The software may also incorporate 2D or 3D photographs to create a realistic and accurate virtual patient [82]. This combination of different files help to position the dentition in its exact spatial relationship with the surrounding craniofacial structures. This process is a significant improvement over a conventional set of fragmented 2D diagnostic records [83]. An addition of accurate root positioning data to the spatial positions of clinical crowns further enhances the predictability of clinical outcomes [42]. A new fully integrated 3D spatial relationship between an entire dentoalveolar complex and its surrounding craniofacial structures is obtained and can be reliably studied and evaluated. Eventually with artificial intelligence and the judicious use of big data, these simulation software will be able to reasonably predict how clinical crowns and roots can be moved in relation to their alveolar bone housing as well as predict clinical changes of their surrounding craniofacial structures [84] (Fig. 1.23).
At the moment, seamless STL-DICOM integration capability is not readily present in commercially available orthodontic simulation software. To circumvent this, several companies are offering new versions of their software with an ability to segment each tooth and root from a DICOM file and then reassemble them as an STL orthodontic model file. Figure 1.24. demonstrates an example of total integration of STL, CBCT, and DPP simulation software to move clinical crowns and roots at the same time [83] (Fig. 1.25).
4 Introduction of Data Mining, Artificial Intelligence, and Machine Learning
An integration of DICOM and STL files provides clinicians a potential to relate clinical crowns and roots of the dentition to their surrounding craniofacial structures in a static state. As all magnitude and direction of each orthodontic movement can be constantly recorded by the software, the next logical step is to input all these collected data into statistical models to improve our understandings of potential correlations that may exist between all diagnostic variables and the resulting movements [85]. This will allow orthodontists to correlate entirely measurable diagnostic findings, with treatment outcomes. These observations will enable clinicians to better recognize patterns that may have been overlooked with conventional 2D diagnostic process.
Zhao and colleagues stated “Physicians lack systematic methods for calibrating diagnostic decisions based on feedback from their outcomes” [86]. This statement also applies to orthodontics since most diagnostic decisions are unidirectional and based on subjective experience of treating orthodontists and treatment outcomes are not used as feedback mechanisms to improve future outcomes (Fig. 1.26).
The next frontier in digital diagnosis is to an introduction of orthodontic data mining. In the past decade, artificial intelligence (AI) and machine learning have revolutionized the use of data in medicine. “Artificial intelligence is a branch of computer science capable of analyzing complex medical data. Their potential to exploit meaningful relationship within a data set can be used in the diagnosis, treatment and predicting outcome in many clinical scenarios” [87]. This quote can be applied to the new 3D orthodontic diagnosis paradigm. AI uses deep learning and neural networks to predict the most probable treatment approach for a specific malocclusion. By creating layers of programming with many different and variables such as overbite, overjet, and crowding, and then assigning weight to each of these variables, AI can “learn” patterns of producing an exact diagnosis and formulating treatment options by studying very large quantity of malocclusions and their outcomes [88]. Contrary to a common misconception, machine learning needs a large amount of knowledge input and can only learn semi-repetitive and constructed patterns on its own. It lacks perception and intuition [89]. Therefore, AI requires the orthodontist’s knowledge and experience as crucial inputs into the machine learning process. AI allows orthodontists to test different probable treatment alternatives while using outcomes in a feedback mechanism to allow the construct of a deeper and more robust learning systems [90]. This new approach or back propagation which consists of constantly correcting the weights given to variables has the potential to vastly improve orthodontic treatment outcomes by allowing large amount of data to be gathered, processed, and analyzed [91]. For example, an integration of artificial intelligence (AI), and machine leaning with large amount of CBCT data may have a potential to better predict facial growth, and create a more focused treatment approach [92]. However, This process still relies on the vast knowledge and experience from orthodontists to be successful (Fig. 1.27).
(a) Conventional method to store 3D data in the cloud and design a treatment plan. (b) Neural network potentially used for orthodontic treatment assistance. Data is inputted into the deep learning neural network. Analyses are performed and a predicted outcome is proposed. The final outcome may be uploaded into the network to strengthen the predictions. The neural network also “learns” from the outcome of treatment and adjusts the weight of the parameters for a given malocclusion
5 Conclusions
In this chapter, a conventional diagnostic process employed in orthodontics was reviewed. The process only allows clinicians to diagnose malocclusions in a “feed forward” direction mostly driven by the operator’s experience and treatment philosophy. This approach often lacks scientific basis and has mainly led to differences of opinions promoting mechanistic rather than comprehensive approaches to treatment. The introduction of the 3D diagnosis has further expanded the diagnostic capabilities of orthodontists by incorporating CBCT and intraoral scans into their armamentarium. Current technologies allow for the addition of considerable diagnostic data acquisitions. However, the orthodontic diagnosis process has by and large remained unchanged despite these technological advances. An entirely new digital diagnosis paradigm with a total integration of all 3D diagnostic data and the use of AI-machine learning is slowly emerging. Neural networks and machine learning processes already used by several aligner companies have the potential to improve diagnostic accuracy and treatment planning capabilities of orthodontists. These advances will be achieved by feeding a large amount of diagnostic data into neural networks to formulate probabilities of outcomes based on successful treatment of a large number of malocclusions. In the end, orthodontists’ knowledge and experience remain very much crucial in this process. When combined with specially designed neural networks, this digitally driven statistically sound diagnostic approach will improve diagnostic and treatment planning capabilities for orthodontists (Fig. 1.28).
Describes a potential neural network developed for orthodontic diagnosis using some of the most common orthodontic variables (1 to n) shown on the far left side of the drawing. Then connectors are used and “weighted” according to the importance of variables on the severity of malocclusion. Nodes arranged in layers are used to mimic neural activity using activation functions. Finally, back propagation happens when the neural network “learns” to recognize patterns and adjusts the “weights” accordingly. These networks can process and correlate vast amount of data that may not appear evident to orthodontists. Probable outcomes are elaborated allowing orthodontists to make the most appropriate decision
References
Lestrel PE. Some approaches toward the mathematical modeling of the craniofacial complex. J Craniofac Genet Dev Biol. 1989;9:77–91.
Harrell WE Jr, Hatcher DC, Bolt RL. In search of anatomic truth: 3-dimensional digital modeling and the future of orthodontics. Am J Orthod Dentofac Orthop. 2002;122:325–30.
Miller AJ, Maki K, Hatcher DC. New diagnostic tools in orthodontics. Am J Orthod Dentofac Orthop. 2004;126:395–6.
Nebbe B, Major PW, Prasad NGN, Hatcher D. Quantitative assessment of temporomandibular joint disk status. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 1998;85:598–607.
Lessa FCR, Enoki C, Feres MFN, Valera FCP, Lima WTA, Matsumoto MAN. Breathing mode influence in craniofacial development. Braz J Otorhinolaryngol. 2005;71:156–60.
Kau CH, Olim S, Nguyen JT. The future of orthodontic diagnostic records. In: Seminars in orthodontics. Elsevier; 2011. p. 39–45.
Sarver DM. Interactions of hard tissues, soft tissues, and growth over time,v and their impact on orthodontic diagnosis and treatment planning. Am J Orthod Dentofac Orthop. 2015;148:380–6.
Broadbent BH. A new X-ray technique and its application to orthodontia: the introduction of cephalometric radiography. Angle Orthod. 1981;51:93–114.
Mehta J. Orthodontic records: why? What? When? & how? Funct Orthod. 1993;10:44–51.
Abdelkarim A, Jerrold L. Orthodontic chart documentation. Am J Orthod Dentofac Orthop. 2017;152:126–30.
Williamson, J. Orthodontic records: more than just models and photos. Int J Orthod Milwaukee. 2003;14(1):33
Broadbent, B. H. The Face of the Normal Child. The Angle Orthodontist. 1937;7(4):183–208
Bondemark L, Jeppsson M, Lindh-Ingildsen L, Rangne K. Incidental findings of pathology and abnormality in pretreatment orthodontic panoramic radiographs. Angle Orthod. 2006;76:98–102.
Graber TM. Panoramic radiography in orthodontic diagnosis. Am J Orthod. 1967;53:799–821.
DiFranco DE, Cham T-J, Rehg JM. Reconstruction of 3D figure motion from 2D correspondences. In: Proceedings of the 2001 IEEE Computer Society conference on computer vision and pattern recognition. CVPR 2001, I-I. IEEE; 2001.
Han UK, Vig KWL, Weintraub JA, Vig PS, Kowalski CJ. Consistency of orthodontic treatment decisions relative to diagnostic records. Am J Orthod Dentofac Orthop. 1991;100:212–9.
Lee K, Torkfar G, Fraser C. An investigation into orthodontic clinical record taking. Int J Orthod Milwaukee. 2015;26:53–7.
McNamara JA Jr. Ordinary orthodontics: starting with the end in mind. World J Orthod. 2000;1:45–54.
Ejersbo LR, Leron U. Revisiting the medical diagnosis problem: reconciling intuitive and analytical thinking. In: Probabilistic thinking. Springer; 2014.
Harrell Jr WE. 3D diagnosis and treatment planning in orthodontics. In: Seminars in orthodontics. Elsevier; 2009. p. 35–41.
Hechler SL. Cone-beam CT: applications in orthodontics. Dent Clin N Am. 2008;52:809–23, vii.
Beuer F, Schweiger J, Edelhoff D. Digital dentistry: an overview of recent developments for CAD/CAM generated restorations. Br Dent J. 2008;204:505.
Hou D, Capote R, Bayirli B, Chan DCN, Huang G. The effect of digital diagnostic setups on orthodontic treatment planning. Am J Orthod Dentofac Orthop. 2020;157:542–9.
Palomo JM, El H, Stefanovic N, Bazina M. Diagnostic value of 3D imaging in clinical orthodontics. In: Craniofacial 3D imaging. Springer; 2019.
Murata S, Lee C, Tanikawa C, Date S. Towards a fully automated diagnostic system for orthodontic treatment in dentistry. In: 2017 IEEE 13th international conference on e-science (e-Science). IEEE; 2017. p. 1–8.
Terry DA, Snow SR, McLaren EA. CE 1-contemporary dental photography: selection and application. Compendium. 2008;29:432.
Claman L, Patton D, Rashid R. Standardized portrait photography for dental patients. Am J Orthod Dentofac Orthop. 1990;98:197–205.
Bengel W. Digital photography in the dental practice—an overview (II). Int J Comput Dent. 2000;3:121–32.
Pickens D. et al. Focal-plane tomography image reconstruction. IEEE Transactions on Nuclear Science. 1980;27(1):489–492
Maestre-Ferrín L, Carrillo-García C, Galán-Gil S, Peñarrocha-Diago M, Peñarrocha-Diago M. Prevalence, location, and size of maxillary sinus septa: panoramic radiograph versus computed tomography scan. J Oral Maxillofac Surg. 2011;69:507–11.
Tsolakis AI, Kalavritinos M, Bitsanis E, Sanoudos M, Benetou V, Alexiou K, Tsiklakis K. Reliability of different radiographic methods for the localization of displaced maxillary canines. Am J Orthod Dentofac Orthop. 2018;153:308–14.
Vandenberghe B, Jacobs R, Bosmans H. Modern dental imaging: a review of the current technology and clinical applications in dental practice. Eur Radiol. 2010;20:2637–55.
Steiner CC. Cephalometrics for you and me. Am J Orthod Dentofac Orthop. 1953;39:729–55.
Scheideman GB, Bell WH, Legan HL, Finn RA, Reisch JS. Cephalometric analysis of dentofacial normals. Am J Orthod. 1980;78:404–20.
Ludlow JB, Gubler M, Cevidanes L, Mol A. Precision of cephalometric landmark identification: cone-beam computed tomography vs conventional cephalometric views. Am J Orthod Dentofac Orthop. 2009;136:312.e1–12.e10.
Ricketts RM, Grummons D. Frontal cephalometrics: practical applications, part I. World J Orthod. 2003;4:297–316.
Proskauer C. The story of dentistry, from the dawn of civilization to the present, 2nd ed. In: JSTOR; 1951.
Yamamoto K, Hayashi S, Nishikawa H, Nakamura S, Mikami T. Measurements of dental cast profile and three-dimensional tooth movement during orthodontic treatment. IEEE Trans Biomed Eng. 1991;38:360–5.
Ackerman M. B. The myth of Janus: Orthodontic progress faces orthodontic history. American Journal of Orthodontics and Dentofacial Orthopedics. 2003;123(6):594–596.
Beglin FM, Firestone AR, Vig KWL, Beck FM, Kuthy RA, Wade D. A comparison of the reliability and validity of 3 occlusal indexes of orthodontic treatment need. Am J Orthod Dentofac Orthop. 2001;120:240–6.
Dolce C, Mansour DA, McGorray SP, Wheeler TT. Intrarater agreement about the etiology of Class II malocclusion and treatment approach. Am J Orthod Dentofac Orthop. 2012;141:17–23.
Paredes V, Gandia JL, Cibrian R. Digital diagnosis records in orthodontics. An overview. Med Oral Patol Oral Cir Bucal. 2006;11:E88–93.
Xiao Z, Liu Z, Gu Y. Integration of digital maxillary dental casts with 3D facial images in orthodontic patients: a three-dimensional validation study. Angle Orthod. 2020;90(3):397–404.
Takada K. Artificial intelligence expert systems with neural network machine learning may assist decision-making for extractions in orthodontic treatment planning. J Evid Based Dent Pract. 2016;16:190–2.
Yagi M, Ohno H, Takada K. Decision-making system for orthodontic treatment planning based on direct implementation of expertise knowledge. In: 2010 annual international conference of the IEEE engineering in medicine and biology, IEEE; 2010, p. 2894–97.
Motohashi N, Kuroda T. A 3D computer-aided design system applied to diagnosis and treatment planning in orthodontics and orthognathic surgery. Eur J Orthod. 1999;21:263–74.
Hennessy J, Al-Awadhi EA. Clear aligners generations and orthodontic tooth movement. J Orthod. 2016;43:68–76.
Eve E. Personalizing orthodontics–precision health methods in orthodontic clinical trials. UCSF; 2018.
Schnipper JL, Linder JA, Palchuk MB, Einbinder JS, Li Q, Postilnik A, Middleton B. “Smart forms” in an electronic medical record: documentation-based clinical decision support to improve disease management. J Am Med Inform Assoc. 2008;15:513–23.
Schabel BJ, Franchi L, Baccetti T, McNamara JA Jr. Subjective vs objective evaluations of smile esthetics. Am J Orthod Dentofac Orthop. 2009;135:S72–9.
Schaaf H, Malik CY, Howaldt H-P, Streckbein P. Evolution of photography in maxillofacial surgery: from analog to 3D photography—an overview. Clin Cosmet Investig Dent. 2009;1:39.
Metzger TE, Kula KS, Eckert GJ, Ghoneima AA. Orthodontic soft-tissue parameters: a comparison of cone-beam computed tomography and the 3dMD imaging system. Am J Orthod Dentofac Orthop. 2013;144:672–81.
Anderson PJ, Yong R, Surman TL, Rajion ZA, Ranjitkar S. Application of three-dimensional computed tomography in craniofacial clinical practice and research. Aust Dent J. 2014;59:174–85.
Sukovic P. Cone beam computed tomography in craniofacial imaging. Orthod Craniofac Res. 2003;6:31–6.
Kapila SD. Cone beam computed tomography in orthodontics: indications, insights, and innovations. Ames: Wiley; 2014.
Tadinada A, Schneider S, Yadav S. Role of cone beam computed tomography in contemporary orthodontics. In: Seminars in orthodontics. Elsevier; 2018. p. 407–15.
Van Vlijmen OJC, Maal T, Bergé SJ, Bronkhorst EM, Katsaros C, Kuijpers-Jagtman AM. A comparison between 2D and 3D cephalometry on CBCT scans of human skulls. Int J Oral Maxillofac Surg. 2010;39:156–60.
Bazina M, Cevidanes L, Ruellas A, Valiathan M, Quereshy F, Syed A, Wu R, Palomo JM. Precision and reliability of Dolphin 3-dimensional voxel-based superimposition. Am J Orthod Dentofac Orthop. 2018;153:599–606.
Lund H, Grondahl K, Grondahl HG. Accuracy and precision of linear measurements in cone beam computed tomography Accuitomo® tomograms obtained with different reconstruction techniques. Dentomaxillofac Radiol. 2009;38:379–86.
Cevidanes LHC, Motta A, Proffit WR, Ackerman JL, Styner M. Cranial base superimposition for 3-dimensional evaluation of soft-tissue changes. Am J Orthod Dentofac Orthop. 2010;137:S120–S29.
Chen M-H, Chang JZ-C, Kok S-H, Chen Y-J, Huang Y-D, Cheng K-Y, Lin C-P. Intraobserver reliability of landmark identification in cone-beam computed tomography-synthesized two-dimensional cephalograms versus conventional cephalometric radiography: a preliminary study. J Dent Sci. 2014;9:56–62.
Cheung LK, Chan YM, Jayaratne YSN, Lo J. Three-dimensional cephalometric norms of Chinese adults in Hong Kong with balanced facial profile. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2011;112:e56–73.
Nada RM, Maal TJJ, Breuning KH, Berge SJ, Mostafa YA, Kuijpers-Jagtman AM. Accuracy and reproducibility of voxel based superimposition of cone beam computed tomography models on the anterior cranial base and the zygomatic arches. PLoS One. 2011;6(2):e16520.
Cevidanes LHS, Bailey LJ, Tucker GR Jr, Styner MA, Mol A, Phillips CL, Proffit WR, Turvey T. Superimposition of 3D cone-beam CT models of orthognathic surgery patients. Dentomaxillofac Radiol. 2014;34(6):369–75.
Fasbinder DJ. Computerized technology for restorative dentistry. Am J Dent. 2013;26:115–20.
Kassis C. CAD/CAM technology: a review. Comput Aided Des (CAD). 1980;2.
Luu NS, Nikolcheva LG, Retrouvey J-M, Flores-Mir C, El-Bialy T, Carey JP, Major PW. Linear measurements using virtual study models: a systematic review. Angle Orthod. 2012;82:1098–106.
Sinthanayothin C, Tharanont W. Orthodontics treatment simulation by teeth segmentation and setup. In: 2008 5th international conference on electrical engineering/electronics, computer, telecommunications and information technology. IEEE; 2008. p. 81–4.
Fleming PS, Marinho V, Johal A. Orthodontic measurements on digital study models compared with plaster models: a systematic review. Orthod Craniofac Res. 2011;14:1–16.
Kumar Y, Janardan R, Larson B, Moon J. Improved segmentation of teeth in dental models. Comput Aided Des Appl. 2011;8:211–24.
Yaqi M, Zhongke L. Computer aided orthodontics treatment by virtual segmentation and adjustment. In: 2010 international conference on image analysis and signal processing. IEEE; 2010. p. 336–9.
Cheng C, Cheng X, Dai N, Liu Y, Fan Q, Hou Y, Jiang X. Personalized orthodontic accurate tooth arrangement system with complete teeth model. J Med Syst. 2015;39:84.
Kondo T, Ong SH, Foong KW. Tooth segmentation of dental study models using range images. IEEE Trans Med Imaging. 2004;23:350–62.
Breuning KH, Kau CH. Digital planning and custom orthodontic treatment. Hoboken: Wiley; 2017.
Dickerson TE. Invisalign with photobiomodulation: optimizing tooth movement and treatment efficacy with a novel self-assessment algorithm. J Clin Orthod. 2017;51:157–65.
Miller RJ, Kuo E, Choi W. Validation of Align Technology’s Treat IIITM digital model superimposition tool and its case application. Orthod Craniofac Res. 2003;6:143–9.
Robertson L, Kaur H, Fagundes NCF, Romanyk D, Major P, Mir CF. Effectiveness of clear aligner therapy for orthodontic treatment: a systematic review. Orthod Craniofac Res. 2020;23(2):133–42.
Jones ML, Hickman J, Middleton J, Knox J, Volp C. A validated finite element method study of orthodontic tooth movement in the human subject. J Orthod. 2001;28:29–38.
Tarraf NE, Ali DM. Present and the future of digital orthodontics✩. In: Seminars in orthodontics. Elsevier; 2018. p. 376–85.
Kwon S-Y, Kim Y, Ahn H-W, Kim K-B, Chung K-R. Computer-aided designing and manufacturing of lingual fixed orthodontic appliance using 2D/3D registration software and rapid prototyping. Int J Dent. 2014;2014(11):164164.
Sachdeva RCL. SureSmile technology in a patient-centered orthodontic practice. J Clin Orthod. 2001;35:245–53.
Widmann G, Berggren JPM, Fischer B, Pichler-Dennhardt AR, Schullian P, Bale R, Puelacher W. Accuracy of image-fusion stereolithographic guides: mapping CT data with three-dimensional optical surface scanning. Clin Implant Dent Relat Res. 2015;17:e736–e44.
Plooij JM, Maal TJJ, Haers P, Borstlap WA, Kuijpers-Jagtman AM, Bergé SJ. Digital three-dimensional image fusion processes for planning and evaluating orthodontics and orthognathic surgery. A systematic review. Int J Oral Maxillofac Surg. 2011;40:341–52.
Joda T, Wolfart S, Reich S, Zitzmann NU. Virtual dental patient: how long until it’s here? Curr Oral Health Rep. 2018;5:116–20.
Chisari JR, McGorray SP, Nair M, Wheeler TT. Variables affecting orthodontic tooth movement with clear aligners. Am J Orthod Dentofac Orthop. 2014;145:S82–91.
Kunz F, Stellzig-Eisenhauer A, Zeman F, Boldt J. Artificial intelligence in orthodontics. J Orofac Orthop/Fortschritte der Kieferorthopädie. 2020;81:52–68.
Zhao JY, Song EAB, Schwartz D, Panesar M, Jackson GP, Elkin PL. Barriers, facilitators, and solutions to optimal patient portal and personal health record use: a systematic review of the literature. In: AMIA annual symposium proceedings, 1913. American Medical Informatics Association; 2017.
Ramesh AN, Kambhampati C, Monson JRT, Drew PJ. Artificial intelligence in medicine. Ann R Coll Surg Engl. 2004;86:334.
Kulikowski CA. Artificial intelligence methods and systems for medical consultation. IEEE Trans Pattern Anal Mach Intell. 1980;PAMI-2:464–76.
Ko C-C, Tanikawa C, Wu T-H, Pastewait M, Jackson CB, Kwon JJ, Lee Y-T, Lian C, Wang L, Shen D. Machine learning in orthodontics: application review. Embracing Novel Technol Dent Orthod. 2019;1001:117.
Martina R, Teti R, D’Addona D, Iodice G. Neural network based system for decision making support in orthodontic extractions. In: Intelligent production machines and systems. Elsevier; 2006.
Jung S-K, Kim T-W. New approach for the diagnosis of extractions with neural network machine learning. Am J Orthod Dentofac Orthop. 2016;149:127–33.
Faber J, et al. Artificial intelligence in orthodontics. APOS Trends in Orthodontics. 2019;9(4):201–205.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Retrouvey, JM., Panayi, N., Tsolakis, A. (2021). Evolution of the Orthodontic Diagnosis in the Age of Artificial Intelligence. In: Retrouvey, JM., Abdallah, MN. (eds) 3D Diagnosis and Treatment Planning in Orthodontics. Springer, Cham. https://doi.org/10.1007/978-3-030-57223-5_1
Download citation
DOI: https://doi.org/10.1007/978-3-030-57223-5_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-57222-8
Online ISBN: 978-3-030-57223-5
eBook Packages: MedicineMedicine (R0)