Abstract
With the advent of newer digital technology-driven tools to aid in the treatment of orthodontic patients, many techniques have been developed for early orthodontic treatment. Some of these procedures will be demonstrated here including treatment planning, monitoring of the developing child, diagnostic aids, design and fabrication of active appliances, and retention.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
2.1 Introduction
The use of digital technology has had great impact on our lives. Its influence in the management of an orthodontic patient is no different.
The chapter has been divided into three sections:
-
1.
The digital workflow in an orthodontic office.
-
2.
Clinical indications and applications for early orthodontic treatment aided with digital technology.
-
3.
Concluding remarks including a discussion on the pitfalls and an overreliance of digital technology.
The following are certain definitions of terms to be used in this chapter which may be helpful:
-
Digital technology – this is an all-encompassing term used nowadays. But its roots lie in the fact that such technology is able to convert information into numbers (a binary format of zero and one) for machines to assimilate and use this information (Fig. 2.1).
-
Artificial Intelligence (AI) – this uses algorithms and digitized patterns to mimic the cognitive function of the human mind to “learn” and “solve problems” (Fig. 2.2).
-
CAD-CAM (computer-aided design-computer-aided manufacturing) – introduced to dentistry in the 1970s, the use of CAD-CAM in orthodontics has exponentially increased in the last 20 years with changes in treatment philosophies and modalities. For example, the use of appliances from 3-D printed models. Figure 2.3 illustrates such an example.
2.2 The Digital Workflow in an Orthodontic Clinic
Emerging technology has improved the digital workflow, resulting in increased patient engagement, time efficiency, and better data acquisition, within the orthodontic office (Christensen 2017) (Fig. 2.4).
Logs of staff, patients, and visitors are kept in a central computer (Fig. 2.5) to monitor attendance and body temperature (a new requirement at our office, ever since the COVID-19 pandemic).
Digital records and attendance keep a log of patient’s information and treatment progress. Patients’ attendance (including time in and out) is an important tool nowadays as well.
Having the ability to view patient records remotely gives flexibility (Fig. 2.6).
Digital data acquisition has enabled efficient means of accessing information. Radiographs and CBCTs can be remotely accessed (Fig. 2.7).
Digital scanners, both intraorally and extraorally, are convenient and a clinically acceptable way for record-keeping and transmitting information. Cloud-based information can be accessed easily and saves on physical storage space (Fig. 2.8).
Digital scans and subsequent simulations, when properly executed, can be used to engage patients, manage expectations, and aid in treatment planning. An example of such a simulation is shown in Fig. 2.9.
Radiograph algorithms can be used to predict certain conditions (Hunter 1966). An example of this is the study of determining the growth and development of an individual using the stages of the cervical vertebra (Bacetti et al. 2002) (Fig. 2.10).
Cervical vertebra stage determination in order to predict growth. For instance, in these two cases of skeletal class III patients both aged 12 but with very different skeletal maturity. Researchers are looking at algorithms (Kok et al. 2019), with the aid of landmarks, to help determine this
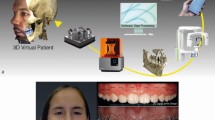
The integration of scans can be used to give a more predictive treatment outcome. Surgical cases especially benefit from such outcomes. An example of this is shown in Fig. 2.11.
Monitoring the progress of cases will increase in demand. The use of phone apps along with highly innovative phone cameras enable orthodontists to monitor their patients remotely (Fig. 2.12). In view of the COVID-19 pandemic, the demand for tele-dentistry and distance diagnosis has become a need more than a luxury (Barenghi et al. 2020). Apps can be used to monitor patient compliance, progress, and oral conditions and hygiene.
Monitoring the progress of patients has become more urgent (Hansa et al. 2020). Actual pictures taken during the COVID-19 pandemic enquiring about dental infection and orthodontic progress
Transfer portals and storage of data are important in today’s digital setting. Cloud-based portals enable safer storage and management of data as well as good accessibility of such data. Storage and transfer of such data is far more hygienic as well. These scans can also be transferred via such portals to laboratories and coworkers reducing physical material handling and improving infection control (Figs. 2.13 and 2.14).
2.3 Clinical Indications and Application for Early Orthodontic Treatment-Aided Digital Technology
Intraoral scanning has made many processes much easier and safer (Chalmers et al. 2016) than impression materials including applications beyond the original scope of the device use such as scanning infants and young patients (Fig. 2.15).
Easily acceptable scans rid the patient of the discomfort of impression materials (Chaudhari & Kharbanda 2017) and overcome the problems of mobile teeth. (a) Cleft case, picture courtesy of Professor Dhirawat Jotikasthira. (b) The second example shows a patient in the mixed dentition with highly mobile first and second primary molars that were removed and a digital study model taken immediately. An alginate impression for both cases would have been very uncomfortable and difficult to undertake
Removable appliances—design and production have benefited greatly from digital technology (Fig. 2.16). Dedicated laboratory software has enabled in-house and lab-based manufacture of simple to custom-made appliances with a faster turnaround time.
Fixed appliances—prescription brackets and wires along with jig placement could change the way we manage our fixed appliance cases (Fig. 2.17).
Customized appliance fabrication can result in personalized tailor-fitted appliances. Force delivery and application can be more precise (Fig. 2.18).
Customized appliance for expansion. Made with the aid of digital technology (Graf 2017). Picture courtesy of Dr. Nikhilesh Vaid
Functional appliances—the augmentation of clear aligners to include mandibular advancement components (Giancotti et al. 2020) is a very interesting avenue to be explored (Fig. 2.19).
Clear aligners have been one of the two technologies (the other being temporary anchorage devices) in orthodontics that have revolutionized the way we approach the management of our patients (Fig. 2.20).
The integration from records to treatment execution has improved by leaps and bounds with regard to the application in clear aligners (Keim 2018). Algorithms have also been refined and data bases increased to present a more predictable treatment option. An example below using Invisalign
Retainers have been another avenue where digital technology can improve. More accurate retainers and shorter manufacturing time would greatly improve retention protocols (Fig. 2.21 and 2.22).
Fixed retainers using digital technology. Memotain by Ormco is a CAD-CAM retainer made by precision cuts of nickel-titanium alloy (Kravitz et al. 2017) to fit exactly into the anatomy of the teeth
2.4 Pitfalls and Overreliance of Digital Technology
I carefully worded the title of this chapter as an aid to orthodontic management. Such technology, though extremely helpful, cannot replace the clinician (see Fig. 2.23).
When dealing with patients, health-care workers have long since recognized that human communication and compassion play a key role in the management of the disease. The dead pan responses of technology cannot replicate this (Dunbar et al. 2014).
Detection and the implication of systemic and oral diseases also require a dental surgeon’s input.
AI, although extremely good at helping to determine an ideal method in obtaining tooth movement, is unable, as yet, to integrate facial forms and bony anatomy completely. Patients also exhibit differing permutations of malocclusion and respond differently to similar treatment modalities. Fine tuning and tailor-made plans are inevitable. Patients’ needs and mental makeup also determine an appropriate treatment plan and goal (Faber et al 2019). Algorithms, as yet, cannot accomplish these requirements.
Finally, one must always be aware that the medicolegal implications of using such technology do not absolve the user from responsibilities.
References
Baccetti T, Franchi L, McNamara JA. An improved version of the cervical vertebral maturation (CVM) method for the assessment of mandibular growth. Angle Orthod. 2002;72(4):316–23.
Barenghi L, Barenghi A, Cadeo C, Di Blasio A. Innovation by computer-aided design/computer-aided manufacturing technology: a look at infection prevention in dental settings. Biomed Res Int. 2020;2019:6092018.
Chalmers EV, McIntyre GT, Wang W, Gillgrass T, Martin CB, Mossey PA. Intraoral 3D scanning or dental impressions for the assessment of dental arch relationships in cleft care. Which is superior? Cleft Palate Craniofac J. 2016;53(5):568–77.
Chaudhari PK, Kharbanda OP. Intraoral 3D scanning in cleft care. Cleft Palate Craniofac J. 2017;54(5):618.
Christensen LR. Digital workflows in contemporary orthodontics. APOS Trends Orthod. 2017;7:12–8.
Dunbar AC, Bearn D, McIntyer G. The influence of using digital diagnostic information on orthodontic treatment planning—a pilot study. J Healthc Eng. 2014;5(4):411–27.
Faber J, Faber C, Faber P. Artificial intelligence in orthodontics. APOS Trends Orthod. 2019;9(4):201–5.
Giancotti A, Cozza P, Mampieri G. Aligners and mandibular advancement: a comprehensive option for phase I treatment of class II, division 1 cases. J Clin Orthod. 2020;54(9):513–24.
Graf S. Direct printed metal devices—the next level of computer-aided design and computer-aided manufacturing applications in the orthodontic care. APOS Trends Orthod. 2017;7:253–9.
Hansa I, Semaan SJ, Vaid NR. Clinical outcomes and patient perspectives of dental monitoring GoLive with Invisalign—a retrospective cohort study. Prog Orthod. 2020;21:16.
Hunter CJ. The correlation of facial growth with body height and skeletal maturation at adolescence. Angle Orthod. 1966;36(1):44–54.
Keim RG. New possibilities for aligners. J Clin Orthod. 2018;52(4):195–6.
Kok H, Acilar AM, Izgi MS. Usage and comparison of artificial intelligence algorithms for determination of growth and development by cervical vertebrae stages in orthodontics. Prog Orthod. 2019;20:41.
Kravitz ND, Grauer D, Schumacher P, Jo Y. Memotain: a CAD/CAM nickel-titanium lingual retainer. AJODO. 2017;151:812–5.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Lee, B. (2022). Digital Technology as an Aid to Early Orthodontic Treatment. In: Harfin, J., Satravaha, S., Lapatki, B.G. (eds) Clinical Cases in Early Orthodontic Treatment . Springer, Cham. https://doi.org/10.1007/978-3-030-95014-9_2
Download citation
DOI: https://doi.org/10.1007/978-3-030-95014-9_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-95013-2
Online ISBN: 978-3-030-95014-9
eBook Packages: MedicineMedicine (R0)