Abstract
Tissue-engineered skin substitutes have proven to be effective in acute and chronic wound management and cell transplantation may be performed by punch minigrafting, split-thickness skin grafting, hair follicle transplantation, suction blisters, epidermal curettage techniques, cultured and non-cultured autologous keratinocytes. The previous surgical and cultured techniques can be time-consuming and in some cases esthetically unsatisfying or painful for the patients. Recently new non-cultured autologous epidermal and dermal products have been developed with similar results to the cultured dermoepidermal techniques, but are simpler, less expensive, and less time-consuming.
The use of tissue-engineered advanced therapies may improve the quality of life, have cost benefits and accelerate healing of complex wounds. Follow-up studies and randomized clinical trials with a standard measure are needed to confirm the efficacy of those therapies but the current results have proved to be very promising.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Normal skin regenerates epidermis injury by stem cells present in basal layer of epidermis [1]. In case of severe deep injury, self-renewal ability is limited and a surgical intervention is needed. Split-thickness grafts are the standard permanent surgical treatment in case of deep wounds or burns; however, skin grafts can be utilized only in small areas of damaged skin. Autografts can be associated with surgical complications such as infections, scarring, and poor esthetic outcomes [2]. In large skin injuries, allografts are a suitable option but can be rejected due to the graft immunogenicity [3].
Skin substitutes were introduced as an effective therapy to reduce skin grafts complications. Bioengineered skin substitutes are advanced medical devices, developed by a cooperation of a multidisciplinary scientists and physician teams [4]. Tissue engineering was described firstly in 1993 and genetically modified substitutes were introduced in 2005 [5, 6]. The aim for appropriate skin substitute is to heal or regenerate the wound maintaining the function and structure of normal skin. Skin equivalents should meet some essential criteria: protective function, promoting biological reactions, cost-effectiveness, minimizing adverse events like toxicity and immunogenicity. The skin equivalents structure should be biodegradable, biocompatible, durable, malleable, flexible and provide an ideal environment for cell proliferation, differentiation, migration, and neovascularization [7, 8].
2 Classifications
Tissue-engineered skin substitutes can be classified using the biomaterial type, the scaffold architecture, the content of cells and growth factors, and the substitute anatomical structure [9].
2.1 Biomaterial Type and Scaffold Architecture
The biomaterial type can be biological (autologous, allogeneic, or xenogeneic) or synthetic (biodegradable or non-biodegradable). In biological biomaterial, the transmission risk of infectious diseases should be evaluated.
Scaffolds are extracellular matrix analogs with a tridimensional structure. The composition includes natural, synthetic, or composite (the combination of natural and synthetic) biomaterials. The scaffolds contribute to cell adhesion, proliferation, differentiation, and neovascularization [9]. Collagen, gelatin, elastin, hyaluronic acid, chitosan, fibronectin, fibrin, pullulan, alginate, and laminin are the most commonly biocompatible materials utilized as natural scaffolds in skin tissue engineering. Hydrocarbons are the components of synthetic biomaterials including polyhydroxyortho esters (POE), polylactic acid (PLA), polylactic-co-glycolic acid (PLGA), polyethylene glycol (PEG), poly-e-caprolactone (PCL), poly-b-hydroxybutyrate (PHB), poly vinyl alcohol (PVA), and polyurethane (PU). Ideal tissue-engineered skin scaffold should mimic the structure and function of the skin. The combination of biocompatible natural structures and mechanical resistance of synthetic polymers shows the most efficient properties [10]. Some example of composite scaffolds characterized by a wide variety of materials are PLLA–collagen, poly ethylene oxide–chitosan, carboxyethyl chitosan/PVA, chitosan/collagen/PEO, and PCL–collagen [11].
Scaffolds should have a solid 3D structure and an appropriate pore size. 100 μm pores are ideal to support cell migration and transportation. Pores larger than 300 μm can increase capillary formation and angiogenesis [12].
2.2 Growth Factors
Growth factors are necessary to create functionally advanced skin substitutes.
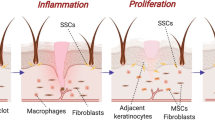
Growth factors like epidermal growth factor (EGF), fibroblast growth factor (FGF), transforming growth factor TGF-α/TGFβ, vascular endothelial growth factor (VEGF), platelet-derived growth factor (PDGF), interleukin-1 (IL-1), interleukin-6 (IL-6), and interleukin-8 (IL-8) stimulate healing processes, cell migration and proliferation, neovascularization and reduce fibrosis and scars formation [9].
2.3 Cells
Different cell types are involved in the skin normal function such as keratinocytes, melanocytes, fibroblasts, endothelial cells, Langerhans cells, Merkel cells, and adipocytes that produce ECM and a variety of growth factors [13].
Fibroblasts are the most important cells of the dermis involved in a variety of functions: collagen and fibronectin formation, release of angiogenic agents, and stimulation of endothelial cells [14]. Papillary fibroblasts control keratinocyte migration and proliferation with keratinocyte growth factor (KGF) [15].
Keratinocytes are the main cells in skin epidermal layer that have principal roles in epithelialization process and they secrete pro-angiogenic growth factors VEGF and PDGF [16].
Melanocytes are located in the basal layer of the epidermis and are necessary for skin pigmentation in normal skin and to avoid hypopigmentation in skin equivalents [17].
Macrophages remove damaged matrix, release growth factors and cytokines, promote angiogenesis [18] but can cause hypertrophic scarring also in skin substitutes [19].
Langerhans cells are located in epidermis layers and are involved in processing and presenting antigens to T lymphocyte of immune system. In skin substitutes, they control skin immune response and immune rejection.
Endothelial cells are the most important cells of blood and lymphatic vessels. Using these cells in 3D scaffold can accelerate blood capillary formation and lymphatic drainage [20].
2.4 Cellular and Acellular Skin Substitutes
Skin substitutes can be divided in two distinct groups including either synthetic acellular materials or natural with different cell types and can be utilized as temporary or permanent wound dressing [21].
Acellular substitutes are used as protections and temporary coverage against environmental contamination and fluid loss and they can include dermal matrix components, cytokines, and growth factors to promote wound healing [22]. Acellular substitutes include a nylon mesh or collagen as dermis and silicon membrane as epidermis. The cellular substitutes are composed of one or two layers of scaffold (mesh or 3D matrix), with autologous or allogeneic cells. The majority of skin substitutes contain only fibroblasts and keratinocytes. Warm/hot sensation, immune regulation, pressure sensation, and pigmentation are altered due to the absence of immune cells, melanocytes, and nerve cells.
Cellular skin substitutes stimulate the healing process with complete restoration of damaged tissue and reduce the graft rejection [23, 24].
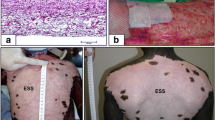
Two main types of cellular autologous skin substitutes are available: cultured epithelial autograft (CEA) and cultured skin substitutes (CSS) [8]. Biomaterial can be natural (collagen, chitosan, HA) and synthetic (PEG, PLA, PLGA and their combinations) [25]. CEAs are cultured autologous keratinocytes obtained from patient’s skin biopsy or from cadaveric skin [26]. Epidermis is separated from dermis and then keratinocytes are enzymatically isolated and cultured in vitro [27]. Possible complications are scar formation, contraction, and hyperkeratosis and incomplete healing of deeper wounds. Autologous keratinocytes suspension can be directly sprayed on the wound injury [28]. CSS is an autologous bilayered skin substitute suitable for permanent wound coverage but is time-consuming and expensive [8].
2.5 Anatomical Structure of Substitutes
The structure of the substitutes is similar to the anatomy of the skin, which is composed by three layers: avascular epidermis, vascularized dermis, and hypodermis [29]. The skin substitute can serve as a replacement for epidermal, dermal, or composite bilayer dermoepidermal tissues [13]. Epidermal substitutes are utilized in superficial wounds and second degree burns. The possible limitations are the high costs, fragility, long preparation, and poor esthetic outcomes [23, 30].
Dermal substitutes can be cellular or acellular and have allogeneic, xenogeneic, or synthetic origin [21]. The first step of a dermal substitute is to provide a dermis-like structure that is replaced by fibroblasts, endothelial cells, and inflammatory cells. The scaffolds are engineered to support cell growth, migration, revascularization, and neodermis formation. Neodermis (new cells and vascularization) is formed in 3 to 4 weeks after grafting [31]. Secondly the substitute can be covered by skin grafts or different tissue-engineered skin substitutes [20]. Dermal substitutes are not always cost-effective procedure and can be associated with pain and complications [32]. Dermoepidermal (composite) substitutes were manufactured since 1990 by association of epidermal and dermal layers and are indicated for full thickness wounds [33]. An ideal dermoepidermal skin substitute provides a suitable skin barrier and is non-immunogenic. The bilayered skin analogs contain autologous or allogeneic keratinocytes and fibroblasts seeded on 3D scaffolds and are indicated for temporary use [34]. Autologous cells are obtained from skin biopsy after 4 weeks of cultivation and insert to collagen-GAG based structure [35]. The possible complications are poor elasticity, graft contraction, and alteration of pigmentation [13].
3 Commercially Available Skin Substitutes
3.1 Epidermal Substitutes
BioSeed-S® is autologous keratinocytes re-suspended in an allogeneic fibrin sealant [21].
CellSpray is a suspension of non-cultured autologous keratinocytes [27].
EpiDex is a CEA composed by autologous keratinocytes derived from hair follicles and silicone membranes [13].
Epicel® is composed by autologous keratinocyte sheets attached and petrolatum gauze support. It was the first CEA autologous skin substitute to become commercially available [36]. 3 to 4 cm2 of donor skin are expanded to 5000- to 10,000-folds in 3–4 weeks. The petrolatum gauze support is removed one week after Epicel transplantation [37].
MySkin™ is composed by autologous keratinocytes with a synthetic silicone layer [27].
3.2 Dermal Substitutes
Alloderm® is an acellular poor immunogenic cadaveric dermal substitute, composed of a collagen scaffold. The scaffold allows the migration of fibroblasts and endothelial cells and can be covered by thin grafts [38].
Biobrane® is an acellular synthetic bilayer skin substitute composed of dermal layer of porcine collagen type I around a 3D nylon filament and an epidermal layer of thin semipermeable silicone film. Biobrane® is utilized as temporary coverage in pediatric and adult wounds [39].
Dermagraft™ is a monolayer allogenic dermal equivalent formed by culturing human fibroblasts in polyglactin mesh scaffold. The fibroblasts produce dermal matrix proteins, collagen, growth factors, and cytokines. The indications are chronic wounds and in particular diabetic foot ulcers [27].
GraftJacket is a cellular cryopreserved allogenic dermal collagen [40].
Integra™ is an acellular non-immunogenic dermal substitute contained a dermal layer of porous crosslinked bovine collagen and chondroitin-6-sulfate GAG and an epidermal layer of synthetic silicone polymer. The silicon layer provides a temporary coverage of the wound and can be covered secondly by a thin autograft. The dermal scaffold allows the migration of dermal cells such as fibroblasts and other cells that synthesize endogenous matrix components [41, 42].
Matriderm® is an acellular bovine collagen type I matrix and α-elastin hydrolysate lyophilized dermis [39].
TransCyte is a porcine dermal type I collagen coated with bio-absorbable polyglactin and with a silicone film, covered to nylon mesh containing allogenic neonatal foreskin fibroblasts [40].
3.3 Dermoepidermal (Composite) Substitutes
Apligraf ™ is a bilayer allogenic skin equivalent composed by epidermal and dermal equivalent layers. The dermal layer is formed by culturing human neonatal fibroblasts and bovine collagen I and provides matrix proteins, growth factors, and cytokines. The epidermal layer is composed by human neonatal keratinocytes cultured on top of the dermal layer and secondly incubating the bilayer substrate in an air–liquid interface to induce keratinocyte cornification [29].
OrCel™ is a bilayer substitute composed of bovine type I collagen matrix, fibroblasts, and cultured neonatal keratinocytes. Fibroblasts release cytokines and growth factors like TGF-α, fibroblast growth factor-1 (FGF-1), and keratinocyte release growth factor-1 (KGF-1, 43).
PolyActive: It is a synthetic polyethylene oxide terephthalate and polybutylene terephthalate (PEO/PBT) scaffold with fibroblast and autologous keratinocytes [15, 22].
TissueTech Autograft System (Laserskin and Hyalograft 3D): Hyalograft® is a dermal substitute, Composed by hyaluronic acid membrane and autologous fibroblasts. Laserskin is an epidermal substitute of autologous keratinocytes [43].
Tiscover™ (A-Skin) is an autologous full thickness cultured skin, composed of a pigmented epidermis on fibroblast dermis [23].
4 Conclusions
The function of skin substitutes is to regenerate partial or full thickness wounds and can be used as temporary or definitive coverage. They can be composed by different biomaterial, scaffolds, cells, and growth factors. Bioactive living cells produce growth factors and cytokines that help recruit host cells into the matrix. The process is often time-consuming and can take about 3–4 weeks in composite substitutes. The possible limitations are scar formation, poor integrity, and high price [44]. Cost analyses showed that despite high initial costs, skin substitutes can improve wound healing and reduce morbidity, compared with standard therapy [45, 46]. Innovations in cell tissue culture approaches and large-scale production will reduce in the future the cost and will produce higher quality skin analogs [47].
References
Catalano E, Cochis A, Varoni E, Rimondini L, Azzimonti B. Tissue-engineered skin substitutes: an overview. J Artif Organs. 2013;16(4):397–403.
MacNeil S. Biomaterials for tissue engineering of skin. Mater Today. 2008;11(5):26–35.
Gómez C, Torrero V, Ferreiro I, Pérez D, Palao R, Martínez E, Llames S, Meana A, Holguín P. Use of an autologous bioengineered composite skin in extensive burns: clinical and functional outcomes. A multicentric study. Burns. 2011;37(4):580–9.
Debels H, Hamdi M, Abberton K, Morrison W. Dermal matrices and bioengineered skin substitutes: a critical review of current options. Plast Reconstr Surg Glob Open. 2015;3(1):e284.
Langer R, Vacanti JP. Tissue engineering. Science. 1993;260(5110):920–6.
Damanhuri M, Boyle J, Enoch S. Advances in tissue-engineered skin substitutes. Wounds Int. 2011;2(1):27–34.
Wang H, Pieper J, Peters F, van Blitterswijk CA, Lamme EN. Synthetic scaffold morphology controls human dermal connective tissue formation. J Biomed Mater Res A. 2005;74(4):523–32.
Vig K, Chaudhari A, Tripathi S, Dixit S, Sahu R, Pillai S, Dennis VA, Singh SR. Advances in skin regeneration using tissue engineering. Int J Mol Sci. 2017;18(4):789.
Nicholas MN, Jeschke MG, Amini-Nik S. Methodologies in creating skin substitutes. Cell Mol Life Sci. 2016;73(18):3453–72.
Sheikholeslam M, Wright ME, Jeschke MG, Amini-Nik S. Biomaterials for skin substitutes. Adv Healthcare Mater. 2017; https://doi.org/10.1021/acsami.6b12325.
Rahmani Del Bakhshayesh A, Annabi N, Khalilov R, Akbarzadeh A, Samiei M, Alizadeh E, Alizadeh Ghodsi M, Davaran S, Montaseri A. Recent advances on biomedical applications of scaffolds in wound healing and dermal tissue engineering. Artif Cells Nanomed Biotechnol. 2017:1–15.
Karageorgiou V, Kaplan D. Porosity of 3D biomaterial scaffolds and osteogenesis. Biomaterials. 2005;26(27):5474–91.
Biedermann T, Boettcher-Haberzeth S, Reichmann E. Tissue engineering of skin for wound coverage. Eur J Pediatr Surg. 2013;23(5):375–82.
Pasparakis M, Haase I, Nestle FO. Mechanisms regulating skin immunity and inflammation. Nat Rev Immunol. 2014;14(5):289.
Dixit S, Baganizi DR, Sahu R, Dosunmu E, Chaudhari A, Vig K, Pillai SR, Singh SR, Dennis VA. Immunological challenges associated with artificial skin grafts: available solutions and stem cells in future design of synthetic skin. J Biol Eng. 2017;11:49.
Pastar I, Stojadinovic O, Yin NC, Ramirez H, Nusbaum AG, Sawaya A, Patel SB, Khalid L, Isseroff RR, Tomic-Canic M. Epithelialization in wound healing: a comprehensive review. Adv Wound Care. 2014;3(7):445–64.
Hachiya A, Sriwiriyanont P, Kaiho E, Kitahara T, Takema Y, Tsuboi R. An in vivo mouse model of human skin substitute containing spontaneously sorted melanocytes demonstrates physiological changes after UVB irradiation. J Gen Intern Med. 2005;20(5):364–72.
Bielefeld KA, Amini-Nik S, Alman BA. Cutaneous wound healing: recruiting developmental pathways for regeneration. Cell Mol Life Sci. 2013;70(12):2059–208.
Koh TJ, DiPietro LA. Inflammation and wound healing: the role of the macrophage. Expert Rev Mol Med. 2011;13:e23.
Larouche D, Cantin-Warren L, Desgagné M, Guignard R, Martel I, Ayoub A, Lavoie A, Gauvin R, Auger FA, Moulin VJ. Improved methods to produce tissue-engineered skin substitutes suitable for the permanent closure of full-thickness skin injuries. BioResearch Open Access. 2016;5(1):320–9.
Shevchenko RV, James SL, James SE. A review of tissue-engineered skin bioconstructs available for skin reconstruction. J R Soc Interface. 2010;7(43):229–58.
Groeber F, Holeiter M, Hampel M, Hinderer S, Schenke-Layland K. Skin tissue engineering—in vivo and in vitro applications. Adv Drug Deliv Rev. 2011;63(4–5):352–66.
Varkey M, Ding J, Tredget EE. Advances in skin substitutes-potential of tissue engineered skin for facilitating anti-fibrotic healing. J Funct Biomater. 2015;6(3):547–63.
Shevchenko RV, James SL, James SE. A review of tissue-engineered skin bioconstructs available for skin reconstruction. J R Soc Interface. 2009; https://doi.org/10.1098/rsif.2009.0403.
Metcalfe AD, Ferguson MW. Tissue engineering of replacement skin: the crossroads of biomaterials, wound healing, embryonic development, stem cells and regeneration. J R Soc Interface. 2007;4(14):413–37.
Supp DM, Boyce ST. Engineered skin substitutes: practices and potentials. Clin Dermatol. 2005;23(4):403–12.
Groeber F, Holeiter M, Hampel M, Hinderer S, Schenke-Layland K. Skin tissue engineering—in vivo and in vitro applications. Adv Drug Deliv Rev. 2011;63(4–5):352–66.
Wood FM, Stoner ML, Fowler BV, Fear MW. The use of a non-cultured autologous cell suspension and Integra® dermal regeneration template to repair fullthickness skin wounds in a porcine model: a one-step process. Burns. 2007;33(6):693–700.
Nicholas MN, Yeung J. Current status and future of skin substitutes for chronic wound healing. J Cutan Med Surg. 2017;21(1):23–30.
Lepow BD, Downey M, Yurgelon J, Klassen L, Armstrong DG. Bioengineered tissues in wound healing: a progress report. Expert Rev Dermatol. 2011;6(3):255–62.
Shakespeare PG. The role of skin substitutes in the treatment of burn injuries. Clin Dermatol. 2005;23(4):413–8.
Branski LK, Herndon DN, Pereira C, Mlcak RP, Celis MM, Lee JO, Sanford AP, Norbury WB, Zhang X-J, Jeschke MG. Longitudinal assessment of Integra in primary burn management: a randomized pediatric clinical trial. Crit Care Med. 2007;35(11):2615–23.
Boyce ST, Goretsky MJ, Greenhalgh DG, Kagan RJ, Rieman MT, Warden GD. Comparative assessment of cultured skin substitutes and native skin autograft for treatment of full-thickness burns. Ann Surg. 1995;222(6):743.
Pham C, Greenwood J, Cleland H, Woodruff P, Maddern G. Bioengineered skin substitutes for the management of burns: a systematic review. Burns. 2007;33(8):946–57.
Böttcher-Haberzeth S, Biedermann T, Reichmann E. Tissue engineering of skin. Burns. 2010;36(4):450–60.
O’Connor N, Mulliken J, Banks-Schlegel S, Kehinde O, Green H. Grafting of burns with cultured epithelium prepared from autologous epidermal cells. Lancet. 1981;317(8211):75–8.
Carsin H, Ainaud P, Le Bever H, Rives J-M, Lakhel A, Stephanazzi J, Lambert F, Perrot J. Cultured epithelial autografts in extensive burn coverage of severely traumatized patients: a five year single-center experience with 30 patients. Burns. 2000;26(4):379–87.
Catalano E, Cochis A, Varoni E, Rimondini L, Azzimonti B. Tissue-engineered skin substitutes: an overview. J Artif Organs. 2013;16(4):397–403.
Halim AS, Khoo TL, Mohd Yussof SJ. Biologic and synthetic skin substitutes: an overview. Indian J Plast Surg. 2010;43(Suppl):S23–8.
Kumar MR, Muzzarelli RA, Muzzarelli C, Sashiwa H, Domb A. Chitosan chemistry and pharmaceutical perspectives. Chem Rev. 2004;104(12):6017–84.
Nyame TT, Chiang HA, Orgill DP. Clinical applications of skin substitutes. Surg Clin. 2014;94(4):839–50.
Mahboob Morshed N, Chowdhury S, Ruszymah B. The current available biomaterials being used for skin tissue engineering. Regen Res. 2014;3:17–22.
Uccioli L. A clinical investigation on the characteristics and outcomes of treating chronic lower extremity wounds using the tissuetech autograft system. Int J Low Extrem Wounds. 2003;2(3):140–15.
MacNeil S. Progress and opportunities for tissueengineered skin. Nature. 2007;445(7130):874.
Schonfeld WH, Villa KF, Fastenau JM, Mazonson PD, Falanga V. (2000) An economic assessment of Apligraf (Graftskin) for the treatment of hard-to-heal venous leg ulcers. Wound Repair Regen 8:251–257. 45.
Redekop WK, McDonnell J, Verboom P, Lovas K, Kalo Z. The cost effectiveness of Apligraf treatment of diabetic foot ulcers. Pharmaco Economics. 2003;21:1171–83.
Shahrokhi S, Arno A, Jeschke MG. The use of dermal substitutes in burn surgery: acute phase. Wound Repair Regen. 2014;22(1):14–22.
Conflict of Interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Agata, J., Marco, R. (2020). Tissue-Engineered Skin Substitutes. In: Fimiani, M., Rubegni, P., Cinotti, E. (eds) Technology in Practical Dermatology. Springer, Cham. https://doi.org/10.1007/978-3-030-45351-0_44
Download citation
DOI: https://doi.org/10.1007/978-3-030-45351-0_44
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-45350-3
Online ISBN: 978-3-030-45351-0
eBook Packages: MedicineMedicine (R0)