Abstract
The creation of skin substitutes has significantly decreased morbidity and mortality of skin wounds. Although there are still a number of disadvantages of currently available skin substitutes, there has been a significant decline in research advances over the past several years in improving these skin substitutes. Clinically most skin substitutes used are acellular and do not use growth factors to assist wound healing, key areas of potential in this field of research. This article discusses the five necessary attributes of an ideal skin substitute. It comprehensively discusses the three major basic components of currently available skin substitutes: scaffold materials, growth factors, and cells, comparing and contrasting what has been used so far. It then examines a variety of techniques in how to incorporate these basic components together to act as a guide for further research in the field to create cellular skin substitutes with better clinical results.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Intact, healthy skin is crucial to maintaining physiological homeostasis. It plays important roles in protection from infections, thermal regulation, and fluid balance. Injuries to the skin affect these functions so it is crucial for the human body to quickly heal skin wounds. Yet there are many instances when the human body cannot adequately heal itself without medical intervention. Skin healing in elderly and in diabetic patients are prominent examples of inadequate healing [1, 2]. In thermal injuries and chronic skin wounds, skin healing is slow and incomplete, leaving the body open to infection and poor thermal and fluid regulation. Currently, the gold standard of treatment in these injuries is to use an autologous skin graft to place over the wound to prevent pathogen entry [3, 4]. However, due to the limit on native skin available, autologous skin grafts can become challenging once these injuries cover a large body surface area [4, 5]. To alleviate this problem, skin substitutes were created to be used in addition to or as a replacement for autologous skin grafts.
Currently there are many skin substitutes used clinically. Each of these products have their advantages and disadvantages. For example Alloderm®, a skin graft derived from human cadavers, provides patients with natural dermal porosity with an intact basement membrane for the hosts skin cells to migrate and adhere onto. However, Alloderm® comes with a risk of infectious disease transmission, a need for multiple surgeries, and a high cost [3]. On the other hand Integra®, an artificial skin graft composed of bovine collagen and chondroitin-6-sulfate, provides patients with a synthetic dermal scaffold that closely mimics human skin allowing the host to form its own dermal layer leading to improved aesthetic and functional outcomes [3]. Yet Integra® also comes with its own disadvantages including lacking an epidermal component, a risk of fluid buildup and subsequent infection underneath the graft, and once again a high cost [3]. Despite the advancements in this field, the ideal skin substitute has yet to be created.
Research in this field has steadily been growing, showcasing novel materials and methodologies in order to create the ideal skin substitutes. Yet as more unique materials and methodologies are created, previous ones are lost in the growing amounts of literature. This review summarizes the different components of skin substitutes as well as highlights the different methodologies used so far for creating these skin substitutes in order to act as a guide for future research in the field.
Criteria for skin substitutes
Although each skin substitute has their own unique characteristics, when making a skin substitute there are five key criteria that need to be met.
Semi-permeable Barrier
The destruction of skin allows pathogens to easily enter the body. As a result, severe infection is a common complication in burns and chronic wounds [6–8]. Early skin grafting to cover the wound decreases the risk of infection making it crucial for skin substitutes to act as a barrier and prevent pathogens from entering the wound [9, 10]. In addition, skin substitutes must prevent the severe fluid loss in certain injuries like full thickness burns while still allowing minimum water exchange to prevent fluid accumulation and thus endogenous bacterial growth beneath the skin substitute [11, 12]. To address this criterion, different skin substitute compositions and morphologies have been tested. For example, incorporating a silicone membrane on skin substitutes, such as what is found on Integra®, creates the same water flux as normal epidermis, 0.5 mL/cm2/h [13].
Cell adherence
Skin substitutes must not only allow cells to adhere to them, but also provide a microenvironment for optimal rates of viability, proliferation, and differentiation. Cell migration and function are influenced by the morphology, particularly thickness, pore size, and interconnecting pores, of the skin substitute [14]. Skin substitute polymer composition also affects cell properties. For example, a strictly gelatin scaffold hinders fibroblast migration compared to collagen-based scaffolds [15, 16]. In acellular skin substitutes, like Alloderm®, host fibroblast migration is an important step to repair the dermal layer of the skin. In skin substitutes seeded with cells in vitro, cells adhere to the skin substitute and need to remain viable before placement of the skin substitute onto the patient. Additionally, adhesion of skin cells is important for further cell differentiation [17]. The end goal for both of these approaches is for skin cells to fully penetrate and remain viable within the entire graft.
Non-toxic, non-inflammatory, non-immunogenic
Excess inflammation is known to impair wound healing [18]. These same inflammatory processes can contribute to graft rejection, a potent reaction causing rapid elimination of donor cells and degradation of the skin substitute risking pathogen entry and/or severe water loss [19]. Due to increased inflammation from graft rejection, there may be increased fibrosis and scarring at the wound site causing poor functional and aesthetic outcomes. A successful skin graft prevents rejection by being non-toxic, non-inflammatory, and non-immunogenic. Autologous skin grafts have almost zero risk of rejection as they use the host’s own cells for grafting while allogeneic skin grafts from human cadavers have a much higher risk of graft rejection due to immunological recognition of foreign antigens [19]. Synthetic skin grafts vary in their risk of rejection depending on the toxicity and immune effects of the compounds and cells used to create the skin substitute.
Durable, malleable, and biodegradable
An ideal skin substitute must be durable enough to prevent tears from shear stress during application, but malleable enough to be placed on areas like knees, hips, and hands. The skin substitute should be biodegradable in order to allow the host’s dermis to eventually replace it. However, the skin substitute cannot degrade too quickly as it provides a scaffold for vascularization of the dermis, a critical step for a viable epidermis. This formation of new blood vessels is significantly affected by the skin substitute’s thickness and porosity [20, 21]. Generally, three weeks is assumed to be enough time for vascularization [3]; however, this process has been reported to occur as fast as one week in one porcine excisional wound study [22]. Overall, skin substitutes should generally biodegrade after this time point once vascularization is completed.
Cost-effective
As healthcare increasingly becomes more expensive, cheaper treatments must be created. Life saving treatments with current skin substitutes can cost up to one hundred thousand US dollars per person [23]. In the future, there will be increased demand for skin substitutes that have the same or better skin regeneration effect, but at a fraction of the cost.
Anatomical features of skin
As research around skin substitutes evolve, there is an increasing push to make skin substitutes that mimic human native skin in gross appearance and histologically. As we are unsure what an identical skin substitute should resemble, comparing it histologically in vitro is one method, while understanding that there are significant changes to skin substitutes’ genetic expression and mechanical properties in in vivo settings compared to in vitro [24, 25]. To do this, it is important to understand the basic skin layers and their functions.
The key layers of human skin consist of the epidermis and dermis. The epidermal layer provides a physical barrier against pathogen entry while allowing water exchange across the skin. The primary cell type in this layer is keratinocytes, which are constantly replaced by basal layer stem cells. Additionally, there are other cell types located here including melanocytes and specialized dendritic cells called Langerhans cells. In skin injuries where only the epidermal layer is damaged, there is usually complete healing without noticeable scarring as keratinocytes are easily able to migrate and re-epithelialize the area.
The dermal layer provides the majority of skin’s structural support. Human dermis is subdivided into two distinct layers, the upper papillary layer composed of loose and fine collagen fibers and the lower reticular layer composed of densely packed collagen fibers and elastic fibers. The primary cell type in this layer is fibroblasts, cells that constantly secrete collagen and fibronectin to form an extracellular matrix (ECM). In skin injuries where the dermal layer is injured, scarring may occur due to differentiation of migrating fibroblasts to myofibroblasts, which secrete significantly increased amounts of ECM [26, 27].
Components of a skin substitute
There are three main categories of materials involved in a skin substitute that must be considered during manufacturing: scaffolds, growth factors, and cells.
Scaffolds
Three-dimensional scaffolds are a critical component of skin substitutes as they act as an extracellular matrix analog guiding cell adhesion, proliferation, and differentiation to create dermal and/or epidermal layers. Additionally, scaffolds provide a template around which new blood vessels form in a process called neovascularization. This process is necessary for viable dermal and epidermal layers at wound sites.
Many different polymers have been used to create these scaffolds. Each polymer has their unique characteristics affecting scaffold morphology, function of nearby cells, and physical properties of the skin substitute.
Collagen
Collagen is the major component of skin ECM. Twenty-nine different collagen types have been characterized with all types displaying a similar triple helix structure [28]. Collagen type I is most commonly used in collagen-based scaffolds due to it being the major structural and functional protein of dermal matrix [29, 30]. Collagen types III and V are also used in combination with collagen type I when using native bovine collagen matrix-derived scaffolds found in skin substitutes such as Matriderm® [31, 32]. To our knowledge, the effects of different types of collagen on skin cells have not been compared and could help guide manufacturers choose the best collagen for use in skin substitutes. Collagen-based scaffolds are capable of providing skin cells with an optimal microenvironment for adhesion, proliferation, and migration. Collagen-based scaffolds comprise the majority of artificially-made skin substitutes currently available for clinical use. A significant problem with using collagen as the main component of scaffolds for skin substitutes is that it has relatively poor mechanical properties [33]. However, these properties can be improved with various cross-linking methods, typically cross-linking collagen with glycosaminoglycans [34–36], but also with hyaluronic acid [37], fibrin [38], chitosan [30, 39, 40], gelatin [41, 42], elastin [43], pullulan [44–46], alginate [47, 48], laminin [49], poly(L-lactic acid) (PLLA) [50], poly(glycolide-co-L-lactide) (PLGA) [51, 52], poly(ethylene glycol) (PEG) [53], and polycaprolactone (PCL) [54].
Glycosaminoglycans
Glycosaminoglycans are long unbranched polysaccharides comprised of repeating disaccharide units. When cross-linked with collagen, glycosaminoglycans increase pore size and decrease stiffness of collagen-based scaffolds [55]. The most commonly used glycosaminoglycan is chondroitin-6-sulfate [34–36, 56–58], which is found in the currently used skin substitute Integra®. Although unable to form scaffolds without being cross-linked to mechanically stronger polymers like collagen, glycosaminoglycans are very helpful in modifying the mechanical properties of scaffolds for skin substitutes.
Hyaluronic acid
Hyaluronic acid is a subgroup of glycosaminoglycans and is the only glycosaminoglycan that is exclusively non-sulfated. Like other glycosaminoglycans, combining hyaluronic acid with collagen creates a more mechanically favorable scaffold. In addition, collagen and hyaluronic acid cross-linked scaffolds show enhanced cell migration and division compared to collagen-only scaffolds [59]. Hyaluronic acid or its derivatives are found in the current skin substitutes LaserSkin®, Hyalomatrix®, and Hyalograft® [60].
Fibronectin and fibrin
Fibronectin is a glycoprotein found in skin extracellular matrix. It contains the peptide sequence arginine-serine-aspartate involved in integrin-mediated cell adhesion [61]. Dermal fibroblasts attach to these sequences through β1-type integrins during migration [62–64]. Fibrin is a fibrous, non-globular protein that closely associates with fibronectin in blood clotting. The advantage of fibrin over fibronectin is that fibrin can be formed into glue for easy application onto scaffolds. This fibrin glue has been used to coat collagen-based scaffolds to promote cell adhesion and migration [39]. These asymmetric scaffolds show improved epidermal cell adhesion while providing a barrier separating epidermal and dermal cells from each other [39]. Fibrin glue has allowed for easy manufacturing of bilayer skin substitutes.
Chitosan
Chitosan is a linear polysaccharide derived from chitin. A few studies have shown positive wound healing effects from chitosan-based hydrogels [30, 39, 40]. Chitosan hydrogels have also been used in controlled release drug formulations due to their non-toxicity and structural stability [65]. Chitosan hydrogels may be a way to have long-term controlled release of growth factors to improve wound healing. Furthermore, chitosan has antibacterial and antiyeast properties, which contribute to its wound healing properties [66, 67]. There have been reports of chitosan by itself taking an excessive amount of time to biodegrade in vivo and therefore caution should be used when incorporating chitosan in a skin scaffold [67]. However, in vitro studies incubating chitosan with lysozyme solution have shown chitosan scaffolds degrading in 5 weeks [68].
Gelatin
Gelatin is an irreversibly denatured form of collagen with the ability to form a scaffold suitable for dermal regeneration without the incorporation of any other polymers [69]. However, as previously mentioned, gelatin only scaffolds have decreased fibroblast migration compared to collagen-based scaffolds [15, 16]. A key advantage in incorporating gelatin into scaffolds is its ability to absorb relatively large quantities of water. When using freeze-drying techniques to create scaffolds, hydrogels that absorb large quantities of water result in more porous structures. The water absorbed in the scaffold is frozen and acts as a porogen during the freeze-drying process. Since gelatin readily absorbs water, porous gelatin scaffolds are quite easily made through freeze-drying processes [70]. The necessity for porous skin substitutes in order to provide an optimal microenvironment for neovascularization and cell migration makes gelatin an excellent polymer to be considered for use in skin substitutes.
Similar to chitosan, gelatin has the ability to be used in long-term controlled release of growth factors. For example, gelatin that has retained basic fibroblast growth factor, a promoter of fibroblast proliferation, has been mixed with collagen to create collagen-gelatin scaffolds that slowly release growth factor while placed in a wound bed. The end result was a significant increase in dermal tissue at 4 weeks compared to the same scaffolds that did not contain any growth factor [71]. The incorporation of growth factors into skin substitutes is becoming increasingly more prevalent giving another reason why gelatin should be considered for use when creating a skin substitute.
Elastin
Elastin is a protein responsible for skin elasticity. Collagen-based skin substitutes can be limited by their lack of elasticity, which promotes excessive scaffold contraction during wound healing [72]. Excessive skin contraction during severe burns causes increased scarring around the burn site. The addition of elastin to skin substitutes significantly decreases scaffold contraction when compared to collagen-based scaffolds [73]. Furthermore, humans are unable to adequately regenerate and repair destroyed elastin fibers during severe wound healing [74]. Elastin expression in regenerated dermis post severe wound may take 4 to 5 years and can be both functionally and spatially disorganized [75]. Matriderm®, a skin substitute previously mentioned, contains three types of collagen as well as elastin. The use of Matriderm® split-thickness skin grafts on full thickness skin injuries created skin with a similar elasticity to normal, uninjured skin [76]. In burn injuries, the use of a split-thickness skin graft +/− Matriderm® showed increased elasticity in the healed wounds when Matriderm® was applied [198]. In hand burn injuries, where skin contractures can significantly impair joint movement and thus quality of life, the use of Matriderm® achieved full range of motion of hand joints with no hypertrophic scars present [77]. To our knowledge, there are no data on the direct effect of elastin in scaffolds on the viability and behavior of skin cells. Nevertheless, the addition of elastin into skin substitutes may help create skin that is functionally and aesthetically more similar to normal skin.
Pullulan
Pullulan has only recently been incorporated into scaffolds for skin substitutes. It is a polysaccharide polymer with antioxidant and anti-inflammatory properties making it an attractive polymer to prevent infection and graft rejection [46, 78]. Pullulan is also relatively inexpensive when compared to other natural polymers and may be further considered for skin substitutes as the pressure for cheaper medical treatments rises. Currently, pullulan has only been incorporated into collagen and, most recently, gelatin scaffolds for skin regeneration studies, but these studies have all shown promising preliminary results [44–46, 78]. More investigation is needed into the effects of this polymer when incorporated into skin substitutes.
Alginate
Alginate is an anionic polysaccharide extracted from the cell walls of brown algae. Similarly to most polymers mentioned, it shows good biodegradability and low toxicity [79]. It has been incorporated into collagen-based scaffolds to improve their structural stability [47]. However, alginate by itself negatively impacts collagen type I deposition from dermal fibroblasts, potentially making them a non-ideal polymer for skin substitutes [80]. Alginate has been largely considered an ideal polymer for skin printers, devices that seed skin cells onto pre-fabricated biodegradable scaffolds, due to its ionic cross-linking mechanism [81, 82]. Skin printer technology will inevitably advance and thus the use of alginate in skin substitutes will increase.
Laminin
Laminin is a major protein that comprises most of the epidermal basement membrane, along with type IV collagen [83]. Laminin incorporated onto the surface of collagen-based scaffolds promotes cell adhesion, migration, and proliferation [49]. In particular, applying laminin to the surface of skin scaffolds helps promote keratinocyte confluence, creating an epidermal layer in bilayer skin subsitutes [84]. A laminin coating separating dermal and epidermal layers may also provide the foundation for the formation of a basement membrane, a key feature of native skin that synthetic skin substitutes still lack [85].
Biochemically manufactured polymers
Biochemically manufactured polymers include, but are not limited to, poly(L-lactic acid) (PLLA), poly(glycolide-co-L-lactide) (PLGA), poly(ethylene glycol) (PEG), and polycaprolactone (PCL). These polymers have been used in various medical applications including medical sutures, drug delivery systems, and imaging for cancer therapy. There are both in vitro and in vivo studies showing that these biochemically manufactured polymers accelerate cellular function and proliferation [50–52, 54, 86–88]. They can also cause similar negative effects, such as PCL, which can be used to increase the mechanical strength of collagen-based scaffolds, but decreases skin cell viability in concentrations greater than 10 % [89]. Additionally, there is a potential concern that using non-biological materials can prevent the creation of biologically compatible scaffolds [90].
In summary, due to advances in chemical engineering, polymers for biomaterials and scaffolds are being discovered at a rapid rate. The current challenge is to perfect the right combination of polymers to augment the function of scaffolds and create the ideal skin substitute.
Growth factors
The use of growth factors in skin substitutes may potentially expedite certain beneficial wound healing processes while inhibiting other detrimental wound healing processes. As skin substitute technology evolves, growth factors can be used to quicken skin cell migration and neovascularization while preventing fibrosis, thus creating novel skin faster with a better functional and aesthetic result.
Fibroblast growth factor (FGF)
In wound healing, fibroblast growth factors play an important role in angiogenesis and skin cell migration and proliferation. Basic fibroblast growth factor, FGF2, has been used in skin substitutes for these purposes. FGF2, when incorporated into skin substitutes, increases neovascularization, increases epidermal and dermal thickness, and inhibits alpha-smooth muscle actin thereby decreasing wound contraction [91–93]. It also decreased differentiation of fibroblasts into myofibroblasts, which contributed to fibrosis [94]. This leads to better wound healing with a better aesthetic outcome making the incorporation of FGF2 into skin substitutes a valuable option.
Epidermal growth factor (EGF)
Epidermal growth factor plays a crucial role in wound healing by stimulating keratinocytes and fibroblasts to migrate and proliferate [95]. EGF additionally promotes neovascularization of new dermis [95]. EGF directly incorporated into dermal substitutes increased stimulation of fibroblasts to produce growth factors that are necessary for wound healing, promoted epithelization, and improved overall wound healing [96–98]. Dermal substitutes merely soaked in a solution containing EGF still showed increased epithelization and increased wound healing in full thickness burns [99]. EGF shows potential in being an easy and feasible option to amplify wound healing effects in pre-fabricated skin substitutes.
Vascular endothelial growth factor (VEGF)
Vascular endothelial growth factor plays a potent role in angiogenesis in embryogenesis and wound healing. However, overexpression of VEGF has been linked to numerous pathologies including several different types of cancers and microvascular complications of diabetes mellitus [100, 101]. A few studies have been performed using VEGF to enhance wound healing. Altering fibroblast VEGF expression has shown potential increases in wound healing and angiogenesis [102, 103]. Yet increasing VEGF has also been shown to increase fibrosis and scar formation in skin [104, 105]. More studies need to investigate the potential pathologic effects of VEGF-incorporated skin substitutes before it should be considered.
Transforming growth factor beta (TGF-β)
Transforming growth factors beta are 25 kilodalton homodimeric proteins having multiple biological functions affecting epithelial- and mesenchymal-derived cells [106]. Three types of TGF-βs appear to have a significant role in wound healing, TGF-β1, TGF-β2, and TGF-β3. Embryonic wounds that heal without scars express low levels of TGF-β1 and TGF-β2, but higher levels of TGF-β3, while adult wounds that scar express high levels of TGF-β1 and TGF-β2, but lower levels of TGF-β3 [107]. In wound studies, mimicking the TGF-β expression profile of embryonic wounds creates scarless wound healing in adult animals [107]. The delivery of TGF-β1 to a collagen skin substitute quickened wound healing in rabbits [108]. However, it is unknown whether this was due to quickened scar formation. Another approach involved modulating TGF-β3 expression; although, a phase 3 randomized control trial using TGF-β3 to decrease scarring was unsuccessful [109]. Manipulation of TGF-β expression in wound healing with skin substitutes may have the potential to create healed wounds with minimal fibrosis, a crucial element still not accomplished by current skin substitutes.
Platelet-derived growth factor (PDGF)
Platelet-derived growth factors are another key factor that contribute to scarless wound healing. PDGFs induce dermal fibroblasts to produce collagen during wound healing [110]. PDGFs incorporated into skin scaffolds improve wound healing due to increased collagen deposition [111]. However, high levels of PDGF are expressed in hypertrophic scars and keloids [112]. Experimentally neutralizing PDGF in adult wound healing results in scarless healing [107]. The increased collagen deposition from adding PDGF to skin substitutes may lead to scars that have worse aesthetic outcomes with lower mechanical strength. PDGF may be best utilized for its ability to prevent scarring, along with TGF-β, rather than its ability to increase collagen deposition in wounds.
Cells
Cells are necessary components of skin as they have various roles to maintain homeostasis and the overall function of skin. While cells are the main producers of extracellular matrix (ECM) and growth factors in intact skin, it has been speculated that cells are not a necessary component of skin substitutes. Acellular skin substitutes, such as Alloderm®, provide the host with a dermal layer in order for the host’s own cells to quickly migrate and take residence in the skin substitute. However, the addition of cells in vitro allows the creator to have increased control over the final skin product. It also, in theory, should quicken healing, as there is no longer the need to wait for host cell migration, a 3-day process, for proper wound healing [113].
A variety of cells have been incorporated into skin substitutes, each with specific purpose and benefit.
Fibroblasts
Fibroblasts are the predominant cell type in the dermal layer. They have a variety of functions that directly impact skin formation. In the dermal layer, fibroblasts secrete ECM compounds, predominantly collagen and fibronectin. The ECM provides skin structural integrity while altering cellular shape and function. The 3D structure of native ECM alters proliferation and differentiation of fibroblasts and thus the subsequent production of ECM proteins and growth factors [113]. ECM is also the driver of cell migration as dermal fibroblasts attach to specific sequences found in the ECM through β1-type integrins during migration [62, 63]. Commercially available synthetic skin substitutes use fibroblasts’ ability to create ECM. Allogeneic fibroblasts are incorporated onto a vicryl (Dermagraft®) or nylon (Transcyte®) mesh and proliferate for several weeks, allowing for production of growth factors and for creation of a fully formed human dermal ECM prior to placement of the skin substitute.
In wound healing, fibroblasts play an additional role in angiogenesis, producing pro-angiogenic soluble mediators such as VEGF and Ang1, stimulating endothelial cell production in 3D models in vitro [114]. This is a major advantage of fibroblast incorporation into skin substitutes, as rapid neovascularization is a crucial step for successful grafting. Fibroblasts also have a pro-inflammatory effect by secreting mediators, such as TGF-β1, interleukins, and certain chemokines, to recruit and activate macrophages, an important initial step in wound healing [115]. However, this same pro-inflammatory effect can lead to chronic inflammation, myofibroblast production, and subsequent fibrosis [115].
In the epidermis, basement membrane development is delayed and keratinocyte viability is inhibited without the presence of dermal fibroblasts in vitro [116]. Fibroblasts secrete keratinocyte growth factor (KGF), also known as FGF7, contributing to keratinocyte migration and proliferation [113]. Fibroblasts also produce key basement membrane compounds, including laminin 111, collagen IV, collagen VII and laminin 332 [117]. Without the presence of fibroblasts, proper epidermal formation, and thus skin formation, is hindered.
Keratinocytes
Keratinocytes comprise the majority of the epidermis. They play significant roles in barrier maintenance and epithelialization in wound healing. Skin barrier properties are due to the outermost stratum corneum along with keratinocyte tight junctions and adherens junctions, helping regulate the flux of molecules both back and forth through the epidermis [118]. It is the epidermal layer that is most important in preventing pathogen entry and severe water loss. Epithelialization is a series of steps occurring during wound healing [119]. It begins with keratinocytes at the wound edge loosening their adhesion, then migrating towards the injured area and adhering to it. Once there are keratinocytes in the wound bed, they will proliferate to form a basal layer and then differentiate creating the suprabasal layers: spinous, granular, and corneum [119]. Each process is complex and a detailed description is beyond the scope of this review, but understanding epithelialization is crucial to understand how to form an epidermal layer in a skin substitute. Briefly, upon acute injury, keratinocytes loosen their cell–cell and cell-substratum contacts and migrate towards the injured area, in a process called epithelial mesenchymal transition [120]. Migration occurs through a switch in integrin binding affinities with basement membrane molecules, particularly laminin 332 [121]. As previously mentioned, this keratinocyte migration is also promoted by dermal fibroblasts through release of paracrine acting growth factors, such as KGF [113]. There is further evidence showing EGFR activation, cytokines including IL-1, IL-6, and TNF-α, and matrix metalloproteinases (MMPs) all having roles in keratinocyte migration [119]. In an in vitro bioengineered skin construct, down regulation of IL-1 and EGF both prevented keratinocyte migration [122]. Although not investigated in this study, a potential mechanism in increasing keratinocyte migration in skin constructs could be upregulating or exogenously adding IL-1 and/or EGF. Like migration, keratinocyte proliferation in the wound bed is heavily influenced by KGF and MMPs [119]. It is also modified by various other growth factors including PDGF and IGF-1. Human keratinocytes that were genetically modified to secrete significantly increased amounts of PDGF or IGF-1 showed significantly advanced epidermal formation compared to unmodified keratinocytes [123]. Once keratinocytes are confluent across the injured area, proliferation signals decrease and the normal differentiation and stratification processes begin again.
There is increasing evidence for the use of both fibroblasts and keratinocytes in skin substitutes due to the crosstalk between them [124, 125]. Dermal fibroblasts secrete growth hormones that increase keratinocyte proliferation and promote angiogenesis. Epidermal keratinocytes secrete IL-1, a cytokine that not only promotes keratinocyte proliferation and differentiation, but also promotes KGF production from dermal fibroblasts [126]. Keratinocytes also secrete pro-angiogenic growth factors including VEGF and PDGF. As mentioned previously, PDGF secretion also plays a secondary role in promoting dermal fibroblast proliferation [127]. Creating bilayer skin substitutes both better resembles native skin and promotes dermal and epidermal viability. This is the knowledge behind the creation of the first clinically available bilayer skin substitute, Apligraf®. Apligraf® is created through a 6-day incubation of allogeneic fibroblasts placed dropwise onto a bovine collagen-derived semi-permeable matrix and submerged in growth media. Allogeneic keratinocytes are then added dropwise onto the matrix and allowed to incubate for four more days. Media is removed on day 10 creating an air-media interface allowing the keratinocytes to fully differentiate creating a stratum corneum layer over the next several days. Air-media interface, growth media composition including calcium concentration, and decreasing incubation temperatures are key factors that support full keratinocyte differentiation [128]. Apligraf® has been approved for treating diabetic foot ulcers and venous leg ulcers [129, 130]. Orcel® is another example of a commercially available bilayer skin substitute currently used clinically that also contains both allogeneic fibroblasts and keratinocytes, but is slightly thicker than Apligraf® and uses a collagen type I sponge as its matrix [3]. Even Epicel®, the only cultured epidermal autograft available clinically and approved for treating thermal injuries, uses proliferation-arrested mouse fibroblasts during the incubation period of the autologous keratinocytes to increase keratinocyte proliferation.
Mesenchymal stem cells
Mesenchymal stem cells (MSCs) are multipotent cells with the ability to differentiate into a variety of cell types. Currently there are three criteria that define MSCs. First, MSCs must be plastic-adherent when cultured in flasks. Second, they must express stromal surface markers CD105, CD73, and CD90, but lack expression of hematopoietic lineage markers CD45, CD34, CD14 or CD11b, CD79α or CD19, and HLA class II. Third, MSCs must be able to differentiate into osteoblasts, adipocytes, and chondrocytes under specific in vitro conditions [131]. In skin, MSCs differentiate into multiple cell types including keratinocytes, endothelial cells, and pericytes [132]. Dermal fibroblasts bare a striking resemblance in phenotype to MSCs and have been differentiated from MSCs in vitro [133, 134]. The ability for MSCs to differentiate into skin cells creates an exciting potential therapy for skin regeneration. Currently, MSCs used for bioengineering originate from three tissue sources: bone marrow, adipose, and umbilical cord.
Bone marrow-derived MSCs
Bone marrow-derived MSCs (BMSCs) are the most well characterized source of adult stem cells. They play a significant role in skin, as a subpopulation of dermal fibroblasts is naturally bone marrow derived. Further evidence shows that production of dermal collagen III is only from these bone marrow-derived fibroblasts [135]. Several studies have shown that transplantation of BMSCs promotes skin regeneration, making them a promising therapeutic approach [135–137]. There is evidence that BMSC transplantation may show better treatment outcomes than autologous skin grafts [138]. However, BMSCs are limited in amount and have poor multipotent ability after extensive passage. Thus, scientists have sought different tissue-derived MSCs for wound healing therapies.
Adipose-derived MSCs
Adipose-derived MSCs (AMSCs) can be derived with high cell yield from adipose tissue. They can be cultured longer than BMSCs without changes to their multipotency [139], yet they show improvements in skin regeneration upon transplantation, similar to BMSCs [140, 141]. AMSCs show increased skin regeneration when incorporated into a commercially available dermal substitute, Integra®, compared to Integra® alone [142]. AMSCs have also been shown to be superior for skin regeneration than dermal fibroblasts. Incorporation of AMSCs instead of dermal fibroblasts in skin substitutes leads to increased epidermal formation due to significantly increased production of KGF and PDGF [142]. Adipose-derived MSCs appear to be a very promising therapeutic approach for skin regeneration. Long-term lineage tracking of these cells is essential in order to verify if the final product of these cells are fibroblasts.
Umbilical cord-derived MSCs
Umbilical cord-derived MSCs (UMSCs) are derived from umbilical cord blood, umbilical vein sub endothelium, and Wharton’s jelly. They have the highest proliferation capacity compared to BMSCs and AMSCs and can be isolated with non-invasive measures, unlike BMSCs and AMSCs. However, the isolation of UMSCs is difficult and UMSCs are restricted in their potency, showing minimal adipogenic differentiation capacity [139]. Still, UMSCs have been differentiated into fibroblasts in culture as well as on three-dimensional scaffolds [134, 143]. A specific population of UMSCs, Wharton’s jelly-derived MSCs (WJMSCs), are less immunogenic, a trait that may fully prevent skin graft rejection and improve efficacy of skin substitutes [144]. It has recently been shown that WJMSCs secretome promotes skin healing without excessive fibrosis from hyper-proliferating fibroblasts [145]. Further studies are needed regarding the benefits of their reduced immunogenicity in skin regeneration when compared to other MSC sources. UMSCs and more specifically WJMSCs will inevitably be increasingly used in the coming years for skin substitutes due to their high proliferation capacity and decreased immunogenicity.
Melanocytes
Melanocytes are cells located in the basal layer of the epidermis and are responsible for producing melanin, the pigment responsible for skin color. The majority of skin grafts lead to hypopigmented skin compared to normal uninjured skin [146]. The addition of melanocytes into skin substitutes has been effective in being able to alter the healed skin’s natural color [147]. Therefore, melanocyte incorporation provides potential in improving aesthetic outcomes in wounds healed with skin substitutes. Due to a limitation in isolating and replicating large quantities of melanocytes, this feature is not yet available in current clinical skin substitutes.
Macrophages
Macrophages have significant roles in skin healing and hypertrophic scar formation [64, 148–150]. Their presence is essential for proper wound healing and can actually be anti-inflammatory. These potentially anti-inflammatory dermal macrophages have been successfully incorporated into scaffolds with dermal fibroblasts and still retained their ability to produce anti-inflammatory cytokines in vitro [151]. However, to our knowledge, no study has shown in vivo effects of incorporating macrophages into skin substitutes. The use of macrophages should be cautioned though, as macrophages under certain circumstances can also lead to hypertrophic scarring [152]. More research is needed to understand the correct conditions for incorporating macrophages into skin substitutes to obtain the ideal anti-inflammatory effects in wound healing.
Endothelial cells
Endothelial cells are the cells responsible for blood capillary and lymphatic network formation. Incorporating endothelial cells into scaffolds led to the formation of functional blood capillary networks in a dermal substitute [153, 154]. This has been accomplished with lymphatic capillaries as well [155]. These blood and lymphatic capillaries successfully anastomosed to in vivo capillaries in a mouse and rat model, respectively [154, 155]. Therefore, endothelial cell incorporation created skin substitutes with a better chance of having appropriate blood supply and lymphatic drainage, which would potentially lead to greater grafting success rates.
Hair follicles stem cells
Current skin substitutes lack hair production as in vitro trichogenesis in skin substitutes has consistently been a challenge. The creation of hair follicles has recently been successfully completed in skin substitutes, although the methodology behind it is lengthy and intricate [156, 157]. Although it may take time for hair follicles stem cells to be incorporated into clinically available skin substitutes, there is hope that at least in vitro trichogenesis is now possible.
Eccrine sweat gland cells
Like hair follicles, current skin substitutes do not contain sweat glands. This leads to skin that does not sweat in patients treated with current skin substitutes [158]. The creation of sweat gland-like structures in vitro in skin substitutes has been completed and there is some evidence that creating these structures has positive effects on wound healing itself [159]. This is another area of research where more exploration is required before it will be available in skin substitutes used clinically.
Creating skin substitutes
Customizing a scaffold’s physical properties
As discussed previously, the majority of skin substitutes require scaffolds. They provide a template for cells to adhere to during wound healing and for neovascularization. The morphology of a scaffold greatly alters the growth capacity, metabolic function, and differentiation potential of adhered cells. The speed and extent of neovascularization is also affected by scaffold morphology. When referring to scaffold morphology, a number of physical characteristics must be looked at, including porosity, structural integrity, swelling, and elasticity.
Porosity
Porosity refers to the void spaces in a material, which provide a route for cell penetration as well as provide a template for neovascularization. In general, the larger the average pore size, the more cell migration [160], cell infiltration [161], ECM secretion [162], and increased vascularization [163]. There are four basic methods of controlling porosity of hydrogels: solvent casting/particle leaching, freeze-drying, gas foaming, and electrospinning. In addition, there are advanced methods including micropatterning and micromolding as well as 3D printing, which controls specific pore features and microarchitecture.
Solvent casting/particle leaching
Solvent casting/particle leaching consists of mixing a porogen of known particle size into a polymer solution. The addition of this porogen solidifies the polymer solution and will be subsequently leached or dissolved from the solidified polymer-porogen solution upon immersion in a selective solvent. This leaves behind a network of pores in the hydrogel [164]. The most common porogen used in skin substitutes are salts, namely sodium chloride. However, using glucose or gelatin as porogens with deionized water as the selective solvent has created porous hydrogels [165, 166]. Solvent casting/particle leaching allows easy manipulation of pore sizes and overall porosity. Altering the particle size creates pores of different sizes, while decreasing the concentration of solute in the polymer-porogen solution decreases overall porosity. One restriction of solvent casting/particle leaching is the limitation of removing solid particles from the middle of a thick material, therefore limiting the width of hydrogels created through this method. This can be mediated by combining solvent casting/particle leaching with another method of creating pores, particularly freeze-drying.
Freeze-drying
Freeze-drying, otherwise known as lyophilization, is a commonly used method of using water as a porogen to create porous hydrogels. Hydrogels that have absorbed water are frozen and the resulting ice crystals are subsequently sublimated under vacuum. This leaves behind pores where the ice crystals were before. This method can be easily altered to affect the pore size and scaffold morphology. First, hydrogel composition can affect pore size. Although gelatin readily absorbs water making it an ideal candidate for hydrogels prepared through freeze-drying, a high proportion of gelatin in a scaffold actually decreases pore size, potentially due to gelatin’s effect on heat transfer and solvent freezing temperature [167]. Second, increasing the freezing temperature creates larger mean pore sizes, for example having a final freezing temperature of −10 °C creates larger pores than having a final freezing temperature of −40 °C [168]. Third, increasing the freezing temperature to −196 °C (in liquid N2) results in parallel sheet structure pores compared to open pore structures when hydrogels are frozen at −20 °C and −80 °C [164]. Freeze-drying is a relatively easy yet time-consuming method that works with most hydrogel materials. However, during the freeze-drying stage, strict control over the hydrogel temperature must be kept as if the temperature is not low enough, surface skin occurs. Surface skin refers to when internal pores in a hydrogel have collapsed due to insufficient structural rigidity during the freeze-drying process. The end result is a porous surface with a dense, non-porous core. To prevent surface skin, a modified freeze-drying technique has been created where the sample is kept in a liquid nitrogen bath while freeze-drying is occurring [169]. Two techniques, freeze gelation and freeze extraction, have also been created to prevent surface skin. These two techniques extract solvents out of hydrogels at freezing temperatures without the need for a commercial freeze-dryer creating highly porous hydrogels without evidence of surface skin [169, 170].
Gas foaming
Gas foaming incorporates gases, commonly CO2, into hydrogels to form porous structures. Briefly, hydrogels are equilibrated with CO2 under high pressures. The CO2 pressure is rapidly dropped causing nucleation and expansion of CO2 bubbles [171]. In another method of gas foaming, a foaming agent, most commonly sodium bicarbonate or ammonium bicarbonate, is mixed into the hydrogel and generates CO2 as it decomposes [164]. Similar to solvent casting/particulate leaching, gas foaming allows control over pore size and morphology through changes in operating temperature and pressure [172]. However, solvent casting/particulate leaching usually requires the use of an organic solvent, which is not conducive to high cell viability. Gas foaming does not require any solvent allowing it to incorporate bioactive molecules, such as protein or plasmid DNA, with minimal degradation [171].
A similar method, the overrun process, combines gas foaming and freeze-drying methodology to create porous hydrogels. N2 gas is injected into a polymer solution as the polymer solution goes through a pre-cooled barrel. When the solution touches the sides of this barrel, ice crystals are formed and later sublimated through freeze-drying. The combination of N2 bubbles and freeze-drying creates hydrogels with homogeneous distribution of pores [173]. However, this process creates closed pore structures, which is not suitable for cell penetration into the hydrogel. Combining the overrun process with particle leaching alleviates this problem, creating uniformly distributed and interconnected open pore structures [174]. Although this method seems promising, a major drawback would be the need for special equipment for the overrun process.
Electrospinning
Electrospinning uses externally applied electric fields to draw fine fibers from a polymer solution as it is injected through a nozzle or syringe. The solvent from the polymer solution evaporates as the fibers are attracted to a grounded collector. Electrospinning has been used for both biodegradable polymers and natural proteins, including PCL [175–177], PLGA [178], collagen [177, 179], elastin [177, 179], and gelatin [175, 177]. However, electrospinning natural proteins like collagen, elastin, and gelatin would create hydrogels that would lose their 3D structure in aqueous conditions without a cross-linking agent [177]. Electrospinning creates large networks of interconnected fibers and pores creating hydrogels with significantly high porosity. Yet electrospinning still has a variety of challenges including poor tensile strength, limited control over pore structures, and the inability to create complex hydrogel architecture [164].
Micropatterning and micromolding
Micropatterning and micromolding are advanced techniques that allow researchers to create hydrogels with unique designs of various geometries and sizes. There are a variety of ways to create these patterns, for example soft lithography. In this method, a hydrogel is micromolded using a stamp made out poly(dimethysiloxane) (PDMS). The PDMS stamp pattern can be created through a number of ways including photolithography, which uses UV light to create patterns directly onto the stamp surface, and microfluidic patterning, which uses transient channels to flow liquid in a limited surface area on the stamp carving out the specific hydrogel pattern [180]. Once the pattern has been created, hydrogels are stamped with the hydrophilic PDMS stamp and cross-linked with UV radiation. Poly(dimethysiloxane) micromolding creates a series of channels running throughout a hydrogel. Altering the design of the stamp and stacking hydrogel layers on top of one another creates these channel-like structures [164]. A unique feature of micromolding is that live cells can be encapsulated within a hydrogel creating a structure that is completely homogeneously distributed with cells [181]. Other methods of micropatterning include sterolithography and laser microstructuration, both using lasers directly onto the hydrogel surface [180].
3D printing
The use of 3D printing is a newer technology that has allowed for precise pore sizes and geometries using different materials. These technologies have been rapidly advancing over the past several years and as such, the accessibility to 3D printing has never been greater. The most common 3D printing methods require specific technology, but can create patient specific designs, potentially improving their clinical benefit [182]. Due to the novelty of this emerging technology, most of these methods have not been tested specifically for skin substitutes, yet one form of 3D printing using laser printing has been proven to be effective providing initial evidence of skin regeneration in in vivo mouse models [183, 184]. The use of microfluidics has also been used with preliminary positive evidence for skin substitutes; however, further research must be completed before any conclusions are to be made [81, 185]. Other 3D printing methods have previously been compared and contrasted in current literature and will not be repeated here [182, 186], but it is important to address the overall limitations of this newer technology. Most 3D printing methods use processing conditions that can damage the biomaterials used. This prevents growth factors from being incorporated into the hydrogel’s biomaterials for sustained growth factor release. Additionally, the majority of 3D printed skin substitutes face problems with durability and malleability. This may be due to the biomaterials used, for instance microfluidic methods for skin substitutes have predominantly used alginate as the basis for their biomaterial. This may also be due to the limitation on maximum hydrogel thickness in terms of oxygen and nutrient diffusion with one study showing cell growth into hydrogels only 200 μm deep on each side [187]. The fragile nature of these skin substitutes can significantly limit their clinical applicability. However, the benefit of creating customizable macro and microarchitecture in skin substitutes outweighs these limitations. Spatial distribution of stem cells and their interactions within their niche are essential steps during tissue development and healing, highlighting the potential advantage of 3D printing [188]. There will inevitably be further advances in this field of research with the use of these technologies for human in vivo studies in the near future.
Structural integrity
Skin substitutes need to be durable enough to withstand constant handling throughout preparation and placement. However, skin substitutes must remain thin—most native skin is 2–3 mm thick—and porous. Thus, skin substitutes must increase their structural integrity through selection of stable polymers either by themselves or by cross-linking non-durable polymers to ones that have high integrity. There are numerous methods to cross-link polymers as described in detail in a review by W.E. Hennink and C.F. van Nostrum [189]. Chemical cross-linking methods are commonly used in skin substitutes due to being highly versatile and easy to use [189]. Commonly used chemicals like glutaraldehyde may delay degradation of hydrogels [190], but can be toxic to cells and induce apoptosis [191]. Genipin, a chemical cross-linker used in hydrogel fabrication, is roughly 10,000 times less cytotoxic than traditional glutaraldehyde [192]. The use of genipin over glutaraldehyde in hydrogels has shown decreased inflammation in vivo when compared to one another [193]. A way to completely avoid the use of potentially cytotoxic and genotoxic chemicals for cross-linking is to resort to physical cross-linking methods. Dehydrothermal treatment, a physical process creating crosslinking within collagen scaffolds through condensation reactions, has been used for dermal substitutes, yet it creates less stiff scaffolds when compared to chemical cross-linkers, such as glutaraldehyde [36, 194]. As previously mentioned, ultraviolet light can be used as a cross-linking agent [181]. Typically, ultraviolet light is seen as toxic to cells, but long-wave ultraviolet light irradiation can be used to cross-link a hydrogel with living cells fully encapsulated inside [195]. Full infiltration of cells into a hydrogel is a difficult process, but is necessary for effective therapeutic results. It is important to note that UV cross-linking methods may affect the resulting hydrogel architecture [196]. In the end, many different cross-linking agents can be used in a skin substitute as long as they are compatible with the polymers involved and do not hinder cell growth and function.
Swelling and elasticity
The ability for a skin substitute to swell is important for nutrient and oxygen diffusion as well as the elasticity of the final product. As skin substitutes develop, there is a further push towards mimicking the elastic properties of skin for both functional and aesthetic purposes. Different ECM stiffnesses can affect the differentiation of MSCs. MSC differentiation is correlated to its native tissue stiffness and elasticity and therefore MSCs grown on hard substrates tend to differentiate toward bone and muscle, while softer substrates tend to support MSC differentiation into fat, cartilage and nerves [197, 198]. Furthermore, the concept of mechanotransduction, the effect of mechanical stimuli on cellular responses, is affected by matrix stiffness. Fibroblasts, such as ones found in skin, prefer to exist under a defined range of interstitial stress (~3–5.5 kPa) and therefore when the matrix they are adhered onto is stretched, increasing the amount of interstitial stress, a fibrotic response occurs [199]. On the other hand, if the matrix has no interstitial stress, fibroblasts will undergo anoikis, a form of programmed cell death [199]. There are also changes to integrin binding to ECM and a cell’s actin cytoskeleton by mechanotransduction that would differ based on different matrix strengths [199]. Therefore, in skin substitutes, matrices that are easily strained or not at all may prevent proper wound healing. These effects on cellular differentiation and mechanotransduction suggest that the matrix for skin substitutes should be similar in stiffness and elasticity as native skin and should perhaps promote the use of different matrices for different areas of human skin. However, although studies have shown skin post-wound healing can have different resulting elasticities when treated with different skin substitutes [146], it is still unknown whether the elasticity of the skin substitutes directly affects the final resulting skin elasticity or whether it is another component or characteristic of the skin substitute. The degree of swelling and elasticity of a hydrogel is dependent on the types of polymers in the hydrogel such as elastin which has previously been mentioned, cross-link density, and polymer concentration [200].
Cross-link density refers to the proportion of polymers cross-linked together. In terms of chemical cross-linking agents, increasing the concentration of a cross-linking agent increases the proportion of polymers cross-linked [201]. This increased proportion of cross-linked polymers decreases the resulting hydrogel’s elasticity, but increases structural stability [202]. An example of altering physical cross-linking methods is the ability to increase ultraviolet light’s cross-linking effectiveness. Photo initiators are incorporated into hydrogels to help initiate photopolymerization upon exposure to ultraviolet light. Increasing concentration of photo initiators and ultraviolet irradiation intensity increases overall polymerization and cross-linking [195]. However, it is important to note that increasing ultraviolet irradiation intensity can lead to higher cytotoxicity.
Increasing polymer concentration decreases a hydrogel’s swelling capacity and decreases its elasticity [200]. When creating novel hydrogels, one should manipulate polymer concentrations to create a hydrogel that is stable enough for preparation and application without sacrificing too much elasticity. The relationship between elasticity and polymer concentration also plays a role on cell physiology. The loss of elasticity from increased polymer concentration has been associated with decreased fibroblast migration in skin substitutes [203].
Cell incorporation into scaffolds
As skin substitute technology advances, there is a greater push towards creating skin substitutes incorporated with viable cells. There is a range of potential techniques to incorporate cells onto a premade scaffold.
Monolayer scaffolds
There are several techniques to incorporate one cell line into a skin substitute as shown in Fig. 1. One potential technique is immersing the scaffold in a solution containing one cell line with its corresponding growth media [204]. This causes cells to adhere onto the surface of the scaffold as the cells settle downwards due to gravity; however, this may lead to suboptimal concentrations of cells adhering to the scaffold. An additional method is growing cells on a surface, placing one side of the scaffold on the surface, and then allowing time for the cells to migrate and adhere to the scaffold [69]. Yet this may require excess time to allow cells to fully migrate and adhere to the scaffold. To increase the concentration of cells adhering to a scaffold in a time-efficient manner, it is possible to place a small amount of growth media mixed with high numbers of cells dropwise onto the surface of the scaffold [46]. To further increase and expedite the adherence and penetration of cells into scaffolds, the use of capillary force seeding [44], matrix degassing to create low pressure environments [205], or different degrees of centrifugation can be incorporated into the seeding process [206]. Following centrifugation, incubating the dermal cells for 72 h allows the cells to migrate throughout the entire scaffold provided that the scaffold’s porosity allows for it [113]. For skin substitutes where problems with cell penetration into the scaffold exist, injecting a solution of cells directly into the scaffolds [207] or creating small incisions in the matrix prior to seeding has been shown to increase penetration of cells in skin substitutes [208]. Both of these techniques require destruction of the original matrix and may not be appropriate in certain circumstances. Another method to improve cell penetration includes the unique method of UV cross-linking scaffold solutions with live cells [209]; however, this requires specific materials for the scaffold as previously mentioned altering the mechanical properties of the skin substitute. Finally, although quite expensive, there is support for the use of bioreactors for different dynamic seeding techniques including rotational seeding for skin substitutes [210]. The use of bioreactors allows for uniform distribution of cells throughout hydrogels and similar seeding densities between different hydrogels decreasing variation in tissue engineering and allowing for mass manufacturing of bioengineered tissues.
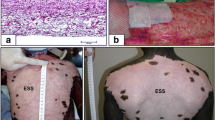
Techniques to incorporate cells into monolayer skin substitutes. a Submerging a scaffold into a solution of cells allows cells to adhere onto the scaffold as they settle to the bottom. b Placing a scaffold onto a surface covered with adhered cells allows cells to slowly migrate and adhere onto the underside of the scaffold. c Placing a drop of media with a high concentration of cells onto the top of the scaffold allows for higher concentrations of cells to adhere onto the surface of the scaffold. d Using centrifugation and matrix degassing allows for increased penetration of a drop of cells deeper into the scaffold. e For scaffolds where cell penetration is an issue, injecting cells directly into the scaffold or f making small incisions in the scaffold prior to seeding allows for cells to adhere into the middle of the scaffold. Using UV light to cross-link scaffold solutions with live cells (not pictured) may also be used for this reason, although it requires unique cross-linking reagents in the scaffold
Bilayer scaffolds
As stated previously, there is increasing evidence for the use of both fibroblasts and keratinocytes in skin substitutes due to the crosstalk between them [124, 125]. The challenge is seeding two cell lines to create a bilayer skin substitute as there needs to be a clear division between the epidermal and dermal layers. After culturing scaffolds with adhered dermal cells, it is possible to seed epidermal cells dropwise onto one surface of the scaffold [211] or by placing the cellularized scaffold onto a surface previously adhered with keratinocytes [69]. Both of these techniques may create a bilayer scaffold, but one significant component is missing, the basement membrane. The use of both fibroblasts and keratinocytes has been shown to improve basement membrane formation, but without pre-existing basement membrane components, polarization of basal keratinocytes and tissue architecture is abnormal [116]. To overcome this challenge, coating scaffolds with basement layer components, such as laminin and/or collagen may help create appropriate bilayer formation as well as provide a physical barrier separating dermal and epidermal layers [116]. Furthermore, the use of specific basement membrane components, such as laminin 332 [212], increases epidermal cell adherence, another common challenge experienced while creating bilayer skin substitutes.
3D cell patterning
As previously mentioned, the use of 3D printing for biomaterials is increasing, but now the use of 3D printing to incorporate cells into hydrogels is also increasing. The benefit of 3D printing for cell incorporation is the ability to allow precise placement of different cell lines, a possibility not accomplished by the previously mentioned cell incorporation techniques. This allows the creation of different cell patterns in hydrogels. In skin substitutes, cell patterning is novel and has mostly been used to incorporate only fibroblasts and keratinocytes in bilayer skin substitutes that mimic native human skin histologically [184, 213]; however, there is potential in creating different patterns that may show different biological effects [183]. The ability to match human skin histologically also allows the addition of further cell lines, such as melanocytes, hair follicle stem cells, and eccrine sweat gland cells. Still, further advancements are needed to increase the precision of cell placement so different cell lines can be placed within micrometers of each other. It will require collaboration from many different people including biomedical engineers and stem cell biologists in order for skin printers to become commonplace for creating skin substitute hydrogels and incorporating cells into them.
Conclusion and perspectives
Over the recent decades, skin tissue engineering research has expanded immensely; however, the ideal skin substitute has not been found. Many research studies focus on studying the effect of one factor, in particular looking at new polymers for creating acellular skin substitutes. It is now time to incorporate everything learned so far to create one comprehensive skin substitute. This would involve incorporating the appropriate scaffold polymers, growth factors, and all cell lines including melanocytes and hair follicle stem cells into one complete skin substitute. It is important to focus not just on the functional outcomes of the healed skin, but the aesthetic ones as well. As we progress, we can create this comprehensive skin substitute using any of the previously mentioned techniques, potentially even utilizing the emerging microfluidic skin printing technique. It is an exciting time for skin tissue engineering and with so much research in the field and demand for a better product, the ideal skin substitute is just around the corner.
References
Jeschke MG, Patsouris D, Stanojcic M, Abdullahi A, Rehou S et al (2015) Pathophysiologic Response to Burns in the Elderly. EBioMedicine 2:1536–1548
Brem H, Tomic-Canic M (2007) Cellular and molecular basis of wound healing in diabetes. J Clin Investig 117:1219–1222
Shahrokhi S, Arno A, Jeschke MG (2014) The use of dermal substitutes in burn surgery: acute phase. Wound repair and regeneration: official publication of the Wound Healing Society [and] the European Tissue Repair Society 22: 14–22
Snyder DL, Sullivan N, Schoelles KM (2012) AHRQ Technology Assessments. Skin Substitutes for Treating Chronic Wounds. Agency for Healthcare Research and Quality (US), Rockville
Branski LK, Herndon DN, Pereira C, Mlcak RP, Celis MM et al (2007) Longitudinal assessment of Integra in primary burn management: a randomized pediatric clinical trial. Crit Care Med 35:2615–2623
Mann EA, Baun MM, Meininger JC, Wade CE (2012) Comparison of mortality associated with sepsis in the burn, trauma, and general intensive care unit patient: a systematic review of the literature. Shock 37:4–16
D’Avignon LC, Hogan BK, Murray CK, Loo FL, Hospenthal DR et al (2010) Contribution of bacterial and viral infections to attributable mortality in patients with severe burns: an autopsy series. Burns 36:773–779
Siddiqui AR, Bernstein JM (2010) Chronic wound infection: facts and controversies. Clin Dermatol 28:519–526
Ong YS, Samuel M, Song C (2006) Meta-analysis of early excision of burns. Burns 32:145–150
Lavery LA, Fulmer J, Shebetka KA, Regulski M, Vayser D et al (2014) The efficacy and safety of Grafix((R)) for the treatment of chronic diabetic foot ulcers: results of a multi-centre, controlled, randomised, blinded, clinical trial. Int Wound J 11:554–560
Namdar T, Stollwerck PL, Stang FH, Siemers F, Mailander P et al (2010) Transdermal fluid loss in severely burned patients. Ger Med Sci 8: Doc28
Woodroof EA (2009) The search for an ideal temporary skin substitute: AWBAT. Eplasty 9:e10
Yannas IV, Burke JF (1980) Design of an artificial skin. I. Basic design principles. J Biomed Mater Res 14:65–81
Wang H, Pieper J, Peters F, van Blitterswijk CA, Lamme EN (2005) Synthetic scaffold morphology controls human dermal connective tissue formation. J Biomed Mater Res A 74:523–532
Suzuki S, Matsuda K, Isshiki N, Tamada Y, Ikada Y (1990) Experimental study of a newly developed bilayer artificial skin. Biomaterials 11:356–360
Hoyt LC (2007) Fibroblast Migration Mediated by the Composition of Tissue Engineered Scaffolds. Dissertation, Virginia Commonwealth University. http://scholarscompass.vcu.edu/etd_retro/164
Jensen PJ, Wheelock MJ (1996) The relationships among adhesion, stratification and differentiation in keratinocytes. Cell Death Differ 3:357–371
Eming SA, Krieg T, Davidson JM (2007) Inflammation in wound repair: molecular and cellular mechanisms. J Invest Dermatol 127:514–525
Benichou G, Yamada Y, Yun SH, Lin C, Fray M et al (2011) Immune recognition and rejection of allogeneic skin grafts. Immunotherapy 3:757–770
François B, Lucie G, Roxane P, François AA (2010) How to achieve early vascularization of tissue-engineered skin substitutes. In: C.K. S (ed) Advances in wound care. New Rochelle, Mary Ann Liebert, Inc. p 445–450
Chiu YC, Cheng MH, Engel H, Kao SW, Larson JC et al (2011) The role of pore size on vascularization and tissue remodeling in PEG hydrogels. Biomaterials 32:6045–6051
Lamme EN, de Vries HJ, van Veen H, Gabbiani G, Westerhof W et al (1996) Extracellular matrix characterization during healing of full-thickness wounds treated with a collagen/elastin dermal substitute shows improved skin regeneration in pigs. J Histochem Cytochem 44:1311–1322
Yildirimer L, Thanh NT, Seifalian AM (2012) Skin regeneration scaffolds: a multimodal bottom-up approach. Trends Biotechnol 30:638–648
Klingenberg JM, McFarland KL, Friedman AJ, Boyce ST, Aronow BJ et al (2010) Engineered human skin substitutes undergo large-scale genomic reprogramming and normal skin-like maturation after transplantation to athymic mice. J Invest Dermatol 130:587–601
Sander EA, Lynch KA, Boyce ST (2014) Development of the mechanical properties of engineered skin substitutes after grafting to full-thickness wounds. J Biomech Eng 136:051008
Darby IA, Hewitson TD (2007) Fibroblast differentiation in wound healing and fibrosis. In: Kwang WJ (ed) International review of cytology. Academic Press, New York, pp 143–179
Poon R, Nik SA, Ahn J, Slade L, Alman BA (2009) Beta-catenin and transforming growth factor beta have distinct roles regulating fibroblast cell motility and the induction of collagen lattice contraction. BMC Cell Biol 10:38
Parenteau-Bareil R, Gauvin R, Berthod F (2010) Collagen-based biomaterials for tissue engineering applications. Materials 3:1863–1887
Glowacki J, Mizuno S (2008) Collagen scaffolds for tissue engineering. Biopolymers 89:338–344
Sarkar SD, Farrugia BL, Dargaville TR, Dhara S (2013) Chitosan–collagen scaffolds with nano/microfibrous architecture for skin tissue engineering. J Biomed Mater Res, Part A 101:3482–3492
Keck M, Haluza D, Lumenta DB, Burjak S, Eisenbock B et al (2011) Construction of a multi-layer skin substitute: simultaneous cultivation of keratinocytes and preadipocytes on a dermal template. Burns 37:626–630
Bottcher-Haberzeth S, Biedermann T, Reichmann E (2010) Tissue engineering of skin. Burns 36:450–460
O’Brien FJ (2011) Biomaterials & scaffolds for tissue engineering. Mater Today 14:88–95
Keogh MB, O’Brien FJ, Daly JS (2010) Substrate stiffness and contractile behaviour modulate the functional maturation of osteoblasts on a collagen-GAG scaffold. Acta Biomater 6:4305–4313
Tierney CM, Haugh MG, Liedl J, Mulcahy F, Hayes B et al (2009) The effects of collagen concentration and crosslink density on the biological, structural and mechanical properties of collagen-GAG scaffolds for bone tissue engineering. J Mech Behav Biomed Mater 2:202–209
Haugh MG, Jaasma MJ, O’Brien FJ (2009) The effect of dehydrothermal treatment on the mechanical and structural properties of collagen-GAG scaffolds. J Biomed Mater Res A 89:363–369
Wang HM, Chou YT, Wen ZH, Wang ZR, Chen CH et al (2013) Novel biodegradable porous scaffold applied to skin regeneration. PLoS One 8:e56330
Filova E, Rampichova M, Handl M, Lytvynets A, Halouzka R et al (2007) Composite hyaluronate-type I collagen-fibrin scaffold in the therapy of osteochondral defects in miniature pigs. Physiol Res 56(Suppl 1):S5–s16
Han CM, Zhang LP, Sun JZ, Shi HF, Zhou J et al (2010) Application of collagen-chitosan/fibrin glue asymmetric scaffolds in skin tissue engineering. J Zhejiang Univ Sci B 11:524–530
Mohd Hilmi AB, Halim AS, Jaafar H, Asiah AB, Hassan A (2013) Chitosan dermal substitute and chitosan skin substitute contribute to accelerated full-thickness wound healing in irradiated rats. Biomed Res Int 2013:795458
Ayvazyan A, Morimoto N, Kanda N, Takemoto S, Kawai K et al (2011) Collagen-gelatin scaffold impregnated with bFGF accelerates palatal wound healing of palatal mucosa in dogs. J Surg Res 171:e247–e257
Morimoto N, Kakudo N, Valentin Notodihardjo P, Suzuki S, Kusumoto K (2014) Comparison of neovascularization in dermal substitutes seeded with autologous fibroblasts or impregnated with bFGF applied to diabetic foot ulcers using laser Doppler imaging. J Artif Organs 17:352–357
Rnjak-Kovacina J, Wise SG, Li Z, Maitz PK, Young CJ et al (2012) Electrospun synthetic human elastin:collagen composite scaffolds for dermal tissue engineering. Acta Biomater 8:3714–3722
Garg RK, Rennert RC, Duscher D, Sorkin M, Kosaraju R et al. (2014) Capillary Force Seeding of Hydrogels for Adipose-Derived Stem Cell Delivery in Wounds. Stem Cells Transl Med 3:1079–1089
Rustad KC, Wong VW, Sorkin M, Glotzbach JP, Major MR et al (2012) Enhancement of mesenchymal stem cell angiogenic capacity and stemness by a biomimetic hydrogel scaffold. Biomaterials 33:80–90
Wong VW, Rustad KC, Galvez MG, Neofytou E, Glotzbach JP et al (2011) Engineered pullulan-collagen composite dermal hydrogels improve early cutaneous wound healing. Tissue Eng Part A 17:631–644
Gaspar A, Moldovan L, Constantin D, Stanciuc AM, Sarbu Boeti PM et al (2011) Collagen-based scaffolds for skin tissue engineering. J Med Life 4:172–177
Lin HY, Peng CW, Wu WW (2014) Fibrous hydrogel scaffolds with cells embedded in the fibers as a potential tissue scaffold for skin repair. J Mater Sci Mater Med 25:259–269
Damodaran G, Tiong WH, Collighan R, Griffin M, Navsaria H et al (2013) In vivo effects of tailored laminin-332 alpha3 conjugated scaffolds enhances wound healing: a histomorphometric analysis. J Biomed Mater Res A 101:2788–2795
Lu H, Oh HH, Kawazoe N, Yamagishi K, Chen G (2012) PLLA–collagen and PLLA–gelatin hybrid scaffolds with funnel-like porous structure for skin tissue engineering. Sci Technol Adv Mater 13:064210
You C, Wang X, Zheng Y, Han C (2013) Three types of dermal grafts in rats: the importance of mechanical property and structural design. Biomed Eng Online 12:125
Cui W, Zhu X, Yang Y, Li X, Jin Y (2009) Evaluation of electrospun fibrous scaffolds of poly(dl-lactide) and poly(ethylene glycol) for skin tissue engineering. Mater Sci Eng, C 29:1869–1876
Sargeant TD, Desai AP, Banerjee S, Agawu A, Stopek JB (2012) An in situ forming collagen-PEG hydrogel for tissue regeneration. Acta Biomater 8:124–132
Gautam S, Chou CF, Dinda AK, Potdar PD, Mishra NC (2014) Surface modification of nanofibrous polycaprolactone/gelatin composite scaffold by collagen type I grafting for skin tissue engineering. Mater Sci Eng C Mater Biol Appl 34:402–409
Stuart K, Panitch A (2008) Influence of chondroitin sulfate on collagen gel structure and mechanical properties at physiologically relevant levels. Biopolymers 89:841–851
McFadden TM, Duffy GP, Allen AB, Stevens HY, Schwarzmaier SM et al (2013) The delayed addition of human mesenchymal stem cells to pre-formed endothelial cell networks results in functional vascularization of a collagen–glycosaminoglycan scaffold in vivo. Acta Biomater 9:9303–9316
Duffy GP, McFadden TM, Byrne EM, Gill SL, Farrell E et al (2011) Towards in vitro vascularisation of collagen-GAG scaffolds. Eur Cell Mater 21:15–30
Corin KA, Gibson LJ (2010) Cell contraction forces in scaffolds with varying pore size and cell density. Biomaterials 31:4835–4845
Nimni ME, Cheung D, Strates B, Kodama M, Sheikh K (1987) Chemically modified collagen: a natural biomaterial for tissue replacement. J Biomed Mater Res 21:741–771
Kamel RA, Ong JF, Eriksson E, Junker JP, Caterson EJ (2013) Tissue engineering of skin. J Am Coll Surg 217:533–555
Maheshwari G, Brown G, Lauffenburger DA, Wells A, Griffith LG (2000) Cell adhesion and motility depend on nanoscale RGD clustering. J Cell Sci 113(Pt 10):1677–1686
Sethi KK, Yannas IV, Mudera V, Eastwood M, McFarland C et al (2002) Evidence for sequential utilization of fibronectin, vitronectin, and collagen during fibroblast-mediated collagen contraction. Wound Repair Regen 10:397–408
Clark RA, Lin F, Greiling D, An J, Couchman JR (2004) Fibroblast invasive migration into fibronectin/fibrin gels requires a previously uncharacterized dermatan sulfate-CD44 proteoglycan. J Invest Dermatol 122:266–277
Bielefeld KA, Amini-Nik S, Whetstone H, Poon R, Youn A et al (2011) Fibronectin and beta-catenin act in a regulatory loop in dermal fibroblasts to modulate cutaneous healing. J Biol Chem 286:27687–27697
Bhattarai N, Gunn J, Zhang M (2010) Chitosan-based hydrogels for controlled, localized drug delivery. Adv Drug Deliv Rev 62:83–99
Koide SS (1998) Chitin-chitosan: properties, benefits and risks. Nutr Res 18:1091–1101
Hayashi Y, Yamada S, Yanagi Guchi K, Koyama Z, Ikeda T (2012) Chitosan and fish collagen as biomaterials for regenerative medicine. Adv Food Nutr Res 65:107–120
Hilmi AB, Halim AS, Hassan A, Lim CK, Noorsal K et al (2013) In vitro characterization of a chitosan skin regenerating template as a scaffold for cells cultivation. Springerplus 2:79
Shevchenko RV, Eeman M, Rowshanravan B, Allan IU, Savina IN et al (2014) The in vitro characterization of a gelatin scaffold, prepared by cryogelation and assessed in vivo as a dermal replacement in wound repair. Acta Biomater 10:3156–3166
Kang H-W, Tabata Y, Ikada Y (1999) Fabrication of porous gelatin scaffolds for tissue engineering. Biomaterials 20:1339–1344
Takemoto S, Morimoto N, Kimura Y, Taira T, Kitagawa T et al (2008) Preparation of collagen/gelatin sponge scaffold for sustained release of bFGF. Tissue Eng Part A 14:1629–1638
Rnjak J, Wise SG, Mithieux SM, Weiss AS (2011) Severe burn injuries and the role of elastin in the design of dermal substitutes. Tissue Eng Part B Rev 17:81–91
Rnjak-Kovacina J, Wise SG, Li Z, Maitz PKM, Young CJ et al (2011) Tailoring the porosity and pore size of electrospun synthetic human elastin scaffolds for dermal tissue engineering. Biomaterials 32:6729–6736
Almine JF, Bax DV, Mithieux SM, Nivison-Smith L, Rnjak J et al (2010) Elastin-based materials. Chem Soc Rev 39:3371–3379
Jones I, Currie L, Martin R (2002) A guide to biological skin substitutes. Br J Plast Surg 55:185–193
Min JH, Yun IS, Lew DH, Roh TS, Lee WJ (2014) The use of matriderm and autologous skin graft in the treatment of full thickness skin defects. Arch Plast Surg 41:330–336
Haslik W, Kamolz LP, Nathschlager G, Andel H, Meissl G et al (2007) First experiences with the collagen-elastin matrix Matriderm as a dermal substitute in severe burn injuries of the hand. Burns 33:364–368
Nicholas MN, Jeschke MG, Amini-Nik S (2016) Cellularized Bilayer Pullulan-gelatin Hydrogel for Skin Regeneration. Tissue Eng Part A. doi: 10.1089/ten.tea.2015.0536
Lee KY, Mooney DJ (2012) Alginate: properties and biomedical applications. Prog Polym Sci 37:106–126
Smith AM, Hunt NC, Shelton RM, Birdi G, Grover LM (2012) Alginate hydrogel has a negative impact on in vitro collagen 1 deposition by fibroblasts. Biomacromolecules 13:4032–4038
Leng L, McAllister A, Zhang B, Radisic M, Gunther A (2012) Mosaic hydrogels: one-step formation of multiscale soft materials. Adv Mater 24:3650–3658
Fang Y, Al-Assaf S, Phillips GO, Nishinari K, Funami T et al (2008) Binding behavior of calcium to polyuronates: comparison of pectin with alginate. Carbohydr Polym 72:334–341
Behrens DT, Villone D, Koch M, Brunner G, Sorokin L et al (2012) The epidermal basement membrane is a composite of separate laminin- or collagen IV-containing networks connected by aggregated perlecan, but not by nidogens. J Biol Chem 287:18700–18709
Masuda R, Mochizuki M, Hozumi K, Takeda A, Uchinuma E et al (2009) A novel cell-adhesive scaffold material for delivering keratinocytes reduces granulation tissue in dermal wounds. Wound Repair Regen 17:127–135
Halim AS, Khoo TL, Mohd Yussof SJ (2010) Biologic and synthetic skin substitutes: an overview. Indian J Plast Surg 43:S23–S28
Park GE, Pattison MA, Park K, Webster TJ (2005) Accelerated chondrocyte functions on NaOH-treated PLGA scaffolds. Biomaterials 26:3075–3082
Lou T, Leung M, Wang X, Chang JY, Tsao CT et al (2014) Bi-layer scaffold of chitosan/PCL-nanofibrous mat and PLLA-microporous disc for skin tissue engineering. J Biomed Nanotechnol 10:1105–1113
Smith LL, Niziolek PJ, Haberstroh KM, Nauman EA, Webster TJ (2007) Decreased fibroblast and increased osteoblast adhesion on nanostructured NaOH-etched PLGA scaffolds. Int J Nanomed 2:383–388
Powell HM, Boyce ST (2009) Engineered human skin fabricated using electrospun collagen-PCL blends: morphogenesis and mechanical properties. Tissue Eng Part A 15:2177–2187
van der Veen VC, van der Wal MB, van Leeuwen MC, Ulrich MM, Middelkoop E (2010) Biological background of dermal substitutes. Burns 36:305–321
Akasaka Y, Ono I, Tominaga A, Ishikawa Y, Ito K et al (2007) Basic fibroblast growth factor in an artificial dermis promotes apoptosis and inhibits expression of alpha-smooth muscle actin, leading to reduction of wound contraction. Wound Repair Regen 15:378–389
Inoue S, Kijima H, Kidokoro M, Tanaka M, Suzuki Y et al (2009) The effectiveness of basic fibroblast growth factor in fibrin-based cultured skin substitute in vivo. J Burn Care Res 30:514–519
Tsuji-Saso Y, Kawazoe T, Morimoto N, Tabata Y, Taira T et al (2007) Incorporation of basic fibroblast growth factor into preconfluent cultured skin substitute to accelerate neovascularisation and skin reconstruction after transplantation. Scand J Plast Reconstr Surg Hand Surg 41:228–235
Spyrou GE, Naylor IL (2002) The effect of basic fibroblast growth factor on scarring. Br J Plast Surg 55:275–282
Bodnar RJ (2013) Epidermal growth factor and epidermal growth factor receptor: the Yin and Yang in the treatment of cutaneous wounds and cancer. Adv Wound Care (New Rochelle) 2:24–29
Kuroyanagi M, Yamamoto A, Shimizu N, Ishihara E, Ohno H et al (2014) Development of cultured dermal substitute composed of hyaluronic acid and collagen spongy sheet containing fibroblasts and epidermal growth factor. J Biomater Sci Polym Ed 25:1133–1143
Yamamoto A, Shimizu N, Kuroyanagi Y (2013) Potential of wound dressing composed of hyaluronic acid containing epidermal growth factor to enhance cytokine production by fibroblasts. J Artif Organs 16:489–494
Kondo S, Kuroyanagi Y (2012) Development of a wound dressing composed of hyaluronic acid and collagen sponge with epidermal growth factor. J Biomater Sci Polym Ed 23:629–643
Matsumoto Y, Kuroyanagi Y (2010) Development of a wound dressing composed of hyaluronic acid sponge containing arginine and epidermal growth factor. J Biomater Sci Polym Ed 21:715–726
Biselli-Chicote PM, Oliveira AR, Pavarino EC, Goloni-Bertollo EM (2012) VEGF gene alternative splicing: pro- and anti-angiogenic isoforms in cancer. J Cancer Res Clin Oncol 138:363–370
Caldwell RB, Bartoli M, Behzadian MA, El-Remessy AE, Al-Shabrawey M et al (2005) Vascular endothelial growth factor and diabetic retinopathy: role of oxidative stress. Curr Drug Targets 6:511–524
Lohmeyer JA, Liu F, Kruger S, Lindenmaier W, Siemers F et al (2011) Use of gene-modified keratinocytes and fibroblasts to enhance regeneration in a full skin defect. Langenbecks Arch Surg 396:543–550
Xie WG, Lindenmaier W, Gryzybowski S, Machens HG (2005) Influence of vascular endothelial growth factor gene modification on skin substitute grafted on nude mice. Zhonghua Shao Shang Za Zhi 21:203–206
Wilgus TA, Ferreira AM, Oberyszyn TM, Bergdall VK, DiPietro LA (2008) Regulation of scar formation by vascular endothelial growth factor. Lab Investig J Tech Methods Pathol 88:579–590
Maurer B, Distler A, Suliman YA, Gay RE, Michel BA et al (2014) Vascular endothelial growth factor aggravates fibrosis and vasculopathy in experimental models of systemic sclerosis. Ann Rheum Dis 73:1880–1887
Roberts AB, Flanders KC, Heine UI, Jakowlew S, Kondaiah P et al (1990) Transforming growth factor-beta: multifunctional regulator of differentiation and development. Philos Trans R Soc Lond B Biol Sci 327:145–154
Ferguson MW, O’Kane S (2004) Scar-free healing: from embryonic mechanisms to adult therapeutic intervention. Philos Trans R Soc Lond B Biol Sci 359:839–850
Pandit A, Ashar R, Feldman D (1999) The effect of TGF-β delivered through a collagen scaffold on wound healing. J Invest Surg 12:89–100
Penn JW, Grobbelaar AO, Rolfe KJ (2012) The role of the TGF-β family in wound healing, burns and scarring: a review. Int J Burns Trauma 2:18–28
Kim MS, Song HJ, Lee SH, Lee CK (2014) Comparative study of various growth factors and cytokines on type I collagen and hyaluronan production in human dermal fibroblasts. J Cosmet Dermatol 13:44–51
Sun W, Lin H, Xie H, Chen B, Zhao W et al (2007) Collagen membranes loaded with collagen-binding human PDGF-BB accelerate wound healing in a rabbit dermal ischemic ulcer model. Growth Factors 25:309–318
Niessen FB, Andriessen MP, Schalkwijk J, Visser L, Timens W (2001) Keratinocyte-derived growth factors play a role in the formation of hypertrophic scars. J Pathol 194:207–216
Nolte SV, Xu W, Rennekampff HO, Rodemann HP (2008) Diversity of fibroblasts–a review on implications for skin tissue engineering. Cells Tissues Organs 187:165–176
Shamis Y, Silva EA, Hewitt KJ, Brudno Y, Levenberg S et al (2013) Fibroblasts derived from human pluripotent stem cells activate angiogenic responses in vitro and in vivo. PLoS One 8:e83755
Kendall RT, Feghali-Bostwick CA (2014) Fibroblasts in fibrosis: novel roles and mediators. Front Pharmacol 5:123
Andriani F, Margulis A, Lin N, Griffey S, Garlick JA (2003) Analysis of microenvironmental factors contributing to basement membrane assembly and normalized epidermal phenotype. J Invest Dermatol 120:923–931
Benny P, Badowski C, Lane B, Raghunath M (2015) Making More Matrix: Enhancing the deposition of dermal-epidermal junction components in vitro and accelerating organotypic skin culture development, using macromolecular crowding. Tissue Eng Part A 21:183–192
Niessen CM (2007) Tight Junctions/Adherens Junctions: basic Structure and Function. J Investig Dermatol 127:2525–2532
Pastar I, Stojadinovic O, Yin NC, Ramirez H, Nusbaum AG et al (2014) Epithelialization in wound healing: a comprehensive review. Adv Wound Care (New Rochelle) 3:445–464
Lamouille S, Xu J, Derynck R (2014) Molecular mechanisms of epithelial-mesenchymal transition. Nat Rev Mol Cell Biol 15:178–196
Nguyen BP, Ryan MC, Gil SG, Carter WG (2000) Deposition of laminin 5 in epidermal wounds regulates integrin signaling and adhesion. Curr Opin Cell Biol 12:554–562
Falanga V, Butmarc J, Cha J, Yufit T, Carson P (2007) Migration of the epidermal over the dermal component (epiboly) in a bilayered bioengineered skin construct. Tissue Eng 13:21–28
Eming SA, Yarmush ML, Morgan JR (1996) Enhanced function of cultured epithelium by genetic modification: cell-based synthesis and delivery of growth factors. Biotechnol Bioeng 52:15–23
Ghahary A, Ghaffari A (2007) Role of keratinocyte-fibroblast cross-talk in development of hypertrophic scar. Wound Repair Regen 15(Suppl 1):S46–S53
Wojtowicz AM, Oliveira S, Carlson MW, Zawadzka A, Rousseau CF et al (2014) The importance of both fibroblasts and keratinocytes in a bilayered living cellular construct used in wound healing. Wound Repair Regen 22:246–255
Maas-Szabowski N, Szabowski A, Stark HJ, Andrecht S, Kolbus A et al (2001) Organotypic cocultures with genetically modified mouse fibroblasts as a tool to dissect molecular mechanisms regulating keratinocyte growth and differentiation. J Invest Dermatol 116:816–820
Barrientos S, Stojadinovic O, Golinko MS, Brem H, Tomic-Canic M (2008) Growth factors and cytokines in wound healing. Wound Repair Regen 16:585–601
Borowiec A-S, Delcourt P, Dewailly E, Bidaux G (2013) Optimal Differentiation of In Vitro Keratinocytes Requires Multifactorial External Control. PLoS One 8:e77507
Falanga V, Sabolinski M (1999) A bilayered living skin construct (APLIGRAF) accelerates complete closure of hard-to-heal venous ulcers. Wound Repair Regen 7:201–207
Dinh TL, Veves A (2006) The efficacy of Apligraf in the treatment of diabetic foot ulcers. Plast Reconstr Surg 117:152S–157S (discussion 158S–159S)
Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F et al (2006) Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 8:315–317
Sasaki M, Abe R, Fujita Y, Ando S, Inokuma D et al (2008) Mesenchymal stem cells are recruited into wounded skin and contribute to wound repair by transdifferentiation into multiple skin cell type. J Immunol 180:2581–2587
Alt E, Yan Y, Gehmert S, Song YH, Altman A et al (2011) Fibroblasts share mesenchymal phenotypes with stem cells, but lack their differentiation and colony-forming potential. Biol Cell 103:197–208
Han Y, Chai J, Sun T, Li D, Tao R (2011) Differentiation of human umbilical cord mesenchymal stem cells into dermal fibroblasts in vitro. Biochem Biophys Res Commun 413:561–565
Fathke C, Wilson L, Hutter J, Kapoor V, Smith A et al (2004) Contribution of bone marrow-derived cells to skin: collagen deposition and wound repair. Stem Cells 22:812–822
Deng W, Han Q, Liao L, Li C, Ge W et al (2005) Engrafted bone marrow-derived flk-(1+) mesenchymal stem cells regenerate skin tissue. Tissue Eng 11:110–119
Basiouny HS, Salama NM, Maadawi ZM, Farag EA (2013) Effect of bone marrow derived mesenchymal stem cells on healing of induced full-thickness skin wounds in albino rat. Int J Stem Cells 6:12–25
Badiavas EV, Falanga V (2003) Treatment of chronic wounds with bone marrow-derived cells. Arch Dermatol 139:510–516
Kern S, Eichler H, Stoeve J, Kluter H, Bieback K (2006) Comparative analysis of mesenchymal stem cells from bone marrow, umbilical cord blood, or adipose tissue. Stem Cells 24:1294–1301
Souza CM, Mesquita LA, Souza D, Irioda AC, Francisco JC et al (2014) Regeneration of skin tissue promoted by mesenchymal stem cells seeded in nanostructured membrane. Transplant Proc 46:1882–1886
Mizuno H, Nambu M (2011) Adipose-derived stem cells for skin regeneration. Methods Mol Biol 702:453–459
Meruane MA, Rojas M, Marcelain K (2012) The use of adipose tissue-derived stem cells within a dermal substitute improves skin regeneration by increasing neoangiogenesis and collagen synthesis. Plast Reconstr Surg 130:53–63
Schneider RK, Pullen A, Kramann R, Bornemann J, Knuchel R et al (2010) Long-term survival and characterisation of human umbilical cord-derived mesenchymal stem cells on dermal equivalents. Differentiation 79:182–193
Kim DW, Staples M, Shinozuka K, Pantcheva P, Kang SD et al (2013) Wharton’s Jelly-derived mesenchymal stem cells: phenotypic characterization and optimizing their therapeutic potential for clinical applications. Int J Mol Sci 14:11692–11712
Arno AI, Amini-Nik S, Blit PH, Al-Shehab M, Belo C et al (2014) Human Wharton’s jelly-mesenchymal stem cells promote skin wound healing through paracrine signaling. Stem Cell Res Ther 5:28
Nicoletti G, Brenta F, Bleve M, Pellegatta T, Malovini A et al (2015) Long-term in vivo assessment of bioengineered skin substitutes: a clinical study. J Tissue Eng Regen Med 9:460–468
Hachiya A, Sriwiriyanont P, Kaiho E, Kitahara T, Takema Y et al (2005) An in vivo mouse model of human skin substitute containing spontaneously sorted melanocytes demonstrates physiological changes after UVB irradiation. J Invest Dermatol 125:364–372
Bielefeld KA, Amini-Nik S, Alman BA (2013) Cutaneous wound healing: recruiting developmental pathways for regeneration. Cell Mol Life Sci 70:2059–2081
Amini-Nik S, Glancy D, Boimer C, Whetstone H, Keller C et al (2011) Pax7 expressing cells contribute to dermal wound repair, regulating scar size through a beta-catenin mediated process. Stem Cells 29:1371–1379
Amini-Nik S, Cambridge E, Yu W, Guo A, Whetstone H et al (2014) beta-Catenin-regulated myeloid cell adhesion and migration determine wound healing. J Clin Invest 124:2599–2610
Bechetoille N, Vachon H, Gaydon A, Boher A, Fontaine T et al (2011) A new organotypic model containing dermal-type macrophages. Exp Dermatol 20:1035–1037
Koh TJ, DiPietro LA (2011) Inflammation and wound healing: the role of the macrophage. Expert Rev Mol Med 13:e23
Liu Y, Luo H, Wang X, Takemura A, Fang YR et al (2013) In vitro construction of scaffold-free bilayered tissue-engineered skin containing capillary networks. Biomed Res Int 2013:561410
Zhang X, Yang J, Li Y, Liu S, Long K et al (2011) Functional neovascularization in tissue engineering with porcine acellular dermal matrix and human umbilical vein endothelial cells. Tissue Eng Part C Methods 17:423–433
Marino D, Luginbuhl J, Scola S, Meuli M, Reichmann E (2014) Bioengineering dermo-epidermal skin grafts with blood and lymphatic capillaries. Sci Transl Med 6:221ra214
Sriwiriyanont P, Lynch KA, Maier EA, Hahn JM, Supp DM et al (2012) Morphogenesis of chimeric hair follicles in engineered skin substitutes with human keratinocytes and murine dermal papilla cells. Exp Dermatol 21:783–785
Sriwiriyanont P, Lynch KA, McFarland KL, Supp DM, Boyce ST (2013) Characterization of hair follicle development in engineered skin substitutes. PLoS One 8:e65664
Moiemen N, Yarrow J, Hodgson E, Constantinides J, Chipp E et al (2011) Long-term clinical and histological analysis of Integra dermal regeneration template. Plast Reconstr Surg 127:1149–1154
Huang S, Xu Y, Wu C, Sha D, Fu X (2010) In vitro constitution and in vivo implantation of engineered skin constructs with sweat glands. Biomaterials 31:5520–5525
Sunami H, Yokota I, Igarashi Y (2014) Influence of the pattern size of micropatterned scaffolds on cell morphology, proliferation, migration and F-actin expression. Biomater Sci 2:399–409
Phipps MC, Clem WC, Grunda JM, Clines GA, Bellis SL (2012) Increasing the pore sizes of bone-mimetic electrospun scaffolds comprised of polycaprolactone, collagen I and hydroxyapatite to enhance cell infiltration. Biomaterials 33:524–534
Lien SM, Ko LY, Huang TJ (2009) Effect of pore size on ECM secretion and cell growth in gelatin scaffold for articular cartilage tissue engineering. Acta Biomater 5:670–679
Joshi VS, Lei NY, Walthers CM, Wu B, Dunn JC (2013) Macroporosity enhances vascularization of electrospun scaffolds. J Surg Res 183:18–26
Annabi N, Nichol JW, Zhong X, Ji C, Koshy S et al (2010) Controlling the porosity and microarchitecture of hydrogels for tissue engineering. Tissue Eng Part B, Rev 16:371–383
Huss FR, Nyman E, Gustafson CJ, Gisselfalt K, Liljensten E et al (2008) Characterization of a new degradable polymer scaffold for regeneration of the dermis: in vitro and in vivo human studies. Organogenesis 4:195–200
Gong Y, Zhou Q, Gao C, Shen J (2007) In vitro and in vivo degradability and cytocompatibility of poly(l-lactic acid) scaffold fabricated by a gelatin particle leaching method. Acta Biomater 3:531–540
Vlierberghe SV, Cnudde V, Dubruel P, Masschaele B, Cosijns A et al (2007) Porous gelatin hydrogels: 1. Cryogenic formation and structure analysis. Biomacromolecules 8:331–337
O’Brien FJ, Harley BA, Yannas IV, Gibson LJ (2005) The effect of pore size on cell adhesion in collagen-GAG scaffolds. Biomaterials 26:433–441
Ho MH, Kuo PY, Hsieh HJ, Hsien TY, Hou LT et al (2004) Preparation of porous scaffolds by using freeze-extraction and freeze-gelation methods. Biomaterials 25:129–138
Hao R, Wang D, Yao A, Huang W (2011) Preparation and characterization of β-TCP/CS scaffolds by freeze-extraction and freeze-gelation. J Wuhan Univer Technol-Mater Sci Ed 26:371–375
Atala A, Lanza RP (2001) Methods of tissue engineering. Academic Press, San Diego
Shih HH, Lee KR, Lai HM, Tsai CC, Chang YC (2004) Method of making porous biodegradable polymers. US Patent 6673286
Kang HG, Lee SB, Lee YM (2005) Novel preparative method for porous hydrogels using overrun process. Polym Int 54:537–543
Kang HG, Kim SY, Lee YM (2006) Novel porous gelatin scaffolds by overrun/particle leaching process for tissue engineering applications. J Biomed Mater Res B Appl Biomater 79:388–397
Zhang Y, Ouyang H, Lim CT, Ramakrishna S, Huang ZM (2005) Electrospinning of gelatin fibers and gelatin/PCL composite fibrous scaffolds. J Biomed Mater Res B Appl Biomater 72:156–165
Yoshimoto H, Shin YM, Terai H, Vacanti JP (2003) A biodegradable nanofiber scaffold by electrospinning and its potential for bone tissue engineering. Biomaterials 24:2077–2082
Heydarkhan-Hagvall S, Schenke-Layland K, Dhanasopon AP, Rofail F, Smith H et al (2008) Three-dimensional electrospun ECM-based hybrid scaffolds for cardiovascular tissue engineering. Biomaterials 29:2907–2914
Li WJ, Laurencin CT, Caterson EJ, Tuan RS, Ko FK (2002) Electrospun nanofibrous structure: a novel scaffold for tissue engineering. J Biomed Mater Res 60:613–621
Boland ED, Matthews JA, Pawlowski KJ, Simpson DG, Wnek GE et al (2004) Electrospinning collagen and elastin: preliminary vascular tissue engineering. Front Biosci 9:1422–1432
Verhulsel M, Vignes M, Descroix S, Malaquin L, Vignjevic DM et al (2014) A review of microfabrication and hydrogel engineering for micro-organs on chips. Biomaterials 35:1816–1832
Yeh J, Ling Y, Karp JM, Gantz J, Chandawarkar A et al (2006) Micromolding of shape-controlled, harvestable cell-laden hydrogels. Biomaterials 27:5391–5398
Chia HN, Wu BM (2015) Recent advances in 3D printing of biomaterials. J Biol Eng 9:4
Koch L, Kuhn S, Sorg H, Gruene M, Schlie S et al (2010) Laser printing of skin cells and human stem cells. Tissue Eng Part C Methods 16:847–854
Michael S, Sorg H, Peck C-T, Koch L, Deiwick A et al (2013) Tissue Engineered Skin Substitutes Created by Laser-Assisted Bioprinting Form Skin-Like Structures in the Dorsal Skin Fold Chamber in Mice. PLoS One 8:e57741
Leng L. BQ, Amini-Nik S, Jeschke M, Guenther A (2013) Skin printer: microfluidic approach for skin regeneration and wound dressing. US Prov. Patent Application (61817860)
Wüst S, Müller R, Hofmann S (2011) Controlled positioning of cells in biomaterials—approaches towards 3D tissue printing. J Funct Biomater 2:119–154
Dunn JC, Chan WY, Cristini V, Kim JS, Lowengrub J et al (2006) Analysis of cell growth in three-dimensional scaffolds. Tissue Eng 12:705–716
Fuchs E (2015) Cell biology: more than skin deep. J Cell Biol 209:629–631
Hennink WE, van Nostrum CF (2002) Novel crosslinking methods to design hydrogels. Adv Drug Deliv Rev 54:13–36
Silva SS, Santos MI, Coutinho OP, Mano JF, Reis RL (2005) Physical properties and biocompatibility of chitosan/soy blended membranes. J Mater Sci Mater Med 16:575–579
Gough JE, Scotchford CA, Downes S (2002) Cytotoxicity of glutaraldehyde crosslinked collagen/poly(vinyl alcohol) films is by the mechanism of apoptosis. J Biomed Mater Res 61:121–130
Sung HW, Huang RN, Huang LL, Tsai CC (1999) In vitro evaluation of cytotoxicity of a naturally occurring cross-linking reagent for biological tissue fixation. J Biomater Sci Polym Ed 10:63–78
Lai JY (2012) Biocompatibility of genipin and glutaraldehyde cross-linked chitosan materials in the anterior chamber of the eye. Int J Mol Sci 13:10970–10985
Haugh MG, Murphy CM, McKiernan RC, Altenbuchner C, O’Brien FJ (2011) Crosslinking and mechanical properties significantly influence cell attachment, proliferation, and migration within collagen glycosaminoglycan scaffolds. Tissue Eng Part A 17:1201–1208
Mironi-Harpaz I, Wang DY, Venkatraman S, Seliktar D (2012) Photopolymerization of cell-encapsulating hydrogels: crosslinking efficiency versus cytotoxicity. Acta Biomater 8:1838–1848
Ward JH, Peppas NA (2001) Preparation of controlled release systems by free-radical UV polymerizations in the presence of a drug. J Control Release 71:183–192
Park JS, Chu JS, Tsou AD, Diop R, Tang Z et al (2011) The effect of matrix stiffness on the differentiation of mesenchymal stem cells in response to TGF-β. Biomaterials 32:3921–3930
Engler AJ, Sen S, Sweeney HL, Discher DE (2006) Matrix elasticity directs stem cell lineage specification. Cell 126:677–689
Humphrey JD, Dufresne ER, Schwartz MA (2014) Mechanotransduction and extracellular matrix homeostasis. Nat Rev Mol Cell Biol 15:802–812
Okay O (2010) General Properties of Hydrogels. In: Gerlach G, Arndt K-F (eds) Hydrogel sensors and actuators. Springer, Berlin, Heidelberg, pp 1–14
Kirchmajer DM, Watson CA, Ranson M, Mih Panhuis (2013) Gelapin, a degradable genipin cross-linked gelatin hydrogel. RSC Adv 3:1073–1081
Orakdogen N, Okay O (2006) Correlation between crosslinking efficiency and spatial inhomogeneity in poly(acrylamide) hydrogels. Polym Bull 57:631–641
Missirlis D, Spatz JP (2013) Combined effects of PEG hydrogel elasticity and cell-adhesive coating on fibroblast adhesion and persistent migration. Biomacromolecules 15:195–205
Kim BM, Suzuki S, Nishimura Y, Um SC, Morota K et al (1999) Cellular artificial skin substitute produced by short period simultaneous culture of fibroblasts and keratinocytes. Br J Plast Surg 52:573–578
Vitacolonna M, Belharazem D, Hohenberger P, Roessner E (2015) Effect of dynamic seeding methods on the distribution of fibroblasts within human acellular dermis. Cell Tissue Bank 16:605–614
Godbey WT, Hindy SB, Sherman ME, Atala A (2004) A novel use of centrifugal force for cell seeding into porous scaffolds. Biomaterials 25:2799–2805
Killat J, Reimers K, Choi CY, Jahn S, Vogt PM et al (2013) Cultivation of keratinocytes and fibroblasts in a three-dimensional bovine collagen-elastin matrix (Matriderm(R)) and application for full thickness wound coverage in vivo. Int J Mol Sci 14:14460–14474
Vitacolonna M, Belharazem D, Hohenberger P, Roessner ED (2013) Effect of static seeding methods on the distribution of fibroblasts within human acellular dermis. Biomed Eng Online 12:55
Erickson IE, Kestle SR, Zellars KH, Farrell MJ, Kim M et al (2012) High mesenchymal stem cell seeding densities in hyaluronic acid hydrogels produce engineered cartilage with native tissue properties. Acta Biomater 8:3027–3034
Helmedag MJ, Weinandy S, Marquardt Y, Baron JM, Pallua N et al (2015) The effects of constant flow bioreactor cultivation and keratinocyte seeding densities on prevascularized organotypic skin grafts based on a fibrin scaffold. Tissue Eng Part A 21:343–352
Mohd Hilmi AB, Hassan A, Halim AS (2015) A bilayer engineered skin substitute for wound repair in an irradiation-impeded healing model on rat. Adv Wound Care 4:312–320
Hartwig B, Borm B, Schneider H, Arin MJ, Kirfel G et al (2007) Laminin-5-deficient human keratinocytes: defective adhesion results in a saltatory and inefficient mode of migration. Exp Cell Res 313:1575–1587
Koch L, Deiwick A, Schlie S, Michael S, Gruene M et al (2012) Skin tissue generation by laser cell printing. Biotechnol Bioeng 109:1855–1863
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nicholas, M.N., Jeschke, M.G. & Amini-Nik, S. Methodologies in creating skin substitutes. Cell. Mol. Life Sci. 73, 3453–3472 (2016). https://doi.org/10.1007/s00018-016-2252-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00018-016-2252-8