Abstract
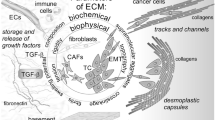
Cancer cells evolve in the tumor microenvironment (TME) by the acquisition of characteristics that allow them to initiate their passage through a series of events that constitute the metastatic cascade. For this purpose, tumor cells maintain a crosstalk with TME non-neoplastic cells transforming them into their allies. “Corrupted” cells such as cancer-associated fibroblasts (CAFs), tumor-associated macrophages (TAMs), and tumor-associated neutrophils (TANs) as well as neoplastic cells express and secrete matrix metalloproteinases (MMPs). Moreover, TME metabolic conditions such as hypoxia and acidification induce MMPs’ synthesis in both cancer and stromal cells. MMPs’ participation in TME consists in promoting events, for example, epithelial-mesenchymal transition (EMT), apoptosis resistance, angiogenesis, and lymphangiogenesis. MMPs also facilitate tumor cell migration through the basement membrane (BM) and extracellular matrix (ECM). The aim of the present chapter is to discuss MMPs’ contribution to the evolution of cancer cells, their cellular origin, and their influence in the main processes that take place in the TME.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Acidosis
- Adipocyte
- Angiogenesis
- CAFs
- EMT
- Hypoxia
- Lymphangiogenesis
- Mast cells
- Metastasis
- MMPs
- TAMs
- TANs
- TME
- TIMPs
- “Warburg effect”
5.1 Introduction
Neoplastic cells from solid tumors are the consequence of a dynamic evolutionary process in which cells acquire characteristics that allow them to survive in a stressful microenvironment until they detach from the primary tumor and disseminate to create a metastatic colony [1]. Moreover, tumor cells at the metastatic site face a new tissue microenvironment in which they must develop strategies to subsist. Thus, to ensure the evolution of cancer cells, a complex interplay among neoplastic cells and the surrounding microenvironment is established, transforming this niche into their own tumor microenvironment (TME) [2]. Molecules, such as growth factors, chemokines, cytokines, structural and non-structural extracellular matrix (ECM) proteins, and basement membrane (BM) components, as well as different types of cells are part of the TME [3]. Likewise, changes in TME metabolic circumstances such as nutrient decrease and hypoxic and acidic conditions drive tumor cells’ development [1]. Moreover, epithelial-mesenchymal transition (EMT), anoikis (apoptosis resistance), angiogenesis, and lymphangiogenesis are processes that take place in the TME during cancer progression. Furthermore, the TME from the primary tumor participates in the preparation of the pre-metastatic niche in a distant tissue [4].
The matrix metalloproteinases (MMPs) are TME proteins with an important participation in cancer evolution. These enzymes can modify several BM and ECM elements; they also release and activate growth factors, cytoskeletal proteins, chemokines, adhesion molecules, and cytokines [5]. Furthermore, MMPs are not only released to the extracellular medium but are also located in different cell organelles such as mitochondria, nucleus, cell membrane, cytoplasmic vesicles, or specific granules [6]. Due to the functions and ubiquity of MMPs, they participate in all cancer progression steps, and therefore, they are considered as prognostic markers and therapeutic targets.
Because of the relevant role played by MMPs in cancer, the aim of this chapter is to review how MMPs contribute to tumor cells’ preparation in the TME to continue with the next steps of the metastatic process. Particularly, this chapter points out the interaction between TME biochemical conditions and MMPs’ expression, the processes that take place in the TME in which MMPs are involved, and the association between different TME non-neoplastic cells and MMPs’ functions.
5.2 The Matrix Metalloproteinases (MMPs)
5.2.1 MMPs’ Basic Molecular Structure
MMPs are endopeptidases that depend on zinc and calcium ions for their enzymatic activity. So far, 28 MMPs have been characterized in vertebrates, of which 24 are present in humans. According to their structural organization and substrate specificity, MMPs are grouped into collagenases, gelatinases, matrilysins, stromelysins, glycosylphosphatidylinositol-anchored MMPs, transmembrane type I and II, and other MMPs (Fig. 5.1) [7].
MMPs’ classification. Human MMPs have been categorized according to their molecular structure and substrate specificity into different groups: collagenases, gelatinases, stromelysins, matrilysins, transmembrane type I, transmembrane type II, GPI-anchored, and others. GPI glycosylphosphatidylinositol, MMPs matrix metalloproteinases
Most MMPs share a basic protein structure that consists of an amino-terminal signal peptide, a pro-peptide that contains the PRCGXPD sequence that includes the cysteine-SH group linked to a zinc ion at the catalytic site, a catalytic cleft, a proline-rich linker region, and a carboxy-terminal hemopexin-like motif that participates in enzymatic regulation and substrate specificity (Fig. 5.2). Besides this basic structure, other domains are present in MMPs; for example, membrane-type MMPs (MT-MMPs) sometimes have a furin recognition site between the pro-peptide and the catalytic center that participates in the intracellular activation of MMP zymogen forms [6]. Likewise, fibronectin and vitronectin motifs are part of the gelatinases (MMP-2 and MMP-9) and MMP-21 catalytic domains, respectively [6]. Similarly, MMP-9 contains a type V collagen-like region.
Basic molecular structure of active MMPs. Domain structure is organized in most MMPs in a signal peptide, a pro-peptide that contains a cysteine that binds to a zinc ion in the catalytic motif that maintains the enzyme in an inactive form, a catalytic region that requires zinc and calcium ions for its activity, a hinge motif rich in proline, and an hemopexin domain
MMPs are synthesized as zymogens with the exception of MMP-23 that has no pro-peptide sequence. The pro-peptide “cysteine switch” with the zinc ion at the catalytic center forms a sphere-like structure that prevents substrate binding [8]. Conformational changes in the pro-domain modify the cysteine switch causing a partial activation of the enzyme. This first step of the pro-enzyme activation may be provoked by a proteolytic cleavage of the pro-peptide by trypsin, other MMPs, or plasmin, by the substrate binding to MMP exosites (sites outside the catalytic domain) that induces an allosteric activation, and by the chemical modifications that directly affect the thiol-zinc link produced for example by reactive oxygen species (ROS). Then the MMP removes the pro-peptide by an autocatalytic process to obtain full enzymatic activity [5]. Pro-MMPs can be also activated through their furin site by furin-like convertases and by forming activation complexes (see below).
5.2.2 MMPs’ Enzymatic Activity Regulation
MMPs are involved in many physiological events such as inflammation, embryogenesis, wound healing, neurite growth, and immunity, but a dysregulation in their enzymatic activity may cause tissue damage as seen in many non-cancerous diseases such as fibrosis, rheumatoid arthritis, epidermolysis bullosa, and aortic aneurysm [9]. Therefore, the enzymatic activity of MMPs must be strictly controlled by the tissue inhibitors of metalloproteinases (TIMPs). The inhibitory capacity of TIMPs is located at the N-terminal region that chelates the zinc ion from the MMP catalytic cleft forming a 1:1 stoichiometric complex [10, 11]. The C-terminal domain is involved in the formation of MMP activation complexes. Besides MMPs’ inhibition, TIMPs also block the enzymatic activity of a disintegrin and metalloproteinases (ADAMs) and ADAMs with thrombospondin motifs (ADAMTSs). Four different TIMPs have been identified: (1) TIMP-1, a 28-kDa glycosylated protein that can inhibit ADAM-10 and most MMPs except some MT-MMPs; (2) TIMP-2, a 21-kDa non-glycosylated protein that blocks MMPs and ADAM-12 enzymatic activity; (3) TIMP-3, a glycosylated molecule with a molecular weight of 24/27 kDa, capable of inhibiting the activity of MMPs, ADAMs, and ADAMTs; and (4) TIMP-4, a 22-kDa non-glycosylated protein that interferes with the activity of MMPs and ADAM-17, ADAM-18, and ADAM-33 (Table 5.1). Interestingly, TIMPs have other functions besides inhibiting the enzymatic activity of MMPs. For example, TIMP-2 participates in the activation of pro-MMP-2 through the formation of the pro-MMP-2/TIMP-2/MMP-14 complex. Briefly, two MMP-14 molecules dimerize in the cell surface and then the N-terminal region of TIMP-2 binds to the catalytic center of one MMP-14 followed by the binding of the hemopexin pro-MMP-2 region with the C-terminal domain of TIMP-2. The free MMP-14 cleaves the pro-peptide and the active MMP-2 is released [12]. This pro-MMP-2 activation mechanism is carried out in the neoplastic cell invadopodia during the invasion process. Likewise, TIMP-1 also forms the pro-MMP-9/TIMP-1/MMP-3 activation complex in which a large MMP-3 stoichiometric amount is necessary to saturate TIMP-1 and activate pro-MMP-9 [13]. The ability of TIMPs to bind to other ligands enables them to participate in processes such as apoptosis, cell proliferation, and angiogenesis, besides ECM turnover [11, 14].
5.2.3 Control of MMPs’ Expression
MMPs are regulated at the genetic level by growth factors, glucocorticoids, cytokines, retinoic acid, and interleukins [15]. MMPs have three different types of promoter sites: (1) promoters with an activator protein-1 (AP-1) (~70 bp) and a TATA box (~30 bp) with the presence of a polyoma enhancer activator protein-3 (PEA-3) binding site located upstream, (2) promoters with a TATA box but no AP-1 site, and (3) promoters with no TATA box but with multiple GC boxes that are attaching zones for specific protein-1 (Sp1) and Sp3. For more details, see Yan C and Boyd DD [15].
Epigenetic processes, such as histones H3 and H4 acetylations that stimulate the synthesis of MMPs and promoter cytosine methylation in CpG that blocks MMPs’ expression, are other ways to control the production of MMPs [15]. Likewise, regulation of MMPs’ synthesis is mediated by the stabilization and destabilization of the transcripts with the participation of trans-acting RNA-binding proteins as well as several microRNAs at the post-transcriptional level [6].
5.3 TME Metabolic Conditions
TME is constituted by all the elements that surround the neoplastic cells and includes different types of cells, ECM components, secretory vesicles, exosomes, and signal molecules, all of which are immersed in particular metabolic conditions that drive cancer progression.
5.3.1 Extracellular Microenvironment Acidification and MMPs
Genetic mutations involved in tumorigenesis may provoke changes in the glucose metabolism of cancer cells. Warburg’s first studies demonstrated that neoplastic cells increase their glucose uptake changing from an aerobic to an anaerobic glycolysis even though O2 concentrations suffice for cell requirements [16]. This is the so-called Warburg effect. The molecular mechanisms involved in this tumor metabolic change are not well known, but it has been pointed out that mutations in the phosphoinositide 3-kinase (PI3K)/Akt pathway are implicated in glucose transporter Glut1 recycling, internalization, and activity augmenting its presence at the cell membrane [17,18,19]. The increase in glucose intake, together with a rise of hexokinase-2, phosphofructokinase-1 (PFK-1), and PFK-2 activities caused also by mutated PIK3, favors the anaerobic glycolysis with the subsequent lactate acid production and acidification of the TME [19]. Likewise, loss of p53 functions favors the Warburg effect since this molecule stimulates the expression of TP53-induced glycolysis and apoptosis regulator (TIGAR) that degrades fructose 2-6 biphosphate (Fru-2,6-P2) because of its similarity with the 6-phosphofructo-2-kinase/fructose-2,6-bisphosphatase (PFK-2/FBPase-2) phosphatase domain [20]. Fru-2,6-P2 low levels provoke a decrease in the PFK-1 activity and an increase in the FBPase-1 action causing the inhibition of the glycolysis pathway. This change in glucose metabolism protects DNA from damage due to ROS produced during aerobic glycolysis [20].
The excessive production of lactic acid decreases the TME pH to around 6.4~7.0 [21]. TME acidification provokes an increase in cell membrane protrusions such as filopodia and invadopodia as well as lysosomes and exosomes trafficking to these structures allowing the location of MMPs and cathepsin B on the cell membrane. Moreover, pro-MMP-2 activation is carried out by cathepsin B instead of the classical mechanism in which the zymogen requires the pro-MMP-2/TIMP-2/MMP-14 complex for activation [22]. Further, it has been confirmed that this cysteine protease is able to activate pro-MMP-2 in HT29 colon cancer cell invadopodia in acidic conditions. Therefore, an increase of TME acidification due to lactic acid secretion or by the Na+/H+ exchanger 1 (NHE1) increases MMP-2 activity through cathepsin B action [21, 22]. Likewise, an increase of active MMP-2, MMP-9, and cathepsin B secretion in invadopodia in MDA-MB-231 metastatic breast cancer cells under acidic conditions has been observed [23]. Moreover, the NHE1 located in the invadopodia creates an acidic extracellular microenvironment suggesting a role of NHE1 in pro-MMP-2 and pro-MMP-9 activation [23]. Similarly, other membrane structures are affected by acidic conditions. Such is the case for caveolae that are dynamic invaginations of the cell membrane involved in signal transduction, endocytosis, and mechanical stress protection [21]. Caveolae have cathepsin B binding protein S100A10, plasminogen activator receptors, and plasminogen receptors [21]. Moreover, one of the caveolae plasminogen receptors is enolase-1 (ENO-1) that contributes to the Warburg effect through the downregulation of oxidative phosphorylation [24]. Interestingly, caveolae contain NHE1 and the voltage-gated sodium channel (NaV) 1.5 that, besides controlling H+ efflux, enhances NHE1 function increasing acidic conditions in the pericellular environment and cathepsin B activation [25]. In addition to cathepsin B’s participation in pro-MMPs’ activation, the presence of the urokinase plasminogen activator receptor (uPAR) in caveolae favors the activation of plasminogen to plasmin and in turn the activation of pro-MMPs [26]. Interestingly, ENO-1 indirectly participates in pro-MMP-2 and pro-MMP-9 activation since this enzyme interacts with plasminogen, uPA, and uPAR in neoplastic cells’ surface favoring cell invasion [27].
5.3.2 Hypoxia and MMPs’ Expression in the TME
The excessive proliferation of cancer cells together with a deficient blood supply produces regions with low pO2 in solid tumors [28]. Levels below 10 mmHg of O2 favor tumor cells’ anaerobic glycolysis contributing to the TME acidification. In response to these metabolic conditions, a change in the gene expression pattern of neoplastic cells is produced [29]. Such is the case of the overexpression of the hypoxia-inducible factors (HIFs) [28]. HIFs are transcription factors composed of an HIF-1α or HIF-2α subunit and a constitutive HIF-1β chain [30]. HIF metabolism is regulated by O2 concentrations. When O2 levels are normal, Pro-402 and Pro-564 from the HIF-α subunits are hydroxylated and the subunits bind to the von Hippel-Lindau (VHL) E3 ubiquitin ligase complex for their degradation by the ubiquitin proteasome system. In contrast, when O2 concentrations are low, HIF-α subunits translocate to the nucleus where they dimerize with HIF-1β chain and form a complex with the coactivator CBP/P300. This complex is responsible of the expression of many proteins from the glycolysis pathway and glucose transporters as well as proteins synthesized during angiogenesis and the metastatic processes [30, 31]. HIF transcription activity can be blocked by its binding to the factor-inhibiting HIF-1 (FIH-1) that interferes with the interaction among the coactivator and HIF-1. Additionally, there is another α-subunit called HIF-3α [32]. This α-chain has different isoforms with different functions according to their structure and tissue location. For example, some full-length HIF-3α act as transcription activators in hypoxic conditions while others compete with HIF-1α and HIF-2α for binding to HIF-1β when HIF-1β is not enough. Likewise, some truncated HIF-3α isoforms behave as negative regulators of HIF-1α and HIF-2α, and other truncated variants have constitutive transcription functions [32].
On the other hand, neoplastic cell invasion increases during hypoxic conditions and therefore the possibility that HIFs are involved in the regulation of MMPs’ expression. For instance, HIF-1α controls MMP-9 expression in MDA-MB-231 breast cancer cells and regulates MMP-15 transcription in pancreatic cancer cells, non-small lung cancer cells, and cervical cancer cells [33, 34]. Likewise, experiments done with HIF-1α siRNA demonstrated a downregulation of MMP-2 and MMP-9 expression together with a decrease in glioma cell migration capacity under hypoxic conditions [35]. Moreover, MMP-1 and MMP-3 synthesis was controlled by HIF-1α in bone marrow mesenchymal stem cells (bmMSCs) [36]. Furthermore, MMP-2 upregulation and E-cadherin downregulation was observed in hypoxic conditions induced by the use of cobalt chloride in esophageal cancer cells in which HIF-1α control was also involved [37]. Additionally, HIF-1α can upregulate MMP-13 expression in cells and in exosomes from nasopharyngeal carcinoma cells [38]. Likewise, an increase of MMP-7, MMP-14, and E-twenty-six-1 (ETS-1) synthesis but not of MMP-2 was detected in HepG2 and Hep3B hepatoma cell lines in hypoxic conditions [39]. However, this increase was independent of HIF-1α regulation since their expression was neither affected by the HIF-1α inhibitor TX-402 nor by the use of the HIF-1α-dominant negative vector (pHIF1αDN) suggesting an independent HIF-1α pathway for the transcription regulation of these genes. It is interesting to note that ETS-1 is a transcription factor that controls the synthesis of different MMP genes even though the increase observed in EST-1 expression in this study was not accompanied by the rise of other MMPs, for example, MMP-1, MMP-9, and MMP-13, that are augmented in ovarian and nasopharyngeal cancer cell lines [40, 41].
Likewise, while hypoxia determines MMP-14 expression in hepatoma cells, low O2 concentrations have no effect on this MMP’s synthesis in breast cancer cells. Moreover, hypoxia induces MMP-14 translocation to invadopodia due to its effects on the small GTPase rhoA in these cells [42]. Additionally, MMPs’ expression could be regulated indirectly by HIF-1α. Such is the case of MMP-1 synthesis controlled by the chemokine receptor-4 (CXCR4) and MMP-17 whose transcription is induced by Slug (also known as Snail2); the expression of both molecules is regulated by HIF-1α [43, 44].
5.4 MMPs’ Induction of Epithelial-Mesenchymal Transition
Under TME pressure, neoplastic cells develop migration capacities through their transformation from well-differentiated cells into mesenchymal-like cells [45]. This process is known as epithelial-mesenchymal transition (EMT) . During EMT, epithelial cells lose their intercellular interactions such as the adherent junctions in which the main protein is E-cadherin [46]. E-cadherin extracellular domain forms dimers that bind to E-cadherin dimers from other cells while the C-terminal intracellular region links to actin filaments through catenins such as β-catenin [46]. The expression of E-cadherin is directly or indirectly downregulated by the transcription factors zinc finger E-box-binding homeobox 1 (ZEB1), ZEB2, forkhead box protein C2 (FOXC2), Kruppel-like factor 8 (KLF8), E47, Snail (also called as Snail-1), Slug, and Twist involved in EMT [47]. In this context, the expression of ZEB1, ZEB2, Twist, Snail, and Slug genes is upregulated by MMP-14 [48]. Therefore, when MMP-14 is increased, mesenchymal markers such as N-cadherin, vimentin, and fibronectin are augmented. MMP-9 has also been implicated in EMT induction. Inhibition of MMP-9 expression using siRNA or the MMPs’ inhibitor GM6001 decreases vimentin and fibronectin expression as well as the migration capacity of highly invasive A433 cervical carcinoma cells [49]. Moreover, MMP-9 knockdown also reduced Snail expression, whereas downregulation of Snail diminished MMP-9 expression together with a diminution of the mesenchymal marker synthesis and of the invasion ability. These results point out the existence of a regulatory loop between MMP-9 and Snail expression. Furthermore, loss of E-cadherin expression in A549 non-small cell lung cancer (NSCLC) cells increases epidermal growth factor receptor-(EGFR)-mitogen activating protein kinase/extracellular signal-regulated kinase (MAPK/ERK, also known as MEK/ERK) activity with an increase of ZEB1 and MMP-2 expression [50]. Interestingly, downregulation of ZEB1 provokes a decrease in MMP-2 synthesis and in cell invasion abilities [50]. Likewise, Snail expression can be regulated by ROS. In this context, SCp2 mouse mammary epithelial cells cultured with exogenous MMP-3 express Rho-related C3 botulinum toxin substrate (Rac)-1b, an isoform from Rac-1. Rac-1b in turn releases ROS to the cytosol. ROS induce the expression of Snail and therefore the downregulation of E-cadherin and the upregulation of EMT markers [51].
Besides downregulation of E-cadherin expression, EMT can be stimulated by the proteolysis of E-cadherin extracellular domain. In this context, the shedding of the E-cadherin ectodomain by several proteases including MMP-3, MMP-7, MMP-9, and MMP-14 has been reported [52,53,54]. Furthermore, breast cancer cells that express the osteoblast differentiation transcription factor known as RUNX2 are able to overexpress MMP-2 that in turn sheds the N-terminal E-cadherin region releasing an 80-kDa soluble E-cadherin (sE-Cad) fragment [55]. These cells also express MMP-11, MMP-12, and MMP-16, but their role in E-cadherin processing is not clear. The sE-Cad fragment is able to bind to the human EGFR also known as HER or ErbB. This binding may be stronger than the one with EGF [56]. Moreover, sE-Cad is able to form complexes with the four EGFRs favoring cancer progression by the activation of the MAPK/ERK and the PKI3/mTOR/Akt signaling pathways [56]. Likewise, the exposure to culture medium from breast cancer cells enriched with sE-cad caused an increase in the synthesis of MMP-2, MMP-9, and MMP-14, as well as in the invasion capacity of human bronchial epithelial cells [57]. Furthermore, sE-Cad can disrupt adhesive junctions by its binding to full-length E-cadherin extracellular domain [58].
On the other hand, the E-cadherin intracellular domain forms a complex with β-catenin attached to the cell membrane thus preventing its transcription activities. When E-cadherin is cleaved, it releases β-catenin to the cytosol in which the canonical Wnt signaling avoids its degradation with its subsequent accumulation and nucleus translocation [59]. Then, β-catenin forms a complex with the T-cell factor/lymphoid enhancer factor 1 (TXF/LEF1) inducing the synthesis of Twist, Snail, Slug, and c-myc that favors EMT and cancer progression, as well as MMP-3, MMP-7, MMP-14, and MMP-26 expression [60]. Interestingly, MMP-3 plays a role in Wnt pathway regulation through its interaction with Wnt3a favoring β-catenin nucleus translocation and transcription functions [60]. Regarding the non-canonical Wnt pathway, expressions of the Wnt5a ligand and its receptor Ror2 are induced by Snail; this complex regulates the synthesis of MMP-2 and MMP-13 in epidermoid carcinoma and osteosarcoma cells, respectively [61]. Likewise, Wnt5a is upregulated in human LNCaP prostate cancer cells that overexpress MMP-14 [54]. Moreover, suppression of Wnt5a synthesis using three different siRNAs inhibits cell migration capacity provoked by MMP-14 expression. In spite of these results, there are controversies about Wnt5a’s role in cancer progression. These differences are due to the existence of two Wnt5a isoforms, Wnt5a-long (-L) and the truncated isoform Wnt5a-short (-S) [62]. Wnt5a-S upregulation promotes cell proliferation while Wnt5a-L has opposite effects in neuroblastoma and breast and cervical cancer cells that seem to grow independently of the canonical pathway [62]. Furthermore, Wnt5a-S knockdown decreases cell proliferation and induces apoptosis with an increase in FAS ligand (FASLG) expression and with downregulation of the tumor necrosis factor receptor superfamily member 11 b (TNFRSF11B) in HCT116 colon cancer cells [63].
EMT provides neoplastic cells with mesenchymal characteristics that allow them to invade the surrounding tissue. For example, experiments done in HT29 colon adenocarcinoma cells that overexpress Snail show that the latter drives cathepsin B and MMP-2 to cell membranes increasing MMP-2 pericellular activity [22]. Moreover, EMT and MMPs are involved in the acquisition of stem cell characteristics. In this context, SCC9 human oral squamous cell carcinoma cells that overexpress MMP-14 have a fibroblast-like morphology and an increase in ZEB1, ZEB2, Twist, N-cadherin, fibronectin, and vimentin expression [64]. These cells also have self-renewal, apoptosis, and neomycin resistance. A summary of MMPs’ effects on EMT factors and the impact on some molecules involved in EMT is presented in Table 5.2.
5.5 The Role of MMPs in the Evolution of Neoplastic Cells
TME metabolic conditions drive the evolution of tumor cells provoking the presence of a great diversity of cancer cells with variations in differentiation grade, metastatic abilities, cell biomarkers, and therapeutic response. There are several theories that try to explain neoplastic cell heterogeneous population in solid tumors: (1) the hierarchical or cancer stem cell (CSC) theory, (2) the stochastic or clonal model, (3) the CSC dynamic scheme, (4) the horizontal gene transfer mechanism, and (5) the cell fusion model [6]. TME metabolic characteristics have influence on neoplastic cell evolution. For example, glioma cells isolated from human brain tumors, grown in low pH (6.5), expressed the glioma stem cell (GSC) markers Oct4, Nanog, and Oli2, developed the ability to establish neurosphere-like structures in vitro, and increased their tumor formation capacity in an in vivo experimental model [65]. Interestingly, the exposure of glioma cells to acidic stress also increased the expression of vascular endothelial growth factor (VEGF), an angiogenic factor, and of HIF-2α in normoxic conditions. The expression of HIF-2α was associated with the maintenance of GSCs [65]. Moreover, prostate cancer cells (PC3 cell line) cultured in acidic medium (pH 6.5) acquired CSC-stemness markers, such as CD133, CD44, Oct4, and Klf4, increased their cell viability, enhanced their capacity to form cell colonies, and raised MMP-9 and VEGF synthesis and secretion [66].
On the other hand, MMPs play a role in the acquisition and regulation of CSC functions. For example, it has been demonstrated that MMP-3 is involved in Wnt pathway control in mammary stem cells (MaSCs) [67]. In general terms, the canonical Wnt signaling favors stem cell characteristics while the noncanonical Wnt route controls cell proliferation. MMP-3 hemopexin domain and its hinge region bind to the noncanonical ligand Wnt5b co-receptor site. Moreover, MMP-3 is able to cleave this Wnt5b region interfering with noncanonical Wnt signaling, favoring the canonical Wnt pathway, and therefore promoting MaSC proliferation and differentiation to CSCs [67].
Likewise, MMP-7 has a role in the transdifferentiation from acinar to ductal cells that apparently have progenitor cell-like properties contributing to the initial metaplastic lesions in pancreatic ductal adenocarcinoma (PDA) [68]. In vitro experiments demonstrated that MMP-7 activates the Notch pathway producing a nestin-positive intermediate followed by the adeno-ductal metaplasia that in turn gives rise to the metaplastic duct lesion associated with PDA [68].
Similarly, MMP-9 overexpression was detected in hematopoietic stem cells (HSCs) from the bone marrow after 5-fluorouracil (5-FU) treatment [69]. This MMP promotes HSC differentiation and migration due to the release of soluble kit ligand (sKitL) from stromal cell membrane that binds to KitL receptor (c-Kit) in HSCs [69]. Moreover, myelosuppression induces stromal cell-derived factor-1 (SDF-1) expression in stromal and HSC cells and is responsible for MMP-9 synthesis [69].
Similarly, MMP-10 expression was observed in bronchio-alveolar stem cells (BASCs) that contain a driving Kras mutation (CMT167, a mouse cell line) [70]. These cells grow as non-adherent oncospheres expressing stem cell markers such as CD133, Hey1, Hey2, Aldh1, Notch23, Notch4, and Nanog that get lost when MMP-10 is downregulated. Comparable results were observed in MMP-10−/− Lewis lung carcinoma (LLC) oncosphere cultures [70]. Besides MMP-10’s role in the regulation of stem cell gene expression and therefore in their maintenance, MMP-10 favors other stem cell functions such as colony expansion and tumor-initiating activity.
Likewise, MMP-14 plays a role in the regulation of HSC differentiation and maintenance through the binding to FIH-1 [71, 72]. This interaction releases HIF-1α allowing the expression of genes such as SDF-1, KitL, interleukin-7 (IL-7), and erythropoietin (Epo) involved in HSC development. Additionally, SDF-1 also maintains HSCs at the bone marrow through its binding to CXCR4 [73]. But the SDF-1-CXCR4 link can be disturbed by MMPs. For example, MMP-2 hemopexin C region binds to SDF-1 to cleave and release a tetrapeptide from the N-terminal domain of SDF-1 blocking its binding to CXCR4 and thus promoting HSC migration [74]. Moreover, a mass spectrometry assay demonstrated that MMP-1, MMP-3, MMP-9, MMP-3, and MMP-14 cleave SDF-1 in the same site that MMP-2 does [74]. Likewise, MMP-8 from neutrophil granulocytes also promotes HSC mobilization by the disruption of SDF-1 N-terminal region, but the cleavage site is different from the other MMPs since MMP-8 releases a tripeptide from the N-domain [75]. It is important to mention that SDF-1’s first two amino acids are involved in cell migration, whereas the next six amino acids participate in SDF-1 binding to CXCR4 [75].
5.6 MMPs and Non-neoplastic Cells from the TME
Besides a great cancer cell heterogeneity, TME is constituted by blood endothelial cells (ECs), lymphatic endothelial cells (LECs), bone marrow-derived cells, pericytes, smooth muscle cells, adipocytes, neutrophils, tumor-associated macrophages (TAMs), neuroendocrine cells, lymphocytes, myeloid-derived suppressor cells (MDSCs), and cancer-associated fibroblasts (CAFs), and their interactions allow cancer progression. Only those cells with activities regulated directly or indirectly by MMPs and cells that express MMPs in the TME and have a role in cancer progression are discussed in this chapter.
5.6.1 Immune Response Cells
TME comprises cells that participate in the immune response (Fig. 5.3). Therefore, tumor cells acquire molecular mechanisms to evade immune surveillance that includes MMPs’ participation (Fig. 5.3). For example, cervical cancer cells decrease T-cell development by the secretion of MMP-2 and MMP-9 that in turn cleave the interleukin-2 receptor α (IL-2Rα) from the membrane of T cells blocking their proliferation [76]. Likewise, tumor cells express on their membrane ligands that join the natural killer group 2D (NKG2D) receptors from the immune cytotoxic cells such as CD8+ T lymphocytes and natural killer (NK) cells [77]. The binding of these tumor ligands activates the immune response. There are three different types of NKG2D ligands: the UL16 binding proteins (ULBP), the major histocompatibility complex (MHC) class I-related chain molecules A (MICA), and MICB [77]. The expression of these tumor ligands might be regulated by the TME; for instance, hypoxia downregulates the expression of MICA through HIF-1α contributing to the escape of tumor cells from the immune surveillance [77]. Moreover, the proteolytic cleavage of MICA and MICB by MMPs produces the release of ligands that in turn compete for the immune cell receptors avoiding cytotoxic effects particularly from NK cells. In this context, MMP-2 is able to cut off MICA from renal carcinoma cells, while MMP-9 cuts it from osteosarcoma cells [78, 79]. Moreover, MMP-14 is involved in MICA shedding from prostate and breast cancer cells [80]. It is important to note that MMP-14’s role in MICA cleavage is independent of MMP-2 and MMP-13 activation. Interestingly, the MMPs from CAFs may also participate in these evasion mechanisms. Melanoma cells cultured with conditioned medium (CM) rich in active MMPs from melanoma-associated fibroblasts decrease their susceptibility to NK-related cytotoxic effects, increase soluble MICA and MICB fragments released to the cultured medium, and reduce MICA and MICB expression in their cell membranes [81]. These effects were reversed by the MMPs’ inhibitor GM6001. The CM comprised several MMPs including MMP-2, MMP-9, and MMP-14, but it was not clear which MMP was responsible for NKG2D shedding.
Crosstalk among neoplastic and inflammatory cells. Neoplastic cell (NC) interferes with the immune response through the release of MMP-2 and MMP-9 that inhibit T-cell proliferation. These MMPs and MMP-14 cut off MICA and MICB from tumor cell membranes to evade the immune response. MICA and MICB fragments bind to immune cell receptors contributing to a decrease in immune surveillance. Tumor cell MMP-2, MMP-9, MMP-13, and MMP-14 activate TGFβ blocking T-cell differentiation and antigen presentation. TAMs release TNFα that increases neoplastic cell MMP-9 expression while IL-1β induces MMP-1, MMP-3, MMP-10, and MMP-14. Periostin upregulates MMP-12 synthesis while periostin and IL-4 promote the expression of MMP- 1 and MMP-12 from TAMs. TAMs also produce MMP-9 and MMP-11. TANs release MMP-9 that favors angiogenesis. MMP-9 pro-angiogenic function is protected by NGAL synthesized by TANs and neoplastic cells. MMP-9 blocks tumor cell apoptosis and increases cell proliferation. MC MMP-9 expression is induced by activated T cells through TNFα. Likewise, MMP-2 and MMP-9 are stimulated by TGFβ and KitL. MC chymase promotes MMP-9 expression from NC. IL interleukin, IL-2Rα interleukin-2 receptor α, KitL kit ligand, MC mast cell, MMP matrix metalloproteinase, MICA MHC class I-related chain molecules A, NC neoplastic cell, NGAL neutrophil gelatinase-associated lipocalin, NK natural killer, TAN tumor-associated neutrophil, TAM tumor-associated macrophage, TGFβ transforming growth factor-β
Tumors also suppress the immune response through the secretion and activation of transforming growth factor-β (TGFβ) located in the ECM or released by other cells. TGFβ is synthesized as a pro-protein in which the pro-peptide has a furin recognition sequence that is cleaved by furin, but other proteases such as thrombin, neutrophil elastase, plasmin, and MMPs can also disturb it [82]. In this context, MMP-2 and MMP-9 can activate TGFβ2 and TGFβ3 with little impact on TGFβ1 [82]. In contrast, MMP-13 seems to have more effect on TGFβ1. Likewise, MMP-14 activates TGFβ when it is presented by αvβ8 integrin on cells’ surface [82]. TGFβ activation suppresses lymphocyte T proliferation and differentiation and interferes with antigen presentation [83]. Moreover, active TGFβ from platelets downregulates tumor NKGD2 decreasing NK cell anti-tumor responsiveness [84].
5.6.2 Tumor-Associated Macrophages (TAMs)
On the other hand, TAMs are the largest innate immune cell population in the TME. TAMs originate from monocytes that are attracted from blood circulation to the tumor by cytokines such as SDF-1 also called C-X-C motif chemokine 12 (CXCL12), chemokine C-C motif ligand 2 (CCL2), RANTES (Regulated on Activation, Normal T cell Expressed and Secreted, also known as CCL5), monocyte colony-stimulating factor (M-CSF), VEGF, and TGFβ, all of which are secreted by cancer and stromal cells [85]. In this context, there is a close interaction among TAMs and neoplastic cells in breast cancer [86]. Tumor cells release the M-CSF while TAMs express the CSF receptor (CSFR), and TAMs produce EFG, whereas neoplastic cells have the corresponding receptor. TAM polarization depends on TME conditions. Differentiation to classically activated M1 macrophages in response to lipopolysaccharide (LPS) and interferon-γ (IFN-γ) is observed in normoxic areas, and alternatively activated M2 cells emerge under the influence of IL-4 and IL-13 mainly in hypoxic zones [85]. M1 macrophages have cytotoxic phenotype since they secrete IL-6, IL-12, reactive nitrogen intermediates, tumor necrosis factor-α (TNFα), and ROS, while M2 macrophages participate in ECM remodeling through the release of MMPs particularly the M2c phenotype and promote angiogenesis, neoplastic cell stemness, and chemotherapy resistance [85, 86]. Since M2 macrophages are associated with cancer progression, in the present chapter, we focus on this type of TAMs. In this context, monocytes’ differentiation into TAM M2 is driven by neoplastic cells. However, TAMs have influence on tumor cells’ behavior. Co-cultures of MKNI gastric carcinoma cells with monocyte cells induce a morphologic change together with a rise in the expression of α5 integrin in their cell membranes and high levels of secreted MMP-9 and fibronectin with an increase in their invasion capacity [87]. These monocytes’ effects on cancer cells are dependent, at least in part, on TNFα. Similarly, M2 cells from renal cell carcinoma synthesize high levels of IL-1β that induce tumor MMP-1, MMP-3, MMP-10, and MMP-14 expression in patients with advanced stages of the disease [88]. Moreover, M2-like macrophages are able to stimulate the synthesis of MMP-2 and MMP-9 in SW480 human colon cancer cells with the induction of EMT and the increase in their invasiveness ability [89]. Likewise, TAM-like cells secrete high levels of MMP-9 [87]. In fact, MMP-9 has been considered as a marker of M2 macrophages and therefore can be used to predict breast cancer patients’ outcome [90]. Furthermore, a co-localization of MMP-9 and MMP-11 in M2 macrophages was demonstrated in tissue samples from cutaneous squamous cell carcinoma [91]. MMP-1 and MMP-12 were also observed in TAMs together with deposits of periostin, a non-structural ECM protein, at the peripheral zones of dermatofibrosarcoma protuberans (DFSP) [92]. In this regard, treatment of CD163+-monocyte-derived macrophages with periostin and IL-4 stimulated the synthesis of MMP-1 and MMP-12, while periostin alone only augmented MMP-12 expression [92]. Interactions among neoplastic cells and TAMs through MMPs are outlined in Fig. 5.3.
5.6.3 Tumor-Associated Neutrophils (TANs)
Even though circulating neutrophils have been considered as cells with a short lifetime and with cytotoxic effects, they are part of the TME and their presence has been correlated with a poor prognosis. Moreover, cytokines, such as IL-1, prolonged their life and contributed to neutrophil polarization allowing them to participate in cancer progression [93]. Like TAMs, there are two different types of tumor-associated neutrophils (TANs) with different functional characteristics. Monocytes exposed to IFNβ differentiate into the N1 type while stimulation by TGFβ promotes N2 polarization [94]. N1 neutrophils are present in cancer early stages, have cytotoxic and anti-tumoral functions, and are able to attract CD4+ and CD8+ lymphocytes to tumor lesions. In contrast, N2 cells possess immunosuppressive characteristics since, under the influence of tumor IL-8, they can suppress CD8+ cytotoxic cells by the secretion of arginase 1, are able to recruit forkhead box P3 (FoxP3+) cells also known as Tregs cells that induce tumor growth and suppress anti-tumor response, and promote angiogenesis [94, 95]. TAN granules contain several proteases such as cathepsin G, neutrophil elastase (NE), and MMPs that contribute to the ECM modification as well as to tumor growth and metastatic capacity (Fig. 5.3) [96]. For instance, NE and MMP-9 are involved in BM disruption favoring the release of VEGF that is a potent pro-angiogenic factor. In fact, TANs are one of the major sources of MMP-9 in TME. For example, MMP-9 was increased in TANs but not in TAMs in NSCLC tissue [97]. Further, it has been observed that MMP-9 was augmented in TANs compared to TAMs at the leading edge of the tumor in a model of murine pancreatic adenocarcinoma [98]. Interestingly, the MMP-9 released by TANs is a TIMP-1-free pro-MMP-9 while the MMP-9 secreted by other cells is in complex with TIMP-1 (see above) [99]. Additionally, only the TIMP-1-free pro-MMP-9 from TANs is able to induce angiogenesis in in vivo models. Furthermore, this TIMP-1-free pro-MMP-9 is activated through MMP-3 in collagen on plants while it undergoes natural activation in in vivo models. Likewise, MMP-9 for its pro-angiogenic function requires both the catalytic and the hemopexin domains [99]. TAN MMP-9 also promotes basic fibroblast growth factor-2 (bFGF2) activation that has pro-angiogenic properties, too [99]. It is important to note that TAMs also produce TIMP-1-free pro-MMP-9 through shutting down TIMP-1 expression when they are polarized to M2-like macrophages [100]. This TAM MMP-9 also induces angiogenesis; however, M2 macrophages release lower quantities of pro-MMP-9 in comparison to TANs that are able to rapidly secrete great amounts of pro-MMP-9 stored in their granules [100]. Additionally, MMP-9 enzymatic activity may be protected and enhanced by the neutrophil gelatinase-associated lipocalin (NGAL) released by neutrophils and cancer cells [101]. MMP-9 and NGAL form a complex that has been associated with an increase in angiogenesis and metastatic potential and therefore is considered as a bad prognosis marker for cancer outcome [102]. Likewise, TAN MMP-9 stimulates tumor cell proliferation and reduces apoptosis [103, 104].
Likewise, tumor-infiltrating neutrophils recruited and polarized to TANs N2 by bladder cancer cells are able to increase neoplastic cell invasion capacity via upregulation of androgen receptor (AR) expression that in turn enhances MMP-13 synthesis [105].
On the other hand, neoplastic cells promote neutrophil extracellular trap (NET) production by neutrophils [106]. NETs are neutrophil DNA decorated with neutrophil peptides. In the case of cancer, among NETs’ components are cathepsin G, neutrophil elastase, and MMP-9. The functions of NETs in cancer are not well defined but probably they favor tumor proliferation, resistance to apoptosis, detachment from the primary tumor, and induction of angiogenesis [106].
5.6.4 Mast Cells
Mast cells (MCs) are recruited from blood circulation to the TME by CCL15 or stem cell factor (SCF) secreted by neoplastic cells. Likewise, TGFβ and cytokines such as IL-3, IL-4, IL-9, IL-10, IL-33, and SDF-1 contribute to MC growth and maintenance [107]. Once in the tumor, the TME might regulate MC behavior, and as TAMs and TANs, MCs differentiate into two types: MCs that contain tryptase (T-MCs) and the MCs that secrete tryptase and chymase (TC-MCs) [108]. Moreover, T-MCs can evolve to TC-MCs depending on the TME conditions such as the presence of IL-4, IL-6, nerve growth factor (NGF), and SCF [108]. Even though it was possible to identify different MC types, it is not clear which one has anti-tumor or pro-cancer characteristics.
Among their anti-cancer actions, MCs are able to engage cells from the innate immune system to establish an anti-tumor immune response, tumor growth suppression by IL-1, IL-6 and TNFα secretion, apoptosis promotion, and inhibition of cell migration [109]. Conversely, MCs are able to induce cancer progression by increasing tumor cell growth and ECM disruption to facilitate neoplastic cell mobilization and to promote angiogenesis [109]. Furthermore, MCs can provoke an immunosuppressive response to NK and T cells by releasing adenosine in the TME [107]. Likewise, cellular immunity is regulated by MC secretion of TNFα, IL-10, and histamine [109]. Interestingly, an intratumoral location of MCs is associated with a good prognostic which indicates that these MCs have anti-tumoral properties. In contrast, MCs that promote cancer progression are located at the tumor invasive front next to the neovascularization areas [109].
On the other hand, MCs synthesize and activate MMPs (Fig. 5.3). For instance, MMP-9 is produced by contact among MCs and activated lymphocytes through TNFα [110]. Moreover, MC MMP-2 as well as MMP-9 expression might be regulated by TGFβ and KitL [111]. Likewise, MMP-9 is expressed in MCs in well-differentiated prostate adenocarcinomas but not in MCs from poorly differentiated tumors that show an enhanced MMP-9 location in cancer cells [112]. These results suggest that, through MMP-9, MCs are involved in prostate cancer development. Similarly, MCs also have the capacity to express MMP-1 although the specific function of this MC MMP in cancer progression has not been examined [113]. In this context, a correlation among MC density and MMP-9 has been reported in multiple melanoma (MM) patients with osteolytic disease [114]. The role of MCs besides angiogenesis promotion is the increase of bone re-absorption in MM progression. Therefore, although MC MMP-1’s presence in this pathology has not been described, it is possible that both MMP-9 and MMP-1 from MCs are involved in angiogenesis and bone re-absorption, respectively.
Likewise, MC chymase can stimulate MMP-9 expression in A549 lung adenocarcinoma and in H520 squamous lung carcinoma cells [115]. Moreover, chymase also participates in EMT induction by shedding E-cadherin from tumor cell surface [115]. Furthermore, MC tryptase plays a role in the activation of MMPs and plasminogen activator (PA) [116].
5.6.5 Cancer-Associated Fibroblasts (CAFs)
The most abundant TME non-neoplastic cells are CAFs . Cell origin of CAFs is variable since they can derive from local fibroblasts, senescent fibroblasts, smooth muscle cells, pericytes, ECs, epithelial cells, adipocytes, hematopoietic stem cells, and bone marrow-derived mesenchymal stem cells (BMDMCs) [117, 118]. Neoplastic cells are responsible for the recruitment and transformation of cells into CAFs through the secretion of different growth factors and cytokines [119]. Once cells arrive to the TME, they might transform into CAFs through different processes, for instance, (1) epithelial cells via EMT, (2) bmMSCs via the osteospondin-myeloid zinc finger 1 (OPN-MZF1)-TGFβ1 pathway, (3) resident fibroblasts through mesenchymal-mesenchymal transition (MMT), and (4) ECs via endothelial-mesenchymal transition (endMT) [118, 120]. These events are also induced by cancer cells. Interestingly, MMPs such as MMP-1, MMP-2, and MMP-14 from the neoplastic cells promote fibroblast MMT [119]. The maintenance of CAFs is mediated by paracrine signals from neoplastic cells and, as it happens with them, CAFs may get independence from the TME by generating autocrine signals for survival [121, 122]. Activated CAFs are able to influence TME cells including cancer cells through the synthesis and secretion of growth factors, cytokines, and ECM structural and non-structural proteins [123]. Likewise, interactions of CAFs with the ECM allow them to sense its stiffness and re-organize its molecules favoring neoplastic cell migration [124]. In this context, CAFs produce proteolytic enzymes such as lysyl oxidases and MMPs. It has been reported that active CAFs are able to express MMP-1, MMP-2, MMP-3, MMP-9, MMP-11, MMP-13, MMP-14, and MMP-19 (Fig. 5.4) [125]. These enzymes allow ECM remodeling through degradation of the BM and of some molecules from the interstitial ECM. Furthermore, cancer cells induce MMP synthesis from CAFs . For example, treatment of human mammary primary fibroblasts with CM from breast carcinoma cells elevated MMP-1 expression and favored transdifferentiation to CAFs [126]. Moreover, CAFs from primary breast cancer synthesized more MMP-1 in comparison to normal mammary fibroblasts. Besides its role in ECM degradation, MMP-1 is able to disrupt the protease receptor-1 (PAR-1) in a specific site that allows its activation and generation of PAR-1-dependent Ca2+ signals promoting tumor cell migration [127]. Moreover, PAR-1 expression is regulated by TGFβ through Smad3 and Smad4 with an increase of osteoclast differentiation, tumor growth, and angiogenesis in an in vitro model of bone giant tumor cells [128]. TGFβ is activated by several MMPs; therefore, MMPs stimulate PAR-1’s functions in a direct and indirect manner in cancer progression [82]. Likewise, CAFs and neoplastic cells at the invasive front move together across tracks formed by CAFs through ECM contraction in which rhoA-dependent kinase (ROCK) is involved and with the ECM remodeling by MMPs and the deposition of ECM components such as tenascin-C and fibronectin [129, 130].
The interactions of CAFs with neoplastic cells. NCs induce normal fibroblast MMP-1 upregulation for their transdifferentiation into CAFs. Disruption of the BM and ECM is driven by several MMPs secreted by CAFs, promoting NC invasion and angiogenesis. Moreover, interstitial MMPs (collagenases) as well as MMP-2 are involved in the creation of paths for NC and CAF mobilization. Likewise, ECM clg I and TGFβ stimulate FSP-1 expression from CAFs and NCs. FSP-1 favors MMP-13 EC expression that induces cell migration during angiogenesis. MMP-2 and MMP-1 secreted by CAFs promote NC proliferation and invasion, respectively. Furthermore, CAFs participate in NC escape from the immune response through MMP-2, MMP-9, and MMP-14 MICA and MICB cutoff. CAFs cancer-associated fibroblasts, clg I type I collagen, EC endothelial cell, ECM extracellular matrix, FSP-1 fibroblast-secreted protein-1, MICA MHC class I-related chain molecules A, MICB MHC class I-related chain molecules B, MMP matrix metalloproteinase, NC neoplastic cell, PAR-1 protease-activated receptor-1, TGFβ transforming growth factor-β
Activated CAFs can also express MMP-2. Immunohistochemical analysis revealed a co-localization of MMP-2 and α-smooth muscle actin (α-SMA) and vimentin, both CAF markers, at the perimeter of lung metastasis [131]. Moreover, a decrease in tumor lesions was observed in MMP-2−/− mice in comparison with wild animals in which tumor cells were injected. The role of MMP-2 in tumor proliferation was tested when MMP-2−/− fibroblasts were cultured in direct contact with tumor cells resulting in a decrease in the spheroid tumor growth [131].
CAFs are able to express MMP-13 and to induce its synthesis by other cells. This MMP is important in cancer progression since MMP-13 increases the invasive growth of cancer cells and favors angiogenesis through the release of VEGF from the ECM [132]. Similarly, MMP-13 activates TGFβ that, with type I collagen, stimulates the expression of fibroblast-secreted protein-1 (FSP-1) also known as S100A4 in CAFs and neoplastic cells [133]. FSP-1 can promote MMP-13 expression and its enzymatic activity in ECs favoring their migration during angiogenesis [134]. Furthermore, FSP-1 also activates plasminogen that has pro-angiogenic properties and induces EMT in cancer cells [133]. Likewise, TGFβ activation upregulates CXCR4, the SDF-1 receptor. The interaction of SDF-1 and CXCR4 increases neoplastic cell proliferation. Moreover, SDF-1 acts as a chemoattractant for those cells that express CXCR4 favoring the recruitment of EC precursors and the migration of cancer cells to LN and to other organs rich in SDF-1 [133]. Paradoxically, MMP-13 cleaves SDF-1 causing its inactivation [133]. In this context, more studies are needed to clarify the role and the molecular mechanism involved in SDF-1 regulation by MMP-13.
Another TME molecule that participates in the regulation of MMPs’ expression in CAFs is the plasmin inhibitor TFPI-2 (tissue factor pathway inhibitor-2). Assays done with lung fibroblasts cultured with CM from TFPI-2 silenced NCI-H460 cells (an NSCLC cell line) showed an increase in MMP-1, MMP-3, and MMP-7 synthesis [135]. Likewise, fibroblasts that overexpress phosphoglycerate kinase-1 (PGK1) have high levels of SDF-1, vimentin, and α-SMA and an increase in their growth index. Moreover, these fibroblasts express high levels of MMP-2 and MMP-3 that participate in prostate cancer cell invasion [136].
5.6.6 Adipocytes
Adipocytes are a major component of the TME. They secrete cytokines, pro-angiogenic factors, and adipokines that favor tumorigenesis and cancer progression. Moreover, they are a source of fatty acids that supply the energetic requirements of neoplastic cells [137]. Adipocytes have a different distribution pattern throughout the tumoral tissue [138]. For instance, there are more adipocytes with a fibroblast-like cell morphology and CAFs than mature adipocytes surrounding neoplastic cells at the tumor invasive front. In this context, adipocytes from this region under the influence of neoplastic cells transdifferentiate into adipocyte-derived fibroblasts (ADFs) via the activation of the Wnt/β-catenin pathway (Wnt canonical pathway) [139]. Interestingly, MMP-7 is expressed by ADFs probably as a consequence of the activation of the Wnt/β-catenin pathway (Fig. 5.5) [139]. It is important to note that other MMPs regulated through this mechanism at the transcriptional level (MMP-3, MMP-14, and MMP-26) can also be expressed by ADFs (see above). Likewise, ADFs acquire CAF markers such as FSP-1, type I collagen, and fibronectin but not α-SMA during their differentiation [140]. ADFs in turn develop into CAFs, although the specific mechanism is not clear.
TME different adipocyte types’ role in cancer progression. NCs induce EMT in adipocytes favoring differentiation into ADFs that can synthesize MMP-3, MMP-7, MMP-14, and MMP-26. NCs also promote adipocyte MMP-11 expression that in turn downregulates PPARγ blocking pre-adipocyte differentiation. MMP-11 provokes metabolic changes in adipocytes transforming them into CAAs. CAAs produce MMP-11 and clg VI. Moreover, MMP-11 degrades clg VI releasing a fragment called ETP. ETP and TGFβ promote EMT and recruit macrophages and ECs to TME. CAAs express MCP-1 that activates pro-MMP-2. Leptin released by CAAs promotes MMP-2, MMP-7, MMP-13, and MMP-14 upregulation in NCs. Pre-adipocyte can induce MMP-9 expression and NC invasion capacity through miR301a regulation. ADF adipocyte-derived fibroblast, CAF cancer-associated fibroblast, CAA cancer-associated adipocyte, clg VI type VI collagen, EC endothelial cell, EMT epithelial-mesenchymal transition, ETP endotrophin, MCP-1 monocyte chemotactic protein-1, MMP matrix metalloproteinase, NC neoplastic cell, PPARγ peroxisome proliferator-activated receptor-γ, TGFβ transforming growth factor-β
Adipocytes also influence tumor cells by promoting CSC characteristics. In this context, breast cancer cells that express the estrogen receptor (ER+) co-cultured with human adipocytes (SGBS cell line) in hypoxic conditions demonstrated an increase of the EMT transcription factors FOXC2 and TWIST together with an increase of N-cadherin expression and a decrease in E-cadherin synthesis [141]. Besides, adipocytes had an increase in TGFβ, lectin-type oxidase LDL receptor-1 (LOX1), and HIF-1α expression.
On the other hand, cancer cells in close proximity to adipocytes induce them to express MMP-11 at the peritumoral area (Fig. 5.5) [142]. MMP-11 inhibits the differentiation of pre-adipocytes to mature adipocytes and their maintenance by downregulation of peroxisome proliferator-activated receptor-γ (PPARγ) involved in adipogenesis. Moreover, MMP-11 promotes adipocyte lipolysis, decreases the size and number of lipid droplets, and induces changes in adipocyte morphology with a loss of adipocyte markers and a reduction in cell size. These adipocytes are called cancer-associated adipocytes (CAAs) that in turn may dedifferentiate into ADFs (see above) [142].
Activated CAAs secrete adipokines such as TNFα, leptin, hepatic growth factor (HGF) and IL-6, MMP-11, type VI collagen, and fibronectin [140]. In this regard, MMP-11 is able to cut off type VI collagen releasing a C-terminal fragment known as endotrophin (ETP) [143]. ETP induces EMT in tumor cells through its interaction with the TGFβ and participates in the recruitment of macrophages and ECs [144]. Moreover, ECs migrate and organize vasculature structures more actively in the presence of ETP [144].
Adipocytes also secrete monocyte chemotactic protein-1 (MCP-1) that favors tumor growth, migration, and invasion and participates in pro-MMP-2 activation without increasing its synthesis (Fig. 5.5) [145]. Likewise, pre-adipocytes have effects on the invasion capacities of prostate cancer cells through the induction of miR301a that decreases AR expression with a subsequent TGFβ, Smad3, and MMP-9 upregulation [146].
CAAs also release leptin, a 16-kDa protein that stimulates growth and proliferation of breast cancer cells when adipocytes are in close proximity to neoplastic cells [140]. The effects on cancer cells are due to the leptin receptors (ObRs) [147]. ObRs are expressed in six isoforms, of which the long form called OB-Rb is present in cancer cell membranes. Leptin binding to OB-Rb induces the activation of several pathways such as PI3K/Akt, MAPK/ERK, and JAK/STAT3 involved in tumor cell proliferation and cancer progression. In this context, activation of JAK/STAT3 signaling pathway induces MMP-13 but not MMP-2, MMP-9, or MMP-7 expression in pancreatic cancer cells (Fig. 5.5) [148]. These results were also observed in glioma cells treated with leptin [149]. Moreover, OB-Rb overexpression was observed associated with MMP-13 upregulation and with an increase in lymph node (LN) metastasis in advanced stages of pancreatic cancer [148]. Likewise, ER+ breast cancer cells co-cultured with adipocyte/stromal stem cells (ASCs) , in which leptin was knocked down, expressed lower levels of MMP-2, IL-6, and serine protease inhibitor E1 (SERPINE1) [150]. Moreover, when breast cancer cells mixed with leptin shRNA ASCs were implanted in the fat pad of mice, tumor growth and metastasis to the liver and lung were decreased in comparison with control animals [150]. Additionally, ASCs synthesize MMP-15 involved in the migration of these cells through the ECM [151].
Leptin promotes activation of c-Jun N-terminal kinase (JNK) and ERK signaling pathways with the induction of MMP-7 expression in ovarian cancer cell lines that express OB-Rb [152]. The induction of MMP-7 synthesis through JNK and ERK pathways was also observed in ovarian cancer cells that expressed mesothelin (MSLN) [153]. This protein induces MMP-7 upregulation via JNK, ERK 1/2, and Akt signaling pathways with an increase in the invasive potential of cancer cells. These findings indicate that leptin and MSLN receptors activate the same molecular mechanisms to promote MMP-7 expression in ovarian tumor cells and probably the synergistic effects of both molecules are involved in ovarian cancer progression. Interestingly, silencing MMP-7 reduces MMP-9 activity but not MMP-9 expression with no effects on MMP-2 [152]. In contrast, MMP-7 was able to induce pro-MMP-9 and pro-MMP-2 activation in other experimental assays [154]. Moreover, these studies showed that MMP-7 dissociated the pro-MMP-2/TIMP-2 complex and activated latent MMP-2 [154].
Leptin also enhances MMP-14 expression and membrane location in gastric cancer cells [155]. MMP-14 location on membrane surface depends on kinesin-like protein 1B (KIF1B) whose expression is also regulated by leptin. As was discussed earlier, leptin stimulates several signaling pathways involved in MMPs’ synthesis. In the case of MMP-14, the interaction between leptin and OB-Rb stimulates the Akt pathway for MMP-14 and KIF1B expression [155]. Furthermore, the effect of leptin on MMP-14 synthesis requires the participation of Notch1 signaling. Blocking Notch1 in human extravillous trophoblast cells treated with leptin also reduced Akt phosphorylation and MMP-14 expression [156]. Therefore, the interaction among Notch1 and PI3K/Akt pathway is important to leptin-induced MMP-14 expression.
5.7 Extracellular Vesicles and MMPs
So far, we have reviewed the intricate crosstalk among the different cellular components of the TME including tumor cells in relation with MMPs’ participation in cancer evolution. This cellular communication induces the release of factors that stimulate MMPs’ synthesis and secretion as well as MMPs’ involvement in cellular behavior and ECM disruption, promoting the detachment of neoplastic cells from the primary tumor and their passage through the next steps of the metastatic cascade. Most of these signals between cells are transmitted through extracellular vesicles (EVs) to neighboring cells or to distant sites such as the pre-metastatic niche. EVs are lipid bilayer structures that carry different molecules such as transmembrane proteins, cytosolic proteins, lipids, DNA, microRNAs, and RNA transcripts. There are different types of EVs: microvesicles, exosomes, oncosomes, and ectosomes [157]. EVs release their cargo molecules spontaneously or under some kind of stimuli at the pericellular space, ECM surrounding, into the corporal fluids such as lymph or blood, or into the target cells through membrane-to-membrane interaction, membrane fusion, or EV internalization [158]. Once EVs are in the cells, they may either be degraded with their cargo components, modified and remitted, or disrupted to release EV transported molecules that influence cells’ behavior. Transportation of macromolecules in EVs protects them from being degraded and allows them to maintain their integrity and activity. In this context, oncosomes (oncogenic-cargo EVs) are able to transport DNA sequences including KRAS and MYC, transcripts such as EGFRvIII and BRAF, or proteins with a pro-cancer activity [158].
Interestingly, some MMPs have been identified within exosomes. For example, pro-MMP-9 and active MMP-9 in EVs were found in fibrosarcoma and breast cancer cells [157]. Moreover, latent and active forms of MMP-2 and MMP-9 have been observed in ovarian cancer cells [159]. Additionally, heat shock protein-90 (Hsp-90) is transported in exosomes to the pre-metastatic niche where it is able to induce MMP-2 expression [159]. MMP-14 together with β1 integrin is also carried in exosomes in melanoma and fibrosarcoma cells [160]. These exosomes are able to activate pro-MMP-2 and to disrupt gelatin and type I collagen.
5.8 Escape Routes from TME
Besides orchestrating non-neoplastic cells’ behavior, tumor cells need to develop strategies to face TME metabolic changes to continue proliferating and to design escape routes to migrate to other tissues. Such is the case of angiogenesis and lymphangiogenesis, processes in which MMPs also have an important role.
5.8.1 Angiogenesis
Angiogenesis consists in the generation of new vessels from preexisting ones under the stimulation of TME conditions. Several angiogenic models have been proposed but the most studied is sprouting [161]. The cells involved in angiogenesis are called tumor endothelial cells (TECs) that may originate from normal ECs, bone marrow-derived progenitor cells, neoplastic cells, and CSCs [6]. TECs respond to different pro-angiogenic factors such as adrenomedullin (AM), EGF, and VEGF [162, 163]. Moreover, TECs produce VEGF in an autocrine manner. Cancer cells as well as other cellular components from the TME also produce pro-angiogenic molecules. For instance, CAFs release TGFβ, SDF-1, and VEGF, and tumor cells produce VEGF, AM, EGF, angiopoietin, and bFGF among others [163]. TECs under the effects of angiogenic factors migrate and participate in the formation of tube structures and stabilization and maturation of the new vessels by the secretion of BM components and pericyte recruitment [164].
Likewise, MMPs are also secreted from tumor and stromal cells contributing to angiogenesis (Fig. 5.6). For instance, MMP-1 increases vascular endothelial growth factor receptor-2 (VEGFR-2) in ECs that in turn binds to VEGF-A involved in blood vessel development [165]. The molecular mechanism consists in the proteolytic activation of PAR-1 by MMP-1. Then PAR-1 activates the nuclear factor κB (NF-κB) pathway (p65/RelA), and its p65 subunit binds to the kinase insert domain receptor (KDR)/VEFR2 promoter. Similarly, MMP-1 and MMP-2 together with EGFR/pan-HER ligand epiregulin (EREG) and cyclooxygenase 2 (COX2) are implicated in the formation of tortuous, dilated, and leaky new blood vessels [166]. These molecules are also involved in the increase of blood vessel permeability and in tumor cell intravasation. MMP-7 also plays a role in angiogenesis. This MMP increases angiogenesis by the disruption of soluble VEGFR-1 blocking the sequestration of VEGF enhancing its bioavailability [167].
Participation of MMPs in angiogenesis. NCs and SCs produce MMPs that modify EC behavior. MMP-1 disrupts PAR-1 promoting EC expression of VEGFR2. MMP-7 degrades sVEGFR1 to enhance VEGF bioavailability. MMP-9 releases VEGF from the ECM. MMPs such as MMP-3, MMP-7, and MMP-19 cleave VEGFA releasing a 16-kDa fragment that binds to VEGFR2. MMP-1 and MMP-2 participate in tubulogenesis. Likewise, MMP-9 from TANs releases VEGF and bFGF-2 from the ECM, participates in pericyte recruitment, and, with MMP-9 from other cellular sources, degrades MMNR2 from EC membranes. MMP-8 induces EC proliferation and participates in EMT promoting TEC activation and migration. TECs secrete MMP-2 and MMP-9 to degrade BM during cell migration. MMP-14 from TEC membrane activates pro-MMP-2 favoring TEC migration. MMP-14 remodels the ECM to form the vascular guidance tunnels. MMP-14 induces TEC aggregates that migrate and regulate tubulogenesis. MMP-14 favors VSMC transdifferentiation to a mesenchymal phenotype that participates in tube maturation. This MMP also promotes pericyte recruitment. TECs secrete MMP-1 and MMP-10 to limit angiogenesis. Pericytes and TECs release TIMP-3 and TIMP-2, respectively, to avoid the collapse of new vessels. BM basement membrane, bFGF-2 basic fibroblast growth factor-2, EC endothelial cell, ECM extracellular matrix, EMT epithelial-mesenchymal transition, MMP matrix metalloproteinase, MMNR2 multimerin-2, NC neoplastic cell, PAR-1 protease-activated receptor-1, SC stromal cell, sVEGFR1 soluble vascular endothelial growth factor receptor-1, TAN tumor-associated neutrophil, TEC tumor endothelial cell, TIMP tissue inhibitor of metalloproteinase, VEGF vascular endothelial growth factor, VEGFR2 vascular endothelial growth factor receptor-2, VSMC vascular smooth muscle cell
Regarding MMP-8, this MMP may participate indirectly in TEC activation and migration through the proteolytic cleavage of angiotensin I to angiotensin II [168]. Angiotensin II has the capacity of upregulating platelet endothelial cell adhesion molecule-1 (PECAM-1) expression that in turn favors β-catenin nuclear translocation and EC proliferation through the expression of CCND1, T-cell factor (TCF) 1B, TCF1E, and frizzled (FZD) genes. Moreover, MMP-8 knockdown in human umbilical vein endothelial cells (HuVECs) inhibits the expression of these genes and cell proliferation [168]. Furthermore, MMP-8 can induce EC migration through the expression of EMT genes regulated by β-catenin (see EMT section). Likewise, MMP-9 makes an important contribution to angiogenesis. MMP-9 from tumoral cells, CAFs, and TANs is able to disrupt the ECM releasing VEGF. In this context, pro-MMP-9 from TANs is not in complex with TIMP-1 allowing a rapid activation by MMP-3 with the subsequent activation of the pro-angiogenic factor bFGF-2 that is also embedded in the ECM. This action of TANs’ MMP-9 occurs faster than the effect caused by MMP-9 from other sources [99]. Likewise, MMP-9 favors EC migration and allows sprouting angiogenesis through the degradation of multimerin-2 (MMRN2) from the EC surface [169]. MMRN2 is involved in the disruption of the VEGFA/VEGFR2 signaling axis suppressing EC movement and angiogenesis progression [170]. Additionally, experiments done in MMP-9−/−mice with neuroblastoma showed that new blood vessels were smaller in size and lower in number with a decrease in pericyte recruitment in comparison with MMP-9+/+ [171]. These authors also observed in neuroblastoma samples that MMP-9 was located mainly around blood vessels particularly in ECs suggesting its participation in vessel maturation. Similarly, when TECs are activated, they degrade BM components trough the secretion of MMP-2 and MMP-9 to migrate to where angiogenesis is taking place driven by tip cells [164]. Additionally, TECs have high amounts of uPAR involved in the activation of plasminogen to plasmin. Plasmin is one of the physiological activators of pro-MMPs [26].
Likewise, MMP-14 is increased in TEC membrane where it favors pro-MMP-2 activation and TEC migration. Moreover, MMP-14 also participates in vascular tunnel formation creating spaces in the ECM called vascular guidance tunnels by the degradation of ECM components [172]. MMP-14 also favors the formation of TEC aggregates that participate in lumen formation. Functions of MMP-14 depend on the endothelial signaling complex formed by Jam-B, Jam-C, Cdc42-GTP, α2β1 integrin, and MMP-14. This complex regulates tubulogenesis [172]. Once the vascular guidance tunnel network is created, TECs regulate tube assembly and vascular remodeling. TECs also produce MMP-1 and MMP-10 that may induce vascular regression and/or the collapse of vascular guidance tunnels and tubes [172]. To avoid this effect and protect and stabilize the new vascular tubes, pericytes secrete TIMP-3 while TECs release TIMP-2 that also has the capacity to block MMP-2 and MMP-14 suppressing type IV collagen degradation [173]. Moreover, pericytes with ECs are responsible for new vessel BM assembly by the secretion of ECM molecules such as type IV collagen, nidogen-1, nidogen-2, laminin, perlecan, and fibronectin [174]. Additionally, MMP-14 facilitates the dedifferentiation of vascular smooth muscle cells (VSMCs) that contribute to vessel maturation [175]. In this context, MMP-14 disrupts low-density lipoprotein (LDL) receptor-related protein 1 (LRP1) decreasing platelet-derived growth factor receptor β (PDGFRβ) polyubiquitin-directed degradation. Stimulation of PDGFRβ by platelet-derived growth factor-BB (PDGF-BB) downregulates the expression of contractile proteins such as calponin and SMA with the increase of vimentin transforming VSMCs from a contractile to a migrant phenotype. Furthermore, MMP-14 also increases PDGFRβ internalization in caveolae [175].
Notwithstanding, not all MMPs have an angiogenic function. Such is the case of MMP-19 that is expressed in the early stages of breast, skin, and colon cancer but is downregulated during the disease progression, probably because of its anti-angiogenic function. In this context, MMP-19 expression was decreased in primary and metastatic nasopharyngeal carcinoma tumors as well as in cell lines due to promoter hypermethylation and to allelic detections [176]. Likewise, experiments done in HuVECs and HMEC-1 cells (dermal endothelial cells) cultured with CM from nasopharyngeal carcinoma cells transfected with MMP-19 mutated in its catalytic region showed an increase in their vascular tube formation capacities while the wild-type MMP-19 has the opposite effects including VEGF synthesis inhibition [176]. These experiments demonstrated that the MMP-19’s anti-angiogenic properties depend on its catalytic site. Moreover, MMP-19 also interferes with VEGF displacement from the ECM reducing its bioavailability. In contrast, other authors have identified that MMP-3, MMP-7, MMP-9, and MMP-19, and in a lower degree MMP-1 and MMP-16, cleave VEGFA releasing a 16-kDa fragment [177]. Moreover, this proteolytic event separates the VEGFA receptor binding domain from the ECM-attaching motif, and the soluble fragments generated in this way are able to phosphorylate the VEGFR promoting angiogenesis [177]. Interestingly, not all VEGF isoforms are susceptible to MMPs’ processing and therefore have a different angiogenic behavior. Tumors that are VEGF MMP-resistant have vascular sprouting and branching with the organization of cords, while VEGF fragments correlate with endothelial migration and cell growing as sheets [177]. These findings do not discard the possibility that MMPs are able to release VEGF from the ECM during the angiogenesis process.
On the other hand, as was mentioned above, angiogenesis must be controlled to prevent vascular regression and protect new vessels’ integrity. Besides TIMPs’ participation, MMPs’ activation is regulated by the presence of plasminogen activator inhibitor (PAI)-1 and PAI-2 that interfere with plasmin production [178]. Likewise, platelet factor-4 (PF4) suppresses the effect of thrombin in the upregulation of MMP-1 and MMP-3 expression blocking EC migration. Angiostatin is also involved in angiogenesis control. This molecule is the product of plasminogen cleavage and, besides other anti-angiogenic proprieties, has the ability to inhibit EC mobilization through the downregulation of MMP-2 and MMP-14 in hypoxic conditions [179].
Additionally, disruption of the BM and ECM components, such as laminin, elastin, type IV collagen, proteoglycans, and fibronectin, by the activity of different proteases including MMPs, releases protein motifs known as matrikines and unmasks cryptic sites in the ECM called matricryptins [180, 181]. Matrikines and matricryptins are involved in the regulation of several processes during cancer progression. Regarding angiogenesis, matricryptins and matrikines can provoke TEC apoptosis and suppress TEC proliferation, mobilization, and tube construction [182]. Interestingly, TECs synthesize and secrete MMPs that degrade collagens type IV, XV, XVIII, and XIX, perlecan, and laminin, whose proteolytic products have an anti-angiogenic effect [183]. This TEC behavior probably is part of the molecular mechanism involved in angiogenesis regulation. For example, endostatin, a matrikine, forms a complex with MMP-2 catalytic motif with the subsequent loss of its enzymatic activity and a decrease in tumor and endothelial invasiveness [184]. For a major review regarding matricryptins and matrikines with anti-angiogenic effects, see Gonzalez-Avila G et al. [6]. Among the MMPs that participate in proteolysis of BM and ECM are MMP-2, MMP-3, MMP-7, MMP-9, MMP-13, and MMP-20 [125, 181, 185].
Reasonably, communication among cells during angiogenesis is regulated by molecules contained in the EVs. For instance, tumor-derived EVs may contain pro-angiogenic factors such as VEGF, sphingomyelin, IL-6, IL-8, FGF, and miRNAs [186]. Remarkably, MMP-2, MMP-9, and MMP-14 expressed by ECs may be stored in cytoplasmic secretory granules and are released in EVs [187]. Moreover, VEGF and FGF increase the number of EVs containing MMPs and stimulate a fast EV shedding. These growth factors also participate in MMP enzymatic activation. EV-associated MMPs have an autocrine effect on TECs increasing their migration and tubular structure formation abilities [187]. EC-derived EVs also contain β1 integrin for their interaction with the surrounding ECM. Likewise, tumor-derived EVs that contain the MMP inducer CD147 promote HuVECs’ MMP-1, MMP-2, and MMP-14 expression and increase their invasiveness and cord formation capacities [188]. Furthermore, EVs derived from ASCs stimulated with PDGF contain MMP-2 and MMP-9 that favor EC migration [186].
5.8.2 Lymphangiogenesis
Lymph vessels (LVs) are another route that neoplastic cells use to escape from the primary TME. As in the case of angiogenesis, lymphangiogenesis consists on the creation of new LVs from preexisting LVs or from veins [189]. In contrast to new blood vessels, LVs are irregular and leaky structures in which gaps between lymphatic endothelial cells (LECs) exist; they are devoid of pericyte and VSMC layers and have a poor deposit of BM components [189, 190].
Two mechanisms that may stimulate lymphangiogenesis have been identified. The first consists in cancer cell recruitment of endothelial progenitor cells from bone marrow that express VEGFR-3 with their later integration to the LV extensions. The second process involves the interaction of pro-lymphangiogenic factors with LECs from preexisting LVs [191]. Interestingly, there is evidence that, under the influence of tumor cells, macrophages may transdifferentiate into LECs, initially generating cell aggregates followed by vesicle formation and their integration into sprouting LVs [192]. However, macrophages exposed to pro-inflammatory molecules such as TNFα enhance the expression and release of VEGF-C favoring the sprouting of preexisting LVs [192]. Neoplastic cells induce lymphangiogenesis by the release of HGF, VEGF-A, VEGF-C, and VEGF-D [193]. Likewise, other factors may also participate such as FGF-2, insulin-like growth factor-1 (IGF-1), IGF-2, endothelin-1 (Et-1), and PDGF-BB secreted by other cells, although the most relevant pro-lymphangiogenic factor is VEGF-C/VEGF-D/VEGFR-3 [193]. Active VEGFR-3 promotes LEC proliferation and migration and prevents their apoptosis through the activation of Akt, ERK, and p42/p44 MAPK pathways [194]. Additionally, VEGFR-3 interacts directly with PI3K inducing its phosphorylation that stimulates LEC migration and tube formation [195]. VEGF-C and VEGF-D also attach to neuropilin-2 (NRP-2) that is co-internalized with VEGFR-3. Both molecules form a complex that drives initial lymphatic sprouting [189, 195]. Similarly, the binding of ET-1 to its receptor EB favors LEC proliferation and migration through the activation of p42/44 MAPK and Akt signaling pathways and by MMP-2 and MMP-9 expression that play a role in tube formation [196]. Notably, during LV formation MMP-2 can disrupt type I collagen matrix allowing LEC mobilization through this ECM component [197]. Moreover, lower MMP-2 expression alters LV formation and branching in zebrafish and mice models. Additionally, the use of the MMPs’ competitive inhibitor SB-3CT suppresses MMP-2 and MMP-9 activity and downregulates VEGF-C and VEGFR-3 expression inducing a decrease in lymphangiogenesis in a corneal model [198]. Likewise, MMP-13 increases VEGF-C expression through the activation of PI3K/Akt signaling pathway favoring lymphangiogenesis and tumor metastasis [199].
MMP-14 also participates in lymphangiogenesis although with controversial roles. On the one hand, MMP-14 favors lymphangiogenesis by inducing LEC migration and LV sprouting, besides its role in pro-MMP-2 activation [200]. On the other hand, MMP-14 cuts off the lymphatic vessel endothelial hyaluronan receptor-1 (LYVE-1) from LEC surface interfering with lymphangiogenesis signaling since LYVE-1 binding to hyaluronic acid (HA) drives LEC growth [201]. Moreover, MMP-14 also suppresses macrophage VEGF-C expression through its binding to PI3K promoter with the subsequent p110δ upregulation [201]. PI3Kδ in turn blocks NF-κB nuclear translocation and VEGF-C synthesis. In this regard, MMP-16 may serve as a pro-lymphangiogenic factor since this MMP sheds MMP-14 from cell surface promoting LEC invasion [202]. Moreover, MMP-16 downregulation switches cancer progression from a lymphatic to a blood invasion process in tumors produced by the implantation of melanoma cells in mice.
5.9 Comments and Future Trends
TME metabolic conditions as well as several non-neoplastic cells contribute to provide tumor cells with characteristics that allow them to proceed with the following steps of the metastatic cascade. Cancer cells acquire the ability to invade the BM and ECM components to reach new lymphatic and blood vessels. In both invasion and intravasation, MMPs play a paramount role. Likewise, tumor invasiveness, neoplastic cell morphology (spike, amoeboid, or mesenchymal forms), migration strategies as single or cell groups, and MMPs’ expression are dependent on ECM stiffness and composition [203,204,205]. For instance, cancer cell interaction with type IV collagen promotes MMP-2 and MMP-9 release while MMP-1 and MMP-13 are secreted when cells bind to type I collagen [206, 207]. Meanwhile, during invasion MMPs are located in membrane extensions such as blebs, filopodia, and invadopodia [208,209,210]. In this context, presence of β1 integrin mediates localization of MMP-2, MMP-9, and MMP-14 in invadopodia to disrupt BM structures. Moreover, cells such as CAFs construct paths where tumor cells transit during invasion (see above). Once cancer cells arrive to blood or lymphatic vessels, they intravasate and travel to different tissues to establish a new metastatic colony with an active participation of MMPs in all this journey [6]. Therefore, MMPs’ expression has been associated with tumor cell aggressiveness and metastatic potential, and consequently these enzymes are considered as bad prognosis biomarkers. However, some MMPs have protective effects particularly at the disease’s early stages. Such is the case of MMP-3, MMP-8, MMP-12, MMP-13, MMP-19, and MMP-26 [6]. Interestingly, MMP-11 has pro-cancer functions during the early stages of illness due to its anti-apoptotic properties and its effects on adipocytes (see above), but it also has metastatic protective capacities during late stages [211, 212]. Likewise, there are differences in MMPs’ expression and functions among cancer types. Therefore, it is important to establish a specific MMPs’ profile for each case taking into account the stage of the disease.
On the other hand, since MMPs play a role in all the steps of cancer dissemination, they have been considered as therapeutic targets. In this context, several strategies have been developed to inhibit their enzymatic activity [213, 214]. However, the expected success has not been achieved due to side effects produced by the MMPs’ inhibitors and to the lack of improvement in patients’ survival rates. Moreover, matrix metalloproteinase inhibitors are not designed to block specific MMPs; therefore, MMPs with protective effects are also targets for these drugs with the subsequent worsening of the disease. Nevertheless, the expectation of inhibiting MMPs’ functions led to the creation of alternative methods to drive a specific drug to a specific tissue, such as the use of nanotechnology [215]. In this context, several delivery systems have been developed to control different TME elements and processes including TAMs, CAFs, and angiogenesis [216]. Furthermore, nanotechnology has been used in the theranostic approach that allows specific diagnosis, treatment, and monitoring of therapy response [217]. For example, the inclusion of a cytotoxic drug such as docetaxel or paclitaxel with a chemical sequence that is cleaved by MMP-2 or MMP-9 in a nanosystem targeted to a specific tumor that overexpresses these MMPs has improved patients’ illness outcomes with fewer side effects [218, 219].
In summary, MMPs have a relevant role in TME with their participation in processes that allow neoplastic cells to acquire characteristics that secure their survival in adverse microenvironmental conditions. Moreover, MMPs provide the escape mechanisms for cancer cells to detach from the primary tumor and invade the surrounding tissue searching for the way that conducts them to a new organ. Furthermore, MMPs also participate in the construction of these routes. Therefore, an early disease diagnosis with the knowledge of which MMPs are implicated in the TME may aid in controlling cancer progression in the very early stages of the disease.
Abbreviations
- 5-FU:
-
5-Fluorouracil
- ADAMS:
-
A disintegrin and metalloproteinases
- ADAMTSs:
-
ADAMs with thrombospondin motifs
- ADFs:
-
Adipocyte-derived fibroblasts
- AM:
-
Adrenomedullin
- AP-1:
-
Activator protein-1
- AR:
-
Androgen receptor
- ASCs:
-
Adipocyte/stromal stem cells
- BASCs:
-
Bronchio-alveolar stem cells
- bFGF2:
-
Basic fibroblast growth factor-2
- BM:
-
Basement membrane
- BMDMCs:
-
Bone marrow-derived mesenchymal stem cells
- bmMSCs:
-
Bone marrow mesenchymal stem cells
- CAAs:
-
Cancer-associated adipocytes
- CAFs:
-
Cancer-associated fibroblasts
- CCL2:
-
Chemokine C-C motif ligand 2
- CM:
-
Conditioned medium
- COX2:
-
Cyclooxygenase 2
- CSCs:
-
Cancer stem cells
- CXCL12:
-
C-X-C motif chemokine 12
- CXCR4:
-
Chemokine receptor-4
- DFSP:
-
Dermatofibrosarcoma protuberans
- ECM:
-
Extracellular matrix
- ECs:
-
Endothelial cells
- EGFR:
-
Epidermal growth factor receptor
- EMT:
-
Epithelial-mesenchymal transition
- endMT:
-
Endothelial-mesenchymal transition
- ENO-1:
-
Enolase-1
- Epo:
-
Erythropoietin
- ER:
-
Estrogen receptor
- EREG:
-
Pan-HER ligand epiregulin
- ERK:
-
Extracellular signal-regulated kinase
- Et-1:
-
Endothelin-1
- ETP:
-
Endotrophin
- ETS:
-
E-twenty-six-1
- EVs:
-
Extracellular vesicles
- FASLG:
-
FAS ligand
- FIH-1:
-
Factor-inhibiting HIF-1
- FOXC2:
-
Forkhead box protein C2
- FoxP3+:
-
Recruit forkhead box P3
- Fru-2,6-P2:
-
Fructose 2-6 biphosphate
- FSP-1:
-
Fibroblast-secreted protein-1
- FZD:
-
Frizzled
- GPI:
-
Glycosylphosphatidylinositol
- GSCs:
-
Glioma stem cells
- HA:
-
Hyaluronic acid
- HGF:
-
Hepatic growth factor
- HIFs:
-
Hypoxia-inducible factors
- HSCs:
-
Hematopoietic stem cells
- Hsp-90:
-
Heat shock protein-90
- HuVECs:
-
Human umbilical vein endothelial cells
- IFN-γ:
-
Interferon-γ
- IGF-1:
-
Insulin-like growth factor-1
- IL:
-
Interleukin
- IL-2Rα:
-
Interleukin-2 receptor α
- JNK:
-
c-Jun N-terminal kinase
- KDR:
-
Kinase insert domain receptor
- KIF1B:
-
Kinesin-like protein 1B
- KitL:
-
Kit ligand
- KLF8:
-
Kruppel-like factor 8
- LECs:
-
Lymphatic endothelial cells
- LLC:
-
Lewis lung carcinoma
- LN:
-
Lymph node
- LOX1:
-
Lectin-type oxidase LDL receptor 1
- LPS:
-
Lipopolysaccharide
- LRP1:
-
Low-density lipoprotein (LDL) receptor-related protein 1
- LVs:
-
Lymph vessels
- LYVE-1:
-
Lymphatic vessel endothelial hyaluronan receptor-1
- MAPK:
-
Mitogen-activating protein kinase
- MaSCs:
-
Mammary stem cells
- MCP-1:
-
Monocyte chemotactic protein-1
- MCs:
-
Mast cells
- M-CSF:
-
Monocyte colony-stimulating factor
- MDSCs:
-
Myeloid-derived suppressor cells
- MHC:
-
Major histocompatibility complex
- MICA:
-
MHC class I-related chain molecules A
- MM:
-
Multiple melanoma
- MMPs:
-
Matrix metalloproteinases
- MMRN2:
-
Multimerin-2
- MMT:
-
Mesenchymal-mesenchymal transition
- MSLN F:
-
Mesothelin
- MT-MMPs:
-
Membrane-type MMPs
- NE:
-
Neutrophil elastase
- NF-κB:
-
Nuclear factor κB
- NGAL:
-
Neutrophil gelatinase-associated lipocalin
- NGF:
-
Nerve growth factor
- NHE1:
-
Na+/H+ exchanger 1
- NK:
-
Natural killer
- NKG2D:
-
Natural killer group 2D
- NRP-2:
-
Neuropilin-2
- NSCLC:
-
Non-small cell lung cancer
- OPN-MZF1:
-
Osteospondin-myeloid zinc finger 1
- PAI:
-
Plasminogen activator inhibitor
- PAR-1:
-
Protease-activated receptor-1
- PDA:
-
Pancreatic ductal adenocarcinoma
- PDGF-BB:
-
Platelet-derived growth factor-BB
- PDGFRβ:
-
Platelet-derived growth factor receptor β
- PEA-3:
-
Polyoma enhancer activator protein-3
- PECAM-1:
-
Platelet endothelial cell adhesion molecule-1
- PF4:
-
Platelet factor-4
- PFK-1:
-
Phosphofructokinase-1
- PFK-2/FBPase-2:
-
6-Phosphofructo-2-kinase/fructose-2,6-bisphosphatase
- PGK1:
-
Phosphoglycerate kinase-1
- PI3K:
-
Phosphoinositide 3-kinase
- PPARγ:
-
Peroxisome proliferator-activated receptor-γ
- Rac:
-
Rho-related C3 botulinum toxin substrate
- RANTES:
-
Regulated on activation, normal T cell expressed and secreted (CCL5)
- ROCK:
-
rhoA-dependent kinase
- ROS:
-
Reactive oxygen species
- SCCs:
-
Squamous carcinoma cells
- SCF:
-
Stem cell factor
- SCs:
-
Stem cells
- SDF-1:
-
Stromal cell-derived factor 1
- sE-Cad:
-
Soluble E-cadherin
- SERPINE1:
-
Serine protease inhibitor E1
- sKitL:
-
Soluble kit ligand
- Sp-1:
-
Specific protein-1
- TAMs:
-
Tumor-associated macrophages
- TANs:
-
Tumor-associated neutrophils
- TCF:
-
T-cell factor
- TECs:
-
Tumor endothelial cells
- TFPI-2:
-
Tissue factor pathway inhibitor-2
- TGFβ:
-
Transforming growth factor-β
- TIGAR:
-
TP53-induced glycolysis and apoptosis regulator
- TIMPs:
-
Tissue inhibitors of metalloproteinases
- TME:
-
Tumor microenvironment
- TNFRSF11B:
-
Tumor necrosis factor receptor superfamily member 11 b
- TNFα:
-
Tumor necrosis factor-α
- TXF/LEF1:
-
T-cell factor/lymphoid enhancer factor 1
- uPAR:
-
Urokinase plasminogen activator receptor
- VEGF:
-
Vascular endothelial growth factor
- VHL:
-
Von Hippel-Lindau
- VSMCs:
-
Vascular smooth muscle cells
- ZEB1:
-
Zinc finger E-box-binding homeobox 1
- α-SMA:
-
α-Smooth muscle actin
References
Maley CC, Aktipis A, Graham TA et al (2017) Classifying the evolutionary and ecological features of neoplasms. Nat Rev Cancer 17(10):605–619. https://doi.org/10.1038/nrc.2017.69
Kim J, Tanner K (2015) Recapitulating the tumor ecosystem along the metastatic cascade using 3D culture models. Front Oncol 5(170). https://doi.org/10.3389/fonc.2015.00170
Wang M, Zhao J, Zhang L et al (2017) Role of tumor microenvironment in tumorigenesis. J Cancer 8(5):761–773. https://doi.org/10.7150/jca.17648
Chen F, Zhuang X, Lin L et al (2015) New horizons in tumor microenvironment biology: challenges and opportunities. BMC Med 13:45. https://doi.org/10.1186/s12916-015-0278-7
Loffek S, Schilling O, Franzke CW (2011) Biological role of matrix metalloproteinases a critical balance. Eur Respir J 38(1):191–208. https://doi.org/10.1183/09031936.00146510
Gonzalez-Avila G, Sommer B, Mendoza-Posada DA et al (2019) Matrix metalloproteinases participation in the metastatic process and their diagnostic and therapeutic applications in cancer. Crit Rev Oncol Hematol 137:57–83. https://doi.org/10.1016/j.critrevonc.2019.02.010
Cui N, Hu M, Khalil RA (2017) Biochemical and biological attributes of matrix metalloproteinases. Prog Mol Biol Transl Sci 147:1–73. https://doi.org/10.1016/bs.pmbts.2017.02.005
Tallant C, Marrero A, Gomis-Rüth FX (2010) Matrix metalloproteinases: fold and function of their catalytic domains. Biochim Biophys Acta 1803(1):20–28. https://doi.org/10.1016/j.bbamcr.2009.04.003
Amălinei C, Căruntu ID, Giuşcă SE et al (2010) Matrix metalloproteinases involvement in pathologic conditions. Romanian J Morphol Embryol 51(2):215–228. DOI: not available
Lambert E, Dassé E, Haye B, Petitfrère E (2004) TIMPs as multifacial proteins. Crit Rev Oncolol Hematol 49(3):187–198. https://doi.org/10.1016/j.critrevonc.2003.09.008
Jackson HW, Defamie V, Waterhouse P et al (2017) TIMPs: versatile extracellular regulators in cancer. Nat Rev Cancer 17(1):38–53. https://doi.org/10.1038/nrc.2016.115
Itoh Y (2015) Membrane-type matrix metalloproteinases: their functions and regulations. Matrix Biol 44–46:207–223. https://doi.org/10.1016/j.matbio.2015.03.004
Ogata Y, Itoh Y, Nagase H (1995) Steps involved in activation of the pro-matrix metalloproteinase 9 (progelatinase B)-tissue inhibitor of metalloproteinase-1 complex by 4- aminophenylmercuric acetate and proteinases. J Biol Chem 270(31):18506–18511. https://doi.org/10.1074/jbc.270.31.18506
Arpino V, Brock M, Gill SE (2015) The role of TIMPs in regulation of extracellular matrix proteolysis. Matrix Biol 44–46:247–254. https://doi.org/10.1016/j.matbio.2015.03.005
Yan C, Boyd DD (2007) Regulation of matrix metalloproteinase gene expression. J Cell Physiol 211(1):19–26. https://doi.org/10.1002/jcp.20948
Warburg O (1925) The metabolism of carcinoma cells. Cancer Res 9(1):148–163. https://doi.org/10.1158/jcr.1925.148
Elstrom RL, Bauer DE, Buzzai M et al (2004) Akt stimulates aerobic glycolysis in cancer cells. Cancer Res 64(11):3892–3899. https://doi.org/10.1158/0008-5472.CAN-03-2904
Wieman HL, Wofford JA, Rathmell JC (2007) Cytokine stimulation promotes glucose uptake via phosphatidylinositol-3 kinase/Akt regulation of Glut1 activity and trafficking. Mol Biol Cell 18(4):1437–1446. https://doi.org/10.1091/mbc.e06-07-0593
Hirschey MD, DeBerardinis RJ, Diehl AME et al (2015) Dysregulated metabolism contributes to oncogenesis. Semin Cancer Biol 35 Suppl:S129–S150. https://doi.org/10.1016/j.semcancer.2015.10.002
Bensaad K, Tsuruta A, Selak MA et al (2006) TIGAR, a p53-inducible regulator of glycolysis and apoptosis. Cell 126(1):107–120. https://doi.org/10.1016/j.cell.2006.05.036
Ji K, Mayernik L, Moin K et al (2019) Acidosis and proteolysis in the tumor microenvironment. Cancer Metastasis Rev. https://doi.org/10.1007/s10555-019-09796-3
Kryczka J, Papiewska-Pajak I, Kowalska MA et al (2019) Cathepsin B is upregulated and mediates ECM degradation in colon adenocarcinoma HT29 cells overexpressing Snail. Cell 8(3):pii:E203. https://doi.org/10.3390/cells8030203
Greco MR, Antelmi E, Busco G et al (2014) Protease activity at invadopodial focal digestive areas is dependent on NHE1-driven acidic pHe. Oncol Rep 31(2):940–946. https://doi.org/10.3892/or.2013.2923
Capello M, Ferri-Borgogno S, Riganti C et al (2016) Targeting the Warburg effect in cancer cells through ENO1 knockdown rescues oxidative phosphorylation and induces growth arrest. Oncotarget 7(5):5598–5612. https://doi.org/10.18632/oncotarget.6798
Brisson L, Gillet L, Calaghan S et al (2011) Na(V)1.5 enhances breast cancer cell invasiveness by increasing NHE1-dependent H(+) efflux in caveolae. Oncogene 30(17):2070–2076. https://doi.org/10.1038/onc.2010.574
Murphy G, Stanton H, Cowell S et al (1999) Mechanisms for pro matrix metalloproteinase activation. APMIS 107(1):38–44. https://doi.org/10.1111/j.1699-0463.1999.tb01524.x
Hsiao KC, Shih NY, Fang HL et al (2013) Surface α-enolase promotes extracellular matrix degradation and tumor metastasis and represents a new therapeutic target. PLoS One 8(7):e69354. https://doi.org/10.1371/journal.pone.0069354
Dhani N, Fyles A, Hedley D et al (2015) The clinical significance of hypoxia in human cancers. Semin Nucl Med 45(2):110–121. https://doi.org/10.1053/j.semnuclmed.2014.11.002
Sullivan R, Graham CH (2007) Hypoxia-driven selection of the metastatic phenotype. Cancer Metastasis Rev 26(2):319–331. https://doi.org/10.1007/s10555-007-9062-2
Lu X, Kang Y (2010) Hypoxia and hypoxia-inducible factors: master regulators of metastasis. Clin Cancer Res 16(4):5928–5935. https://doi.org/10.1158/1078-0432.CCR-10-1360
Tsai YP, Wu KJ (2012) Hypoxia-regulated target genes implicated in tumor metastasis. J Biomed Sci 19:102. https://doi.org/10.1186/1423-0127-19-102
Duan C (2016) Hypoxia-inducible factor 3 biology: complexities and emerging themes. Am J Physiol Cell Physiol 310(4):C260–C269. https://doi.org/10.1152/ajpcell.00315.2015
Choi JY, Jang YS, Min SY et al (2011) Overexpression of MMP-9 and HIF-1α in breast cancer cells under hypoxic conditions. J Breast Cancer 14(2):88–95. https://doi.org/10.4048/jbc.2011.14.2.88
Zhu S, Zhou Y, Wang L et al (2011) Transcriptional upregulation of MT2-MMP in response to hypoxia is promoted by HIF-1α in cancer cells. Mol Carcinog 50(10):770–780. https://doi.org/10.1002/mc.20678
Fujiwara S, Nakagawa K, Harada H et al (2007) Silencing hypoxia-inducible factor 1α inhibits cell migration and invasion under hypoxic environment in malignant gliomas. Int J Oncol 30(4):793–802. https://doi.org/10.3892/ijo.30.4.793
Lin JL, Wang MJ, Lee D et al (2008) Hypoxia-inducible factor-1α regulates matrix metalloprotease-1 activity in human bone marrow-derived mesenchymal stem cells. FEBS Lett 582(17):2615–2619. https://doi.org/10.1016/j.febslet.2008.06.033
Jing SW, Wang YD, Kuroda M et al (2012) HIF-1α contributes to hypoxia-induced invasion and metastasis of esophageal carcinoma via inhibiting E-cadherin and promoting MMP-2 expression. Acta Med Okayama 66(5):399–407. https://doi.org/10.18926/AMO/48964
Shan Y, You B, Shi S et al (2018) Hypoxia-induced matrix metalloproteinase 13 expression in exosomes from nasopharyngeal carcinoma enhances metastases. Cell Death Dis 9(3):382. https://doi.org/10.1038/s41419-018-0425-0
Miyoshi A, Kitajima Y, Ide T et al (2006) Hypoxia accelerates cancer invasion of hepatoma cells by upregulating MMP expression in aHIF-1α-independent manner. Int J Oncol 29(6):1533–1539. https://doi.org/10.3892/ijo.29.6.1533
Ghosh S, Basu M, Roy SS (2012) ETS-1 protein regulates vascular endothelial growth factor-induced matrix metalloproteinase-9 and matrix metalloproteinase-13 expression in human ovarian carcinoma cell line SKOV-3. J Biol Chem 287(18):15001–15015. https://doi.org/10.1074/jbc.M111.284034
Pang JS, Yen JH, Wu HT et al (2017) Gallic acid inhibited matrix invasion and AP-1/ETS-1-mediated MMP-1 transcription in human nasopharyngeal carcinoma cells. Int J Mol Sci 18(7).pii: E1314.). https://doi.org/10.3390/ijms18071354
Muñoz-Najar UM, Neurath KM, Vumbaca F et al (2006) Hypoxia stimulates breast carcinoma cell invasion through MT1-MMP and MMP-2 activation. Oncogene 25(16):2379–2392. https://doi.org/10.1038/sj.onc.1209273
Sun X, Wei L, Chen Q et al (2010) CXCR4/SDF1 mediate hypoxia induced chondrosarcoma cell invasion through ERK signaling and increase MMP-1 expression. Mol Cancer 9:17. https://doi.org/10.1186/1476-4598-9-17
Huang CH, Yang WH, Chang SY et al (2009) Regulation of membrane-type 4 matrix metalloproteinase by SLUG contributes to hypoxia-mediated metastasis. Neoplasia 11(12):1371–1382. https://doi.org/10.1593/neo.91326
Jung HY, Fattet L, Yang J (2015) Molecular pathways: linking tumor microenvironment to epithelial-mesenchymal transition in metastasis. Clin Cancer Res 21(5):962–968. https://doi.org/10.1158/1078-0432.CCR-13-3173
Wong SHM, Fang CM, Chuah LH (2018) E-cadherin: its dysregulation in carcinogenesis and clinical implications. Crit Rev Oncol Hematol 121:11–22. https://doi.org/10.1016/j.critrevonc.2017.11.010
Diaz VM, Viñas-Castells R, García de Herreros A (2014) Regulation of the protein stability of EMT transcription factors. Cell Adhes Migr 8(4):418–428. https://doi.org/10.4161/19336918.2014.969998
Li W, Li W, Deng L et al (2015) Decreased MT1-MMP in gastric cancer suppressed cell migration and invasion via regulating MMPs and EMT. Tumour Biol 36(9):6883–6889. https://doi.org/10.1007/s13277-015-3381-7
Lin CY, Tsai PH, Kandaswami CC et al (2011) Matrix metalloproteinase-9 cooperates with transcription factor Snail to induce epithelial-mesenchymal transition. Cancer Sci 102(4):815–827. https://doi.org/10.1111/j.1349-7006.2011.01861.x
Bae GY, Choi SJ, Lee JS et al (2013) Loss of E-cadherin activates EGFR-MEK/ERK signaling which promotes invasion via the ZEB1/MMP-2 axis in non-small cell lung cancer. Oncotarget 4(12):2512–2522. https://doi.org/10.18632/oncotarget.1463
Radisky DC, Levy DD, Littepage LE et al (2005) Rac1b and reactive oxygen species mediate MMP-3-induced EMT and genomic instability. Nature 436(7047):123–127. https://doi.org/10.1038/nature03688
Noë V, Fingleton B, Jacobs K et al (2001) Release of an invasion promoter E-cadherin fragment by matrilysin and stromelysin-1. J Cell Sci 114(Pt 1):111–118. DOI: not available
Synowicz J, Adley BP, Gleason KJ et al (2007) Engagement of collagen binding integrins promotes matrix metalloproteinase-9-dependent E-cadherin ectodomain shedding in ovarian carcinoma cells. Cancer Res 67(5):2020–2039. https://doi.org/10.1158/0008-5472.CAN-06-2808
Cao J, Chiarelli C, Richman O (2008) Membrane type 1 matrix metalloproteinase induces epithelial-to-mesenchymal transition in prostate cancer. J Biol Chem 283(10):6232–6240. https://doi.org/10.1074/jbc.M705759200
Brusgard JL, Choe M, Chumsri S et al (2015) RUNX2 and TAZ-dependent signaling pathways regulate soluble E-cadherin levels and tumorsphere formation in breast cancer cells. Oncotarget 6(29):28132–28150. https://doi.org/10.18632/oncotarget.4654
Hu QP, Kuang JY, Yang QK et al (2016) Beyond a tumor suppressor: soluble E-cadherin promotes the progression of cancer. Int J Cancer 138(12):2804–2812. https://doi.org/10.1002/ijc.29982
Nawrocki-Raby B, Giles C, Polette M et al (2003) Upregulation of MMPs by soluble E-cadherin in human lung tumor cells. Int J Cancer 105(6):790–795. https://doi.org/10.1002/ijc.11168
David JM, Rajasekaran AK (2012) Dishonorable discharge: the oncogenic roles of cleaved E-cadherin fragments. Cancer Res 72(12):2917–2923. https://doi.org/10.1158/0008-5472.CAN-11-3498
Sherwood V (2015) WNT signaling: an emerging mediator of cancer cell metabolism? Mol Cell Biol 35(1):2–10. https://doi.org/10.1128/MCB.00992-14
Blavier L, Lazaryev A, Shi XH et al (2010) Stromelysin-1 (MMP-3) is a target and a regulator of Wnt1-induced epithelial-mesenchymal transition (EMT). Cancer Biol Ther 10(2):198–208. https://doi.org/10.4161/cbt.10.2.12193
Ren D, Minami Y, Nishita M (2011) Critical role of Wnt5a-Ror2 signaling in motility and invasiveness of carcinoma cells following Snail-mediated epithelial-mesenchymal transition. Genes Cells 16(3):304–315. https://doi.org/10.1111/j.1365-2443.2011.01487.x
Bauer M, Bénard J, Gaasterland T, Willert K, Cappellen D (2013) WNT5A encodes two isoforms with distinct functions in cancers. PLoS One 8(11):e80526. https://doi.org/10.1371/journal.pone.0080526
Huang TC, Lee PT, Wu MH (2017) Distinct roles and differential expression levels of Wnt5a mRNA isoforms in colorectal cancer cells. PLoS One 12(8):e0181034. https://doi.org/10.1371/journal.pone.0181034
Yang CC, Zhu LF, Xu XH et al (2013) Membrane type 1 matrix metalloproteinase induces an epithelial to mesenchymal transition and cancer stem cell-like properties in SCC9 cells. BMC Cancer 13:171. https://doi.org/10.1186/1471-2407-13-171
Hjelmeland AB, Wu Q, Heddleston JM et al (2011) Acidic stress promotes a glioma stem cell phenotype. Cell Death Differ 18(5):829–840. https://doi.org/10.1038/cdd.2010.150
Huang S, Tang Y, Peng X et al (2016) Acidic extracellular pH promotes prostate cancer bone metastasis by enhancing PC-3 stem cell characteristics, cell invasiveness and VEGF-induced vasculogenesis of BM-EPCs. Oncol Rep 36(4):2025–2032. https://doi.org/10.3892/or.2016.4997
Kessenbrock K, Dijkgraaf GJ, Lawson DA et al (2013) A role for matrix metalloproteinases in regulating mammary stem cell function via the Wnt signaling pathway. Cell Stem Cell 13(3):300–313. https://doi.org/10.1016/j.stem.2013.06.005
Sawey ET, Johnson JA, Crawford HC (2007) Matrix metalloproteinase 7 controls pancreatic acinar cell transdifferentiation by activating the Notch signaling pathway. Proc Natl Acad Sci U S A 104(49):19327–19332. https://doi.org/10.1073/pnas.0705953104
Heissig B, Hattori K, Dias S et al (2002) Recruitment of stem and progenitor cells from the bone marrow niche requires MMP-9 mediated release of kit-ligand. Cell 109(5):625–637. https://doi.org/10.1016/S0092-8674(02)00754-7
Justilien V, Regala RP, Tseng IC et al (2012) Matrix metalloproteinase-10 is required for lung cancer stem cell maintenance, tumor initiation and metastatic potential. PLoS One 7(4):e35040. https://doi.org/10.1371/journal.pone.0035040
Nishida C, Kusubata K, Tashiro Y et al (2012) MT1-MMP plays a critical role in hematopoiesis by regulating HIF-mediated chemokine/cytokine gene transcription within niche cells. Blood 119(23):5405–5416. https://doi.org/10.1182/blood-2011-11-390849
Sakamoto T, Seiki M (2010) A membrane protease regulates energy production in macrophages by activating hypoxia-inducible factor-1 via a non-proteolytic mechanism. J Biol Chem 285(39):29951–29964. https://doi.org/10.1074/jbc.M110.132704
Levesque JP, Hendy J, Takamatsu Y (2003) Disruption of the CXCR4/CXCL12 chemotactic interaction during hematopoietic stem cell mobilization induce by GCSF or cyclophosphamide. J Clin Invest 111(2):187–196. https://doi.org/10.1172/JCI15994
McQuibban GA, Butler GS, Gong JH et al (2001) Matrix metalloproteinase activity inactivates the CXC chemokine stromal cell-derived factor-1. J Biol Chem 276(47):43503–43508. https://doi.org/10.1074/jbc.M107736200
Steinl C, Essl M, Schreiber TD et al (2013) Release of matrix metalloproteinase-8 during physiological trafficking and induced mobilization of human hematopoietic stem cells. Stem Cells Dev 22(9):1307–1318. https://doi.org/10.1089/scd.2012.0063
Sheu BC, Hsu SM, Ho HN et al (2001) A novel role of metalloproteinase in cancer-mediated immunosuppression. Cancer Res 61(1):237–242. DOI: not available
Yamada N, Yamanegi K, Ohyama H et al (2012) Hypoxia downregulates the expression of cell surface MICA without increasing soluble MICA in osteosarcoma cells in a HIF-1α dependent manner. Int J Oncol 41(6):2005–2012. https://doi.org/10.3892/ijo.2012.1630
Yang FQ, Liu M, Yang FP et al (2014) Matrix metallopeptidase 2 (MMP-2) mediates MHC class I polypeptide-related sequence A (MICA) shedding in renal cell carcinoma. Actas Urol Esp 38(3):172–178. https://doi.org/10.1016/j.acuro.2013.09.015
Sun D, Wang X, Zhang H et al (2011) MMP9 mediates MICA shedding in human osteosarcomas. Cell Biol Int 35(6):569–574. https://doi.org/10.1042/CBI20100431
Liu G, Atteridge CL, Wang X et al (2010) The membrane type matrix metalloproteinase MMP14 mediates constitutive shedding of MHC class 1 chain-related molecule A independent of A disintegrin and metalloproteinases. J Immunol 184(7):3346–3350. https://doi.org/10.4049/jimmunol.0903789
Ziani L, Safta-Saadoun TB, Gourbeix J et al (2017) Melanoma-associated fibroblasts decrease tumor cell susceptibility to NK cell-mediated killing through matrix-metalloproteinases secretion. Oncotarget 8(12):19780.19794. https://doi.org/10.18632/oncotarget.15540
Jenkins G (2008) The role of proteases in transforming growth factor-beta activation. Int J Biochem Cell Biol 40(6–7):1068–1078. https://doi.org/10.1016/j.biocel.2007.11.026
Gorelik L, Flavell RA (2001) Immune-mediated eradication of tumors through the blockade of transforming growth factor-beta signaling in T cells. Nat Med 7(10):1118–1122. https://doi.org/10.1038/nm1001-1118
Kopp HG, Placke T, Salih HR (2009) Platelet-derived transforming growth factor-beta down-regulates NKG2D thereby inhibiting natural killer cell antitumor reactivity. Cancer Res 69(19):7775–7783. https://doi.org/10.1158/0008-5472.CAN-09-2123
Bonavita E, Galdiero MR, Jaillon S et al (2015) Phagocytes as corrupted policemen in cancer-related inflammation. Adv Cancer Res 128:141–171. https://doi.org/10.1016/bs.acr.2015.04.013
Sousa S, Brion R, Lintunen M et al (2015) Human breast cancer cells educate macrophages toward the M2 activation status. Breast Cancer Res 17:101. https://doi.org/10.1186/s13058-015-0621-0
Kamoshida G, Matsuda A, Miura R et al (2013) Potentiation of tumor cell invasion by co-culture with monocytes accompanying enhance production of matrix metalloproteinase and fibronectin. Clin Exp Metastasis 30(3):289–297. https://doi.org/10.1007/s10585-012-9536-7
Whipple CA (2015) Tumor talk: understanding the conversation between the tumor and its microenvironment. Cancer Cell Microenviron 2(2):e773. DOI: not available.
Vinnakota K, Zhang Y, Selvanesan BC et al (2017) M2-like macrophages induce colon cancer cell invasion via matrix metalloproteinases. J Cell Physiol 232(12):3468–3480. https://doi.org/10.1002/jcp.25808
Pelekanou V, Villarroel-Espindola F, Schalper KA et al (2018) CD68, CD163, and matrix metalloproteinase 9 (MMP-9) co-localization in breast tumor microenvironment predicts survival differently in ER-positive and -negative cancers. Breast Cancer Res 20(1):154. https://doi.org/10.1186/s13058-018-1076-x
Pettersen JS, Fuentes-Duculan J, Suárez-Fariñas M, et al (2011) Tumor-associated macrophages in the cutaneous SCC microenvironment are heterogeneously activated. J Invest Dermatol 131(6):1322–1330. https://doi.org/10.1038/jid.2011.9
Fujimura T, Kakizaki A, Sato Y et al (2017) The immunological roles of periostin/tumor-associated macrophages axis in development of dermatofibrosarcoma protuberans. Anticancer Res 37(6):2867–2873. https://doi.org/10.21873/anticanres.11639
Mantovani A (2009) The yin-yan of tumor-associate neutrophils. Cancer Cell 16(3):173–174. https://doi.org/10.1016/j.ccr.2009.08.014
Varol C, Sagi I (2018) Phagocyte-extracellular matrix crosstalk empowers tumor development and dissemination. FEBS J 285(4):734–751. https://doi.org/10.1111/febs.14317
Singh S, Mehta N, Lilian J et al (2017) Initiative action of tumor-associated macrophage during tumor metastasis. Biochim Open 4:8–18. https://doi.org/10.1016/j.biopen.2016.11.002
Hurt B, Schulick R, Edil B et al (2017) Cancer-promoting mechanisms of tumor-associated neutrophils. Am J Surg 214(5):938–944. https://doi.org/10.1016/j.amjsurg.2017.08.003
Vannitamby A, Seow HJ, Anderson G et al (2017) Tumour-associated neutrophils and loss of epithelial PTEN can promote corticosteroid-insensitive MMP-9 expression in the chronically inflamed lung microenvironment. Thorax 72(12):1140–1143. https://doi.org/10.1136/thoraxjnl-2016-209389
Benson DD, Meng X, Fullerton DA et al (2012) Activation state of stromal inflammatory cells in murine metastatic pancreatic adenocarcinoma. Am J Physiol Regul Intergr Comp Physiol 302(9):R1067–R1075. https://doi.org/10.1152/ajpregu.00320.2011
Ardi VC, Van den Steen PE, Opdenakker G et al (2009) Neutrophil MMP-9 proenzyme, unencumbered by TIMP-1, undergoes efficient activation in vivo and catalytically induces angiogenesis via basic fibroblast growth factor (FCG-2)/FGFR-2 pathway. J Biol Chem 284(38):25854–25866. https://doi.org/10.1074/jbc.M109.033472
Deryugina EI, Zajac E, Juncker-Jensen A et al (2014) Tissue-infiltrating neutrophils constitute the major in vivo source of angiogenesis-inducing MMP-9 in the tumor microenvironment. Neoplasia 16(10):771–788. https://doi.org/10.1016/j.neo.2014.08.013
Yan L, Borregaard N, Kjeldsen L et al (2001) The high molecular weight urinary matrix metalloproteinase (MMP) activity is a complex of gelatinase B/MMP-9 and neutrophil gelatinase associated lipocalin (NGAL). Modulation of MMP-9 activity by NGAL. J Biol Chem 276(40):37258–37265. https://doi.org/10.1074/jbc.M106089200
Bolignano D, Donato V, Lacquaniti A et al (2010) Neutrophil gelatinase-associated lipocalin (NGAL) in human neoplasias: a new protein enters the scene. Cancer Lett 288(1):10–16. https://doi.org/10.1016/j.canlet.2009.05.027
Coussens LM, Tinkle CL, Hanahan D et al (2000) MMP-9 supplied by bone marrow-derived cells contributes to skin carcinogenesis. Cell 103(3):481–490. https://doi.org/10.1016/s0092-8674(00)00139-2
Acuff HB, Carter KJ, Fingleton B et al (2006) Matrix metalloproteinase-9 from bone marrow derived cells contributes to survival but not growth of tumor cells in the lung microenvironment. Cancer Res 66(1):259–266. https://doi.org/10.1158/0008-5472.CAN-05-2502
Lin C, Lin W, Yeh S et al (2015) Infiltrating neutrophils increase bladder cancer cell invasion via modulation of androgen receptor (AR)/MMP-13 signals. Oncotarget 6(40):43081–43089. https://doi.org/10.18632/oncotarget.5638
Cools-Lartigue J, Spicer J, Najmeh S et al (2014) Neutrophil extracellular traps in cancer progression. Cell Mol Life Sci 71(21):4179–4194. https://doi.org/10.1007/s00018-014-1683-3
Komi DEA, Redegeld FA (2019) Role of mast cells in shaping the tumor microenvironment. Clin Rev Allergy Immunol. https://doi.org/10.1007/s12016-019-08753-w
Theoharides TC, Conti P (2004) Mast cells: the Jekyll and Hyde of tumor growth. Trends Immunol 25(5):235–241. https://doi.org/10.1016/j.it.2004.02.013
Dyduch G, Kaczmarczyk K, Okoń K (2012) Mast cells and cancer: enemies or allies? Pol J Pathol 63(1):1–7. DOI: not available
Baram D, Vaday GG, Salamon P et al (2001) Human mast cells release metalloproteinase-9 on contact with activated T cells: juxtacrine regulation by TNF-alpha. J Immunol 167(7):4008–4016. https://doi.org/10.4049/jimmunol.167.7.4008
Fang KC, Wolters PJ, Steinhoff M et al (1999) Mast cell expression of gelatinases A and B is regulated by kit ligand and TGF-beta. J Immunol 162(9):5528–5535. DOI: not available
Pittoni P, Tripodo C, Piconese S et al (2011) Mast cell targeting hampers prostate adenocarcinoma development but promotes the occurrence of highly malignant neuroendocrine cancers. Cancer Res 71(18):5987–5997. https://doi.org/10.1158/0008-5472.CAN-11-1637
Di Girolamo N, Wakefield D (2000) In vitro and in vivo expression of interstitial collagenase/MMP-1 by human mast cells. Dev Immunol 7(2–4):131–142. https://doi.org/10.1155/2000/82708
Vyzoukaki R, Tsirakis G, Pappa CA et al (2015) The impact of mast cell density on the progression of bone disease in multiple myeloma patients. Int Arch Allergy Immunol 168(4):263–268. https://doi.org/10.1159/000443275
Jiang Y, Wu Y, Hardie WJ et al (2017) Mast cell chymase affects the proliferation and metastasis of lung carcinoma cells in vitro. Oncol Lett 14(3):3193–3198. https://doi.org/10.3892/ol.2017.6487
Ribatti D (2013) Mast cells and macrophages exert beneficial and detrimental effects on tumor progression and angiogenesis. Immunol Lett 152(2):83–88. https://doi.org/10.1016/j.imlet.2013.05.003
Räsänen K, Vheri A (2010) Activation of fibroblasts in cancer stroma. Exp Cell Res 16(17):2713–2722. https://doi.org/10.1016/j.yexcr.2010.04.032
Shiga K, Hara M, Nagasaki T et al (2015) Cancer-associated fibroblasts: their characteristics and their roles in tumor growth. Cancers (Basel) 7(4):2443–2458. https://doi.org/10.3390/cancers7040902
Heneberg P (2016) Paracrine tumor signaling induces transdifferentiation of surrounding fibroblasts. Crit Rev Oncol Hematol 97:303–311. https://doi.org/10.1016/j.critrevonc.2015.09.008
Weber CE, Kothari AN, Wai PY et al (2015) Osteopontin mediates an MZF1-TGF-β1-dependent transformation of mesenchymal stem cell into cancer-associated fibroblast in breast cancer. Oncogene 34(37):4821–4833. https://doi.org/10.1038/onc.2014.410
Tsellou E, Kiaris H (2008) Fibroblast independency in tumors: implications in cancer therapy. Future Oncol 4(3):427–432. https://doi.org/10.2217/14796694.4.3.427
De Wever O, Van Bockstal M, Mareel M et al (2014) Carcinoma-associated fibroblasts provide operational flexibility in metastasis. Semin Cancer Biol 25:35–46. https://doi.org/10.1016/j.semcancer.2013.12.009
Kwa MQ, Herum KM, Brakebusch C (2019) Cancer-associated fibroblasts: how do they contribute to metastasis? Clin Exp Metastasis 36(2):71–86. https://doi.org/10.1007/s10585-019-09959-0
Liu T, Zhou L, Li D et al (2019) Cancer-associated fibroblasts build and secure the tumor microenvironment. Front Cell Dev Biol 7(60). https://doi.org/10.3389/fcell.2019.00060
Kessenbrock K, Plaks V, Werb Z (2010) Matrix metalloproteinases: regulators of the tumor microenvironment. Cell 141(1):52–67. https://doi.org/10.1016/j.cell.2010.03.015
Eck SM, Côté AL, Winkelman WD et al (2009) CXCR4 and matrix metalloproteinase-1 are elevated in breast carcinoma-associated fibroblasts and in normal mammary fibroblasts exposed to factors secreted by breast cancer cells. Mol Cancer Res 7(7):1033–1044. https://doi.org/10.1158/1541-7786.MCR-09-0015
Boire A, Covic L, Agarwal A et al (2005) PAR1 is a matrix metalloprotease-1 receptor that promotes invasion and tumorigenesis of breast cancer cells. Cell 120(3):303–313. https://doi.org/10.1016/j.cell.2004.12.018
Wang T, Jia J, Zhang H et al (2017) TGF-β induced PAR-1 expression promotes tumor progression and osteoclast differentiation in giant cell tumor of bone. Int J Cancer 141(8):1630–1642. https://doi.org/10.1002/ijc.30862
Gaggioli C, Hooper S, Hidalgo-Carcedo C et al (2007) Fibroblast-led collective invasion of carcinoma cells with differing roles for RhoGTPases in leading and following cells. Nat Cell Biol 9(12):1392–1400. https://doi.org/10.1038/ncb1658
Yamaguchi H, Sakai R (2015) Direct interaction between carcinoma cells and cancer associated fibroblasts for the regulation of cancer invasion. Cancers (Basel) 7(4):2054–2062. https://doi.org/10.3390/cancers7040876
Bates AL, Pickup MW, Hallett MA et al (2015) Stromal matrix metalloproteinase 2 regulates collagen expression and promotes the outgrowth of experimental metastases. J Pathol 235(5):773–783. https://doi.org/10.1002/path.4493
Lederle W, Hartentein B, Meides A et al (2010) MMP13 as a stromal mediator in controlling persistent angiogenesis in skin carcinoma. Carcinogenesis 31(7):1175–1184. https://doi.org/10.1093/carcin/bgp248
Egelbad M, Littlepage LE, Werb Z (2005) The fibroblastic coconspirator in cancer progression. Cold Sping Harb Symp Quant Biol 70:383–388. https://doi.org/10.1101/sqb.2005.70.007
Schmidt-Hansen B, Ornas D, Grigorian M et al (2004) Extracellular S100A4(mts1) stimulates invasive growth of mouse endothelial cells and modulates MMP-13 matrix metalloproteinase activity. Oncogene 23(32):5487–5495. https://doi.org/10.1038/sj.onc.1207720
Gaud G, Iochmann S, Guillon-Munos A et al (2011) TFPI-2 silencing increases tumour progression and promotes metalloproteinase 1 and 3 through tumour-stromal cell interactions. J Cell Mol Med 15(2):196–208. https://doi.org/10.1111/j.1582-4934.2009.00989.x
Wang J, Ying G, Wang J (2010) Characterization of phosphoglycerate kinase-1 expression of stromal cells derived from tumor microenvironment in prostate cancer progression. Cancer Res 70(2):471–480. https://doi.org/10.1158/0008-5472.CAN-09-2863
Nieman KM, Romero IL, Houten B et al (2013) Adipose tissue and adipocytes support tumorigenesis and metastasis. Biochim Biopys Acta 1831(10):1533–1541. https://doi.org/10.1016/j.bbalip.2013.02.010
Tan J, Buache E, Chenard MP et al (2011) Adipocyte is a non-trivial, dynamic partner of breast cancer cells. Int J Dev Biol 55(7–9):851–859. https://doi.org/10.1387/ijdb.113365jt
Bochet L, Lehuédé C, Dauvillier S et al (2013) Adipocyte-derived fibroblasts promote tumor progression and contribute to the desmoplastic reaction in breast cancer. Cancer Res 73(18):5657–5668. https://doi.org/10.1158/0008-5472.CAN-13-0530
Choi J, Cha YJ, Koo JS (2018) Adipocyte biology in breast cancer: from silent bystander to active facilitator. Prog Lipid Res 69:11–20. https://doi.org/10.1016/j.plipres.2017.11.002
Yao-Borengasser A, Monzavi-Karbassi B, Hedges RA et al (2015) Adipocyte hypoxia promotes epithelial-mesenchymal transition-related gene expression and estrogen receptor-negative phenotype in breast cancer cells. Oncol Rep 33(6):2689–2694. https://doi.org/10.3892/or.2015.3880
Andarawewa KL, Motrescu ER, Chenard MP et al (2005) Stromelysin-3 is a potent negative regulator of adipogenesis participating to cancer cell-adipocyte interaction/crosstalk at the tumor invasive front. Cancer Res 65(23):108562–110871. https://doi.org/10.1158/0008-5472.CAN-05-1231
Motrescu ER, Blaise S, Etique N et al (2008) Matrix metalloproteinase-11/sromelysin-3 exhibits collagenolytic function against collagen VI under normal and malignant conditions. Oncogene 27(49):6347–6355. https://doi.org/10.1038/onc.2008.218
Park J, Scherer PE (2012) Adipocyte-derived endotrophin promotes malignant tumor progression. J Clin Invest 122(11):4243–4256. https://doi.org/10.1172/JCI63930
Ito Y, Ishiguro H, Kobayashi N et al (2015) Adipocyte-derived monocyte chemotactic protein-1(MCP-1) promotes prostate cancer progression trough the induction of MMP-2 activity. Prostate 75(10):1009–1019. https://doi.org/10.1002/pros.22972
Xie H, Li L, Zhu G et al (2015) Infiltrated pre-adipocytes increase prostate cancer metastasis via modulation of the miR-301a/androgen receptor (AR)/TGFβ1/Smad/MMP9 signals. Oncotarget 6(14):12326–12339. https://doi.org/10.18632/oncotarget.3619
Ghasemi A, Saeidi J, Azimi-Nejad M et al (2019) Leptin-induced signaling pathways in cancer migration and invasion. Cell Oncol (Dordr) 42(3):243–260. https://doi.org/10.1007/s13402-019-00428-0
Fan Y, Gan Y, Shen Y et al (2015) Leptin signaling enhances cell invasión and promotes the metastasis of human pancreatic cancer via increasing MMP-13 production. Oncotarget 6(18):16120–16134. https://doi.org/10.18632/oncotarget.3878
Yeh WL, Lu DY, Lee MJ et al (2009) Leptin induces migration and invasion of glioma cells through MMP-13 production. Glia 57(4):454–464. https://doi.org/10.1002/glia.20773
Strong AL, Ohlstein JF, Biagas BA, et al (2015) Leptin produced by obese adipose stromal /stem cells enhances proliferation and metastasis of estrogen receptor positive breast cancers. Breast Cancer Res 17:112. https://doi.org/10.1186/s13058-015-0622-z
Strong AL, Semon JA, Strong TA, et al (2012) Obesity-associated dysregulation of calpastatin and MMP-15 in adipose-derived stromal cells results in their enhanced invasion. Stem Cells 30(12):2774-2783. https://doi.org/10.1002/stem.1229
Ghasemi A, Hashemy SI, Aghaei M et al (2018) Leptin induces matrix metalloproteinase 7 expression to promote ovarian cancer cell invasion by activating ERK and JNK pathways. J Cell Biochem 119(2):2333–2344. https://doi.org/10.1002/jcb.26396
Chang MC, Chen CA, Chen PJ et al (2012) Mesothelin enhances invasion of ovarian cancer by inducing MMP-7 through MAPK/ERK and JNK pathways. Biochem J 442(2):293–302. https://doi.org/10.1042/BJ20110282
Wang FQ, So J, Reierstad S et al (2005) Matrilysin (MMP-7) promotes invasion of ovarian cancer cells by activation of progelatinase. Int J Cancer 114(1):19–31. https://doi.org/10.1002/ijc.20697
Dong Z, Xu X, Du L et al (2013) Leptin-mediated regulation of MT1-MMP localization is KIF1B dependent and enhances gastric cancer cell invasion. Carcinogenesis 34(5):974–983. https://doi.org/10.1093/carcin/bgt028
Wang H, Cheng H, Shao Q et al (2014) Leptin-promoted human extravillous trophoblast invasion is MMP14 dependent and requires the cross talk between Notch1 and PI3K/Akt signaling. Biol Reprod 90(4):78. https://doi.org/10.1095/biolreprod.113.114876
Shimoda M, Khokha R (2017) Metalloproteinases in extracellular vesicles. Biochim Biophys Acta, Mol Cell Res 1864(11 PtA):1989–2000. https://doi.org/10.1016/j.bbamcr.2017.05.027
Choi D, Lee TH, Spinelli C et al (2017) Extracellular vesicle communication pathways as regulatory targets of oncogenic transformation. Semin Cell Dev Biol 67:11.22. https://doi.org/10.1016/j.semcdb.2017.01.003
Shay G, Lynch CC, Fingleton B (2015) Moving targets: emerging roles for MMPs in cancer progression and metastasis. Matrix Biol 44–46:200–206. https://doi.org/10.1016/j.matbio.2015.01.019
Hakulinen J, Sankkila L, Sugiyama N et al (2008) Secretion of active membrane type 1 matrix metalloproteinase (MMP-14) into extracellular space in microvesicular exosomes. J Cell Biochem 105(5):1211–1218. https://doi.org/10.1002/jcb.21923
Carmeliet P, Jain RK (2011) Molecular mechanisms and clinical applications of angiogenesis. Nature 473(7347):298–307. https://doi.org/10.1038/nature10144
Tsuchiya K, Hida K, Hida Y et al (2010) Adrenomedullin antagonist suppresses tumor formation in renal cell carcinoma through inhibitory effects on tumor endothelial cells and endothelial progenitor mobilization. Int J Oncol 36(6):1379–1386. https://doi.org/10.3892/ijo_00000622
Hida K, Kawamoto T, Ohga N et al (2011) Altered angiogenesis in the tumor microenvironment. Pathol Int 61(11):630–637. https://doi.org/10.1111/j.1440-1827.2011.02726.x
Ucuzian A, Am Gassman AA, East AT et al (2010) Molecular mediators of angiogenesis. J Burn Care Res 31(1):158–175. https://doi.org/10.1097/BCR.0b013e3181c7ed82
Mazor R, Asaigh T, Shaked H et al (2013) Matrix metalloproteinase-1-mediated up-regulation of vascular endothelial growth factor-2 in endothelial cells. J Biol Chem 288(1):598–607. https://doi.org/10.1074/jbc.M112.417451
Gupta GP, Nguyen DX, Chiang AC et al (2007) Mediators of vascular remodeling co-opted for sequential steps in lung metastasis. Nature 446(7137):765–770. https://doi.org/10.1038/nature05760
Ito TK, Ishii G, Saito S et al (2009) Degradation of soluble VEGF receptor-1 by MMP-7 allows VEGF access to endothelial cells. Blood 113(10):2363–2369. https://doi.org/10.1182/blood-2008-08-172742
Fang C, Wen G, Zhang L et al (2013) An important role of matrix metalloproteinase-8 in angiogenesis in vitro and in vivo. Cardiovasc Res 99(1):146–155. https://doi.org/10.1093/cvr/cvt060
Andreuzzi E, Colladel R, Pellicani R et al (2017) The angiostatic molecule Multimerin 2 is processed by MMP-9 to allows sprouting angiogenesis. Matrix Biol 64:40–53. https://doi.org/10.1016/j.matbio.2017.04.002
Lorenzon E, Colladel R, Andreuzzi E et al (2012) MULTIMERIN2 impairs tumor angiogenesis and growth by interfering with VEGF-A/VEGFR2 pathway. Oncogene 31(26):3136–3147. https://doi.org/10.1038/onc.2011.487
Chantrain CF, Shimada H, Jodele S et al (2004) Stromal matrix metalloproteinase-9 regulates the vascular architecture in neuroblastoma by promoting pericyte recruitment. Cancer Res 64(5):1675–1686. https://doi.org/10.1158/0008-5472.can-03-0160
Davis GF, Statman AN, Sacharidou A et al (2011) Molecular basis for endothelial lumen formation and tubulogenesis during vasculogenesis and angiogenic sprouting. Int Rev Cell Mol Bio 288:101–165. https://doi.org/10.1016/B978-0-12-386041-5.00003-0
Saunders WB, Bohnsack BL, Faske JB et al (2006) Coregulation of vascular tube stabilization by endothelial cell TIMP-2 and pericyte TIMP-3. J Cell Biol 175(1):179–191. https://doi.org/10.1083/jcb.200603176
Stratman AN, Malotte KM, Mahan RD et al (2009) Pericyte recruitment during vasculogenic tube assemble stimulates endothelial basement membrane matrix formation. Blood 114(24):5091–5101. https://doi.org/10.1182/blood-2009-05-222364
Lehti K, Rose NF, Valavaara S et al (2009) MT1-MMP promotes vascular smooth muscle dedifferentiation through LRP1 processing. J Cell Sci 122(Pt1):126–135. https://doi.org/10.1242/jcs.035279
Chan KC, Ko JM, Lung HL et al (2011) Catalytic activity of matrix metalloproteinase-19 is essential for tumor suppressor and anti-angiogenic activities in nasopharyngeal carcinoma. Int J Cancer 129(8):1826–1837. https://doi.org/10.1002/ijc.25855
Lee S, Jilani SM, Nikolova GV et al (2005) Processing of VEGF-A by matrix metalloproteinases regulates bioavailability and vascular patterning in tumors. J Cell Biol 269(64):681–691. https://doi.org/10.1083/jcb.200409115
Tabruyn SP, Griffioen AW (2007) Molecular pathways of angiogenesis inhibition. Biochem Biophys Res Commun 355(1):1–5. https://doi.org/10.1016/j.bbrc.2007.01.123
Radziwon-Balicka A, Ramer C, Moncada del la Rosa C et al (2013) Angiostatin inhibits endothelial MMP-2 and MMP-14 expression: a hypoxia specific mechanism of action. Vasc Pharmacol 58(4):280–291. https://doi.org/10.1016/j.vph.2012.11.003
Monboisse JC, Oudart JB, Ramont L et al (2014) Matrikines from basement membrane collagens: a new anti-cancer strategy. Biochim Biophys Acta 1840(8):2589–2598. https://doi.org/10.1016/j.bbagen.2013.12.029
Ricard-Blum S, Salza R (2014) Matricryptins and matrikines: biologically active fragments of the extracellular matrix. Exp Dermatol 23(7):457–463. https://doi.org/10.1111/exd.12435
Ricard-Blum VSD (2016) Matricryptins network with matricellular receptors at the surface of endothelial and tumor cells. Front Pharmacol 7(11). https://doi.org/10.3389/fphar.2016.00011
Kalluri R (2003) Basement membranes: structure, assembly and role in tumour angiogenesis. Nat Rev Cancer 3(6):422–433. https://doi.org/10.1038/nrc1094
Lee SJ, Jang JW, Kim YM et al (2002) Endostatin binds to the catalytic domain of matrix metalloproteinase-2. FEBS Lett 519(1–3):147–152. https://doi.org/10.1016/s0014-5793(02)02742-4
Bellon G, Martiny L, Robinet A (2004) Matrix metalloproteinases and matrikines in angiogenesis. Crit Rev Oncol Hematol 49(3):203–220. https://doi.org/10.1016/j.critrevonc.2003.10.004
Kholia S, Ranghino A, Garnieri P et al (2016) Extracellular vesicles as new players in angiogenesis. Vasc Pharmacol 86:64–70. https://doi.org/10.1016/j.vph.2016.03.005
Taraboletti G, D’Ascenzo S, Borsotti P et al (2002) Shedding of the matrix metalloproteinases MMP-2, MMP-9 and MT1-MMP as membrane vesicle-associated components by endothelial cells. Am J Pathol 160(2):673–680. https://doi.org/10.1016/S0002-9440(10)64887-0
Millimaggi D, Mari M, D’Ascenzo S et al (2007) Tumor vesicle-associated CD147 modulates the angiogenic capability of endothelial cells. Neoplasia 9(4):349–357. https://doi.org/10.1593/neo.07133
Tammela T, Alitalo K (2010) Lymphangiogenesis: molecular mechanisms and future promise. Cell 140(4):460–476. https://doi.org/10.1016/j.cell.2010.01.045
Cao Y (2005) Opinion: emerging mechanisms of tumour lymphangiogenesis and lymphatic metastasis. Nat Rev Cancer 5(9):735–743. https://doi.org/10.1038/nrc1693
Qiu X, Yao S, Zhang S (2010) Advances in the research on lymphangiogenesis in carcinoma tissues. Oncol Lett 1(4):579–582. https://doi.org/10.3892/ol_00000102
Kerjaschki D (2005) The crucial role of macrophages in lymphangiogenesis. J Clin Invest 115(9):2316–2319. https://doi.org/10.1172/JCI26354
Karaman S, Detmar M (2014) Mechanisms of lymphatic metastasis. J Clin Invest 124(3):922–928. https://doi.org/10.1172/JCI71606
Archen MG, Stacker SA (2008) Molecular control of lymphatic metastasis. Ann N Y Acad Sci 1131:225–2234. http://doi.org/10.1196/annals.1413.020
Zheng W, Aspelund A, Alitalo K (2014) Lymphangiogenic factors, mechanisms, and applications. J Clin Invest 124(3):878–887. https://doi.org/10.1172/JCI71603
Spinella F, Caprara V, Garrafa E et al (2010) Endothelin axis induces metalloproteinase activation an invasiveness in human lymphatic endothelial cells. Can J Physiol Pharmacol 88(8):782–787. https://doi.org/10.1139/Y10-050
Detry B, Erpicum C, Paupert J et al (2012) Matrix metalloproteinase-2 governs lymphatic vessel formation as an interstitial collagenase. Blood 119(21):5048–5056. https://doi.org/10.1182/blood-2011-12-400267
Du HT, Du LL, Tang XL et al (2017) Blockade of MMP-2 and MMP-9 inhibits corneal lymphangiogenesis. Graefes Arch Clin Exp Ophthalmol 255(8):1573–1579. https://doi.org/10.1007/s00417-017-3651-8
Xu L, Sun K, Xia M et al (2015) MMP13 regulates aggressiveness of pediatric multiple myeloma through VEGF-C. Cell Physiol Biochem 36(2):509–516. https://doi.org/10.1159/000430116
Ingvarsen S, Porse A, Erpicum C et al (2013) Targeting a single function of the multifunctional matrix metalloproteinase MT1-MMP: impact on lymphangiogenesis. J Biol Chem 288(15):10195–10204. https://doi.org/10.1074/jbc.M112.447169
Wong HL, Jin G, Cao R et al (2016) MT1-MMP sheds LYVE-1 on lymphatic endothelial cells and suppresses VEGF-C production to inhibit lymphangiogenesis. Nat Commun 7:10824. https://doi.org/10.1038/ncomms10824
Tatti O, Gucciardo E, Pekkonen P et al (2015) MMP16 mediates a proteolytic switch to promote cell-cell adhesion, collagen alignment, and lymphatic invasion in melanoma. Cancer Res 75(10):2083–2094. https://doi.org/10.1158/0008-5472.CAN-14-1923
Butcher DT, Alliston T, Weaver VM (2009) A tense situation: forcing tumour progression. Nat Rev Cancer 9(2):108–122. https://doi.org/10.1038/nrc2544
Lu P, Weaver VM, Werb Z (2012) The extracellular matrix: a dynamic niche in cancer progression. J Cell Biol 196(4):395–406. https://doi.org/10.1083/jcb.201102147
Pandya P, Orgaz JL, Sanz-Moreno V (2017) Modes of invasion during tumour dissemination. Mol Oncol 11(1):5–27. https://doi.org/10.1002/1878-0261.12019
Schütz A, Röser K, Klitzsch J et al (2015) Lung adenocarcinoma and lung cancer cell lines show association of MMP-1 expression with STAT3 activation. Transl Oncol 8(2):97–105. https://doi.org/10.1016/j.tranon.2015.02.002
Orgaz JL, Pandya P, Dalmeida R et al (2014) Diverse matrix metalloproteinase functions regulate cancer amoeboid migration. Nat Commun 5:4255. https://doi.org/10.1038/ncomms5255
Ridley AJ (2011) Life at the leading edge. Cell 145(7):1012–1022. https://doi.org/10.1016/j.cell.2011.06.010
Sabeh F, Shimizu-Hirota R, Weiss SJ (2009) Protease-dependent versus-independent cancer cell invasion programs: three-dimensional amoeboid movement revisited. J Cell Biol 185(1):11–19. https://doi.org/10.1083/jcb.200807195
Jacob A, Prekeris R (2015) The regulation of MMP targeting to invadopodia during cancer metastasis. Front Cell Dev Biol 3(4). https://doi.org/10.3389/fcell.2015.00004
Andarawewa KL, Boulay A, Masson R et al (2003) Dual stromelysin-3 function during natural mouse mammary tumor virus-ras tumor progression. Cancer Res 63(18):5844–5849. DOI: not available
Brasse D, Mathelin C, Leroux K et al (2010) Matrix metalloproteinase 11/stromelysin-3 exerts both activator and repressor functions during the hematogenous metastatic process in mice. Int J Cancer 127(6):1347–1355. https://doi.org/10.1002/ijc.25309
Li W, Saji S, Sato F et al (2013) Potential clinical application of matrix metalloproteinase inhibitors and their future prospects. Int J Biol Markers 28(2):117–130. https://doi.org/10.5301/jbm.5000026
Yang JS, Lin CW, Su SC et al (2016) Pharmacodynamic considerations in the use of matrix metalloproteinase inhibitors in cancer treatment. Expert Opin Drug Metab Toxicol 12(2):191–200. https://doi.org/10.1517/17425255.2016.1131820
Bahrami B, Hojjat-Farsangi M, Mohammadi H et al (2017) Nanoparticles and targeted drug delivery in cancer therapy. Immunol Lett 190:64–83. https://doi.org/10.1016/j.imlet.2017.07.015
Li M, Zhang F, Su Y et al (2018) Nanoparticles designed to regulate tumor microenvironment for cancer therapy. Life Sci 201:37–44. https://doi.org/10.1016/j.lfs.2018.03.044
Roy Chowdhury M, Schumann C, Bhakta-Guha D et al (2016) Cancer nanotheranostics: strategies, promises and impediments. Biomed Pharmaother 84:291–304. https://doi.org/10.1016/j.biopha.2016.09.035
Li R, Wu W, Liu Q et al (2013) Intelligently targeted drug delivery and enhanced antitumor effect by gelatinase-responsive nanoparticles. PLoS One 8(7):e69643. https://doi.org/10.1371/journal.pone.0069643
Zhu L, Wang T, Perche F et al (2013) Enhanced anticancer activity of nanopreparation containing an MMP2-sensitive PEG-drug conjugate and cell-penetrating moiety. Proc Natl Acad Sci U S A 110(42):17047–17052. https://doi.org/10.1073/pnas.1304987110
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Gonzalez-Avila, G., Sommer, B., García-Hernández, A.A., Ramos, C. (2020). Matrix Metalloproteinases’ Role in Tumor Microenvironment. In: Birbrair, A. (eds) Tumor Microenvironment. Advances in Experimental Medicine and Biology, vol 1245. Springer, Cham. https://doi.org/10.1007/978-3-030-40146-7_5
Download citation
DOI: https://doi.org/10.1007/978-3-030-40146-7_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-40145-0
Online ISBN: 978-3-030-40146-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)