Abstract
Sex-related differences have been identified in various ophthalmic disorders. Sex hormone receptors, such as estrogen receptors, have been found throughout the eye including retina and retinal pigment epithelium (RPE), indicating the importance of hormone regulation in these tissues. In this chapter we will discuss sex differences within the eye and how they relate to retina and RPE health and function. As many autoimmune diseases occur more often in women, we will also examine autoimmune diseases and the secondary effects that may arise within the eye. In addition, the role estrogen plays in systemic inflammation may help in understanding the role of estrogen in the eye. By further understanding the differences between males and females in ocular health, we can provide more tailored treatments for disease and design preventative care aimed at regaining hormonal balance.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
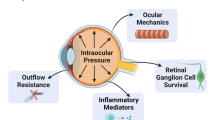
Gender and Sex-Based Differences in Retinal Disease
From cardiovascular to neurological diseases, differences have been observed in disease occurrence between males and females [1,2,3,4]. These sex-based differences are largely attributed to hormone variation, which in females fluctuate at various stages of life such as puberty, pregnancy, menstrual cycles, and menopause [3]. While we know that sex-based differences in disease penetrance and severity exist between females and males, there is still much we do not understand about the factors underlying sex and gender-based differences in disease pathogenesis. Our lack of understanding is largely due to the previous practice in which clinical studies were mainly restricted to male test subjects. By excluding pre-menopausal women from research, it reduced the risk of harm to a fetus in the event of pregnancy, and by excluding women of all ages it was found to reduce experimental deviation brought about by hormone oscillation. This practice also extended into basic science research, with male animals being used primarily for rodent studies. Unfortunately, excluding women from research studies made it impossible to investigate sex and gender differences in disease progression, treatment response, pharmacokinetics, and multiple other critical areas. The NIH Revitalization Act of 1993 established guidelines requiring the inclusion of women and minorities in clinical research. Over two decades later, the NIH has started to implement policies requiring the use of male and female animal and cell-based models in pre-clinical trials as well. These new guidelines have helped to strengthen our understanding of the role that gender and sex-differences play in health and disease. In this chapter, we will explore what is known about sex-differences in ocular diseases, specifically diseases affecting the retina and retinal pigment epithelium (RPE). A greater understanding of sex differences in ocular disease pathogenesis will allow for the development of advanced therapeutics for these diseases. Both gender and sex play a role in women’s health. Gender, which refers to social and cultural differences between men and women, can have a large impact on women’s ocular health. Women have been reported to make up 60% of blindness worldwide [5], with socioeconomical factors believed to play a role. In many parts of the world women are less educated, and have less financial stability than males, resulting in impeded access to healthcare [6, 7]. As ocular trauma due to domestic abuse is more prevalent in women, it may also be considered a gender-based difference [8, 9]. In contrast to gender differences, sex differences refer to biological variables that are different between male and females, such as reproductive organs, encoded DNA, and hormones. Males and females produce different sex-specific hormones (SSH). For women, estrogen and progesterone are produced and released predominantly by the ovaries, while in men, the testes are the main source of androgen production, primarily testosterone. Testosterone in both sexes is also secreted in small amounts by the adrenal glands [10]. Hormone levels fluctuate at different stages of the female menstrual cycle, where estrogen levels peak during the ovulatory phase, and progesterone levels increase during the luteal phase. During pregnancy, estrogen levels remain low, but increase dramatically during the final trimester. In addition, both estrogen and progesterone levels dramatically decrease following menopause. These fluctuations in female hormone levels have been found to correlate with various ocular complications. Intraocular pressure (IOP) is found to be lower during pregnancy [11,12,13,14,15]. However, after menopause when estrogen levels decrease, IOP levels increase [11,12,13,14,15,16]. Differences to the cornea have also been documented with pregnancy, resulting in increased thickness [17, 18], steepening [19] and reduction in cornea sensitivity [20, 21]. In the retina, central serous chorioretinopathy [22] and diabetic retinopathy [23,24,25,26] are associated with pregnancy [22]. Dry age-related macular degeneration (AMD) incident is associated with the start of menopause at an increased age [27]. In general, females are known to have increased risk for dry eye [28], certain forms of glaucoma (although open-angle glaucoma has a lower prevalence in women [29,30,31]), and cataracts [32, 33]. Diseases such as Leber’s Hereditary Optic Neuropathy (LHON) and Coat’s disease, however, are more common in males [34,35,36]. Unlike estrogen, which can fluctuate drastically at different stages of a woman’s life, testosterone levels appear to remain fairly level in men following puberty. Overall, testosterone production is ~20 times greater in males than in females, with plasma clearance of testosterone being approximately twice the amount in females [37, 38]. Progesterone levels between males and females are similar, except during the luteal phase of a woman’s cycle, when levels rise ~3-fold. Based on these sex-specific findings, it is no surprise that hormone regulation can occur in the eye and hormone receptors have been identified throughout the eye.
Retina/RPE Function and Sex Differences
As estrogen levels fluctuate throughout the lifespan of healthy women, effects of these changes on visual function should be examined. Eisner and colleagues measured visual sensitivity through a series of test-wavelengths at different stages of the menstrual cycle [39]. This study observed modulation of short-wavelength sensitive (SWS)-cone mediated sensitivities for one individual out of six that peaked near ovulation, indicating that in some individuals menstrual-related changes in retinal function may occur.
Differences in spatial acuity and contrast sensitivity can be analyzed in rodents using optokinetic reflex (OKR) analyses [40]. Van Alphen and colleagues determined that 4-month old female C57BL/6J mice had no difference in absolute spatial acuity [41]. Our unpublished results, observing the optomoter response to moving sine-wave gratings (OptoMotry), confirm the observation on spatial acuity; with absolute thresholds recorded at 100% contrast, being indistinguishable between 3-month old C57BL/6J males and females (Fig. 11.1a; P = 0.2663). Interestingly in the same study performed by van Alphen, it was determined that 4 month old female C57BL/6J mice had a lower OKR gain when compared to males [41]. This finding further indicates the importance of providing sex-matched controls when studying animals for visual sensitivity.
Sex-differences in C57BL/6J mice RPE response. (a) Optomoter responses were measured for 3 month old male and female C57BL/6J mice. Spatial frequency threshold at a constant speed (12 deg/s) and contrast (100%) was used to measure visual acuity. Here we observed no significant difference in spatial frequency between male and female mice (n = 6–9 mice/group; P = 0.27). (b) Optical coherence tomography (Bioptigen) analysis indicated no significant difference between males and females for RPE (P = 0.64), outer segments (OS; P = 0.97), inner segments (IS; P = 0.72), outer nuclear layer (ONL; P = 0.68), inner nuclear layer (INL; P = 0.42), or whole retina (WR, P = 0.91). (c) Prior to recording fullfield ERG response, mice were dark-adapted overnight. Mice were anesthetized using xylazine (20 mg/kg) and ketamine (80 mg/kg) before pupils were dilated with 2.5% phenylephrine and 1% atropine. Goniovisc (Rancho Cucamonga, CA) was dropped onto the eye to create an electrical contact between the electrode and the cornea, as well as keep the eyes hydrated. The UTAS E-4000 System (LKC Technologies, Gaithersburg, MD) was used to record c-waves in response to 4 s flashes of 100 cd s mm−2. In order to analyze response, the baseline to peak of the c-wave was measured (n = 4 mice/8 eyes per group; P < 0.05). Data are all expressed mean ± SEM
Advances in optical coherence tomography (OCT) technology allows for specific retinal layer thickness and volume to be analyzed in order to monitor healthy and diseased eyes. In a recent study, comparisons between males and females demonstrated significant differences in mean retinal layer thickness, with men having significantly thicker retinal nerve fiber layer, ganglion cell layer, inner plexiform layer, inner retina, inner nuclear layer and outer plexiform layer in the fovea, and outer plexiform layer in the pericentral ring [42]. In contrast, women were shown to have a greater mean thickness of the outer nuclear layer than men [42]. This difference appears to be specific for the human retina, as no sex-specific differences in overall thickness have been observed in 3-month-old C57BL/6J mice, analyzing retina structure by OCT (Bioptigen; Fig. 11.1b).
Electroretinogram (ERG) recordings have also demonstrated varying results between male and females. Females have demonstrated larger amplitudes than males from single flash illumination under scotopic conditions [43,44,45]. In addition, photopic multifocal electroretinogram (mfERG) recording of neuroretinal function have demonstrated shorter implicit times in females than males subjects <50 years of age [46]. In a study of sex differences in Sprague-Dawley rats, female rats from 60 to 200 days old had a significant increase in scotopic a and b-wave response when compared to age-matched males [47]. It has been noted previously that estrus cycle levels reach a maximum by day 240 in mice [48]. Therefore, the time period of 60–200 days old may coincide with an increase of estrogen levels for the female rats during this period [47]. In our laboratory, we have also found a significant difference between male and female mice in RPE electrical response (c-waves) using full field ERG. In this experiment healthy 3-month old C57BL/6J mice were dark adapted overnight before recording of c-waves in response to 4 s flashes of 100 cd s mm−2 using the UTAS E-4000 System (LKC Technologies, Gaithersburg, MD). Measurement of baseline to peak of each c-wave illustrated a significant increase in RPE response in female mice when compared to age-matched males (Fig. 11.1c; P < 0.05). This study however, did not take into account estrous levels, which however, may additionally affect the c-wave results.
Hormone Regulation and Ocular Health
Natural Hormones
There are three types of estrogen: estrone (E1), estradiol (E2 or 17-β-estradiol), and estriol (E3). Estrone is produced primarily in the ovaries and is converted from testosterone by way of estradiol or directly from androstenedione. In addition to the ovaries, estrone can be produced in the placenta and in adipose tissue in men and postmenopausal women. As the ovaries of post-menopausal women continue to produce androstenedione and testosterone, a significant amount of estrone is produced in older women. Estriol, a metabolite of estradiol or estrone, is only found in significant amounts during pregnancy when it is produced by the placenta [49]. Estradiol, the most abundant estrogen, is needed for the development of the female reproductive system. In men, estradiol is produced in the testes to prevent sperm cell apoptosis [50]. Estradiol also plays a key role in promoting bone [51], brain [52], skin health [53], and is important in eye health [54]. Estradiol is able to bind to estrogen receptor α (ERα) and estrogen receptor β (ERβ). These two types of nuclear estrogen receptors are present throughout the human eye tissue including cornea [55, 56], lens [56, 57], lacrimal gland [56], meibonian gland [58], iris and ciliary body [56, 57] conjunctiva [56, 59], and retina [13, 57, 60]. In the retina, ERα is expressed in neuronal cells and localized to the outer synaptic layer (outer plexiform layer, OPL) [61]. ERβ is expressed to a lesser extent in the neuronal cells of the retina and more predominately in the inner synaptic layer (inner plexiform layer, IPL) [5]. Estrogen hormone signaling can be activated through genomic or non-genomic pathways. In the genomic pathway, hormone binding to the receptor allows for the receptor to translocate from the cytosol into the nucleus [62]. In the nucleus, the receptor forms homodimers or heterodimers before binding to the hormone response element (HRE) [63]. Once bound to the HRE, transcription of the different response genes is regulated. The non-genomic pathway varies from the genomic pathway in that steroid activation takes place rapidly [64]. This pathway often involves secondary messenger and signal-transduction cascades, which can alter protein kinase pathways, ion flux, and cyclic AMP [64].
In addition to estrogen receptors , androgen and progesterone receptors are also present throughout the eye, where they too have been found in the cornea [55, 56, 65], lens [56, 65, 66], iris [55, 56], lacrimal gland [56, 67], meibomian gland [56, 65], conjunctiva [56, 65], retina [56, 65, 66, 68], as well as the RPE [65]. The androgen receptor (AR) is also known as the nuclear receptor subfamily 3, group C, member 4 (NR3C4). Like the estrogen receptors, the AR is a nuclear receptor that is activated in the cytoplasm before being translocated into the nucleus [69]. The AR is activated by binding of testosterone or dihydrotestosterone (DHT). DHT, also known as 5α-DHT, acts as potent agonist for the AR [70, 71], which , based on its impact on the expression of lipid and keratin related genes, has been suggested to potentially play a therapeutic role in the alleviation of dry eye disease [72]. Dry eye, which can affect both males and females, results from dysfunction of the meibomian gland [73, 74], a target site for androgens [75]. Finally, androgens have also been found to play a role in wound healing [76], stimulation of mitosis [77] and suppression of angiogenesis [78]. Sex Hormone receptors identified in the retina and RPE are summarized in Table 11.1.
The protective effects of progesterone have also been investigated for the treatment of retinal neurodegenerative diseases, specifically retinitis pigmentosa [79, 80]. Norgestrel, a synthetic progesterone has been acknowledged to provide a protective effect against photoreceptor cell death in both the light damage model of retinal degeneration as well as the rd10 mouse (Pde6b mutation) [80]. In a study by Jackson and colleagues, the specific progesterone receptors A and B, progesterone receptor membrane complex 1 and 2 (PGRMC1, PGRMC2) and membrane progesterone receptor isoforms α, β, and γ have been identified in adult mouse retina using QRT-PCR [79]. Of note, PGRMC1 knockdown in 661w photoreceptors or pharmacological inhibition of PGRMC1 in rd10 retinal explants cultures reduced the effects of Norgestrel, indicating the importance of this receptor in retinal photoreceptor neuroprotection [79]. Recent studies have suggested that in addition to activation through the classical genomic pathway, these receptors may also be activated through the non-genomic pathway [81, 82].
Hormone Regulation and RPE/Retinal Health
Dysfunction of the RPE and retina are associated with many ocular diseases such as retinitis pigmentosa, diabetic retinopathy, Stargardt disease, and age-related macular degeneration. As part of the retina, the RPE’s basolateral membrane sits on top of Bruch’s membrane, with the RPE’s apical membrane being in contact with the photoreceptor outer segments. The RPE plays a vital role in maintaining retina health by forming tight junctions with neighboring endothelial cells, thereby constituting the outer blood-retinal barrier. These tight junctions allow for the RPE to help facilitate the fluctuation of various ions and nutrients required by the retina. Bruch’s membrane, which is an extracellular matrix (ECM) deposited by the RPE, choroidal endothelial cells as well as fibroblast during development and beyond, also assists in controlling the diffusion of nutrients and molecules [83,84,85,86]. When RPE homeostasis is impaired, the structural elements of the ECM may get damaged, leading to the accumulation of deposits under the RPE layer [87]. More specifically, deregulation of matrix metalloproteinases (MMP)-2, an enzyme needed for collagen IV digestion, can lead to an increase of collagen IV and concomitant thickening of Bruch’s membrane [87], leading to a decrease in fluid movement and transport of metabolites [88, 89]. Interestingly, estrogen has been found to correlate with MMP activity and subretinal deposit formation. In a study performed by Cousin’s and colleagues, older female mice (16 month) compared to age-matched male mice, and ovaricectomized middle-aged mice (9 months) compared to ovary intact age-matched females had increased sub-RPE deposits [90]. Sub-retinal deposits formation was also increased in estrogen deficient mice [91]. As deposit formation was not decreased with the addition of hormone replacement therapy alone, it is believed that loss of MMP-2 activity, which participates in ECM homeostasis [92], and dysregulation of matrix turnover played a role [90]. Using primary RPE cells from either ERα or ERβ deficient mice, it was identified that ERβ alone is able to promote higher MMP-2 baseline activity and therefore promote a positive regulatory effect within RPE cells [93]. In addition to MMP-2, MMP-14, and TIMP-2 (tissue inhibitors of metalloproteinase-2) are also found to play an important role in allowing for activation of MMP-2 and ERβ in the presence of 17β-estradiol [93].
Proliferative vitreoretinopathy (PVR), like AMD, is affected by local inflammation in the eye [94]. In this disease, proliferative fibrocellular tissue formed by RPE cells differentiate into fibroblast-like cells and thereby produce extracellular matrix leading to collagen contraction and retinal detachment [95]. However, 17β-estradiol and, to a lesser extent, progesterone were found to inhibit this collagen contraction through inhibition of TGF-β2 [95]. The DNA transcription factor NF-κB has also been associated with estrogen receptor signaling. Studies show that estrogen receptors are able to inhibit NF-κB DNA binding, therefore suppressing interleukin 6 (IL-6) production [96, 97], a pro-inflammatory cytokine found to be elevated in the eyes of PVR [98] as well as serum of AMD patients [99].
Supplemented Hormones
Synthetic forms of progesterone and estrogen introduced into the body through oral contraceptives or hormone replacement therapy can also affect ocular health. By decreasing the release of follicle-stimulating hormone and thereby inhibiting the surge in luteinizing hormone that results in ovulation, synthetic progesterone taken through contraceptive use are able to prevent pregnancy [100]. Oral contraceptives combining both progesterone and estrogen are often prescribed in the United States and Western Europe [101] with low doses of estrogen used to inhibit follicular development and stabilize the endometrium [102]. A report published in 2014 by the Center for Disease Control and the U.S. Department of Health and Human Services, stated that approximately 16% of women between the ages of 15 and 44 use oral contraception [103]. Investigation into the role that oral contraceptives might have on ocular disease has revealed an increase in self-reported glaucoma or ocular hypertension in subjects on birth control [104]. Use of oral contraceptives has also been documented to result in rare cases of retinal vascular occlusion [105,106,107], pigmentary retinopathy [108], and acute macular retinopathy [109, 110]. While uncommon, if not treated, retinal vein occlusion can lead to macular edema, neovascularization, increased eye pressure, and even blindness.
In addition to hormones used for contraception, hormone replacement therapy (HRT) taken during menopause is also linked to eye health. Prescribed to alleviate the symptoms of menopause as the result of diminished estrogen and progesterone levels, HRT involves synthetic use of estrogen (estradiol) and progesterone. Women currently using postmenopausal hormones consisting of estrogen only or estrogen-plus progesterone for a period of 3 or more years had a significantly higher risk of early AMD compared to women never using postmenopausal hormones [111]; in contrast, their risk for advanced neovascular AMD was significantly reduced [111, 112].
The effect of synthetic hormones on ocular health may also be classified as gender-based differences. With primarily women receiving oral contraceptives to prevent pregnancy or hormone replacement therapy to treat menopause, they are more likely to be affected by the role that synthetic hormones play in ocular disease. In addition, as the majority of synthetic hormones are prescribed in the United States and Western Europe, these gender-based differences are more likely to occur in these geographical regions where the use of synthetic hormones are readily accessible and socially accepted.
Preclinical Studies
The role of estradiol in the retina has been a subject of interest in recent years, sparking further basic science research. Estradiol, also referred to as 17β-estradiol or 17β-E2, is the most abundant estrogen and is biosynthesized from cholesterol. In the retina, cholesterol can be either taken up from the circulation, or synthesized de novo in the RPE [113, 114], the latter expressing various lipoproteins and scavenger receptors [114]. Recent studies indicate that estradiol provides a protective effect against inflammation [97, 115]. In addition, Elliot and colleagues have shown that female estrogen receptor β knockout (ERβKO) mice have increased accumulation of subretinal deposits and thickening of Bruch’s membrane [116]. Experiments performed by our laboratory have identified neuroprotective effects of ERβ activation. Using light-induced retinal degeneration as a model for dry AMD, female 3-month-old Balb/C mice were exposed to constant fluorescent light (~1500 lux) for 10 days as previously described [117]. To determine the effects of estrogen, mice received either 0.2 mg/kg dosage of 17β-E2 each day, 25 μg/kg every 2 days of the selective estrogen ERβ receptor antagonist 4-[2-Phenyl-5,7-bis(trifluoromethyl)pyrazolo[1,5-a]pyrimidin-3-yl]phenol (PHTPP), a combination of both, or a vehicle control by intraperitoneal injections. Histological analyses of retina sections stained with 0.1% toluene blue [118] revealed that animals receiving estrogen treatment contained significantly more photoreceptors following light damage compared to animals receiving vehicle alone (Fig. 11.2a; P < 0.001; n = 5–10 per condition). While the administration of PHTPP alone did not alter the rate of photoreceptor cell death, it eliminated the protective effect of estrogen when co-administered. Better rod survival was found to result in improved rod-photoreceptor-driven ERG responses. Estrogen supplementation led to improved scotopic photoreceptor function across all three light intensities tested when compared to the vehicle control group (Fig. 11.2b; P < 0.01), whereas ERG amplitudes in PHTTP−, or estrogen + PHTTP-treated animals did not differ from vehicle control animals (Fig. 11.2c, d; P > 0.05). Cones on the other hand, are more resistant to cell death induced by light damage [119]. Nevertheless, immunohistochemical analyses using an antibody against the predominant form of mouse cone opsin (UV cone opsin) (acc # 16186377) showed that following 10 days of light damage significant shortening of the cone outer segments had occurred (Fig. 11.3b, g), whereas long cone outer segments were observed in age-matched control mice reared under cyclic light (Fig. 11.3a). This effect was ameliorated in mice treated with estrogen (Fig. 11.3c, g). Again, the protective effect of estrogen was reversed in the presence of estrogen + PHTPP (Fig. 11.3e, g), whereas no effect was observed with PHTPP alone (Fig. 11.3d, g). As a secondary control, no cone staining was present in the absence of a primary antibody (Fig. 11.3f). Estradiol has also been found to reduce light damage in Sprague-Dawley rats by modulating antioxidant activity [120]. In a study by Wang and colleagues, it was determined that female ovariectomized rats had a reduction in superoxide dismutase (SOD) 1 and 2, glutathione peroxidase (GPx) 2 and 4, whereas male rats had an increase in GPx1, Gpx2, GPx4, and Nrf2 following light damage [120]. Interestingly, in both male as well as ovariectomized female rats, exogenous application of estradiol upregulated all of the antioxidant genes [120]. These results suggest that further research is warranted to explore the therapeutic effects of estrogen in retinal degenerative disorders.
Estrogen reduces light-induced rod photoreceptor cell death and function. (a) Rows of photoreceptors were counted in ten different locations across the retina from ventral to dorsal to obtain an average row count per retina. After 10 days of constant light, vehicle-treated Balb/c mice had ~4.5 rows of photoreceptors. Animals treated with estrogen (17β-ED) contained an additional ~1.5 rows (P < 0.001). While PHTPP (ERβ-antagonist) did not increase cell death due to light damage, it negated the protective effect of estrogen (estrogen + PHTTP; P < 0.0001) (n = 5–10 per condition). (b–d) Photoreceptor cell function was determined using electroretinography. Dark-adapted scotopic conditions were used to measure rod function (3 light intensities using white light; 10, 6 and 0 dB of attenuation; max intensity 2.48 photopic cd s/m2). Here, averaged % baseline ERG amplitudes are presented for the individual animals. (b) Mice treated daily with estrogen showed a significant increase in scotopic ERG amplitudes. Similar to the results obtained in the histological studies, (c) PHTPP by itself did not lead to further deterioration of function; but blunted the protective effects of estrogen when co-administered (d) (n = 5–10 animals per condition)
Estrogen prevents light-induced UV cone opsin loss. Retina sections were labeled with an antibody against UV-opsin to evaluate the presence of cone outer segments. (a) Long cone outer segments can be demonstrated in control, cyclic light reared age-matched controls. (b) Vehicle-treated animals have very short outer segments; whereas UV cone opsin immunoreactivity levels were increased in LD mice after estrogen treatment (c). ERβ inhibitor (PHTTP) treatment did not alter cone OS structure when compared to controls (d), but PHTTP treatment coadministered with estrogen reversed the protective effect of estrogen alone (e). No primary antibody was used as a control (f). (g) UV opsin protein levels were quantified from binarized and thresholded images normalized to a fixed size using Image J software. Estrogen treatment significantly elevated UV opsin level in light damaged mice (P < 0.01), an effect that reversed by co-administration with PHTTP (P < 0.01). No difference was observed between vehicle control, PHTPP and PHTPP and estrogen co-treated groups
Autoimmune Disease and Retinal/RPE Health
As previously mentioned, fluctuations in a woman’s estrogen levels can have significant effects in the eye. This is true also in relation to autoimmune disease and the role that estrogen levels play in disease severity. Diagnosis of autoimmune disease, such as systemic lupus erythematosus (SLE), scleroderma, rheumatoid arthritis (RA), hyperthyroidism, and multiple sclerosis (MS) are all more common in women than men. Women diagnosed with RA prior to menopause, when levels of estradiol are higher, exhibited decreased severity of symptoms compared to woman over the age of 50 [121, 122]. Disease severity for women at this age is comparable to men and interestingly, men with RA have higher levels of serum estradiol compared to men who do not have RA [123]. During pregnancy when estriol levels are increased, many women with RA experience a decrease in RA symptoms [124]. Patients with MS also experience relief from symptoms when levels of estriol are at pregnancy levels [125]. Still, Jorgensen and colleagues found that with increased numbers of pregnancies, women are more likely to experience greater severity in disease symptoms [126]. Like RA, SLE is also diagnosed in a higher percentage of women. However, while RA symptoms seem to be exacerbated following menopause, women with SLE have more severe symptoms during their reproductive years. In addition to RA and SLE, patients with other rheumatological conditions such as Wegener’s granulomatosis, relapsing polychronditis, polyarteritis nodosa, seronegative spondyloathropathies, Behecet’s disease, plymyagia, rheumatic, sarcoidosis, and systemic sclerosis have increased risk of ocular disorders including corneal melt, retinitis, glaucoma, cataract scleritis, and uveitis [7]. When RA patients were examined for ocular manifestations dry eye, episcleritis, scleritis, peripheral ulceratie karatitis and sclerosing keratitis were identified [127]. For patients with SLE, 10% suffer from retinal disease [128]. Retinal conditions such as severe vaso-occlusive retinopathy, central retinal vein occlusion branch retinal vein occlusion, central retinal arteriole occlusion, branch retinal arteriole occlusion, and exudative retinal detachment can all lead to vision loss in SLE patients [128]. As with retina and RPE dysfunction, estrogen receptors have been found to play a role in autoimmune disorders. Synovial tissue from RA patients has been found to be positive for ERα and ERβ [129, 130]. In SLE patients, ERα levels are decreased while ERβ levels are increased, suggesting an ERβ-mediated effect on inflammation [14]. Oxidative stress, which can affect many inflammatory diseases as well as ocular diseases, is shown to increase the expression of ERβ [131].
In some cases secondary ocular disorders in autoimmune diseases can result from medications given to treat the autoimmune diseases; however, for these reports, no data is available that stratifies the results based on sex. With an increased prevalence for autoimmune diseases diagnosis in women, it is important to be aware of the role that these prescriptions play in ocular disorders in women’s health. Hydroxychloroquine (HCQ) is commonly used to treat autoimmune disorders including RA and SLE. This drug inhibits the immune response through a variety of mechanisms and is being investigated as a therapeutic for other diseases. Currently HCQ is being investigated as a drug to use in high dose in combination with various chemotherapy drugs [132,133,134,135]. While this drug serves as a potent immunosuppressor, there is still concern over its ability to induce retinal toxicity. The mechanism of retinal toxicity by HCQ is still being investigated, however research has shown that it is able to bind in the RPE as well as the retina [136]. As an inhibitor of all-trans-retinol in primary human RPE cells [137], HCQ may have an adverse effect on the visual cycle. Indomethacin, a non-steroidal inflammatory drug (NSAIDs), has also been linked to retinopathy with pigmentary scattering of the RPE observed [138]. The use of biologics has also been associated with ocular side effects. Rituximab, a monoclonal antibody used for the treatment of RA, was found in a small percentage of patients to result in loss of visual function [139]. Recombinant interferon (IFNs), an anti-viral medication used in the treatment of MS has reported ophthalmic side effects that include retinal vascular abnormalities [140,141,142]. Methotrexate is an antifolate that serves as an effective immunosuppressant for diseases such as RA and lupus. However, in the absence of folate supplementation, use of methotrexate can result in ocular side effects. In one reported case, b-wave amplitudes in full-field ERG was reduced after prolonged methotrexate use [143]. Interestingly, folate is transported by RPE cells by folate receptors found in the RPE and retina [144]. Studies have also linked the use of folic acid in AMD prevention [145]. Therefore it may be especially important for individuals with AMD to use caution when using methotrexate. High doses of corticosteroid use among MS patients can result in retinal detachment due to central serous chorioretinopathy [146].
General modifications to lifestyle such as diet, exercise, and cessation of smoking are noted as beneficial for both autoimmune and ocular diseases such as AMD. Though not accounting for sex differences, dietary sodium has recently been linked as a risk factor for MS, with mouse studies showing an increase of Th17 cells and experimental autoimmune encephyalomyelitis (EAE) in the presence of a high sodium diet [147, 148]. Using the SJL mouse strain, it was observed that dietary sodium exacerbated the effects of EAE in females but not males [149]. Conversely to dietary sodium, current studies are investigating the protective effect of vitamin D in AMD [150] and rheumatic diseases [151]. It has been found that higher levels of 25-hydroxyvitamin D resulted in a lower incidence in female patients with MS, indicating a sex-specific difference in vitamin D benefits [152, 153].
Secondary ocular disorders may also be increased in autoimmune patients even in the absence of harmful medications, and for some of these reports, effects of estradiol is presented. Patients with RA have an increased diagnosis of Sjorgen’s Syndrome, a disease which results in chronic dry eye. Studies have investigated the correlation between RA and AMD. One study concluded that RA patients had a reduced risk for AMD diagnosis, which they believed was most likely the result of long-term NSAID use [154]. Using a much larger cohort, however, Keenan and colleagues determined that patients with RA are at a higher risk of developing AMD and this risk is highest after first hospital admission with RA [155]. As many inflammatory cytokines are present in both autoimmune disease and AMD, it is interesting to note that estradiol is able to down-regulate pro-inflammatory cytokines including interleukin-6 (IL-6) and monocyte chemotactic protein 1 (MCP-1) [156]. Inflammation in various autoimmune diseases as well as in AMD has been shown to be regulated, in part, by the complement pathway. While it is still unknown how exactly sex differences may affect complement activity, studies have shown that classical and alternative complement pathway activity is weaker in female mice [157,158,159,160,161]. This has been confirmed more recently when terminal pathway component C9 was found to have 4- to 7-times less activity in female mouse serum when compared to males [162]. Sex differences in the human complement system await further analysis.
Summary
The purpose of this chapter has been to review some of the previous and current literature exploring the role that sex plays in the pathogenesis of retinal/RPE dysfunction and disease. As discussed, estrogens play an important role in inflammation whether it is in a systemic autoimmune disease or locally within the eye. It is important to continue to investigate the role of sex-related hormones in disease in order to develop more effective therapeutics and be more proactive in preventative care. In the future, estrogen screenings may prove to be valuable in assessment of drug treatment plans for women suffering from one or more inflammatory disease. In addition, we may be able to better identify women at risk for ocular disorders and regularly monitor their eye health with ophthalmology tools such as OCT. As new treatments are developed to fight systemic inflammation, it is important that the effects of these drugs on ocular health be monitored. As discussed, biological differences in retinal layer thickness and visual responses between men and women make it essential to compare sex-differences when monitoring disease. In addition, a woman’s hormonal status also must be accounted for in the analysis. The use of oral contraceptives and hormone replacement therapies may also result in ocular gender-based differences. Taken together, current research demonstrates a significant role of sex hormones in multiple ocular tissues, including retina and RPE. Therefore, we further emphasize the importance of accounting for sex-differences in RPE and retinal disease pathogenesis and function.
References
Popkov VA, Plotnikov EY, Silachev DN, Zorova LD, Pevzner IB, Jankauskas SS, et al. Diseases and aging: gender matters. Biochem Biokhim. 2015;80(12):1560–70.
Podcasy JL, Epperson CN. Considering sex and gender in Alzheimer disease and other dementias. Dialogues Clin Neurosci. 2016;18(4):437–46.
Ober C, Loisel DA, Gilad Y. Sex-specific genetic architecture of human disease. Nat Rev Genet. 2008;9(12):911–22.
Arain FA, Kuniyoshi FH, Abdalrhim AD, Miller VM. Sex/gender medicine. The biological basis for personalized care in cardiovascular medicine. Circ J. 2009;73(10):1774–82.
Stevens GA, White RA, Flaxman SR, Price H, Jonas JB, Keeffe J, et al. Global prevalence of vision impairment and blindness: magnitude and temporal trends, 1990-2010. Ophthalmology. 2013;120(12):2377–84.
Wagner H, Fink BA, Zadnik K. Sex- and gender-based differences in healthy and diseased eyes. Optometry (St Louis, MO). 2008;79(11):636–52.
Clayton JA, Davis AF. Sex/gender disparities and women’s eye health. Curr Eye Res. 2015;40(2):102–9.
Beck SR, Freitag SL, Singer N. Ocular injuries in battered women. Ophthalmology. 1996;103(1):148–51.
Hartzell KN, Botek AA, Goldberg SH. Orbital fractures in women due to sexual assault and domestic violence. Ophthalmology. 1996;103(6):953–7.
Longcope C. Adrenal and gonadal androgen secretion in normal females. Clin Endocrinol Metab. 1986;15(2):213–28.
Akar Y, Yucel I, Akar ME, Zorlu G, Ari ES. Effect of pregnancy on intraobserver and intertechnique agreement in intraocular pressure measurements. Ophthalmologica. 2005;219(1):36–42.
Qureshi IA. Intraocular pressure: association with menstrual cycle, pregnancy and menopause in apparently healthy women. Chin J Physiol. 1995;38(4):229–34.
Qureshi IA, Xi XR, Wu XD. Intraocular pressure trends in pregnancy and in the third trimester hypertensive patients. Acta Obstet Gynecol Scand. 1996;75(9):816–9.
Qureshi IA. Measurements of intraocular pressure throughout the pregnancy in Pakistani women. Chin Med Sci J. 1997;12(1):53–6.
Phillips CI, Gore SM. Ocular hypotensive effect of late pregnancy with and without high blood pressure. Br J Ophthalmol. 1985;69(2):117–9.
Qureshi IA. Ocular hypertensive effect of menopause with and without systemic hypertension. Acta Obstet Gynecol Scand. 1996;75(3):266–9.
Weinreb RN, Lu A, Beeson C. Maternal corneal thickness during pregnancy. Am J Ophthalmol. 1988;105(3):258–60.
Ziai N, Ory SJ, Khan AR, Brubaker RF. Beta-human chorionic gonadotropin, progesterone, and aqueous dynamics during pregnancy. Arch Ophthalmol. 1994;112(6):801–6.
Park SB, Lindahl KJ, Temnycky GO, Aquavella JV. The effect of pregnancy on corneal curvature. CLAO J. 1992;18(4):256–9.
Millodot M. The influence of pregnancy on the sensitivity of the cornea. Br J Ophthalmol. 1977;61(10):646–9.
Riss B, Riss P. Corneal sensitivity in pregnancy. Ophthalmologica. 1981;183(2):57–62.
Gass JD. Central serous chorioretinopathy and white subretinal exudation during pregnancy. Arch Ophthalmol. 1991;109(5):677–81.
Klein BE, Moss SE, Klein R. Effect of pregnancy on progression of diabetic retinopathy. Diabetes Care. 1990;13(1):34–40.
Chan WC, Lim LT, Quinn MJ, Knox FA, McCance D, Best RM. Management and outcome of sight-threatening diabetic retinopathy in pregnancy. Eye (London, England). 2004;18(8):826–32.
Dinn RB, Harris A, Marcus PS. Ocular changes in pregnancy. Obstet Gynecol Surv. 2003;58(2):137–44.
Ohrt V. The influence of pregnancy on diabetic retinopathy with special regard to the reversible changes shown in 100 pregnancies. Acta Ophthalmol. 1984;62(4):603–16.
Smith W, Mitchell P, Wang JJ. Gender, oestrogen, hormone replacement and age-related macular degeneration: results from the Blue Mountains eye study. Aust N Z J Ophthalmol. 1997;25(Suppl 1):S13–5.
Schaumberg DA, Sullivan DA, Dana MR. Epidemiology of dry eye syndrome. Adv Exp Med Biol. 2002;506(Pt B):989–98.
Wolfs RC, Borger PH, Ramrattan RS, Klaver CC, Hulsman CA, Hofman A, et al. Changing views on open-angle glaucoma: definitions and prevalences--the Rotterdam study. Invest Ophthalmol Vis Sci. 2000;41(11):3309–21.
Leske MC, Connell AM, Wu SY, Nemesure B, Li X, Schachat A, et al. Incidence of open-angle glaucoma: the Barbados eye studies. The Barbados Eye Studies Group. Arch Ophthalmol. 2001;119(1):89–95.
Leske MC, Wu SY, Hennis A, Honkanen R, Nemesure B, Group BES. Risk factors for incident open-angle glaucoma: the Barbados eye studies. Ophthalmology. 2008;115(1):85–93.
Mukesh BN, Le A, Dimitrov PN, Ahmed S, Taylor HR, McCarty CA. Development of cataract and associated risk factors: the visual impairment project. Arch Ophthalmol. 2006;124(1):79–85.
Klein BE, Klein R, Lee KE. Incidence of age-related cataract: the Beaver Dam Eye Study. Arch Ophthalmol. 1998;116(2):219–25.
Cahill M, O’Keefe M, Acheson R, Mulvihill A, Wallace D, Mooney D. Classification of the spectrum of Coats’ disease as subtypes of idiopathic retinal telangiectasis with exudation. Acta Ophthalmol Scand. 2001;79(6):596–602.
Shields JA, Shields CL, Honavar SG, Demirci H. Clinical variations and complications of coats disease in 150 cases: the 2000 Sanford Gifford Memorial Lecture. Am J Ophthalmol. 2001;131(5):561–71.
Smithen LM, Brown GC, Brucker AJ, Yannuzzi LA, Klais CM, Spaide RF. Coats’ disease diagnosed in adulthood. Ophthalmology. 2005;112(6):1072–8.
Southren AL, Gordon GG, Tochimoto S, Pinzon G, Lane DR, Stypulkowski W. Mean plasma concentration, metabolic clearance and basal plasma production rates of testosterone in normal young men and women using a constant infusion procedure: effect of time of day and plasma concentration on the metabolic clearance rate of testosterone. J Clin Endocrinol Metab. 1967;27(5):686–94.
Southren AL, Tochimoto S, Carmody NC, Isurugi K. Plasma production rates of testosterone in normal adult men and women and in patients with the syndrome of feminizing testes. J Clin Endocrinol Metab. 1965;25(11):1441–50.
Eisner A, Burke SN, Toomey MD. Visual sensitivity across the menstrual cycle. Vis Neurosci. 2004;21(4):513–31.
Prusky GT, Alam NM, Beekman S, Douglas RM. Rapid quantification of adult and developing mouse spatial vision using a virtual optomotor system. Invest Ophthalmol Vis Sci. 2004;45(12):4611–6.
van Alphen B, Winkelman BH, Frens MA. Age- and sex-related differences in contrast sensitivity in C57BL/6 mice. Invest Ophthalmol Vis Sci. 2009;50(5):2451–8.
Won JY, Kim SE, Park YH. Effect of age and sex on retinal layer thickness and volume in normal eyes. Medicine. 2016;95(46):e5441.
Birch DG, Anderson JL. Standardized full-field electroretinography. Normal values and their variation with age. Arch Ophthalmol. 1992;110(11):1571–6.
Vainio-Mattila B. The clinical electroretinogram; II. The difference between the electroretinogram in men and in women. Acta Ophthalmol. 1951;29(1):25–32.
Zeidler I. The clinical electroretinogram. IX. The normal electroretinogram. Value of the b-potential in different age groups and its differences in men and women. Acta Ophthalmol. 1959;37:294–301.
Ozawa GY, Bearse MA Jr, Harrison WW, Bronson-Castain KW, Schneck ME, Barez S, et al. Differences in neuroretinal function between adult males and females. Optom Vis Sci. 2014;91(6):602–7.
Chaychi S, Polosa A, Lachapelle P. Differences in retinal structure and function between aging male and female Sprague-Dawley rats are strongly influenced by the Estrus Cycle. PLoS One. 2015;10(8):e0136056.
Nelson JF, Felicio LS. Hormonal influences on reproductive aging in mice. Ann N Y Acad Sci. 1990;592:8–12; discussion 44–51.
Tulchinsky D, Hobel CJ. Plasma human chorionic gonadotropin, estrone, estradiol, estriol, progesterone, and 17 alpha-hydroxyprogesterone in human pregnancy. 3. Early normal pregnancy. Am J Obstet Gynecol. 1973;117(7):884–93.
Pentikainen V, Erkkila K, Suomalainen L, Parvinen M, Dunkel L. Estradiol acts as a germ cell survival factor in the human testis in vitro. J Clin Endocrinol Metab. 2000;85(5):2057–67.
Wang Q, Nicholson PH, Suuriniemi M, Lyytikainen A, Helkala E, Alen M, et al. Relationship of sex hormones to bone geometric properties and mineral density in early pubertal girls. J Clin Endocrinol Metab. 2004;89(4):1698–703.
Pansiot J, Mairesse J, Baud O. Protecting the developing brain by 17beta-estradiol. Oncotarget. 2017;8(6):9011–2.
Rittie L, Kang S, Voorhees JJ, Fisher GJ. Induction of collagen by estradiol: difference between sun-protected and photodamaged human skin in vivo. Arch Dermatol. 2008;144(9):1129–40.
Freeman EE, Munoz B, Schein OD, West SK. Hormone replacement therapy and lens opacities: the Salisbury Eye Evaluation project. Arch Ophthalmol. 2001;119(11):1687–92.
Suzuki T, Kinoshita Y, Tachibana M, Matsushima Y, Kobayashi Y, Adachi W, et al. Expression of sex steroid hormone receptors in human cornea. Curr Eye Res. 2001;22(1):28–33.
Wickham LA, Gao J, Toda I, Rocha EM, Ono M, Sullivan DA. Identification of androgen, estrogen and progesterone receptor mRNAs in the eye. Acta Ophthalmol Scand. 2000;78(2):146–53.
Ogueta SB, Schwartz SD, Yamashita CK, Farber DB. Estrogen receptor in the human eye: influence of gender and age on gene expression. Invest Ophthalmol Vis Sci. 1999;40(9):1906–11.
Auw-Haedrich C, Feltgen N. Estrogen receptor expression in meibomian glands and its correlation with age and dry-eye parameters. Graefes Arch Clin Exp Ophthalmol. 2003;241(9):705–9.
Fuchsjager-Mayrl G, Nepp J, Schneeberger C, Sator M, Dietrich W, Wedrich A, et al. Identification of estrogen and progesterone receptor mRNA expression in the conjunctiva of premenopausal women. Invest Ophthalmol Vis Sci. 2002;43(9):2841–4.
Marin-Castano ME, Elliot SJ, Potier M, Karl M, Striker LJ, Striker GE, et al. Regulation of estrogen receptors and MMP-2 expression by estrogens in human retinal pigment epithelium. Invest Ophthalmol Vis Sci. 2003;44(1):50–9.
Cascio C, Russo D, Drago G, Galizzi G, Passantino R, Guarneri R, et al. 17beta-estradiol synthesis in the adult male rat retina. Exp Eye Res. 2007;85(1):166–72.
Chan L, O’Malley BW. Mechanism of action of the sex steroid hormones (first of three parts). N Engl J Med. 1976;294(24):1322–8.
Singh S, Gupta PD. Induction of phosphoinositide-mediated signal transduction pathway by 17 beta-oestradiol in rat vaginal epithelial cells. J Mol Endocrinol. 1997;19(3):249–57.
Simoncini T, Mannella P, Fornari L, Caruso A, Varone G, Genazzani AR. Genomic and non-genomic effects of estrogens on endothelial cells. Steroids. 2004;69(8–9):537–42.
Rocha EM, Wickham LA, da Silveira LA, Krenzer KL, Yu FS, Toda I, et al. Identification of androgen receptor protein and 5alpha-reductase mRNA in human ocular tissues. Br J Ophthalmol. 2000;84(1):76–84.
Tachibana M, Kobayashi Y, Kasukabe T, Kawajiri K, Matsushima Y. Expression of androgen receptor in mouse eye tissues. Invest Ophthalmol Vis Sci. 2000;41(1):64–6.
Rocha FJ, Wickham LA, Pena JD, Gao J, Ono M, Lambert RW, et al. Influence of gender and the endocrine environment on the distribution of androgen receptors in the lacrimal gland. J Steroid Biochem Mol Biol. 1993;46(6):737–49.
Bigsby RM, Cardenas H, Caperell-Grant A, Grubbs CJ. Protective effects of estrogen in a rat model of age-related cataracts. Proc Natl Acad Sci U S A. 1999;96(16):9328–32.
Lu NZ, Wardell SE, Burnstein KL, Defranco D, Fuller PJ, Giguere V, et al. International Union of Pharmacology. LXV. The pharmacology and classification of the nuclear receptor superfamily: glucocorticoid, mineralocorticoid, progesterone, and androgen receptors. Pharmacol Rev. 2006;58(4):782–97.
Saartok T, Dahlberg E, Gustafsson JA. Relative binding affinity of anabolic-androgenic steroids: comparison of the binding to the androgen receptors in skeletal muscle and in prostate, as well as to sex hormone-binding globulin. Endocrinology. 1984;114(6):2100–6.
Purushottamachar P, Njar VC. A new simple and high-yield synthesis of 5alpha-dihydrotestosterone (DHT), a potent androgen receptor agonist. Steroids. 2012;77(14):1530–4.
Khandelwal P, Liu S, Sullivan DA. Androgen regulation of gene expression in human meibomian gland and conjunctival epithelial cells. Mol Vis. 2012;18:1055–67.
Knop E, Knop N, Millar T, Obata H, Sullivan DA. The international workshop on meibomian gland dysfunction: report of the subcommittee on anatomy, physiology, and pathophysiology of the meibomian gland. Invest Ophthalmol Vis Sci. 2011;52(4):1938–78.
Kang YS, Lee HS, Li Y, Choi W, Yoon KC. Manifestation of meibomian gland dysfunction in patients with Sjogren’s syndrome, non-Sjogren’s dry eye, and non-dry eye controls. Int Ophthalmol. 2018;38(3):1161–7.
Sullivan DA, Sullivan BD, Ullman MD, Rocha EM, Krenzer KL, Cermak JM, et al. Androgen influence on the meibomian gland. Invest Ophthalmol Vis Sci. 2000;41(12):3732–42.
Schumacher H, Machemer R. [Experimental studies on the therapy of corneal lesions due to cortisone]. Klin Monbl Augenheilkd. 1966;148(1):121–6.
Tsai TH, Scheving LE, Scheving LA, Pauly JE. Sex differences in circadian rhythms of several variables in lymphoreticular organs, liver, kidney, and corneal epithelium in adult CD2F1 mice. Anat Rec. 1985;211(3):263–70.
Yamamoto T, Terada N, Nishizawa Y, Petrow V. Angiostatic activities of medroxyprogesterone acetate and its analogues. Int J Cancer. 1994;56(3):393–9.
Jackson AC, Roche SL, Byrne AM, Ruiz-Lopez AM, Cotter TG. Progesterone receptor signalling in retinal photoreceptor neuroprotection. J Neurochem. 2016;136(1):63–77.
Doonan F, O’Driscoll C, Kenna P, Cotter TG. Enhancing survival of photoreceptor cells in vivo using the synthetic progestin Norgestrel. J Neurochem. 2011;118(5):915–27.
Moussatche P, Lyons TJ. Non-genomic progesterone signalling and its non-canonical receptor. Biochem Soc Trans. 2012;40(1):200–4.
Petersen SL, Intlekofer KA, Moura-Conlon PJ, Brewer DN, Del Pino SJ, Lopez JA. Nonclassical progesterone signalling molecules in the nervous system. J Neuroendocrinol. 2013;25(11):991–1001.
Liotta LA, Steeg PS, Stetler-Stevenson WG. Cancer metastasis and angiogenesis: an imbalance of positive and negative regulation. Cell. 1991;64(2):327–36.
Van Agtmael T, Bruckner-Tuderman L. Basement membranes and human disease. Cell Tissue Res. 2010;339(1):167–88.
Bai X, Dilworth DJ, Weng YC, Gould DB. Developmental distribution of collagen IV isoforms and relevance to ocular diseases. Matrix Biol. 2009;28(4):194–201.
Schittny JC, Yurchenco PD. Basement membranes: molecular organization and function in development and disease. Curr Opin Cell Biol. 1989;1(5):983–8.
Leu ST, Batni S, Radeke MJ, Johnson LV, Anderson DH, Clegg DO. Drusen are cold spots for proteolysis: expression of matrix metalloproteinases and their tissue inhibitor proteins in age-related macular degeneration. Exp Eye Res. 2002;74(1):141–54.
Booij JC, Baas DC, Beisekeeva J, Gorgels TG, Bergen AA. The dynamic nature of Bruch’s membrane. Prog Retin Eye Res. 2010;29(1):1–18.
Nita M, Strzalka-Mrozik B, Grzybowski A, Mazurek U, Romaniuk W. Age-related macular degeneration and changes in the extracellular matrix. Med Sci Monitor. 2014;20:1003–16.
Cousins SW, Marin-Castano ME, Espinosa-Heidmann DG, Alexandridou A, Striker L, Elliot S. Female gender, estrogen loss, and sub-RPE deposit formation in aged mice. Invest Ophthalmol Vis Sci. 2003;44(3):1221–9.
Espinosa-Heidmann DG, Marin-Castano ME, Pereira-Simon S, Hernandez EP, Elliot S, Cousins SW. Gender and estrogen supplementation increases severity of experimental choroidal neovascularization. Exp Eye Res. 2005;80(3):413–23.
Nagase H, Visse R, Murphy G. Structure and function of matrix metalloproteinases and TIMPs. Cardiovasc Res. 2006;69(3):562–73.
Elliot S, Catanuto P, Fernandez P, Espinosa-Heidmann D, Karl M, Korach K, et al. Subtype specific estrogen receptor action protects against changes in MMP-2 activation in mouse retinal pigmented epithelial cells. Exp Eye Res. 2008;86(4):653–60.
Limb GA, Little BC, Meager A, Ogilvie JA, Wolstencroft RA, Franks WA, et al. Cytokines in proliferative vitreoretinopathy. Eye (London, England). 1991;5(Pt 6):686–93.
Kimura K, Orita T, Fujitsu Y, Liu Y, Wakuta M, Morishige N, et al. Inhibition by female sex hormones of collagen gel contraction mediated by retinal pigment epithelial cells. Invest Ophthalmol Vis Sci. 2014;55(4):2621–30.
Stein B, Yang MX. Repression of the interleukin-6 promoter by estrogen receptor is mediated by NF-kappa B and C/EBP beta. Mol Cell Biol. 1995;15(9):4971–9.
Paimela T, Ryhanen T, Mannermaa E, Ojala J, Kalesnykas G, Salminen A, et al. The effect of 17beta-estradiol on IL-6 secretion and NF-kappaB DNA-binding activity in human retinal pigment epithelial cells. Immunol Lett. 2007;110(2):139–44.
Kauffmann DJ, van Meurs JC, Mertens DA, Peperkamp E, Master C, Gerritsen ME. Cytokines in vitreous humor: interleukin-6 is elevated in proliferative vitreoretinopathy. Invest Ophthalmol Vis Sci. 1994;35(3):900–6.
Ambreen F, Ismail M, Qureshi, IZ. Association of gene polymorphism with serum levels of inflammatory and angiogenic factors in Pakistani patients with age-related macular degeneration. Mol. Vis. 2015; 21:985–99.
Ahn RS, Choi JH, Choi BC, Kim JH, Lee SH, Sung SS. Cortisol, estradiol-17beta, and progesterone secretion within the first hour after awakening in women with regular menstrual cycles. J Endocrinol. 2011;211(3):285–95.
Brynhildsen J. Combined hormonal contraceptives: prescribing patterns, compliance, and benefits versus risks. Ther Adv Drug Safety. 2014;5(5):201–13.
Sech LA, Mishell DR Jr. Oral steroid contraception. Womens Health (London, England). 2015;11(6):743–8.
Daniels K, Daugherty J, Jones J, Mosher W. Current contraceptive use and variation by selected characteristics among women aged 15–44: United States, 2011-2013. Natl Health Stat Rep. 2015(86):1–14.
Wang YE, Kakigi C, Barbosa D, Porco T, Chen R, Wang S, et al. Oral contraceptive use and prevalence of self-reported glaucoma or ocular hypertension in the United States. Ophthalmology. 2016;123(4):729–36.
Thapa R, Paudyal G. Central retinal vein occlusion in young women: rare cases with oral contraceptive pills as a risk factor. Nepal Med Coll J. 2009;11(3):209–11.
Klein R, Klein BE, Knudtson MD, Meuer SM, Swift M, Gangnon RE. Fifteen-year cumulative incidence of age-related macular degeneration: the Beaver Dam Eye Study. Ophthalmology. 2007;114(2):253–62.
Aggarwal RS, Mishra VV, Aggarwal SV. Oral contraceptive pills: a risk factor for retinal vascular occlusion in in-vitro fertilization patients. J Hum Reprod Sci. 2013;6(1):79–81.
Giovannini A, Consolani A. Contraceptive-induced unilateral retinopathy. Ophthalmologica. 1979;179(5):302–5.
Pellegrini F, Interlandi E, Pavesio C, Ferreyra HA. We cannot see what she cannot ignore. Surv Ophthalmol. 2017;62:882–5.
Rush JA. Acute macular neuroretinopathy. Am J Ophthalmol. 1977;83(4):490–4.
Feskanich D, Cho E, Schaumberg DA, Colditz GA, Hankinson SE. Menopausal and reproductive factors and risk of age-related macular degeneration. Arch Ophthalmol. 2008;126(4):519–24.
Edwards DR, Gallins P, Polk M, Ayala-Haedo J, Schwartz SG, Kovach JL, et al. Inverse association of female hormone replacement therapy with age-related macular degeneration and interactions with ARMS2 polymorphisms. Invest Ophthalmol Vis Sci. 2010;51(4):1873–9.
Cascio C, Deidda I, Russo D, Guarneri P. The estrogenic retina: the potential contribution to healthy aging and age-related neurodegenerative diseases of the retina. Steroids. 2015;103:31–41.
Fliesler SJ, Bretillon L. The ins and outs of cholesterol in the vertebrate retina. J Lipid Res. 2010;51(12):3399–413.
Stork S, von Schacky C, Angerer P. The effect of 17beta-estradiol on endothelial and inflammatory markers in postmenopausal women: a randomized, controlled trial. Atherosclerosis. 2002;165(2):301–7.
Elliot SJ, Catanuto P, Espinosa-Heidmann DG, Fernandez P, Hernandez E, Saloupis P, et al. Estrogen receptor beta protects against in vivo injury in RPE cells. Exp Eye Res. 2010;90(1):10–6.
Lohr HR, Kuntchithapautham K, Sharma AK, Rohrer B. Multiple, parallel cellular suicide mechanisms participate in photoreceptor cell death. Exp Eye Res. 2006;83(2):380–9.
Rohrer B, Matthes MT, LaVail MM, Reichardt LF. Lack of p75 receptor does not protect photoreceptors from light-induced cell death. Exp Eye Res. 2003;76(1):125–9.
Organisciak DT, Vaughan DK. Retinal light damage: mechanisms and protection. Prog Retin Eye Res. 2010;29(2):113–34.
Wang S, Wang B, Feng Y, Mo M, Du F, Li H, et al. 17beta-estradiol ameliorates light-induced retinal damage in Sprague-Dawley rats by reducing oxidative stress. J Mol Neurosci. 2015;55(1):141–51.
Tengstrand B, Ahlmen M, Hafstrom I. The influence of sex on rheumatoid arthritis: a prospective study of onset and outcome after 2 years. J Rheumatol. 2004;31(2):214–22.
Seriolo B, Cutolo M, Garnero A, Accardo S. Relationships between serum 17 beta-oestradiol and anticardiolipin antibody concentrations in female patients with rheumatoid arthritis. Rheumatology (Oxford, England). 1999;38(11):1159–61.
Tengstrand B, Carlstrom K, Fellander-Tsai L, Hafstrom I. Abnormal levels of serum dehydroepiandrosterone, estrone, and estradiol in men with rheumatoid arthritis: high correlation between serum estradiol and current degree of inflammation. J Rheumatol. 2003;30(11):2338–43.
Nelson JL, Ostensen M. Pregnancy and rheumatoid arthritis. Rheum Dis Clin N Am. 1997;23(1):195–212.
Sicotte NL, Liva SM, Klutch R, Pfeiffer P, Bouvier S, Odesa S, et al. Treatment of multiple sclerosis with the pregnancy hormone estriol. Ann Neurol. 2002;52(4):421–8.
Jorgensen C, Picot MC, Bologna C, Sany J. Oral contraception, parity, breast feeding, and severity of rheumatoid arthritis. Ann Rheum Dis. 1996;55(2):94–8.
Vignesh AP, Srinivasan R. Ocular manifestations of rheumatoid arthritis and their correlation with anti-cyclic citrullinated peptide antibodies. Clin Ophthalmol (Auckland, NZ). 2015;9:393–7.
Sivaraj RR, Durrani OM, Denniston AK, Murray PI, Gordon C. Ocular manifestations of systemic lupus erythematosus. Rheumatology (Oxford, England). 2007;46(12):1757–62.
Ushiyama T, Inoue K, Nishioka J. Expression of estrogen receptor related protein (p29) and estradiol binding in human arthritic synovium. J Rheumatol. 1995;22(3):421–6.
Ishizuka M, Hatori M, Suzuki T, Miki Y, Darnel AD, Tazawa C, et al. Sex steroid receptors in rheumatoid arthritis. Clin Sci (London, England: 1979). 2004;106(3):293–300.
Tamir S, Izrael S, Vaya J. The effect of oxidative stress on ERalpha and ERbeta expression. J Steroid Biochem Mol Biol. 2002;81(4–5):327–32.
Goldberg SB, Supko JG, Neal JW, Muzikansky A, Digumarthy S, Fidias P, et al. A phase I study of erlotinib and hydroxychloroquine in advanced non-small-cell lung cancer. J Thorac Oncol. 2012;7(10):1602–8.
Mahalingam D, Mita M, Sarantopoulos J, Wood L, Amaravadi RK, Davis LE, et al. Combined autophagy and HDAC inhibition: a phase I safety, tolerability, pharmacokinetic, and pharmacodynamic analysis of hydroxychloroquine in combination with the HDAC inhibitor vorinostat in patients with advanced solid tumors. Autophagy. 2014;10(8):1403–14.
Rangwala R, Chang YC, Hu J, Algazy KM, Evans TL, Fecher LA, et al. Combined MTOR and autophagy inhibition: phase I trial of hydroxychloroquine and temsirolimus in patients with advanced solid tumors and melanoma. Autophagy. 2014;10(8):1391–402.
Rangwala R, Leone R, Chang YC, Fecher LA, Schuchter LM, Kramer A, et al. Phase I trial of hydroxychloroquine with dose-intense temozolomide in patients with advanced solid tumors and melanoma. Autophagy. 2014;10(8):1369–79.
Rosenthal AR, Kolb H, Bergsma D, Huxsoll D, Hopkins JL. Chloroquine retinopathy in the rhesus monkey. Invest Ophthalmol Vis Sci. 1978;17(12):1158–75.
Xu C, Zhu L, Chan T, Lu X, Shen W, Madigan MC, et al. Chloroquine and hydroxychloroquine are novel inhibitors of human organic anion transporting polypeptide 1A2. J Pharm Sci. 2016;105(2):884–90.
Graham CM, Blach RK. Indomethacin retinopathy: case report and review. Br J Ophthalmol. 1988;72(6):434–8.
Foran JM, Rohatiner AZ, Cunningham D, Popescu RA, Solal-Celigny P, Ghielmini M, et al. European phase II study of rituximab (chimeric anti-CD20 monoclonal antibody) for patients with newly diagnosed mantle-cell lymphoma and previously treated mantle-cell lymphoma, immunocytoma, and small B-cell lymphocytic lymphoma. J Clin Oncol. 2000;18(2):317–24.
Tokai R, Ikeda T, Miyaura T, Sato K. Interferon-associated retinopathy and cystoid macular edema. Arch Ophthalmol. 2001;119(7):1077–9.
Perez-Alvarez AF, Jimenez-Alonso J, Reche-Molina I, Leon-Ruiz L, Hidalgo-Tenorio C, Sabio JM. Retinal vasculitis and vitreitis in a patient with chronic hepatitis C virus. Arch Intern Med. 2001;161(18):2262.
Jain K, Lam WC, Waheeb S, Thai Q, Heathcote J. Retinopathy in chronic hepatitis C patients during interferon treatment with ribavirin. Br J Ophthalmol. 2001;85(10):1171–3.
Ponjavic V, Granse L, Stigmar EB, Andreasson S. Reduced full-field electroretinogram (ERG) in a patient treated with methotrexate. Acta Ophthalmol Scand. 2004;82(1):96–9.
Bridges CC, El-Sherbeny A, Ola MS, Ganapathy V, Smith SB. Transcellular transfer of folate across the retinal pigment epithelium. Curr Eye Res. 2002;24(2):129–38.
Christen WG, Glynn RJ, Chew EY, Albert CM, Manson JE. Folic acid, pyridoxine, and cyanocobalamin combination treatment and age-related macular degeneration in women: the Women’s Antioxidant and Folic Acid Cardiovascular Study. Arch Intern Med. 2009;169(4):335–41.
Sharma T, Shah N, Rao M, Gopal L, Shanmugam MP, Gopalakrishnan M, et al. Visual outcome after discontinuation of corticosteroids in atypical severe central serous chorioretinopathy. Ophthalmology. 2004;111(9):1708–14.
Kleinewietfeld M, Manzel A, Titze J, Kvakan H, Yosef N, Linker RA, et al. Sodium chloride drives autoimmune disease by the induction of pathogenic TH17 cells. Nature. 2013;496(7446):518–22.
Wu C, Yosef N, Thalhamer T, Zhu C, Xiao S, Kishi Y, et al. Induction of pathogenic TH17 cells by inducible salt-sensing kinase SGK1. Nature. 2013;496(7446):513–7.
Krementsov DN, Case LK, Hickey WF, Teuscher C. Exacerbation of autoimmune neuroinflammation by dietary sodium is genetically controlled and sex specific. FASEB J. 2015;29(8):3446–57.
Annweiler C, Drouet M, Duval GT, Pare PY, Leruez S, Dinomais M, et al. Circulating vitamin D concentration and age-related macular degeneration: systematic review and meta-analysis. Maturitas. 2016;88:101–12.
Cutolo M. Further emergent evidence for the vitamin D endocrine system involvement in autoimmune rheumatic disease risk and prognosis. Ann Rheum Dis. 2013;72(4):473–5.
Kragt J, van Amerongen B, Killestein J, Dijkstra C, Uitdehaag B, Polman C, et al. Higher levels of 25-hydroxyvitamin D are associated with a lower incidence of multiple sclerosis only in women. Mult Scler. 2009;15(1):9–15.
Vasile M, Corinaldesi C, Antinozzi C, Crescioli C. Vitamin D in autoimmune rheumatic diseases: a view inside gender differences. Pharmacol Res. 2017;117:228–41.
McGeer PL, Sibley J. Sparing of age-related macular degeneration in rheumatoid arthritis. Neurobiol Aging. 2005;26(8):1199–203.
Keenan TD, Goldacre R, Goldacre MJ. Associations between age-related macular degeneration, osteoarthritis and rheumatoid arthritis: record linkage study. Retina (Philadelphia, PA). 2015;35(12):2613–8.
Stubelius A, Andersson A, Islander U, Carlsten H. Ovarian hormones in innate inflammation. Immunobiology. 2017;222(8–9):878–83.
Churchill WH Jr, Weintraub RM, Borsos T, Rapp HJ. Mouse complement: the effect of sex hormones and castration on two of the late-acting components. J Exp Med. 1967;125(4):657–72.
Beurskens FJ, Kuenen JD, Hofhuis F, Fluit AC, Robins DM, Van Dijk H. Sex-limited protein: in vitro and in vivo functions. Clin Exp Immunol. 1999;116(3):395–400.
Buras JA, Rice L, Orlow D, Pavlides S, Reenstra WR, Ceonzo K, et al. Inhibition of C5 or absence of C6 protects from sepsis mortality. Immunobiology. 2004;209(8):629–35.
Ong GL, Mattes MJ. Mouse strains with typical mammalian levels of complement activity. J Immunol Methods. 1989;125(1–2):147–58.
Ong GL, Baker AE, Mattes MJ. Analysis of high complement levels in Mus hortulanus and BUB mice. J Immunol Methods. 1992;154(1):37–45.
Kotimaa J, Klar-Mohammad N, Gueler F, Schilders G, Jansen A, Rutjes H, et al. Sex matters: systemic complement activity of female C57BL/6J and BALB/cJ mice is limited by serum terminal pathway components. Mol Immunol. 2016;76:13–21.
Kobayashi K, Kobayashi H, Ueda M, Honda Y. Estrogen receptor expression in bovine and rat retinas. Invest Ophthalmol Vis Sci. 1998;39(11):2105–10.
Munaut C, Lambert V, Noel A, Frankenne F, Deprez M, Foidart JM, et al. Presence of oestrogen receptor type beta in human retina. Br J Ophthalmol. 2001;85(7):877–82.
Acknowledgements
We thank Mausumi Bandyopadhyay for her expertise and effort in data generated in Figs. 11.1 and 11.2, as well as her overall intellectual expertise, Lara Seidman for her technical assistance with Figs. 11.1 and 11.2, and Kathleen Brady for critical review.
The authors’ responsibilities were as follows: E.O. and G.S. conducted research and analyzed data; G.S wrote manuscript; B.R. assisted with research design and manuscript edits; and all authors read and approved the final manuscript.
This work was sponsored in part by the National Institutes of Health (NIH) K12HD055885 Building Interdisciplinary Research Careers in Women’s Health (BIRCWH) fellowship. Additional research was supported by the National Institutes of Health (NIH) (R01EY019320), Department of Veterans Affairs (I01 RX000444), and the South Carolina SmartState Endowment. All animal experiments were performed in accordance with the ARVO Statement for the Use of Animals in Ophthalmic and Vision Research, and were approved by the University Animal Care and Use Committee.
Author information
Authors and Affiliations
Corresponding authors
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Schnabolk, G., Obert, E., Rohrer, B. (2020). Sex Related Differences in Retinal Pigment Epithelium and Retinal Disease. In: Klettner, A., Dithmar, S. (eds) Retinal Pigment Epithelium in Health and Disease. Springer, Cham. https://doi.org/10.1007/978-3-030-28384-1_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-28384-1_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-28383-4
Online ISBN: 978-3-030-28384-1
eBook Packages: MedicineMedicine (R0)