Abstract
Purpose
To investigate the correlation between estrogen receptor-positive basal cells of the meibomian glands of the lower lid with age, gender, and subjective and objective dry-eye parameters.
Methods
Sixteen lower lid specimens were collected from 7 female and 9 male patients (age range 22–88 years) during tumor surgery requiring whole-thickness excision. Prior to surgery the patients were asked about any dry-eye symptoms (score 0–4, where 0= no dry-eye symptoms). Tear break-up time was measured, and Schirmer I and II tests were performed. We obtained histological sections from the outer margins of the formalin-fixed and paraffin-embedded specimens and performed immunohistochemical staining for estrogen, progesterone and androgen receptors. At least 500 cells were counted per specimen, and the proportion of positively stained cells was calculated and correlated to the age and dry-eye parameters.
Results
All meibomian glands had positive nuclear staining with antibodies for estrogen receptors in their outer cell layers, i.e., the basal cell layer. The proportion of cells expressing estrogen receptors increased with age independent of gender (correlation coefficient=0.67, P<0.005). No correlation was found between estrogen receptor positivity and subjective dry-eye symptoms, tear break-up time, or Schirmer I and II test results. There was no difference in the proportion of cells expressing estrogen receptors between female and male patients (P=0.5).
Conclusions
The amount of meibomian gland cells expressing estrogen receptors in the lower lid seems to increase with age independent of gender and seems not to affect the fat layer and stability of the tear film.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Disturbances of tear film are often found in patients with various conditions of hormonal imbalance, e.g., menopause, pregnancy or intake of hormonal contraceptives. Thus, it seems obvious that some kind of hormonal regulation of the tear-producing system exists. Esmaeli et al. [2] confirmed this assumption a few years ago when they demonstrated estrogen receptors (ERs) in the basal cells of the meibomian glands of the upper lid immunohistochemically.
We became interested in examining the correlation of ER-positive basal cells of the meibomian glands of the lower lid with age, gender, and subjective and objective dry-eye parameters.
Patients and methods
Patients and dry-eye parameters
The 16 consecutive patients included 7 women and 9 men (age range 22–78 years, median 64.5 years) with a lower lid tumor requiring whole-thickness excision (Table 1). The tumors did not affect the inner lid margin and we could assume that the dry-eye parameters (see below) were not influenced by the tumor. Patients with concomitant entropion or ectropion were excluded. Prior to surgery the patients were queried about dry-eye symptoms such as burning or foreign body sensation and excess tearing (score 0–4,where 0= no dry-eye symptoms). In addition, tear break-up time was measured and Schirmer I and II tests were performed. We used a small drop of fluorescein 2.5% to measure the tear break-up time two or three times. For the Schirmer I test a piece of Schirmer filter paper was inserted at the edge of the lateral part of the lower lid for 5 min. The Schirmer II test included the application of proxymetacaine hydrochloride (2×) and the removal of excess eye drops prior to the insertion of the filter paper, whereby the result was measured after 2 min.
Tissues
All specimens were fixed in 4% formaldehyde in 0.075 M phosphate buffer for 24 h, dehydrated in increasing concentrations of ethanol (70%–99%) and infiltrated with paraffin (Merck, Darmstadt, Germany) at 60°C. Serial sections were cut from the lateral and medial border of each paraffin block—which in most cases contained no tumor tissue—at a thickness of 3 μm and floated on de-ionized water at 45°C, and single sections were mounted on Superfrost Plus glass slides (Menzel-Glaser, Germany). Slides were subsequently dried at 60°C for 1 h.
Furthermore, control sections of histologically normal breast and prostate were obtained from the archives of the Institute of Pathology, Freiburg. These sections were processed in the manner described above.
Immunohistochemistry
Immunohistochemical staining was performed on slides of all specimens within a single procedure for each antibody to minimize procedural variations. We used the avidin–biotin method including antigen retrieval using a pressure cooker for 5 min before the mouse monoclonal antibodies for the α form of ERs (Clone 6F11, Novocastra, Newcastle-upon-Tyne, UK) were applied for 2 h. All specimens except the positive control specimens (breast and prostate, respectively) were negative for staining procedures using antibodies for progesterone (clone 2F12) and androgen receptors (clone 1A6, Novocastra).
Counting and statistical method
At least 500 cells were counted per specimen, and the proportion of positively stained cells was calculated and correlated to the age and dry-eye parameters using analysis of variance.
Results
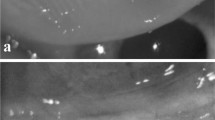
All specimens revealed meibomian glands displaying positive nuclear staining with antibodies for ERs in their outer cell layers, i.e., the basal cell layer. The more mature, inner parts of the meibomian glands showed only faintly positive or negative cytoplasmic staining; the ducts were completely negative (Fig. 1).
Age and gender
The proportion of cells expressing ERs increased with age independent of gender (correlation coefficient=0.67, P<0.005; Fig. 2). There was no difference in the proportion of cells expressing ERs between female and male patients (P=0.5).
Dry-eye symptoms
No correlation was found between ER positivity and subjective dry-eye symptoms (Fig. 3), tear break-up time (Fig. 4), or Schirmer I and II test results (Fig. 5) (Table 1).
Only one patient (case 3) was put on systemic hormonal treatment with 1 mg estradiol + 0.5 mg norethisterone acetate/day. The amount of ER-positive cells in her meibomian glands was comparable with that of other women of similar age (63%).
Discussion
Bulbar as well as tarsal structures contribute to the normal tear film and the disturbance of each of them can lead to the dry-eye syndrome. The cells of the bulbar conjunctival surface in the dry-eye syndrome have been examined by means of impression cytology in numerous studies [1, 8, 9]. Reduction in the goblet cell density and membrane mucin expression have been found [8], as has, interestingly, an overexpression of inflammatory markers such as HLA-DR and ICAM-1 [9] and of apoptotic markers like CD40 and CD40 ligand [1].
Esmaeli et al. [2] were the first to report immunohistochemical evidence of ERs in the meibomian glands, which represent one component of the tarsal structures contributing to the tear film. The specimens they examined originated from the upper lid, removed during ptosis surgery. They did not find a correlation between the proportion of ER-positive cells and age. In contrast to this, we found that the proportion of ER-positive basal cells in the meibomian gland increased significantly with age. This might be due to decreasing hormone levels in the blood with age in women and in men, where the testosterone serum level decreases with age [6], resulting in ER up-regulation [3]. In men, 20% of the serum estrogen originates from the Leydig cells of the testes and 80% from peripheral fat tissue, where circulating testosterone is metabolized by a cytochrome P450-dependent aromatase system in fibroblasts. In addition, the aromatase transforms testosterone into estrogen in almost all the tissues where ERs are also present, such as brain, muscle, bone, heart, and adrenal cortex [10]. Thus, it is possible that men present locally high concentrations of estrogen compared to their very low overall estrogen serum levels (7–23 pg/ml [5]). This could explain why no sex-related difference in ER density in the meibomian gland was found. Our findings partially parallel those of ERα in the supraoptic nucleus of the brain, where elderly women showed more nuclear and cytoplasmic ERα in neurons than young women [4].
The fact that one female (case #3) taking hormone replacement therapy (estradiol) had a similar proportion of ER-positive cells in her meibomian glands compared to other women of her age without hormonal substitution led us to assume that she had had a lower estrogen level compared to the others prior to hormonal substitution, and that that had been compensated for afterwards – perhaps to the same level as that of the other female patients.
Tear break-up time depends mainly on the tear film's lipid layer. Because the lipid layer originates in the meibomian glands, we expected a correlation between tear break-up time and the proportion of ER-positive cells, namely, that lower values of tear break-up time would be associated with a higher proportion of ER-positive cells of the meibomian glands. We were nevertheless unable to demonstrate any correlation between tear break-up time and the proportion of ER-positive cells. This seems to indicate that the proportion of ER-positive cells of the meibomian glands does not affect the fat layer of the tear film.
The tear break-up time was quite low in almost all patients, in contrast to scant subjective complaints. The question is whether despite a "normal" bulbar/tarsal conjunctival interface surface, irregularities occur due to the tumor that decrease tear break-up time but are not clinically relevant to the patient—i.e., dry-eye symptoms. Might it be that a correlation exists between tear break-up time and the proportion of ER of the meibomian glands which could be revealed only if completely normal eyelids covered the same eye? We cannot offer a definitive answer to this question as one cannot ethically defend a biopsy of a completely normal eyelid in order to discover the truth.
It is not surprising that we found no correlation between the Schirmer I and II test results and the amount of ER-positive cells, because the Schirmer I test reflects the reactive production of the water layer of the tear film by the lacrimal gland and the Schirmer II test applies to the basal secretion of the accessory lacrimal glands. It would be more useful to correlate the Schirmer test with the expression of ER in the conjunctiva and the lacrimal gland. Klüppel et al. [7] recently found ER in the conjunctiva and the lacrimal gland using the polymerase chain reaction. Nevertheless, we could not detect ER in the tarsal conjunctiva of our specimens immunohistochemically.
In conclusion, the amount of meibomian gland cells expressing estrogen receptors in the lower lid seems to increase with age independent of gender and seems not to affect the fat layer and stability of the tear film.
References
Brignole F, Pisella PJ, Goldschild M, De Saint Jean M, Goguel A Baudouin C (2000) Flow cytometric analysis of inflammatory markers in conjunctival epithelial cells of patients with dry eyes. Invest Ophthalmol Vis Sci 41:1356–1363
Esmaeli B, Harvey JT, Hewlett B (2000) Immunohistochemical evidence for estrogen receptors in Meibomian glands. Ophthalmology 107:180–184
Htun H, Holth LT, Walker D, Davie JR Hager GL (1999) Direct visualization of the human estrogen receptor alpha reveals a role for ligand in the nuclear distribution of the receptor. Mol Biol Cell 10:471–486
Ishunina TA, Kruijver FP, Balesar R, Swaab DF (2000) Differential expression of estrogen receptor alpha and beta immunoreactivity in the human supraoptic nucleus in relation to sex and aging. J Clin Endocrinol Metab 85:3283–3291
Jockenhövel F (1999) Männlicher Hypogonadismus—aktuelle Aspekte der Androgensubstitution. Uni-Med, Bremen
Keck C, Neulen J, Breckwoldt M (1997) Endokrinologie Reproduktionsmedizin Andrologie. Thieme, Stuttgart
Klüppel M, Reinhard T, Gläser M, Niederacher D, Beckmann MW (2000) Detection of estrogen-receptors (ERs) in conjunctiva, lacrimal gland and eyelids of healthy volunteers. Ophthalmologe 97:S20
Pflugfelder SC, Tseng SC, Yoshino K, Monroy D, Felix C, Reis BL (1997) Correlation of goblet cell density and mucosal epithelial membrane mucin expression with rose bengal staining in patients with ocular irritation. Ophthalmology 104:223–235
Pisella PJ, Brignole F, Debbasch C, Lozato PA, Creuzot-Garcher C, Bara J, Saiag P, Warnet JM, Baudouin C (2000) Flow cytometric analysis of conjunctival epithelium in ocular rosacea and keratoconjunctivitis sicca. Ophthalmology 107:1841–1849
Sharpe RM (1998) The roles of oestrogen in the male. Trend Endocrinol Metab 9:371–377
Acknowledgements
We thank Mrs. Gabriele Korth and Mrs. Renate Buchen for technical assistance and Prof. Dr. Michael Bach for assistance in statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was presented at the annual meeting of the Association for Research in Vision and Ophthalmology in May 2002
Rights and permissions
About this article
Cite this article
Auw-Haedrich, C., Feltgen, N. Estrogen receptor expression in meibomian glands and its correlation with age and dry-eye parameters. Graefe's Arch Clin Exp Ophthalmol 241, 705–709 (2003). https://doi.org/10.1007/s00417-003-0699-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-003-0699-4