Abstract
Radiofrequency catheter ablation (RFCA) of different arrhythmias carries inherent risks due to the nature of the tissue disruption obtained by heating the tip of the ablation catheter. Perforation of heart chambers and bleeding, thromboembolic complications, and complete AV block when ablating in the AV node-His area are the most feared. Most of these complications are related to the access, positioning of the catheters and radiofrequency itself and not to the imaging modality use to guide catheter navigation in the heart and the afferent or efferent vessels. We describe how to prevent and manage complications arising from the new paradigm of an EP lab working without fluoroscopy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
It is a global trending in EP labs all around the world to try to reduce fluoroscopy; to reduce impact on patients, but also in personnel working at those labs, much more exposed to radiation everyday. As with any new approach, safety should be a main topic to consider. X-rays have been so much time in use that despite the low resolution we have all learnt to work with, but the use of radiation has never prevented the complications related to RFCA.
With the development of new technologies such as very precise 3D mapping systems, contact force catheters, intravascular ultrasound and other technologies adding more and useful information about the position of the catheters and its interaction with the cardiac structures fluoroscopy became a dispensable tool.
In the next paragraphs, we describe how to change the paradigm using as close to zero radiation as possible, for most ablation procedures, and to prevent and manage related complications.
The more radiofrequency (RF) applied, the more the chances to have complications. RFCA of atrial fibrillation is by far the procedure that needs more RF, and it is even worse when non PVI foci are target (substrate modification); in a recent series with 10,795 patients from Japan, the total rate of complications occurred in 3% of patients; with pericardial effusion in 1%, massive bleeding in 1%, stroke 0.05% and atrial-oesophageal fistula in 0.02% of patients [1].
The next substrate that requires considerable amounts of RFCA is ventricular arrhythmias ; a multicentre report on idiopathic PVC ablation, with 1185 patients, showed fluoroscopy times of 30 ± 24 min, RF time of 12 ± 11 min, with a total of 5.5% of complications (2.4% of major complications, including 0.8% of cardiac tamponades, 1.3% of major groin complications, and one complete AV block; no strokes and no deaths were reported) [2]. A Chinese series of 1231 patients, single centre, on the same substrate reported 2.7% of complications, mostly pericardial effusion and tamponade, but also with stroke reported and two deaths [3]. Finally, a retrospective analysis of RFCA of ventricular arrhythmias in 34,907 patients (51.6% with structural heart disease, SHD); major complications occurred in 6.3% of SHD patients compared to 2.1% of patients without SHD; death rate was also superior in patients with SHD 2.5% versus 0.12% in patients without SHD [4].
In supraventricular RFCA a paediatric report of more than 20 years and three different registries shows a complication rate varying between 3.2% before 1996 (n = 3653), 4% between 1999 and 2001 (n = 2761), and 3.6% between 2014 and 2015 (n = 1417); cryoablation was used in 53% of AVNRT resulting in a 0.1% of complete AV block; the use of 3-D mapping systems reduced fluoroscopy times from 47.6 ± 40 min in the previous registries to 7 ± 12 min in the latter registry [5].
A report on 519951 adult patients in the USA ablated from 2000 to 2013 showed that 5.46% of patients had at least one complication (rates increased from 3.07% in 2000 to 7.04% in 2013) (mostly bleeding or hematoma at access sites in 2.57% followed by pericardial complications in 1.3% of patients); ventricular tachycardia ablation had the highest rate of complications 9.9%, followed by atrial fibrillation ablation 7.21%, and supraventricular ablations with only 3.29% of reported complications [6].
In the NO-PARTY trial, a prospective, multicentre, randomized controlled trial in six electrophysiology laboratories in Italy, comparing a minimally fluoroscopic radiofrequency catheter ablation (MFA) with conventional fluoroscopy-guided ablation for supraventricular tachycardia, 231 patients underwent an ablation following the EP study with a complications rate of 1.1% (P = ns). The procedural complications were as follows: one arteriovenous fistula solved by compression in MFA group and two first-degree atrioventricular node blocks spontaneously solved in 48 h in ConvA group. The mean follow-up time was 12 + 4 months, during which no procedure-related complication occurred [7]. Sommer et al. showed in a cohort of 1000 patients who underwent AF ablation using near-zero fluoroscopy approach an overall complication rate of 2.0% including femoral pseudoaneurysm (n = 10, 1%), arteriovenous fistula (n = 1, 0.1%), pericardial effusion (n = 7, 0.7%), phrenic nerve palsy (n = 1, 0.1%), and stroke (n = 1, 0.1%). The median procedure time was 120 min, median fluoroscopy time was 0.90 min, and the median fluoroscopy dose was 345.1 cGy/cm2 [8].
There are mainly three types of complications we want to prevent: perforation of vascular structures and bleeding, thromboembolic complications, and damage of the normal conduction system. We are going to discuss how to avoid and manage each one of these complications.
Bleeding
-
1.
Vascular access : Venous and arterial punctures carry the inherent risk of bleeding. The need of fluoroscopy in this seeting is, in some labs, the visualization of the femoral head, to guide a high arterial puncture, and the potential use of an arterial closing device at the end of the procedure without the risk of blocking the femoral bifurcation, which also needs an arteriography at the end. If it is the case, a way to reduce fluoroscopy utilization could be an arterial puncture guided by vascular ultrasound, but at the end the arteriography will would be still necessary, before the deployment of the vascular closing device; if the puncture was done too close to the bifurcation, manual compression is needed. For most of EP procedures however, venous punctures are needed, they do not need any special equipment or fluoroscopy, but vascular ultrasound is also gaining acceptability to reduce the risks of inadvertent arterial puncture. Some labs use the left antecubital venous access to place a non-deflectable coronary sinus 6F catheter from above, it is an area easier to compress and with less bleeding risk than the usual groin access. Even in left-sided procedures with retrograde access we routinely use 7F introducers, and manual compression is the default, applied by trained nurses in an adjacent compression room, to speed workflow at our busy lab. Arterial closure devices and “figure-of-eight” suture [9, 10] have dramatically reduced bleeding after introducer retrieval, even if full anticoagulation is used. Finally, the use of 3-D mapping systems helps to reduce the number of catheters needed, in our lab the two-catheter technique is the default setting for the clear majority of substrates, and less punctures mean also less risk of complications.
-
2.
Catheter placement: Once the vascular access is achieved, catheters need to follow the vessel chosen to arrive to the heart chambers; unless extreme force is applied, it is very unlikely to cause any bleeding while advancing the catheters; radiofrequency is never used while the ablation catheter progresses (and once the ablation catheter is in the vasculature, we keep power in zero values until it is time to ablate, to prevent inadvertent activation of the RF pedal). If there is abnormal resistance to catheter advancement, we should try first to introduce a softer and smaller catheter; we can try to advance a long guide wire and then connect it to the 3-D mapping system (please refer to Chap. 5) to confirm the position and use it as a rail for a longer introducer (especially for arterial retrograde access in patients with vascular peripheral disease), or if a guidewire does not progress easily, sometimes fluoroscopy and arteriography is needed to exclude dissection. One helpful manoeuvre using deflectable catheters is to full bend the catheter just after it went through the sheath for preventing it to go into smaller collateral branches of the vessel. Arriving to the right atrium through the inferior vena cava has no major challenges, other than catheters sometimes directing to hepatic or diaphragmatic veins; all systems allow visualization of the catheters at this level and even further, gentle retrieval, torque and advancement allow the catheter to arrive to the atrium and record atrial EGMs. Arriving to the aorta possess a different challenge; the catheter should start acquiring the virtual anatomy at the arch level, and movements of advancement, rotation and retrieval should be done smoothly; while working with fluoroscopy most centres would perform a selective angiography to guide then the procedure; in a non-fluoroscopic environment, the coronary arteries are not visualized and their ostia cannot be estimated unless the aortic valve cusps are depicted; once the ascending aorta shell has been created, we can flex the ablation catheter and use both RAO and LAO incidences to protrude into the ventricle. Intracardiac echocardiography (ICE) is very useful in aortic cusp assessment and is also capable of showing the ostium of the coronary arteries. Transeptal puncture is extensively discussed in the atrial fibrillation chapter. it is impossible to achieve without the use of ICE or TEE, to prevent perforation and bleeding.
-
3.
Ablation: The higher the force applied and the higher the power delivered at any location, the higher the chances to cause perforation and bleeding. The contact force and power setting applied are independent of the fluoroscopy utilization, but it is a common knowledge the usefulness of fluoroscopy to assess the heart silhouette and the heart moving to rule out perforation and tamponade. To prevent perforation there are different options available: we can use proprietary catheters displaying the force applied (Carto and Abbot have catheters available); but, as it would be too expensive to use these catheters in a daily basis for all substrates, we should also carefully titrate the power delivered based on the location targeted. Most of the sensible locations as the junction of the inferior vena to the cavotricuspid isthmus, the coronary sinus, the right atrial appendage, the superior vena cava, the right ventricular outflow tract, and the aortic cusps rarely need more than 20–30 W to achieve ablation with non-irrigated catheters and 20 W when an irrigated catheter is used. Ablation in the left atrium also needs titration between 30 and 40 W (exception to high power short application time emerging as a new modality of atrial fibrillation ablation). If despite our efforts perforation occurs, to wait until a “silent heart” is observed in fluoroscopy is usually too late, we should recognize faster the complication, to react in a timely manner: Hemodynamic monitoring (arterial line or beat-to-beat blood pressure if patient heavily sedated or general anaesthesia used) and ultrasound readily available (most of EP labs have now ultrasound machines in the lab) are the best friends to easily recognize a perforation and impending tamponade. Every unexpected drop in blood pressure (even if associated to a vagal phenomenon) should be investigated. Sudden impedance rise and steam popping are ominous markers of charring and perforation if in sensitive areas, they should trigger a quick look ultrasound before continuing RF. Finally, if a pericardiocentesis is needed, ultrasound guided puncture is now the recommended mean to place the drain, making fluoroscopy rarely necessary, even if a complication arise.
Thromboembolic Complications
The more thrombogenic material we put into the vasculature, the higher the risk of thrombosis. There is also a relation between anticoagulation levels used and the risk of bleeding. It should be stated that any bleeding is easier to deal than a thromboembolic complication; if we need to balance bleeding risk versus thromboembolic risk, we should always prefer more bleeding and less thromboembolic events in any setting or ablation procedure.
We routinely administer empiric 5000 units IV of unfractionated heparine once the venous punctures are achieved for any procedure (even right sided), and switch to full anticoagulation (targeting with ACT monitoring depending on ablation type) if for any reason a left-sided access is needed. In atrial fibrillation ablation setting, most of the labs perform now the ablation on uninterrupted warfarine , and there is also evidence that uninterrupted dabigatran is as safe warfarin in this setting [11]. Flutter ablation is also performed with uninterrupted anticoagulation, there is few evidence available, but ablation with uninterrupted warfarine has been tested safer than bridge with heparine, in this setting [12].
The potential need of fewer catheters when a 3-D system is used could contribute to diminish also the risk of thromboembolic complications .
AV Block
In AVNRT , para-Hisian accessory pathways , or any other septal ablation—as some outflow tract ventricular arrhythmias—there is an associated risk of AV block. The goal to prevent AV nodal or His damage is to be able to visualize always catheter movement, a task rarely feasible with fluoroscopy, as it would mean the constant use of radiation; even most conservative labs would not use fluoroscopy every time the radiofrequency is on. 3-D mapping systems allows to visualize all catheters, always, and not only in standard simultaneous RAO and LAO views; but other, multiple and infinite angulations are also possible, depending on the area of interest.
Using 3-D mapping systems for all arrhythmia settings, we have developed the habit to annotate any His recording seen in the virtual anatomy (as only two catheter approach is used, we do not place an extra His catheter), to prevent the ablation catheter to move close.
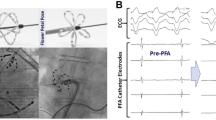
As we describe in the AVNRT ablation chapter, tagging all His potentials found in the virtual anatomy, we recorded a mean His area of 1.44 cm2; it is clearly not a fact that a His bundle occupies that big area, but the His displaces with every heart beat and respiratory movements, while our shell of virtual anatomy is a still structure. We judge than working in a non-fluoroscopy environment, no RF lesion should be applied closer than 10 mm far (caudal) from the lowest His found and tagged (Fig. 15.1a, b) [13]. Ablation of para-Hisian accessory pathways is also a challenge, but we should keep in mind that any accessory pathway has always a ventricular insertion (in this case, the para-Hisian one), but also an atrial insertion, with some anecdotic reports showing this insertion sometimes faraway (as aortic cusps) making it safe for RF to ablate [14].
(a, b) Carto 3 system . LAO for both figures. (a) Shows the distance between successful ablation sites and the highest His recorded (usually where a His catheter sits, a comfortable 24.5 mm); (b) shows that His signals can be recorded far down, and that the real distance was 13.7 mm from the successful RF site and lowest His recorded
If security versus cost is not a trade-off situation, cryoablation provides—at a higher cost—unsurpassed security while dealing with ablation in the septal area close to the His or AV node. Any cryocatheter can be used with Abbot Nav-X or Boston Rythmia systems ; Carto needs a Navistar plugged in order to construct the virtual anatomy to navigate; some centres use a Navistar and a cryoablation catheter, especially in young patients; as described in the AVNRT ablation chapter, we use a previous patient Navistar catheter placed in a bag beneath the thoracic region (usually under the mattress) of the new case, the virtual anatomy is then created with a decaNAV catheter , and finally the cryocatheter is now visualized as any other catheter and used for ablation. If there is no data showing when cryoablation is mandatory, when 1% of risk is deemed too high, the newer cryocatheters have shown a similar efficacy profile, with a lesser risk [15].
Catheter Entrapment
One mandatory need of fluoroscopy in a non-fluoroscopic ablation setting is to prevent catheter entrapment. To date we can visualize only the distal part of catheters, when a 3-D mapping system is used to reduce or eliminate fluoroscopy; there are some rare situations when a catheter “loops” while entering in the vasculature, we had in more than 700 procedures done without fluoroscopy, three cases when it occurred. Systematically, the first feature detected was that the catheter was not responding to torque applied in the usual way. While trying to remove the catheter it blocked with the loop entrapped outside the introducer, at the groin level; further effort to remove the catheter “shrinks” the introducer (always with the loop out of it) to a level that it was impossible to either advance neither retrieve the catheter. A vascular surgery was prevented, accessing the vessel from the contralateral groin with a “lasso” catching the tip of the catheter to undo the loop. It can occur either in the venous or in the arterial bed. The advice is, once a catheter is not answering in a standard fashion to torque applied, please use the fluoroscopy, advance the catheter forcing the loop to enter a heart chamber (it is almost impossible to unloop a catheter in the inferior vena cava or the aorta) and turn it to undo the loop; the procedure can be continued then without fluoroscopy (Fig. 15.2).
A looped ablation catheter (at the inferior vena cava level) was advanced until the loop entered the right atrium. It was then easy to turn the catheter (the tip is located almost at the cervical level) to undo the loop. If we try to just retrieve the catheter, the loop becomes small and it can be entrapped “shrinking” the introducer at the groin level
Finally, a very rare catheter entrapment case happened us also once, using the Rhythmia Orion basket catheter without fluoroscopy: when the case was finished we close the basket catheter and tried to retrieve it but even if it well advanced until the groin level, it was impossible to remove; the fluoroscopy showed the ablation catheter entrapped between the splines of the basket catheter; we advanced the Orion back to the atrium, we open the splines, remove the ablation catheter and then easily retrieve the basket catheter without further difficulty. We recommend so, to remove all catheters before the basket catheter, and while it is still at the heart level with the splines yet open.
Conclusion
The non-fluoroscopic approach is a feasible and safe alternative to fluoroscopy for any ablation procedure. We have described some methods to prevent and deal with complications that could arise when using this approach. Newer developments on catheter visualization would help to easy our journeys without fluoroscopy.
Finally, we should keep in mind that the main propose of the non-fluoroscopic ablation is to make the procedure safer (for the patient and for the operator). So, we should never have to hesitate in use a few seconds of fluoroscopy trying to avoid further complications if necessary.
References
Murakawa Y, Yamane T, Goya M, Inoue K, Naito S, Kumagai K, Miyauchi Y, Morita N, Nogami A, Shoda M, Okumura K, Hirao K, Japanese Heart Rhythm Society Members. Influence of substrate modification in catheter ablation of atrial fibrillation on the incidence of acute complications: analysis of 10 795 procedures in J-CARAF study 2011–2016. J Arrhythm. 2018;34(4):435–40.
Latchamsetty R, Yokokawa M, Morady F, Kim HM, Mathew S, Tilz R, Kuck KH, Nagashima K, Tedrow U, Stevenson WG, Yu R, Tung R, Shivkumar K, Sarrazin JF, Arya A, Hindricks G, Vunnam R, Dickfeld T, Daoud EG, Oza NM, Bogun F. Multicenter outcomes for catheter ablation of idiopathic premature ventricular complexes. JACC Clin Electrophysiol. 2015;1(3):116–23.
Wang JS, Shen YG, Yin RP, Thapa S, Peng YP, Ji KT, Liao LM, Lin JF, Xue YJ. The safety of catheter ablation for premature ventricular contractions in patients without structural heart disease. BMC Cardiovasc Disord. 2018;18(1):177.
Ogunbayo GO, Charnigo R, Darrat Y, Shah J, Patel R, Suffredini J, Wilson W, Parrott K, Kusterer N, Biase LD, Natale A, Morales G, Elayi CS. Comparison of complications of catheter ablation for ventricular arrhythmias in adults with versus without structural heart disease. Am J Cardiol. 2018;122(8):1345–51.
Dubin AM, Jorgensen NW, Radbill AE, Bradley DJ, Silva JN, Tsao S, Kanter RJ, Tanel RE, Trivedi B, Young ML, Pflaumer A, McCormack J, Seslar SP. What have we learned in the last 20 years? A comparison of a modern era pediatric and congenital catheter ablation registry to previous pediatric ablation registries. Heart Rhythm. 2019;16(1):57–63. https://doi.org/10.1016/j.hrthm.2018.08.013. pii: S1547-5271(18)30800-2
Hosseini SM, Rozen G, Saleh A, Vaid J, Biton Y, Moazzami K, Heist EK, Mansour MC, Kaadan MI, Vangel M, Ruskin JN. Catheter ablation for cardiac arrhythmias: utilization and in-hospital complications, 2000 to 2013. JACC Clin Electrophysiol. 2017;3(11):1240–8.
Casella M, Dello Russo A, Pelargonio G, Del Greco M, Zingarini G, Piacenti M, Di Cori A, Casula V, Marini M, Pizzamiglio F, Zucchetti M, Riva S, Russo E, Narducci ML, Soldati E, Panchetti L, Startari U, Bencardino G, Perna F, Santangeli P, Di Biase L, Cichocki F, Fattore G, Bongiorni M, Picano E, Natale A, Tondo C. Near zerO fluoroscopic exPosure during catheter ablAtion of supRavenTricular arrhYthmias: the NO-PARTY multicentre randomized trial. Europace. 2016;18(10):1565–72.
Sommer P, Bertagnolli L, Kircher S, Arya A, Bollmann A, Richter S, Rolf S, Hindricks G. Safety profile of near-zero fluoroscopy atrial fibrillation ablation with non-fluoroscopic catheter visualization: experience from 1000 consecutive procedures. Europace. 2018;20(12):1952–8.
Aytemir K, Canpolat U, Yorgun H, Evranos B, Kaya EB, Sahiner ML, Ozer N. Usefulness of ‘figure-of-eight’ suture to achieve haemostasis after removal of 15-French calibre femoral venous sheath in patients undergoing cryoablation. Europace. 2016;18:1545–50.
Kottmaier M, Bourier F, Reents T, Reiter A, Kornmayer M, Semmler V, Telishevska M, Koch-Büttner K, Deiss M, Brooks S, Grebmer C, Lennerz C, Kolb C, Hessling G, Deisenhofer I. Safety and feasibility of subcutaneous purse-string suture of the femoral vein after electrophysiological procedures on uninterrupted oral anticoagulation. Am J Cardiol. 2017;119(11):1781–4.
Calkins H, Willems S, Gerstenfeld EP, Verma A, Schilling R, Hohnloser SH, Okumura K, Serota H, Nordaby M, Guiver K, Biss B, Brouwer MA, Grimaldi M, RE-CIRCUIT Investigators. Uninterrupted dabigatran versus warfarin for ablation in atrial fibrillation. N Engl J Med. 2017;376(17):1627–36.
Finlay M, Sawhney V, Schilling R, Thomas G, Duncan E, Hunter R, Virdi G, Abrams D, Sporton S, Dhinoja M, Earley M. Uninterrupted warfarin for periprocedural anticoagulation in catheter ablation of typical atrial flutter: a safe and cost-effective strategy. J Cardiovasc Electrophysiol. 2010;21(2):150–4.
Chaumont J, Al Baridi E, Roux J-F, Badra M, Arseneau F, Ayala-Paredes F. His area is closer than expected to RF ablation lesions in AVNR Tachycardia. Abstract 612. CCS Congress. October 30, 2012. Toronto. Canada. Can J Cardiol. 2012;28(5):S327.
Liao Z, Zhan X, Wu S. Successful radiofrequency ablation of a parahisian accessory pathway from the right coronary cusp. Int J Cardiol. 2015;186:41–2.
Wells P, Dubuc M, Klein GJ, Dan D, Roux JF, et al. Intracardiac ablation for atrioventricular nodal re-entry tachycardia using a 6 mm distal electrode cryoablation catheter: prospective, multicenter, North American study (ICY-AVNRT). J Cardiovasc Electrophysiol. 2018;29(1):167–76.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Klein, A.C., Proietti, R., Ayala-Paredes, F. (2019). Complications of Radiofrequency Catheter Ablation and Prevention Methods. In: Proietti, R., Wang, Y., Yao, Y., Zhong, G., Lin Wu, S., Ayala-Paredes, F. (eds) Cardiac Electrophysiology Without Fluoroscopy. Springer, Cham. https://doi.org/10.1007/978-3-030-16992-3_15
Download citation
DOI: https://doi.org/10.1007/978-3-030-16992-3_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-16991-6
Online ISBN: 978-3-030-16992-3
eBook Packages: MedicineMedicine (R0)