Abstract
Purpose of review
This review discusses the role of radiofrequency (RF) catheter ablation for the treatment of cardiac arrhythmias and how recent advances in the understanding of RF biophysics have increased procedural safety and efficacy.
Recent findings
For the treatment of atrial arrhythmias, strategies that can achieve transmural lesions while avoiding collateral injury to neighboring structures are essential. Advancements such as contact force sensing, high-power short-duration RF application, ablation lesion indices, and esophageal protection have improved the safety and efficacy of catheter ablation in the atrium. In contrast to atrial arrhythmias, substrate in ventricular myocardium is often deep and may be surrounded by fibrosis, fat, and calcified scar, which can impair delivery of RF and prevent adequate lesion formation. Understanding RF biophysics allows the operator to optimize energy delivery to create deeper and larger lesions. Strategies such as RF delivery with careful power titration, high impedance irrigants, bipolar ablation, and needle intramyocardial ablation with the SERF system allow successful treatment of ventricular arrhythmias that are refractory to conventional approaches.
Summary
Advancements in the understanding of RF biophysics continue to be fundamental to the evolution of the treatment of cardiac arrhythmias.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Opinion Statement
Radiofrequency (RF) catheter ablation has been the primary energy source in cardiac electrophysiology for over 30 years, facilitating a safe, effective, and minimally invasive treatment option for the treatment of cardiac arrhythmias. This method delivers electrical energy to targeted myocardium via a catheter, which induces tissue heating and myocardial necrosis. Advancements in the understanding of RF biophysics, ablation catheter and RFA generator designs have allowed electrophysiologists to improve the safety and efficacy of catheter ablation treatment for atrial and ventricular arrhythmias.
Ongoing research and clinical trials promise further refinements in RF catheter ablation. These advancements continue to expand the therapeutic options for managing cardiac arrhythmias and provide clinicians with a safer and more sophisticated toolkit for addressing a spectrum of cardiac rhythm disorders.
Introduction
Catheter ablation with RF has been the predominant energy modality for the treatment of cardiac arrhythmias since the early 1990s [1, 2]. The popularity of RF can be attributed to its effectiveness, controllability, convenience, minimally invasive approach, and relatively affordable cost. A comprehensive grasp of the fundamental biophysics governing the delivery of RF energy is crucial for operators to enhance the success of the procedure while minimizing risk to patients. The power utilized in RF applications generally range from 20 to 50 Watts, with the recent introduction of systems that can deliver up to 90 Watts in a temperature-controlled setting [3]. The primary mechanism underlying RF-induced injury to myocardium is thermal, with myocardial injury and death occurring when a temperature of approximately 50 °C is reached [4]. Consequently, the primary objective of RF catheter ablation is to attain this critical temperature elevation in the targeted tissues while avoiding adverse thermal effects such as coagulum formation, steam pops, and heating of adjacent structures. To optimize this process, a thorough exploration of the biophysics of RF catheter ablation is essential, particularly focusing on the electrical properties of RF current delivery and the thermodynamics of RF heating in tissue.
Radiofrequency Catheter Ablation for the Management of Arrhythmias
Biophysics of Radiofrequency Ablation
RF energy used for cardiac ablation is an alternating current oscillating at approximately 500 kHz and is delivered to the body between a metal electrode located on the tip of an ablation catheter and a distal grounding electrode, usually in the form of a skin patch, which serve as the anode and cathode, respectively. Current travels through the body between the two electrodes and results in tissue heating that is directly proportional to current density. This flow of electric current induces ohmic heating in the tissue, referred to as resistive heating. The magnitude of resistive heating is directly proportional to the square of the current density, with current density inversely proportional to the square of the distance from the ablation electrode. Consequently, the dissipation of power per unit volume diminishes significantly with distance, and resistive heating decreases with the distance from the ablation electrode to the fourth power [5]. Myocardial tissue closest to the ablation catheter electrode undergoes resistive heating, and adjacent tissue will experience heating via conductive heat transfer. Resistive heating is immediate and is related to the resistance of the tissue at the electrode and tissue interface, with approximately 90% of the energy absorbed within the first 2 mm of tissue [6]. Tissue beyond this zone experiences passive heating via conductive heat transfer. Myocardial tissue undergoes necrosis at 50◦C and the size of the RF ablation lesion is dependent on resistive heating, conductive heat transfer, and tissue cooling from blood flow, catheter irrigation, and myocardial perfusion [4, 6, 7] (Fig. 1).
Thermodynamics of radiofrequency catheter ablation. Radiofrequency energy is delivered by a generator between an electrode on the tip of the ablation catheter and a grounding pad. High current density at the catheter tip causes a zone of immediate resistive heating close to the electrode-tissue interface and subsequent conductive heating. There is catheter and tissue cooling from catheter irrigation, blood flow within the cardiac chambers, and coronary perfusion
Treatment Options
Optimizing Biophysics of RF for Ablation of Atrial Myocardium
Pulmonary vein isolation (PVI) has become a cornerstone treatment for atrial fibrillation ever since Haissaguerre et al. described their role in initiating atrial fibrillation [8]. Contemporary PVI is achieved with a set of lesions that encompasses a wide antral circumferential ablation (WACA) area [9] and may also include additional lesion sets such as posterior wall isolation, a lateral mitral isthmus line, or a cavotricuspid isthmus line. Achieving transmural lesions in thin atrial tissue while minimizing thermal injury to adjacent structures, especially along the left atrial posterior wall which is adjacent to the esophagus, remains a challenge.
Contact Force Sensing
The integration of contact force (CF) sensing in RF ablation represents a significant advancement. CF, the amount of pressure exerted by the catheter on the tissue, has emerged as a crucial determinant influencing the size and effectiveness of lesions created [10], with increasing contact force resulting in significantly larger lesion size and incidence of steam pop. CF sensing provides real-time feedback to operators, allowing them to gauge the force applied during ablation and achieve the desired therapeutic effect while minimizing the risks associated with excessive or insufficient force. There is a significant increase in freedom from atrial arrhythmia when achieving a target CF and catheter stability [11].
Lesion Formation Indices
Ablation Index (AI), a proprietary formula used with the CARTO electroanatomic mapping system (Biosense Webster, INC, Diamond Bar, CA), represents an innovative metric for assessing the quality of ablation lesions in the atrium, encompassing power, contact force (CF), and time. This formula has demonstrated accuracy in estimating ablation lesion depth through preclinical studies, enabling operators to predict transmularity of lesions during the procedure [12]. A multicenter retrospective investigation involving protocol-mandated repeat procedures after two months was used to define the minimum regional AI target values. These values, crucial for preventing acute and late pulmonary vein (PV) reconnection, were identified as 550 for anterior and roof segments and 400 for posterior and inferior left atrial (LA) segments [13].
This ablation endpoint was later implemented in the CLOSE protocol, an ablation strategy aiming to further improve durable pulmonary vein isolation. Point-by-point RF delivery was delivered to create a contiguous circle encompassing the pulmonary veins. Ablation index with predefined settings for catheter stability (3 mm for 8 s), minimum CF (30% of time > 4 g) and ablation index (AI) of ≥ 400 at the posterior wall/roof and ≥ 550 at the anterior wall. The maximal inter-lesion distance between two neighboring lesions was limited to ≤ 6 mm. By closely monitoring CF, catheter stability, inter-lesion distance, and AI, the CLOSE protocol was shown to have superior freedom from atrial arrhythmias compared to conventional contact force-guided ablation [14].
Lesion size index (LSI) (St. Jude Medical, St. Paul, Minnesota) is another metric that has been shown to correlate with lesion formation [15]. In contrast to AI, which only uses operator-controlled variables (power, CF and time), LSI also uses impedance, which encompasses myocardial tissue changes during lesion formation. An LSI of greater than 5.2 on the anterior wall and 4.0 on the posterior wall have been identified as optimal targets to minimize conduction gaps and LSI > 5.0 is associated with higher first pass isolation rates [16, 17].
AI and LSI combine multiple parameters into a simple metric that allows operators to assess lesion formation. These indices have been shown to shorten procedure time, reduce total RF delivery, reduce fluoroscopy time, increase first pass pulmonary vein isolation rates and likely increase freedom from atrial arrhythmias [14, 18].
High Power Short Duration Ablation
High power short duration (HPSD) is an RF ablation strategy that creates lesions by prioritizing myocardial resistive heating and limiting conductive heat transfer, thereby causing myocardial tissue destruction while limiting heating of adjacent structures (Fig. 2). HPSD settings are generally accepted as RF energy between 40 to 90 watts for less than 15 s [19]. In in vivo and computational ablation models, HPSD compared to standard RF settings results in lesions with greater surface area, similar depth, improved lesion uniformity and an increase in lesion contiguity [20]. Interestingly, one animal study showed that HPSD ablation with 90 watts for 4 s resulted in greater thermal latency compared to lower power applications, suggesting that a significant portion of the lesion continues to form after the termination of RF due to conductive heating [21]. This raises the possibility of heat stacking, which is the accumulation of tissue heating from contiguous lesions and may increase the risk of adjacent tissue injury [22]. However, the peak tissue temperature and total time above the 50 °C (myocardial lethal isotherm) was lower with 90 watts for 4 s compared to lesions created with 50 watts for 10 s or 30 watts for 30 s, suggesting that even if conductive heating plays a significant role in lesion formation, remote heating remains less with HPSD [17].
High-Power Short Duration versus Standard Low Power Long Duration Radiofrequency Ablation (RF). A Low power, long duration RF has a smaller zone of resistive heating and a greater portion of tissue heating due to conductive heating compared to (B) high power, short duration RF, where there is less conductive heating and therefore a lower risk of heating adjacent organs.
Clinical experience using HPSD ablation compared to conventional power settings show that there is a higher first pass PVI rate, shorter RF time, fluoroscopy time, total procedural time, LA dwell time, lower rates of chronic PV reconnections and a higher freedom from atrial arrhythmias without a significant difference in rates of esophageal injury [23]. A large retrospective analysis of HPSD including 13,974 ablations in 10,284 patients found that complication rates using HPSD were extremely low, with pericardial tamponade occurring in 0.24%, stroke within 30 days in 0.086%, steam pops in 0.014%, atrioesophageal fistula in 1 patient (0.009%), and two deaths (0.014%; one due to stroke and one due to atrioesophageal fistula) [24]. One concern of HPSD ablation is the trend in increased asymptomatic cerebral emboli compared to conventional power ablation [25]. The clinical impact of these findings is not clear as there are no apparent acute neurologic sequalae and most resolve on follow up imaging [26]. Furthermore, the cause of asymptomatic cerebral emboli remains unknown and may be due to char, thrombus, or bubbles from saline irrigation and may vary with different catheter and generator designs [25].
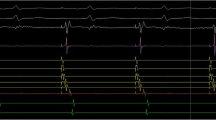
A majority of HPSD ablation is performed using 50 watts, which is the maximum output of most generators currently in use. However, a new system (QDOT MICRO, Biosense Webster, Diamond Bar, CA) shows promise in improving upon current HPSD ablation by utilizing a novel catheter and temperature-controlled generator that can deliver up to 90 watts over 4 s, known as very high-power short duration ablation (vHPSD). Thermocouples in the catheter provide real-time tissue-temperature feedback, allowing the system to titrate catheter irrigation and power (Fig. 3), which has been shown to reduce the incidence of steam pops [27] and improve procedural times without compromise to effectiveness or safety [28]. Furthermore, the contribution of contact force to lesion formation may be less in vHPSD, allowing operators to target a lower contact force without impacting lesion transmurality in areas at risk for collateral injury to adjacent organs, such as the esophagus [29].
QDOT Temperature-Guided Power Titration. The QDOT catheter has six temperature probes that simultaneously monitor temperature distribution around the tip of the catheter. When delivering 90 watts, these probes are used to titrate power in case it exceeds a pre-established temperature threshold. This figure illustrates power truncation when a threshold temperature was reached during RF delivery (at 2 s). Once temperature falls below the threshold, power is increased back to 90 watts. Key: QDOT (QDOT MICRO catheter (Biosense Webster, INC, Diamond Bar, CA)); radiofrequency (RF)
Esophageal Protection
The anatomical proximity of the left atrium (LA) to the esophagus holds relevance in RF ablation procedures. The posterior wall of the left atrium overlies the esophagus and is only separated by < 5 mm [30]. Tissue heat capacitance may lead to accumulation of conductive heat from consecutive lesions, a phenomenon known as heat stacking, which can lead to esophageal injury. In rare instances (< 0.1% to 0.25%) this can cause atrioesophageal [31] and pericardioesophageal [32] fistulas, which have a mortality rate of 100% without treatment and up to 41% with surgical treatment [33,34,35]. Strategies that attempt to reduce the risk of esophageal injury include esophageal temperature monitoring [36], mechanical esophageal deviation [37], avoidance of contiguous lesions, increasing time between RF applications, and HPSD ablation strategy [22, 38, 39]. However, these protective strategies have variable efficacy and have separate safety concerns related to their use or may impact RF ablation efficacy.
Optimizing Biophysics of RF to Target Deep Ventricular Substrate
In contrast to ablation in atrial tissue, arrhythmia substrate in ventricular myocardium is often deep and may be surrounded by fibrosis, fat, and calcified scar, which can impair delivery of RF and prevent adequate lesion formation. Understanding the biophysics of RF allows for the optimization of current delivery to maximize lesion depth (Table 1). While deep lesion formation is a priority when performing an ablation, caution should be taken to prevent major complications associated with excessive heating. Heating at the catheter-tissue interface may lead to coagulum or char formation, which increases the risk of thromboembolism [6]. Cooling via catheter irrigation has significantly reduced the risk of these events [40]. However, a risk that remains is a phenomenon known as steam pops, which is the accumulation of steam bubbles within heated tissue that can culminate in an explosion of myocardial tissue. A steam pop results in an audible explosion with characteristic tactile feedback through the ablation catheter [41]. Steam pops can be catastrophic and are associated with cardiac perforation and de novo ventricular septal defects [42, 43].
The formation of deep lesions is primarily achieved via conductive tissue heating. Lesion size is proportional to total RF time and RF power, however, compared to an increase in RF duration, the same proportional increase in RF power yields a significantly larger lesion size. In an ex vivo model, lesions continued to increase in size up to 90 s, at which point ablation was stopped [44]. However, there is evidence that lesions continue to increase in size with RF of more than 90 s. Prolonged duration of RF ablation targeting ventricular arrhythmias originating from the LV summit found that RF delivery for durations up to 5 min with careful titration of RF power achieved acute procedural success in 84% of patients compared to in 68% in which standard RF duration (< 120 s) was used [45].
Strategies that optimize current delivery into the myocardium rather than the blood pool will further increase myocardial current density, tissue heating and lesion formation. The use of a high impedance irrigant, such as half normal saline, through the ablation catheter has been shown to increase lesion size by up to 60% compared to irrigation with normal saline [46]. Irrigation with half-normal saline replaces the low impedance blood pool with a high impedance cloud and shunts current into the myocardial tissue, which is the path of lower resistance. A multicenter prospective study in patients with deep myocardial substrate that was refractory to standard ablation found that the use of half-normal saline irrigant was safe and achieved acute success in 83% of those patients. However, ablation using half-normal saline was associated with steam pops in 12.8% of patients. No adverse clinical events were observed secondary to the steam pops [47].
Bipolar Ablation
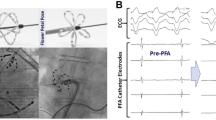
Bipolar radiofrequency catheter ablation is an important therapeutic option for ventricular arrhythmias resistant to standard treatments. Rather than delivering RF energy between an ablation catheter and a remote grounding pad, bipolar RF is delivered between two catheters across the target tissue, which serve as the anode and cathode, creating lesions that are deeper, narrower, and more likely transmural compared to unipolar ablation [48] (Fig. 4). This strategy is particularly advantageous in addressing intramural arrhythmias, providing a promising solution for challenging cases. The benefits of bipolar ablation are evident in its ability to achieve high success rates, even in patient populations known for high rates of ablation failure and arrhythmia recurrence. Notably, the effectiveness of bipolar ablation is further enhanced when employed in a strategic manner, such as through low-to-high energy titration or in combination with prior sequential unipolar ablation. Overall, bipolar ablation emerges as a valuable and versatile approach, providing clinicians with a powerful tool to address therapy-refractory ventricular arrhythmias with improved precision and efficacy [49]. Nevertheless, it is worth noting that the high tissue current density resulting from this strategy also increases the risks for major complications, such as steam pops, and has been associated with de novo ventricular septal defects [50].
Bipolar ablation setup for targeting a left ventricular summit PVC. The electroanatomic mapping system (A) and fluoroscopy (B) show the active catheter in the left ventricular outflow tract and the return catheter in the distal coronary sinus. C Application of RF causes successful PVC suppression. Key: PVC (premature ventricular contraction); radiofrequency (RF). (Used with permission of Elsevier Inc., from Enriquez A, et al. Heart Rhythm O2 2024;5:24–33, permission conveyed through Copyright Clearance Center, Inc.) [49]
Sequential and Simultaneous Unipolar Ablations
As bipolar ablation setups are not commercially available, other strategies using commercially available equipment has been described aiming to target intramural arrhythmic foci. For instance, sequential unipolar ablation has been described as a suitable alternative in cases were conventional ablation approaches are unable to reach intramural VT origin [51]. It is usually performed for ventricular arrhythmias originating from the intramural interventricular septum. A first lesion is usually delivered at the site of earliest activation and a second one is delivered on the opposite side of the septum with the goal of achieving transmurality.
On the other hand, simultaneous unipolar RFA involves the delivery of RF energy from two catheter tips positioned on either side of a targeted area within the heart. This approach allows for modification of ablation sites based on anatomical landmarks to encompass the tissue of interest, potentially resulting in larger lesion size and depth, as shown in preclinical studies [52]. Yamada et al. demonstrated the safety and efficacy of this technique in targeting intramural foci, particularly in the left ventricular outflow tract, and its utility in nonischemic cardiomyopathy [53].
In this method, two open-irrigated ablation catheters are utilized, with power settings ranging from 30 to 50 W, adjusted to achieve a minimum impedance drop of 10%, monitored at each RF generator. Research involving patients with nonischemic cardiomyopathy and deep septal substrate indicated that simultaneous unipolar ablation resulted in VT-free survival in two-thirds of cases following the failure of sequential unipolar ablation [54].
Emerging Therapies
Needle intramyocardial ablation, utilizing a deployable needle and the Saline-Enhanced Radiofrequency (SERF) system, presents an advanced strategy for managing ventricular arrhythmias. Heated saline is injected directly into the myocardium via the deployable needle along with RF energy delivery, resulting in large and transmural lesions that surpass the capabilities of traditional radiofrequency ablation. In contrast to conventional approaches relying on resistive heating, SERF introduces a novel mechanism by injecting heated saline through a deployable needle, significantly enhancing convective heating within the myocardial wall. Preclinical studies have demonstrated the predictability of lesion volumes, highlighting the method's versatility [55]. Needle intramyocardial ablation with SERF addresses challenges associated with traditional methods, especially in cases refractory to antiarrhythmic drugs and conventional catheter ablation. The method's success is bolstered by careful catheter placement, real-time monitoring, and accumulated experience, contributing to a reduction in adverse events over time [56]. The innovative biophysical mechanisms and targeted approach of needle intramyocardial ablation with SERF hold promise for effectively reducing VT burden in high-risk patient groups unresponsive to conventional treatments.
Another strategy for improving RF lesion size and durability is with the targeted delivery of a cardiotoxic agent via heat sensitive liposomes. In a proof-of-concept study, Sauer et al. showed that facilitated ablation with doxorubicin containing heat sensitive liposomes (HSL-dox) improved RF lesion durability. This effect was more pronounced in lesions delivered with higher power and longer durations, presumably due to increased tissue heating and doxorubicin delivery. While the toxicity of doxorubicin prevents the clinical use of HSL-dox facilitated ablation, this study does demonstrate the feasibility of using HSL for the localized delivery of an agent and their potential future use for improving lesion formation and durability [57].
Conclusions
In summary, RF ablation creates tissue heating via resistive and conductive heating. Ablation of atrial arrhythmias has moved towards using a HPSD ablation strategy, which allows for less conductive heating of collateral structures. In addition, advancements in contact force sensing, ablation lesion indices, and esophageal protection have further improved the efficacy and safety of catheter ablation in the atrium. Effective ablation of ventricular arrhythmias requires the creation of deep lesions, which are created by optimizing tissue current delivery while avoiding the dangers of excessive heating at the catheter-tissue interface and within the myocardium. Strategies that enhance tissue current delivery, such as the use of long duration lesions with careful power titration, high-impedance irrigants, bipolar ablation, and needle intramyocardial ablation with SERF system are important strategies for the treatment of ventricular arrhythmias that are refractory to conventional ablation. As the field evolves, optimizing RFA biophysics remains crucial to enhancing the efficacy and safety of catheter ablation and expanding therapeutic options in managing cardiac arrhythmias.
Data Availability
No datasets were generated or analysed during the current study.
References
Sharma E, Varley A, Osorio J, et al. Procedural trends in catheter ablation of persistent atrial fibrillation: insights from the real-AF registry. Circ Arrhythm Electrophysiol. 2023;16:e011828.
Haines DE. The biophysics of radiofrequency catheter ablation in the heart: the importance of temperature monitoring. Pacing Clin Electrophysiol. 1993;16:586–91.
Hussein AA, Delaughter MC, Monir G, et al. Paroxysmal atrial fibrillation ablation with a novel temperature-controlled CF-sensing catheter: Q-FFICIENCY clinical and healthcare utilization benefits. J Cardiovasc Electrophysiol. 2023;34:2493–503.
Nath S, DiMarco JP, Haines DE. Basic aspects of radiofrequency catheter ablation. J Cardiovasc Electrophysiol. 1994;5:863–76.
Nándor S, László G. High-power, short-duration ablation in the treatment of atrial fibrillation patients. In: Mart M, Gabriel C, editors. Cardiac Rhythm Management. Ch. 6. Rijeka: IntechOpen; 2021.
Wittkampf FH, Nakagawa H. RF catheter ablation: Lessons on lesions. Pacing Clin Electrophysiol. 2006;29:1285–97.
Wood M, Goldberg S, Lau M, et al. Direct measurement of the lethal isotherm for radiofrequency ablation of myocardial tissue. Circ Arrhythm Electrophysiol. 2011;4:373–8.
Haissaguerre M, Jais P, Shah DC, et al. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med. 1998;339:659–66.
Proietti R, Santangeli P, Di Biase L, et al. Comparative effectiveness of wide antral versus ostial pulmonary vein isolation: a systematic review and meta-analysis. Circ Arrhythm Electrophysiol. 2014;7:39–45.
Ikeda A, Nakagawa H, Lambert H, et al. Relationship between catheter contact force and radiofrequency lesion size and incidence of steam pop in the beating canine heart: electrogram amplitude, impedance, and electrode temperature are poor predictors of electrode-tissue contact force and lesion size. Circ Arrhythm Electrophysiol. 2014;7:1174–80.
Natale A, Reddy VY, Monir G, et al. Paroxysmal AF catheter ablation with a contact force sensing catheter: results of the prospective, multicenter SMART-AF trial. J Am Coll Cardiol. 2014;64:647–56.
Hussein A, Das M, Riva S, et al. Use of ablation index-guided ablation results in high rates of durable pulmonary vein isolation and freedom from arrhythmia in persistent atrial fibrillation patients: The PRAISE study results. Circ Arrhythm Electrophysiol. 2018;11:e006576.
Das M, Loveday JJ, Wynn GJ, et al. Ablation index, a novel marker of ablation lesion quality: prediction of pulmonary vein reconnection at repeat electrophysiology study and regional differences in target values. Europace. 2017;19:775–83.
Phlips T, Taghji P, El Haddad M, et al. Improving procedural and one-year outcome after contact force-guided pulmonary vein isolation: the role of interlesion distance, ablation index, and contact force variability in the ’CLOSE’-protocol. Europace. 2018;20:f419–27. Findings from this study show that a standardized RF delivery strategy that optimizes lesion formation and contiguity results in improved freedom from atrial fibrillation.
Calzolari V, De Mattia L, Indiani S, et al. In vitro validation of the lesion size index to predict lesion width and depth after irrigated radiofrequency ablation in a porcine Model. JACC Clin Electrophysiol. 2017;3:1126–35.
Kanamori N, Kato T, Sakagami S, et al. Optimal lesion size index to prevent conduction gap during pulmonary vein isolation. J Cardiovasc Electrophysiol. 2018;29:1616–23.
Venkatesh Prasad K, Bonso A, Woods CE, et al. Lesion Index-guided workflow for the treatment of paroxysmal atrial fibrillation is safe and effective - Final results from the LSI Workflow Study. Heart Rhythm. 2022;O2(3):526–35.
Liu X, Gui C, Wen W, He Y, Dai W, Zhong G. Safety and efficacy of high power shorter duration ablation guided by ablation index or lesion size index in atrial fibrillation ablation: a systematic review and meta-analysis. J Interv Cardiol. 2021;2021:5591590.
Naniwadekar A, Dukkipati SR. High-power short-duration ablation of atrial fibrillation: A contemporary review. Pacing Clin Electrophysiol. 2021;44:528–40.
Barkagan M, Contreras-Valdes FM, Leshem E, Buxton AE, Nakagawa H, Anter E. High-power and short-duration ablation for pulmonary vein isolation: Safety, efficacy, and long-term durability. J Cardiovasc Electrophysiol. 2018;29:1287–96.
Nakagawa H, Ikeda A, Sharma T, et al. Comparison of in vivo tissue temperature profile and lesion geometry for radiofrequency ablation with high power-short duration and moderate power-moderate duration: effects of thermal latency and contact force on lesion formation. Circ Arrhythm Electrophysiol. 2021;14:e009899. Findings from this study show that RF delivery with very high power and short duration (90 watts for 4 seconds) has a lower peak tissue temperature and less time over 50 degrees celsius (the lethal isotherm) compared to lower power RF, but still had a portion of lesion formation due to conductive heating.
Steiger N, Qian PC, Foley G, et al. Measured temperatures using uninterrupted and interrupted sequences of radiofrequency applications in a phantom gel model: implications for esophageal injury. J Interv Card Electrophysiol. 2023;66:1925–8.
Ravi V, Poudyal A, Abid QU, et al. High-power short duration vs. conventional radiofrequency ablation of atrial fibrillation: a systematic review and meta-analysis. Europace. 2021;23:710–21.
Winkle RA, Mohanty S, Patrawala RA, et al. Low complication rates using high power (45–50 W) for short duration for atrial fibrillation ablations. Heart Rhythm. 2019;16:165–9.
Lee AC, Voskoboinik A, Cheung CC, et al. A Randomized Trial of High vs Standard Power Radiofrequency Ablation for Pulmonary Vein Isolation: SHORT-AF. JACC Clin Electrophysiol. 2023;9:1038–47. One of the only randomized control trials comparing HPSD to standard settings in the treatment of atrial fibrillation. Findings from this study show that HPSD is more efficient and effective, however, there was a signal for increased asymptomatic cerebral emboli.
Wieczorek M, Lukat M, Hoeltgen R, et al. Investigation into causes of abnormal cerebral MRI findings following PVAC duty-cycled, phased RF ablation of atrial fibrillation. J Cardiovasc Electrophysiol. 2013;24:121–8.
Leshem E, Zilberman I, Barkagan M, et al. Temperature-controlled radiofrequency ablation using irrigated catheters: maximizing ventricular lesion dimensions while reducing steam-pop formation. JACC Clin Electrophysiol. 2020;6:83–93.
Reddy VY, Grimaldi M, De Potter T, et al. Pulmonary vein isolation with very high power, short duration, temperature-controlled lesions: The QDOT-FAST trial. JACC Clin Electrophysiol. 2019;5:778–86.
Steiger N, McClennen L, Bilenker J, et al. Relative contribution of contact force to lesion depth using high power shor durantion radiofrequency application. Heart Rhythm. 2024. https://doi.org/10.1016/j.hrthm.2024.03.042.
Ho SY, Cabrera JA, Sanchez-Quintana D. Left atrial anatomy revisited. Circ Arrhythm Electrophysiol. 2012;5:220–8.
Canakci ME, Ovali C, Aydogdu I, Tiryaki Bastug B, Ahmadzai O, Bozdogan RF. Atrioesophageal fistula as a complication of radiofrequency ablation for atrial fibrillation. Prehosp Disaster Med. 2021;36:495–7.
Kheslat HH, Kelly S, Singh H, Crozier I. Esophagopericardial fistula following radiofrequency ablation for atrial fibrillation: insights into its management. JACC Case Rep. 2021;3:1132–5.
Calkins H, Kuck KH, Cappato R, et al. 2012 HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design. Europace. 2012;14:528–606.
Singh SM, d’Avila A, Singh SK, et al. Clinical outcomes after repair of left atrial esophageal fistulas occurring after atrial fibrillation ablation procedures. Heart Rhythm. 2013;10:1591–7.
Kapur S, Barbhaiya C, Deneke T, Michaud GF. Esophageal injury and atrioesophageal fistula caused by ablation for atrial fibrillation. Circulation. 2017;136:1247–55.
Leung LWM, Akhtar Z, Sheppard MN, Louis-Auguste J, Hayat J, Gallagher MM. Preventing esophageal complications from atrial fibrillation ablation: A review. Heart Rhythm. 2021;O2(2):651–64.
Parikh V, Swarup V, Hantla J, et al. Feasibility, safety, and efficacy of a novel preshaped nitinol esophageal deviator to successfully deflect the esophagus and ablate left atrium without esophageal temperature rise during atrial fibrillation ablation: The DEFLECT GUT study. Heart Rhythm. 2018;15:1321–7.
Perzanowski C, Teplitsky L, Hranitzky PM, Bahnson TD. Real-time monitoring of luminal esophageal temperature during left atrial radiofrequency catheter ablation for atrial fibrillation: observations about esophageal heating during ablation at the pulmonary vein ostia and posterior left atrium. J Cardiovasc Electrophysiol. 2006;17:166–70.
Vassallo F, Meigre LL, Serpa E, et al. Reduced esophageal heating in high-power short-duration atrial fibrillation ablation in the contact force catheter era. Pacing Clin Electrophysiol. 2021;44:1185–92.
Waldo AL, Wilber DJ, Marchlinski FE, et al. Safety of the open-irrigated ablation catheter for radiofrequency ablation: safety analysis from six clinical studies. Pacing Clin Electrophysiol. 2012;35:1081–9.
Nakagawa H, Yamanashi WS, Pitha JV, et al. Comparison of in vivo tissue temperature profile and lesion geometry for radiofrequency ablation with a saline-irrigated electrode versus temperature control in a canine thigh muscle preparation. Circulation. 1995;91:2264–73.
Tokuda M, Kojodjojo P, Epstein LM, et al. Outcomes of cardiac perforation complicating catheter ablation of ventricular arrhythmias. Circ Arrhythm Electrophysiol. 2011;4:660–6.
Schonbauer R, Sommer P, Misfeld M, et al. Relevant ventricular septal defect caused by steam pop during ablation of premature ventricular contraction. Circulation. 2013;127:e843–4.
Borne RT, Sauer WH, Zipse MM, Zheng L, Tzou W, Nguyen DT. Longer duration versus increasing power during radiofrequency ablation yields different ablation lesion characteristics. JACC Clin Electrophysiol. 2018;4:902–8.
Garg L, Daubert T, Lin A, et al. Utility of prolonged duration endocardial ablation for ventricular arrhythmias originating from the left ventricular summit. JACC Clin Electrophysiol. 2022;8:465–76. Findings from this study show that long duration RF application with careful power titration can successfully suppress arrhythmias with a deep myocardial focus.
Nguyen DT, Gerstenfeld EP, Tzou WS, et al. Radiofrequency ablation using an open irrigated electrode cooled with half-normal saline. JACC Clin Electrophysiol. 2017;3:1103–10.
Nguyen DT, Tzou WS, Sandhu A, et al. Prospective multicenter experience with cooled radiofrequency ablation using high impedance irrigant to target deep myocardial substrate refractory to standard ablation. JACC Clin Electrophysiol. 2018;4:1176–85.
Nguyen DT, Zheng L, Zipse MM, et al. Bipolar radiofrequency ablation creates different lesion characteristics compared to simultaneous unipolar ablation. J Cardiovasc Electrophysiol. 2019;30:2960–7.
Enriquez A, Hanson M, Nazer B, et al. Bipolar ablation involving coronary venous system for refractory left ventricular summit arrhythmias. Heart Rhythm. 2024;O2(5):24–33.
Maher TR, Raza A, Tapias C, et al. Ventricular septal defect as a complication of bipolar radiofrequency ablation for ventricular tachycardia. Heart Rhythm. 2024. 21(6):950–955.
Sudo K, Kuroki K, Asakawa T, Aonuma K, Sato A. Management of refractory intramural left ventricular summit ventricular arrhythmia: Acute success using bipolar radiofrequency catheter ablation with recurrence. J Arrhythm. 2023;39:979–83.
Chang RJ, Stevenson WG, Saxon LA, Parker J. Increasing catheter ablation lesion size by simultaneous application of radiofrequency current to two adjacent sites. Am Heart J. 1993;125:1276–84.
Yamada T, Maddox WR, McElderry HT, Doppalapudi H, Plumb VJ, Kay GN. Radiofrequency catheter ablation of idiopathic ventricular arrhythmias originating from intramural foci in the left ventricular outflow tract: efficacy of sequential versus simultaneous unipolar catheter ablation. Circ Arrhythm Electrophysiol. 2015;8:344–52.
Yang J, Liang J, Shirai Y, et al. Outcomes of simultaneous unipolar radiofrequency catheter ablation for intramural septal ventricular tachycardia in nonischemic cardiomyopathy. Heart Rhythm. 2019;16:863–70.
Dickow J, Suzuki A, Henz BD, et al. Characterization of lesions created by a heated, saline irrigated needle-tip catheter in the normal and infarcted canine heart. Circ Arrhythm Electrophysiol. 2020;13:e009090.
Packer DL, Wilber DJ, Kapa S, et al. Ablation of refractory ventricular tachycardia using intramyocardial needle delivered heated saline-enhanced radiofrequency energy: a first-in-man feasibility trial. Circ Arrhythm Electrophysiol. 2022;15:e010347.
Sauer WH, Steiger NA, Tzou WS, Schuller JL, Zheng L, Nguyen DT. Facilitated myocardial ablation using heat-sensitive liposomes containing doxorubicin: A proof-of-concept preclinical study. JACC Clin Electrophysiol. 2023;9:1404–8.
Bhaskaran A, Chik W, Pouliopoulos J, et al. Five seconds of 50–60 W radio frequency atrial ablations were transmural and safe: an in vitro mechanistic assessment and force-controlled in vivo validation. Europace. 2017;19:874–80.
Bennett R, Campbell T, Byth K, Turnbull S, Kumar S. Catheter ablation using half-normal saline and dextrose irrigation in an ovine ventricular model. JACC Clin Electrophysiol. 2021;7:1229–39.
Nguyen DT, Tzou WS, Brunnquell M, et al. Clinical and biophysical evaluation of variable bipolar configurations during radiofrequency ablation for treatment of ventricular arrhythmias. Heart Rhythm. 2016;13:2161–71.
John RM, Connell J, Termin P, et al. Characterization of warm saline-enhanced radiofrequency ablation lesions in the infarcted porcine ventricular myocardium. J Cardiovasc Electrophysiol. 2014;25:309–16.
Funding
No funding was used for the creation of this manuscript.
Author information
Authors and Affiliations
Contributions
C.M, J.R., and N.S. wrote the main manuscript text. C.M. prepared the figures and tables. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Jorge Romero reports grants from Boston Scientific; consulting fees from Boston Scientific, Atricure, Biosense Webster, and Medtronic; payment or honoraria from Boston Scientific, Biosense Webster, and Atricure; and participation on a Data Safety Monitoring Board or Advisory Board for Boston Scientific. Carlos Matos and Nathaniel Steiger declare that they have no conflicts of interest relevant to this article.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Matos, C.D., Romero, J.E. & Steiger, N.A. Biophysics of Radiofrequency Ablation for Cardiac Arrhythmias: A Current Review. Curr Treat Options Cardio Med 26, 221–231 (2024). https://doi.org/10.1007/s11936-024-01043-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11936-024-01043-5