Abstract
The major challenges to the clinical application of zidovudine are its moderate aqueous solubility, relative short half-life, and incapability to go across BBB after systemic administration makes the brain one of the dominant HIV reservoirs. We investigated the development of zidovudine-loaded NLCs based on docosanol and oleic acid which were further surface modified with PEG4000 and HAS. The drug content and entrapment efficiencies were assessed by UV analysis. The mean diameter of the SyLN was found to be at 54.7 ± 1.4 nm with a zeta potential of −21.6 ± 0.2 mV and relatively low polydispersity. The NLCs showed excellent stability in the refrigerated condition, in blood serum and were safe for IV administration. In vitro release studies showed a sustained release profile of zidovudine in aCSF. In vivo plasma and brain pharmacokinetics investigation in a rat model showed that SyLN and SyLN-Peg NLCs rapidly reached the brain and yielded higher MRT, Cmax, and AUC. The rat brain pharmacokinetic data confirm the brain localization and accumulation of the developed NLCs delivering AZT in a sustained manner for a prolonged period of time, which is further confirmed by CLSM images of brain cryosections labeled with SyLN-C6 NLCs. Our results suggest that the developed docosanol NLCs could be a promising drug delivery system for long-term brain delivery of zidovudine in the treatment of Neuro-AIDS .
The original version of this chapter was revised. The correction to this chapter is available at https://doi.org/10.1007/978-3-030-06115-9_26
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Acquired immunodeficiency syndrome (AIDS) is one of the deadliest diseases known to humankind. According to WHO reports, AIDS has killed an estimated 39 million people until the year 2014. Today, about 37.3 million people are living with HIV, which results in 1.2 million deaths every year. Destroying the human body defense system by infecting the macrophages and CD4 T-cells are the primary hematopoietic targets of HIV. In the brain, the perivascular and parenchymal macrophages/microglia, oligodendrocytes, endothelial cells , neurons , and astrocytes are the targets of HIV. The process of neuroinvasion by HIV occurs via the HIV-infected circulating monocytes entering the brain during the course of routine immune surveillance and replacement of the perivascular macrophages. The HIV then replicates within the central nervous system (CNS), causing adverse neurological dysfunctions like the AIDS–dementia complex, which includes motor, cognitive, and behavioral impairments that culminate in morbidity at advanced stages of the infection [1, 2]. Zidovudine (AZT) was the first drug approved by the US FDA to treat HIV and AIDS in the year 1986. AZT shows its activity by inhibiting the HIV-encoded reverse transcriptase (RT) enzyme after conversion to AZT-5′-triphosphate by host cell kinases. AZT prevents the mother-to-child spread of HIV during birth or after a needle stick injury or other potential exposure. The oral and intravenous AZT induces immunologic, virologic, and neurologic improvements in HIV-1 infected patients [3]. On administering with other antiretroviral drugs, AZT reduces the blood level of the viruses below detectable ranges. While untreated AIDS patients have an average lifespan of 11 years after infections, AZT-treated patients can live a rather normal life [4]. The half-life of AZT in plasma is approximately 1 h, which necessitates frequent doses to maintain effective therapeutic AZT levels [5]. Although AZT enters cerebrospinal fluid readily, its ability to cross the blood–brain barrier (BBB) is less than optimal. The concentration ration of the CSF and plasma is about 0.06 [3, 5]. AZT is a high water-soluble drug belonging to the class III of the Biopharmaceutics Classification System (BCS). For adults, the recommended oral dose of AZT is 600 mg per day in divided doses (300 mg every 12 h or 200 mg orally every 8 h). The oral bioavailability of administered AZT is about 64 ± 10%. The IC50 and IC90 values (50% and 90% inhibitory concentrations) of AZT are 3–13 ng/mL and 30–130 ng/mL, respectively. The LD50 of AZT is 3084 mg/kg B.W [6].
Literature survey showed that AZT-loaded solid lipid nanoparticles [7,8,9], solidified lipid microparticles [10], liposomes [11], and polymeric nanoparticles have already been developed for effective brain delivery of AZT [12]. The major drawbacks of these formulations are larger particle size , poor brain target ability, toxicity , instability, drug loss on storage, expensive, no sustained release properties inside the brain, and lack of commercial viability.
NLCs are one of the latest drug delivery systems designed to deliver drugs to various tissues and organs. It is the next generation of the solid lipid nanoparticles (SLNs) which eliminates the drugs leakage on standing from SLN particles, the main disadvantage of SLNs. It has several advantages over other polymeric drug delivery systems. NLC can be utilized to target a wide range of body areas like tumors, brain, blood cells, and body cavities. It can be administered through different routes like oral, intravenous, and topical. The NLC is a suitable carrier for both lipophilic and hydrophilic drugs and has higher drug loading capability over SLNs and liposomes. NLCs are less or nontoxic, easily eliminable, biocompatible, and biodegradable [13, 14]. The main advantage of NLC is that it can be very easily scaled up for industrial production. Therefore, zidovudine loaded docosanol NLCs could eliminate all disadvantages of all the previously reported novel nanocarrier systems. Until date, no brain targeted NLC formulation of zidovudine has been reported. However, human brain cell line (C6) compatible nano lipid carriers (NLCs) of azidothymidine had been reported [15] with no in vivo efficacy.
1-Docosanol, also known as behenyl alcohol, is a saturated fatty alcohol used traditionally as an emollient, emulsifier and thickener in cosmetics and nutritional supplement, either alone or with other constituents of policosanol, which is effective as a lipid-lowering agent [16,17,18,19]. Docosanol is easily metabolized by oxidation to n-docosanoic acid and then incorporated as an acyl group on polar lipids and internalized by cells [20, 21]. Studies have shown that docosanol is nontoxic to rats, rabbits, and dogs [22, 23]. Docosanol has been approved by the US FDA as a 10% over-the-counter cream for the treatment of recurrent orolabial herpes. NLC formulations have been developed and reported with behenyl alcohol as well as glyceryl behenate (Compritol 888 ATO) [24] for topical application. No brain targeting NLC formulation have yet been developed using docosanol [24].
Oleic acid is the most widely utilized liquid lipid in the development of NLC formulations due to its great stability, easy availability, and nontoxic nature [25,26,27]. Brain-targeted SLN and NLC formulations have also been developed and reported with oleic acid [28].
The reticuloendothelial system (RE system) recognized NLC formulations as xenobiotics. Hence, RE system tends to eliminate the carrier system from blood as soon as possible. The surface coating of the NLC formulation with the hydrophilic material (e.g., PEG) , or with other material that is indigenous to the human body, like human serum albumin (HAS), the carrier systems can be protected from the RE system. The surface modification increases the chances of reaching the delivery systems to its target site before being eliminated by the RE system [29,30,31]. Moreover, the nanocarrier surface coating changes the way the particles interact with the biological membranes. An altered zeta potential or altered lipophilicity changes the affinity by which the particles bind to the membranes and moves through them.
In our current study, we investigated the development of zidovudine-loaded NLCs based on docosanol and oleic acid which were further surface-modified with PEG4000 and HAS for effective brain delivery of zidovudine . The brain targeting efficiency of the developed NLCs was investigated in rat model via intravenous administration.
2 Materials and Methods
2.1 Materials
AZT was gifted by Macleods Pharmaceuticals, Mumbai, India. Ethanol was purchased from Merck Millipore, Mumbai, India. 1-Docosanol (Behenyl alcohol) and Oleic acid were purchased from Tokyo Chemicals Industry Co., Ltd. Tokyo, Japan. Tween 80 and Polyethylene glycol 4000 (PEG4000) was purchased from Sisco Research Laboratories Pvt. Ltd., Mumbai, India. Human serum albumin (HAS) was purchased from Sigma-Aldrich Co., USA. Urethane, adult bovine serum, coumarin 6 (C6), and phosphate buffer saline, pH 7.4 were purchased from HiMedia, Mumbai, India. All other chemicals and reagents used were of analytical grade.
2.2 Preparation of Docosanol NLCs
The Docosanol NLC was prepared using previously reported ‘modified emulsion method’ with slight modifications [14, 32]. Briefly, 10 mg of docosanol, 7.5 mg of oleic acid, and 5 mg of AZT were dissolved in 2 mL of absolute ethanol in a beaker. This mixture was heated to 55 °C over a hot plate-cum-magnetic stirrer (IKA® RCT basic, IKA, Germany). In another beaker, 10 mL aqueous solution of 1% w/v Tween 80 was heated to 55 °C on a hot plate-cum-magnetic stirrer with continuous stirring at 500 rpm. The optimum amount of solid lipid, liquid lipid, drug, and surfactant was determined by trial formulations in different ratios of the excipients. The ethanol mixture was taken in a 2-mL syringe fitted with a 24-gauge needle and gradually injected into the stirring Tween 80 solution in the beaker. The mixture was stirred for 5 min at the same temperature before ultrasonication for 20 min in a bath sonicator (UCB 30, Spectra Lab, Navi Mumbai, India). The NLC formulation was then magnetically stirred until the smell of ethanol disappears indicating complete evaporation of the solvent.
To remove the unentrapped drug and excess amounts of surfactant from the formulation suspension, it was filtered through PD-10 Desalting Columns (GE Healthcare Bio-Sciences AB, Sweden) containing Sephadex™ G-25 resin . The eluent fractions containing the NLC formulations were then concentrated back to its initial volume using Vivaspin6® (Sartorius Stedim Biotech, Germany, MWCO 100). Formulations were finally kept in airtight polypropylene centrifuge tubes at 4–8 °C protected from light [4, 32].
2.3 Coating of Docosanol NLCs
Freshly prepared NLC formulation (SyLN) was separately coated with polyethylene glycol 4000 (PEG4000) and human serum albumin (HAS). The weighted amount of coating material was added to the NLC suspension to make 1% w/v solution of the coating material. The optimum concentration of the coating material was finalized by trial-and-error method based on particle size . This mixture was then stirred for 1 h on a magnetic stirrer at room temperature. The coated formulation was stored in polypropylene centrifuge tubes at 4–8 °C for future applications [30, 33].
2.4 Particle Size and Zeta Potential
A 1:100 dilution of newly formulated SyLN, SyLN-Peg, and SyLN-HSA in double-distilled water was used for the measurements. The average particle size and polydispersity index (PDI) of the formulations were measured by particle size analyzer (NanoBrook 90Plus, Brookhaven Instruments Corporation, New York; USA). The zeta potential of the formulations was measured by Zetasizer (Nano ZS90, Malvern, Worcestershire; UK). The particle size of the NLCs was measured at a 90° scattering angle using Dynamic Light Scattering. The zeta potential of the NLCs was measured by using laser Doppler micro-electrophoresis [34].
2.5 Entrapment Efficiency (EE) and Drug Loading
The entrapment efficiency (EE) was determined using the size exclusion chromatography. The amount of entrapped drug was determined by subtracting the amount of free drug from the total drug added during the formulation process [5, 35]. The EE was calculated based on the equation below:
To determine drug loading, 1 mL of the NLC formulation was lyophilized in a lyophilizer (SS1-LYO, Southern Scientific Lab Instruments, Chennai, India). The weight of the dried sample was determined from the tare weight of the vessel and the final weight of the vessel. To the dried formulation, 10 mL of ethanol was added and mixed well to a vortex mixture (Swirlex-Vortex Shaker, Abdos Labtech Private Limited, New Delhi, India). The mixture was then centrifuged at 13,000 rpm for 15 min. The amount of AZT was determined spectrophotometrically by measuring the absorbance of the clear supernatant at λ max of 265 nm. Each experiment was performed in triplicate. Placebo formulation treated like that of the sample was used as blank for UV absorbance [25, 36]. The percentage drug loading was calculated based on the equation below:
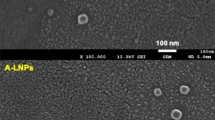
2.6 Transmission Electron Microscopy (TEM)
The shape and size of the uncoated and coated NLC formulations were studied using a transmission electron microscope (JEM-2100, 200 kV, Jeol Ltd., Tokyo, Japan). Each sample was diluted 100 times with deionized water and one drop was deposited on a carbon film-covered copper grid to form a thin-film specimen. The solvent was then evaporated by heating the grids in a hot-air oven at 45 °C. The sample was then examined and photographed under the microscope [37].
2.7 Compatibility Study of NLC Formulation
To determine any incompatibility between the components of the NLC formulation, differential scanning calorimetry (DSC), Fourier transform infrared spectroscopy (FT-IR) study, and powder X-ray diffraction (XRD) studies were performed. For that, NLC formulation was lyophilized with 5% mannitol in a lyophilizer. In all the studies, the spectrum of the individual components, the physical mixture of the components and the lyophilized formulation were obtained [27, 38].
For IR study, powder samples were analyzed by the FT-IR instrument (Bruker, ALPHA, Billerica, Massachusetts, USA) over a wave number region of 400–4000 cm−1 (wavelength of 2.5–25 μ) and spectra were recorded.
DSC study was done with a differential scanning calorimeter (PerkinElmer, DSC 4000, Waltham, Massachusetts, USA) using a closed aluminum crucible. Indium was used to calibrate the DSC apparatus. 5–10 mg of the sample powder was placed in the alumina crucible and heated from 30 to 445 °C with nitrogen flow at 50 mL/min at a heating rate of 10 °C/min and a thermogram was recorded [39].
The X-ray diffraction (XRD) patterns were analyzed using an X-ray diffractometer (D8 Focus, Bruker AXS, Germany.). Scanning for the powder samples was conducted over 2θ, ranging from 10° to 80°, at a voltage of 45 kV and a current of 40 mA [38].
2.8 Stability Study of NLC Formulation
To determine the stability of the formulated NLC in its aqueous suspension form, the uncoated, PEG4000 and HSA coated formulations were put in 1 mL Eppendorf tubes and stored at cold temperature (4–8 °C) and at room temperature for 6 months. A 100-μL sample was withdrawn at 1, 2, 3, and 6 months and analyzed for particle size and entrapment efficiency. After 6 months of study, zeta potential and in vitro drug release pattern of the samples were studied and compared with the initial data [40, 41].
2.9 In Vitro Drug Release Study
The in vitro drug release study was performed using dialysis tubes having a molecular weight cut-off 12,000 Da in artificial cerebrospinal fluid (aCSF). The aCSF was prepared by dissolving sodium chloride (8.66 g), potassium chloride (0.224 g), calcium chloride dihydrate (0.206 g), and magnesium chloride hexahydrate (0.163 g) in 500 mL of pyrogen-free, sterile water. NLC formulation containing a specific amount of encapsulated AZT was loaded into a dialysis bag and both the ends were tied with thread. The bag was then immersed in 100 mL of the dissolution medium (aCSF) kept in a beaker under continuous stirring (100 rpm) over a hot plate-cum-magnetic stirrer. The temperature of the medium was maintained at 37 °C. A 1-mL sample was withdrawn at time intervals of 1, 2, 4, 8, 24, and 48 h, which was replaced with 1 mL of fresh medium. The same study was conducted with AZT solution also. Samples were analyzed using a UV spectrophotometer at 266 nm against the blank medium [42].
The estimation of AZT in the samples collected from in vitro studies was performed by UV spectrophotometric method. An accurately weight amount of AZT was solubilized in artificial cerebrospinal fluid (aCSF) and adult bovine serum with saline (50% v/v) to obtain primary standards in the concentration range of 0.5–100 μg/mL. The calibration curve was obtained by measuring their absorbance at predetermined λ max of 266 nm with a UV–Vis spectrophotometer (UV 1800, Shimadzu, Japan). The concentration of AZT in test samples was calculated using the linear regression equation of the calibration curve in aCSF (Absorbance = 0.0071 + 0.3457 × Concentration, R 2 = 0.9999) and 50% v/v adult bovine serum with saline (Absorbance = 0.0001 + 0.9955 × Concentration, R 2 = 0.9997). The high value of correlation coefficient (R 2) indicates the linearity of the calibration curve and the curve did not deviate significantly from the origin as indicated by its very low value of intercept. The method was validated for accuracy and precision. When a standard drug solution was assayed repeatedly (n = 3), mean standard error (accuracy) and RSD (precision) were found to be 0.27% and 0.49%, respectively, in aCSF and 0.13% and 0.36%, respectively in 50% v/v adult bovine serum with saline. The purity of AZT in in vitro samples was validated recording UV spectrum using a UV–VIS Spectrophotometer. The spectrum was found comparable with the UV spectrum of pure AZT in the respective medium. The λ max of AZT was appeared at 266.27 nm in the UV spectrum of in vitro samples, which indicated the drug had not been deteriorated and there was no interference from the components of in vitro release medium.
To study the drug release behavior of the NLC formulations in blood serum, a 50% v/v mixture of adult bovine serum and saline was used as dissolution medium. NLC formulation containing a specific amount of encapsulated AZT was mixed with equal volume of the bovine serum–saline mixture and loaded into a dialysis bag. Both ends of the dialysis bag were tied with thread and then immersed into 100 mL of the above serum–saline mixture kept in a beaker and was stirred (100 rpm) continuously on a hot plate-cum-magnetic stirrer. The temperature of the medium was maintained at 37 °C. 100 μL of the sample was withdrawn at time intervals of 1, 2, 4, 8, and 24 h, which was replaced with fresh medium. The sample was mixed with 1 mL acetonitrile followed by centrifugation at 10,000 rpm for 10 min. The supernatant was collected. This process was repeated three times. Finally, collected acetonitrile was combined in an Eppendorf tube and was evaporated completely by heating it in a hot-air oven at 45 °C. Four milliliters of double distilled water was added to the dried residue and analyzed UV spectrophotometrically at 266 nm against blank formulation sample [5, 43].
The data obtained from serum stability study was fitted in different mathematical models of the kinetics of drug release to find the best fit depending on the regression analysis. The type of formulation (matrix or reservoir type) and the mechanism of drug release (diffusion controlled or erosion controlled) were determined from the observed mathematical models of the kinetics of drug release data [44, 45].
2.10 In Vitro Safety Evaluation of NLC Formulation
In vitro hemolysis: To test hemolysis, blood was drawn from the vein of the healthy human volunteer. The collected blood was put in an ice-cooled heparin tube and centrifuged (4000 rpm for 5 min) to separate the RBCs. After discarding the supernatant, the residue was resuspended in normal saline solution (pH 7.4). The washing steps were repeated three times and finally, RBCs were resuspended in phosphate-buffered saline, and volume was made up to 10 mL. The erythrocyte suspension (0.5 mL) was mixed with SyLn to obtain concentrations of 10, 100, and 500 μg/mL and the mixture was incubated at 37 °C for 1 h in a shaker under gentle agitation. After incubation, the reaction mixture was centrifuged at 4000 rpm for 5 min and the absorbance of the supernatant was read in a spectrophotometer at 540 nm. As a negative hemolysis control (0% hemolysis), erythrocytes were incubated in phosphate-buffered saline in the same condition as the samples. As a positive control to determine the value of 100% hemolysis, erythrocytes were incubated with distilled water, also in the same experimental condition. All the tests were performed in triplicate [46,47,48]. The percentage of hemolysis was calculated from the measured absorbance values by using Eq. (14.3):
2.11 In Vivo Pharmacokinetic and Brain Distribution Study
The animal study was approved by the Institutional Animal Ethical Committee (IAEC) of Dibrugarh University, Dibrugarh, Assam, India (Approval No. IAEC/DU/120 dated 18/02/2016). For the study, 60 healthy young adult male and female Wistar rats, nulliparous, nonpregnant and weighing 80–150 g were selected. Animals were acclimatized for 15 days before using them for the study. Rats were divided into four major groups (A, B, C, and D) each containing 15 rats. They were then again divided into five subgroups (1, 2, 4, 8, and 24 h) each containing three animals. Identification of the rats was done by putting marker pen marks on the tail. The animals of subgroups were kept in polypropylene cages (55 × 32.7 × 19 cm), bottom covered with paddy husk in an air and temperature controlled room (23 ± 2 °C). Rats were fed with laboratory animal food pellets (Oxbow Regal Rat Food, Rhinelander, Wisconsin, USA) with water ad libitum.
One hour before the experiment, animals were anesthetized by injecting urethane (1.2 g/kg B.W.) intraperitoneally. Group-A animals were injected with 5 mg/kg B.W. AZT solution in water for injection through the tail vein. Group-B animals were injected with SyLN, group-C received SyLN-Peg and group-D received SyLN-HSA with formulation amount equivalent to 5 mg/kg B.W. of AZT. Blood was collected from the hearts of the animals at predefined time intervals after dosing (1, 2, 4, 8, and 24 h.) and was kept in ice-cooled heparinized blood collection tubes. Rats were then sacrificed by cervical dislocation and the chest area was cut open. The brain of the rats was perfused by pumping 0.9% w/v sterile physiological saline solution through the common carotid artery to remove blood from the blood vessels of the brain [49, 50]. Perfusing the brains assures that no AZT is remained in the blood vessels of the brain as free drug or in the NLC formulation and the drug concentration in the brain shown by the analytical procedures is only the amount of AZT that has actually crossed the BBB . The rat brains were then collected by opening the cranium and kept in 15 mL centrifuge tubes after thorough wash of the brain with 0.9% w/v sterile physiological saline solution. Soon after collecting, blood samples were centrifuged at 5000 rpm for 15 min at 20 °C to separate plasma from blood cells. Separated plasma was collected in Eppendorf tubes and kept in −20 °C until further use. The brains were also kept in −20 °C until further use.
Brain Sample Preparation
Collected brains were homogenized with 10 mL deionized water in a tissue homogenizer and 100 μL of homogenate was taken in 2 mL Eppendorf tube. Tissue proteins were precipitated by mixing with 1 mL of acetonitrile followed by centrifugation at 13,000 rpm for 15 min. The supernatant was collected. This process was repeated thrice with the residue and the supernatants were finally combined and evaporated at 45 °C in a hot-air oven. It was reconstituted with 100 μL of HPLC mobile phase and 20 μL was injected into the column for the detection of AZT (𝜆max 265 nm).
Plasma Sample Preparation
Plasma samples were deproteinized by mixing 1 mL Acetonitrile with 100 μL of plasma sample followed by centrifugation at 13,000 rpm for 15 min. The supernatant was collected in a tube. This procedure was repeated thrice with the residue. The supernatants were combined and evaporated to dryness at 45 °C in a hot-air oven. It was reconstituted in 100 μL of HPLC mobile phase and 20 μL was injected into the HPLC column for the detection of the AZT (𝜆max 265 nm) [8].
2.12 Instruments and Chromatographic Conditions
An RP-HPLC system (Agilent Technologies, 1260 Infinity HPLC, California; USA) was used to quantify AZT in plasma and brain samples. The HPLC system was equipped with photodiode array detector set at 265 nm and Agilent Technologies mRP-C18 column (250 mm × 4.60 mm, ID; 5 μm particle size ) associated with guard column (50 mm × 4.60 mm, ID; 5 μm particle size). AZT was eluted by isocratic flow at a rate of 1 mL/min at ambient temperature, with a mobile phase comprising a mixture of aqueous Ortho-phosphoric acid solution (0.1% w/v) and Methanol at a ratio of 60:40.
Standard Solutions
The AZT was weighed and dissolved in HPLC mobile phase at room temperature to obtain a stock solution of 2.0 mg/mL. Serial dilutions of the stock solutions were made, and 20 μL was injected into the HPLC column to prepare the calibration standards. The calibration curve for AZT was prepared with seven concentrations : 500, 750, 1000, 2500, 5000, 10,000, and 100,000 ng/mL. Stock and working standard solutions were protected from light and stored at −20 °C until used [51].
Assay Validation
To validate the assay in rat plasma, the following parameters were investigated: selectivity, linearity, precision and accuracy, limit of quantification, limit of detection and recovery.
Selectivity
Selectivity indicates the lack of interfering peaks at the retention times of the assayed drug. The specificity of the method was determined by comparing the chromatograms obtained from the samples containing AZT with those obtained from blank plasma and brain samples.
Recovery and Linearity
In the analysis of AZT in rat plasma, the analytical recovery of AZT was determined at concentrations of 500, 2500, and 100,000 ng/mL (n = 3). Samples of the plasma and brain tissue without drug were spiked with known amounts of the drug to achieve the specified concentration. These samples were processed by the analytical method described above and peak areas were compared to that obtained by direct injection of the drug with the mobile phase, that is, the standard curve data. To calculate linearity, calibration curves were constructed by linear regression within the range of 500–100,000 ng/mL of AZT, using seven standard solutions.
The limit of quantification (LOQ) was determined as the lower value in the calibration curve. For the LOD, three samples at concentrations near to the smallest concentration of the standard curve (triplicate) were analyzed in order to obtain the standard deviations.
Precision and Accuracy
Precision was determined by the coefficient of variation (CV) and accuracy as the percent relative error (RE). Intraday precision and accuracy data were obtained by analyzing aliquots of plasma samples at low (500 ng/mL), medium (2500 ng/mL), and high (100,000 ng/mL) levels of the AZT concentration (n = 3). Inter-day reproducibility was determined over 3 days.
2.13 Pharmacokinetic Study
Pharmacokinetic analysis was carried out by using the Kinetica Professional software (Version 5.0; Copyright 2017; Adept Scientific, Manchester; UK). Two compartmental intravascular bolus dose analysis methods were employed for the pharmacokinetic parameter analysis.
2.14 The Drug-Targeting Index (DTI)
DTI is considered an important parameter for tissue targeting efficiency. It is basically a comparison between the tissue-targeting efficiency of the developed carrier system and the free drug solution. DTI gives an idea of the performance of the carrier system in delivering the drug to an organ in comparison to the free drug solution. The DTI to the brain can be calculated using the following formula [Eq. (14.4)]:
2.15 Rat Brain Localization and Accumulation of NLCs
In order to confirm and visualize that the intact NLCs had crossed the BBB and localized in the rat brain tissues, ex vivo imaging of rat brain cryosections were performed using the confocal laser scanning microscope (CLSM). Coumarin 6 (C6)-labeled docosanol NLCs (SyLN-C6) were prepared using the same method as described earlier in the section ‘Preparation of Docosanol NLCs’ with minor modification . C6 was first dissolved in absolute ethanol (1 mg/mL) added to the lipid–ethanol mixture and mixed well. The rest of the formulation process was unaltered. After labeled with C6, the physicochemical properties of SyLN NLCs did not show any significant change in particle size and zeta potential (data not reported). The SyLN-C6 NLCs were injected intravenously in healthy rats through tail vein (Fig. 14.8a). Then, rats were sacrificed by perfusion at 1, 2, 4, 8, and 24 h and brains were collected (Fig. 14.8b), washed thoroughly with PBS and were stored at −80 °C until further processing. The brain tissues were sliced into sections (6–10 μm in thickness) using a Shandon Cryotome E (Thermo Electron Corporation, USA) and further stained with DAPI (1 μg/mL) for 2 min, washed three times with PBS pH 7.4. The stained tissues were mounted on microscopy slides before analysis by CLSM. The brain tissues were imaged under a confocal laser scanning microscope (TCS SP8, Leica, Germany) using the wavelengths for DAPI (Ex./Em. = 358/461 nm) and C6 (Ex./Em. = 465/505 nm). The images obtained from excitation with both the wavelengths were finally merged using the microscope software [52, 53].
2.16 Statistical Analysis
All pharmacokinetic parameters of AZT solution and NLC formulations were expressed as the mean ± standard deviation (SD). The data were analyzed with Graph Pad Prism (Version 5.03, Copyright 2017, GraphPad Software, Inc.; USA). One-way ANOVA study was done to determine the significant difference between the formulations and AZT solution. The significance of the difference between AZT solution and NLC formulation data was determined with Student’s t-test. A statistical difference p > 0.05 was considered significant.
3 Results and Discussion
3.1 Particle Size and Zeta Potential
The particle size of the optimized NLCs was found to be 54.5 ± 1.3 nm with a PDI of 0.287. The particle size of the PEG4000 and HSA coated formulations were 57.8 ± 2.2 nm (PDI 0.293) and 59.6 ± 1.7 nm (PDI 0.295), respectively. The developed NLCs, both uncoated and coated, were small enough to cross the BBB . Previous literature shows that nanocarriers having a particle size below 100 nm cross the BBB and get into the brain very easily [54]. The uncoated and coated Docosanol NLCs had a small PDI value indicating that the particles are very close to monodispersity, that is, the particle size variation is very small. The reports of the particle size analysis of SyLN, SyLN-Peg, and SyLN-HSA have been given in Fig. 14.1b. The increase in particle size of coated NLCs indicated that the coating materials had been deposited on the surface of the NLC particles.
Characterization of Docosanol NLCs : (a) Coating of Docosanol NLC with PEG4000/HSA. Freshly prepared Docosanol NLCs were coated with 1%w/v solution of PEG4000 and HSA for 1 h at room temperature by continuous stirring. The coating changes the particle size and zeta potentials of the NLCs confirming that the coating was successful; (b) Size distribution of SyLN from DLS measurement. The uncoated formulation shows the nanometric dimension of 54.5 nm with low PDI of 0.287. Coating with PEG4000 and HSA slightly increases the particle size (57.5 nm and 59.6 nm, respectively); (c) Zeta potential of SyLN from Zetasizer. The uncoated NLC formulation has a Zeta potential of −21.6 mV. Coating the NLC with PEG4000 and HSA makes the particles more electronegative (−26 mV and −38.5 mV, respectively)
The zeta potential of the optimized SyLN formulation was found to be −21.6 ± 0.2 mV (Fig. 14.1c). Coating increased the zeta potential by a great margin. The particle size and Zeta potential of SyLN, SyLN-Peg, and SyLN-HSA have been given in Table 14.1. The difference between the zeta potentials of SyLN, SyLN-Peg, and SyLN-HAS was statistically significant (t-test, p > 0.05).
The coating of NLCs involves the physical adsorption of coating materials on NLC surface. The coating might have taken place due to the charge differences between the NLC surface and the coating material. As zeta potential suggests in Table 14.1, the surface of the NLC formulation was negative in nature (i.e., anionic). The freshly prepared NLC formulations have an acidic pH due to the presence of Tween 80 in the medium (the pH of 1% w/v Tween 80 solution is approximately 5.5). Hence, the amine group of HSA ionizes and gives positive ions. These positive ions have a great affinity to interact with the negative ions of the hydroxyl group of Tween 80, present on the surfaces of NLC particles. This interaction of positive and negative ions leads to the coating of the NLC surface [7]. The carboxylic acid group present in the structure of HSA makes the coated NLCs more negative (zeta potential = −38.5). The coating process has been discussed schematically in Fig. 14.1a. The hydroxyl groups present in the chemical structures of the PEG4000 remain unionized in the acidic medium of the freshly prepared NLCs. PEG4000 has a higher viscosity, which facilitates it to forms a flexible layer on the surface of NLCs leading to the formation of the coating and make them more negative (zeta potential = −26).
The hydrophilic coating on the surface of the NLCs would prevent the adsorption of opsonins via steric hindrance and their subsequent uptake by phagocytic cells [55, 56]. Hence, the surface modified NLCs would remain in the blood for a longer duration of time as compared to an uncoated formulation which may or may not increase the targeting efficacy of the formulation as several reports point out that PEGylation may negatively influence the performance of nanocarriers as a drug carrier [57].
3.2 EE and Drug Loading
The EE and drug loading of AZT in SyLN were found to be 84.4 ± 0.56% and 11.32%, respectively. Higher EE signifies that most of the drug added in the formulation process has entrapped and hence the loss of valuable API is very less. The removal of ingredients that are used in excess quantities to ease the formulation process by gel filtration, like surfactant (Tween 80), led to a higher drug loading.
3.3 Transmission Electron Microscopy (TEM)
The transmission electron microscopy image as shown in Fig. 14.2(I) reveals that the NLC particles are spherical in shape. In the TEM images of SyLN-Peg and SyLN-HSA, a shell-like structure can be seen over the surface of the lipid core. This confirms the coating of the NLC formulations. On higher magnifications, droplet-like spherical structures can be seen inside the NLC particles. These droplets are of the liquid lipid entrapped inside the solid lipid matrix. On further magnification, some patches of nonhomogeneous amorphous substances could be seen inside those droplets. These patches can be of the entrapped AZT inside the liquid lipid droplets. The internal structures of SyLN have been visualized with the help of highly magnified TEM images in Fig. 14.2 (II).
(I) TEM micrographs of (A) SyLN, (B) SyLN-Peg, (C) SyLN-HSA. An increased particle size of the coated particles and a shell-like structure on the surface of the NLC particles confirms the coating of the particles. Scale Bar: 100 nm (A, C) and 200 nm (B); (II) TEM images of SyLN in higher magnifications. The higher magnifications of NLCs show that the solid lipid cores contain droplets of liquid lipids containing amorphous AZT entrapped in them. Scale Bar: 0.2 μm (D), 50 nm (E) and 10 nm (F)
3.4 Compatibility Study of NLC Formulation
The IR spectra of AZT, lyophilized SyLN, and the physical mixture were compared (Fig. 14.3a). The spectra of the formulation and the physical mixture have the same major peak. No additional peak appeared in the IR spectrum of the formulation or the physical mixture. This explains that all the components are compatible, as if there was any incompatibility, some additional peaks might have appeared. The interpretation of peaks appearing in the spectra is given in Table 14.2.
Compatibility studies of NLC formulation: (a) FT-IR spectra of AZT, NLC formulation and physical mixture of AZT with the NLC formulation components. The spectrum of physicalFig. 14.3 (continued) mixture and the NLC formulation shows the same peaks. Peaks of AZT are present in the spectra of NLC formulation and physical mixture. This indicates that AZT has not undergone any chemical modification during formulation process and is compatible with other components of the NLC formulation; (b) DSC thermograms of AZT, NLC formulation and physical mixture of AZT with the NLC formulation components. The thermograms of physical mixture and the NLC formulation show same endothermic peaks at 60, 72, 102 and 345 °C. The peak of AZT at 102 °C is clearly visible in both thermograms. Flattening of the peaks in the NLC formulation thermogram as compared to the physical mixture means that the drug becomes amorphous in the NLC formulation; (c) XRD spectra of AZT, NLC formulation and physical mixture of AZT with the NLC formulation components. The spectra of physical mixture and the NLC formulation show same peaks except one. The missing peak in NLC formulation spectrum is of AZT, indicating AZT was converted to amorphous form during the formulation process
On comparing the DSC thermograms of AZT, lyophilized SyLN, and the physical mixture (Fig. 14.3b) it was observed that thermograms of lyophilized SyLN and its physical mixture contain the same endothermic peaks. The peak for AZT was clearly visible in both thermograms. The absence of any unusual peak in the thermograms shows that the components don’t react to each other [58].
On comparing the powder X-ray diffractograms of AZT, lyophilized SyLN and the physical mixture (Fig. 14.3c), it was observed that the peak of AZT was absent in the diffractogram of lyophilized SyLN, though it was clearly visible in the diffractogram of the physical mixture. This confirms that AZT might have undergone a state change, from crystalline to amorphous [38], but no new substance has developed during the formulation process of NLCs.
All the above study results confirm that there is no incompatibility between the excipients used in the NLC formulation [59].
3.5 Stability Study of NLC Formulation
The NLC samples kept at 4–8 °C showed no significant change in the particle size , zeta potential, %EE of all the formulations even after 6 months of stability study. However, for the NLC samples kept at room temperature, particle size starts increasing from the very first month and goes on increasing until the end of the study. Entrapment efficiency reduced with time indicating that the formulation was losing the entrapped drug on standing at room temperature. In vitro release studies of stability samples after 6 months of storage shows that the drug release pattern of the NLC samples kept at 4–8 °C remains almost same as the freshly prepared NLCs. The NLC samples kept at room temperature released its drug content much faster than initial. The detailed observation of particle size, %EE and Zeta potential for stability samples has been presented in Table 14.3.
3.6 In Vitro Drug Release Study
The in vitro drug release study of the developed NLCs in aCSF showed slow release profile of AZT. The percentage of drug released from the different NLC formulations (SyLN, SyLN-Peg, and SyLN-HSA) was between 10.18% and 10.57% at 48 h (Fig. 14.4A). The release of free drug through the dialysis membrane was rapid and nearly 84.88% at 48 h. The observed drug release profile of the docosanol NLCs is significantly different from the previously reported lipid nanocarriers with different drugs (AZT loaded NLC has not been reported yet). The previous studies reported that more than 80% of the entrapped drug get released in vitro within 24 h [37, 38, 60, 61]. In our study, TEM images of SyLN (Fig. 14.2 (II)) confirm that AZT was evenly internalized in the liquid lipid core, which was further entrapped within the solid lipid matrix of NLCs and showed very slow drug release in vitro. Thus, the developed docosanol NLCs in the present study showed better sustained release profile of AZT. However, this does not confirm that the developed nanocarriers would equally perform in vivo, as the environment in vivo is different from in vitro. The different lipolytic enzymes may breakdown the NLCs as soon as it reaches the blood stream making the carrier system short living. To determine how the docosanol NLCs may performs in vivo, stability and drug release properties of the formulations were studied ex vivo in bovine serum saline.
In vitro drug release study of SyLN, SyLN-Peg, and SyLN-HSA in (A) aCSF (b–d). As compared to the AZT solution (a), the drug release from the NLC formulations is very less even after 48 h of study. This shows the sustained release properties of the NLC formulations. The coating does not alter the in vitro drug release properties of the NLC formulation to a great extent; (B) 50% v/v adult bovine serum with the saline medium (e–g). Both coated and uncoated formulations show similar drug release properties. Though most of the entrapped drugs are released within 24 h from the formulations, some drugs are remained to be released. This shows that the formulation is stable in blood serum for more than 24 h and can release drug for an extended period of time
The data obtained from the drug release study with the 50% v/v mixture of bovine serum and saline solution shows that a great amount of drug (83.79%) was released within 24 h from the SyLN formulation. SyLN-Peg and SyLN-HSA show similar types of release properties in this medium (Fig. 14.4B). These drug release data were fit in different mathematical models of the kinetics of drug release (Fig. 14.5). The mathematical models of the kinetics of drug release with the highest R 2 value were the best-fitted model. The R 2 values of all the formulations have been shown in Table 14.4.
Fitting the drug release data of SyNL in adult bovine serum in the mathematical models of the kinetics of drug release. The respective R 2 of all the models are being shown in the graphs. Data show that the formulation is best fitted in zero order and Korsmeyer–Peppas models. Similarly, the kinetic analysis of drug release data of SyLN-Peg and SyLN-HAS (Figure not shown) confirm that the coated NLCs are also best fitted in Zero order and Korsmeyer–Peppas models
R 2 values show that all the formulations are best fitted to zero-order and Korsmeyer–Peppas model. Fitting to zero-order model indicates that the formulations are of matrix type in nature, that is, the drug is evenly distributed in the lipid core. When the data is well fitted to Korsmeyer–Peppas model and the ‘n’ value is >0.89, the drug release follows the super case II transport and drug release is erosion-controlled [45]. In our study, the observed “n” value is much higher than 0.89 (Table 14.4), indicating AZT release from NLCs is based on erosion of the lipid matrix in blood serum.
3.7 In Vitro Safety Evaluation of NLC Formulation
Assessment of the hemolytic potential against a suspension of erythrocytes illustrated the security of the NLC formulation in vivo. The hemolysis of erythrocytes of NLC formulation having a concentration of 500 μg/mL was 3.98% after incubating at 37 °C for 1 h. The small hemolytic effect of SyLN in such a higher concentration suggested that the formulation was safe for intravenous administration.
3.8 In Vivo Pharmacokinetic and Brain Distribution Study
The reversed-phase HPLC-UV method described, validated, and used for AZT quantification, provides great sensitivity and specificity, and high sample throughput required for pharmacokinetic studies. The chromatograms showed a good baseline separation and the mobile phase used resulted in optimal separation. The method was selective for AZT since it shows that no interfering peaks appeared near the retention time of the compound of interest (Fig. 14.6, I–III) The LOQ and LOD values were low, indicating the good sensitivity of this HPLC method.
(I) HPLC chromatogram of an aqueous solution of AZT. The chromatogram shows a single peak without any interfering peaks; (II) HPLC chromatograms demonstrating selectivity with plasma samples (A) Blank rat plasma; (B) Rat plasma spiked with AZT (2000 ng/mL); (III) HPLC Chromatograms demonstrating selectivity with rat brain samples (A) Blank rat brain; (B) Rat brain spiked with AZT (2000 ng/mL)
The precision of the applied analytical method was very accurate. The observed value of precision for different concentrations ranged from 0.09 to 0.95%. The coefficient of variation did not exceed 15% in the analyses. Accuracy and recovery were also in good agreement with acceptable values for the validation of an analytical procedure (i.e., 100 ± 20%). The observed accuracy value varied from 100.29 to 102.52%. The accuracy of intra and inter day analysis varied between 100.29–103.77% and 100.30–105.23%, respectively. The precision of intra and inter day analysis varied between 0.07–1.31% and 0.07–0.55%, respectively.
The sample preparation used in this study involved only a single step (i.e., deproteinization with acetonitrile). This condition was optimal for sample preparation as it resulted in clean chromatograms.
The mean plasma concentration -time profiles of the AZT solution, SyLN, SyLN-Peg, and SyLN-HSA are presented in Fig. 14.7b. Pharmacokinetic parameters of AZT solution, SyLN, SyLN-Peg, and SyLN-HSA were determined using two-compartmental analysis, and the data are presented in Table 14.5. As shown at all points in Fig. 14.7b, the AZT plasma concentration was higher in rats administered with SyLN-Peg and SyLN-HSA than those administered with AZT solution and SyLN (p < 0.05) except the first sampling point. There was no difference in 𝑇max of AZT when it was given as NLC formulation. The AUC0−𝑡 and AUC0−∞ value of SyLN-HSA have been found to be 1.73 and 1.61 times higher than AZT solution (p < 0.05), respectively. But AUC0−𝑡 and AUC0−∞ values of SyLN and SyLN-Peg was lesser than that of AZT solution. The half-life of AZT in plasma was decreased with the NLC formulations (p < 0.05). Compared with AZT solution, the mean resident time (MRT) was also shortened with NLC formulations (p < 0.001). These observations indicated that the AZT is more rapidly removed from the plasma compartment when incorporated in NLC formulations. This may happen in two ways (viz., rapid elimination of AZT loaded NLCs from blood through the excretory routes, or a rapid tissue distribution to the peripheral compartments). In both cases the concentration of AZT in plasma reduces rapidly [62].
(a) Brain pharmacokinetic profile of AZT solution, SyLN, SyLN-Peg, and SyLN-HSA. Uncoated AZT loaded docosanol NLCs (SyLN) increases the brain AZT concentration significantly (p > 0.05). Coating the NLC decreases the brain delivering efficiency of the NLC formulation; (b) Plasma pharmacokinetic profile of AZT solution, SyLN, SyLN-Peg, and SyLN-HSA. SyLN-HSA shows similar plasma concentration–time profile as AZT solution after intravenous injection and attains C max after 1 h of I.V. injection. SyLN and SyLN-Peg attain C max after 2 h of administration
The mean concentration versus time profile of AZT solution, SyLN, SyLN-Peg, and SyLN-HSA in the brain have been presented in Fig. 14.7a. The pharmacokinetic parameters of AZT solution, SyLN, SyLN-Peg, and SyLN-HSA in the brain were determined using two-compartmental analysis and the pharmacokinetic parameters are tabulated in Table 14.6. Some previous studies have shown that AZT enters the brain when administered in solution form [8]. However, in our study, no AZT was detected in the rat brain with intravenous AZT solution in water. This may be due to various reasons like the difference in route of administration, the dose of AZT administered, improper or no brain perfusion, animal’s physiological conditions, and application of the different analytical method [63, 64]. In previous studies, the oral AZT solution was administered in rat at 10 mg/kg B.W. The brain was not perfused to remove any traces of AZT from the brain blood vessels . These may be the reasons for detection of AZT in the brain samples [8]. In our study, intravenous AZT solution was administered at 5 mg/kg B.W of rat and the brain was harvested after complete perfusion by pumping 0.9% w/v sterile physiological saline solution through the common carotid artery to remove blood with any traces of AZT from the blood vessels of the brain. The C max for SyLN and SyLN-Peg in collected brain tissue appeared to be 8 h after injection in rats, which is 4 h for SyLN-HSA. Both SyLN and SyLN-Peg enter the brain very rapidly and maintains a constant concentration of AZT in the brain for the entire duration of treatment (Table 14.6). SyLN shows a tendency of decreasing AZT concentration after 24 h. However, for SyLN-Peg, the concentration is almost constant. SyLN-HSA does not enter brain immediately after injection. It enters brain after 2 h of injection and is eliminated from brain very rapidly, as no AZT was detected after 8 h of treatment in the brain. Reduced brain permeability of PEG4000 coated NLC formulation as compared to uncoated formulation may be due to its increased particle size (57.5 ± 2.2 nm) or more negative zeta potential (−26 ± 0.7 mV). The same thing has also happened for the HSA coated formulation. HSA coating increases the particle size (59.6 ± 1.7 nm) and makes the particles drastically more electronegative in nature (−38.5 ± 0.9 mV). It is well known that physiological membranes like BBB are electronegative in nature. Hence, the more electronegative NLCs are repulsed by the BBB [64, 65]. Therefore, more electronegative PEG4000 and HSA coated NLC formulations are poorly permeated through the BBB into rat brain.
Lower plasma concentration of AZT for NLC formulation as compared to AZT solution can be explained using the brain AZT concentration data. The NLC formulations are indeed rapidly distributed to the peripheral tissues including brain, ultimately reducing the AZT plasma concentration. The pharmacokinetic parameters for SyLN, SyLN-Peg, and SyLN-HSA in the brain have been shown in Table 14.6. The C max for SyLN is higher as compared to the other two coated formulations. AUC value clearly shows that the SyLN is the best among all the formulations in delivering AZT to the brain for a prolonged duration of time.
3.9 The Drug-Targeting Index (DTI)
For SyLN, SyLN-Peg , and SyLN-HSA, the calculated value for brain DTI is “α” (infinity) as the free drug solution was unable to deliver AZT to the brain. Hence the denominator of the Eq. 14.4 becomes zero and making the result of the calculation a “α.” This shows that the NLC formulations are much better in delivering AZT to the brain than the free drug solution.
3.10 Rat Brain Localization and Accumulation of NLCs
For a clear assessment of the trafficking and accumulation of NLCs in rat brain in vivo, we took advantage of the CLSM imaging of brain tissues (brain cryosections) from a qualitative point of view after intravenous administration of fluorescent -labeled NLCs. C6, a green fluorescent marker, was incorporated in SyLN NLCs to detect their biodistribution in vivo in rat brain. SyLN-C6 NLCs did not show any significant changes in the physicochemical properties as compared to SyLN NLCs. The selection of SyLN NLCs in brain localization and accumulation study was based on its satisfactory brain pharmacokinetics as shown in Table 14.6. The intravenous injection of SyLN-C6 resulted in a significant increase of SyLN NLCs in the rat brain at each time point. At 1 h post injection, SyLN NLCs were widely distributed in the rat brain (Fig. 14.8c F-2). The quantity of SyLN NLCs in the brain increased as time progressed and maximum brain localization of NLCs was observed at 4 h (Fig. 14.8c H-2). The intensity of fluorescence signals in the brain decreased as the time progressed past 4 h. Moreover, fluorescence signals were still detected in the brain at 24 h post injection (Fig. 14.8c J-2). As shown in the images (Fig. 14.8c, first column), the brain tissues/cells are readily identified by nuclei staining (DAPI, blue color) and the cells in the brain tissues were of less density because of their slow proliferation rate in the normal healthy rat brain. The merged images (Fig. 14.8c, third column) showed that SyLN NLCs were accumulated in the brain tissues and likely internalized into the cells including nucleus. Combining these results, the SyLN NLCs could cross the BBB , accumulated in brain tissues giving controlled delivery of AZT until 24 h.
Brain delivery of docosanol NLCs in rat model. (a) Wistar albino rat treated with intravenous SyLn-C6 NLCs through tail vein; (b) Rat brain collected at 1, 2, 4, 8, and 24 h; (c) CLSM images of brain cryosections labeled with DAPI (blue), SyLn-C6 NLCs (green) at 1, 2, 4, 8, and 24 h. Scale Bar: 100 μm
4 Conclusion
The docosanol NLCs were successfully developed by modified emulsion method for effective brain delivery of AZT. The developed NLCs were the best stable in refrigerated condition, in blood serum and safe for intravenous administration. The NLCs showed sustained release profile of AZT in aCSF and in vivo in rat brain. The in vivo plasma and brain pharmacokinetic investigation in rat model revealed that SyLN and SyLN-Peg NLCs rapidly reached the brain and yielded higher MRT, C max, and AUC in rat brain compared to those data with AZT solution. The free drug solution was unable to deliver AZT to the brain. The rat brain pharmacokinetic data and CLSM imaging of rat brain cryosections confirm that the developed NLCs had effectively crossed the BBB delivering AZT in a sustained manner for a prolonged period of time and the SyLN is the best among all the formulations investigated in delivering AZT to the brain. This may provide an effective therapeutic strategy to combat the challenges of HIV infection in the brain. Further, preclinical and clinical development studies are warranted.
Change history
07 May 2019
This book was inadvertently published with incorrect affiliation of the authors Lopamudra Dutta and Biswajit Mukherjee in Chapter 14 and it should be Department of Pharmaceutical Technology, Jadavpur University, Kolkata, West Bengal, India
References
Koyuncu, O. O., Hogue, I. B., & Enquist, L. W. (2013). Virus infections in the nervous system. Cell Host and Microbe, 13, 379–393. https://doi.org/10.1016/j.chom.2013.03.010.
Schnell, G., Joseph, S., Spudich, S., Price, R. W., & Swanstrom, R. (2011). HIV-1 replication in the central nervous system occurs in two distinct cell types. PLoS Pathogens, 7, e1002286. https://doi.org/10.1371/journal.ppat.1002286.
Klecker, R. W., Collins, J. M., Yarchoan, R., Thomas, R., Jenkins, J. F., Broder, S., et al. (1987). Plasma and cerebrospinal fluid pharmacokinetics of 3′-azido-3′-deoxythymidine: A novel pyrimidine analog with potential application for the treatment of patients with AIDS and related diseases. Clinical Pharmacology and Therapeutics, 41, 407–412.
Fan, H., Liu, G., Huang, Y., Li, Y., & Xia, Q. (2014). Development of a nanostructured lipid carrier formulation for increasing photo-stability and water solubility of phenylethyl resorcinol. Applied Surface Science, 288, 193–200. https://doi.org/10.1016/j.apsusc.2013.10.006.
Lim, W. M., Rajinikanth, P. S., Mallikarjun, C., & Kang, Y. B. (2014). Formulation and delivery of itraconazole to the brain using a nanolipid carrier system. International Journal of Nanomedicine, 9, 2117–2126. https://doi.org/10.2147/IJN.S57565.
De Clercq, E. (2010). Antiretroviral drugs. Current Opinion in Pharmacology, 10, 507–515. https://doi.org/10.1016/j.coph.2010.04.011.
Kuo, Y.-C., & Chung, J.-F. (2011). Physicochemical properties of nevirapine-loaded solid lipid nanoparticles and nanostructured lipid carriers. Colloids and Surfaces. B, Biointerfaces, 83, 299–306. https://doi.org/10.1016/j.colsurfb.2010.11.037.
Purvin, S., Vuddanda, P. R., Singh, S. K., Jain, A., & Singh, S. (2014). Pharmacokinetic and tissue distribution study of solid lipid nanoparticles of zidovudine in rats. Journal of Nanotechnology, 2014, 1–7. https://doi.org/10.1155/2014/854018.
Singh, S., Dobhal, A. K., Jain, A., Pandit, J. K., & Chakraborty, S. (2010). Formulation and evaluation of solid lipid nanoparticles of a water soluble drug: Zidovudine. Chemical and Pharmaceutical Bulletin (Tokyo), 58, 650–655.
Uronnachi, E. M., Ogbonna, J. D., Kenechukwu, F. C., Chime, S. A., Attama, A. A., & Okore, V. C. (2014). Formulation and release characteristics of zidovudine-loaded solidified lipid microparticles. Tropical Journal of Pharmaceutical Research, 13, 199–199. https://doi.org/10.4314/tjpr.v13i2.5.
Deepak Sunil, B., Rajendra, D., & Narendra, D. (2010). Liposomal drug delivery system for zidovudine: Design and characterization. International Journal of Drug Development and Research, 2, 8–14.
Shibata, A., McMullen, E., Pham, A., Belshan, M., Sanford, B., Zhou, Y., et al. (2013). Polymeric nanoparticles containing combination antiretroviral drugs for HIV type 1 treatment. AIDS Research and Human Retroviruses, 29, 746–754. https://doi.org/10.1089/aid.2012.0301.
Das, S., Ng, W. K., & Tan, R. B. H. (2012). Are nanostructured lipid carriers (NLCs) better than solid lipid nanoparticles (SLNs): Development, characterizations and comparative evaluations of clotrimazole-loaded SLNs and NLCs? European Journal of Pharmaceutical Sciences, 47, 139–151. https://doi.org/10.1016/j.ejps.2012.05.010.
Doktorovová, S., Araújo, J., Garcia, M. L., Rakovský, E., & Souto, E. B. (2010). Formulating fluticasone propionate in novel PEG-containing nanostructured lipid carriers (PEG-NLC). Colloids and Surfaces. B, Biointerfaces, 75, 538–542. https://doi.org/10.1016/j.colsurfb.2009.09.033.
Joshy, K. S., & Sharma, C. P. (2012). Blood compatible nanostructured lipid carriers for the enhanced delivery of azidothymidine to brain. Journal of Computational and Theoretical Nanoscience, 6(1), 47–55.
Marcelletti, J. F. (2002). Synergistic inhibition of herpesvirus replication by docosanol and antiviral nucleoside analogs. Antiviral Research, 56, 153–166.
Nanjwade, B. K., Kadam, V. T., & Manvi, F. V. (2013). Formulation and characterization of nanostructured lipid carrier of ubiquinone (Coenzyme Q10). Journal of Biomedical Nanotechnology, 9, 450–460.
Pope, L. E., Marcelletti, J. F., Katz, L. R., Lin, J. Y., Katz, D. H., Parish, M. L., et al. (1998). The anti-herpes simplex virus activity of n-docosanol includes inhibition of the viral entry process. Antiviral Research, 40, 85–94. https://doi.org/10.1016/S0166-3542(98)00048-5.
Souto, E. B., Mehnert, W., & Muller, R. H. (2006). Polymorphic behaviour of Compritol888 ATO as bulk lipid and as SLN and NLC. Journal of Microencapsulation, 23, 417–433. https://doi.org/10.1080/02652040600612439.
Pope, L. E., Marcelletti, J. F., Katz, L. R., & Katz, D. H. (1996). Anti-herpes simplex virus activity of n-docosanol correlates with intracellular metabolic conversion of the drug. Journal of Lipid Research, 37, 2167–2178.
TOXNET: 1-DOCOSANOL [WWW Document]. (n.d.). Retrieved October 19, 2017, from http://toxnet.nlm.nih.gov/cgi-bin/sis/search2/r?dbs+hsdb:@term+@DOCNO+5739
Iglesias, G., Hlywka, J. J., Berg, J. E., Khalil, M. H., Pope, L. E., & Tamarkin, D. (2002a). The toxicity of behenyl alcohol: I. Genotoxicity and subchronic toxicity in rats and dogs. Regulatory Toxicology and Pharmacology, 36, 69–79. https://doi.org/10.1006/rtph.2002.1566.
Iglesias, G., Hlywka, J. J., Berg, J. E., Khalil, M. H., Pope, L. E., & Tamarkin, D. (2002b). The toxicity of behenyl alcohol: II. Reproduction studies in rats and rabbits. Regulatory Toxicology and Pharmacology, 36, 80–85. https://doi.org/10.1006/rtph.2002.1566.
Aburahma, M. H., & Badr-Eldin, S. M. (2014). Compritol 888 ATO: A multifunctional lipid excipient in drug delivery systems and nanopharmaceuticals. Expert Opinion on Drug Delivery, 11, 1865–1883. https://doi.org/10.1517/17425247.2014.935335.
Chinsriwongkul, A., Chareanputtakhun, P., Ngawhirunpat, T., Rojanarata, T., Sila-on, W., Ruktanonchai, U., et al. (2012). Nanostructured lipid carriers (NLC) for parenteral delivery of an anticancer drug. AAPS PharmSciTech, 13, 150–158. https://doi.org/10.1208/s12249-011-9733-8.
Gönüllü, Ü., Üner, M., Yener, G., Karaman, E. F., & Aydoğmuş, Z. (2015). Formulation and characterization of solid lipid nanoparticles, nanostructured lipid carriers and nanoemulsion of lornoxicam for transdermal delivery. Acta Pharmaceutica, 65, 1–13. https://doi.org/10.1515/acph-2015-0009.
Patel, D., Dasgupta, S., Dey, S., Ramani, Y. R., Ray, S., & Mazumder, B. (2012). Nanostructured lipid carriers (NLC)-based gel for the topical delivery of aceclofenac: Preparation, characterization, and in vivo evaluation. Scientia Pharmaceutica, 80, 749–764. https://doi.org/10.3797/scipharm.1202-12.
Azhar Shekoufeh Bahari, L., & Hamishehkar, H. (2016). The impact of variables on particle size of solid lipid nanoparticles and nanostructured lipid carriers; a comparative literature review. Advanced Pharmaceutical Bulletin, 6, 143–151. https://doi.org/10.15171/apb.2016.021.
Shaji, J., & Jain, V. (2010). Solid lipid nanoparticles: A novel carrier for chemotherapy. International Journal of Pharmacy and Pharmaceutical Sciences, 2, 8–17.
Uner, M., & Yener, G. (2007). Importance of solid lipid nanoparticles (SLN) in various administration routes and future perspectives. International Journal of Nanomedicine, 2, 289–300.
Wang, L., Luo, Q., Lin, T., Li, R., Zhu, T., Zhou, K., et al. (2015). PEGylated nanostructured lipid carriers (PEG-NLC) as a novel drug delivery system for biochanin A. Drug Development and Industrial Pharmacy, 41, 1204–1212. https://doi.org/10.3109/03639045.2014.938082.
Tamjidi, F., Shahedi, M., Varshosaz, J., & Nasirpour, A. (2014). Design and characterization of astaxanthin-loaded nanostructured lipid carriers. Innovative Food Science and Emerging Technologies, 26, 366–374. https://doi.org/10.1016/j.ifset.2014.06.012.
Kashanian, S., & Rostami, E. (2014). PEG-stearate coated solid lipid nanoparticles as levothyroxine carriers for oral administration. Journal of Nanoparticle Research, 16, 2293. https://doi.org/10.1007/s11051-014-2293-6.
Tsai, M. J., Wu, P. C., Huang, Y. B., Chang, J. S., Lin, C. L., Tsai, Y. H., et al. (2012). Baicalein loaded in tocol nanostructured lipid carriers (tocol NLCs) for enhanced stability and brain targeting. International Journal of Pharmaceutics, 423, 461–470. https://doi.org/10.1016/j.ijpharm.2011.12.009.
Pardeike, J., Weber, S., Haber, T., Wagner, J., Zarfl, H. P., Plank, H., et al. (2011). Development of an Itraconazole-loaded nanostructured lipid carrier (NLC) formulation for pulmonary application. International Journal of Pharmaceutics, 419, 329–338. https://doi.org/10.1016/j.ijpharm.2011.07.040.
Yuan, H., Wang, L.-L., Du, Y.-Z., You, J., Hu, F.-Q., & Zeng, S. (2007). Preparation and characteristics of nanostructured lipid carriers for control-releasing progesterone by melt-emulsification. Colloids and Surfaces. B, Biointerfaces, 60, 174–179. https://doi.org/10.1016/j.colsurfb.2007.06.011.
Thatipamula, R., Palem, C., Gannu, R., Mudragada, S., & Yamsani, M. (2011). Formulation and in vitro characterization of domperidone loaded solid lipid nanoparticles and nanostructured lipid carriers. Daru, 19, 23–32.
Gaba, B., Fazil, M., Khan, S., Ali, A., Baboota, S., & Ali, J. (2015). Nanostructured lipid carrier system for topical delivery of terbinafine hydrochloride. Bulletin of Faculty of Pharmacy, Cairo University, 53, 147–159. https://doi.org/10.1016/j.bfopcu.2015.10.001.
Tita, B., Ledeti, I., Bandur, G., & Tita, D. (2014). Compatibility study between indomethacin and excipients in their physical mixtures. Journal of Thermal Analysis and Calorimetry, 118, 1293–1304. https://doi.org/10.1007/s10973-014-3986-x.
Gartziandia, O., Egusquiaguirre, S. P., Bianco, J., Pedraz, J. L., Igartua, M., Hernandez, R. M., et al. (2016). Nanoparticle transport across in vitro olfactory cell monolayers. International Journal of Pharmaceutics, 499, 81–89. https://doi.org/10.1016/j.ijpharm.2015.12.046.
Praveen, S., Gowda, D. V., Srivastava, A., & Osmani, R. A. M. (2016). Formulation and evaluation of nanostructured lipid carrier (NLC) for glimepiride. Der Pharmacia Lettre, 8, 304–309. https://doi.org/10.20959/wjpps20164-6398.
Patlolla, R. R., Chougule, M., Patel, A. R., Jackson, T., Tata, P. N. V., & Singh, M. (2010). Formulation, characterization and pulmonary deposition of nebulized celecoxib encapsulated nanostructured lipid carriers. Journal of Controlled Release, 144, 233–241. https://doi.org/10.1016/j.jconrel.2010.02.006.
D’Souza, S., & Souza, S. (2014). A review of in vitro drug release test methods for nano-sized dosage forms. Advances in Pharmacy, 2014, 1–12. https://doi.org/10.1155/2014/304757.
Ahmad, A. M. (2007). Recent advances in pharmacokinetic modeling. Biopharmaceutics and Drug Disposition, 28, 135–143. https://doi.org/10.1002/bdd.
Dash, S., Murthy, P. N., Nath, L., & Chowdhury, P. (2010). Kinetic modeling on drug release from controlled drug delivery systems. Acta Poloniae Pharmaceutica, 67, 217–223. https://doi.org/10.1016/S0928-0987(01)00095-1.
Hu, X., Yang, F., Liao, Y., Li, L., & Zhang, L. (2017). Cholesterol–PEG comodified poly (N -butyl) cyanoacrylate nanoparticles for brain delivery: In vitro and in vivo evaluations. Drug Delivery, 24, 121–132. https://doi.org/10.1080/10717544.2016.1233590.
Khatik, R., Dwivedi, P., Shukla, A., Srivastava, P., Rath, S. K., Paliwal, S. K., et al. (2014). Development, characterization and toxicological evaluations of phospholipids complexes of curcumin for effective drug delivery in cancer chemotherapy. Drug Delivery, 23, 1–12. https://doi.org/10.3109/10717544.2014.936988.
Li, C., Shen, Y., Sun, C., Nihad, C., & Tu, J. (2014). Immunosafety and chronic toxicity evaluation of monomethoxypoly(ethylene glycol)-b-poly(lactic acid) polymer micelles for paclitaxel delivery. Drug Delivery, 23, 1–8. https://doi.org/10.3109/10717544.2014.920429.
Bondonna, T. J., Jacquet, Y., & Wolf, G. (1977). Perfusion-fixation procedure for immediate histologic processing of brain tissue. Physiology and Behavior, 19, 345–347. https://doi.org/10.1016/0031-9384(77)90351-1.
Gage, G. J., Kipke, D. R., & Shain, W. (2012). Whole animal perfusion fixation for rodents. Journal of Visualized Experiments, 65, 1–9. https://doi.org/10.3791/3564.
Mainardes, R. M., Palmira, D., & Gremiao, M. (2009). Reversed phase HPLC determination of zidovudine in rat plasma and its pharmacokinetics after a single intranasal dose administration. Biological Research, 42, 357–364. https://doi.org/10.4067/S0716-97602009000300010.
Yuan, Z. Y., Hu, Y. L., & Gao, J. Q. (2015). Brain localization and neurotoxicity evaluation of polysorbate 80-modified chitosan nanoparticles in rats. PLoS One, 10, e0134722. https://doi.org/10.1371/journal.pone.0134722.
He, C., Cai, P., Li, J., Zhang, T., Lin, L., Abbasi, A. Z., et al. (2017). Blood-brain barrier-penetrating amphiphilic polymer nanoparticles deliver docetaxel for the treatment of brain metastases of triple negative breast cancer. Journal of Controlled Release, 246, 98–109.
Shilo, M., Sharon, A., Baranes, K., Motiei, M., Lellouche, J.-P. M., & Popovtzer, R. (2015). The effect of nanoparticle size on the probability to cross the blood-brain barrier: An in-vitro endothelial cell model. Journal of Nanobiotechnology, 13, 19. https://doi.org/10.1186/s12951-015-0075-7.
Drobek, T., Spencer, N. D., & Heuberger, M. (2005). Compressing PEG brushes. Macromolecules, 38, 5254–5259. https://doi.org/10.1021/ma0504217.
Storm, G., Belliot, S. O., Daemen, T., & Lasic, D. D. (1995). Surface modification of nanoparticles to oppose uptake by the mononuclear phagocyte system. Advanced Drug Delivery Reviews, 17, 31–48. https://doi.org/10.1016/0169-409X(95)00039-A.
Amoozgar, Z., & Yeo, Y. (2012). Recent advances in stealth coating of nanoparticle drug delivery systems. Wiley Interdisciplinary Reviews. Nanomedicine and Nanobiotechnology, 4, 219–233. https://doi.org/10.1002/wnan.1157.
Łaszcz, M., Kosmacińska, B., Korczak, K., Śmigielska, B., Glice, M., Maruszak, W., et al. (2007). Study on compatibility of imatinib mesylate with pharmaceutical excipients. Journal of Thermal Analysis and Calorimetry, 88, 305–310. https://doi.org/10.1007/s10973-006-8001-8.
Manikandan, M., Kannan, K., & Manavalan, R. (2013). Compatibility studies of camptothecin with various pharmaceutical excipients used in the development of nanoparticle formulation. International Journal of Pharmacy and Pharmaceutical Sciences, 5, 315–321.
Nagaich, U., & Gulati, N. (2016). Nanostructured lipid carriers (NLC) based controlled release topical gel of clobetasol propionate: Design and in vivo characterization. Drug Delivery and Translational Research, 6, 289–298. https://doi.org/10.1007/s13346-016-0291-1.
Ribeiro, L. N. M., Breitkreitz, M. C., Guilherme, V. A., da Silva, G. H. R., Couto, V. M., Castro, S. R., et al. (2017). Natural lipids-based NLC containing lidocaine: From pre-formulation to in vivo studies. European Journal of Pharmaceutical Sciences, 106, 102–112. https://doi.org/10.1016/j.ejps.2017.05.060.
Barre, J., Urien, S., Albengres, E., & Tillement, J. P. (1988). Plasma and tissue binding as determinants of drug body distribution. Possible applications to toxicological studies. Xenobiotica, 18(Suppl 1), 15–20.
Sane, R., Agarwal, S., & Elmquist, W. F. (2012). Brain distribution and bioavailability of elacridar after different routes of administration in the mouse. Drug Metabolism and Disposition, 40, 1612–1619. https://doi.org/10.1124/dmd.112.045930.
Lockman, P. R., Koziara, J. M., Mumper, R. J., & Allen, D. D. (2004). Nanoparticle surface charges alter blood–brain barrier integrity and permeability. Journal of Drug Targeting, 12, 635–641. https://doi.org/10.1080/10611860400015936.
Voigt, N., Henrich-Noack, P., Kockentiedt, S., Hintz, W., Tomas, J., & Sabel, B. A. (2014). Surfactants, not size or zeta-potential influence blood-brain barrier passage of polymeric nanoparticles. European Journal of Pharmaceutics and Biopharmaceutics, 87, 19–29. https://doi.org/10.1016/j.ejpb.2014.02.013.
Acknowledgments
The authors gratefully acknowledge the experimental/analytical support of Guwahati Biotech Park, Technology Complex, IIT Guwahati and The Sophisticated Analytical Instrument Facility (SAIF), NEHU Shillong, and College of Veterinary Science, Guwahati. This work was financially supported by the Department of Biotechnology, Ministry of Science & Technology, Government of India under Grant No. BT/504/NE/TBP/2013.
Declaration
All figures and tables are original and self-made.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Chakraborty, T., Das, M.K., Dutta, L., Mukherjee, B., Das, S., Sarma, A. (2019). Successful Delivery of Zidovudine-Loaded Docosanol Nanostructured Lipid Carriers (Docosanol NLCs) into Rat Brain. In: Pathak, Y. (eds) Surface Modification of Nanoparticles for Targeted Drug Delivery. Springer, Cham. https://doi.org/10.1007/978-3-030-06115-9_14
Download citation
DOI: https://doi.org/10.1007/978-3-030-06115-9_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-06114-2
Online ISBN: 978-3-030-06115-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)