Abstract
Despite advances in diagnosis and treatment of subarachnoid hemorrhage (SAH), combined morbidity and mortality rate in SAH patients accounted for greater than 50%. Many prognostic factors have been reported including delayed cerebral ischemia, cerebral vasospasm-induced infarction, and shunt-dependent hydrocephalus as potentially preventable or treatable causes. Recent experimental studies emphasize that early brain injury, a concept to explain acute pathophysiological events that occur in brain before onset of cerebral vasospasm within the first 72 h of SAH, may be more important than cerebral vasospasm, a classically important determinant of poor outcome, in post-SAH outcome. Galectin-3 is known for one of matricellular proteins and a mediator of inflammation in the central nervous system. Galectin-3 was also reported to contribute to poor outcomes in SAH patients, but the role of galectin-3 after SAH has not been determined. We produced experimental SAH mice, of which the top of the internal carotid artery was perforated by 4-0 monofilament, and evaluated effects of a galectin-3 inhibitor. We assessed neurological scores and brain water content at 24 h. The administration of a galectin-3 inhibitor significantly ameliorated brain edema and neuronal score in experimental SAH mice.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Early brain injury (EBI) is thought to be a pivotal determinant for poor outcome after subarachnoid hemorrhage (SAH). EBI is defined as acute pathophysiological events that occur in the brain before onset of cerebral vasospasm within 72 h of SAH and consists of any pathophysiological mechanisms except for iatrogenic brain injury [1]. We previously reported the possible mechanisms of EBI, focusing on inflammation and microcirculatory disturbance [2,3,4] . SAH not only induces transient global brain ischemia secondary to elevated intracranial pressure and mechanical stress but also produces various substances including heme, fibrinogen, intracellular components, and inflammation-related proteins. These substances stimulate cell surface receptors including toll-like receptor 4 and induce several inflammatory pathways [5]. Mitogen-activated protein kinase (MAPK) pathway seems to be a major inflammatory pathway related with early brain injury [2,3,4] . Finally, proinflammatory substances such as matrix metalloproteinase-9 (MMP-9) and tenascin-C (TNC) cause and exacerbate cerebral vasospasm, neuronal apoptosis, and blood-brain barrier disruption [2,3,4, 6] .
Galectin-3 belongs to galectin family, which consists of β-galactoside-binding lectins participating in a wide range of biological processes including immune responses, cell–cell/extracellular matrix interaction, and apoptosis. Galectin-3 is the only chimera-type galectin and reported to be involved in brain inflammatory responses [7] . We previously reported that plasma galectin-3 levels in non-severe SAH patients were significantly correlated with the occurrence of delayed cerebral ischemia (DCI) and delayed cerebral infarction [8] . In this study, first, we elucidated whether a high concentration of plasma galectin-3 in SAH patients, including those with severe World Federation of Neurological Surgeons (WFNS) grade, was associated with poor outcome. Then, we evaluated whether inhibition of galectin-3 reduced brain edema in experimental SAH models.
Materials and Methods
Clinical Measurements of Plasma Galectin-3 Levels in SAH Patients
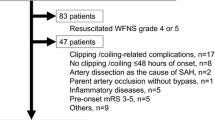
We collected blood samples from patients who participated in the Prospective Registry for Searching Mediators of Neurovascular Events After Aneurysmal SAH [pSEED] performed at eight tertiary referral centers in Mie prefecture in Japan between September 2013 and December 2015 [8] . Inclusion criteria were as follows: ≥20 years of age at onset, SAH on computed tomography (CT) scans or lumbar puncture, saccular aneurysm as the cause of SAH confirmed on three-dimensional CT angiography, magnetic resonance (MR) angiography, digital subtraction angiography, aneurysmal obliteration by clipping or endovascular coiling within 48 h of onset, and post-clipping or post-coiling blood sampling on days 1–3 after onset [8] . SAH that was not due to a ruptured saccular aneurysm, patients who underwent parental artery occlusion, patients who had angiographic or treatment-related complications, patients with pre-onset modified Rankin scale (mRS) 3–5, patients who could not receive enough anti-DCI therapy due to severe medical complications, and patients who had past medical history of concomitant inflammatory diseases that are known to upregulate galectin-3 were excluded [8] . All blood samples were centrifuged for 5 min at 3000 × g, and the supernatant fluid was stored at −78 °C until assayed. Plasma galectin-3 levels were blindly determined by enzyme-linked immunosorbent assay kit for human galectin-3 (code no. 27755; Immuno-Biological Laboratories, Fujioka, Japan) [8] . We defined poor outcome as mRS 3–6 at 3 months of post-SAH.
Experimental Study as to the Role of Galectin-3 in SAH
All procedures were approved by the Animal Ethics Review Committee of Mie University and followed the institution’s Guidelines for Animal Experiments. C57BL/6 wild-type (WT) male adult mice (weight, 25–30 g) were used for this study. To make SAH, endovascular filament perforation was performed as previously described [9] . Briefly, after midline skin incision of neck, the left external carotid artery (ECA) was exposed, and ECA was cut to insert 4-0 nylon monofilament, perforating the bifurcation of internal carotid artery. At 30 min after modeling, an intraventricular injection of 4 μg modified citrus pectin (MCP), which is known to be a galectin-3 inhibitor [10, 11], or vehicle (sterile phosphate-buffered saline [PBS]), was performed as previously described [9] .
To assess the effect of MCP on EBI, 26 WT mice were randomly divided into 3 groups: sham + vehicle (n = 7), SAH + vehicle (n = 10), and SAH + MCP (n = 9) groups. Neurological score, SAH severity, and brain water content were evaluated at 24 h after modeling. Neurological score was blindly evaluated by modified Garcia’s scale as previously described [4] . Animals were given a total score of 2 to 18 in 1-number steps, and higher scores indicated better function. SAH severity was blindly evaluated using high-resolution pictures of the base of the brain taken at each sacrifice as previously reported [4] , and mice with moderate severity of SAH were enrolled in this study. Brain water content was measured by the wet/dry method for assessing brain edema. In brief, the brain of sacrificed mice under deep anesthesia was quickly removed and separated into the left and right hemispheres, cerebellum, and brain stem. Each part of the brain was weighed as wet weight, and then they were dried for 24 h at 105 °C and weighed again as dry weight. The percentage of water content was calculated according to the following formula: [(wet weight − dry weight)/wet weight] × 100%.
Statistical Analysis
Categorical variables were reported as the number and percentage, and continuous variables were reported as the mean ± standard deviation (SD) and compared between two groups using the unpaired t-test or among three groups using one-way analysis of variance with Tukey-Kramer post hoc tests. A P value ≤0.05 was considered significant.
Results
High Concentrations of Plasma Galectin-3 Associated with Poor Outcome in SAH Patients
249 patients were registered in pSEED between September 2013 and December 2015, and 149 patients were eligible for inclusion criteria. Mean age was 63.9 ± 13.5, and there were 107 females. Fifty-four patients developed poor outcome defined as mRS 3–6. Plasma concentrations of galectin-3 on days 1–3 were significantly higher in patients with poor outcomes than those with good outcomes (5.43 ± 3.39 vs. 3.77 ± 2.24 ng/mL, P < 0.001; Fig. 1).
Inhibition of Galectin-3 Ameliorates Brain Edema in Experimental SAH Mice
No sham-operated mice died, and the mortality rate was not significantly different between the SAH + vehicle group (30%) and SAH + MCP group (22%). SAH grade was similar between the SAH + vehicle group and SAH + MCP group (Fig. 2a). The SAH-MCP group showed significant improvement of neurological score and brain water content in the left hemisphere compared with the SAH-vehicle group (P < 0.001, P = 0.020, respectively, Fig. 2b, c).
Discussion
Clinically, elevated plasma galectin-3 levels were reported to be correlated with the severity and poor outcome in spontaneous brain hemorrhage and traumatic brain injury [12, 13], and these results suggested the possibility of the linkage between galectin-3 and inflammation [12, 13]. Our previous study elucidated that elevated plasma galectin-3 levels in non-severe SAH patients were significantly correlated with the incidence of DCI and delayed cerebral infarction without cerebral vasospasm and consequently might contribute to poor outcome [8] . However, the former study did not include severe SAH patients defined as WFNS grade 4–5 because of the difficulty in detecting neurological worsening due to its severe state [8] . Therefore, in this preliminary study, we first demonstrated that higher concentrations of plasma galectin-3 were significantly associated with poor outcome in SAH patients, including those with worse WFNS grades.
Our preliminary experimental study showed that administration of MCP ameliorated both neuronal score and brain edema in experimental SAH mice. In the process of development of the central nervous system, galectin-3 is expressed in various glial cells and induces migration of neural stem cell and myelination of oligodendrocyte [14] . However, in rodent brain-resident immune cells, correlating with Janus kinase/signal transducers and activator of transcription (JAK-STAT) pathway, galectin-3 acts as an inflammatory mediator [15] . Buruguillos et al. reported that galectin-3 induces sustained microglial activation and prolonged inflammatory response through binding to toll-like receptor 4 (TLR4) [7, 16] . Yip et al. demonstrated that galectin-3, binding to TLR4, promotes inflammation and neuronal death in traumatic brain injury models of mice [17]. On the other hand, neuroinflammation after SAH, which is included in the mechanisms of EBI, induces brain permeability and neuronal apoptosis [1]. Therefore, galectin-3 might induce the brain permeability as an inflammatory mediator.
The limitations of this study are as follows: the number of rodent models was too small, and the mechanism how galectin-3 caused brain edema was undetermined. Therefore, further studies are needed to elucidate the role of galectin-3 after SAH.
References
Suzuki H. What is early brain injury? Transl Stroke Res. 2015;6:1–3.
Fujimoto M, Shiba M, Kawakita F, Liu L, Shimojo N, Imanaka-Yoshida K, Yoshida T, Suzuki H. Deficiency of tenascin-C and attenuation of blood-brain barrier disruption following experimental subarachnoid hemorrhage in mice. J Neurosurg. 2016;124:1693–702.
Liu L, Fujimoto M, Kawakita F, Nakano F, Imanaka-Yoshida K, Yoshida T, Suzuki H. Anti-vascular endothelial growth factor treatment suppresses early brain injury after subarachnoid hemorrhage in mice. Mol Neurobiol. 2016;53:4529–38.
Liu L, Kawakita F, Fujimoto M, Nakano F, Imanaka-Yoshida K, Yoshida T, Suzuki H. Role of periostin in early brain injury after subarachnoid hemorrhage in mice. Stroke. 2017;48:1108–11.
Okada T, Suzuki H. Toll-like receptor 4 as a possible therapeutic target for delayed brain injuries after aneurysmal subarachnoid hemorrhage. Neural Regen Res. 2017;12:193–6.
Fujimoto M, Shiba M, Kawakita F, Liu L, Shimojo N, Imanaka-Yoshida K, Yoshida T, Suzuki H. Effects of Tenascin-C knockout on cerebral vasospasm after experimental subarachnoid hemorrhage in mice. Mol Neurobiol. 2018;55(3):1951–8. https://doi.org/10.1007/s12035-017-0466-x.
Burguillos Miguel A, Svensson M, Schulte T, Boza-Serrano A, Garcia-Quintanilla A, Kavanagh E, Santiago M, Viceconte N, Oliva-Martin Maria J, Osman Ahmed M, Salomonsson E, Amar L, Persson A, Blomgren K, Achour A, Englund E, Leffler H, Venero Jose L, Joseph B, Deierborg T. Microglia-secreted Galectin-3 acts as a Toll-like receptor 4 ligand and contributes to microglial activation. Cell Rep. 2015;10:1626–38.
Nishikawa H, Nakatsuka Y, Shiba M, Kawakita F, Fujimoto M, Suzuki H. Increased plasma Galectin-3 preceding the development of delayed cerebral infarction and eventual poor outcome in non-severe aneurysmal subarachnoid hemorrhage. Transl Stroke Res. 2018;9(2):110–9. https://doi.org/10.1007/s12975-017-0564-0.
Altay O, Suzuki H, Hasegawa Y, Caner B, Krafft PR, Fujii M, Tang J, Zhang JH. Isoflurane attenuates blood-brain barrier disruption in ipsilateral hemisphere after subarachnoid hemorrhage in mice. Stroke. 2012;43:2513–6.
Ma Z, Han Q, Wang X, Ai Z, Zheng Y. Galectin-3 inhibition is associated with neuropathic pain attenuation after peripheral nerve injury. PLoS One. 2016;11:e0148792. https://doi.org/10.1371/journal.pone.0148792.
Vergaro G, Prud'homme M, Fazal L, Merval R, Passino C, Emdin M, Samuel JL, Cohen Solal A, Delcayre C. Inhibition of Galectin-3 pathway prevents isoproterenol-induced left ventricular dysfunction and fibrosis in mice. Hypertension. 2016;67:606–12.
Shen YF, Yu WH, Dong XQ, Du Q, Yang DB, Wu GQ, Zhang ZY, Wang H, Jiang L. The change of plasma galectin-3 concentrations after traumatic brain injury. Clin Chim Acta. 2016;456:75–80.
Yan XJ, Yu GF, Jie YQ, Fan XF, Huang Q, Dai WM. Role of galectin-3 in plasma as a predictive biomarker of outcome after acute intracerebral hemorrhage. J Neurol Sci. 2016;368:121–7.
Shin T. The pleiotropic effects of galectin-3 in neuroinflammation: a review. Acta Histochem. 2013;115:407–11.
Jeon SB, Yoon HJ, Chang CY, Koh HS, Jeon SH, Park EJ. Galectin-3 exerts cytokine-like regulatory actions through the JAK-STAT pathway. J Immunol. 2010;185:7037–46.
Kawakita F, Fujimoto M, Liu L, Nakano F, Nakatsuka Y, Suzuki H. Effects of Toll-like receptor 4 antagonists against cerebral vasospasm after experimental subarachnoid hemorrhage in mice. Mol Neurobiol. 2017;54(8):6624–33. https://doi.org/10.1007/s12035-016-0178-7.
Yip PK, Carrillo-Jimenez A, King P, Vilalta A, Nomura K, Chau CC, Egerton AM, Liu ZH, Shetty AJ, Tremoleda JL, Davies M, Deierborg T, Priestley JV, Brown GC, Michael-Titus AT, Venero JL, Burguillos MA. Galectin-3 released in response to traumatic brain injury acts as an alarmin orchestrating brain immune response and promoting neurodegeneration. Sci Rep. 2017;7:41689. https://doi.org/10.1038/srep41689.
Acknowledgments
We thank Ms. Chiduru Yamamoto, Department of Neurosurgery, Mie University Graduate School of Medicine, for providing technical assistance.
Conflict of interest: The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Nishikawa, H. et al. (2020). The Role of Galectin-3 in Subarachnoid Hemorrhage: A Preliminary Study. In: Martin, R., Boling, W., Chen, G., Zhang, J. (eds) Subarachnoid Hemorrhage. Acta Neurochirurgica Supplement, vol 127. Springer, Cham. https://doi.org/10.1007/978-3-030-04615-6_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-04615-6_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-04614-9
Online ISBN: 978-3-030-04615-6
eBook Packages: MedicineMedicine (R0)