Abstract
A matricellular protein galectin-3 is involved in tissue injury and inflammation, but the role of galectin-3 remains unclear in aneurysmal subarachnoid hemorrhage (SAH). The purpose of this study was to assess whether acute-stage galectin-3 levels were associated with the subsequent development of neurovascular events and outcome after SAH. This study included 83 consecutive patients diagnosed with aneurysmal SAH of resuscitated World Federation of Neurological Surgeons (WFNS) grades 1–3. Plasma galectin-3 levels were once measured on days 1–3 (the day after clipping or coiling). Fifteen patients had poor outcomes, which were associated with increasing age, female, pre-onset morbidity, worse WFNS grade, modified Fisher computed tomography scale, acute hydrocephalus, and higher galectin-3 levels compared with good outcomes. Multivariate analyses revealed that plasma galectin-3 was an independent determinant for poor outcome (odds ratio, 3.08; 95% confidence interval, 1.58–6.00; p = 0.001). Among post-SAH neurovascular events occurring on day 4 and thereafter, delayed cerebral ischemia and infarction, but not angiographic vasospasm and shunt-dependent hydrocephalus, showed significantly higher plasma galectin-3 levels on days 1–3. The receiver operating characteristic curve indicated that plasma galectin-3 with a cutoff value of 3.30 or 3.48 ng/ml predicted delayed cerebral infarction development or poor outcome (specificity, 62.5%, 70.6%; sensitivity, 90.9%, 73.3%, respectively). The findings suggest that plasma galectin-3 levels on days 1–3 would be a useful biomarker for predicting subsequent development of delayed cerebral infarction and eventual poor outcome and provide a new candidate, which may mediate between post-SAH early brain injury or inflammation and delayed cerebral infarction without vasospasm.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The outcome of aneurysmal subarachnoid hemorrhage (SAH) remains poor despite advances in the diagnosis and treatment [1]. Many prognostic factors have been reported including delayed cerebral ischemia (DCI), cerebral vasospasm-induced infarction, and shunt-dependent hydrocephalus as potentially preventable or treatable causes [1, 2]. Recent experimental studies emphasize that early brain injury (EBI), a concept to explain acute pathophysiological events that occur in brain before the onset of cerebral vasospasm within the first 72 h of SAH, may be more important than cerebral vasospasm, a classically important determinant of poor outcome, in post-SAH outcome [3,4,5]. Some of EBIs may be a pre-cursor for cerebral vasospasm and/or vasospasm-unrelated DCI, and others of EBIs may contribute to increased tissue vulnerability to secondary insults [3]. Thus, to find a biomarker representing EBI may be useful to perform early diagnosis and treatment for DCI and to improve outcome after SAH.
Galectins are β-galactoside-binding lectins that participate in a wide range of biological processes, including immune responses, cell–cell/extracellular matrix interaction, and apoptosis, and are classified as proto-, chimera-, or tandem repeat types based on their structures [6]. Among 20 kinds of galectins [6], a matricellular protein galectin-3 was reported to be involved in brain inflammatory responses in ischemic brain injury in mice and rats [7, 8]. In a clinical setting, plasma galectin-3 concentrations had close relation to inflammation, trauma severity, and clinical outcome after acute traumatic brain injury [9]. A recent study also reported that admission plasma galectin-3 levels were correlated with World Federation of Neurological Surgeons (WFNS) grade and modified Fisher computed tomography (CT) scale and predicted 6-month outcomes after aneurysmal SAH [10]. However, it is well known that poor-grade or severe SAH patients have worse outcomes [1], while there are no studies investigating the relationships between acute-stage galectin-3 levels and delayed-onset secondary neurovascular events such as DCI, which is an important modifiable prognostic factor [1,2,3]. Thus, this study targeted non-severe SAH patients in whom DCI is easily detected, and examined relationships between acute-stage plasma galectin-3 levels and variables that can be obtained in an acute stage (until day 3), and delayed neurovascular events that occur on day 4 and thereafter, or outcome.
Methods
Patient and Clinical Variables
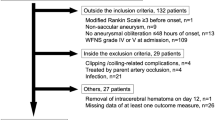
This is a prospective cohort study (Prospective Registry for Searching Mediators of Neurovascular Events After Aneurysmal SAH [pSEED]) performed at eight tertiary referral centers in Mie Prefecture in Japan (listed in the Appendix) between September 2013 and December 2015. The study was approved by the Institutional Ethics Committee, and written informed consent was obtained from the relatives. Two hundreds and thirteen SAH patients were registered, and 83 patients met the following inclusion criteria: pre-onset modified Rankin Scale (mRS) zero to two, ≥ 20 years of age at onset, resuscitated WFNS grades 1–3 [11], SAH on CT scans or lumbar puncture, saccular aneurysm as the cause of SAH confirmed on three-dimensional CT angiography, digital subtraction angiography (DSA) or magnetic resonance (MR) angiography, aneurysmal obliteration by clipping or coiling within 48 h of onset, and blood sampling on days 1–3 after onset (the day after clipping or coiling) (Fig. 1). Excluded from the study were patients with ruptured fusiform, dissecting, traumatic, mycotic, and arteriovenous malformation-related aneurysms or SAH of unknown etiology; patients who were treated by parent artery occlusion without bypass surgery; patients who had angiographic or treatment-related complications such as cerebral infarction or hemorrhage; patients who could not receive enough anti-DCI treatment due to serious pre-morbidity such as heart, respiratory, or renal failure; and patients with concomitant inflammatory diseases that are known to upregulate galectin-3 [12, 13]. The timing of aneurysmal obliteration, selection of clipping or coiling, and other medical management or treatment strategies were decided by the onsite investigators and not limited.
Baseline demographic and clinical data included age, sex, pre-onset mRS, past medical history (hypertension, diabetes mellitus, dyslipidemia, cerebral infarction), smoking, admission and resuscitated WFNS grades, modified Fisher CT scale on admission [14], acute hydrocephalus [15], ruptured aneurysm location (anterior or posterior circulation), and treatment modality (clipping or coiling) used for aneurysmal obliteration. As factors that potentially affected outcomes, the following were evaluated: DCI, angiographic vasospasm, delayed cerebral infarction, and shunt-dependent hydrocephalus. The procedure-related hemorrhagic or ischemic complications were ruled out on CT or MR images on the first post-operative or post-intervention day. DCI was defined as otherwise an unexplained clinical deterioration (i.e., focal neurological impairments, a decrease of at least two points on the Glasgow Coma Scale, or both), which lasted for at least 1 h [16]. Other potential causes of clinical deterioration, such as hydrocephalus, rebleeding, or seizures, were rigorously excluded on clinical assessments, CT, MR images, or laboratory studies. Angiographic vasospasm was defined as a 50% reduction in the baseline vessel diameter on CT angiography, DSA, or MR angiography. Delayed cerebral infarction was defined as a new infarct on CT or MR images that was not visible on admission or immediate post-operative or post-intervention scans, or both. Shunt-dependent hydrocephalus was diagnosed when clinical deterioration with no detectable causes other than hydrocephalus that occurred after day 14 post-hemorrhage and when the ventricular size progressively increased and the Evans index became greater than 0.30, being treated by cerebrospinal shunting [17]. Determination of these complications was made at each center, and the organizing committee qualified them. Outcome was blindly assessed using mRS at 3 months and was classified as good (mRS 0–2) or poor (mRS 3–6).
Measurement of Galectin-3
At the day after aneurysmal clipping or coiling (days 1–3 after onset), blood samples were once collected with minimal stasis from a vein. All samples were centrifuged for 5 min at 3000×g, and the supernatant fluid was stored at − 78 °C until assayed. The study group gathered the samples and blindly determined plasma galectin-3 concentrations using a commercially available enzyme-linked immunosorbent assay kit for human galectin-3 (code no. 27755; Immuno-Biological Laboratories, Fujioka, Japan).
As a control group, 10 patients with unruptured cerebral aneurysms were enrolled, and the plasma samples were analyzed as well.
Statistical Analysis
There were no missing data in the patients who met the inclusion criteria in the study. Variables were recorded as categorical or continuous variables. Categorical variables were reported as the number and percentage and analyzed using the chi-squared or Fisher exact test, as appropriate. Continuous variables were reported as the mean ± standard deviation (SD) and compared between two groups using the unpaired t test or among three groups using one-way analysis of variance with Tukey–Kramer post hoc tests. The impact of each variable on outcome was determined by multivariate unconditional logistic regression analysis using the 3-month dichotomous mRS outcome (good or poor) as the dependent variable. The baseline variables significantly related to poor outcome on univariate analyses; treatment modality and plasma galectin-3 concentrations were considered independent variables, although only the variable with the smallest probability value was used as a candidate variable among similar clinical variables that were intercorrelated, and the variables that Pearson’s correlation coefficient showed significant correlation with plasma concentrations of galectin-3 were excluded. The adjusted odds ratios (ORs) with 95% confidence intervals (CIs) were calculated, and independence of variables was tested using the likelihood ratio test on reduced models. Sensitivity and specificity were estimated for different sets of cutoff values of plasma concentrations of galectin-3. To minimize the potential bias introduced by choosing a single cutoff value for positivity, a receiver operating characteristic (ROC) curve was constructed. A p value ≤ 0.05 was considered significant.
Results
Plasma Galectin-3 Levels in Patients with Unruptured Cerebral Aneurysms
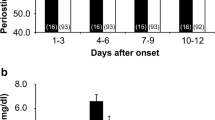
The control group consisted of five females and five males with the age of 67.7 ± 8.9 years. The past medical history included smoking (n = 5), hypertension (n = 5), dyslipidemia (n = 4), and diabetes mellitus (n = 4). There were no relationships observed between plasma galectin-3 levels and age (r = 0.09, p = 0.806) or pre-onset mRS (r = 0.39, p = 0.269; Pearson’s correlation coefficient analyses). The SAH patients showed significantly higher concentrations of plasma galectin-3 than the control patients (3.42 ± 1.60 versus 2.21 ± 1.16 ng/ml, p = 0.023).
Baseline Variables Related to Poor Outcome After SAH
Fifteen of 83 SAH patients were classified as poor outcomes based on the 3-month mRS. Among baseline variables that could be obtained by day 3, age, sex, pre-onset mRS, admission and resuscitated WFNS grade, modified Fisher CT scale, and acute hydrocephalus were significantly associated with poor outcomes (Table 1). Other baseline variables including treatment modality (clipping or coiling) used for aneurysmal obliteration were not significantly different between good and poor outcomes.
Known Major Outcome Determinants and Poor Outcome After SAH
As known outcome determinants that occur on day 4 and thereafter, DCI, angiographic vasospasm, delayed cerebral infarction, and shunt-dependent hydrocephalus were evaluated. The incidence of DCI, delayed cerebral infarction, and shunt-dependent hydrocephalus, but not angiographic vasospasm, was significantly higher in patients with poor outcomes compared with those with good outcomes (Table 2).
Relationships Between Acute-Stage Plasma Galectin-3 Levels and Known Major Outcome Determinants or Outcome after SAH
Plasma concentrations of galectin-3 on days 1–3 were significantly higher in patients with poor outcomes than those with good outcomes (5.33 ± 2.35 versus 3.00 ± 0.98 ng/ml, p < 0.001; Fig. 2a). Patients with DCI or delayed cerebral infarction also showed significantly higher plasma concentrations of galectin-3 on days 1–3 compared with those without them (4.61 ± 1.37 versus 3.24 ± 1.56 ng/ml, p = 0.007; 4.65 ± 2.19 versus 3.17 ± 1.33 ng/ml, p = 0.001, respectively), whereas there were no significant relationships between acute-stage plasma concentrations of galectin-3 and angiographic vasospasm or shunt-dependent hydrocephalus (Fig. 2b–e). The patients who subsequently had DCI or delayed cerebral infarction without angiographic vasospasm but not with vasospasm had significantly higher plasma galectin-3 levels on days 1–3 compared with those without DCI or delayed cerebral infarction (Fig. 3). Plasma galectin-3 levels were not significantly different between clipping (3.49 ± 1.59 ng/ml) and coiling (3.15 ± 1.64 ng/ml) cases.
Multivariate Analyses for Poor Outcome After SAH
Among baseline variables and plasma concentrations of galectin-3 on days 1–3 post-SAH, Pearson’s correlation coefficient analyses revealed a significant correlation between post-SAH plasma concentration of galectin-3 and age at the onset (r = 0.50, p < 0.001) or pre-onset mRS (r = 0.47, p < 0.001) (Fig. 4). There was also a strong correlation between admission and resuscitated WFNS grades (r = 0.83, p < 0.001). Therefore, first, baseline variables significantly related to poor outcome on univariate analyses except for age, pre-onset mRS and admission WFNS grade (having a higher p value than resuscitated WFNS grade), as well as plasma galectin-3 concentrations and treatment modality, all of which could be determined in an acute stage (days 0–3) of SAH and are potential determinants for post-SAH outcomes, were used in multivariate analyses. Multivariate analyses revealed that higher plasma concentrations of galectin-3 on days 1–3 were the sole independent determinant for poor outcomes (OR, 3.08; 95% CI, 1.58–6.00; p = 0.001) (Table 3). Then, another multivariate analysis using age and pre-onset mRS in addition to variables in Table 3 was performed and showed that increasing age (OR, 1.12; 95% CI, 1.01–1.24; p = 0.036), resuscitated WFNS grade (OR, 5.17; 95% CI, 1.02–26.20; p = 0.047), and higher plasma galectin-3 levels (OR, 2.38; 95% CI, 1.11–5.10; p = 0.026) were independent determinants for poor outcomes (Table 4).
Prediction of Poor Outcome After SAH
When a ROC curve was generated for the performance of plasma concentrations of galectin-3 on days 1–3 according to poor and good outcomes, the area under the ROC curve (AUC) was 0.80. To predict poor outcome, the ROC curve indicated that plasma galectin-3 with a cutoff value of 3.48 ng/ml resulted in a specificity of 70.6% and a sensitivity of 73.3% on days 1–3 (Fig. 5a). The AUC of galectin-3 levels was the best compared with admission or resuscitated WFNS grade and modified Fisher CT scale (Table 5). The specificity was 63.8% and sensitivity 78.6% when a ROC curve was generated according to DCI and no DCI with a cutoff value of 3.37 ng/ml (Fig. 5b). The specificity was 62.5% and sensitivity 90.9% when a ROC curve was generated according to delayed cerebral infarction and no infarction with a cutoff value of 3.30 ng/ml (Fig. 5c).
Discussion
The novel findings in the present study were as follows: (1) higher plasma galectin-3 concentration on days 1–3 was an independent predictor for poor outcomes in non-severe SAH patients; (2) higher plasma galectin-3 levels on days 1–3 post-SAH were correlated with increasing age and worse pre-onset mRS; and (3) higher plasma galectin-3 levels on days 1–3 were associated with subsequent development of DCI and delayed cerebral infarction, but not angiographic vasospasm.
Galectins are members of a family of proteins defined by their conserved peptide sequence elements, which are crucial for their affinities to β-galactoside-containing carbohydrate moieties of glycoconjugates, and they are classified as proto-type (galectin-1, 2, 5, 7, 10, 11, 13–20), chimera-type (galectin-3), or tandem repeat type (galectin-4, 6, 8, 9, 12) based on their structures [6]. Galectins are distributed both inside and outside cells and are believed to have roles in both intra- and extracellular milieus [6]. Extracellular galectins exhibit bivalent or multivalent interactions with glycans on cell surfaces and induce various cellular responses, including production of cytokines and other inflammatory mediators, cell adhesion, migration, and apoptosis [18]. Intracellular galectins can participate in signaling pathways and alter biological responses, including apoptosis, cell differentiation, and cell motility [18]. Galectins may play important roles in acute and chronic inflammatory responses, as well as other diverse pathological processes [7, 8, 18]. Galectin-3 is the only one found in the chimera category, which has one carbohydrate-recognition domain and a long non-lectin domain, and can exist in a monomeric form or can associate via the non-lectin domain into multivalent complexes up to a pentameric form in a concentration-dependent manner [18]. This allows galectin-3 to bridge effectively between different ligands and to exert different functions [18]. Galectin-3 is not only a matricellular protein but also actively secreted from live cells, potentially being useful as a prognostic biomarker in traumatic brain injury, intracerebral hemorrhage, and SAH [9, 10, 19].
DCI and delayed cerebral infarction are one of the most important determinants for poor outcomes after aneurysmal SAH [16]. Recent studies have shown that DCI and delayed cerebral infarction are caused by cerebral vasospasm and other various pathophysiologies [2, 3, 20,21,22,23]. EBI also may contribute to the development of cerebral vasospasm and vasospasm-unrelated DCI [3]. This study revealed that increased galectin-3 on days 1–3 was unrelated to subsequent development of angiographic vasospasm, but related to DCI and delayed cerebral infarction. The findings suggest that galectin-3 may mediate between EBI and DCI without vasospasm. Although another matricellular protein tenascin-C is also reported to mediate between EBI and DCI, tenascin-C may cause both vasospasm-induced and vasospasm-unrelated DCI [5, 21,22,23,24]. SAH impacts brain parenchyma by activating astrocytes and microglia and triggering upregulation of pro-inflammatory cytokines [25]. An in vitro study reported that galectin-3 expression was enhanced in activated glia, which were stimulated by galectin-3 and produced pro-inflammatory mediators via the activation of the Janus kinase–signal transducers and activator of the transcription pathway [26]. It was also reported that microglia-secreted galectin-3 acted as a toll-like receptor 4 ligand and contributed to microglial activation [27] and that toll-like receptor 4 was involved in the development of DCI after experimental SAH [28]. In a clinical setting, plasma galectin-3 was a determinant of post-traumatic cerebral infarction: galectin-3 possibly contributed to the development of posttraumatic cerebral infarction via activating inflammation [9]. These findings suggest that galectin-3 acts as an endogenous danger signaling molecule mediating between EBI and DCI and plays an important role in the development of post-SAH delayed cerebral infarction.
Another interesting finding in this study was the correlation between age and concentrations of plasma galectin-3 on days 1–3 post-SAH. Matricellular proteins such as galectin-3 are usually downregulated under normal conditions in adult and upregulated under pathological conditions [29, 30]. Papaspyridonos et al. [31] reported that galectin-3 is an amplifier of inflammation in atherosclerotic plaque progression. Harvey et al. [32] reported that plasma galectin-3 levels correlated positively with increasing age and cardiovascular risk factors. Sanchis-Gomar et al. [33] suggested that lower plasma galectin-3 levels are associated with successful aging at least in individuals of highly advanced age, possibly by reflecting the conditions free of major chronic or aging-related disorders. In this study, there were no relationships between age or pre-onset mRS and plasma galectin-3 levels in patients with unruptured cerebral aneurysms, although the number of patients was limited. In addition, it remains unknown if plasma galectin-3 levels in patients with unruptured cerebral aneurysms affect those after the rupture. Therefore, further studies are needed in these regards. However, the previous reports suggest that elderly patients or patients with pre-onset morbidities have chronic inflammation with arteriosclerosis, which may provide a propensity to promote production of galectin-3 by the stimuli of SAH. As well as higher plasma galectin-3 levels on days 1–3 in this study, aging did not affect the incidence of angiographic vasospasms, but increased the incidence of DCI [34].
The limitations in this study include a relatively small number of patients, exclusion of patients with factors that potentially affect galectin-3 levels, no inclusion of poor-grade patients, and no consideration of treatments other than aneurysmal obliteration as well as a small number of control (non-SAH) patients. It is also unknown if the sampling point in this study is appropriate, because the pathophysiology of SAH patients may change every hour. In addition, functional significance of galectin-3 and the relationships between galectin-3 levels and other inflammation-related or known possible biomarkers remain obscure. However, it is a remarkable point that an increased plasma galectin-3 level on days 1–3 was an independent predictor for poor outcomes irrespective of treatment strategies and was related to subsequent development of DCI and delayed cerebral infarction without angiographic vasospasm. Galectin-3 may be a novel therapeutic target to prevent delayed cerebral infarction and to improve outcomes after SAH. Both experimental and clinical studies are further needed to clarify the function, mechanisms and clinical usefulness of post-SAH galectin-3 induction, including primary cell culture studies to examine molecular mechanisms, animal studies to test effects of galectin-3 blockage on brain injuries after SAH, and a large-scale prospective study to confirm the usefulness of galectin-3 as a biomarker associated with a large control group.
References
Taki W, Sakai N, Suzuki H, Prospective Registry of Subarachnoid Aneurysms Treatment (PRESAT) group. Determinants of poor outcome after aneurysmal subarachnoid hemorrhage when both clipping and coiling are available: PRESAT in Japan. World Neurosurg. 2011;76:437–45.
Suzuki H, Shiba M, Nakatsuka Y, Nakano F, Nishikawa H. Higher cerebrospinal fluid pH may contribute to the development of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Transl Stroke Res. 2017;8:165–73.
Suzuki H. What is early brain injury? Transl Stroke Res. 2015;6:1–3.
Liu L, Fujimoto M, Kawakita F, Nakano F, Imanaka-Yoshida K, Yoshida T, et al. Anti-vascular endothelial growth factor treatment suppresses early brain injury after subarachnoid hemorrhage in mice. Mol Neurobiol. 2016;53:4529–38.
Fujimoto M, Shiba M, Kawakita F, Liu L, Shimojo N, Imanaka-Yoshida K, et al. Deficiency of tenascin-C and attenuation of blood-brain barrier disruption following experimental subarachnoid hemorrhage in mice. J Neurosurg. 2016;124:1693–702.
Arikawa T, Simamura E, Shimada H, Nakamura T, Hatta T, Shoji H. Significance of sugar chain recognition by galectins and its involvement in disease-associated glycosylation. Congenit Anom (Kyoto). 2014;54:77–81.
Walther M, Kuklinski S, Pesheva P, Guntinas-Lichius O, Angelov DN, Neiss WF, et al. Galectin-3 is upregulated in microglial cells in response to ischemic brain lesions, but not to facial nerve axotomy. J Neurosci Res. 2000;61:430–5.
Lalancette-Hebert M, Swarup V, Beaulieu JM, Bohacek I, Abdelhamid E, Weng YC, et al. Galectin-3 is required for resident microglia activation and proliferation in response to ischemic injury. J Neurosci. 2012;32:10383–95.
Shen YF, Yu WH, Dong XQ, Du Q, Yang DB, Wu GQ, et al. The change of plasma galectin-3 concentrations after traumatic brain injury. Clin Chim Acta. 2016;456:75–80.
Liu H, Liu Y, Zhao J, Liu H, He S. Prognostic value of plasma galectin-3 levels after aneurysmal subarachnoid hemorrhage. Brain Behav. 2016;6:e00543.
Giraldo EA, Mandrekar JN, Rubin MN, Dupont SA, Zhang Y, Lanzino G, et al. Timing of clinical grade assessment and poor outcome in patients with aneurysmal subarachnoid hemorrhage. J Neurosurg. 2012;117:15–9.
Gao P, Simpson JL, Zhang J, Gibson PG. Galectin-3: its role in asthma and potential as an anti-inflammatory target. Respir Res. 2013;14:136. https://doi.org/10.1186/1465-9921-14-136.
Zuberi RI, Hsu DK, Kalayci O, Chen HY, Sheldon HK, Yu L, et al. Critical role for galectin-3 in airway inflammation and bronchial hyperresponsiveness in a murine model of asthma. Am J Pathol. 2004;165:2045–53.
Claassen J, Bernardini GL, Kreiter K, Bates J, Du YE, Copeland D, et al. Effect of cisternal and ventricular blood on risk of delayed cerebral ischemia after subarachnoid hemorrhage: the Fisher scale revisited. Stroke. 2001;32:2012–20.
Dupont S, Rabinstein AA. Extent of acute hydrocephalus after subarachnoid hemorrhage as a risk factor for poor functional outcome. Neurol Res. 2013;35:107–10.
Vergouwen MD, Vermeulen M, van Gijn J, Rinkel GJ, Wijdicks EF, Muizelaar JP, et al. Definition of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage as an outcome event in clinical trials and observational studies: proposal of a multidisciplinary research group. Stroke. 2010;41:2391–5.
Nakatsuka Y, Kawakita F, Yasuda R, Umeda Y, Toma N, Sakaida H, et al. Preventive effects of cilostazol against the development of shunt-dependent hydrocephalus after subarachnoid hemorrhage. J Neurosurg. 2016 Aug;5:1–8.
Liu FT, Rabinovich GA. Galectins: regulators of acute and chronic inflammation. Ann N Y Acad Sci. 2010;1183:158–82.
Yan XJ, Yu GF, Jie YQ, Fan XF, Huang Q, Dai WM. Role of galectin-3 in plasma as a predictive biomarker of outcome after acute intracerebral hemorrhage. J Neurol Sci. 2016;368:121–7.
Woitzik J, Dreier JP, Hecht N, Fiss I, Sandow N, Major S, et al. Delayed cerebral ischemia and spreading depolarization in absence of angiographic vasospasm after subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2012;32:203–12.
Shiba M, Fujimoto M, Imanaka-Yoshida K, Yoshida T, Taki W, Suzuki H. Tenascin-C causes neuronal apoptosis after subarachnoid hemorrhage in rats. Transl Stroke Res. 2014;5:238–47.
Suzuki H, Kanamaru K, Shiba M, Fujimoto M, Kawakita F, Imanaka-Yoshida K, et al. Tenascin-C is a possible mediator between initial brain injury and vasospasm-related and -unrelated delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Acta Neurochir Suppl. 2015;120:117–21.
Suzuki H, Kawakita F. Tenascin-C in aneurysmal subarachnoid hemorrhage: deleterious or protective? Neural Regen Res. 2016;11:230–1.
Fujimoto M, Shiba M, Kawakita F, Liu L, Shimojo N, Imanaka-Yoshida K, et al. Effects of tenascin-C knockout on cerebral vasospasm after experimental subarachnoid hemorrhage in mice. Mol Neurobiol. 2017 Feb 27; https://doi.org/10.1007/s12035-017-0466-x.
Fujii M, Yan J, Rolland WB, Soejima Y, Caner B, Zhang JH. Early brain injury, an evolving frontier in subarachnoid hemorrhage research. Transl Stroke Res. 2013;4:432–46.
Jeon SB, Yoon HJ, Chang CY, Koh HS, Jeon SH, Park EJ. Galectin-3 exerts cytokine-like regulatory actions through the JAK-STAT pathway. J Immunol. 2010;185:7037–46.
Burguillos MA, Svensson M, Schulte T, Boza-Serrano A, Garcia-Quintanilla A, Kavanagh E, et al. Microglia-secreted galectin-3 acts as a toll-like receptor 4 ligand and contributes to microglial activation. Cell Rep. 2015;10:1626–38.
Kawakita F, Fujimoto M, Liu L, Nakano F, Nakatsuka Y, Suzuki H. Effects of toll-like receptor 4 antagonists against cerebral vasospasm after experimental subarachnoid hemorrhage in mice. Mol Neurobiol. 2016. https://doi.org/10.1007/s12035-016-0178-7.
Jayakumar AR, Apeksha A, Norenberg MD. Role of matricellular proteins in disorders of the central nervous system. Neurochem Res. 2017;42:858–75.
Elola MT, Wolfenstein-Todel C, Troncoso MF, Vasta GR, Rabinovich GA. Galectins: matricellular glycan-binding proteins linking cell adhesion, migration, and survival. Cell Mol Life Sci. 2007;64:1679–700.
Papaspyridonos M, McNeill E, de Bono JP, Smith A, Burnand KG, Channon KM, et al. Galectin-3 is an amplifier of inflammation in atherosclerotic plaque progression through macrophage activation and monocyte chemoattraction. Arterioscler Thromb Vasc Biol. 2008;28:433–40.
Harvey A, Montezano AC, Lopes RA, Rios F, Touyz RM. Vascular fibrosis in aging and hypertension: molecular mechanisms and clinical implications. Can J Cardiol. 2016;32:659–68.
Sanchis-Gomar F, Santos-Lozano A, Pareja-Galeano H, Garatachea N, Alis R, Fiuza-Luces C, et al. Galectin-3, osteopontin and successful aging. Clin Chem Lab Med. 2016;54:873–7.
Lanzino G, Kassell NF, Germanson TP, Kongable GL, Truskowski LL, Torner JC, et al. Age and outcome after aneurysmal subarachnoid hemorrhage: why do older patients fare worse? J Neurosurg. 1996;85:410–8.
Acknowledgements
We thank Ms. Chiduru Yamamoto, Department of Neurosurgery, Mie University Graduate School of Medicine, for providing technical assistance.
Funding
This work was funded by a Grant-in-Aid for Scientific Research from the Mie Medical Research Foundation (grant number, N/A), which was awarded to Dr. Suzuki.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
This article does not contain any studies with animals performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
The pSEED group members along with their affiliations listed in the Appendix.
Appendix. Prospective Registry for Searching Mediators of Neurovascular Events After Aneurysmal Subarachnoid Hemorrhage (pSEED) Group
Appendix. Prospective Registry for Searching Mediators of Neurovascular Events After Aneurysmal Subarachnoid Hemorrhage (pSEED) Group
Department of Neurosurgery, Kuwana West Medical Center, Kuwana (Masatoshi Muramatsu, Kazuhide Hamada), Mie Prefectural General Medical Center, Yokkaichi (Yusuke Kamei, Keiji Fukazawa), Suzuka Kaisei Hospital, Suzuka (Tomohiro Araki, Yoichi Miura, Naoki Ichikawa), Mie University Graduate School of Medicine, Tsu (Hidenori Suzuki, Masato Shiba, Yoshinari Nakatsuka, Hirofumi Nishikawa), Mie Chuo Medical Center, Tsu (Fujimaro Ishida, Satoru Tanioka), Matsusaka Chuo General Hospital, Matsusaka (Shigehiko Niwa, Kazuhiko Tsuda), Saiseikai Matsusaka General Hospital, Matsusaka (Hiroto Murata, Masashi Fujimoto, Fumihiro Kawakita), Ise Red Cross Hospital, Ise (Fumitaka Miya, Takanori Sano, Yotaro Kitano).
Rights and permissions
About this article
Cite this article
Nishikawa, H., Nakatsuka, Y., Shiba, M. et al. Increased Plasma Galectin-3 Preceding the Development of Delayed Cerebral Infarction and Eventual Poor Outcome in Non-Severe Aneurysmal Subarachnoid Hemorrhage. Transl. Stroke Res. 9, 110–119 (2018). https://doi.org/10.1007/s12975-017-0564-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-017-0564-0