Abstract
Toll-like receptor 4 (TLR4) signaling may play a crucial role in the occurrence of cerebral vasospasm after subarachnoid hemorrhage (SAH). The main purpose of this study was to assess if selective blockage of TLR4 on cerebral arteries prevents cerebral vasospasm development and neurological impairments after SAH in mice. One hundred fourteen mice underwent endovascular perforation SAH or sham operation and were randomly divided into the following 6 groups: sham+vehicle, sham+LPS-RS ultrapure 8 μg, sham+LPS-RS ultrapure 40 μg, SAH+vehicle, SAH+LPS-RS ultrapure 8 μg, and SAH+LPS-RS ultrapure 40 μg. A selective TLR4 antagonist, LPS-RS ultrapure (8 or 40 μg), was administered intracerebroventricularly to mice at 30 min, and the effects were evaluated by neurobehavioral tests and India-ink angiography at 24–48 h, and Western blotting and immunohistochemistry on cerebral arteries at 24 h post-SAH. Higher but not lower dosages of LPS-RS ultrapure significantly prevented post-SAH neurological impairments and ameliorated cerebral vasospasm. SAH caused TLR4 activation and cyclooxygenase-1 (COX1) upregulation in the endothelial cells and smooth muscle cells of spastic cerebral arteries, both of which were significantly suppressed by LPS-RS ultrapure. Another selective TLR4 antagonist, IAXO-102, which has a different binding site from LPS-RS ultrapure, also showed similar protective effects to LPS-RS ultrapure. These findings suggest that TLR4 signaling is implicated in cerebral vasospasm development at least partly via COX1 upregulation, and that TLR4 antagonists have therapeutic potential as a new therapy against cerebral vasospasm.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebral vasospasm still remains a major cause of morbidity and mortality after aneurysmal subarachnoid hemorrhage (SAH) [1]. Radiographic vasospasm is found in 50 to 70 % of patients surviving SAH, and half of those are associated with delayed cerebral ischemia (DCI) [2]. Although recent investigations suggest that other factors such as early brain injury also cause DCI [3], it is well-known that DCI more frequently occurs associated with severe vasospasm [4]. Thus, cerebral vasospasm remains an important therapeutic target, but the exact molecular mechanisms of vasospasm development are obscure.
Neuroinflammation is a well-recognized consequence of SAH and may be responsible for neurovascular events after SAH. Toll-like receptor 4 (TLR4) belongs to a large family of pattern recognition receptors that are potential links between inflammation and vascular dysfunction [5]. Higher TLR4 levels on peripheral blood mononuclear cells were reported to be an independent predictive factor for the occurrence of cerebral vasospasm, DCI, and poor outcome after aneurysmal SAH in a clinical setting [6]. In experimental SAH, TLR4 was also activated in neurons, microglia cells, and capillary endothelial cells [7] as well as in the endothelial and smooth muscle cells of spastic basilar artery [8]. TLR4 is activated by many endogenous ligands, such as heme, fibrinogen, matricellular protein tenascin-C, intracellular components of ruptured cells, and products of genes that are activated by inflammation, which are produced after SAH [5, 9–11]. TLR4 signaling activates nuclear factor (NF)-κB transcription factors and mitogen-activated protein kinases, leading to upregulation of many inflammatory mediators [12]. Some pharmaceutical agents actually reduced experimental vasospasm associated with downregulation of TLR4 and the various downstream inflammatory mediators [13–15]. In addition, our recent study showed that a selective TLR4 antagonist inhibited tenascin-C-induced constriction of cerebral arteries as well as TLR4 expression in the endothelial and smooth muscle cells of the arteries in healthy rats [11]. Taken together, previous findings suggest that TLR4 signaling in the endothelial and smooth muscle cells of cerebral arteries play a pivotal role in the development of cerebral vasospasm, although there are many kinds of Toll-like receptors expressing in the central nervous system [16]. However, the role of TLR4 in cerebral vasospasm remains indistinct, because the effects of selective blockage of TLR4 have never been investigated. Hanafy [17] reported that TLR4 knockout suppressed cerebral vasospasm in a prechiasmatic cistern blood injection model in mice, but this study examined neither the effects of TLR4 knockout on post-SAH neurological impairments nor the role of TLR4 expression in cerebral arteries. Thus, the aim of this study was to examine if selective TLR4 antagonists prevent cerebral vasospasm development and neurological impairments in an established endovascular perforation model of SAH in mice [18]. In this study, cyclooxygenases (COXs) were also investigated in cerebral arteries as a downstream inflammatory mediator of TLR4 signaling pathway, because COXs may be responsible for cerebral vasospasm via multiple mechanisms [19, 20].
Materials and Methods
All procedures were approved by the Animal Ethics Review Committee of Mie University and were in accordance with the institution’s Guidelines for Animal Experiments.
SAH Model and Study Protocol
The endovascular perforation model of SAH was produced in C57BL/6 mice (male; weight, 25–30 g) as previously described [18]. Each animal was anesthetized by an intraperitoneal injection of tribromoethanol (250 μg/g body weight). A sharpened 4–0 monofilament nylon suture was advanced rostrally into the left internal carotid artery (ICA) from the external carotid artery stump to perforate the bifurcation of the left anterior (ACA) and middle cerebral arteries (MCA). Blood pressure and heart rate were measured noninvasively from the tail. Sham-operated mice underwent identical procedures except that the suture was withdrawn without puncture.
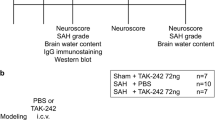
First, 114 mice underwent endovascular perforation SAH or sham operation. At 30 min after surgery, 86 surviving mice were randomly divided into 6 groups (sham+phosphate-buffered saline [PBS; n = 15], sham+LPS-RS 8 μg [n = 3], sham+LPS-RS 40 μg [n = 3], SAH+PBS [n = 30], SAH+LPS-RS 8 μg [n = 7], and SAH+LPS-RS 40 μg [n = 28]), and a selective TLR4 antagonist, LPS-RS ultrapure (InvivoGen, San Diego, CA) or vehicle (PBS), was administered intracerebroventricularly. Cerebral vasospasm was evaluated by means of neurobehavioral tests and India-ink angiography at 24–48 h, and Western blotting and immunohistochemistry at 24 h post-SAH.
Second, to confirm the involvement of TLR4 in the development of vasospasm, another selective TLR4 antagonist, IAXO-102 (Adipogen, San Diego, CA), was administered intracerebroventricularly to 6 surviving SAH mice at 30 min post-SAH, and the effects were compared with those in the SAH+PBS mice. Vasospasm was evaluated by neurobehavioral tests, India-ink angiography, and immunohistochemistry at 24 h post-SAH. IAXO-102 was also administered intracerebroventricularly to 3 sham-operated mice at 30 min post-surgery, whose effects were compared with those in the sham+PBS mice by means of neurobehavioral tests and India-ink angiography at 24 h post-surgery.
Severity of SAH
The severity of SAH was assessed blindly at each sacrifice as previously described [21]. The basal cistern was divided into six segments, and each segment was allotted a grade from 0 to 3 depending on the amount of SAH. The animals received a total score ranging from 0 to 18 by summing the scores.
Intracerebroventricular Infusion
The intracerebroventricular infusion was performed by a modification of the method previously described [18]. The needle of a 2-μL Hamilton syringe (Hamilton Company, Reno, Nev) was inserted through a burr hole into the left lateral ventricle using the following coordinates relative to the bregma: 0.2 mm posterior, 1.0 mm lateral, and 2.2 mm below the horizontal plane of the bregma. Vehicle (PBS, 2 μL) or TLR4 antagonists (8 or 40 μg LPS-RS ultrapure in 2-μL vehicle; and 117 ng IAXO-102 in 2-μL vehicle) were infused at a rate of 0.5 μL/min irrespective of the animal’s body weight. The needle was removed 10 min after an infusion, and the wound was quickly sutured.
Each dosage of the drugs was calculated on the basis of a previous report [11] and each drug’s datasheet. In our previous study, 200 μg LPS-RS was injected into the cisterna magna in rats and completely inhibited cerebral arterial constriction by tenascin-C [11]. As the cerebrospinal fluid (CSF) volume of mice is considered to be 1/4 to 1/9 of that of rats [22], 22 to 50 μg LPS-RS may be enough to get an equivalent CSF LPS-RS concentration in mice. Thus, 8 and 40 μg of LPS-RS ultrapure dissolved in 2 μL of PBS was selected in this study. The dosage of IAXO-102 was calculated for working concentrations of 5 μmol/L on the basis of the datasheet: 117 ng of IAXO-102 was dissolved in 0.02 μL of 50 % dimethyl sulfoxide and ethanol (volume ratio = 1:1), diluted 100 times in 1.98 μL of PBS (final concentration of dimethyl sulfoxide and ethanol = 0.5 %, respectively) and injected to achieve an equivalent CSF concentration of IAXO-102 in mice, whose total CSF volume is presumed to be 40 μL [23].
Neurobehavioral Test
Neurological scores (3–18 points) were assessed by summing up six test scores (spontaneous activity, spontaneous movement of four limbs, forepaw outstretching, climbing, body proprioception, and response to whisker stimulation) as previously described [21].
India-Ink Angiography
Gelatin–India-ink solution was made by dissolving gelatin powder (7 g) in 100 mL PBS and mixing with 100 mL India ink (Kuretake Co., Nara, Japan) [24]. The ascending aorta was cannulated with a blunted 18-gauge needle attached to flexible plastic tubing, which was connected to a pressure transducer (Nihon Kohden Co., Tokyo, Japan) and a syringe on an automatic infusion pump. After an incision was made in the right atrium to allow for the outflow of perfusion solution, 50 mL of PBS, 15 min of 10 % formalin, and 10 min of 3.5 % gelatin–India-ink solution were infused through the closed circuit. All perfusates were passed through a 0.2-μm pore filter and delivered at 60–80 mmHg [24]. Then, the mouse was refrigerated at 4 °C for 24 h to allow gelatin solidification. The brains were harvested and stored in 10 % neutral-buffered formalin for immunohistochemistry after high-resolution images of the circle of Willis and basilar arteries (BAs) were taken with a scale. An experienced person who was unaware of the treatment groups measured the smallest lumen diameter within each vascular segment of intracranial cerebral arteries (sphenoidal segment of the MCA, precommunicating segment of the ACA, intradural ICA, and BA) three times using Image J software (National Institutes of Health, Bethesda, MD) and determined the mean value per segment.
Western Blot Analyses
Western blot analyses were performed as previously described [24]. The circle of Willis and BAs was harvested under a microscope and homogenized. Equal amounts of protein samples (1 μg) were loaded on SDS-PAGE gels, electrophoresed, and transferred onto a polyvinylidene difluoride membrane. The membranes were blocked with 2 % bovine serum albumin, followed by incubation overnight at 4 °C with the rabbit polyclonal anti-TLR4 antibody (1:800; Bioss, Woburn, MA), rabbit polyclonal anti-phosphorylated TLR4 (1:2000; ThermoFisher, Waltham, MA), rabbit polyclonal anti-cyclooxygenase-1 (COX1) (1:200, Abnova, Buckingham, MK), and rabbit polyclonal anti-cyclooxygenase-2 (COX2) (1:500, Proteintech, Rosemont, IL) antibodies. Blot bands were detected with a chemiluminescence reagent kit (ECL Plus; Amersham Bioscience, Arlington Heights, IL) and quantified by densitometry with Image J software. β-tubulin (1:1000; Santa Cruz Biotechnology, Santa Cruz, CA) was blotted onto the same membrane as a loading control.
Immunohistochemistry
The stored brains after India-ink angiography were used. Immunohistochemistry was performed for formalin-fixed paraffin-embedded sections as described previously [11]. Four micron-thick coronal sections at 1.0 mm posterior to bregma were cut. After dewaxing and rehydration, the sections were treated with 3 % hydrogen peroxide for 10 min to block endogenous peroxidase activities, placed in 1 mmol ethylenediaminetetraacetic acid (pH 8.0) and heated in an autoclave at 121 °C for 1 min. The sections were then blocked with 5 % goat or horse serum and incubated overnight at 4 °C with the rabbit polyclonal anti-phosphorylated TLR4 (1:2000; ThermoFisher) and rabbit polyclonal COX1 (1:25, Abnova) antibodies. They were subsequently incubated with biotinylated anti-rabbit immunoglobulin (Vector Laboratories, Burlingame, CA) for 30 min and then with an avidin–biotin complex for 30 min at room temperature. Color reactions were developed in diaminobenzidine/hydrogen peroxide solution and the sections were counterstained with hematoxylin solution for light microscopic examination. Negative controls consisted of serial sections incubated with buffer alone instead of the primary antibodies.
Hematoxylin and eosin (HE) staining was also performed to examine the morphology of cerebral arteries.
Statistics
In the statistical analysis, we calculated the power of the tests. The number of animals per group necessary to reach the desired power of 0.800 was in the range of 4 to 6 in SAH mice. Mortality was compared by chi-square tests. SAH grade and neurological scores were expressed as the median ± 25th–75th percentiles and were analyzed using the Mann–Whitney U test or Kruskal–Wallis test, followed by Steel–Dwass multiple comparisons. Other values were expressed as the mean ± standard deviation, and unpaired t test or one-way analysis of variance (ANOVA) with Student–Newman–Keuls post hoc tests was used as appropriate. P < 0.05 was considered significant.
Results
Post-SAH LPS-RS Ultrapure Prevents Vasospasm
Comparisons of physiological parameters revealed no significant differences among the groups (data not shown). None of 21 sham-operated mice died within the 48-h observation period. Twenty-eight (30.1 %) of 93 SAH mice died within 30 min after surgery and before the drug injection. The mortality of SAH mice after randomization into each treatment group was not significantly different among the PBS (13.3 %, 4 of 30 mice), 8 μg (14.3 %, 1 of 7 mice), and 40 μg (7.1 %, 2 of 28 mice) of LPS-RS ultrapure groups (chi-square tests). The median SAH grading score was similar among the groups in each analysis at both 24 and 48 h post-SAH (Fig. 1 upper). Among surviving animals, 2 PBS-treated and 2 40 μg of LPS-RS ultrapure-treated SAH mice were not used for further analysis, because their SAH grading scores were mild and 7 or less at 24 h [21].
Effects of Toll-like receptor 4 antagonist LPS-RS ultrapure treatment on the severity of subarachnoid hemorrhage (SAH; upper) and neurological scores (lower) at 24 h (left) and 48 h (right) post-SAH. PBS phosphate-buffered saline; data, median ± 25th–75th percentiles; *P < 0.01, **P < 0.05, Kruskal–Wallis tests
LPS-RS ultrapure injections did not cause neurological impairments in sham-operated animals (Online Resource, Figure S1). Neurological scores at 24 h were significantly impaired after SAH in comparison with the sham groups (Fig. 1 lower left). Post-SAH administration of 40 μg but not 8 μg LPS-RS ultrapure significantly improved neurological scores compared with the SAH+PBS group (Kruskal–Wallis test). The neuroprotective effect was also shown at 48 h post-SAH (Fig. 1 lower right).
LPS-RS ultrapure injections had no effects on the vessel diameter of cerebral arteries in sham-operated animals (Online Resource, Figure S2). Higher dosages but not lower dosages of LPS-RS ultrapure significantly attenuated post-SAH vasospasm in the left ACA, MCA, ICA, and right MCA at both 24 and 48 h post-SAH compared with the SAH+PBS group (ANOVA; Fig. 2, and Online Resource, Figure S3).
Effects of Toll-like receptor 4 antagonist LPS-RS ultrapure treatment on cerebral vasospasm at 24 h after subarachnoid hemorrhage (SAH). a Representative India-ink angiograms (lower magnification of upper square areas). b Vessel diameter of each cerebral artery. Thick arrow, anterior cerebral artery; arrowhead, middle cerebral artery; thin arrow, internal carotid artery; PBS phosphate-buffered saline; data, mean ± standard deviation; *P < 0.01, **P < 0.05, ANOVA
Effects of LPS-RS Ultrapure on Protein Expression Changes in Cerebral Arteries After SAH
Western blot analyses showed that SAH significantly increased phosphorylated TLR4 levels in the spastic cerebral arteries compared with the sham-operated animals, although expression levels of TLR4 were not significantly changed (Fig. 3). SAH also increased COX1 levels compared with the sham animals (Fig. 3). Higher dosages of LPS-RS ultrapure significantly suppressed expression levels of both phosphorylated TLR4 and COX1 in the post-SAH cerebral arteries. COX2 levels were not significantly changed by SAH or LPS-RS ultrapure.
Representative Western blots (a) and effects of Toll-like receptor 4 (TLR4) antagonist LPS-RS ultrapure treatment on expression of TLR4 (b), phosphorylated TLR4 (p-TLR4) (c), cyclooxygenase-1 (COX1) (d), and cyclooxygenase-2 (COX2) (e) in cerebral arteries at 24 h after subarachnoid hemorrhage (SAH). Expression levels of each protein are expressed as a ratio of β-tubulin levels for normalization and as the mean ± standard deviation. PBS phosphate-buffered saline; *P < 0.05, ANOVA
Immunohistochemistry of the intracranial ICA showed that both phosphorylated TLR4 and COX1 were increased mainly in the endothelial and smooth muscle cells of the spastic cerebral arteries in the SAH+PBS group. These immunoreactivities were attenuated in the SAH+LPS-RS 40-μg group (Fig. 4).
Effects of Toll-like receptor 4 (TLR4) antagonist LPS-RS ultrapure treatment on immunohistochemical staining of the intracranial internal carotid artery at 24 h after subarachnoid hemorrhage (SAH). HE hematoxylin and eosin, p-TLR4 phosphorylated TLR4, COX1 cyclooxygenase-1, PBS phosphate-buffered saline. Arrowhead, immunoreactive endothelial cell; arrow, immunoreactive smooth muscle cell
Effects of Another TLR4 Antagonist IAXO-102 on Vasospasm
Comparisons of physiological parameters revealed no significant differences among the groups (data not shown). Two (25 %) of 8 SAH mice died within 30 min after surgery and before the drug injection. The mortality of SAH mice after randomization into either treatment group was not significantly different between the PBS (13.3 %, 4 of 30 mice) and IAXO-102 (0 %, 0 of 6 mice) groups (chi-square tests). The median SAH grading score was similar between the groups (Fig. 5a).
Effects of Toll-like receptor 4 antagonist IAXO-102 treatment on the severity of subarachnoid hemorrhage (SAH) (a), neurological scores (b), and cerebral vasospasm (representative India-ink angiograms: lower magnification of upper square areas (c), vessel diameter of the left intracranial internal carotid artery (d)) at 24 h post-SAH. PBS phosphate-buffered saline; data, median ± 25th–75th percentiles (a, b) or mean ± standard deviation (d); *P < 0.01, Mann–Whitney U test; **P < 0.05, unpaired t test; thick arrow, anterior cerebral artery; arrowhead, middle cerebral artery; thin arrow, internal carotid artery
IAXO-102 injections had no effects on neurological scores and vessel diameters of cerebral arteries in sham-operated animals at 24 h post-injection (Online Resource, Figures S4 and S5). Post-SAH administration of IAXO-102 significantly improved both neurological scores (Mann–Whitney U test) and vasospasm (unpaired t test) compared with the SAH+PBS group (Fig. 5 and Online Resource, Figure S6).
Immunohistochemistry of the intracranial ICA also showed that IAXO-102 attenuated post-SAH vasospasm, associated with the suppression of post-SAH TLR4 activation and COX1 upregulation in the endothelial and smooth muscle cell layers of the cerebral arteries (Fig. 6).
Effects of Toll-like receptor 4 (TLR4) antagonist IAXO-102 treatment on immunohistochemical staining of the intracranial internal carotid artery at 24 h after subarachnoid hemorrhage (SAH). HE hematoxylin and eosin, p-TLR4 phosphorylated TLR4, COX1 cyclooxygenase-1, PBS phosphate-buffered saline. Arrowhead, immunoreactive endothelial cell; arrow, immunoreactive smooth muscle cell
Discussion
The novel findings of the present study are as follows: (1) SAH induced TLR4 activation and COX1 upregulation in the endothelial and smooth muscle cell layers of the spastic cerebral arteries in a mouse endovascular perforation model, (2) two kinds of selective TLR4 antagonists suppressed post-SAH COX1 upregulation as well as TLR4 activation in the cerebral artery, and (3) two kinds of selective TLR4 antagonists prevented cerebral vasospasm and neurological impairments after SAH. These findings suggest that post-SAH TLR4 activation causes cerebral vasospasm and neurological impairments at least partly via COX1 upregulation, which is effectively inhibited by TLR4 antagonists.
TLR4-mediated NF-κB signaling pathway is increasingly recognized to play a vital role in the initiation of cerebral inflammation in central nervous system diseases [25]. NF-κB is a transcriptional factor required for the gene expression of many inflammatory mediators, such as interleukin (IL)-1β, tumor necrosis factor (TNF)-α, IL-6, intercellular adhesion molecule (ICAM)-1, and monocyte chemoattractant protein (MCP)-1 [12]. TLR4 is expressed in various cell types in the central nervous system, including microglia, neurons, astrocytes and capillary endothelial cells in brain, endothelial and smooth muscle cells in cerebral artery, and in peripheral blood cells, such as leukocytes, macrophages, and platelets [5, 7, 8]. In aneurysmal SAH patients, higher TLR4 levels on peripheral blood mononuclear cells were an independent predictive factor for cerebral vasospasm and poor outcome [6]. In cultured vascular smooth muscle cells from rat aorta, oxyhemoglobin induced TLR4 expression and TNF-α production [26]. In experimental SAH, expression of TLR4 was increased in the endothelial and smooth muscle cells of basilar artery with vasospasm in a rabbit double blood injection model into the cisterna magna [8]. Peroxisome proliferator-activated receptor gamma agonist rosiglitazone reduced SAH-mediated upregulation of TLR4 and increased production of myeloperoxidase and ICAM-1, and attenuated vasospasm in the basilar artery in a rat double hemorrhage model into the cisterna magna [15]. Ursolic acid, a natural pentacyclic triterpenoid acid, reduced proinflammatory mediators such as TNF-α, IL-1β, IL-6, ICAM-1, inducible nitric oxide (NO) synthase, and matrix metalloproteinase-9 possibly by suppressing TLR4 and NF-κB in post-SAH cerebral cortex, and prevented vasospasm in the basilar artery in a rat SAH model by endovascular perforation [13]. Glycyrrhizin, a traditional herbal remedy, also prevented TLR4 upregulation and vasospasm in the basilar artery associated with suppression of cytokine levels in the cerebrospinal fluid such as IL-1β, IL-6, IL-8, and MCP-1 in a rat model of SAH by a single blood injection into the cisterna magna [14]. In addition, TLR4 knockout suppressed cerebral vasospasm and neuronal apoptosis in a prechiasmatic cistern blood injection model in mice: the early phase was dependent on myeloid differentiation primary response gene pathway, while the late phase was dependent on Toll receptor-associated activator of interferon pathway [17]. In the study, microglial TLR4 receptor was necessary for vasospasm development possibly via TNF-α induction [17]. In this study, two kinds of selective TLR4 antagonists, LPS-RS ultrapure that inhibits the interaction of MD-2 with TLR4 [27] and IAXO-102 that interferes selectively with the TLR4 co-receptors CD14 and MD-2 [28], were used, and it was first demonstrated that selective blockage of TLR4 could effectively prevent post-SAH cerebral vasospasm and neurological impairments as well as COX1 upregulation in cerebral arteries in a clinically relevant endovascular perforation model in mice. The endovascular perforation model mimics clinical mechanism of artery rupture and shows a high mortality and acute metabolic changes similar to clinical findings, thus being the most attractive model for studies of pathophysiology after SAH [29].
COXs catalyze the conversion of arachidonic acid to prostaglandin H2, which is further converted to many prostaglandins and thromboxanes. Various arachidonic acid metabolites, including thromboxane A2, prostaglandin F2α, and prostacyclin, contribute to endothelium-dependent contractions that are ultimately attributable to activation of thromboxane–prostanoid receptors of the vascular smooth muscle [30]. Thus, COXs may cause vasospasm by producing vasoconstrictor arachidonic acid metabolites [19]. In addition, COXs have other actions potentially causing cerebral vasospasm: (1) COXs may be involved in the mechanism of vascular endothelial dysfunction, especially in a disturbance in cross-talk between endothelin (ET)-1 and NO, causing vasospasm [20] and (2) COXs may induce phenotypic modulation of vascular smooth muscle cells or vascular remodeling [31], playing a role in vasospasm development [32]. COXs can be divided into two isoforms, COX1 and COX2. Whereas the expression and/or presence of COX1 is usually stable under most experimental conditions, COX2 can be induced or upregulated by a number of stimuli, in particular cytokines [33]. In experimental SAH, only COX2 was examined and has been reported to play an important role in the pathogenesis of vasospasm [20]. A recent study reported that COX2 induction was mainly observed in the endothelial cells of rabbit basilar artery after SAH, associated with upregulation of ET-1 and ETA receptor expression and downregulation of endothelial NO synthase expression, possibly causing endothelial cell dysfunction and thereby vasospasm [20]. However, COX1 is the major source of endothelium-derived contracting factors, and the exposure of the endothelial cells to high glucose results in increased oxidative stress and overexpression of both COX1 and COX2 in the arteries of normotensive diabetic animals [34]. TLR4-induced COX1 activation was also responsible for endothelial dysfunction and augmented endothelium-derived contracting factor-mediated contractions in carotid arteries of obese and diabetic mice [35]. This study first showed that COX1 was induced in cerebral arteries after SAH and that TLR4 antagonists suppressed both post-SAH COX1 induction and vasospasm, suggesting the involvement of COX1 induction in cerebral vasospasm development.
This study is somewhat limited. First, the degree of vasospasm in mice is less severe compared with that in large animal models; therefore, the effects of TLR4 antagonists should be confirmed using large animal models. Secondly, only an immediate post-SAH intracerebroventricular injection of TLR4 antagonists was tested and showed that the TLR4 antagonists attenuated vasospasm and neurological impairments effectively. To be more translational, the effects of single or multiple systemic administrations at different dosages or time courses on vasospasm and brain injury as well as long-term functional outcomes should be examined in future preclinical evaluations. Thirdly, this study demonstrated that TLR4 antagonists prevented vasospasm via inhibiting COX1 upregulation. However, we cannot exclude the possibility that TLR4 inactivation prevented vasospasm without the involvement of COX1. In addition, neither ligands that activated TLR4 nor the exact mechanism of how TLR4 inactivation reduced arterial smooth muscle contraction is missing in this study. Thus, further studies are needed.
In conclusion, this study showed that TLR4-COX1 signaling pathway could be a promising therapeutic target for post-SAH vasospasm, which was effectively inhibited by selective TLR4 antagonists. The findings of this study warrant further studies.
Abbreviations
- ACA:
-
Anterior cerebral artery
- ANOVA:
-
Analysis of variance
- BA:
-
Basilar artery
- COX:
-
Cyclooxygenase
- COX1:
-
Cyclooxygenase-1
- COX2:
-
Cyclooxygenase-2
- CSF:
-
Cerebrospinal fluid
- DCI:
-
Delayed cerebral ischemia
- ET:
-
Endothelin
- HE:
-
Hematoxylin and eosin
- ICA:
-
Internal carotid artery
- ICAM:
-
Intercellular adhesion molecule
- IL:
-
Interleukin
- MCA:
-
Middle cerebral artery
- MCP:
-
Monocyte chemoattractant protein
- NO:
-
Nitric oxide
- PBS:
-
Phosphate-buffered saline
- NF:
-
Nuclear factor
- SAH:
-
Subarachnoid hemorrhage
- TLR4:
-
Toll-like receptor 4
- TNF:
-
Tumor necrosis factor
References
Taki W, Sakai N, Suzuki H, Prospective Registry of Subarachnoid Aneurysms Treatment (PRESAT) group (2011) Determinants of poor outcome following aneurysmal subarachnoid hemorrhage when both clipping and coiling are available: PRESAT in Japan. World Neurosurg 76:437–445
Keyrouz S, Diringer M (2007) Clinical review: prevention and therapy of vasospasm in subarachnoid hemorrhage. Crit Care 11:220. doi:10.1186/cc5958
Suzuki H (2015) What is early brain injury? Transl Stroke Res 6:1–3
Crowley RW, Medel R, Dumont AS, Ilodigwe D, Kassell NF, Mayer SA, Ruefenacht D, Schmiedek P et al (2011) Angiographic vasospasm is strongly correlated with cerebral infarction after subarachnoid hemorrhage. Stroke 42:919–923
Fang H, Wang PF, Zhou Y, Wang YC, Yang QW (2013) Toll-like receptor 4 signaling in intracerebral hemorrhage-induced inflammation and injury. J Neuroinflammation 10:27. doi:10.1186/1742-2094-10-27
Ma C, Zhou W, Yan Z, Qu M, Bu X (2015) Toll-like receptor 4 (TLR4) is associated with cerebral vasospasm and delayed cerebral ischemia in aneurysmal subarachnoid hemorrhage. Neurol Med Chir (Tokyo) 55:878–884
Zhang T, Su J, Guo B, Wang K, Li X, Liang G (2015) Apigenin protects blood-brain barrier and ameliorates early brain injury by inhibiting TLR4-mediated inflammatory pathway in subarachnoid hemorrhage rats. Int Immunopharmacol 28:79–87
Zhou ML, Wu W, Ding YS, Zhang FF, Hang CH, Wang HD, Cheng HL, Yin HX et al (2007) Expression of Toll-like receptor 4 in the basilar artery after experimental subarachnoid hemorrhage in rabbits: a preliminary study. Brain Res 1173:110–116
Johnson GB, Brunn GJ, Platt JL (2003) Activation of mammalian Toll-like receptors by endogenous agonists. Crit Rev Immunol 23:15–44
Suzuki H, Kawakita F (2016) Tenascin-C in aneurysmal subarachnoid hemorrhage: deleterious or protective? Neural Regen Res 11:230–231
Fujimoto M, Suzuki H, Shiba M, Shimojo N, Imanaka-Yoshida K, Yoshida T, Kanamaru K, Matsushima S et al (2013) Tenascin-C induces prolonged constriction of cerebral arteries in rats. Neurobiol Dis 55:104–109
Lee SJ, Lee S (2002) Toll-like receptors and inflammation in the CNS. Curr Drug Targets Inflamm Allergy 1:181–191
Zhang T, Su J, Guo B, Zhu T, Wang K, Li X (2014) Ursolic acid alleviates early brain injury after experimental subarachnoid hemorrhage by suppressing TLR4-mediated inflammatory pathway. Int Immunopharmacol 23:585–591
Chang CZ, Wu SC, Kwan AL (2014) Glycyrrhizin attenuates Toll like receptor-2, -4 and experimental vasospasm in a rat model. J Immunol Res 2014:740549. doi:10.1155/2014/740549
Wu Y, Tang K, Huang RQ, Zhuang Z, Cheng HL, Yin HX, Shi JX (2011) Therapeutic potential of peroxisome proliferator-activated receptor γ agonist rosiglitazone in cerebral vasospasm after a rat experimental subarachnoid hemorrhage model. J Neurol Sci 305:85–91
Paschon V, Takada SH, Ikebara JM, Sousa E, Raeisossadati R, Ulrich H, Kihara AH (2016) Interplay between exosomes, microRNAs and Toll-like receptors in brain disorders. Mol Neurobiol 53:2016–2028
Hanafy KA (2013) The role of microglia and the TLR4 pathway in neuronal apoptosis and vasospasm after subarachnoid hemorrhage. J Neuroinflammation 10:83. doi:10.1186/1742-2094-10-83
Altay O, Suzuki H, Hasegawa Y, Caner B, Krafft PR, Fujii M, Tang J, Zhang JH (2012) Isoflurane attenuates blood-brain barrier disruption in ipsilateral hemisphere after subarachnoid hemorrhage in mice. Stroke 43:2513–2516
Sasaki T, Murota SI, Wakai S, Asano T, Sano K (1981) Evaluation of prostaglandin biosynthetic activity in canine basilar artery following subarachnoid injection of blood. J Neurosurg 55:771–778
Munakata A, Naraoka M, Katagai T, Shimamura N, Ohkuma H (2016) Role of cyclooxygenase-2 in relation to nitric oxide and endothelin-1 on pathogenesis of cerebral vasospasm after subarachnoid hemorrhage in rabbit. Transl Stroke Res 7:220–227
Sugawara T, Ayer R, Jadhav V, Zhang JH (2008) A new grading system evaluating bleeding scale in filament perforation subarachnoid hemorrhage rat model. J Neurosci Methods 167:327–334
Zappaterra MW, LaMantia AS, Walsh CA, Lehtinen MK (2013) Isolation of cerebrospinal fluid from rodent embryos for use with dissected cerebral cortical explants. J Vis Exp 73:e50333
Yaksh TL (1999) Spinal cerebrospinal fluid chemistry and physiology. In: Artru AA (ed) Spinal drug delivery, 1st Ed. Elsevier, Amsterdam, pp. 216–217
Suzuki H, Hasegawa Y, Chen W, Kanamaru K, Zhang JH (2010) Recombinant osteopontin in cerebral vasospasm after subarachnoid hemorrhage. Ann Neurol 68:650–660
Buchanan MM, Hutchinson M, Watkins LR, Yin H (2010) Toll-like receptor 4 in CNS pathologies. J Neurochem 114:13–27
Wu Y, Zhao XD, Zhuang Z, Xue YJ, Cheng HL, Yin HX, Shi JX (2010) Peroxisome proliferator-activated receptor gamma agonist rosiglitazone attenuates oxyhemoglobin-induced Toll-like receptor 4 expression in vascular smooth muscle cells. Brain Res 1322:102–108
Visintin A, Halmen KA, Latz E, Monks BG, Golenbock DT (2005) Pharmacological inhibition of endotoxin responses is achieved by targeting the TLR4 coreceptor, MD-2. J Immunol 175:6465–6472
Peri F, Piazza M, Calabrese V, Damore G, Cighetti R (2010) Exploring the LPS/TLR4 signal pathway with small molecules. Biochem Soc Trans 38:1390–1395
Titova E, Ostrowski RP, Zhang JH, Tang J (2009) Experimental models of subarachnoid hemorrhage for studies of cerebral vasospasm. Neurol Res 31:568–581
Vanhoutte PM (2011) Endothelium-dependent contractions in hypertension: when prostacyclin becomes ugly. Hypertension 57:526–531
Mukherjee K, Gitlin JM, Loftin CD (2012) Effectiveness of cyclooxygenase-2 inhibition in limiting abdominal aortic aneurysm progression in mice correlates with a differentiated smooth muscle cell phenotype. J Cardiovasc Pharmacol 60:520–529
Shimamura N, Ohkuma H (2014) Phenotypic transformation of smooth muscle in vasospasm after aneurysmal subarachnoid hemorrhage. Transl Stroke Res 5:357–364
Flavahan NA (2007) Balancing prostanoid activity in the human vascular system. Trends Pharmacol Sci 28:106–110
Vanhoutte PM (2009) COX-1 and vascular disease. Clin Pharmacol Ther 86:212–215
Liang C-F, Liu JTC, Wang Y, Xu A, Vanhoutte PM (2013) Toll-like receptor 4 mutation protects obese mice against endothelial dysfunction by decreasing NADPH oxidase isoforms 1 and 4. Arterioscler Thromb Vasc Biol 33:777–784
Acknowledgments
We thank Ms. Chiduru Yamamoto (Department of Neurosurgery, Mie University Graduate School of Medicine) for her technical assistance. This work was supported by a Grant-in-Aid for Scientific Research from SENSHIN Medical Research Foundation to Dr. Suzuki, and Japan Society for the Promotion of Science to Dr. Fujimoto.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was funded by a Grant-in-Aid for Scientific Research from SENSHIN Medical Research Foundation to Dr. Suzuki, and Japan Society for the Promotion of Science to Dr. Fujimoto.
Conflict of Interest
The authors declare that they have no conflict of interest.
Research Involving Animals
All procedures were approved by the Animal Ethics Review Committee of Mie University and were carried out according to the institution’s Guidelines for Animal Experiments.
Electronic supplementary material
ESM 1
(PDF 4714 kb)
Rights and permissions
About this article
Cite this article
Kawakita, F., Fujimoto, M., Liu, L. et al. Effects of Toll-Like Receptor 4 Antagonists Against Cerebral Vasospasm After Experimental Subarachnoid Hemorrhage in Mice. Mol Neurobiol 54, 6624–6633 (2017). https://doi.org/10.1007/s12035-016-0178-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-016-0178-7