Abstract
Regulatory T cells (Tregs) are increased in peripherally circulating blood cells and in the solid tumor masses of patients afflicted with many different cancer histologies. Cancer Tregs not only are capable of impeding endogenous protective anti-tumor immunity from optimal functioning but are also capable of impeding the efficacy of anti-cancer immunotherapy. Tumor-associated Tregs represent heterogeneous populations, differing by their origins and in their mechanisms used to impede anti-tumor immunity. Their properties can differ compared to those in peripheral circulation. Most studies now report that Treg content in the tumor inversely correlates with survival or therapeutic response, but a few reports suggest that Tregs are beneficial to patients with certain types of cancers. Therapeutic strategies to manage Treg capacity to mediate immune dysfunction include depletion, regulatory functional blockade, differentiation blockade, altering trafficking, differentiation diversion, or raising the threshold of anti-cancer effector cells for Treg-mediated regulation. Several clinical trials have shown the feasibility and relative safety of managing Tregs in human cancer, although treatment effects are modest. This chapter will review contemporary knowledge of Tregs in cancers, including origins, mechanisms of action, interactions with other immune cells and strategies for therapeutic management, addresses the major questions facing the field and suggests additional important areas for future research. The focus is on CD4+CD25+Foxp3+ Tregs, but other cancer-associated regulatory cells will be addressed in brief.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Malignancies post significant immunologic challenges for the host. On the one hand, they are antigenic and pathological, and should thus be amenable to immune destruction. On the other hand, irrespective of how abnormal the malignant cells have become, they nonetheless derive from self-tissues. Thus, the powerful host machinery of peripheral tolerance intervenes to prevent autoimmune (anti-tumor) attack indistinguishable from pathologic autoimmunity, consequently impeding what could otherwise be clinically protective anti-tumor immunity. Tumors also employ a devastating array of other immune escape features, discussed below and in detail in other chapters (see especially Chaps. 2, 4, 8, and 10).
Many potentially self-reactive T cells are deleted in the fetal thymus in central tolerance. However, imperfections in central tolerance prevent removal of all potentially self-reactive T cells, some of which enter peripheral tissues including blood, lymph nodes and gut, posing life-long risks for development of autoimmune problems. Those self-reactive T cells not eliminated through central tolerance must thus be dealt with using additional strategies, including peripheral immune tolerance. In peripheral immune tolerance, a potentially autoimmune attack in progress is sensed and inhibited typically before clinically apparent pathologic consequences arise. Sakaguchi and others elegantly showed that a subset of T cells within the CD4+CD25+ population were key mediators of peripheral tolerance1.
Nonetheless, activated T cells, including anti-tumor effector T cells can also express the identical CD4+CD25+ phenotype. Thus, Tregs cannot usually be identified by flow cytometric phenotype alone. We now know that the forkhead/winged helix nuclear transcription factor Foxp3 regulates Treg differentiation and function2–4. Thus, Tregs usually express high Foxp3, although not all Foxp3+ T cells are Tregs5. Additional phenotypic features of Tregs (mouse and human) include high expression of CTLA-4 and GITR, and expression of additional markers including CD62L, CCR7, LAG3, CD103, and others, and low expression of CD127, IL-2, IL-17, and interferon (IFN)-γ6. Nonetheless, these features are also common to many activated non-Treg CD4+ T cells. Appropriate Treg identification with confirmatory functional studies continues to confound interpretations of clinical and preclinical data on potential immunopathogenic functions of Tregs in various settings.
Data derived from small animal models and from human patients have established that Tregs are numerically increased in peripheral blood and the solid tumor masses of epithelial carcinomas, lymphomas and sarcomas, and in lymph nodes draining these tumors7–24. Initial Treg work focused on cells in blood circulation as they were easy and safe to access. Tregs circulate in increased numbers in the blood of patients during the blood phase of their hematologic malignancies, such as in acute myelogenous leukemia25. CD4+CD25+FOXP3+ T cells are found in brain metastases in human melanoma and non-small cell carcinoma, and in metastatic brain lesions in mouse models for breast and colon cancer, and metastatic melanoma26, suggesting that Treg management strategies could also be effective in tumors in the central nervous system. It is now clear that the numbers, phenotypes, and functions of Tregs determined from studies of peripherally circulating cells might not reflect accurately local events in the tumor microenvironment. Immunological and clinical implications of these compartment-specific differences are still incompletely understood.
1.1 Categorizing Tregs
Although Tregs have been categorized in different schemes, a useful and durable concept was proposed by Jeff Bluestone27. In this scheme, Tregs arising in the thymus through homeostatic processes are defined as natural Tregs (nTregs), and are thought primarily to function as mediators of peripheral tolerance against autoimmune attack. Adaptive or induced Treg (iTregs) are induced extrathymically during inflammation or extrathymic T cell activation (including antigen encounter) under tolerizing conditions, likely to help control inflammation, among other functions (Fig. 9.1). nTregs appear to regulate immune processes through direct cell-to-cell contact despite producing IL-10 and TGF-β. iTregs regulate immunity through a variety of mechanisms including both cell-to-cell contact as well as soluble factors, reflecting their heterogeneous origins. nTregs and iTregs are phenotypically indistinguishable despite differences in in vivo function and mechanisms of action, although recently the nuclear transcription factor Helios was reported to identify nTregs relatively exclusively in both mice and humans28. It is not yet clear whether Helios will be useful to distinguish nTregs versus iTregs in inflammatory conditions, such as in cancer. This inability to distinguish nTregs from iTregs has impeded progress in understanding contributions to normal and pathologic process from each. A recent, pivotal study from the Rudensky lab29 describes a mouse deficient in iTreg generation owing to experimental deletion of the CNS1 region of the foxp3 gene that his group showed to be critical for iTreg generation30. These studies confirmed a role for iTregs in regulating inflammation and for nTregs in mediating autoimmune protection, although much additional work is required for a fuller understanding of their physiologic roles in a variety of contexts.
Differentiation and phenotypes of nTregs and iTregs. (a) An uncommitted thymocyte in the thymus receives many instructions regarding its differentiation fate including from T cell receptor (TCR) engagement by antigen, cytokines binding the γc chain (such as IL-2), and other signals to be fully determined such as neighboring thymocytes or stromal cells, or host genetic factors. “X” represents signals yet to be discovered. (b) Early thymic signals begin a differentiation pathway. If the integration of signals induces Foxp3, cells start to differentiate into the Treg pathway and begin to express phenotypic features such as high-level CD25 and CTLA-4. These cells may still express Th2 cytokines such as IL-4, Th17 cytokines such as IL-17 or Tr1 cytokines such as IL-10 but are not suppressive. These cells resemble the TFN cells or Tregs from FILIG mice. (c) Foxp3 expression reinforces its own expression, and in conjunction with continuing and new signals develops the fully developed Treg phenotype with higher CD25 and CTLA-4 expression than in b, suppressive function, reduced Th cytokines, and reduced phosphodiesterase (PDE) 3b. This is now a natural Treg, developing in the thymus and suppressing through contact-dependent mechanisms. It can exit the thymus to circulate or migrate to peripheral lymphoid organs such as lymph nodes and spleen. (d) A Foxp3− thymocyte exiting the thymus can encounter local conditions that induce Foxp3 (such as vascular endothelial growth factor in a tumor) and lead to extrathymic Treg development from this Foxp3− cell, producing adaptive Tregs (ITregs) that can suppress through soluble or contact-dependent mechanisms depending on speficics of their generation. The natural Foxp3+ Treg (nTreg) exiting the thymus (upper right part of lower panels) can encounter additional factors that change its properties as an iTreg. (e) Foxp3 can regulate gene expression either through binding to the forkhead domain (top), induction of regulatory mi-R155 (middle) or in cooperation with NFAT (lower). Additional levels of regulation occur when induced genes then mediate downstream effects. Reproduced from T. Curiel Nature Medicine 13:250–253 2007. Graphic: Katie Ris.
Remarkably, yet predictably, additional Treg subsets have been identified based on functional attributes, including subsets specialized to inhibit specific immune functions such as Th2 or Th17 CD4+ T cell function. An exhaustive review of Treg differentiation pathways and factors was recently published6, which is an excellent reference for additional reading.
2 Properties of Tumor-Associated Tregs
2.1 General Properties
Tumor-associated Tregs are a heterogeneous mix of cells that have developed in distinct developmental pathways from cells arising in various anatomic compartments. They mediate disparate functions through diverse mechanisms as a result, which was the subject of an excellent review31. No definitive reports thus far document the relative contributions of various developmental pathways (such as iTreg versus nTreg) in the various Treg populations of a given tumor. Nonetheless, in a mouse model for cancer, nTregs and iTregs each contribute to tumor tolerance32. The recent generation of iTreg-deficient mice29 will greatly aid further studies.
Tumor-associated Tregs are not typically distinguishable phenotypically from Tregs in other pathologic conditions. That is, tumor Tregs are CD3+ T cells expressing CD4, CD25, GITR, and CTLA-4 among other features common to most Tregs identified to date.
2.2 Tumor-Specific Properties of Tregs
Tumor-associated Tregs also have specific and unique characteristics as a consequence of tumor microenvironment influences. For instance, blood CD4+CD25+FOXP3+ Tregs in prostate cancer patients are more suppressive than comparable cells in blood from control subjects, despite similar total numbers33. Tregs in tumors of some human cancers could be more likely to induce CD8+ effector T cell apoptosis through FasL-mediated interactions34. Tumor-associated TGF-β production promotes local Treg generation from naïve T cells35. A novel population of CD4+CD25−CD69+ Tregs suppressing T cell function through membrane-bound TGF-β was reported in mouse cancer models including melanoma, hepatocellular carcinoma, and lung cancer36. Lack of expression of CD127 (IL-7 receptor α chain) is a feature of functional Tregs in human blood from normal subjects37. CD127 expression in relationship to function is relatively unstudied in tumor Tregs. We found that CD4+CD25+FOXP3+CD127+ and CD4+CD25+FOXP3+CD127− T cells in blood and ascites of ovarian carcinoma patients both contained highly suppressive Tregs (manuscript submitted). Neuropilin-1 expression defines functional Tregs in mice38. A similarly functionally suppressive Neuropilin-1+ population has been described in human cervical cancer39. These cells resided preferentially in lymph nodes draining the tumor and were reduced by cytotoxic chemotherapy in direction relationship to reduction of the tumor mass. Additional differences between homeostatic and tumor-associated Tregs are likely to be described.
Apparent malignancies deriving from Tregs appear to occur, which is not altogether surprising, as hematologic neoplasms derived from essentially all hematopoietic elements have been described. FOXP3 expression is reported in subsets of cutaneous T cell lymphomas. The malignant FOXP3+ T cells have suppressive function in in vitro assays akin to typical CD4+Foxp3+ Tregs40. Mycosis fungoides cells undergoing large cell transformation express FOXP3 along with their clinically aggressive behavior41. In a study of lymphoma patients, FOXP3+ and FOXP3− leukemia/lymphoma cases did not differ by major prognostic factors including tumor stage, patient age, tumor distribution, and concentrations of serum lactate dehydrogenase or serum calcium, and there was no difference in overall survival42.
Recent observations of tumor Tregs suggest that they can promote metastasis in breast cancer through RANK/RANK ligand signals from RANK ligand produced by Tregs interacting with tumor RANK43. Tumor hypoxia can contribute to tumor Treg accumulation through hypoxia-driven CCL28 production44.
3 Issues in Identifying Bona Fide Functional Tumor Tregs
3.1 Functional Testing Issues
As discussed further below, testing the function of putative Treg populations remains the gold standard to confirm Treg identity in specific settings. Further, it is now recognized that tests of Treg function are still limited. A useful distinguishing feature between Tregs and other activated CD4+ T cells is the relative in vitro anergy of the former, despite significant proliferative potential in vivo 45. The classic Shevach assay16 tests the ability of a candidate Treg population to suppress proliferation of naïve T cells in vitro. Although useful, the assay is incomplete as it might not fully or accurately reflect the regulatory properties of that particular Treg population in vivo. For example, Tregs also suppress T cell IL-2 production which can be a major in vivo suppressive mechanism46. Aside from regulating T cell function, Tregs also affect antigen presenting cell function and the effects of various other immune cells (reviewed in 31, 46).
Even with relatively standardized tests, specific aspects of the functional tests can alter findings, leading to differing results and conclusions. For example, T cell receptor signaling strength partly determines the susceptibility of the responder T cells whose proliferative suppression is used to gauge Treg effects in standard in vitro Treg functional tests. Tregs can also exert effects on a specific T cell subset not tested in vitro, among other considerations. We have used Richard Flavell’s FIR mice, in which viable Tregs can be flow cytometrically sorted based on red fluorescence protein expression under foxp3 promoter control47. Bona fide Tregs from FIR mice can be transferred into tumor-bearing mice for specific tests of in vivo effects on tumor growth, tumor-specific immunity, and de novo Treg generation48.
Because human samples are generally limiting, some investigators have tested T cell proliferation in mixed cell populations before and after CD25+ cell depletion as a surrogate for specific Treg testing49. Testing suppression of T cell activation markers in vitro either with Treg addition or CD25+ T cell depletion can give some information about the existence of functional Treg populations while using relatively small quantities of blood. We have shown that malignant human ascites is a good source of functional tumor-associated Tregs8.
3.2 Surrogates for Functional Testing
As numbers of Treg are usually limiting in human tissues, additional techniques that can corroborate Treg identity in human tumors have been investigated. For example, FOXP3 expression identifies functional Tregs in selected human carcinomas50. FOXP3 methylation has been suggested as a way to identify functional Tregs when only small specimen quantities are available51. CD39 expression might distinguish functional Tregs from other T cells expressing the CD4+CD25hi phenotype, including in patients with cancer52. Additional work is required to determine which nonfunctional surrogate tests are adequate for Treg identification in specific conditions. This issue is especially important following immune-based interventions, because treatments can have unexpected and unstudied effects on T cell phenotype that require additional study. Our lab policy is to confirm the functional identity of a potential Treg population in a setting for which such function has not previously been specifically established. We also continue to perform confirmatory functional testing in each experimental animal or human subject to the extent possible to continue to understand how reliable the phenotypic descriptors of potentially functional cell populations are. For example, we have found that interferon-α increased the prevalence of Foxp3+ T cells in mice and humans with ovarian cancer, although these induced Foxp3+ T cells do not necessarily have Treg function (manuscript submitted).
4 Significant Issues in Understanding a Role for Tregs in Tumor Immunopathology
Important questions to address include: (1) What mechanisms induce tumor-associated Tregs? (2) Why are Tregs increased in most cancers? (3) What are the specific roles for specific Treg subsets in tumor immunopathology? (4) What mechanisms do tumor-associated Tregs use to mediate cancer immunopathology? Answering these overarching questions helps understand cancer immunopathology and helps generate tools to develop novel and effective anti-tumor immunotherapies, a goal that has proven relatively elusive thus far.
4.1 Origins of Tumor Tregs
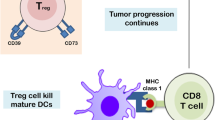
Tregs accumulate in tumors and the patients with them for various reasons including: (i) control of autoimmunity, (ii) control of inflammation, (iii) de novo local differentiation (which means iTreg generation), (iv) recruitment from distant compartments, (v) local proliferation, and (vi) decreased death. Details of these potential mechanisms will be addressed in turn. Specific mechanisms for Treg actions, however, could nonetheless differ by tumor type and perhaps stage, and also could differ based on the anatomic compartment for any given tumor. Figure 9.2 illustrates how many factors generate Tregs at the same time that anti-tumor immunity is generated.
Critical elements of tumor-associated immune dysfunction. Although anti-tumor immunity is elicited as shown in the top half of this figure, active tumor-driven immune dysfunction (red box in bottom half of the figure) thwarts immune cancer elimination. Antigen presenting cells, which in the top half can activate tumor-specific immunity, can also elicit dysfunctional immune cells that turn anti-tumor immunity off, or inhibit it through subversion by tumor factors. Factors responsible for this dysfunction can derive from the tumor itself, or from local stroma or immune cells. These agents include immune suppressive vascular endothelial growth factor (VEGF), transforming growth factor (TGF)-β, and interleukin (IL)-10. These molecules can directly inhibit immunity, such as the ability of TGF-β, IL-10, or VEGF to inhibit T cell activation, or can indirectly elicit other dysfunctional cells. In this latter instance, tumor IL-10 or VEGF can promote antigen presenting cells to express B7-H1, an immune molecule that can directly inhibit T cells, or promote generation of regulatory T cells (Tregs) that inhibit anti-tumor immunity. Tumors can attract Tregs through CCL22, CCL28, and other factors. Novel strategies to overcome these complex and potent tumor-driven active defenses against anti-tumor immunity represent major new opportunities to improve the efficacy of anti-tumor immunotherapy. Figure adapted from Curiel, TJ. Drug Resistance Updates 2012;15(1–2):106–13.
4.1.1 Control of Autoimmunity
The identification of increased Tregs specific for self-antigens is consistent with dysfunctional attempts to control autoimmunity as the basis for their increased numbers. Such normal self-antigen-specific Tregs in cancers have been described for a subset of self-antigens that are also tumor-associated antigens. As an example in humans, Tregs specific for the autoantigens gp100, TRP, NY-ESO-1, and survivin have been described in melanoma53.
4.1.2 Control of Inflammation
Inflammation is a dual-edged sword in cancer. Chronic inflammation contributes to development of some cancers, and cancers generally promote a pro-inflammatory environment54. Thus, it is plausible that some tumor-associated Tregs are iTregs generated or attracted to help control the tumor microenvironmental inflammation. Thus far, described normal Tregs including those isolated from the tumor microenvironment can inhibit production of inflammatory cytokines in vitro. Nonetheless, to my knowledge, Treg accumulation specifically to control tumor-associated inflammation has not yet been formally demonstrated. However, consistent with the concept that Treg-mediated reductions in chronic inflammation can help prevent cancer, in a mouse model for chronic inflammation in the colon, Tregs lowered colorectal cancer incidence by inhibiting local inflammation55. Further, it is now clear that specific Treg subsets have defects in controlling certain types of inflammation29, 56, 57, suggesting that some cancer-driven inflammation could be from reduced iTreg-mediated control, and suggesting possible means for novel therapeutic attack.
4.1.3 Enhanced de Novo Local Differentiation
Some experimental data support the notion that tumor environmental factors can facilitate Treg differentiation locally. Tumor cells can promote Treg differentiation by direct action on T cells, or indirectly by altering local antigen presenting cells, particularly dendritic cells31 and likely other cells as well. Soluble as well as contact-dependent tumor mechanisms that promote local Treg generation have been described. Soluble mediators include cyclooxygenase-2, which is associated with (although not proven to mediate) increased Treg numbers in patients with head and neck cancers58. TGF-β produced by tumor cells differentiates naïve CD4+CD25− T cells into Tregs (iTregs) in mouse models of renal cell carcinoma and prostate cancer35. The human SK-OVCAR3 cell line produces TGF-β that differentiates naïve CD4+CD25− human T cells into Tregs (iTregs) in vitro 59 . Indoleamine 2,3-dioxygenase produced by human leukemia cells (and from other sources) induces Tregs in vitro and in vivo 60. B cell CD70 signals in non-Hodgkin lymphoma can boost FOXP3 expression in naïve human CD4+CD25− T cells in vitro 61. Gal1 from Reed-Sternberg cells in classic Hodgkin lymphoma can facilitate immune suppression directly and also indirectly by helping generate Tregs62. We found that tumor B7-H1 signals contribute to iTreg generation in mice with B16 melanoma48, including sexually dimorphic effects discussed further in Chap. 13. Additional, tumor-associated factors whose identity remains unknown or poorly understood also contribute to tumor Treg generation63, 64.
The tumor can render local cells dysfunctional by promoting generation of iTregs or enhancing their function. For example, plasmacytoid dendritic cells in tumor draining lymph nodes in a mouse cancer model directly activated preexisting Tregs through indoleamine 2,3-dioxygenase production. The suppressive mechanism in this case (B7-H1/PD-1 signaling) is distinct from Tregs activated without indoleamine 2,3-dioxygenase65. Ovarian cancer-derived IL-10 and vascular endothelial growth factor induce dendritic cell B7-H1 expression that generates IL-10 producing Tregs in human ovarian cancer66. Tumor-conditioned human plasmacytoid dendritic cells also can redirect T cell differentiation to either FOXP3+ Tregs or to IL-10+ Tregs67.
The relative importance of individual mechanisms for local cancer Treg generation remains poorly defined and likely will differ by tumor and by anatomic compartment.
4.1.4 Enhanced Recruitment
Different types of tumors produce factors preferentially recruiting local Tregs. The best studied axis is via CCR4 expressed on Tregs and the chemokines CCL17 or CCL22 in the tumor microenvironment (reviewed in 31). Specific examples include Treg attraction in ovarian8 or gastric68 carcinoma via CCL17 or CCL22 signaling. CXCR4+ Tregs might also be attracted to the tumor microenvironment through local CXCL12 production, as preliminarily suggested in malignant mesothelioma69. The cytokine IL-2 is FDA-approved to treat specific cancers including malignant melanoma. However, it is now recognized that therapeutic IL-2 can increase CXCR4 expression on Tregs, increasing their accumulation in ovarian cancer patients70. Whether CXCR4/CXCL12 signaling boosts Treg accumulation in ovarian cancer patients not treated with IL-2 remains to be established. Elements in tumor stroma also might help attract Tregs locally to the tumor microenvironment. For example, tumor-associated macrophages in ovarian cancer secrete the chemokine CCL22 that can attract Tregs locally through a CCR4 interaction8. Local tumor hypoxia can generate CCL28 that attracts Tregs44.
4.1.5 Enhanced Local Proliferation
TGF-β from certain tumors can impede local, myeloid dendritic cell maturation, contributing to local Treg proliferation71. Additional work supports the concept that tumors produce soluble factors and surface-expressed molecules that can promote local Treg proliferation32. Other factors that impede dendritic cell maturation and thus Treg generation, such as vascular endothelial growth factor72, can induce Tregs, but specific effects on Treg proliferation are not reported.
4.1.6 Reduced Local Treg Death
Increased death could be a mechanism to augment Treg accumulation in the tumor microenvironment, but such a mechanism remains to be demonstrated experimentally. There are therapeutic strategies known to increase Treg death locally in the tumor environment73.
4.1.7 Miscellaneous Host Factors
Several models using genetically defined conditions have identified host factors that could alter tumor surveillance or anti-tumor immunity through Treg effects. As an example, IRAK-M−/− mice (lacking IRAK-M, a negative regulator of innate immunity) exhibit increased anti-tumor T cell immunity and reduced Tregs74. B7-H1 T cell cosignaling can generate IL-10+ Tregs in human ovarian cancer66 and female B7-H1−/− mice have reduced Treg function compared to wild-type females75 that is a sexually dimorphic B7-H1 effect on Tregs48. We have recently demonstrated that estrogen regulates B7-H1 T cell co-signaling effects in Treg generation (manuscript submitted) that is further discussed in Chap. 13.
5 Clinical Relevance of Tumor Treg Content
5.1 Treg Content and Prognosis
FOXP3 expression in immune cells in the tumor has been proposed as a prognostic biomarker76. Nonetheless, FOXP3 expression can be transient and/or reversible, thus altering the function of T cells in which it is expressed77, 78. Foxp3+ T cell differentiation is now also known to be highly plastic79. For example, in human ulcerative colitis and colon cancers developing in that setting, FOXP3+ Treg are functionally suppressive, but also produce cytokines not produced by homeostatic Tregs, including TNF-α, IFN-γ, and IL-1780. It is thus unlikely that simple analysis of immune cell or tumor cell Foxp3 content alone will be a highly specific predictive tool without additional information including functional data from FOXP3-expressing cells, the content of other local immune cells, and the anatomic relationships of immune cells to each other and to the tumor, among many additional considerations.
Tumor Treg numbers correlate negatively with survival or treatment response in several studies, including in ovarian cancer8, R0 (fully resected) gastric carcinoma81 and hepatocellular carcinoma82, 83. Intratumoral Foxp3+ T cells positively correlated with local recurrence in the vertical phase of melanoma84.
By contrast, a few studies, notably in hematologic malignancies85, suggest that increased Tregs are beneficial to survival or prognosis. In colorectal cancer, tumor FOXP3+ cell number was positively correlated with survival whereas FOXP3+ cell number in unaffected tissue in the same patients was negatively associated with survival86. In head and neck cancer, tumor Treg positively correlated with regional cancer control87. Studies in experimental animal cancer models provide at least one plausible mechanism by which Tregs function could benefit anti-tumor immunity. In a mouse melanoma model, Tregs augmented anti-tumor immunity, potentially by inhibiting complete tumor eradication. Residual tumor could potentially generate sufficient tumor antigen to stimulate anti-tumor immunity without clinical detrimental effects88. Functionally suppressive FOXP3+ Treg in ulcerative colitis produce TNF-α, IFN-γ, and IL-17 as noted above80 that could promote anti-tumor immunity.
Finally, a few studies show that Treg content conveys no prognostic value including the finding that tumor-infiltrating FOXP3+CD4+CD25+ T cells had no predictive power in renal cell carcinoma89. In anal cancer, Treg cell content was not prognostic90, but patients were studied following radio-chemotherapy treatments, potentially confounding results. The differing conclusions and results in these various studies could owe to a number of factors, including issues discussed above, and those to be addressed below. A recent review of Tregs and prognosis is available76 for additional reading.
5.2 Tregs and Treatment Response
Levels of blood Tregs (CD4+CD25hi T cells) in human cancer patients prior to therapy predicted overall survival after treatment with a dendritic cell vaccine in which some patients were also simultaneously treated with activated T cells91. Reduction of tumor-infiltrating FOXP3+ cells with simultaneous increase in tumor-infiltrating CD8+ cells correlated positively with pathologic complete response after neoadjuvant therapy in human breast cancer92. In prostate cancer patients receiving anti-cancer vaccination plus androgen deprivation, Treg did not predict clinical efficacy93, 94. In head and neck cancer patients with squamous cell carcinomas and no evident disease after conventional treatment, increased peripherally circulating Tregs were more suppressive than in patients not getting similar treatments95, suggesting that therapy boosted numbers and function of suppressive Tregs even while affording a net clinical benefit. If results such as these are confirmed, especially by demonstrating the identity of putative Tregs with functional tests, these data could be useful to help develop algorithms predictive of long-term treatment efficacy, help identify individuals most likely to respond, or help screen out individuals unlikely to benefit from treatments.
5.3 Additional Sources of Confusion in Studies of the Prognostic Significance of Tumor Tregs
Demonstrating Treg function can be difficult, particularly in human tissues as sample size is usually limiting. Consequently, prognostic studies often use FOXP3 expression as a surrogate for functional Tregs, but without doing confirmatory functional testing. Some studies use immunohistochemistry to detect Foxp3+ cells but do not demonstrate that Foxp3+ cells are CD3+ T cells. Such approaches could lead to confusion because FOXP3 expression is not an absolute or specific marker for functional Tregs5. In this regard, it was recently suggested that FOXP3 expression plus cytokine profiling could help distinguish FOXP3+ Tregs from FOXP3+ activated effector cells in certain epithelial carcinomas50. Another potential source of conflicting results is that patient populations and factors known to confound survival estimates or treatment response data are not fully defined or identified in some studies.
Absolute numbers and/or functional status of Tregs are prognostic indicators as discussed, but Tregs also appear to have prognostic importance based on their specific anatomic location, or distribution within this anatomic location. For example, in gastric carcinoma, survival was affected by Treg distribution in the tumor but not on total FOXP3+ tumor Treg numbers96. The ratio of Tregs to various immune cells, including anti-tumor effector cells also predicts survival in some studies. For example, a low ratio of CD8+ T cells to Tregs predicted a poor prognosis in patients with cervical cancer97. The ratio of FOXP3+ cells to granzyme B+ cells predicted survival in Hodgkin lymphoma patients98. The timing of these changes can also be important. For example, the simultaneous reduction of FOXP3+ cells with increased infiltration into breast carcinoma tissue of CD8+ cells was the best predictor of pathologic complete response following cytotoxic breast cancer chemotherapy92. As we understand specific aspects of tumor-associated Tregs better, it is likely that better algorithms to predict treatment responses (including to surgery, radiation and cytotoxic agents) and survival will be produced. These advances will also be further facilitated as we better understand how to identify tumor Tregs with logistically tractable tests.
6 Tregs and Cancer Prevention
Efforts to understand the immunopathologic role of cancer Tregs have focused on their immunopathologic influences on clinically apparent cancer. Nonetheless, because Tregs dampen anti-tumor immunity it is plausible that they could also affect the degeneration of a premalignant lesion to a frank malignancy, or could affect the immunoediting that occurs after malignant degeneration but before the tumor is clinically apparent (the immune equilibrium phase). A significant finding in this regard is that Tregs mediate loss of concomitant immunity99, making it biologically plausible that they could inhibit anti-tumor immunity early in preclinical cancer progression. Tregs inhibit tumor immune surveillance in skin and connective tissues in a mouse model for carcinogen-induced sarcoma100. It has been proposed that a mechanism for ultraviolet radiation-induced skin cancer could include the induction of dermal Tregs101 and that Tregs could contribute to malignant progression in cervical cancer19. As many cancers, including cervical carcinomas are virus-associated, Tregs could contribute to malignant progression by suppressing immunity to virus-associated antigens in addition to any effects on nonviral antigen immunity102, also supported by the finding of human papilloma virus antigen-specific Tregs in human cervical cancer103, a cancer in which human papilloma virus is a key etiologic agent. In a chronic inflammation model for colorectal cancer in mice, Tregs decreased colorectal cancer development by blunting microbe-driven local inflammation55. Managing Tregs in cancer prevention remains little explored yet merits additional attention. Significant issues with clinical application of this concept include the many obvious difficulties of their pharmacologic manipulations (and possible side effects) when there is no clinical malignancy.
7 Tumor Treg Effects of Anti-Cancer Therapies
Increased attention to the immunopathologic effects of cancer Treg effects has demonstrated some surprising findings regarding Treg effects on treatment outcomes for some cancers. At present, detailed mechanisms of how Tregs affect clinical outcomes in cancer patients remain unknown, with studies generally describing correlations. Future work is likely to shed considerable light on mechanistic details.
7.1 Vaccine Effects on Tregs
While it has long been known that active vaccinations generate vaccine antigen-specific effector T and B cells, recent work now establishes that such vaccines can also generate antigen-specific Tregs in mouse cancer models104. In humans, a vaccine for cervical cancer-induced CD4+CD25+FOXP3+ cells105, but Treg functional capacity and vaccine antigen specificity, remain to be demonstrated. Conversely, in a human anti-tumor vaccination trial to treat B cell chronic lymphocytic leukemia, vaccination reduced CD4+CD25+FOXP3+ T cells suggesting Treg reduction106, although Treg function of these cells was not tested. A MAGE-A3 peptide vaccine-induced MAGE-A3-specific CD4+CD25+FOXP3+ T cells with regulatory properties detected in peripheral blood of melanoma patients107 and a dendritic cell vaccine expanded functionally suppressive blood CD4+CD25+FOXP3+ Tregs in multiple myeloma patients108. Thus, active vaccination in cancer patients clearly appears to have potential to induce vaccine antigen-specific Tregs, along with any beneficial cells that might concurrently be generated.
In recognition of the issue of vaccine-induced Tregs, development of vaccines that foster generation of antigen-specific anti-tumor effector cells over generation of antigen-specific Tregs has been proposed109. Approaches include combining a CD40 agonist with Toll-like receptor activation110 and a DOTAP (N-[1-(2,3-dioleoyloxy)propyl]-N,N,N-trimethylammonium methyl-sulfate) vaccine against human papilloma virus E7 antigen that generates CD8+ T cells with concurrent Foxp3+ T cell reductions in a mouse cancer vaccine model111. Challenge of mice with tumors engineered to express ectopic CD137 single chain antibody generates better anti-tumor immunity and simultaneously generates lower numbers of Tregs than challenge with wild-type tumor cells112. Dendritic cells from multiple myeloma patients inhibited T cell activation, and tumor cell lysates from multiple myeloma or anti-myeloma idiotype antibodies-induced CD4+CD25+FOXP3+ cells in vitro 113. In this study, forced calnexin expression in these dendritic cells with a lentivirus vector boosted tumor antigen-specific effector T cell generation without increasing the generation of FOXP3+ T cells.
7.2 Cytokine Treatment Effects on Tregs
IL-2 is FDA-approved to treat renal cell carcinoma and malignant melanoma. Its clinical development was based on its activating and proliferation-inducing effects on T cells generally, and anti-tumor effector T cells specifically. However, more recent work demonstrates that a key physiologic function of IL-2 in vivo is maintenance of peripheral tolerance through critical growth and differentiation effects on Tregs114, 115 (see also Chap. 7). In light of this new understanding, therapeutic consequences of IL-2 in relationship to its effects on Tregs were undertaken. IL-2 given systemically in patients with ovarian cancer altered molecules involved in Treg trafficking and boosted numbers of Tregs70. Administration of IL-2 (combined with gp100 peptide vaccination) in three phase II melanoma clinical trials had variable effects on circulating CD4+CD25+FOXP3+ T cells (suggesting Tregs) in circulation, with increases and decreases that bore no clear relationship to clinical outcomes116. Other cytokines can also alter numbers of Tregs, and their differentiation, function or migration. As an example, gene therapy with IL-12 reduced Treg generation in a mouse model for hepatocellular carcinoma117.
7.3 Additional Agents That Alter Tregs
7.3.1 Drugs That Reduce Treg Numbers or Function
Relatively low doses of the anti-cancer cytotoxic alkylating agent cyclophosphamide (Cytoxan) can reduce Treg numbers in mice and humans118. Addition of cyclophosphamide can boost the efficacy of dendritic cell vaccines efficacy in mouse models for melanoma or colon carcinoma, association with reduced phenotypic Treg numbers that is thought to a mechanism119. At the high doses used in standard cancer treatment protocols, it is unlikely that Treg depletion alone is a significant immune mechanism for the anti-cancer effects of cyclophosphamide. The aromatase inhibitor letrozole can reduce Tregs in breast cancer120. Low dose metronomic temozolomide is reported to reduce phenotypic Tregs in a rat model for glioma, but function of the phenotypic Tregs was not tested121. The kinase inhibitor imatinib mesylate (Gleevec) enhances vaccine-induced anti-tumor immunity in mice, thought at least in part by reducing Treg numbers and function122. Imatinib mesylate actions on Tregs appear to be partly through reducing T cell receptor signaling, including reduced expression of the ZAP70 component of the T cell receptor signaling complex122. Cyclooxygenase-2 inhibitors have been proposed to reduce colorectal cancer risk in part by reducing Treg function, based on suggestive but not definitive evidence123, including the finding that cyclooxygenase-2 inhibitors can reduce FOXP3+ cell content in human colorectal cancers124.
7.3.2 Drugs That can Increase Treg Numbers or Function
Histone deacetylase inhibitors are another class of drug gaining much research attention for direct effects on tumor cell proliferation, but they can also increase Treg suppressive functions and numbers125, 126. IL-2 can further boost this effect of histone deacetylase inhibitors on Tregs127. Retinoids, including all-trans retinoic acid used in specific acute leukemias can promote generation of Tregs that preferentially home to gut128. The mTOR inhibitor rapamycin is in cancer clinical trials as an anti-proliferative agent. It is widely considered to be immunosuppressive and thought to increase Treg numbers based on the finding that mTOR suppression is required for optimal Treg function129. In our studies of normal mice given chronic oral rapamycin based on its longevity extension effects130, we found no increase in Treg numbers or function and no evidence for immune suppression when given for up to 19 consecutive months (manuscript submitted). The thalidomide congeners lenalidomide and pamolidomide reduce Treg numbers and function131 possibly by reducing Foxp3 expression in CD4+ T cells rather than by altering their production of IL-10 or TGF-β. Trastuzumab (Herceptin), an anti-Her2/neu antibody, effected a decrease in peripheral blood Treg numbers while simultaneously increasing IL-17-producing Th17 T cells in patients being treated for breast cancer, suggesting that the Th17/Treg Th differentiation pathway had been skewed132. Additional effects of other drugs for other indications have been identified133, 134.
Given the significant Treg effects of these agents, and additional immune effects of these and other agents that are being discovered, it is worthwhile to reassess the mechanisms of action of certain anti-cancer drugs, including active vaccines, passive adoptive cell transfers, tyrosine kinase and/or growth factor signaling inhibitors, anti-angiogenesis agents, and a variety of others. Such studies might suggest new insights into mechanisms of action or help identify subsets of patients that could benefit from, or be harmed by, certain treatment strategies. The dual effect of IL-2 on promoting proliferation of anti-cancer effector T cells and inducing dysfunctional Tregs in cancer is an excellent example discussed above. The National Cancer Institute’s Provocative Questions Program in 2011 addressed the issue of novel uses for well-known agents in its provocative question 5 (http://provocativequestions.nci.nih.gov/rfa).
8 Strategies to Manage Tregs
Cancer-associated Tregs appear to reduce the efficacy of endogenous and therapeutically induced anti-cancer immunity in most cancers so studied, reviewed in 31. The concept that reducing cancer Treg function will be therapeutically beneficial is thus a logical supposition133. In support of such thinking, experimental Treg depletion improves de novo anti-tumor immunity14, and increases tumor-specific immunity135 including shared tumor antigens136. Experimental Treg depletion also improves the immune and clinical activity of other therapeutic approaches including active vaccination137, 138. Our increasing understandings of mechanisms governing tumor Treg function and local accumulation31, 139, suggest distinct categories of strategies to approach reducing tumor Treg function: depletion; blocking differentiation, trafficking or effector functions; raising effector cell suppression threshold, or diversion into alternate Th differentiation pathways133, 134. Outright depletion is the best studied strategy thus far in preclinical cancer models and in human trials133, 140–144. However, the clinical and immunologic effects of Treg depletion alone are usually limited by Treg regeneration that in some cases yields Treg numbers that exceed pre-depletion levels145, 146. Thus, managing Tregs in conceptually a better approach to frame strategic thinking. The following sections outline Treg management strategies that have been or could be tested.
8.1 Nonspecific Treg Depletion
A basic feature of most Tregs studied thus far is the uniformly high expression of IL-2 receptor alpha chain (CD25). Targeting anti-CD25 through antibodies (usually clone PC61) is the most commonly employed approach in preclinical mouse cancer models1. We and others have demonstrated that denileukin diftitox (ONTAK), a recombinant fusion protein of the majority of human IL-2 plus the toxin moiety of diphtheria toxin147 that targets cells expressing IL-2 receptor148, has been used to deplete Tregs in renal cell carcinoma149, melanoma141, 142, 150, and ovarian cancer148. We have also depleted Tregs with denileukin diftitox in patients with breast, pancreatic, bladder, and lung cancer in addition to melanoma (manuscript submitted). One group failed to demonstrate that denileukin diftitox could deplete Tregs in melanoma143. The basis for this discrepant result is unknown at present, but does not appear due to differences in doses or schedule, or prior treatments with IL-2. We recently reported that aged mice have increased numbers of CD25lo but Foxp3+ functional Tregs151. Denileukin diftitox depleted these Tregs, but consequences for tumor immunotherapy remain to be fully established.
The alkylating agent cyclophosphamide118 (Cytoxan), improves the clinical efficacy of dendritic cell vaccines in preclinical mouse models for colon carcinoma and melanoma in association with reducing Treg numbers119. ICOS+ and TNFR2+ Tregs are reportedly more suppressive than the total CD4+CD25hi T cell population that includes Tregs; cyclophosphamide appears selectively to deplete numbers of these highly suppressive Tregs152. Metronomic low dose schedules of cyclophosphamide can deplete functional Tregs in peripheral blood of cancer patients118. Fludarabine can deplete Tregs, although it is toxic to most T cells153. Paclitaxel-based chemotherapy in non-small cell lung cancer patients reduced Treg numbers in peripheral blood, which in vitro tests suggested was specifically due to the paclitaxel154.
Immunity generated against Foxp3-expressing cells (including Tregs) increased tumor immunity in a mouse model for renal cell carcinoma155. However, mechanisms of action of this approach could include attack against Foxp3 expression reported in some non-hematologic cancers156.
LMB-2 is a Pseudomonas immunotoxin conjugated to the Fv moiety of an anti-CD25 antibody targeting the toxin to CD25+ cells and depletes Tregs in human cancer patients157. Although depleting CD25+ T cells from hematopoietic stem cell transplant in a mouse cancer model boosted anti-tumor immunity158, depleting CD25+ cells (including, but not exclusively Tregs) in an autologous cell adoptive cell transfer protocol in combination with high-dose IL-2 in vivo did not affect prolonged Treg reduction in a clinical trial159.
The anti-CD25 monoclonal antibody daclizumab was recently demonstrated to deplete human Tregs in breast cancer patients, and reprogram their Tregs as evidenced by increased IFN-γ production140.
CpG treatment in melanoma patients can reduce lymph node FOXP3+ T cell numbers160, but functional status of FOXP3+ cells was not reported in this study. The small-molecule STAT3 inhibitor JSI-124 augmented activated effector T cell infiltration into tumor and reduced cells with a Treg function in a mouse melanoma model when combined with CpG treatment161. Adding cyclophosphamide to OX40 ligation enhances anti-tumor immunity and promotes tumor rejection in a mouse melanoma model, thought in part due to increasing local Treg apoptosis73. Many more examples similar to these have also been described. Foxp3DTR mice are engineered for diphtheria toxin expression under control of the Foxp3 promoter162. Using these mice, it is definitively established that depleting just Tregs alone can significantly enhance anti-tumor immunity and clinical tumor rejection163. Due to the technical challenges inherent in human Treg work, the clinical and immunologic effects exclusively attributable to depleting Tregs has not been definitively demonstrated in any human cancer. Chesney, et al., showed that denileukin diftitox improved clinical and immune outcomes in advanced-stage human melanoma, including with cerebral metastases, but attributed effects to transient T cell depletion of the immunotoxin141. A follow-up study by the same group confirmed the efficacy of the immunotoxin and its ability to deplete human Tregs in metastatic melanoma142.
8.2 Antigen-Specific Treg Targeting
Tumor antigen-specific Tregs have now been described as occurring de novo, with no prior vaccinations or other interventions53, 164, although they are also described as increasing in response to active cancer vaccination104. Significant pathologic autoimmunity from Treg depletion in human cancer patients has yet to be reported, contrasting with many reports of significant autoimmune complications of anti-CTLA-4 antibody treatment165 (and see Chap. 8). Lack of significant autoimmunity with current attempts to deplete Tregs no doubt is partly due to the relatively inefficiency of the approaches evaluated, as total Treg depletion can induce significant autoimmunity even in naive mice162. Nonetheless, if tumor antigen-specific Tregs could be specifically targeted for destruction, it could be possible to improve anti-tumor immunity with minimal induction of unwanted pathologic autoimmunity from Treg depletion. No technique that manages human antigen-specific Treg function uniquely has yet been described. In some cancers, folate receptor 4-expressing tumor Tregs includes a population of tumor antigen-specific Tregs the reduction of which augments clinically significant anti-tumor immunity in a mouse cancer model166.
8.3 Raising the Effector Cell Suppression Threshold
The anti-CTLA-4 antibody ipilimumab was FDA-approved to treat metastatic melanoma in March 2011. It can increase the proliferation of Tregs in human subjects despite its clinically proven efficacy167. It was initially thought perhaps to work by reducing Treg numbers, but that is probably not a significant mechanism, and if anything Treg numbers can increase after anti-CTLA-4168–170. Mechanisms for its clinical effects include reducing Treg function and increasing the threshold for Treg-mediated suppression of effector cells by action on the latter. The relative contributions of each mechanism of action is incompletely understood and might depend on tumor type and anatomic compartment, although increasing the Treg suppression threshold appears generally to be more important. Anti-CTLA-4 antibody treatment reduced CD3+CD4+FOXP3+ T cells in blood that phenotypically appeared to be Tregs in a human trial. Nonetheless, CD8+ cytotoxic T cell numbers in blood did not change significantly. Further, CD3+CD4+FOXP3+ T cells quickly returned to baseline numbers, and their function as Tregs was not confirmed171. Please see Chap. 8 for many additional details on anti-CTLA-4 effects.
In an alternative approach to raising effector T cell suppression threshold, A20 (a zinc finger protein) was genetically silenced in dendritic cells. In a mouse cancer model, tumor-infiltrating T cells previously activated with A20-silenced dendritic cells resisted Treg-mediated suppression172. The cytokine IL-7 raises effector T cell threshold for Treg-mediated suppression in mouse models of autoimmunity173, but IL-7 effects in this regard in tumors have not been reported. Notch signaling in effector T cells appears important in modulating Treg-mediated suppression when the suppression involves membrane-bound TGF-β174, but Notch effects on resistance to human Tregs have not yet been reported.
8.4 Altering Treg Trafficking
Specifically impeding the trafficking of Treg ingress into areas where anti-tumor immunity is primed8 or executing its effector functions is likely to be a beneficial treatment strategy. Improving effector T cell trafficking over Treg trafficking into tumor could be a useful treatment strategy, as was demonstrated using cyclophosphamide plus anti-OX40 antibody in a mouse model for melanoma73. We showed that anti-CL22 antibody prevented Tregs from infiltrating into human ovarian cancer cells xenografted into immunodeficient mice, promoting immune-mediated rejection by adoptively transferred autologous CD8+ T cells (T. Curiel, W. Zou, et al., unpublished data). CCL22 also attracts Tregs in human breast cancer175. However, CCL22 may also facilitate trafficking of effector T cells. Therefore, any potential benefit of CCL22 blockade or of interrupting other trafficking signals requires further study as to potential therapeutic utility. Selective in silico studies identified small-molecule chemokine receptor antagonists or monoclonal antibodies able to block in vitro CCL22-mediated recruitment of human Treg and Th2 cells176 and have gone into phase I clinical trials177. Therapeutic utility may be limited by the binding promiscuity of chemokine receptors, the redundancy of chemokine/ligand pairs, or the role of chemokines in normal tissue homeostasis or anti-tumor immunity. These additional effects of chemokine/receptor antagonism must be taken into account in strategies to block chemokines and their receptors.
Therapeutic IL-2 administration can alter Treg trafficking, and increase numbers of circulating Tregs70, 178 even if their functionality could be reduced178.
8.5 Inhibiting Treg Suppressive Functions
Tumor Tregs use a variety of mechanisms to exert suppression of anti-tumor immunity31. Mitigating or preventing these mechanisms could be therapeutically beneficial133, 134. Inoculation of Escherichia coli engineered to express the Listeriolysin-O gene promoted generation of specific cytotoxic T lymphocytes, but also simultaneously made local Tregs nonfunctional179. Inhibiting STAT3 reduces Treg suppressive function180, and specific ablation of STAT3 signaling reduces the capacity of Tregs to restrain Th17-polarized T cells56, which was also recently suggested in endogenous Tregs in aged mice181. As detailed in Chap. 2, IL-17-producing cells and Th17-polarized immunity have incompletely understood roles in anti-tumor immunity80, 182. Thus, how these findings will translate into specific anti-cancer therapies remains unclear. Agonizing OX40 expressed on tumor-infiltrating Tregs with a specific antibody blunts their capacity to inhibit anti-tumor effector T cell activity and thus promotes improved immune-mediated tumor rejection146. Agonizing GITR signals in vitro with monoclonal antibodies reduces the suppressive capacity of Tregs in mice183, 184, but whether the approach will work with human Tregs remains unclear185. Toll-like receptor signaling in virus-based anti-tumor vaccines can reduce Treg-mediated immunosuppression. Because dendritic cell-based vaccines do not induce Toll-like receptor signaling in the absence of some additional manipulations, they could be maximally effective in promoting the efficacy of anti-tumor CD8+ T cells either by reducing Treg function or by coadministration of a Toll-like receptor agonist186. There is much interest in reducing Treg function using Toll-like receptor ligation (e.g., TLR9 ligation with CpG oligonucleotides) as an effective way to improve the efficacy of some cancer vaccines. Sendai virus reduced Treg function in a mouse model for colorectal cancer in which virus-induced IL-6 was suggested as a mechanism187. Additional considerations to block Treg function include interrupting Foxp3 interactions with NFAT, which is required for Treg suppressive function188, and blocking Treg effector molecules such as IL-10, TGF-β, or IL-35 among other strategies. Most of these strategies have not yet been assessed in human trials.
8.6 Blocking Treg Differentiation
The nuclear transcription factor Foxp3 controls Treg differentiation through mechanisms that are increasingly understood30, 189, 190 that could be used in therapeutic applications. For example, the CNS1 region of Foxp3 controls induced Treg generation29, 30 that could be silenced to reduce tumor-driven Treg generation. Tumor environmental products such as vascular endothelial growth factor retard maturation of local dendritic cells191. These tumor-associated immature dendritic cells can contribute to defective T cell activation, and to generation of Tregs. Thus, preventing dysfunctional dendritic cell activation of T cells could help reduce Treg generation in tumors. We showed that interferon-α improves dendritic cell maturation in a mouse model for ovarian cancer associated with reduced Treg generation and function and that adding it to denileukin diftitox improved clinical responses in ovarian cancer in mice and in human patients (manuscript submitted).
8.7 Subverting Treg Differentiation
Tumor-associated Tregs include those that are tumor antigen-specific53, 164. If these antigen-specific T cells could be reprogrammed into a clinically useful pathway, for example, a Th1-polarized or polarizing pathway, these counterproductive tumor-specific Tregs could be induced to become tumor-specific effector T cells. Using the common aryl hydrocarbon receptor to redirect T cells into a Th17 differentiation pathway over Treg differentiation192 is an example of a means to subverting Treg differentiation, assuming that the resulting Th17 cells are not detrimental and that a safe common aryl hydrocarbon receptor targeting molecule is identified. Th17 immunity is beneficial in some tumors182, 193 (and see Chap. 2 for details). For example inhibiting indoleamine 2,3-dioxygenase in a B16 mouse melanoma model skews Tregs towards the Th17 pathway that could promote anti-tumor immunity194. In this same melanoma model, treating dendritic cells ex vivo with an anti-B7-DC antibody facilitated the conversion of antigen-specific Tregs into tumor antigen-specific Th17 effector cells that mediated anti-tumor immunity195. A recent report demonstrated that the anti-CD25 monoclonal antibody daclizumab depleted Tregs and also reprogrammed them towards a Th1 phenotype as evidenced by IFN-γ production in a clinical trial of an hTERT vaccine in metastatic breast cancer140.
8.8 Combining Treg Management with Other Treatment Modalities
The timing of treatment modalities for anti-cancer immunotherapy can have significant influences on immunologic and clinical efficacy, including the timing of Treg depletion in relationship to other treatments196. Our understanding of how best to combine various Treg management strategies with other treatments remains limited. Transient lymphodepletion to foster homeostatic effector T cell expansion combined with Treg depletion is a testable concept, and could help explain some of the treatment effects of denileukin diftitox141. Another approach worth additional exploration is combining radiation, or selected doses of certain cytotoxic197 or hormonal agents94 that can increase tumor immunogenicity (such as by generating release of, or improving the immunogenicity of, tumor antigens as an endogenous vaccination) with Treg management. Further, the timing of chemotherapy can slow Treg re-accumulation after other approaches198.
8.9 Additional Treg Management Considerations
Even when Treg management itself is highly effective in reducing functional Tregs, clinical efficacy can nonetheless be hampered by poor intrinsic effector cell function, low effector cell trafficking into the correct compartment or immunoediting199, 200, among many other factors. For example, the efficacy of depleting Tregs in a mouse melanoma model was hampered due to relatively poor effector cell trafficking to appropriate sites. Combining Treg depletion with endothelial damage from external beam irradiation significantly improved appropriate effector cell trafficking and immune and clinical efficacy of Treg depletion167.
Relatively little has been studied regarding age or gender effects on tumor immunity generally, the effects of Tregs specifically and responses to tumor immunotherapy. Lack of age-specific studies is particularly striking as age is the biggest risk factor for cancer201. The effects of aging on Treg function in naïve mice and humans have led to contradictory results181. In our BL6 mice, there is little age-associated decline in Treg function in naïve and tumor-bearing hosts163, 181. Nonetheless, depleting Tregs is ineffective in improving anti-tumor immunity and clinical effects in B16 melanoma in aged mice, whereas it is highly effective in young mice. Lack of efficacy was found due to a compensating increase in myeloid-derived suppressor cells in aged, but not young B16-bearing hosts following Treg depletion. Combining Treg plus myeloid-derived suppressor cell depletion was thus effective in aged mice, whereas adding myeloid cell depletion to young B16-bearing mice provided no additional benefit. By contrast, Treg depletion was effective in aged hosts in a model of MC-38 colorectal cancer because myeloid-derived suppressor cells did not increase after denileukin diftitox-mediated Treg depletion163.
Regarding gender differences, we showed that estrogen and B7-H1 immune co- improve anti-tumor immunity and clinical responses in females better than males in a mouse B16 melanoma model. Differences owed in part to greater Treg functional reduction with B7-H1 blockade or deficiency in females, whereas Treg depletion was equally efficacious in either sex48. Please see Chap. 13 for many additional miscellaneous strategies and details.
9 Other Regulatory Cells
In some mouse models for cancer, Tregs might not be the significant mediators of immune dysfunction, and in such cancers, managing Tregs might not be the optimal therapeutic approach. As one example, immune suppression is reportedly mediated principally by CD4+ NKT cells, not CD4+ Tregs in a mouse model for lung metastasis due to CT26 colon cancer202. Nonetheless the role of Tregs in lung metastasis, and their role for affecting tumor growth in other anatomic compartments was not specifically reported. In the TRAMP mouse model for prostate cancer, Treg depletion with the anti-CD25 antibody PC61 did not improve tumor-specific tolerance or increase tumor rejection203. In humans, Tregs do not always correlate negatively with clinical responses to treatment or to survival as discussed above in the Section 5. Thus, it is likely that other regulatory cells are also immunopathologically relevant to clinical cancer outcomes.
In this regard, CD8+ T cells, certain myeloid cells and NKT cells have also been reported as mediating dysfunctional immune suppression in cancer204. CD8+FOXP3+ T cells in prostate cancer can suppress in a contact-dependent manner, which effects are blunted by TLR8 agonists205. CD8+CD25+Foxp3+ suppressive T cells have been reported in peripheral blood and the solid tumor mass in patients with colorectal cancer. These CD8+ Tregs expressed high CTLA-4 and GITR and suppressed the proliferation of, and cytokine secretion from CD4+CD25− T cells in vitro, similar to conventional CD4+CD25hiFoxp3+ Tregs206. In a mouse leukemia model of allograft rejection, anti-CD3 antibody treatment induced CD8+FOXP3+ suppressor T cells mitigating graft versus host, but not graft versus leukemia responses207. In a mouse colon cancer model a specific subpopulation of NKT cells and IL-13 were implicated in immune suppression208. This immune suppression was specifically suggested not to be Treg-dependent202. How these various suppressive and immune dysfunctional mediators contribute to tumor immunopathology, and how their management will contribute to novel anti-cancer immunotherapy strategies remain fully to be defined, and are interesting and important areas for additional investigation. For example, we recently identified how Treg depletion affects myeloid-derived suppressor cells, and how their combined management was superior to management of either alone in aged mice with B16 melanoma163.
10 Summary and Challenges
Recent detailed studies make plain that not all types of malignancies, or at all pathological stages, and not all hosts will benefit from specific Treg management strategies proposed here. For example, Tregs could contribute to immunopathology in specific lymphomas. Nonetheless, steroids that are used in some treatment strategies could blunt clinically meaningful activation of effector T cells. Alternatively, if Tregs are beneficial in some lymphomas as suggested, reducing their function could be detrimental. Understanding which agents are most useful in Treg management, and in what combination and in which order are important details generally not known at present. Treg-specific agents are not currently available for use in humans, but with our rapid understanding of Treg biology, development of a specific management agent in the near term is a realistic expectation.
Practically applicable, accurate immune assays that predict Treg function and clinical outcomes following Treg management interventions must be developed and validated to assess clinical and immune consequences of proposed interventions. As an example, to understand the effects of Treg-mediated T cell suppression, methods to isolate large numbers of viable immune cells at high purity must be developed that do not compromise patient safety. Clinical trial design must address appropriate proof-of-concept issues that account for the unique, specific challenges inherent in understanding effects of these novel approaches. For example, assays to link Treg management strategies with alterations in tumor-specific immunity will be important to develop, to show conclusively that Treg function (however defined) is accomplished with a specific intervention, and that this reduction is a mechanism for any improved clinical and immune outcomes observed. Developing tests of local tumor microenvironmental changes is challenging in human subjects where patient safety and limiting tissue amounts are major considerations. Thus, developing a blood test or relatively non-invasive test that will convey the relevant data needed to come to meaningful conclusions regarding mechanisms of Treg management strategies would be a significant advance.
Despite our current state of relatively incomplete understandings, there is reason for much optimism given the rapid and useful advances made in the past 5 years alone. Developing clinically useful and logistically tractable Treg management strategies to treat cancer is a reasonable and realistic goal for the near term.
References
Sakaguchi S, Sakaguchi N, Asano M, Itoh M, Toda M (1995) Immunologic self-tolerance maintained by activated T cells expressing IL-2 receptor alpha-chains (CD25). Breakdown of a single mechanism of self-tolerance causes various autoimmune diseases. J Immunol 155:1151–1164
Fontenot JD, Gavin MA, Rudensky AY (2003) Foxp3 programs the development and function of CD4 + CD25+ regulatory T cells. Nat Immunol 4:330–336
Fontenot JD et al (2005) Regulatory T cell lineage specification by the forkhead transcription factor foxp3. Immunity 22:329–341
Hori S, Nomura T, Sakaguchi S (2003) Control of regulatory T cell development by the transcription factor foxp3. Science 299:1057–1061
Curiel TJ (2007) Regulatory T-cell development: is Foxp3 the decider? Nat Med 13:250–253
Josefowicz SZ, Lu LF, Rudensky AY (2012) Regulatory T Cells: mechanisms of differentiation and function. Annu Rev Immunol 30:531–64
Woo EY et al (2001) Regulatory CD4(+)CD25(+) T cells in tumors from patients with early- stage non-small cell lung cancer and late-stage ovarian cancer. Cancer Res 61:4766–4772
Curiel TJ et al (2004) Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival. Nat Med 10:942–949
Woo EY et al (2002) Regulatory T cells from lung cancer patients directly inhibit autologous T cell proliferation. J Immunol 168:4272–4276
Javia LR, Rosenberg SA (2003) CD4 + CD25+ suppressor lymphocytes in the circulation of patients immunized against melanoma antigens. J Immunother 26:85–93
Somasundaram R et al (2002) Inhibition of cytolytic T lymphocyte proliferation by autologous CD4+/CD25+ regulatory T cells in a colorectal carcinoma patient is mediated by transforming growth factor-beta. Cancer Res 62:5267–5272
Wolf AM et al (2003) Increase of regulatory T cells in the peripheral blood of cancer patients. Clin Cancer Res 9:606–612
Sasada T, Kimura M, Yoshida Y, Kanai M, Takabayashi A (2003) CD4 + CD25+ regulatory T cells in patients with gastrointestinal malignancies: possible involvement of regulatory T cells in disease progression. Cancer 98:1089–1099
Shimizu J, Yamazaki S, Sakaguchi S (1999) Induction of tumor immunity by removing CD25 + CD4+ T cells: a common basis between tumor immunity and autoimmunity. J Immunol 163:5211–5218
Liyanage UK et al (2002) Prevalence of regulatory T cells is increased in peripheral blood and tumor microenvironment of patients with pancreas or breast adenocarcinoma. J Immunol 169:2756–2761
Shevach EM (2002) CD4+ CD25+ suppressor T cells: more questions than answers. Nat Rev Immunol 2:389–400
Bach JF (2003) Regulatory T cells under scrutiny. Nat Rev Immunol 3:189–198
Loskog A et al (2007) Human bladder carcinoma is dominated by T-regulatory cells and Th1 inhibitory cytokines. J Urol 177:353–358
Visser J et al (2007) Frequencies and role of regulatory T cells in patients with (pre)malignant cervical neoplasia. Clin Exp Immunol 150:199–209
Kaporis HG et al (2007) Human basal cell carcinoma is associated with Foxp3+ T cells in a Th2 dominant microenvironment. J Invest Dermatol 127:2391–2398
Lau KM et al (2007) Increase in circulating Foxp3 + CD4 + CD25(high) regulatory T cells in nasopharyngeal carcinoma patients. Br J Cancer 96:617–622
Mourmouras V et al (2007) Evaluation of tumour-infiltrating CD4 + CD25 + FOXP3+ regulatory T cells in human cutaneous benign and atypical naevi, melanomas and melanoma metastases. Br J Dermatol 157:531–539
Ling KL et al (2007) Increased frequency of regulatory T cells in peripheral blood and tumour infiltrating lymphocytes in colorectal cancer patients. Cancer Immun 7:7
Nagorsen D et al (2007) Tumor-infiltrating macrophages and dendritic cells in human colorectal cancer: relation to local regulatory T cells, systemic T-cell response against tumor-associated antigens and survival. J Transl Med 5:62
Szczepanski MJ et al (2009) Increased frequency and suppression by regulatory T cells in patients with acute myelogenous leukemia. Clin Cancer Res 15:3325–3332
Sugihara AQ, Rolle CE, Lesniak MS (2009) Regulatory T cells actively infiltrate metastatic brain tumors. Int J Oncol 34:1533–1540
Bluestone JA, Abbas AK (2003) Natural versus adaptive regulatory T cells. Nat Rev Immunol 3:253–257
Thornton AM et al (2010) Expression of Helios, an Ikaros transcription factor family member, differentiates thymic-derived from peripherally induced Foxp3+ T regulatory cells. J Immunol 184:3433–3441
Josefowicz SZ et al (2012) Extrathymically generated regulatory T cells control mucosal TH2 inflammation. Nature 482:395–399
Zheng Y et al (2010) Role of conserved non-coding DNA elements in the Foxp3 gene in regulatory T-cell fate. Nature 463:808–812
Zou W (2006) Regulatory T cells, tumour immunity and immunotherapy. Nat Rev Immunol 6:295–307
Zhou G, Levitsky HI (2007) Natural regulatory T cells and de novo-induced regulatory T cells contribute independently to tumor-specific tolerance. J Immunol 178:2155–2162
Yokokawa J et al (2008) Enhanced functionality of CD4 + CD25highFoxP3+ regulatory T cells in the peripheral blood of patients with prostate cancer. Clin Cancer Res 14:1032–1040
Strauss L, Bergmann C, Whiteside TL (2009) Human circulating CD4 + CD25highFoxp3+ regulatory T cells kill autologous CD8+ but not CD4+ responder cells by Fas-mediated apoptosis. J Immunol 182:1469–1480
Liu VC et al (2007) Tumor evasion of the immune system by converting CD4 + CD25- T cells into CD4 + CD25+ T regulatory cells: role of tumor-derived TGF-beta. J Immunol 178:2883–2892
Han Y, Guo Q, Zhang M, Chen Z, Cao X (2009) CD69+ CD4+ CD25- T cells, a new subset of regulatory T cells, suppress T cell proliferation through membrane-bound TGF-beta 1. J Immunol 182:111–120
Liu W et al (2006) CD127 expression inversely correlates with FoxP3 and suppressive function of human CD4+ T reg cells. J Exp Med 203:1701–1711
Bruder D et al (2004) Neuropilin-1: a surface marker of regulatory T cells. Eur J Immunol 34:623–630
Battaglia A et al (2008) Neuropilin-1 expression identifies a subset of regulatory T cells in human lymph nodes that is modulated by preoperative chemoradiation therapy in cervical cancer. Immunology 123:129–138
Yano H et al (2007) Regulatory T-cell function of adult T-cell leukemia/lymphoma cells. Int J Cancer 120:2052–2057
Hallermann C, Niermann C, Schulze HJ (2007) Regulatory T-cell phenotype in association with large cell transformation of mycosis fungoides. Eur J Haematol 78:260–263
Karube K et al (2008) The relationship of FOXP3 expression and clinicopathological characteristics in adult T-cell leukemia/lymphoma. Mod Pathol 21:617–625
Tan W et al (2011) Tumour-infiltrating regulatory T cells stimulate mammary cancer metastasis through RANKL-RANK signalling. Nature 470:548–553
Facciabene A et al (2011) Tumour hypoxia promotes tolerance and angiogenesis via CCL28 and T(reg) cells. Nature 475:226–230
Darrasse-Jeze G et al (2009) Feedback control of regulatory T cell homeostasis by dendritic cells in vivo. J Exp Med 206:1853–1862
Shevach EM (2009) Mechanisms of foxp3+ T regulatory cell-mediated suppression. Immunity 30:636–645
Wan YY, Flavell RA (2007) Regulatory T-cell functions are subverted and converted owing to attenuated Foxp3 expression. Nature 445:766–770
Lin PY et al (2010) B7-H1-dependent sex-related differences in tumor immunity and immunotherapy responses. J Immunol 185:2747–2753
Mold JE et al (2008) Maternal alloantigens promote the development of tolerogenic fetal regulatory T cells in utero. Science 322:1562–1565
Kryczek I et al (2009) FOXP3 defines regulatory T cells in human tumor and autoimmune disease. Cancer Res 69:3995–4000
Wieczorek G et al (2009) Quantitative DNA methylation analysis of FOXP3 as a new method for counting regulatory T cells in peripheral blood and solid tissue. Cancer Res 69:599–608
Mandapathil M, Lang S, Gorelik E, Whiteside TL (2009) Isolation of functional human regulatory T cells (Treg) from the peripheral blood based on the CD39 expression. J Immunol Methods 346:55–63
Vence L et al (2007) Circulating tumor antigen-specific regulatory T cells in patients with metastatic melanoma. Proc Natl Acad Sci USA 104:20884–20889
Grivennikov SI, Greten FR, Karin M (2010) Immunity, inflammation, and cancer. Cell 140:883–899
Poutahidis T et al (2007) Rapid reversal of interleukin-6-dependent epithelial invasion in a mouse model of microbially induced colon carcinoma. Carcinogenesis 28:2614–2623
Chaudhry A et al (2009) CD4+ regulatory T cells control TH17 responses in a Stat3-dependent manner. Science 326:986–991
Zheng Y et al (2009) Regulatory T-cell suppressor program co-opts transcription factor IRF4 to control T(H)2 responses. Nature 458:351–356
Bergmann C, Strauss L, Zeidler R, Lang S, Whiteside TL (2007) Expansion of human T regulatory type 1 cells in the microenvironment of cyclooxygenase 2 overexpressing head and neck squamous cell carcinoma. Cancer Res 67:8865–8873
Li X et al (2007) Human ovarian carcinoma cells generate CD4(+)CD25(+) regulatory T cells from peripheral CD4(+)CD25(−) T cells through secreting TGF-beta. Cancer Lett 253:144–153
Munn DH (2011) Indoleamine 2,3-dioxygenase, Tregs and cancer. Curr Med Chem 18:2240–2246
Yang ZZ, Novak AJ, Ziesmer SC, Witzig TE, Ansell SM (2007) CD70+ non-Hodgkin lymphoma B cells induce Foxp3 expression and regulatory function in intratumoral CD4+ CD25 T cells. Blood 110:2537–2544
Juszczynski P et al (2007) The AP1-dependent secretion of galectin-1 by Reed Sternberg cells fosters immune privilege in classical Hodgkin lymphoma. Proc Natl Acad Sci USA 104:13134–13139
Mittal S et al (2008) Local and systemic induction of CD4 + CD25+ regulatory T cell population by non-Hodgkin’s lymphoma. Blood 111:5359–5370
Baumgartner J et al (2007) Melanoma induces immunosuppression by up-regulating FOXP3(+) regulatory T cells. J Surg Res 141:72–77
Sharma MD et al (2007) Plasmacytoid dendritic cells from mouse tumor-draining lymph nodes directly activate mature Tregs via indoleamine 2,3-dioxygenase. J Clin Invest 117:2570–2582
Curiel TJ et al (2003) Blockade of B7-H1 improves myeloid dendritic cell-mediated antitumor immunity. Nat Med 9:562–567
Zou W et al (2001) Stromal-derived factor-1 in human tumors recruits and alters the function of plasmacytoid precursor dendritic cells. Nat Med 7:1339–1346
Mizukami Y et al (2008) CCL17 and CCL22 chemokines within tumor microenvironment are related to accumulation of Foxp3+ regulatory T cells in gastric cancer. Int J Cancer 122:2286–2293
Shimizu Y et al (2009) CXCR4 + FOXP3 + CD25+ lymphocytes accumulate in CXCL12-expressing malignant pleural mesothelioma. Int J Immunopathol Pharmacol 22:43–51
Wei S et al (2007) Interleukin-2 administration alters the CD4 + FOXP3+ T-cell pool and tumor trafficking in patients with ovarian carcinoma. Cancer Res 67:7487–7494
Ghiringhelli F et al (2005) Tumor cells convert immature myeloid dendritic cells into TGF-beta-secreting cells inducing CD4 + CD25+ regulatory T cell proliferation. J Exp Med 202:919–929
Gabrilovich D (2004) Mechanisms and functional significance of tumour-induced dendritic-cell defects. Nat Rev Immunol 4:941–952
Hirschhorn-Cymerman D et al (2009) OX40 engagement and chemotherapy combination provides potent antitumor immunity with concomitant regulatory T cell apoptosis. J Exp Med 206:1103–1116
Xie Q, Gan L, Wang J, Wilson I, Li L (2007) Loss of the innate immunity negative regulator IRAK-M leads to enhanced host immune defense against tumor growth. Mol Immunol 44:3453–3461
Habicht A et al (2007) A link between PDL1 and T regulatory cells in fetomaternal tolerance. J Immunol 179:5211–5219
Schreiber TH (2007) The use of FoxP3 as a biomarker and prognostic factor for malignant human tumors. Cancer Epidemiol Biomarkers Prev 16:1931–1934
Pillai V, Karandikar NJ (2007) Human regulatory T cells: a unique, stable thymic subset or a reversible peripheral state of differentiation? Immunol Lett 114:9–15
Zhou X et al (2009) Instability of the transcription factor Foxp3 leads to the generation of pathogenic memory T cells in vivo. Nat Immunol 10:1000–1007
Miyao T et al (2012) Plasticity of foxp3(+) T cells reflects promiscuous foxp3 expression in conventional T cells but not reprogramming of regulatory T cells. Immunity 36:262–275
Kryczek I et al (2011) IL-17+ regulatory T cells in the microenvironments of chronic inflammation and cancer. J Immunol 186:4388–4395
Perrone G et al (2008) Intratumoural FOXP3-positive regulatory T cells are associated with adverse prognosis in radically resected gastric cancer. Eur J Cancer 44:1875–1882
Kobayashi N et al (2007) FOXP3+ regulatory T cells affect the development and progression of hepatocarcinogenesis. Clin Cancer Res 13:902–911
Sasaki A et al (2008) Prognostic value of tumor-infiltrating FOXP3+ regulatory T cells in patients with hepatocellular carcinoma. Eur J Surg Oncol 34:173–179
Miracco C et al (2007) Utility of tumour-infiltrating CD25 + FOXP3+ regulatory T cell evaluation in predicting local recurrence in vertical growth phase cutaneous melanoma. Oncol Rep 18:1115–1122
Tzankov A et al (2008) Correlation of high numbers of intratumoral FOXP3+ regulatory T cells with improved survival in germinal center-like diffuse large B-cell lymphoma, follicular lymphoma and classical Hodgkin’s lymphoma. Haematologica 93:193–200
Salama P et al (2009) Tumor-infiltrating FOXP3+ T regulatory cells show strong prognostic significance in colorectal cancer. J Clin Oncol 27:186–192
Badoual C et al (2006) Prognostic value of tumor-infiltrating CD4+ T-cell subpopulations in head and neck cancers. Clin Cancer Res 12:465–472
Kakinuma T et al (2007) Small numbers of residual tumor cells at the site of primary inoculation are critical for anti-tumor immunity following challenge at a secondary location. Cancer Immunol Immunother 56:1119–1131
Siddiqui SA et al (2007) Tumor-infiltrating Foxp3-CD4 + CD25+ T cells predict poor survival in renal cell carcinoma. Clin Cancer Res 13:2075–2081
Grabenbauer GG, Lahmer G, Distel L, Niedobitek G (2006) Tumor-infiltrating cytotoxic T cells but not regulatory T cells predict outcome in anal squamous cell carcinoma. Clin Cancer Res 12:3355–3360
Wada J et al (2008) Regulatory T-cells are possible effect prediction markers of immunotherapy for cancer patients. Anticancer Res 28:2401–2408
Ladoire S et al (2008) Pathologic complete response to neoadjuvant chemotherapy of breast carcinoma is associated with the disappearance of tumor-infiltrating foxp3+ regulatory T cells. Clin Cancer Res 14:2413–2420
Derhovanessian E et al (2009) Pretreatment frequency of circulating IL-17+ CD4+ T-cells, but not Tregs, correlates with clinical response to whole-cell vaccination in prostate cancer patients. Int J Cancer 125:1372–1379
Sorrentino C, Musiani P, Pompa P, Cipollone G, Di Carlo E (2011) Androgen deprivation boosts prostatic infiltration of cytotoxic and regulatory T lymphocytes and has no effect on disease-free survival in prostate cancer patients. Clin Cancer Res 17:1571–1581
Strauss L, Bergmann C, Gooding W, Johnson JT, Whiteside TL (2007) The frequency and suppressor function of CD4 + CD25highFoxp3+ T cells in the circulation of patients with squamous cell carcinoma of the head and neck. Clin Cancer Res 13:6301–6311
Mizukami Y et al (2008) Localisation pattern of Foxp3(+) regulatory T cells is associated with clinical behaviour in gastric cancer. Br J Cancer 98:148–153
Jordanova ES et al (2008) Human leukocyte antigen class I, MHC class I chain-related molecule A, and CD8+/regulatory T-cell ratio: which variable determines survival of cervical cancer patients? Clin Cancer Res 14:2028–2035
Kelley TW, Pohlman B, Elson P, Hsi ED (2007) The ratio of FOXP3+ regulatory T cells to granzyme B + cytotoxic T/NK cells predicts prognosis in classical Hodgkin lymphoma and is independent of bcl-2 and MAL expression. Am J Clin Pathol 128:958–965
Turk MJ et al (2004) Concomitant tumor immunity to a poorly immunogenic melanoma is prevented by regulatory T cells. J Exp Med 200:771–782
Betts G et al (2007) The impact of regulatory T cells on carcinogen-induced sarcogenesis. Br J Cancer 96:1849–1854
Beissert S, Loser K (2008) Molecular and cellular mechanisms of photocarcinogenesis. Photochem Photobiol 84:29–34
Molling JW et al (2007) CD4(+)CD25hi regulatory T-cell frequency correlates with persistence of human papillomavirus type 16 and T helper cell responses in patients with cervical intraepithelial neoplasia. Int J Cancer 121:1749–1755
van der Burg SH et al (2007) Association of cervical cancer with the presence of CD4+ regulatory T cells specific for human papillomavirus antigens. Proc Natl Acad Sci USA 104:12087–12092
Zhou G, Drake CG, Levitsky HI (2006) Amplification of tumor-specific regulatory T cells following therapeutic cancer vaccines. Blood 107:628–636
Welters MJ et al (2008) Induction of tumor-specific CD4+ and CD8+ T-cell immunity in cervical cancer patients by a human papillomavirus type 16 E6 and E7 long peptides vaccine. Clin Cancer Res 14:178–187
Hus I et al (2008) Vaccination of B-CLL patients with autologous dendritic cells can change the frequency of leukemia antigen-specific CD8+ T cells as well as CD4 + CD25 + FoxP3+ regulatory T cells toward an antileukemia response. Leukemia 22:1007–1017
Francois V et al (2009) The CD4(+) T-cell response of melanoma patients to a MAGE-A3 peptide vaccine involves potential regulatory T cells. Cancer Res 69:4335–4345
Banerjee DK, Dhodapkar MV, Matayeva E, Steinman RM, Dhodapkar KM (2006) Expansion of FOXP3high regulatory T cells by human dendritic cells (DCs) in vitro and after injection of cytokine-matured DCs in myeloma patients. Blood 108:2655–2661
Palucka AK, Ueno H, Fay JW, Banchereau J (2007) Taming cancer by inducing immunity via dendritic cells. Immunol Rev 220:129–150
Ahonen CL et al (2008) Enhanced efficacy and reduced toxicity of multifactorial adjuvants compared to unitary adjuvants as cancer vaccines. Blood 111:3116–3125
Chen W, Yan W, Huang L (2008) A simple but effective cancer vaccine consisting of an antigen and a cationic lipid. Cancer Immunol Immunother 57:517–530
Yang Y et al (2007) Tumor cells expressing anti-CD137 scFv induce a tumor-destructive environment. Cancer Res 67:2339–2344
Han S et al (2008) Overcoming immune tolerance against multiple myeloma with lentiviral calnexin-engineered dendritic cells. Mol Ther 16:269–279
Malek TR, Porter BO, Codias EK, Scibelli P, Yu A (2000) Normal lymphoid homeostasis and lack of lethal autoimmunity in mice containing mature T cells with severely impaired IL-2 receptors. J Immunol 164:2905–2914
Malek TR, Yu A, Vincek V, Scibelli P, Kong L (2002) CD4 regulatory T cells prevent lethal autoimmunity in IL-2Rbeta-deficient mice. Implications for the nonredundant function of IL-2. Immunity 17:167–178
Sosman JA et al (2008) Three phase II cytokine working group trials of gp100 (210 M) peptide plus high-dose interleukin-2 in patients with HLA-A2-positive advanced melanoma. J Clin Oncol 26:2292–2298
Zabala M et al (2007) Induction of immunosuppressive molecules and regulatory T cells counteracts the antitumor effect of interleukin-12-based gene therapy in a transgenic mouse model of liver cancer. J Hepatol 47:807–815
Brode S, Cooke A (2008) Immune-potentiating effects of the chemotherapeutic drug cyclophosphamide. Crit Rev Immunol 28:109–126
Liu JY et al (2007) Single administration of low dose cyclophosphamide augments the antitumor effect of dendritic cell vaccine. Cancer Immunol Immunother 56:1597–1604
Generali D et al (2009) Immunomodulation of FOXP3+ regulatory T cells by the aromatase inhibitor letrozole in breast cancer patients. Clin Cancer Res 15:1046–1051
Banissi C, Ghiringhelli F, Chen L, Carpentier AF (2009) Treg depletion with a low-dose metronomic temozolomide regimen in a rat glioma model. Cancer Immunol Immunother 58:1627–1634
Larmonier N et al (2008) Imatinib mesylate inhibits CD4+ CD25+ regulatory T cell activity and enhances active immunotherapy against BCR-ABL- tumors. J Immunol 181:6955–6963
Yaqub S et al (2008) Regulatory T cells in colorectal cancer patients suppress anti-tumor immune activity in a COX-2 dependent manner. Cancer Immunol Immunother 57:813–821
Lonnroth C et al (2008) Preoperative treatment with a non-steroidal anti-inflammatory drug (NSAID) increases tumor tissue infiltration of seemingly activated immune cells in colorectal cancer. Cancer Immun 8:5
Li B et al (2007) FOXP3 interactions with histone acetyltransferase and class II histone deacetylases are required for repression. Proc Natl Acad Sci USA 104:4571–4576
Tao R et al (2007) Deacetylase inhibition promotes the generation and function of regulatory T cells. Nat Med 13:1299–1307
Kato Y et al (2007) Synergistic in vivo antitumor effect of the histone deacetylase inhibitor MS-275 in combination with interleukin 2 in a murine model of renal cell carcinoma. Clin Cancer Res 13:4538–4546
Kang SG, Lim HW, Andrisani OM, Broxmeyer HE, Kim CH (2007) Vitamin A metabolites induce gut-homing FoxP3+ regulatory T cells. J Immunol 179:3724–3733
Haxhinasto S, Mathis D, Benoist C (2008) The AKT-mTOR axis regulates de novo differentiation of CD4 + Foxp3+ cells. J Exp Med 205:565–574
Harrison DE et al (2009) Rapamycin fed late in life extends lifespan in genetically heterogeneous mice. Nature 460:392–395
Galustian C et al (2009) The anti-cancer agents lenalidomide and pomalidomide inhibit the proliferation and function of T regulatory cells. Cancer Immunol Immunother 58:1033–1045
Horlock C et al (2009) The effects of trastuzumab on the CD4 + CD25 + FoxP3+ and CD4 + IL17A + T-cell axis in patients with breast cancer. Br J Cancer 100:1061–1067
Curiel TJ (2008) Regulatory T cells and treatment of cancer. Curr Opin Immunol 20:241–246
Rüter J et al (2009) Altering regulatory T cell function in cancer immunotherapy: a novel means to boost efficacy. Front Biosci 14:1761–1770
Tanaka H, Tanaka J, Kjaergaard J, Shu S (2002) Depletion of CD4+ CD25+ regulatory cells augments the generation of specific immune T cells in tumor-draining lymph nodes. J Immunother 25:207–217
Golgher D, Jones E, Powrie F, Elliott T, Gallimore A (2002) Depletion of CD25+ regulatory cells uncovers immune responses to shared murine tumor rejection antigens. Eur J Immunol 32:3267–3275
Steitz J, Bruck J, Lenz J, Knop J, Tuting T (2001) Depletion of CD25(+) CD4(+) T cells and treatment with tyrosinase-related protein 2-transduced dendritic cells enhance the interferon alpha-induced, CD8(+) T-cell-dependent immune defense of B16 melanoma. Cancer Res 61:8643–8646
Sutmuller RP et al (2001) Synergism of cytotoxic T lymphocyte-associated antigen 4 blockade and depletion of CD25(+) regulatory T cells in antitumor therapy reveals alternative pathways for suppression of autoreactive cytotoxic T lymphocyte responses. J Exp Med 194:823–832
Curiel TJ (2007) Tregs and rethinking cancer immunotherapy. J Clin Invest 117:1167–1174
Rech AJ et al (2012) CD25 blockade depletes and selectively reprograms regulatory T-cells and cooperates with immunotherapy in cancer patients. Sci Transl Med 4:134ra62
Rasku MA et al (2008) Transient T cell depletion causes regression of melanoma metastases. J Transl Med 6:12
Telang S et al (2012) Phase II trial of the regulatory T cell-depleting agent, denileukin diftitox, in patients with unresectable stage IV melanoma. BMC Cancer 11:515
Attia P, Maker AV, Haworth LR, Rogers-Freezer L, Rosenberg SA (2005) Inability of a fusion protein of IL-2 and diphtheria toxin (Denileukin Diftitox, DAB389IL-2, ONTAK) to eliminate regulatory T lymphocytes in patients with melanoma. J Immunother 28:582–592
Attia P et al (2006) Selective elimination of human regulatory T lymphocytes in vitro with the recombinant immunotoxin LMB-2. J Immunother 29:208–214
Colombo MP, Piconese S (2007) Regulatory-T-cell inhibition versus depletion: the right choice in cancer immunotherapy. Nat Rev Cancer 7:880–887
Piconese S, Valzasina B, Colombo MP (2008) OX40 triggering blocks suppression by regulatory T cells and facilitates tumor rejection. J Exp Med 205:825–39
Foss FM (2000) DAB(389)IL-2 (ONTAK): a novel fusion toxin therapy for lymphoma. Clin Lymphoma 1:110–116, discussion 117
Barnett B, Kryczek I, Cheng P, Zou W, Curiel TJ (2005) Regulatory T cells in ovarian cancer: biology and therapeutic potential. Am J Reprod Immunol 54:369–377
Dannull J et al (2005) Enhancement of vaccine-mediated antitumor immunity in cancer patients after depletion of regulatory T cells. J Clin Invest 115:3623–3633
Mahnke K et al (2007) Depletion of CD4 + CD25+ human regulatory T cells in vivo: kinetics of Treg depletion and alterations in immune functions in vivo and in vitro. Int J Cancer 120:2723–2733
Hurez V et al (2012) Mitigating age-related immune dysfunction heightens the efficacy of tumor immunotherapy in aged mice. Cancer Res 72:2089–2099
van der Most RG et al (2009) Tumor eradication after cyclophosphamide depends on concurrent depletion of regulatory T cells: a role for cycling TNFR2-expressing effector-suppressor T cells in limiting effective chemotherapy. Cancer Immunol Immunother 58:1219–1228
Shaffer J et al (2007) Regulatory T-cell recovery in recipients of haploidentical nonmyeloablative hematopoietic cell transplantation with a humanized anti-CD2 mAb, MEDI-507, with or without fludarabine. Exp Hematol 35:1140–1152
Zhang L et al (2008) Differential impairment of regulatory T cells rather than effector T cells by paclitaxel-based chemotherapy. Clin Immunol 129:219–229
Nair S, Boczkowski D, Fassnacht M, Pisetsky D, Gilboa E (2007) Vaccination against the forkhead family transcription factor Foxp3 enhances tumor immunity. Cancer Res 67:371–380
Zuo T et al (2007) FOXP3 is an X-linked breast cancer suppressor gene and an important repressor of the HER-2/ErbB2 oncogene. Cell 129:1275–1286
Powell DJ Jr et al (2007) Administration of a CD25-directed immunotoxin, LMB-2, to patients with metastatic melanoma induces a selective partial reduction in regulatory T cells in vivo. J Immunol 179:4919–4928
Jing W, Orentas RJ, Johnson BD (2007) Induction of immunity to neuroblastoma early after syngeneic hematopoietic stem cell transplantation using a novel mouse tumor vaccine. Biol Blood Marrow Transplant 13:277–292
Powell DJ Jr, de Vries CR, Allen T, Ahmadzadeh M, Rosenberg SA (2007) Inability to mediate prolonged reduction of regulatory T cells after transfer of autologous CD25-depleted PBMC and interleukin-2 after lymphodepleting chemotherapy. J Immunother 30:438–447
Molenkamp BG et al (2007) Intradermal CpG-B activates both plasmacytoid and myeloid dendritic cells in the sentinel lymph node of melanoma patients. Clin Cancer Res 13:2961–2969
Molavi O et al (2008) Synergistic antitumor effects of CpG oligodeoxynucleotide and STAT3 inhibitory agent JSI-124 in a mouse melanoma tumor model. Immunol Cell Biol 86:506–514
Kim JM, Rasmussen JP, Rudensky AY (2007) Regulatory T cells prevent catastrophic autoimmunity throughout the lifespan of mice. Nat Immunol 8:191–197
Hurez V et al (2012) Mitigating age-related immune dysfunction heightens the efficacy of tumor immunotherapy in aged mice. Cancer Res 72:2089–2099
Wang HY et al (2004) Tumor-specific human CD4+ regulatory T cells and their ligands: implications for immunotherapy. Immunity 20:107–118
Phan GQ et al (2003) Cancer regression and autoimmunity induced by cytotoxic T lymphocyte-associated antigen 4 blockade in patients with metastatic melanoma. Proc Natl Acad Sci USA 100:8372–8377
Yamaguchi T et al (2007) Control of immune responses by antigen-specific regulatory T cells expressing the folate receptor. Immunity 27:145–159
Quezada SA et al (2008) Limited tumor infiltration by activated T effector cells restricts the therapeutic activity of regulatory T cell depletion against established melanoma. J Exp Med 205:2125–2138
Kavanagh B et al (2008) CTLA4 blockade expands FoxP3+ regulatory and activated effector CD4+ T cells in a dose-dependent fashion. Blood 112:1175–1183
Maker AV, Attia P, Rosenberg SA (2005) Analysis of the cellular mechanism of antitumor responses and autoimmunity in patients treated with CTLA-4 blockade. J Immunol 175:7746–7754
Ralph C et al (2010) Modulation of lymphocyte regulation for cancer therapy: a phase II trial of tremelimumab in advanced gastric and esophageal adenocarcinoma. Clin Cancer Res 16:1662–1672
O'Mahony D et al (2007) A pilot study of CTLA-4 blockade after cancer vaccine failure in patients with advanced malignancy. Clin Cancer Res 13:958–964
Song XT et al (2008) A20 is an antigen presentation attenuator, and its inhibition overcomes regulatory T cell-mediated suppression. Nat Med 14:258–265
Calzascia T et al (2008) CD4 T cells, lymphopenia, and IL-7 in a multistep pathway to autoimmunity. Proc Natl Acad Sci USA 105:2999–3004
Ostroukhova M et al (2006) Treg-mediated immunosuppression involves activation of the Notch-HES1 axis by membrane-bound TGF-beta. J Clin Invest 116:996–1004
Gobert M et al (2009) Regulatory T cells recruited through CCL22/CCR4 are selectively activated in lymphoid infiltrates surrounding primary breast tumors and lead to an adverse clinical outcome. Cancer Res 69:2000–2009
Bayry J et al (2008) In silico identified CCR4 antagonists target regulatory T cells and exert adjuvant activity in vaccination. Proc Natl Acad Sci USA 105:10221–10226
Yamamoto K et al (2010) Phase I study of KW-0761, a defucosylated humanized anti-CCR4 antibody, in relapsed patients with adult T-cell leukemia-lymphoma and peripheral T-cell lymphoma. J Clin Oncol 28:1591–1598
van der Vliet HJ et al (2007) Effects of the administration of high-dose interleukin-2 on immunoregulatory cell subsets in patients with advanced melanoma and renal cell cancer. Clin Cancer Res 13:2100–2108
Nitcheu-Tefit J et al (2007) Listeriolysin O expressed in a bacterial vaccine suppresses CD4 + CD25high regulatory T cell function in vivo. J Immunol 179:1532–1541
Pallandre JR et al (2007) Role of STAT3 in CD4 + CD25 + FOXP3+ regulatory lymphocyte generation: implications in graft-versus-host disease and antitumor immunity. J Immunol 179:7593–7604
Sun L et al (2012) Aged regulatory T cells protect from autoimmune inflammation despite reduced STAT3 activation and decreased constraint of IL-17 producing T cells. Aging Cell 11:509–519
Wilke CM et al (2011) Th17 cells in cancer: help or hindrance? Carcinogenesis 32:643–649
Shimizu J, Yamazaki S, Takahashi T, Ishida Y, Sakaguchi S (2002) Stimulation of CD25(+)CD4(+) regulatory T cells through GITR breaks immunological self-tolerance. Nat Immunol 3:135–142
Kanamaru F et al (2004) Costimulation via glucocorticoid-induced TNF receptor in both conventional and CD25+ regulatory CD4+ T cells. J Immunol 172:7306–7314
Levings MK et al (2002) Human CD25 + CD4+ T suppressor cell clones produce transforming growth factor beta, but not interleukin 10, and are distinct from type 1 T regulatory cells. J Exp Med 196:1335–1346
Yang Y, Huang CT, Huang X, Pardoll DM (2004) Persistent Toll-like receptor signals are required for reversal of regulatory T cell-mediated CD8 tolerance. Nat Immunol 5:508–515
Kurooka M, Kaneda Y (2007) Inactivated Sendai virus particles eradicate tumors by inducing immune responses through blocking regulatory T cells. Cancer Res 67:227–236
Ono M et al (2007) Foxp3 controls regulatory T-cell function by interacting with AML1/Runx1. Nature 446:685–689
Li B et al (2007) Biochemistry and therapeutic implications of mechanisms involved in FOXP3 activity in immune suppression. Curr Opin Immunol 19:583–588
Mantel PY et al (2007) GATA3-driven Th2 responses inhibit TGF-beta1-induced FOXP3 expression and the formation of regulatory T cells. PLoS Biol 5:e329
Gabrilovich DI et al (1996) Production of vascular endothelial growth factor by human tumors inhibits the functional maturation of dendritic cells [published erratum appears in Nat Med 1996 Nov;2(11):1267]. Nat Med 2:1096–1103
Quintana FJ et al (2008) Control of Treg and TH17 cell differentiation by the aryl hydrocarbon receptor. Nature 453:65–71
Kryczek I et al (2011) Human TH17 cells are long-lived effector memory cells. Sci Transl Med 3:104ra100
Sharma MD et al (2009) Indoleamine 2,3-dioxygenase controls conversion of Foxp3+ Tregs to TH17-like cells in tumor-draining lymph nodes. Blood 113:6102–6111
Radhakrishnan S et al (2008) Reprogrammed FoxP3+ T regulatory cells become IL-17+ antigen-specific autoimmune effectors in vitro and in vivo. J Immunol 181:3137–3147
Litzinger MT et al (2007) IL-2 immunotoxin denileukin diftitox reduces regulatory T cells and enhances vaccine-mediated T-cell immunity. Blood 110:3192–3201
Obeid M et al (2007) Calreticulin exposure dictates the immunogenicity of cancer cell death. Nat Med 13:54–61
Egilmez NK, Kilinc MO, Gu T, Conway TF (2007) Controlled-release particulate cytokine adjuvants for cancer therapy. Endocr Metab Immune Disord Drug Targets 7:266–270
DuPage M, Mazumdar C, Schmidt LM, Cheung AF, Jacks T (2012) Expression of tumour-specific antigens underlies cancer immunoediting. Nature 482:405–409
Matsushita H et al (2012) Cancer exome analysis reveals a T-cell-dependent mechanism of cancer immunoediting. Nature 482:400–404
Feng Z, Hu W, Rajagopal G, Levine AJ (2008) The tumor suppressor p53: cancer and aging. Cell Cycle 7:842–847
Park JM, Terabe M, van den Broeke LT, Donaldson DD, Berzofsky JA (2005) Unmasking immunosurveillance against a syngeneic colon cancer by elimination of CD4+ NKT regulatory cells and IL-13. Int J Cancer 114:80–87
Degl'Innocenti E et al (2008) Peripheral T-cell tolerance associated with prostate cancer is independent from CD4 + CD25+ regulatory T cells. Cancer Res 68:292–300
Zou W (2005) Immunosuppressive networks in the tumour environment and their therapeutic relevance. Nat Rev Cancer 5:263–274
Kiniwa Y et al (2007) CD8+ Foxp3+ regulatory T cells mediate immunosuppression in prostate cancer. Clin Cancer Res 13:6947–6958
Chaput N et al (2009) Identification of CD8 + CD25 + Foxp3+ suppressive T cells in colorectal cancer tissue. Gut 58:520–529
Zhang C et al (2007) Donor CD8+ T cells mediate graft-versus-leukemia activity without clinical signs of graft-versus-host disease in recipients conditioned with anti-CD3 monoclonal antibody. J Immunol 178:838–850
Terabe M et al (2000) NKT cell-mediated repression of tumor immunosurveillance by IL-13 and the IL-4R-STAT6 pathway. Nat Immunol 1:515–520
Acknowledgements
I regret that space limitations preclude citing many important works from my colleagues. Thanks to Vincent Hurez, Lishi Sun, Mark Kious, Suzanne Thibodeaux, Kruthi Murthy, Srilaskmi Pandaswara, AiJie Liu, and Sara Ludwig for expert technical assistance. Suzanne Thibodeaux helped create graphics. This work was supported by CA105207, CA054174, FD003118, the Fanny Rippel Foundation, the Voelcker Trust, the Hayes Endowment, The Holly Beach Public Library Association, The Owens Foundation The Hogg Foundation and UTHSCSA endowments.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Curiel, T.J. (2013). Managing Regulatory T Cells to Improve Cancer Immunotherapy. In: Curiel, T. (eds) Cancer Immunotherapy. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-4732-0_9
Download citation
DOI: https://doi.org/10.1007/978-1-4614-4732-0_9
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-4731-3
Online ISBN: 978-1-4614-4732-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)