Abstract
The development of cross-sectional and bronchoscopic technique making advantage of optical and ultrasound imaging technology as well as therapeutic interventional options has had considerable impact on the management of pulmonary diseases. While interventional pulmonology is mainly limited to the central half of the tracheobronchial system, CT and even more MRI are limited to the central tracheobronchial structure. However, cross-sectional imaging provides information distally to a stenosis, e.g., the relation of a lesion to the adjacent anatomy, and allows for detailed evaluation of the parenchyma. This includes the whole lung from apex to bases, while bronchoscopy is limited to a certain point of view. Furthermore, CT and MRI provide the possibility for functional judgment of parenchyma and bronchi in terms of perfusion, ventilation, collapsibility, and others, while endoscopy is capable for real-time imaging during continuous respiration including the option for manipulation, biopsy, and even treatment. A wide range of synergies of radiological and advanced interventional endoscopic procedures in patients with both central and peripheral airway disease is the result of this concept.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Virtual Bronchoscopy
- Global Quantification
- Bronchial Wall Thickness
- Bronchial Disease
- Expiratory Breath Hold
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Computed Tomography
Since multislice CT scanners (MSCT), which are able to scan the whole lung in thin sections (<0.5 mm) within a single breath hold, are widely available, CT has become a new role in imaging of the tracheobronchial tree. Three-dimensional, time-resolved, and four-dimensional visualization as well as quantitative analysis became possible by fast scanners with higher resolution in z-axis. Many of these multidimensional visualizations have to be experienced interactively at the workstation or at least reviewed as an animated movie (Figs. 8.1, 8.2, 8.3, 8.4, 8.5, 8.6, and 8.7). This cannot be demonstrated in this two-dimensional book and is therefore displayed limitedly.
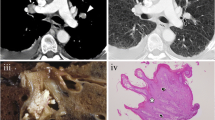
Nonenhanced thin-section CT scan of a 26-year-old female who underwent bilateral lung transplantation 6 months before due to cystic fibrosis. She went to hospital due to recurrent fever, emesis with some nonproductive cough, and global deterioration. FEV1 was 2.3l (71%). CMV pp65 antigenemia was mild positive (260 IU/ml). Bronchopneumonic infiltration was evident on CT in the right lower lobe (B + C) as well as the causal stenosis of the right main stem bronchus (a). Multiplanar reformat and postprocessing helped to identify the stenosis and to quantify its severity and extent (b, c, d). Virtual bronchoscopy was calculated for demonstration purposes and matches well with real bronchoscopic view. Biopsy was taken to differentiate between graft rejection and infection (the latter was the reason). (a) Transversal CT scan, (b) coronal reformat, (c) paracoronal reformat (single oblique), (d) surface-shaded rendering, (e) virtual bronchoscopy
The 57-year-old patient acquired 30 pack years and suffered from COPD IV°. She was planned for interventional emphysema therapy and therefore underwent paired inspiratory (a) and expiratory (b) thin-section CT scan. A special window-level setting (width 1,000 HU, level – 800 HU) demonstrated the inhomogeneous density of the lung parenchyma in both breath holds (a + b), especially in the expiratory one (b). There are subsegmental regions with adequate increase after expiration (right lower lobe), representing a relative increase of tissue per voxel. In contrast, other subsegmental areas did not change their density in expiration (left lower lobe), indicating air trapping as an indirect sign of obstructive small airway disease. Besides the indirect signs, also direct collapse of the segmental airways is visible in this image pair: All segmental bronchi are open at inspiratory CT (a), while almost all airways appear to be collapsed at the expiratory scan (b)
(a + b) Prescan, (c + d) presentation, and (e + f) 6 months later, (a + c + e) at an lower lobe segmental ramification level. (b + d + f) Bronchus intermedius level. The 70-year-old patient was upper lobectomized right 4 years before due to stage I non-small-cell lung cancer and reported cough and bronchial infection since some weeks. The CT scan (c + d) demonstrated focal ill-defined nodules in the right lower lobe (c), which were newly developed as compared to the prescan (b). While analyzing the feeding bronchi, a bronchial kinking was evident in middle and right lower lobes. Together with the evident clinical symptoms, this was rated as bronchopneumonia, while pulmonary metastases were considered unlikely. The findings disappeared at the routine follow-up (e + f), indicating the infection to be treated successfully
The 81-year-old patient acquired 40 pack years and suffered from COPD III. He was planned for interventional emphysema therapy and therefore underwent paired inspiratory (a + c) and expiratory (b + d) thin-section CT scan. The comparison of the mainstem bronchi at inspiratory and expiratory CT indicates a relevant luminal change. The coronal reformat of the expiratory scan shows severe staring artifacts due to respiratory effect (d): Expiratory breath holding requires more compliance and pulmonary reserve as compared to inspiratory breath holding and is therefore frequently limited in patients suffering from severe lung disease. In this clinical scenario, fast CT scanning is relevant in particular since respiration artifacts occur in the expiratory scan (d). (a) Inspiratory breath hold, (b) expiratory breath hold, (c) coronal reformat of inspiratory breath hold, (d) coronal reformat of expiratory breath hold
(a) inspiratory breath hold, (b) expiratory breath hold, (c) maximal lumen in cine-CT, (d) expiratory breath hold. The 67-year-old patient was tracheotomized after substitution of mitral valve due to postoperative complications including seizure and pneumonia 2 months ago. Paired inspiratory and expiratory CT showed stenosis of the trachea at the level of tracheotomy (a + b). Cine-CT acquired during continuous respiration demonstrated additionally a relevant collapse at this level (c + d). Thus, an end-to-end resection of 3.5-cm trachea was performed
The 61-year-old male patient acquired 60 pack years and presented COPD IV (FEV1 0.5 l, 6-min walk test 150 m). CT revealed severe diffuse bilateral centrilobular emphysema (emphysema index 48%, 15th percentile -983HU). After endobronchial placement of three valves in the right upper lobe, subtotal upper lobe atelectasis was observed and analysis improved to FEV1 0.8 l (25%), 6-min walk test 200 m, emphysema index 46%, and 15th percentile -981HU. (a) Prescan, (b) post valve implantation
While transversal CT images are frequently sufficient for evaluating many of the airway abnormalities, there are several limitations that should lead to further postprocessing:
-
Inadequate representation of airways oriented obliquely to the axial plane
-
Underestimation of the three-dimensional extent of disease and therefore
-
Limited possibility to visualize the complex three-dimensional relationship of the disease to airways and adjacent mediastinal structures
-
Impossibility to display the surfaces and therefore stenosis of airways that lie parallel to the transversal plane (Figs. 8.1 and 8.8)
Fig. 8.8 The 68-year-old male patient presented with dyspnea. Global airway quantification from CT revealed a mean wall percentage of 45.5% in the baseline scan (mean wall thickness, 1.28) and a mean wall thickness of 46.6% in the follow-up scan (mean wall thickness, 1.43 mm). Thus, a relevant increase in the global bronchial wall thickness was measured. (a) Baseline, (b) 2-year follow-up
Due to the need of thin-section volumetric CT, a large number of images containing hundreds of images are generated. As a consequence, the use of retrospectively reconstructed 2D and 3D images should be considered routinely in preparation of bronchoscopy. MSCT starts with a reconstruction of these two-dimensional images, which can be reformatted in further dimensions. Adequate imaging of the airways to be reformatted, visualizing down to a segmental level requires a maximal slice thickness of 1 mm or below. If thinner slices and/or larger overlap are available (typically 0.5–0.75 mm, 50% overlap), especially small lesions, thin stenosis and oblique structure are significantly better visualized after reformat. These thin sections require substantial storage capacity at the scanner, at the postprocessing workstation, and at the PACS (picture archiving computer system). However, they are essential for adequate postprocessing (30 cm long, 0.75-mm slice thickness, 50% overlap \( \Rightarrow \)600 images \( \Rightarrow \)300 MB). Fast data acquisition is also essential in imaging of the airways since many patients suffer from dyspnea. Severe artifacts as a result of continuous respiration cut the diagnostic quality impressively and occur in secondary reformats (Fig. 8.4d).
The usage of nonenhanced low-dose technique (e.g., 70mAs as in Fig. 8.1) is sufficient to evaluate the central airways and the peripheral airways as well if three-dimensional reformats are intended. Also, emphysema quantification requires nonenhanced scans; intravenous contrast enhancement might be used if additional questions are to be answered (e.g., pulmonary embolism, relationship to a tumor or vessel). Additional acquisitions paired inspiratory and expiratory breath hold, cine-CT [,] or in prone position can help to evaluate airway stability (bronchial collapse) and air trapping as a sign of obstructive small airway disease (Figs. 8.2 and 8.5).
Multiplanar Reformation
Besides cross-sectional postprocessing with multiplanar reformats, surface-shaded techniques are helpful to display the tracheobronchial tree from inside. Virtual bronchoscopy (VB) as an artificial substitute to real bronchoscopy (RB) allows for similar inspection of the central airways. In contrast to real bronchoscopy, the user can pass an obstructing lesion, accurately measure its dimension, and turn round the virtual bronchoscope to take a look from each direction onto a lesion, including backward from distal to proximal. Also, the time effort is limited by neither patient nor anesthesia. However, color coding in VR is artificial and might be misleading (e.g., mucus might appear as soft tissue), spatial resolution is worse, and the interventional manipulative options of RB are missing. Thus, VB is mainly complementary to bronchoscopy in the assessment of patients with suspicion of airway stenosis. To get advantages of both techniques, CT should be done prior to bronchoscopy as a navigation system. This provides valuable information, e.g., whether the airway is obstructed by extrinsic compression, intraluminal disease, or an intrinsic airway disease. Also, the relationship of the airway to the adjacent anatomy is displayed by cross-sectional imaging. CT is therefore essential in decision whether the patient is a candidate for surgical resection, radiation therapy, or interventional treatment. If airway stenting is planned, CT findings can help to determine the type, size, and length of the individually appropriate stent. Then, several techniques are available to merge computer-assisted VR and RB in real time.
Interventional Lung Volume Reduction
Besides conservative treatment of patients suffering from severe emphysema and lung transplantation, a variety of surgical and interventional strategies are established and under investigation to improve the function of residual lung parenchyma. The main mechanism is the interventional or surgical deflation of severely emphysematous destroyed lung parenchyma. Those procedures can either be reversible (device placement) or irreversible (i.e., glue or steam instillation or surgical resection). For adequate identification of the individual treatment strategy and optimal target identification, the extent and severity of disease as identified by CT has proved one of the most important predictors of a successful outcome (Fig. 8.7). Currently CT-based fissure analysis is paid attention to predict collateral ventilation and/or prediction of atelectasis. Besides the morphological information as derived by CT, regional functional data from V/Q scanning is applied here. In the future, CT perfusion mapping as well as MRI based perfusion and ventilation mapping will play a relevant role to identify the optimal target for regional emphysema treatment as well as for monitoring of lung disease in conservative therapies.
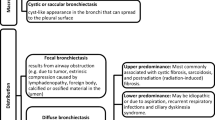
Bronchial Wall Quantification
In diffuse bronchial disease such as COPD or cystic fibrosis, the global quantification of bronchial wall thickness might serve as a surrogate parameter of the activity, e.g., of inflammation (Fig. 8.8). Therefore, several approaches have been introduced to measure the bronchial wall thickness at several localizations with or without computer assistance. Selection bias, spatial volume effect, and limited reproducibility are some of the limitations herein which can partially be overcome by a global quantification of all bronchial walls. This approach, however, is biased mainly by the assessment of bronchi for segmentation, which might be caused, e.g., by mucus impaction.
Suggested Reading
Amdo T, Godoy MC, Ost D, Naidich DP. Imaging–bronchoscopic correlations for interventional pulmonology. Radiol Clin North Am. 2009;47(2):271–87. doi:10.1016/j.rcl.2008.11.005.
Naidich DP, Gruden JF, McGuinness G, et al. Volumetric (helical/spiral) CT (VCT) of the airways. J Thorac Imaging. 1997;12:11–28.
Grenier PA, BeigelmanAubry C, Fetita C, et al. Multidetector-row CT of the airways. Semin Roentgenol. 2003;38:146–57.
Heussel CP, Kappes J, Hantusch R, Hartlieb S, Weinheimer O, Kauczor HU, Eberhardt R. Contrast enhanced CT-scans are not comparable to non-enhanced scans in emphysema quantification. Eur J Radiol. 2009;74(3):473–8.
Ederle JR, Heussel CP, Hast J, Fischer B, Van Beek EJ, Ley S, Thelen M, Kauczor HU. Evaluation of changes in central airway dimensions, lung area and mean lung density at paired inspiratory/expiratory high-resolution computed tomography. Eur Radiol. 2003;13(11):2454–61.
Fleiter T, Merkle EM, Aschoff AJ, et al. Comparison of real-time virtual and fiberoptic bronchoscopy in patients with bronchial carcinoma: opportunities and limitations. Am J Roentgenol. 1997;169:1591–5.
Finkelstein SE, Schrump DS, Nguyen DM, et al. Comparative evaluation of super high-resolution CT scan and virtual bronchoscopy for the detection of tracheobronchial malignancies. Chest. 2003;124:1834–40.
Eberhardt R, Kahn N, Gompelmann D, Schumann M, Heussel CP, Herth FJF. LungPoint®: a new approach to peripheral lesions. J Thoracic Oncol. 2010;5:1559–63.
Eberhardt R, Anantham D, Herth F, Feller-Kopman D, Ernst A. Electromagnetic navigation diagnostic bronchoscopy in peripheral lung lesions. Chest. 2007;131:1800–5.
Heussel CP, Ley S, Biedermann A, Rist A, Gast KK, Schreiber W, Kauczor H-U. Respiratory lumenal change of pharynx and trachea in normal subjects and COPD patients: assessment by cine-MRI. Eur Radiol. 2004;14:2188–97.
Boiselle PM, Ernst A. State-of-the-art imaging of the central airways. Respiration. 2003;70:383–94.
Sciurba FC, Ernst A, Herth FJ, Strange C, Criner GJ, Marquette CH, Kovitz KL, Chiacchierini RP, Goldin J, McLennan G. VENT Study Research Group: a randomized study of endobronchial valves for advanced emphysema. N Engl J Med. 2010;363:1233–44.
Sanchez PG, Kucharczuk JC, Su S, Kaiser LR, Cooper JD. National Emphysema Treatment Trial redux: accentuating the positive. J Thorac Cardiovasc Surg. 2010;140:564–72.
Nakano Y, Muro S, Sakai H, Hirai T, Chin K, Tsukino M, Nishimura K, Itoh H, Paré PD, Hogg JC, Mishima M. Computed tomographic measurements of airway dimensions and emphysema in smokers. Am J Respir Crit Care Med. 2000;162:1102–8.
Weinheimer O, Achenbach T, Bletz C, Duber C, Kauczor H-U, Heussel CP. About objective 3D analysis of airway geometry in computerized tomography. Trans Med Imaging. 2008;27:64–74.
Acknowledgements
Dr. rer. nat. Oliver Weinheimer for the development of the fully automatic analyzing YACTA software and the processing of so many CT data sets (Figs. 8.7 and 8.8).
Miss Melanie Segovic for the analysis of many CT data sets in adequate quality and the reliable data management together with Carola de Silva.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Heussel, C.P. (2013). Airway Imaging. In: Ernst, A., Herth, F. (eds) Principles and Practice of Interventional Pulmonology. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-4292-9_8
Download citation
DOI: https://doi.org/10.1007/978-1-4614-4292-9_8
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-4291-2
Online ISBN: 978-1-4614-4292-9
eBook Packages: MedicineMedicine (R0)