Abstract
The purpose of this study was to use cine-MRI during continuous respiration to measure the respiratory lumenal diameter change in the pharynx and at an upper tracheal level. Fifteen non-smokers and 23 chronic obstructive pulmonary disease (COPD) patients with smoking history (median 50 pack-years) were included. Cine-MRI with seven frames/s was performed during continuous respiration. Minimal and maximal cross-sectional lumenal diameters within the pharynx and the upper tracheal lumen area were measured. The median diameter change in the pharynx (tracheal area) was 70% (1.4 cm2) in volunteers and 76% (1.7 cm2) in smokers (P=0.98, P=0.04). Tracheal lumenal collapse was a median of 43% in volunteers and 64% in smokers (P=0.011). No clear disease-related difference of the pharynx-lumen was found. The maximal cross-sectional area of the upper trachea lumen as well as the respiratory collapse was larger in COPD patients than in normal subjects. This information is important for the modelling of ventilation and prediction of drug deposition, which are influenced by the airway diameter.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The respiratory lumenal diameter change of the airways plays a significant role in a variety of diseases. Obstructive sleep apnoea syndrome (OSA) [1–4], chronic obstructive pulmonary disease (COPD) [5–8], Wegener’s granulomatosis [7], tracheobronchomalacia [7, 9] and neoplasm [10] are known to affect the mechanical properties of the airways. Due to the significant difference of mural properties, at least the upper and lower airways have to be considered separately. The wall of the upper respiratory tract is completely different from the wall of the tracheobronchial tree: the tracheal and bronchial walls are characterised by cartilage and elastic fibres. In the pharynx, in contrast, voluntary muscular movement of, e.g., the tongue and passive movement of the soft palate coexist and affect lumenal diameter.
Examples for the medical necessity to pay separate attention to the upper respiratory tract are mask anaesthesia [11, 12], modelling of ventilation [13], deposition of inhaled drugs [14] or calculation of airway elasticity, e.g., for monitoring progression of COPD. A deposition of 46–98% of the inhaled drugs in the upper airways is known [15]. This depends on the individual shape, lumen and potential incidental movement of the pharyngeal muscles: aerosols might precipitate and therefore deposit in the pharynx. This is unfavourable for intended pulmonary delivery for the topic (e.g., spasmolysis) or the upcoming application of systemic drugs (e.g., insulin or morphine). Dynamic changes of the tracheobronchial tree are currently not taken into account for modelling of inhaled therapies [14]. A profound knowledge about the cyclic behaviour of the whole respiratory tract during respiration is necessary. This is crucial in airway disease, such as COPD, which is characterised by the narrowing and/or collapse of airways due to a loss of elastic fibres [6]. This leads to broncho-spasm, air-trapping and emphysema [6], which are reflected by the changing of certain parameters in lung function testing. These changes can be correlated with functional imaging parameters [8] such as forced expiratory volume in one second (FEV1), which reflects large airway obstruction and intrathoracic gas volume/functional residual capacity (ITGV/FRC), which corresponds to hyperinflation, and air trapping reflects air-trapping.
Usually, an inspiratory CT scan is used for imaging of the airways [10]. However, changes of the airway lumen and lung during respiration have a major effect on these measurements [7, 9, 16]. Therefore, paired inspiratory and expiratory CT scans are obtained to compare different respiratory phases [8, 16, 17]. This approach considers two separate respiratory breath-holds. However, the dynamic respiratory lumenal diameter change is not addressed. After closing the vocal cord for a breath-hold, the intratracheal pressure can be positive, and the airways can be distended. During continuous respiration, however, negative pressure and a significant airway collapse can occur. This is not detected by paired CT scans [7, 9]. Therefore, dynamic cine-CT is used, e.g., in the investigation of tracheomalacia as an alternative [7–9, 14]. Though relevant the local radiation dose is a major restriction for cine-CT. Cine-MRI offers the possibility for radiation-free dynamic imaging at least within the upper respiratory tract [4, 7].
The purpose of this study was to use cine-MRI as a dynamic single-slice technique during continuous respiration to measure the respiratory lumenal diameter change in the pharynx and the upper trachea.
Material and methods
Patients
After approval of the local ethics committee and signed informed consent, 15 healthy life-long non-smokers [FEV1>70% predicted, median FEV1: 85%, median age 62 years, range 48–74 years, median body-mass index (BMI) 25 kg/m2, range 16–35 kg/m2] and 23 continuous in-patients and out-patients of the Pulmonology Department suffering from COPD (FEV1<70%, median FEV1: 61%, smoking history median 50 pack-years, range 15–100 pack-years, median age 59 years, range 41–68 years, median BMI 27 kg/m2, range 21–32 kg/m2) were included prospectively into the study. A lung function test was performed within 1 week before MRI. Bronchodilators were stopped 24 h before the examination. Computed tomography was available in 21/23 (chest X-ray: 2/23) COPD patients with a median interval to MRI of 5 days and in 4/15 healthy volunteers. Evidence of emphysema was scored from 0= none to 3= severe by a chest radiologist.
Cine-MRI
Cine-MRI was performed on a Siemens Magnetom Vision 1.5-T (Siemens Medical Systems, Erlangen, Germany) in the supine position using a head/neck array coil. Imaging started with localisation of the upper respiratory tract using transversal gradient echo scout images and T2-weighted half-Fourier single-shot turbo spin-echo (HASTE) images. An ultrafast spoiled gradient-echo pulse sequence with spin-density weighting was used for cine-MRI during continuous respiration. Imaging parameters were: repetition time 2.4 ms, echo time 1.2 ms, flip angle 8°, field of view 300 mm, acquisition matrix 54–64×128 and slice thickness 8 mm. The acquisition time was 140–150 ms/image (approximately seven frames/s); imaging was performed for 13 s. Images were acquired continuously without inter-scan delay or trigger. Before image reconstruction, raw data were hamming filtered, zero filled to a 256×256 raw matrix, and then reconstructed using a half-Fourier algorithm.
Gradient noise prevented oral communication. Therefore, patients were instructed prior to image acquisition to breath slowly and deeply through the open mouth during imaging. Slices were positioned in the oropharynx (hard palate), base of the tongue (soft palate) and subglottic trachea (Fig. 1). Respiratory airflow and chest wall or diaphragmatic excursion were not measured at this stage of the investigation. This information can in principle be archived using a simultaneous pneumotachography and a separate cine-MR measurement, since the chest is not covered with the used coil.
Three cine measurements were performed in the coronal, oblique and transverse orientation, respectively. The sequence plane was positioned perpendicular to the respective airway lumen. Sagittal imaging was performed additionally for demonstration purposes. The whole MRI examination took about 15 min.
Image analysis
The signal-to-noise ratio was signal measured in a ROI within the pharyngeal muscle divided by the standard deviation of background noise. The signal intensity reached its steady-state value within the first ten images. Therefore, measurements were evaluated beginning with image number 11 of each respective series. The measurements were done manually by a blinded experienced radiologist on a workstation (Magic-View, Siemens Medical Systems, Erlangen, Germany) using a standard window/level setting of 150/40 (Fig. 2). The “draw in segment” ROI mode generates a ROI that is fixed to a certain monitor position and calculates the ROI parameters actually as an image appears at this view-port. This mode enables image scrolling (cine review) using a constant ROI with a pre-defined threshold setting and automatically updated ROI results (Figs. 3, 4, 5, 6, 7, 8, 9, 10). Images showing swallowing were excluded.
Dynamic change of right-left and cranio-caudal distance in the palate in a COPD patient and in a volunteer. The time unit in the x-axis is the image number, while the frame time is 150 ms. Note that the curves show several respiratory cycles. No clear respiratory-associated oscillation can be detected
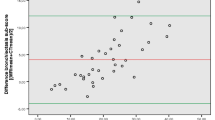
Dynamic change of cross-sectional area (cm2) in upper trachea in a COPD patient and in a volunteer. The time unit in the x-axis is the image number, while the frame time is 150 ms. Note that the curves show several respiratory cycles. The COPD patient demonstrated two different amplitudes in cross-sectional tracheal lumen during the first, and the two following cycles. However, the amplitudes in the three depicted respiratory cycles of the volunteer are quite uniform
Box-whisker plot (quartile) maximum change in diameter of the palate relative to the individual maximal lumen. Separate measurement of distances in left-right and cranio-caudal direction and simplified calculation of relative cross-sectional change in diameter by multiplication of absolute values. No relevant difference between COPD patients and volunteers is evident
Box-whisker plot (quartile) of the tracheal collapse relative to the individual maximal lumen, e.g., 100% collapse describes a total collapse, 20% collapse describes a decrease of the lumen by 20% during respiration. A relevant difference between COPD patients and volunteers is evident (P=0.011) and a primary result of the larger maximal lumen of the trachea in smokers (Fig. 4)
Coronal cine-MRI of the palate in COPD patients (65-year-old male, 75 pack-years, bronchial carcinoma, FEV1=56%, 70-year-old male, 70 pack-years, FEV1=30%, 64-year-old male, 70 pack-years, suspicion of bronchial carcinoma, FEV1=65%) and a volunteer (65-year-old female, FEV1=93%) demonstrating minimal and maximal right-left diameter (arrow) [(see Electronic Supplementary Material)]
Trachea
In the upper trachea, a double-threshold-based measurement on a transversal plane using a ROI that includes the trachea and the adjacent tissue was feasible due to the high signal intensity of tissue surrounding the trachea (Fig. 9): the lower threshold was set to zero. The upper threshold was set to signal noise plus two times the standard deviation of the noise. The values for the resulting lumen curve was assessed manually for the whole respiratory cycle and is shown exemplarily in Fig. 3. The analysis of the dynamic change of the cross-sectional area was done visually using a graph as shown in Fig. 3. The constriction of the lumen was calculated relative to the maximal cross-sectional area. A collapse of more that 50% of the maximal cross-sectional area was assessed as pathological collapse, keeping the varying technique into mind [18].
Palate
Compared with this, threshold-based measurement of the cross-sectional area of the palate was not feasible (Figs. 1, 2, 8). Low signal of the adjacent cortical bone and teeth as well as metal artefacts resulted in false high values of an initially planned threshold-based measurement (leaking out of segmentation) [(Fig. 8)]. Therefore, a different (i.e., manual) approach using anatomical landmarks on a coronal plane was necessary. Initially, the images demonstrating the widest and narrowest distance were selected manually using a cine review mode of the image stack [7, 9]. After that, reproducible anatomical landmarks were used for measurement of the maximal and minimal lumenal diameter using an automatic ruler. In contrast to that, the lumenal diameter in all images of a respective series was measured for demonstration purposes only in a single case per group (Fig. 2). A simplified cross-sectional area was calculated as the product of minimal and maximal cranio-caudal and right-left distance. Since anatomical landmarks in the soft palate were not reproducible due to irregular, chaotic and multi-plane movement during respiration, the measurement of the soft palate lumen was omitted from this trial.
Statistical analysis
The cross-sectional collapse of the trachea and palate in volunteers and COPD patients was considered a major variable. Data were tested using a Wilcoxon test for non-normal data. In these, a probability of error (P) less than 5% was considered to be significant. The Pearson test was used for correlation analysis.
Results
MRI
The cine-MRI sequence achieved a sufficient signal-to-noise ratio of 40, which enables automatic measurement of the upper tracheal lumen as described above.
Palate
Cranio-caudal
The minimal cranio-caudal diameter of the palate as measured manually in a coronal plane was a median of 0.6 cm (range 0.0–1.3 cm) in volunteers and 0.7 cm (range 0.2–1.4 cm) in COPD patients. The maximal cranio-caudal diameter of the palate was a median of 1.4 cm (range 0.6–2.1 cm) in volunteers and 1.4 cm (range 0.9–2.1 cm) in COPD patients. The relative change in the cranio-caudal diameter of the palate was a median of 53% (range 33–100%) in volunteers and a median of 49% (range 26–88%) in COPD patients (P=0.20) [(Table 1)].
Right-left
The minimal right-left diameter of the palate as measured manually in a coronal plane was a median of 1.8 cm (0.0–2.7) in volunteers and 1.7 cm (range 0.6–5.2 cm) in COPD patients. The maximal right-left diameter of the palate was a median of 3.6 cm (range 2.1–5.8 cm) in volunteers and 3.3 cm (range 1.9–6.2 cm) in COPD patients. The relative change in right-left diameter of the palate was a median of 45% (range 16–100%) in volunteers and a median of 45% (range 3–84%) in COPD patients (P=0.39) [(Table 1)].
Cross-section
There was a moderate correlation of the relative individual change of the right-left palate diameter with the cranio-caudal palate diameter in volunteers (r=65%), whereas in COPD patients no relevant correlation was found (r=43%).
The median of the simplified calculated relative cross-sectional change in the diameter of the palate was 78% (range 40–100%) in volunteers and 76% (range 37–93%) in COPD patients (P=0.98) [(Fig. 5)]. No relevant correlation was found between the simplified calculated relative cross-sectional maximum change in diameter of the palate and FEV1 (r=−0.15).
The curve of the complete set of diameters in the palate during the whole respiration cycle (measured exemplarily for demonstration purposes) is displayed in Fig. 2. An increase and decrease of the distances without a clear frequency or oscillation can be seen (Fig. 2).
Trachea
The minimal cross-sectional area of the upper trachea as measured automatically in a transversal plane was a median of 0.8 cm2 (range 0.2–1.5 cm2) in volunteers and 0.8 cm2 (range 0.0–2.0 cm2) in COPD patients (P=0.28). The maximal cross-sectional area of the upper trachea was a median of 1.4 cm2 (range 0.6–2.1 cm2) in volunteers and 1.7 cm2 (0.7–3.4 cm2) in COPD patients (P=0.04). A moderate correlation was found between relative tracheal collapse and FEV1 (r=−0.58). Taking the threshold of 50% for pathological tracheal collapse into account [18], a pathological collapse occurred in 5 out of 15 volunteers and in 16 out of 23 COPD patients.
The relative collapse of the trachea resulted in a median of 42% (range 20–83%) in volunteers and 64% (range 29–100%) in COPD patients (P=0.011). That means a collapse by 2/5 of the lumen in volunteers and by 3/5 of the lumen in COPD patients (Fig. 6) [(Table 1)].
Due to the semiautomatic measurement of the cross-sectional tracheal lumen, curves of the respiratory cycle were evaluated (Fig. 3). An oscillation became obvious with a frequency of about 10–15 min−1 (i.e., 25–40 images at 150 ms), which appears to correspond to a typical respiration frequency. However, due to the lack of respiratory registration this connection remains uncertain (Fig. 3). In the visual assessment of these curves, two different amplitudes have been detected in 8 out of 23 COPD patients, whereas the amplitude of the remaining COPD patients and all volunteers was uniform in visual assessment (Fig. 3). The median cross-sectional collapse of the trachea in this subgroup of eight COPD patients was 77% (range 37–95%) and was also significantly higher in comparison to the volunteers (P=0.002).
Chest imaging
A median emphysema score of 2 (moderate) was rated in 23 COPD patients. This score did not show any influence upon tracheal collapse and breath-by-breath variability in COPD patients.
Discussion
Respiratory changes of the whole airways have clinical impact, e.g., in OSA [1–4], clinical importance, e.g., for monitoring of drug treatment in COPD and scientific effect, e.g., in ventilation modelling for drug deposition [14].
Inhalation
Since actual developments introduce inhalative drug application, modelling of drug distribution is a central task in this progress [14, 15]. The airway diameter affects air velocity. The margin of convective and diffusive gas transport is affected by airway size, which influences drug deposition. The upper respiratory system also has a large influence upon the distribution of inhaled air or drugs. Individual CT scans of the whole airway tract [14] and stereolithographically made anatomical models [15] have already been used for modelling and measurement of aerosol distribution. However, they were acquired during a static inspiratory breath-hold. Any dynamic change during respiration was neglected. But dynamic changes in the airway lumen will clearly affect air velocity and drug deposition [14, 15]. Especially in COPD patients, collapse as well as a dilatation of the airways after a deep breath are known as a result of a loss of (elastic) connective tissue support [6, 19].
As FEV1 reflects best the progression of COPD, it was used as an inclusion criterion (together with appropriate smoking history) to differentiate a group of COPD patients from normal subjects [20]. The correlation of airway collapse was moderate, possibly since the underlying breathing manoeuvres are totally different (forced expiration in lung function analysis, slow breathing in cine-MRI).
Airway function
The tracheal shape (e.g., saber sheath trachea) and respiratory motion of the tracheobronchial tree has already been addressed, especially in CT trials [8, 17, 21]. Using paired inspiratory and expiratory scans, the cross-sectional area of the trachea and the main-stem bronchi was significantly higher in inspiration compared to expiration [17]. However, this approach provides limited information concerning the dynamic (patho-)physiological process in trachea, bronchi and lung parenchyma [7, 9]. Therefore, no relevant difference in airway diameters was obtained on paired CT techniques among obstructive, restrictive and pulmonary unimpaired patients [17, 21]. However, significant differences in the tracheal shape were found between inspiratory and expiratory scans [21]. Thus, cine-CT and cine-MRI already have been introduced into dynamic respiratory imaging of tracheal instability [7, 9].
Cine-MRI
Cine-MRI has already been used in imaging fast moving processes. In periodical events with a high reproducibility such as beating of the heart, segmented k-space filling is an option to acquire sufficient signal [22]. Since respiration has a limited reproducibility (Fig. 3), the use of a respiration trigger for measurement of airway wall imaging is limited. However, it has been introduced in vocal phonation [23] and is currently under development for non-breath-hold lung imaging. Therefore, continuous dynamic imaging has been tested previously [4, 24]. Clinically relevant information concerning pharyngeal lumenal diameter change has been obtained, even with a limited temporal resolution of approximately one frame/s [4, 24]. Our sequence used a similar approach with a lower spatial resolution (matrix of 128×128), while increasing the temporal resolution to approximately seven frames/s [7]. Comparing the images from Mrs Donnelly et al. [4] as a movie (http://radiology.rsnajnls.org/cgi/content/full/223/1/176/DC1, 21/3/03) and those acquired during this trial side by side, and looking at the temporal curve as shown in Fig. 3, the necessity for more than one frame/s becomes obvious. This limitation is probably a result of performing the trial in paediatric patients [4, 24]. In these patients, signal and the field of view are limited. A pixel size of 2.3 mm (interpolated 1.2 mm) limits the accuracy of distance and area measurement in the faster sequence than we used. The zigzag line in Fig. 3 is probably a result of this limitation together with image noise. Another limitation is the uncertainty whether a collapse takes place during inspiration or expiration, at the beginning or in-between, and whether the tidal volume has an effect. These interesting questions could be answered using pneumotachography [1, 3], which was not part of this first trial. However, this technique might be helpful, e.g., in a further clarification of incidentally deep breathing COPD patients (see below) and to improve the functional input into ventilation and inhalation modelling algorithms. The time point of lumenal change might be valuable information, e.g., for modelling of drug deposition since inhalation is usually applied at early inspiration [14].
Endoscopic and fluoroscopic investigations do not suffer from limited temporal resolution [4, 7], but superimposition is a major limit. Direct or indirect inspection is limited to the upper view, and local irritation will prevent normal local lumenal diameter change [9, 7]. Cine-CT is used, e.g., in the investigation of tracheomalacia as a relevant alternative [7–9, 14]. Since a local radiation dose of more than 50 mGy for a single scan is a restriction [7], its use for functional imaging has to be indicated carefully. The nearness of lens and thyroid as radiation sensitive organs worsens this circumstance. In fact, COPD patients do not suffer from a malignant disease, but life expectancy is limited by the loss of lung function as the disease progresses [25]. Finally, the short-term repetition that might be necessary for monitoring of drug-treatment might cause dose accumulation.
However, the simultaneous high spatial (sub-millimetre) and temporal resolution (ten frames/s using incremental reconstruction at a rotation time of less that 500 ms) of cine-CT is outstanding and cannot be reached by current MRI technique [7, 9]. On the other hand, MRI offers the possibility for imaging in free planes; however, especially MRI is limited to the supine (or prone) positions. Coronal cine-CT can be done in a recline position, whereas sagittal cine-CT of the neck cannot be performed. Thus, in principle, all functional pharyngeal distances and upper trachea lumen area, as measured in this trial, could be obtained using cine-CT and cine-MRI as well. Cine-MRI was the appropriate tool in this trial for comparison of COPD patients with volunteers due to ethical and radiation reasons. In individual planning, however, cine-CT would promise more reliable data [7, 9].
Dynamic airway diameter change
Palate
No clear respiratory lumenal diameter change of the soft palate, tongue and hypopharynx could be visualised at cine-MRI of the pharynx in patients and volunteers (Figs. 7a,b, 10) [4, 24]. Thus, no significant difference between both groups could be obtained. A sampling error due to a mismatch in BMI was excluded. This fact would influence also the patient’ positioning as visible in Fig. 7a,b as compared to Fig. 7c,d. If there is a disease-related change in the respiratory lumenal diameter change of the pharynx, the included subject number either was to small or the extent could not be differentiated from voluntary muscle motion. Probably, an investigation during sleep could overcome this limitation. Since the sequence is very loud, subjects will wake up at once. Sedation for this kind of study does not seem to be ethically reasonable and alters, e.g., muscular tonicity. On the other hand, the influence of lip position upon airflow characteristics is known and was only controlled to a limited degree by the patient instruction, “open mouth” [26].
The respiratory motion inside the pharynx is a result of active and passive movement of the tongue and palate. Their changes during sleep have already been investigated extensively [4, 12]. In sedation, a relevant movement of the nasopharynx, oropharynx and hypopharynx was found in normal subjects [4]. Significantly more pharyngeal collapses have been seen in young patients suffering from OSA, compared to normal subjects [24]. Even an increase in lung resistance, caused by a collapse of the upper airways, has been detected in patients suffering from OSA [3].
Trachea
While the minimal cross-sectional area of the upper trachea was comparable in COPD patients and volunteers, a larger maximal cross-sectional area was observed in COPD patients (Figs. 2, 4). The detected absolute value of the tracheal lumenal area in normals (0.8–1.4 cm2) is smaller as compared to literature (1.8–2.8 cm2) [18]. This is probably a result of a totally different technique (MR, limited spatial resolution, local gradients) and eventually also the investigated level of the trachea (aortic arch [18] vs. extrathoracic).
After compilation of the tracheal cross-sectional area, a significantly higher relative collapse was found in COPD patients as compared to volunteers. Furthermore, 70% of COPD patients demonstrated a collapse of more than 50%. Stern et al. describe this decrease as pathological; however, a different technical approach was used [18]. Thirty percent of volunteers also showed a pathological collapse after all. This points out that the calculated values of tracheal lumen collapse in the present study cannot be interpreted using the 50% threshold alone derived from previous studies and different techniques and patients [18]. This contains a reference to the clinical importance of the larger maximal cross-sectional area, which was observed in COPD patients (Figs. 2, 4).
A higher relative collapse can be mathematically the result of a higher maximum, a lower minimum or both. This means that COPD patients have a higher maximal cross-sectional area of the upper trachea, which collapses significantly more than in volunteers, down to a comparable size to volunteers. This instability of the tracheal wall fits well to the known loss of elastic fibres, which enables inflation and collapse during respiration (Figs. 2, 4) [6]. Furthermore, airway dilatation after a deep breath is known in COPD patients [19].
This can also be an explanation for the visually detected different amplitudes in 8 out of 23 COPD patients, while all volunteers demonstrated uniform respiration (Fig. 3). Even during the requested respiratory procedure, COPD patients incidentally breathe more deeply (had a sigh) [27, 28]. These findings influenced the calculation of tracheal collapse (Fig. 6). The breath-by-breath variability depended mainly upon irregularities in tidal breathing, and has also been described previously [27, 28]. Patients suffering from COPD not only have altered blood-gas and acid-base status, but also have different mechanical constraints to breathe and a different pattern of muscle recruitment for respiration as compared to normal subjects [27]. However, the variability between volunteers and COPD patients was not different, tested at rest and exertion [27]. However, the size of the subgroup identified in this trial appears to be too small for further interpretation. Furthermore, no online physiological data were recorded because this finding was beyond the horizon of this trial.
Finally, the discussed results of larger maximal diameter together with higher collapse of the upper trachea in COPD patients cannot be easily transferred to the lower airways. Since the extrathoracic trachea can easily be measured using cross-sectional imaging, in vivo data can be obtained. This is more difficult in the intrathoracic trachea and bronchi, since respiratory movement and oblique course biases the accuracy of luminal measurement [7, 9, 17]. Intratracheal trachea was not measured in this trial since only the upper trachea was covered with the used neck coil. Additionally to the respiratory cranio-caudal movement of carina and central bronchi, a pilot using body coil scans demonstrated an anterior-posterior postponement of these structures, which leave the section during breathing (not shown). Together with the oblique course of bronchi, cine-CT or cine-MR is not possible using the current technique. Up to now, bronchial lumen measurement is limited to paired inspiratory-expiratory scans together with manual correction for the anatomical position [17]. Doing this, significantly smaller diameters have already been measured on expiratory scans compared to inspiratory scans [17].
Dynamic investigations (i.e., during respiration) in this anatomical region are actually limited to ex vivo trials, e.g., specimens after surgical resection or in animal models [19]. These references report unexpected findings in the behaviour of airways derived from COPD patients, probably due to the loss of alveolar attachment [19]. In the future, the use of a 16-slice CT scanner with respiratory trigger and gating capabilities together with a low pitch factor will deliver four dimensional data-sets for the dynamic evaluation of the whole lung and the whole tracheobronchial tree.
Conclusion
-
Sufficient spatial and temporal resolution for dynamic imaging of the pharynx and upper trachea during continuous respiration was achievable using cine-MRI.
-
Cine-MRI for measurement of dynamic lumenal diameter change of the upper trachea is a possible tool for therapeutic monitoring, e.g., in new therapeutic strategies for treatment of COPD.
-
Obvious respiratory motion within the pharynx was detectable; however, no clear disease-related difference between COPD patients and volunteers was found.
-
The maximal cross-sectional area of the upper trachea lumen was larger in COPD patients compared to normal subjects. The respiratory collapse is frequently pathological and significantly larger in COPD patients compared to volunteers.
-
The respiratory change of the airway lumen in both groups and at both levels is relevant information, e.g., for modelling of individual drug inhalation. This dynamic parameter probably needs special consideration.
References
Smith PL, O’Donnell CP, Allan L, Schwartz AR (2003) A physiologic comparison of nasal and oral positive airway pressure. Chest 123:689–694
Terris DJ, Kunda LD, Gonella MC (2002) Minimally invasive tongue base surgery for obstructive sleep apnoea. J Laryngol Otol 116:716–721
Bijaoui EL, Champagne V, Baconnier PF, Kimoff RJ, Bates JH (2002) Mechanical properties of the lung and upper airways in patients with sleep-disordered breathing. Am J Respir Crit Care Med 165:1055–1061
Donnelly LF, Casper KA, Chen B, Koch BL (2002) Defining normal upper airway motion in asymptomatic children during sleep by means of cine-MR techniques. Radiology 223:176–180
Huppmann M, Schenk E, Kummer F (1990) Significance of expiratory bronchiolar collapse symptoms in the diagnosis of emphysema. Pneumologie 44:771–776
Stockley RA (2000) New approaches to the management of COPD. Chest 117(Suppl 2):58S–62S
Heussel CP, Hafner B, Lill J, Thelen M, Kauczor H-U (2001) Paired inspiratory/expiratory spiral-CT and continuous respiration cine-CT in the diagnosis of tracheal instability. Eur Radiol 11:982–989
Kauczor HU, Hast J, Heussel CP, Schlegel J, Mildenberger P, Thelen M (2002) CT attenuation of paired HRCT scans obtained at full inspiratory/expiratory position: comparison with pulmonary function tests. Eur Radiol 12:2757–2763
Heussel CP, Hafner B, Lill J, Thelen M, Kauczor H-U (2000) Diagnosis of tracheal instability: inspiratory and expiratory spiral CT and cine CT. Fortschr Roentgenstr 172:115–121
Ferretti GR, Kocier M, Calaque O, ArbibF, Righini C, Coulomb M, Pison C (2003) Follow-up after stent insertion in the tracheobronchial tree: role of helical computed tomography in comparison with fiberoptic bronchoscopy. Eur Radiol 13:1172–1178
Eastwood PR, Szollosi I, Platt PR, Hillman DR (2002) Collapsibility of the upper airway during anesthesia with isoflurane. Anesthesiology 97:786–793
Eastwood PR, Szollosi I, Platt PR, Hillman DR (2002) Comparison of upper airway collapse during general anaesthesia and sleep. Lancet 359(9313):1207–1209
Kauczor HU, Hanke A, Van Beek EJ (2002) Assessment of lung ventilation by MR imaging: current status and future perspectives. Eur Radiol 12:1962–1670
Ley S, Mayer D, Brook BS, van Beek EJR, Heussel CP, Rinck D, Hose R, Markstaller K, Kauczor H-U (2002) Radiological imaging as the basis for a simulation software of ventilation in the tracheo-bronchial tree. Eur Radiol 12:2218–2228
Janssens HM, De Jongste JC, Hop WC, Tiddens HA (2003) Extra-fine particles improve lung delivery of inhaled steroids in infants: a study in an upper airway model. Chest 123:2083–2088
Vikgren J, Johansson A, Gustavsson S, Moonen M, Bake B, Tylén U (2003) On visual determination of full inspiration on CT images. Eur Radiol 13:1235–1240
Ederle JR, Heussel CP, Hast J, Fischer B, Van Beek EJR, Ley S, Thelen M, Kauczor HU (2003) Evaluation of changes in central airway dimensions, lung area and mean lung density at paired inspiratory/expiratory high-resolution computed tomography. Eur Radiol 13:2454–2461. DOI 10.1007/s00330-003-1909-5
Stern EJ, Graham CM, Webb WR, Gamsu G (1993) Normal trachea during forced expiration: dynamic CT measurements. Radiology 187:27–31
Tiddens HA, Hofhuis W, Bogaard JM, Hop WC, de Bruin H, Willems LN, de Jongste JC (1999) Compliance, hysteresis, and collapsibility of human small airways. Am J Respir Crit Care Med 160:1110–1118
Roca J, Burgos F, Sunyer J, Saez M, Chinn S, Anto JM, Rodriguez-Roisin R, Quanjer PH, Nowak D, Burney P (1998) References values for forced spirometry. Group of the European Community Respiratory Health Survey. Eur Respir J 11:1354–1362
Muro S, Nakano Y, Sakai H, Takubo Y, Oku Y, Chin K, Nishimura K, Hirai T, Kawakami K, Nakamura T, Mishima M (2000) Distorted trachea in patients with chronic obstructive pulmonary disease. Respiration 67:638–644
Hennig J (1999) K-space sampling strategies. Eur Radiol 9:1020–1031
Kane AA, Butman JA, Mullick R, Skopec M, Choyke P (2002) A new method for the study of velopharyngeal function using gated magnetic resonance imaging. Plast Reconstr Surg 109:472–481
Donnelly LF, Surdulescu V, Chini BA, Casper KA, Poe SA, Amin RS (2003) Upper airway motion depicted at cine-MR imaging performed during sleep: comparison between young patients with and those without obstructive sleep apnea. Radiology 227:239–245
American Thoracic Society (1999) Pulmonary rehabilitation. Am J Respir Crit Care Med 159:1666–1682
Perlyn CA, Schmelzer RE, Sutera SP, Kane AA, Govier D, Marsh JL (2002) Effect of distraction osteogenesis of the mandible on upper airway volume and resistance in children with micrognathia. Plast Reconstr Surg 109:1809–1818
Puente-Maestu L, Abad MJ, Godoy R, Perez-Parra JM, Cubillo JM, Whipp BJ (2002) Breath-by-breath fluctuations of pulmonary gas exchange and ventilation in COPD patients. Eur J Appl Physiol 87:535–541
Myers J, Walsh D, Sullivan M, Froelicher V (1990) Effect of sampling on variability and plateau in oxygen uptake. J Appl Physiol 68:404–410
Acknowledgement
The authors acknowledge the statistical assistance of Dr Karl-Heinz Schicketanz.
Author information
Authors and Affiliations
Corresponding author
Additional information
This manuscript includes major parts of the doctoral thesis of Anja Rist.
Rights and permissions
About this article
Cite this article
Heussel, C.P., Ley, S., Biedermann, A. et al. Respiratory lumenal change of the pharynx and trachea in normal subjects and COPD patients: assessment by cine-MRI. Eur Radiol 14, 2188–2197 (2004). https://doi.org/10.1007/s00330-004-2461-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-004-2461-7