Abstract
In recent years, the number of systems for dynamic stabilization of the lumbar spine has grown significantly. These nonfusion systems are designed to maintain or restore the intersegmental motion of the intact spine and have no adverse effects on adjacent segments [1–3]. However, today the gold standard system for the stabilization of the lumbar spine remains internal fixation, although the idea of dynamic fixation has aroused increasing interest in surgery of the lumbar spine.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Pedicle Screw
- Dynamic Stabilization
- Disc Degeneration
- Degenerative Spondylolisthesis
- Adjacent Segment Degeneration
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
In recent years, the number of systems for dynamic stabilization of the lumbar spine has grown significantly. These nonfusion systems are designed to maintain or restore the intersegmental motion of the intact spine and have no adverse effects on adjacent segments [1–3]. However, today the gold standard system for the stabilization of the lumbar spine remains internal fixation, although the idea of dynamic fixation has aroused increasing interest in surgery of the lumbar spine.
The fusion systems make use of different technical solutions, ranging from complete replacement of the disk, to keeping the core intact annulus, to maintenance of the disk but keeping under control the whole segment motion. Internal fixators are generally used as an adjunct to fusion, where, in many instances, the disc is replaced by either intervertebral cages, allograft, or autologous bone graft [4–6].
Improvements are needed in the predictability of pain relief, the reduction of treatment-related morbidities, and overall clinical success rates of pain reduction and function [7]. Recent advances in fusion techniques have elevated arthrodesis rates, without an equivalent improvement in relief of pain. Fusion is intended to alleviate pain secondary to abnormal motion or instability. Recent reports, however, have demonstrated relative success with implants that permit movement rather than eliminate it [7].
Abnormal patterns of load transmission are recognized as a principal cause of osteoarthritic changes in other joints. Spinal osteoarthritic changes may be caused by similar forces across the lumbar disc. Dynamic stabilization, or “soft stabilization,” systems seek to alter the mechanical loading of the motion segment by unloading the disc, without the loss of motion required by fusion surgery [7, 8]. Low-back symptoms often implicate abnormal loading rather than motion as the primary source of pain. Many patients complain of postural or positional pain as a prevailing symptom [9]. Radiographs of these patients often fail to demonstrate motion on dynamic studies. Furthermore, many patients with low-back pain fail to improve following a successful lumbar fusion [9]. These observations suggest that low-back pain may have etiologies related to load, and successful treatments may exist beyond fusion.
Pain at a symptomatic motion segment may originate from the vertebral endplates, the disc anulus, vertebral periosteum, facet joints, and/or surrounding supportive soft tissue structures [10]. As the lumbar spine ages, these structures undergo well-described degenerative changes, such as disc space dehydration and collapse, and corresponding facet arthropathy. The increased stiffness that accompanies these changes may further aggravate global spinal function by diminishing sagittal balance and disrupting coronal and sagittal contour [11–13].
Rationale for Dynamic Stabilization
Dynamic stabilization has several theoretical advantages over fusion. By allowing limited motion, dynamic stabilization may negate the deleterious effects of fusion on adjacent levels and on overall sagittal balance [7, 14]. Fusion has been implicated in accelerated disease of adjacent motion segments and, in the case of surgical posterior distracting procedures, major deformities such as flat back syndrome [7, 15]. Even well-performed fusions impose considerable postural stress on levels above the fusion. Fusions from L4 to S1 place considerable rotatory stress on the sacroiliac joints during sitting [7, 16]. Dynamic systems may allow the motion segment to be altered in an anatomic fashion when subjected to postural changes. Furthermore, solid posterolateral fusions do not stop loading of the disc. Although the pattern of load transmission may be altered, fusion may also prevent the spine from taking up a position where normal loading occurs [7].
Spinal fusion remains the gold standard for surgical management of instability and mechanical low-back pain. However, even in carefully selected patients, successful clinical results can be difficult to achieve. Reasons for failure include pseudarthrosis and adjacent segment disease. Although dynamic stabilization seems promising in some clinical reports, a cautious approach should be taken to any new spinal-implant system. Whereas an implant for fusion only has to provide temporary stabilization until fusion has taken place, a dynamic stabilization system has to provide stability throughout its life. Implant loosening following fusion surgery is common in the presence of pseudarthrosis. With dynamic stabilization, the implant has to stay anchored to the bone despite allowing movement. Any mismatch between the kinematics of the implant system and the motion segment and, in particular, any discrepancy between their instantaneous axis of rotation would result in the implant bearing unexpected load at certain ranges of motion. The need for strict bench testing in the laboratory, therefore, is critical. The few dynamic stabilization systems that have had clinical applications so far have produced some clinical outcomes comparable to that of fusion [17].
In the course of the degenerative process, during which the segment undergoes various anatomic alterations, there are significant changes in both the motion characteristics of, and the load distribution across, the affected (and possibly also neighboring) segments [18–20]. The loading pattern and motion are, to a certain extent, interdependent, and alterations in either (or both) may contribute to the generation of pain [18–20]. The concept of spinal fusion originally arose from the notion that a degenerated motion segment is often “unstable” or shows “movement abnormalities,” and that, accordingly, the elimination of motion in the affected segment would prevent it from undertaking the movements associated with the generation of pain. Recent thinking, however, suggests that the prevention of movement may not be the most important factor accounting for the success of fusion [18–20].
Different Strategies for Dynamic Stabilization of the Lumbar Spine
Lumbar dynamic stabilization devices provide dynamic or “soft” stabilization by providing a posterior tension band. This places the motion segment in extension while allowing limited movements in other planes. The dynamic stabilization devices that have been described from time to time and used clinically may be classified into four categories:
-
1.
Ligaments across pedicle screws
-
Graf ligament
-
Dynesys device
-
-
2.
Interspinous distraction devices
-
Minns silicone distraction device
-
Wallis system
-
X-STOP
-
-
3.
Interspinous ligament devices
-
Elastic ligament (Bronsard’s ligament across the spinous processes)
-
Loop system
-
-
4.
Semi-rigid metallic devices across the pedicle screws
-
FASS system
-
DSS system
-
Graf Ligament
The Graf ligament system was one of the first such devices used. It consists of a posterior nonelastic band that serves as a ligament between two pedicle-based screws [7, 21]. The inventor, Henri Graf, thought that abnormal rotatory motion was responsible for pain generation; therefore, the device was primarily designed to control rotatory movement by locking the lumbar facets in the extended position. Limited flexion was allowed within the range of normal movement. By providing posterior tensioning, the system probably unloads the anterior disc and may redistribute the load transmission of the painful disc. Although widely used, the clinical effects of the Graf system have not been rigorously studied. Some analyses, however, have demonstrated clinical success of the Graf ligamentoplasty similar to fusion procedures [6, 7, 22]. In two separate studies, clinical rates of excellent to good outcomes were in the 75 % range at 2-year follow-up [7, 22, 23]. It is recommended by the authors that the device be used in younger patients with adequate lumbar musculature, and in whom facet arthropathy is minimal.
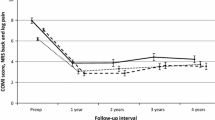
The Graf ligament stabilizes the lumbar segment through the coaptation of the bilateral facet joints, and it is the first posterior dynamic stabilization device to be widely clinically evaluated. The Graf procedure reportedly has the potential to treat flexion instability but cannot correct vertebral slippage or deformity. The most common surgical indication is degenerative lumbar disorder with less than 25 % of vertebral slip, minimal disc space narrowing, and facet arthrosis. In the mid- and long term, Graf ligamentoplasty may reduce the risk of adjacent segment degeneration. Kanayama et al. [17, 24] reported the adjacent-segment morbidity after Graf ligamentoplasty compared to posterolateral lumbar fusion at a minimum of 5-year follow-up in 45 patients.
Although there was no difference in the preoperative adjacent-segment disc condition between the two groups, radiographic evidence of adjacent-segment degeneration at final follow-up was more frequent in the posterolateral-lumbar-fusion group than the Graf group (25 and 6 % at L1–L2, 38 and 6 % at L2–L3, 38 and 18 % at L3–L4, and 43 and 18 % at L5–S1, respectively). One case in the Graf group (6 %) and five cases in the posterolateral-lumbar-fusion group (19 %) required additional surgery for adjacent-segment degeneration. The authors concluded that in well-selected patients, Graf ligamentoplasty lowers the rate of adjacent-segment degeneration [17, 24] (Figs. 10.1 and 10.2).
Dynesys System
The Dynesys system (Zimmer Spine, Warsaw, IN) includes a design that provides both controlled flexion and extension by combining a tension band with a plastic tube, which resides between pedicle screws. In flexion, motion is controlled by tension on the band, while during extension the plastic cylindrical tubes act as a partially compressible spacer, thereby allowing limited extension [7, 25, 26]. Indeed, these plastic cylinders can be partially weight bearing in extension. In order to function properly, application of the Dynesys device must follow careful technical guidelines. Inappropriately long plastic spacers, for example, may cause a focal kyphosis, a scenario that has been associated with poor outcomes [7, 27]. The Dynesys system may have some advantage over pure band-like devices in that it provides some protection against compression of the posterior anulus, a structure known to contribute to painful load bearing.
The dynamic neutralization system for the spine (Dynesys) is a nonfusion pedicle screw stabilization system, which was developed more than 10 years ago [18, 27]. In view of the arguments presented above, and the suggestion that prevention of all movement within fused segments may not only be detrimental to sagittal balance and overall function, but may also elicit accelerated degenerative changes in neighboring segments, “soft stabilization” was developed. Although the system has now been in clinical use for almost a decade, there are few studies in the literature that report on patient-oriented outcome after Dynesys implantation [18, 27].
Dynesys was developed based upon all the current knowledge of and experience with conventional rigid pedicle systems. It establishes a mobile load transfer and controls motion of the segment in all planes, while inducing stability. Thus, the bilateral implant system controls motion in all planes. Stability with controller segmental motion is established, achieving a more physiological condition as compared with the sole decompression of an unstable segment or as compared with fusion of such a segment. In connection with decompressive procedures, the system re-establishes stability and avoids iatrogenic instability. Schnake et al. [17, 28] evaluated whether elastic stabilization with the Dynesys system provides enough stability to prevent instability after decompression for spinal stenosis with degenerative spondylolisthesis. Twenty-six patients with lumbar spinal stenosis and degenerative spondylolisthesis underwent interlaminar decompression and dynamic stabilization with the Dynesys system. Minimum follow-up was 2 years. Mean leg pain decreased significantly (P < 0.01), and mean walking distance improved significantly to more than 1,000 m (P < 0.01). There were five patients (21 %) who still had some claudication. A total of 21 patients (87.5 %) were satisfied and indicated that they would undergo the same procedure again. Radiographically, no significant progression of spondylolisthesis could be detected. The implant failure rate was 17 %, and none of the implant failures was clinically symptomatic. In elderly patients with spinal stenosis with degenerative spondylolisthesis, dynamic stabilization with the Dynesys system in addition to decompression leads to similar clinical results as seen in established protocols using decompression and fusion with pedicle screws. Dynesys also maintains enough stability to prevent further progression of spondylolisthesis or instability [17, 28].
Dynamic stabilization may prevent further degeneration of the lumbar spine. Putzier et al. [17, 29] evaluated the addition of dynamic stabilization to lumbar discectomy procedures in an attempt to investigate the effect of dynamic stabilization on segmental degeneration after discectomy. Eighty-four patients with initial-stage disc degeneration (Modic 1) underwent discectomy for symptomatic disc herniation and 35 had the addition of Dynesys stabilization. At mean 34-months follow-up, a significant increase in Oswestry Disability Scores and Visual Analog Scale results was observed only in the nonstabilized group. No progression of disc degeneration was noted in the Dynesys group at follow-up, whereas radiographic signs of accelerated degeneration were noted only in the discectomy group. The authors concluded that dynamic stabilization is useful to prevent progression of initial disc degeneration in segments after lumbar discectomy [17, 29] (Figs. 10.3, 10.4, and 10.5).
X-STOP Device
Another alternative system to lumbar fusion is the X-STOP interspinous process distraction device. The X-STOP (Fig. 10.6) implant is a rigid titanium-alloy device that is placed between the spinous processes to reduce the canal and foraminal narrowing that occurs in extension. The X-STOP device is designed to distract the posterior elements of the stenotic lumbar segment and place it in flexion to treat neurogenic claudication. Anderson et al. [30] reported the results of X-STOP for the treatment of neurogenic claudication in patients with degenerative spondylolisthesis. Forty-two patients underwent X-STOP surgery and 33 patients were treated nonoperatively. Two-year follow-up data were obtained in 70 of the 75 patients. There was statistically significant improvement in the SF-36 scores of the X-STOP device-treated patients but not in those of the nonoperative controls. Overall clinical success occurred in 63 % of the X-STOP-treated patients and only 13 % of the controls. Spondylolisthesis and segmental kyphosis were unaltered. The authors concluded that the X-STOP device was more effective than nonoperative management of neurogenic claudication secondary to degenerative lumbar spondylolisthesis [30].
Spinal fusion has been accepted as the definitive surgical treatment of symptomatic lumbar degenerative disk disease and/or instability. The rationale for spinal arthrodesis as a treatment modality for low-back pain centers on the assumption that abnormal intervertebral motion causes pain and that immobilization of adjacent vertebral bodies will lead to a reduction in mechanical back pain. Unfortunately, the potential benefits and the results of arthrodesis can often be compromised by symptomatic adjacent segment degeneration and/or pseudarthrosis [31–37] (Fig. 10.7).
AccuFlex
The AccuFlex rod (Globus Medical, Inc., Audubon, PA) is designed with helical cuts within its substance to minimize rigidity. This more flexible rod is currently FDA approved as an adjunct for single-level fusions. In a 1-year prospective, randomized study of 170 patients treated with the AccuFlex rod system (Fig. 10.8), comparable fusion rates and clinical outcomes were reported between interbody fusion using the traditional rigid instrumentation versus the flexible rods [38].
Isobar TTL
One of the first introduced semi-rigid rods is the Isobar TTL system (Scient’x USA, Maitland, FL). This implant has been used in Europe for over 10 years and was granted FDA clearance for use as an adjunct to spinal fusion in 1999. Perrin and Cristini reported a retrospective study with a mean follow-up of 8.27 years using the Isobar TTL system (Fig. 10.9) in 22 patients with lumbar spondylolisthesis. The upper levels were treated with a PEEK cage followed by a two-level posterior fixation with the Isobar TTL system. All patients went on to fusion at the rigidly fixed level, with no device failure or revision surgery required. Long-term clinical outcomes were excellent, with 68.2 % of patients reporting mild leg pain, 72 % no or mild back pain, and 91 % of patients very satisfied with the procedure. The adjacent level also appeared to be protected using this type of rod [15, 31].
Truedyne PDS
The Truedyne PDS (Disc Motion Technologies, Boca Raton, FL) is a pedicle screw-based adjustable posterior dynamic stabilizer, in which 5 mm of flexion and 3 mm of extension and rotation can be set separately (Fig. 10.10). It is designed to move in an arc that elongates in flexion, ensuring normal angular segmental motion, and because of its closed design, it is also stable to shear forces. This system is designed to allow synchronous motion resulting in less strain on the disc above. The dynamic pedicle screw still allows motion between the head and shaft of the screw after being locked down. This minimizes screw loosening and also allows the screw to be used for multilevel nonfusion constructs in degenerative scoliosis. This system is currently in preclinical testing [31, 39].
Stabilimax NZ
The range at which there is minimal resistance to motion by the disc during normal spine motion is referred to as the neutral zone (NZ). The NZ is believed to increase with disc degeneration or injury, resulting in more “instability” and pain. The Stabilimax NZ (Applied Spine Technologies (AST) Inc., New Haven, CT) device (Fig. 10.11) was created to reduce the impact of the NZ on mechanical back pain. The Stabilimax NZ system uses a rod with dual concentric springs to maintain the spinal segment in a neutral position during spinal motion, serving as a sort of internal splint. The Stabilimax NZ is currently undergoing randomized clinical trials for dynamic fusion applications in the United States [31, 40].
Cosmic Posterior Dynamic System
The Cosmic posterior dynamic system (Ulrich GmbH & Co. KG, Ulm, Germany) uses hinged pedicle heads to allow for segmental motion. We have analyzed a study in the literature, carried out by Van Strempel et al., which examined patients with chronic lumbar degenerative disease treated with this system. The results were quite comparable with those obtained in patients treated with spinal fusion. Thus, this system could be an alternative to traditional therapy with arthrodesis. However, long-term follow-up studies are needed to assess its impact on adjacent level degeneration [41].
BioFlex Spring Rod Pedicle Screw System
The BioFlex System is a flexible rod system that has been used to preserve motion at the area of implantation. It is a pedicle screw-based system that uses a Nitinol rod shaped with one or two loops intended to confer stability in flexion, extension, and lateral bending (Fig. 10.12). Nitinol is an alloy of nickel and titanium that belongs to a class of materials called shape memory alloys. Ni and Ti are the chemical symbols for nickel and titanium, and the “nol” of Nitinol stands for the Naval Ordnance Laboratory, where the material was discovered. Nitinol implants have the following characteristics: high elasticity, high tensile force, flexibility (below 10 °C) but rigidity (above 30 °C), and biological compatibility [42].
CD Horizon Agile
The CD Horizon® Agile™ (Medtronic Sofamor Danek, Inc. Memphis, TN) dynamic stabilization device was intended to provide posterior dynamic stabilization through a floating cable design that allows for an axial compressive load while retaining constant stiffness. This system was designed to provide more movement than other dynamic stabilization systems. However, because of successive failures it has been withdrawn from the market. The implants were found to break due to shear-related failure of the cable component, which was more likely to occur with advanced instability.
NFlex
The NFlex controlled stabilization system (Synthes Spine Inc., West Chester, PA) consists of polyaxial titanium alloy pedicle screws that are fixed to a semi-rigid polycarbonate urethane sleeved rod (Figs. 10.13 and 10.14). The integrated polycarbonate urethane (PCU) spacer is surrounded by a central titanium ring, to which a pedicle screw is locked. The controlled pistoning of this spacer along the axis of the central titanium core provides a shock absorber effect, reducing the overall rigidity of the construct [31]. The rods are low profile, may be used in single- or multi-level applications, and require a relatively short distance between screws of only 9 mm. The rod may be attached to pedicle screws in the standard fashion, with one pedicle screw attached to the titanium ring of the sleeve and one or more pedicle screws attached to the solid portion of the titanium rod [31, 43, 44]. Biomechanical study of this device demonstrated that, in all loading modes, the NFlex device provided a decompressed lumbar segment with sufficient stability but significantly less rigidity than a similar segment stabilized with a solid rod, suggesting the applicability of this implant as a dynamic fixation device in clinical practice [43]. The system is a viable method of retaining stable motion at the implanted levels and appears comparable to other presently available methods used to preserve segmental motion.
Discussion
The hypothesis behind dynamic stabilization is that control of abnormal motions and more physiological load transmission will relieve pain and prevent adjacent segment degeneration. A remote expectation is that, once normal motion and load transmission is achieved, the damaged disc may repair itself, unless of course the degeneration is too advanced. The pertinent questions in dynamic stabilization, therefore, are (a) how much control of motion is desirable, and (b) how much load should be shared by the system, to unload the damaged disc. The question in the long term is how to prevent implant failure, in view of constant movement of the stabilized segment. A pseudarthrosis often leads to fatigue failure of implants used for rigid fixation, because the rigidity of the implant does not permit them to accommodate any motion originated at the pseudarthrosis. Flexible stabilization may accommodate this movement and may avoid a fatigue failure. However, a closer look at the kinematics of the dynamic stabilization leads to further consideration before its fatigue life may be determined. Normally, the disc is loaded both during flexion and extension. The average disc pressure rises during flexion and also during extension, and is lowest during the early phase of extension. Let us consider a dynamic stabilization system that shares 30 % of the load during flexion, allowing only 70 % of the load to pass through the damaged disc. During extension, if the system forces the instantaneous axis of rotation (IAR) to be shifted posterior to the disc, the disc will be increasingly distracted toward the end of extension. This will be evident by a progressive lowering of the disc pressure toward the end of extension, which indicates that the dynamic stabilization system becomes an increasingly load-bearing structure in extension.
Conclusion
While soft stabilization appears to be promising, a cautious approach should be taken to any new implant system. This implant for fusion only has to serve a temporary stabilization until fusion has taken place; on the other hand, a soft stabilization system has to provide stability throughout its life. After soft stabilization, the implant must stay anchored to the bone and still allow movement. The flexibility of the implant system should be able to protect it from loosening at the anchor point into the bone; the soft stabilization system is intended to load share with the disc and the facet joint only partially and unloads the motion segment. Dynamic stabilization systems have theoretical advantages over rigid spinal implants. They may allow similar or improved patient outcomes compared with fusions in patients in whom disc load characteristics represent a modifiable solution over the sagittal plane of the vertebral endplates. Some design features must be addressed, as well as placement of the devices with preservation of the surrounding spinal structures. Ultimately, a well-designed system would need to prove its clinical effectiveness in a well-designed prospective randomized clinical trial. The few posterior dynamic stabilization systems that have had clinical applications so far have produced outcomes somewhat comparable with fusion. No severe adverse events caused by these implants have been reported. Long-term follow-up data and well-controlled, prospective randomized studies do not exist, but are essential to prove the safety, efficacy, appropriateness, and economic viability of these methods.
References
Link HD. History, design and biomechanics of the LINK SB Charite artificial disc. Eur Spine J. 2002;11 Suppl 2:S98–105.
Mayer HM, Wiechert K, Korge A, et al. Minimally invasive total disc replacement: surgical technique and preliminary clinical results. Eur Spine J. 2002;11 Suppl 2:S124–30.
Ray CD. The PDN, prosthetic disc-nucleus device. Eur Spine J. 2002;11 Suppl 2:S137–42.
Stoll TM, Dubois G, Schwarzenbach O. The dynamic neutralization system for the spine: a multi-center study of a novel non-fusion system. Eur Spine J. 2002;11 Suppl 2:S170–8.
Freudiger S, Dubois G, Lorrain M. Dynamic neutralisation of the lumbar spine confirmed on a new lumbar spine simulator in vitro. Arch Orthop Trauma Surg. 1999;119:127–32.
Grevitt MP, Gardner AD, Spilsbury J, et al. The Graf stabilisation system: early results in 50 patients. Eur Spine J. 1995;4:169–75; discussion 35.
Russ P. Nockels dynamic stabilization in the surgical management of painful lumbar spinal disorders. Spine. 2005;30(16S):S68–72.
Troum OM, Crues 3rd JV. The young adult with hip pain: diagnosis and medical treatment, circa 2004. Clin Orthop. 2004;418:9–17.
Smith D, McMurray N, Disler P. Early intervention for acute back injury: can we finally develop an evidence-based approach? Clin Rehabil. 2002;16:1–11.
Gibson JN, Grant IC, Waddell G. The Cochrane review of surgery for lumbar disc prolapse and degenerative lumbar spondylosis. Spine. 1999;24:1820–32.
Bogduk N. The innervation of the lumbar spine. Spine. 1983;8:286–93.
Fujiwara A, Lim TH, An HS, et al. The effect of disc degeneration and facet joint osteoarthritis on the segmental flexibility of the lumbar spine. Spine. 2000;25:3036–44.
Fujiwara A, Tamai K, An HS, et al. The relationship between disc degeneration, facet joint osteoarthritis, and stability of the degenerative lumbar spine. J Spinal Disord. 2000;13:444–50.
Korovessis P, Papazisis Z, Koureas G, et al. Rigid, semirigid versus dynamic instrumentation for degenerative lumbar spinal stenosis: a correlative radiological and clinical analysis of short-term results. Spine. 2004;29:735–42.
Okuda S, Iwasaki M, Miyauchi A, et al. Risk factors for adjacent segment degeneration after PLIF. Spine. 2004;29:1535–40.
Lazennec JY, Ramare S, Arafati N, et al. Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J. 2000;9:47–55.
Robert W. Molinari dynamic stabilization of the lumbar spine. Curr Opin Orthop. 2007;18:215–20.
Grob D, Benini A, Junge A, Mannion AF. Clinical experience with the Dynesys semirigid fixation system for the lumbar spine surgical and patient-oriented outcome in 50 cases after an average of 2 years. Spine. 2005;30(3):324–31.
Kirkaldy-Willis WH, Farfan H. Instability of the lumbar spine. Clin Orthop. 1982;165:110–23.
Mulholland RC, Sengupta DK. Rationale, principles and experimental evaluation of the concept of soft stabilization. Eur Spine J. 2002;11 Suppl 2:198–201.
Graf H. Lumbar instability: surgical treatment without fusion. Rachis. 1992;412:123–37.
Brechbuhler D, Markwalder TM, Braun M. Surgical results after soft system stabilization of the lumbar spine in degenerative disc disease–long-term results. Acta Neurochir (Wien). 1998;140:521–5.
Markwalder TM, Wenger M. Dynamic stabilization of lumbar motion segments by use of Graf’s ligaments: results with an average follow-up of 7.4 years in 39 highly selected, consecutive patients. Acta Neurochir (Wien). 2003;145:209–14.
Kanayama M, Hashimoto T, Shigenobu K, et al. Nonfusion surgery for degenerative spondylolisthesis using artificial ligament stabilization: surgical indication and clinical results. Spine. 2005;30:588–92.
Rajaratnam SS, Shepperd JAN, Mulholland RC. Dynesis stabilization of the lumbo-sacral spine. Second combined meeting of the BSS BASS BCSS SBSR, Birmingham; 2002
Schmoelz W, Huber JF, Nydegger T, et al. Dynamic stabilization of the lumbar spine and its effects on adjacent segments: an in vitro experiment. J Spinal Disord Tech. 2003;16:418–23.
Stoll TM, Dubois G, Schwarzenbach O. The dynamic neutralization system for the spine: a multi-center study of a novel non-fusion system. Eur Spine J. 2002;11 Suppl 2:170–8.
Schnake KJ, Schaeren S, Jeanneret B. Dynamic stabilization in addition to decompression for lumbar spinal stenosis with degenerative spondylolisthesis. Spine. 2006;31:442–9.
Putzier M, Schneider SV, Funk JF, et al. The surgical treatment of the lumbar disc prolapse: nucleotomy with additional transpedicular dynamic stabilization versus nucleotomy alone. Spine. 2005;30:E109–14.
Anderson PA, Tribus CB, Kitchel SH. Treatment of neurogenic claudication by interspinous decompression: application of the X STOP device in patients with lumbar degenerative spondylolisthesis. J Neurosurg Spine. 2006;4:463–71.
Song JJ, Barrey CY, Ponnappan RK, Bessey JT, Shimer AL, Vaccaro AR. Pedicle screw-based dynamic stabilization of the lumbar spine. PAN Arab J Neurosurg. 2010;14(1):1–141.
Barr JS. Ruptured intervertebral disc and sciatic pain. J Bone Joint Surg. 1947;29:429–37.
Bono CM, Lee CK. Critical analysis of trends in fusion for degenerative disc disease over the past 20 years: influence of technique on fusion rate and clinical outcome. Spine. 2004;29(4):455–63; discussion Z5.
Coppes MH, Marani E, Thomeer RT, Groen GJ. Innervation of “painful” lumbar discs. Spine. 1997;22(20):2342–9; discussion 2349–50.
Fritzell P, Hagg O, Wessberg P, Nordwall A, Swedish Lumbar Spine Study Group. Chronic low back pain and fusion: a comparison of three surgical techniques: a prospective multicenter randomized study from the Swedish Lumbar Spine Study Group. Spine. 2002;27(11):1131–41.
Kirkaldy-Willis WH, Farfan HF. Instability of the lumbar spine. Clin Orthop Relat Res. 1982;165:110–23.
Mulholland RC, Sengupta DK. Rationale, principles and experimental evaluation of the concept of soft stabilization. Eur Spine J. 2002;11 Suppl 2:S198–205.
Mandigo CE, Sampath P, Kaiser MG. Posterior dynamic stabilization of the lumbar spine: pedicle based stabilization with the AccuFlex rod system. Neurosurg Focus. 2007;22(1):E9.
Goel VK, Kiapour A, Faizan A, Krishna M, Friesem T. Finite element study of matched paired posterior disc implant and dynamic stabilizer (360° motion preservation system). SAS J. 2007;1(1):55–61.
Yue JJ, Timm JP, Panjabi MM, Jaramillo-de la Torre J. Clinical application of the Panjabi neutral zone hypothesis: the Stabilimax NZ posterior lumbar dynamic stabilization system. Neurosurg Focus. 2007;22(1):E12.
Von Strempel A, Moosmann D, Stoss C, Martin A. Stabilisation of the degenerated lumbar spine in the nonfusion technique with cosmic posterior dynamic system. World Spine J. 2006;1(1):40–7.
Kim YS, Zhang HY, Moon BJ, Park KW, Ji KY, Lee WC, et al. Nitinol spring rod dynamic stabilization system and Nitinol memory loops in surgical treatment for lumbar disc disorders: short-term follow up. Neurosurg Focus. 2007;22:E10.
Coe JD, Kitchel SH, Meisel HJ, Wingo CH, Lee SE, Jahng T-A. NFlex dynamic stabilization system: two-year clinical outcomes of multi-center study. J Korean Neurosurg Soc. 2012;51:343–9.
Wallach CJ, Teng AL, Wang JC. NFlex. In: Yue JJ, Bertagnoli R, McAfee PC, An HS, editors. Motion preservation surgery of the spine. Philadelphia: Saunders; 2008. p. 505–10.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag London
About this chapter
Cite this chapter
Doria, C., Muresu, F., Leali, P.T. (2014). Dynamic Stabilization of the Lumbar Spine: Current Status of Minimally Invasive and Open Treatments. In: Menchetti, P. (eds) Minimally Invasive Surgery of the Lumbar Spine. Springer, London. https://doi.org/10.1007/978-1-4471-5280-4_10
Download citation
DOI: https://doi.org/10.1007/978-1-4471-5280-4_10
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-5279-8
Online ISBN: 978-1-4471-5280-4
eBook Packages: MedicineMedicine (R0)