Abstract
Purpose of the study
To evaluate the results of a novel rigid–dynamic stabilization technique in lumbar degenerative segment diseases (DSD), expressly pointing out the preservation of postoperative lumbar lordosis (LL).
Materials and methods
Forty-one patients with one level lumbar DSD and initial disc degeneration at the adjacent level were treated. Circumferential lumbar arthrodesis and posterior hybrid instrumentation were performed to preserve an initial disc degeneration above the segment that has to be fused. Clinical and spino-pelvic parameters were evaluated pre- and postoperatively.
Results
At 2-year follow-up, a significant improvement of clinical outcomes was reported. No statistically significant difference was noted between postoperative and 2-year follow-up in LL and in disc/vertebral body height ratio at the upper adjacent fusion level.
Conclusions
When properly selected, this technique leads to good results. A proper LL should be achieved after any hybrid stabilization to preserve the segment above the fusion.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lumbar degenerative disease is a common cause of back pain and neurogenic claudication in the elderly. Low back pain resulting from degenerative lumbar spine disease is a major cause of morbidity, disability and absenteeism, and it is a significant health care issue [1, 2].
The majority of these clinical problems can be treated conservatively, whereas approximately 15 % may require surgical intervention. The commonest surgical treatment for these patients is “rigid stabilization” and fusion (with or without decompression) [3, 4]. Since spinal fusion has shown acceptable outcomes, spine surgeons have trusted in rigid instrumentation. However, rigid instrumentation may cause undesirable effects such as increase of low back pain, fracture of the vertebral body and the pedicle, pedicle screw loosening and adjacent segment degeneration (ASD) [5]. There is some evidence that fusion may increase the biomechanical stresses imposed on the adjacent segments leading to overload disease [6]. On the other hand, regenerative approaches addressing vertebral disc degeneration are far to be an available option in the everyday clinical setting [7].
Limitations and problems with rigid instrumentation have led some investigators to explore the motion-preserving surgeries such as dynamic systems, to obtain posterior dynamic stabilization. This should theoretically decrease the number of ASD and reduce further progression of disc degeneration.
Clinical effectiveness of these devices, if used alone without interbody fusion, still remains controversial [8].
Moreover, Legaye reported an unfavorable influence of the dynamic neutralization system on sagittal balance of the spine, especially in terms of postoperative loss of LL, compensatory pelvic retroversion and implant mechanical stress [9].
Chen et al. compared the variation of sagittal spino-pelvic parameters after implantation of dynamic and hybrid pedicle screw-based stabilization systems. The hybrid stabilization system could better preserve the lordosis of instrumented segments, subsequently reducing the compensatory lordosis increase at the cranial adjacent segment. This could theoretically prevent the development of an ASD [10].
On the basis of this evidence; we tested a hybrid stabilization technique based on lumbar interbody fusion associated with a new dynamic system (CD HORIZON BalanC™ Spinal System, Medtronic Minnesota, USA). We believe that initial disc deterioration adjacent to a segment that has to be fused could be instrumented with a dynamic fixation. The dynamic implant is expected to reduce disc loads at that level and to preserve disc function, consequently preventing the progression of degeneration.
The aim of our study is to assess the preliminary clinical and radiological results of a novel hybrid stabilization system in lumbar degenerative diseases, and mainly to point out the role of LL preservation after the hybrid construct.
Materials and methods
The authors performed a retrospective multicentric study of 41 consecutive patients treated with a hybrid system (circumferential fusion with a posterior dynamic stabilization at the upper adjacent level) from February 2012 to July 2013.
The inclusion criteria were: (1) one lumbar level degenerative disc disease (DDD) (2) degenerative grade 1–2 spondylolisthesis (with or without stenosis) (3) a normal sagittal profile or a minimal sagittal imbalance (LL ≥ PI − 5°) (3) an initial disc degeneration at the upper adjacent level (Pfirrmann 1–3).
Exclusion criteria were: (1) idiopathic and degenerative scoliosis (2) grade 3–4 spondylolisthesis (3) failed back surgery (3) significant sagittal imbalance (LL < PI − 5°) (4) BMI over 35 and (5) absolute clinical contraindications to surgery.
We obtained informed and private consents for all participants. As this paper deals with retrospective data no approval of the Ethical Committee was necessary.
Demographic characteristics of the patients such as age, sex, BMI and baseline comorbidities were recorded.
Preoperative standing X-rays, CT and MRI study of the lumbosacral spine were obtained at the admission at our department.
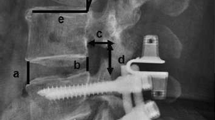
Functional status and pain severity were evaluated with Oswestry Disability Index (ODI) and Visual Analog Scale (VAS) for back and leg pain. Radiological parameters as Pelvic Incidence (PI, measured according to Duval-Beaupère [11]) and LL (evaluated using the Cobb angle) were evaluated.
The disc state at the adjacent level was assessed qualitatively on MRI study according to Pfirrmann’s classification and quantitatively with disc/vertebral body height ratio.
Continuous variables are reported as mean ± standard deviations, while categorical variables are expressed as the number of cases. All medical records and radiological images were retrospectively reviewed. The data were analyzed using the t Student test.
Study population
The population demographic distribution was: twenty-five male (61 %) and sixteen female (39 %), with a mean age of 68.9 ± 6.2 years and a mean BMI of 25.7 ± 2.7 kg/m2. Case distribution was: 28 degenerative spondylolisthesis (68 %) and 13 DSD (32 %). Baseline comorbidities included tobacco use (n = 10, 24 %) and diabetes mellitus (n = 7, 17 %).
L4–L5 with initial degeneration L3–L4 was the most commonly affected level (n = 21, 51 %), followed by L5–S1 with initial degeneration L4–L5 (n = 13, 32 %) and L3–L4 with initial degeneration L2–L3 (n = 7, 17 %).
VAS back and leg was recorded preoperatively, in the postoperative, at 6 months and at 2 years after surgery. ODI score was obtained only preoperatively, at 6 months and at 2 year after surgery. Spinopelvic parameters and disc/vertebral body height ratio were evaluated preoperatively, in the postoperative and at 2 years.
Surgical technique
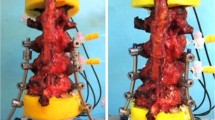
All operations were performed by two senior authors (M.F, C.F) on a prone position, using a Maquet operating table system to avoid pressure on the abdomen and the great abdominal vessels. In this position, the gravity forces the lumbar vertebrae into a lordotic position. A midline surgical approach was performed in all patients. If necessary, formal decompression with removal of affected posterior structures was performed. Intersomatic arthrodesis was performed at the unstable level with transforaminal lumbar interbody fusion (TLIF, 32 patients 78 %), posterior lumbar interbody fusion (PLIF, seven patients 17 %) or anterior lumbar interbody fusion (ALIF, two patients 5 %) using cages filled with autologous bone. Posterior stabilization was performed with CD HORIZON BalanC™ Spinal System (Medtronic Minnesota, USA) with rods pre-customized in four different shapes according to the lordosis of the patient. The rigid part of the polyetheretherketone (PEEK) rods was implanted at the fusion level while the dynamic “bumpers” at the adjacent upper level. This dynamic portion is designed to maintain motion, creating a transitional zone between the fused and mobile segments. Meticulous decortication of the posterior elements, facets, and transverse processes was performed in all patients at the fusion level.
All the patients were periodically followed up with clinical and radiographic evaluations.
A sample case of hybrid stabilization in severe DDD L5–S1 and initial (Pfirrmann 3) DDD L4–L5 is reported (Figs. 1, 2).
Results
Thirty-eight patients concluded the 2-year follow-up. Three patients dropped out the follow-up, in one case at 12 months and in two cases at 24 months. No significant intraoperative complications occurred. One superficial infection of the surgical wound occurred and it was easily solved by targeted antibiotic therapy. Five patients required blood transfusion for postoperative anemia. At 2-year follow-up, we did not observe any screw loosening or breakage on X-ray evaluation.
Preoperative mean score of back and leg pain on the visual analog scale (VAS) were 7.87 ± 1.39 and 4.77 ± 1.98, respectively. In the postoperative, the VAS mean value of back pain was 1.98 ± 1.04. Mean point of VAS leg pain was 1.87 ± 1.15. Mean improvement in back and leg pain after surgery on VAS was 5.80 ± 1.52 (p < 0.01) and 3.08 ± 1.65 (p < 0.01).
The 6-month mean VAS leg score was 0.86 ± 0.64, with a mean improvement of 0.87 ± 1.00 (p < 0.01); the mean VAS back was 1.21 ± 0.75 with an improvement 0.55 ± 0.99 (p < 0.01). The back and leg pain level at 2 years had a VAS score of 0.42 ± 0.53 and 0.37 ± 0.90. Mean improvement between 6-month and 2-year follow-up was 0.57 ± 0.67 (p < 0.01) and 0.38 ± 0.55 (p < 0.01).
The preoperative ODI averaged 62.18 % ± 13.10 and significantly improved to 23.21 % ± 6.34 at 6-month (p < 0.01), and to 18.11 % ± 4.78 at 2-year follow-up (p < 0.01).
All the patients exhibited a significant improvement in pain and functional status after surgery, which were maintained up to the 2-year follow-up (Table 1).
The mean PI was 51.67° ± 7.61 with a mean baseline LL of 49.56° ± 7.38. Mean postoperative LL was 56.57° ± 7.34. The mean post-surgical increase in global LL was 7.03° ± 4.01 compared to baseline figures. Postoperative global LL was greater than PI value in all patients. A statistically significant difference (p < 0.01) in radiological data was also noted pre- and postoperatively. At 2-year follow-up, the mean lumbar lordosis was 56.93° ± 7.21; no statistical significant difference was noted between postoperative and 2 years follow-up.
The preoperative value of disc/vertebral body height ratio was 0.278 ± 0.032, it moves to 0.282 ± 0.027 in the postoperative and to 0.269 ± 0.041 at final follow-up. No statistical significant difference was noted between preoperative and 2-year follow-up data.
Discussion
Low back pain caused by degenerative lumbar diseases is traditionally described as a mechanical pain mainly due to instability of the involved lumbar motion segment. The conventional treatment is characterized by rigid spinal fusion. Nevertheless, long-term follow-up revealed problems such as sacrifice of motion, ASD, infections, instrumentation failures and pseudarthrosis [12]. Fusion procedures focus on stop all segmental motion (both normal and abnormal) but they do not solve the degenerative problem from biomechanical point of view. Indeed, the risk of adjacent segment overload after spinal fusion is well documented. Gillet reported 41 % rate of transitional segment alterations after lumbar arthrodesis, and 20 % needed a secondary operation for extension of the fusion [13]. Sengupta et al. [14] pointed out that improvement in back pain after surgery depends mainly from the creation of a normal loading pattern than from the inhibition of motion. Schmoelz et al. [15] suggested that dynamic stabilization could be considered as an alternative method to fusion surgery while the motion segment is preserved.
These motion-preserving systems were firstly approved for dynamic instability in early stages of lumbar degeneration. Other indications were symptomatic mono- or multi-segmental DSD, degenerative spondylolisthesis, iatrogenic instability and stenosis with early stages of degenerative scoliosis [14, 16, 17].
In literature, some studies showed poor results in terms of global LL preservation with dynamic and hybrid systems. Especially, a postoperative loss of lordosis of the instrumented area is described. Moreover, an increased overload in lordosis at the upper adjacent segment with a compensatory retrolisthesis is reported. This can lead to a long-term deterioration of the upper adjacent segment. The poor result in LL preservation might be the consequence of the stabilization systems, which do not allow proper sagittal alignment preservation [9, 10].
Chen et al. outlined a minor worsening of segmental lordosis and a reduction of compensatory mechanisms at the cranial adjacent segment in the hybrid stabilization system if compared to a pure dynamic technique. Theoretically, this could prevent the development of an ASD [10].
In this intricate background, we tested a hybrid stabilization technique in single level degenerative instability with early adjacent segment degeneration. We used a new device (CD HORIZON BalanC™). To our knowledge, no previous clinical reports have been performed to evaluate outcomes of this particular hybrid stabilization system.
The construct is made mainly of PEEK with a portion of silicone in the dynamic section. PEEK is a biocompatible, radiolucent and inert semi-crystalline thermoplastic polymer; it has a modulus of elasticity between cortical and cancellous bone, significantly lower than titanium, with the potential to decrease mechanical overload complications [18].
Melnyk et al. compared four types of posterior spinal implants (three non-dynamic and CD HORIZON BalanC™) to assess the load-sharing features of this new spinal system. The authors concluded that the C-shape design of the dynamic portion decrease the axial stiffness, likely desired for the motion-preserving implants, while maintaining the load-supporting capabilities in anterior shear stress [19]. The four different degrees of lordosis of the rods arrange with the four distinctive shapes of lumbar spine according to the Roussouly classification [20]. As hypothesized by Harrison et al., 2/3 of the global lumbar lordosis is given by the L4–S1 segment and 85 % by the L3–S1 segment. According to these findings, the majority of lordosis amplitude is obtained in the distal side of the rod to mimic the anatomical lumbar spine morphology [21]. In our opinion the pre-customized lordotic rods together with the biomechanical features of the material (PEEK) and the dynamic element (bumper) allow the preservation of a correct sagittal balance and therefore the protection of the junctional segment.
Our preliminary results showed how this kind of treatment leads to good outcomes. We noticed a statistically significant and long-lasting improvement after surgery on all clinical scores.
In every patient, postoperative lumbar lordosis was higher than PI. Sagittal balance status has been demonstrated to be an independent predictor of clinical status and outcomes in subjects affected by several spine disorders [21–23]. The ideal postoperative LL is established to be predicted by the formula: LL = PI + 9° [24, 25]. We do not succeed in obtaining the ideal lumbar lordosis in every patient. Nevertheless, clinical outcomes after 2 years were satisfactory.
No statistical significant difference was noted in LL values between postoperative and 2-year follow-up. This result validates the proper sagittal alignment preservation.
Additionally, no statistically significant difference of the disc/vertebral body height ratio at the adjacent fusion level was observed between preoperative and 2-year follow-up. These data suggest the role of the device to prevent ASD above the area of arthrodesis.
Since we bring preliminary results of a novel technique, the study has some limitations that include a relative small sample size and a short-term follow-up. Moreover, our data originate from a non-controlled trial.
Nevertheless, the literature on hybrid stabilization constructs is limited, especially no previous clinical studies on CD Horizon BalanC are reported.
In our short follow-up period, no screw loosening or breakage has been recorded. Moreover, we did not notice any kyphosis nor loss of lordosis at the dynamic instrumented segment. Furthermore, we did not observed clinical or radiological signs of adjacent segment degeneration above or below the instrumented area.
We underline the importance of a precise indication to the hybrid stabilization technique. Indeed, unbalanced patients that require an important surgical correction and arthrodesis should be peremptorily excluded from any hybrid or dynamic construct to avoid early failures.
Conclusion
Considering our satisfactory results, this new hybrid stabilization device represents a feasible and alternative option to rigid fixation in several monosegmental lumbar degenerative pathologies. To our knowledge, this is the first clinical report concerning the use of CD HORIZON BalanC™. Considering the current literature, this is the only study demonstrating a tangible postoperative preservation of lumbar lordosis using a hybrid rigid-dynamic construct.
We finally remark that hybrid stabilization has specific indications. Spinal deformities or sagittal imbalance are considered as risks factors predicting surgical failure. However, additional high-quality trials specifically comparing this new hybrid technique to traditional fusion are needed to further define its effective role.
References
Goh KJ, Khalifa W, Anslow P, Cadoux-Hudson T, Donaghy M (2004) The clinical syndrome associated with lumbar spinal stenosis. Eur Neurol 52:242–249
Schwarzer AC, Aprill CN, Derby R, Fortin J, Kine G, Bogduk N (1995) The prevalence and clinical features of internal disc disruption in patients with chronic low back pain. Spine 20(17):1878–1883
Bridwell KH, Sedgewick TA, O’Brien MF, Lenke LG, Baldus C (1993) The role of fusion and instrumentation in the treatment of degenerative spondylolisthesis with spinal stenosis. J Spinal Disord 6:461–472
Nockels RP (2005) Dynamic stabilization in the surgical management of painful lumbar spinal disorders. Spine 30(16 Suppl):S68–S72
Shono Y, Kaneda K, Abumi K et al (1998) Stability of posterior spinal instrumentation and its effects on adjacent motion segments in the lumbosacral spine. Spine 23:1550–1558
Kanayama M, Hashimoto T, Shigenobu K, Togawa D, Oha F (2007) A minimum 10-year follow-up of posterior dynamic stabilization using graf artificial ligament. Spine 32:1992–1996
Formica M, Cavagnaro L, Formica C, Mastrogiacomo M, Basso M, Di Martino A (2015) What is the preclinical evidence on platelet rich plasma and intervertebral disc degeneration? Eur Spine J. doi:10.1007/s00586-015-4189-2
Korovessis P, Papazisis Z, Koureas G, Lambiris E (2004) Rigid, semirigid versus dynamic instrumentation for degenerative lumbar spinal stenosis: a correlative radiological and clinical analysis of short-term results. Spine 29(7):735–742 (Phila Pa 1976)
Legaye J (2005) Unfavorable influence of the dynamic neutralization system on sagittal balance of the spine. Rev Chir Orthop Repar Appar Mot 91(6):542–550
Chen H, Charles YP, Bogorin I, Steib JP (2011) Influence of two different dynamic stabilization systems on sagittal spinopelvic alignment. J Spinal Disord Tech 24(1):37–43
Legaye J, Duval-Beaupère G, Hecquet J, Marty C (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7(2):99–103
Beastall J, Karadimas E, Siddiqui M, Nicol M, Hughes J, Smith F et al (2007) The Dynesys lumbar spinal stabilization system: a preliminary report on positional magnetic resonance imaging findings. Spine 32:685–690
Gillet P (2003) The fate of the adjacent motion segments after lumbar fusion. J Spinal Disord Tech 16(4):338–345
Sengupta DK, Herkowitz HN (2005) Degenerative spondylolisthesis: review of current trends and controversies. Spine 30:S71–S81
Schmoelz W, Huber JF, Nydegger T, Dipl-Ing Claes L, Wilke HJ (2003) Dynamic stabilization of the lumbar spine and its effects on adjacent segments. J Spinal Disord Tech 16(4):418–423
Putzier M, Schneider SV, Funk J, Perka C (2004) Application of a dynamic pedicle screw system (DYNESYS) for lumbar segmental degenerations-comparison of clinical and radiological results for different indications. Z Orthop Ihre Grenzgeb 142(2):166–173
Di Silvestre M, Lolli F, Bakaloudis G, Parisini P (2010) Dynamic stabilization for degenerative lumbar scoliosis in elderly patients. Spine 35(2):227–234 (Phila Pa 1976); 15
Turner JL, Paller DJ, Murrell CB (2010) The mechanical effect of commercially pure titanium and polyetheretherketone rods on spinal implants at the operative and adjacent levels. Spine 35(21):E1076–E1082
Melnyk AD, Chak JD, Singh V, Kelly A, Cripton PA, Fisher CG, Dvorak MF, Oxland TR (2015) Characterization of the behavior of a novel low-stiffness posterior spinal implant under anterior shear loading on a degenerative spinal model. Eur Spine J (Epub ahead of print)
Roussouly P, Gollogly S, Berthonnaud E, Dimnet J (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine 30(3):346–353
Harrison DD, Cailliet R, Janik TJ, Troyanovich SJ, Harrison DE, Holland B (1998) Elliptical modeling of the sagittal lumbar lordosis and segmental rotation angles as a method to discriminate between normal and low back pain subjects. J Spinal Disord 11(5):430–439
Formica M, Berjano P, Cavagnaro L, Zanirato A, Piazzolla A, Formica C (2014) Extreme lateral approach to the spine in degenerative and post traumatic lumbar diseases: selection process, results and complications. Eur Spine J 23(Suppl 6):684–692
Cecchinato R, Berjano P, Bassani R, Sinigaglia A, Lamartina C (2014) How do interbody devices affect sagittal plane alignment. J Neurosurg Sci 58(2 Suppl 1):87–90
Schwab F, Lafage V, Patel A, Farcy JP (2009) Sagittal plane considerations and the pelvis in the adult patient. Spine 34:1828–1833
Lamartina C, Berjano P, Petruzzi M, Sinigaglia A, Casero G, Cecchinato R, Damilano M, Bassani R (2012) Criteria to restore the sagittal balance in deformity and degenerative spondylolisthesis. Eur Spine J 21(Suppl 1):S27–S31
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Formica, M., Cavagnaro, L., Basso, M. et al. Is it possible to preserve lumbar lordosis after hybrid stabilization? Preliminary results of a novel rigid–dynamic stabilization system in degenerative lumbar pathologies. Eur Spine J 24 (Suppl 7), 849–854 (2015). https://doi.org/10.1007/s00586-015-4264-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-4264-8