Abstract
Bipolar spectrum disorders carry a significant public health burden. Disproportionately high rates of suicide, incarceration, and comorbid medical conditions necessitate an extraordinary focus on understanding the intricacies of this disease. Elucidating granular, intracellular details seems to be a necessary preamble to advancing promising therapeutic opportunities. In this chapter, we review a wide range of intracellular mechanisms including mitochondrial energetics, calcium signaling, neuroinflammation, the microbiome, neurotransmitter metabolism, glycogen synthase kinase 3-beta (GSK3β), protein kinase C (PKC) and diacylglycerol (DAG), and neurotrophins (especially BDNF), as well as the glutamatergic, dopaminergic, purinergic, and neurohormonal systems. Owing to the relative lack of understanding and effective therapeutic options compared to the rest of the spectrum, special attention is paid in the chapter to the latest developments in bipolar depression. Likewise, from a therapeutic standpoint, special attention should be paid to the pervasive mechanistic actions of lithium as a means of amalgamating numerous, disparate cascades into a digestible cognitive topology.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Brain-derived neurotrophic factor (BDNF)
- Glycogen synthase kinase 3-beta (GSK3β)
- Lithium
- Protein kinase C (PKC) and diacylglycerol (DAG)
1 Introduction
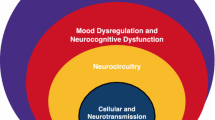
BD has a lifetime prevalence of approximately 4% in the general population and imposes substantial medical and psychosocial morbidity on patients and families (Kessler et al. 2005). Bipolar disorder (BD) has been associated with a wide range of neurobiological models whose pathophysiological mechanisms have not yet been fully characterized. As our attempts to understand and treat this disease evolve, the clearer it becomes that BD is a multifactorial disease comprised of many dynamic, interdependent systems. Findings in recent decades have encouraged a transition from research predominantly centered around monoamine neurotransmission to intracellular signaling, synaptic/neural plasticity, and other cellular mechanisms. Cumulative data also demonstrates that conventional mood stabilizers and other efficacious compounds work by modulating many of these pathways. In this present chapter, we provide updated descriptions of the prominent pathophysiologic models as well as the latest therapeutic developments in the treatment of BD.
2 Mitochondrial Dysfunction
Dysfunction in brain-energy metabolism has been considered a key mechanism in the pathophysiology of BD (Zuccoli et al. 2017). Mitochondria primarily regulate intracellular energy metabolism, and abnormalities in both mitochondrial structure and function have been associated with the development of BD. In that regard, cells from individuals with BD demonstrate distinct abnormalities in mitochondrial structure (Cataldo et al. 2010). Moreover, some reports have indicated that patients with various mitochondrial diseases demonstrate up to a 20-fold higher incidence of BD than the general population (Goodwin and Jamison 2007). Accumulated deletions in mitochondrial DNA (ΔmtDNA) of transgenic mice have been shown to result in recurrent, spontaneous depression-like episodes which are both prevented SSRI therapy and worsened by lithium withdrawal (Kato 2017). Postmortem analysis of brain tissue from BD patients also demonstrates increased rates of ΔmtDNA (Kato et al. 1997; Sequeira et al. 2012).
Mitochondria regulate energy production in the cell, and their dysfunction can result in neuronal damage via multiple pathways: oxidative damage, decreased ATP production, abnormal calcium sequestration, and apoptosis via activation of caspase proteases. During times of cellular stress and increased energy demand, ATP production through the anaerobic pathway is upregulated. This results in an increased buffering burden for neuronal lactate, forming more lactic acid and decreasing intracellular pH. This process also enhances the production of various reactive oxygen species, which can lead to further free-radical damage. Due to its relatively higher energy demand and limited buffering capacity, the brain is far more susceptible to this paradigm than other body systems. In line with this theory, there have been several magnetic resonance spectroscopy (MRS) studies in BD patients showing increased neuronal lactate and decreased pH levels.
Furthermore, patients with BD in a current major depressive episode have shown a significant decrease in cingulate cortex lactate after being treated with a 6-week course of lithium monotherapy (Machado-Vieira et al. 2017b; Clay et al. 2011; Dager et al. 2004). Another indication of mitochondrial dysfunction is the decreased levels of N-acetyl-aspartate (NAA) seen in BD patients compared to normal controls (Kubo et al. 2017). NAA is produced in the mitochondria and is one of the most abundant brain metabolites, also serving as an important marker of neuronal viability (Rosso et al. 2017). In a clinical trial assessing NAA levels using MRS, BD patients were shown to have significantly lower NAA levels than controls. Furthermore, they had significant NAA increases after treatment with a 12-week course of lamotrigine (Croarkin et al. 2015). In addition to mitochondrial dysfunction, elevations of peripheral markers of oxidative stress have been described in BD patients, which correlate with a longer duration and earlier onset of illness (Machado-Vieira et al. 2007; Brown et al. 2014). De Sousa et al. have further demonstrated that a reactive increase in antioxidant enzymes occurs early in the developmental course of BD, especially during depressive phases. Additionally, BD patients have been shown to exhibit a decrease in lipid peroxidation following lithium treatment (de Sousa et al. 2014). Thus, oxidative damage appears to play a significant inciting role in the development of BD, subsequently interfering with endogenous repair mechanisms if left untreated.
Within the mitochondria itself, the electron transport chain (ETC) serves as a major mediator of oxidation/reduction and overall mitochondrial function. Postmortem analysis of cerebral tissue in patients with bipolar disorder demonstrates a decrease in ETC complex I concentration (Andreazza et al. 2010). Furthermore, lithium has been shown to increase mitochondrial complex I activity in BD patients significantly, and post-treatment complex I activity positively correlates with plasma lithium levels (de Sousa et al. 2015a, b). This strongly suggests that beyond its acute therapeutic mechanisms (discussed elsewhere), lithium provides a long-term, neuroprotective benefit to patients by reducing overall oxidative damage to neurons.
Converging lines of this hypothesis have proffered several substances as mitochondrial activity modulators: omega-3 fatty acids, coenzyme Q10, acetyl-L-carnitine, N-acetylcysteine (NAC), S-adenosylmethionine (SAM), alpha-lipoic acid, creatine monohydrate, melatonin, L-tryptophan, magnesium, folic acid, and branched-chain amino acids (BCAAs) (Nierenberg et al. 2013; Sarris et al. 2011). Overall, NAC has demonstrated the largest effect size in treating bipolar depression. Mixed, but mostly positive, evidence also supports the use of omega-3 fatty acids. Significant reductions in mania have also been demonstrated with the use of L-tryptophan, magnesium, folic acid, and BCAAs (Sarris et al. 2011). While some of these compounds may demonstrate efficacy as monotherapies, ultimately, this class may prove most effective as augmentation therapy for conventional BD treatments (Sarris et al. 2009; Mischoulon 2009). Larger, more-robust clinical trials are needed before their use becomes commonplace.
3 Calcium Channel Modulators
Ca2+ signaling is a tightly regulated process that plays an important role in a variety of cellular processes, including neuronal excitability, neurotransmitter synthesis/release, synaptogenesis, and plasticity. Even small perturbations in the balance between intracellular and extracellular calcium can trigger cell-death programs which are unresponsive to molecular rescue. Two cellular organelles, mitochondria and endoplasmic reticula (ER), are critical in maintaining a delicate balance of intracellular Ca2+ concentrations through sequestration, buffering, and mobilization. As previously discussed, increasing evidence suggests that mitochondrial function plays a key role in governing the synaptic properties of neuronal circuits that govern complex human behaviors. Mitochondrial dysfunction has also been implicated in a wide array of neurological and psychiatric disorders (Kato 2017).
In 1922, Weston and Howard observed that individuals with mania had lower spinal fluid concentrations of Ca2+ compared to depressed individuals (Weston 1922). This realization was subsequently obscured by decades of controversial findings regarding Ca2+ homeostasis in BD. However, more recent studies have revived this hypothesis by demonstrating that, compared to healthy controls, BD patients have elevated Ca2+ levels in platelets and lymphocytes, in addition to increased Ca2+ ATPase activity in red blood cells (Dubovsky et al. 1992; Warsh et al. 2004). As mitochondrial structure plays a significant role in Ca2+ homeostasis, these findings are in accordance with an ion-imbalance hypothesis in BD (Clay et al. 2011).
Various lines of pharmacologic evidence also support the relationship between calcium signaling and mood disorders. In animal and human models, lithium has been shown to significantly reduce NMDA receptor-stimulated Ca2+ responses (Nonaka et al. 1998). Moreover, both lithium and valproate are potent enhancers of Bcl-2 expression (Chen and Chuang 1999). The Bcl-2 family of proteins promote neuronal survival in part by inhibiting Ca2+ release from the ER (Rong and Distelhorst 2008). SNPs of the Bcl-2 gene, which are associated with developing BD, are also associated with elevated basal calcium levels and increased cytosolic Ca2+ release (Machado-Vieira et al. 2011). This alteration in membrane excitability may disrupt several neural components responsible for controlling mood and behavior.
Additionally, through separate pathways, lithium and valproate both cause depletion of inositol, a key calcium signaling intermediary. Lithium inhibits inositol monophosphatase (IMPase) involved in phosphatidylinositol 4,5-biphosphate (PIP2) turnover, which in turn reduces calcium entry into the cell and thus overall neuronal excitability. This may partially explain the efficacy of lithium in correcting neurotransmission, which has been shown to be altered in BD (Berridge 2014). Furthermore, inositol depletion has been shown to increase synapse formation between hippocampal neurons in vitro (Kim and Thayer 2009). Thus, modulation of calcium signaling appears to have multiple benefits, acutely stabilizing neurotransmission as well as the long-term potentiation of synaptogenesis.
As follows, researchers have investigated various calcium channel antagonists (CCAs) as possible therapeutic targets for BD. Studies indicate that only slow-gated L-type channels (LTCCs) are sensitive to CCAs in neurons. In that regard, three antihypertensive medications with LTCC activity, verapamil, nimodipine, and diltiazem were initially tested, with mixed results. Verapamil was first to be compared to lithium and placebo to treat mania. Both compounds had similar anti-manic effects, which were superior to placebo (Giannini et al. 1984). Despite this initial promise, recent reviews have shown inconsistent findings. Janicak et al. (1998) found no benefit over placebo in treating mania (Janicak et al. 1998). Keck et al. (2000) found both positive and negative results, suggesting the need for further investigation (Keck et al. 2000). Giannini et al. (2000) found that verapamil combined with magnesium oxide was superior to verapamil monotherapy (Giannini et al. 2000). More recently, verapamil was compared to lithium in a double-blind continuation study for acute mania. Individuals unresponsive to lithium (phase 1) were randomized to either continue lithium or switch to verapamil (phase 2). Non-responders in phase 2 were further allocated to verapamil-lithium combination treatment (phase 3). Authors found some efficacy for verapamil as monotherapy, but no significant difference compared to lithium and no superiority in combination (Mallinger et al. 2008).
In 1998, Pazzaglia et al. conducted a double-blind placebo-controlled study investigating the efficacy of nimodipine in 30 patients with refractory affective disorders (23 with bipolar and 7 with unipolar depression). One-third of the patients showed a significant response to nimodipine monotherapy. Non-responders (n = 14) added carbamazepine, with roughly another third achieving remission. Authors further noted that individuals with rapid-cycling BD were more apt to respond to the carbamazepine-nimodipine combination therapy (Pazzaglia et al. 1998). Subsequent studies were conducted around this time, most with modest results, and some evidence suggesting that low baseline CSF somatostatin may predict response to nimodipine (Frye et al. 2003).
Lastly, investigators have attempted to demonstrate the efficacy of diltiazem as add-on therapy in BD. In 2000, researchers conducted an open-label study with eight women in either a manic or depressive episode, generating promising findings. In comparing the 6 months before and after starting the add-on therapy, they observed a significant improvement in manic/depressive symptoms (Silverstone and Birkett 2000). However, several studies have reported that verapamil and diltiazem may enhance lithium excretion, increase carbamazepine levels, and create a synergistic, neurotoxic effect with either mood stabilizer (Brodie and MacPhee 1986; Bahls et al. 1991; Price and James Giannini 1986).
Despite a lack of definitive clinical outcomes and potential adverse side effects, recent preclinical research has reinforced the importance of aberrant calcium signaling in BD (Harrison 2016; Heyes et al. 2015). Specifically, genomic data shows that several LTCC-subunit-encoding genes, especially the CACNA1C locus, are associated with BD, schizophrenia, and MDD (Craddock and Sklar 2013). Additionally, neuron-like cells derived from BD patients show increased CACNA1C gene expression and enhanced calcium signaling (Yoshimizu et al. 2015). Mertens et al. further found that induced stem-cell-derived (iPSC) hippocampal neurons from patients with BD display a characteristic, hyperexcitable phenotype in relation to calcium signaling. Importantly, this phenotype was selectively reversed by lithium in vitro, only in neurons derived from patients that responded to lithium clinically (Mertens et al. 2015).
In summary, despite contradictory findings in the early twentieth century, more recent preclinical evidence has strongly implicated alterations in mitochondrial function and calcium signaling in the pathogenesis of BD. Elevated endogenous calcium concentrations in bipolar patients and reductions calcium hyperexcitability caused by lithium clearly demonstrate promise for this line of investigation. Building on this hypothesis, conventional CCAs (verapamil, diltiazem, nimodipine) demonstrated some initial promise. However, subsequent, more-rigorously designed studies failed to replicate these findings, in addition to revealing several adverse side effects. Despite this obstacle, the large quantity of in vitro evidence underscores a need for further proof-of-concept trials, potentially involving other CCAs. Given the wide distribution of LTCCs throughout the body, future clinical interventions should focus on developing more-targeted and genome-directed compounds with greater blood-brain barrier penetration and higher specificity for CNS-LTCC ligands. Most importantly, genomic evidence strongly suggests that future patients should be selectively enrolled in trails based on genetic and phenotypic amenability to such therapies.
4 Intracellular Signaling and Inflammation
Numerous studies support the role of the immune dysfunction in the development of BD (Rosenblat and McIntyre 2015; Munkholm et al. 2013; Goldstein et al. 2009; Leboyer et al. 2012). Bipolar disorder has been implicated in increased rates (1.5–3 times) of premature death due to medical comorbidities, higher prevalence of metabolic syndrome, and greater cardiovascular mortality than that in the adult general population (Leboyer et al. 2012). Furthermore, there is evidence that patients with BD have a reduced life expectancy (9–14 years) and exhibit shortened telomeres compared to the general population (Rizzo et al. 2013; Chang et al. 2015). BD has also been associated with numerous other immunological conditions: systemic lupus erythematosus, autoimmune thyroiditis, psoriasis, rheumatoid arthritis, multiple sclerosis, inflammatory bowel disease, and others (Rosenblat and McIntyre 2015). Though causality in this regard has yet to be established, recent research indicates that the relationship is likely bidirectional (Perugi et al. 2014).
These associations are reinforced by several cross-sectional studies which have demonstrated that, compared to healthy controls, patients with BD have significant elevations in proinflammatory cytokines such as TNF-α, IL-1β, IL-4, IL-6, and others. These studies have even suggested a state-dependent association with various inflammatory markers. For example, during manic episodes, BD patients demonstrate increased expression of TNF-α, IL-4, IL-6, CXCL10, and other inflammatory molecules (Barbosa et al. 2014; Modabbernia et al. 2013). Many of these markers have not yet been robustly investigated in bipolar depression; however evidence from MDD patients suggests that similar cytokine alterations also occur during depressive episodes (Rosenblat et al. 2014; Felger and Lotrich 2013). A recent meta-analysis of 32 inflammation studies found TNF-α to be the only biomarker elevated in both mania and bipolar depression (Rowland et al. 2018). Though further longitudinal research is necessary to fully validate a causal link in this regard, mounting evidence suggests that BD patients experience a chronic, low-grade inflammatory state which may be enhanced during acute mood episodes (Rosenblat et al. 2014; Fillman et al. 2014).
It is important to note that the majority of the aforementioned studies measure peripheral cytokine levels. While the direct observation of CNS inflammation may be more desirable, doing so is typically a highly invasive and cost-prohibitive endeavor. As with most neuroinflammatory conditions, altered blood-brain barrier (BBB) permeability allows for the bidirectional passage of peripheral and central immune mediators. Additionally, recent paradigm-shifting animal research has demonstrated a contiguous link between systemic lymphatic drainage and dural sinus vasculature, further allowing for the amalgamation of CNS and systemic immune constituents (Louveau et al. 2015). As follows, numerous BD studies have demonstrated a correlation between peripheral and central cytokine expression (Munkholm et al. 2013; Barbosa et al. 2014).
Several mechanisms have been proposed as to the specific, deleterious effects of inflammation in mood disorders. Under normal conditions, CNS macrophages (microglia) play several vital roles: immune surveillance, scavenging unwanted cellular products, and pruning of underutilized synaptic pathways. However, in states of elevated inflammation, microglia disproportionately adopt a proinflammatory phenotype leading to unwanted pruning, increased BBB permeability, and resultant influx of peripheral immune cells (Stertz et al. 2013). Evidence for this mechanism is supported by both PET imaging and postmortem tissue analysis, demonstrating increased microglial activity in the hippocampus and prefrontal cortex of BD patients (Haarman et al. 2014a, b; Rao et al. 2010). Proinflammatory cytokines have also been shown to alter the concentration of monoamines, for example, by decreasing the conversion of tryptophan to serotonin, accelerating serotonin breakdown, and increasing levels of depressogenic tryptophan metabolites (Capuron et al. 2003; Zhang et al. 2001). This process has been shown to be mediated in part by HPA axis over-activation and resultant hypercortisolemia (Maes et al. 2011). A detailed explanation of the HPA axis and cortisol overproduction in BD is discussed elsewhere in this chapter. In short, cortisol upregulates hepatic tryptophan 2,3-dioxygenase activity, causing unwanted monoamine catabolism. Additionally, proinflammatory cytokines interfere with hypothalamic glucocorticoid receptor function, disrupting normal feedback inhibition on cortisol production (Pace and Miller 2009).
With regard to systemic inflammation, significant attention has recently been directed towards elucidating a connection between the enteric nervous system (ENS) and the CNS, otherwise known as the “gut-brain axis.” Numerous in vitro and animal studies have suggested that the mucosal microbiome may exert substantial influence on behavior and cognition via alterations in immune function and neurotransmitter metabolism. Though microbiome research in psychiatry is in its relative infancy, there has been a long-standing association between various gastrointestinal pathologies and psychiatric disorders (Severance et al. 2015; Lee et al. 2015). Recent research suggests that an imbalance in gut microflora (dysbiosis) may cause luminal inflammation which facilitates microbial translocation into systemic circulation (Dickerson et al. 2017).
Recently, researchers have developed antibodies to diagnose Crohn’s disease, which detect the presence of normal gut microbes in systemic circulation (Desplat-Jego et al. 2007). Elevated antibody production against one such yeast (Saccharomyces cerevisiae) has been detected in patients with both schizophrenia and BD. Importantly, titers were significantly higher in individuals experiencing recent-onset of their disorder and those who were antipsychotic-naïve, suggesting an inciting mechanism that cannot be solely attributed to medication usage (Severance et al. 2012, 2014). Dickerson et al. have conducted several longitudinal observation studies which demonstrated that, compared to healthy controls, BD patients in acute manic episodes have increased production of antibodies directed against gliadin (a marker of gluten sensitivity), NR2 (an NMDA receptor peptide), Mason-Pfizer monkey virus 24, and Toxoplasma gondii. These findings appeared to be state-dependent, as titers did not differ from controls at 6-month follow-up.
Furthermore, elevated inflammation scores during initial manic episodes were predictive of psychiatric re-hospitalization during the follow-up period (Dickerson et al. 2012a, b, 2013). Though initial findings are intriguing, more research is needed to delineate specific microbial-inflammatory mechanisms. We must also assess the influence of confounding variables such as environment, medication usage, and smoking. Furthermore, there is a relative paucity of evidence regarding the interplay between gut dysbiosis and neurotransmitter-mediated, retrograde communication between the ENS and CNS. In that regard, more information is needed to bolster therapeutic efforts, as initial studies with general probiotics have yet to yield impactful results (Dickerson et al. 2017).
Current knowledge gaps notwithstanding, specifically targeting immune dysfunction in BD, is highly desirable, especially given that doing so can potentially ameliorate numerous associated comorbidities. Emerging evidence suggests that some antipsychotics and lithium downregulate the expression of inflammatory genes in the cells of BD patients (Haarman et al. 2014a, b). However, the exact mechanism by which these agents exert their anti-inflammatory effects is unknown. As previously mentioned, the anti-inflammatory/antioxidant compound N-acetylcysteine (NAC) has shown significant promise as an adjunct treatment in BD. Multiple DBRPCTs have demonstrated significant reductions in depressive symptoms compared to placebo in bipolar patients (Berk et al. 2008, 2012). A small number of trials have also investigated the efficacy of the anti-inflammatory agents like celecoxib (Arabzadeh et al. 2015) and aspirin (Berk et al. 2013) as adjunctive treatment in BD, with mixed results. Specifically, Arabzadeh et al. found celecoxib 400 mg to be superior to placebo as adjunctive therapy to sodium valproate in treating bipolar mania without psychotic features.
Pioglitazone is a peroxisome proliferator-activated receptor-gamma agonist with well-established, potent anti-inflammatory and anti-hyperglycemic properties. In a 2015 double-blind RCT of BD patients in a current major depressive episode (MDE), Zeinoddini et al. found that pioglitazone caused significant reductions in depressive symptoms after 6 weeks (Zeinoddini et al. 2015). Further research has shown it to be particularly effective in reducing depressive symptoms when used as an adjunct therapy in BD patients with comorbid metabolic dysfunction (Kemp et al. 2014). Importantly, in this study, elevated baseline levels of the proinflammatory cytokine IL-6 correlated with greater reductions in depression severity. Likewise, a recent 12-week, randomized, double-blind, placebo-controlled, parallel-group trial of 60 participants investigated the use of adjunctive infliximab in the treatment of adults with bipolar I/II depression. Despite being a negative trial overall infliximab significantly reduced depressive symptoms compared to placebo in patients with baseline elevations in serum CRP and TNF-α.
Preclinical evidence supports an intricate association between immune function, the microbiome, BD, and many of its comorbid conditions. Immune cells and inflammatory signaling molecules have been shown to produce local damage, prevent repair, and affect downstream neurotransmitter metabolism through a myriad of interconnected pathways. Beyond demonstrating therapeutic potential, several trials of anti-inflammatory compounds have importantly shown enhanced efficacy in patients with elevated levels of pre-treatment inflammation. This underscores the significant need for further investigation in this area, both in developing targeted therapies and screening/selecting patients based on their inflammatory profile. Numerous immune modulators have been approved for various systemic conditions over the last two decades, only a handful of which have been evaluated in the treatment of psychiatric disorders. Thus, given the ability to bypass significant startup costs and regulatory obstacles inherent to developing novel agents, it would seem prudent going forward to dedicate more resources towards clinical trials which investigate the efficacy of approved but untested medications in this class.
5 Glycogen Synthase Kinase 3-Beta (GSK3β)
Several lines of investigation have implicated the enzyme GSK3β in the parthenogenesis of BD. In 1996, GSK3β was discovered to be a target of lithium, specifically mediated by a magnesium-competitive inhibition mechanism (Klein and Melton 1996). Since that time, researchers have uncovered nearly 50 substrates of GSK3β that are key modulators in several processes related to neuronal function. The most prominent group of these compounds are known as Wnt molecules. Throughout early development and adult life, Wnt ligands mediate cell patterning, differentiation, proliferation, neuronal morphology, and cellular-integration into established neuronal circuits. The Wnt pathway facilitates these processes by first inhibiting the constituently active GSK3β enzyme, leading to the nuclear translocation of β-catenin and subsequent activation of several enhancers/transcription factors involved in neurotrophic generation (BDNF), circadian regulation, and inflammatory modulation (Valvezan and Klein 2012). Indeed, GSK3β overactivity has been linked to dysfunction in all of these domains, causing decreased BDNF production (Machado-Vieira et al. 2009), prevention of medication-mediated mood-stabilization and neurogenesis (Hussaini et al. 2014), increased expression of pro-inflammatory cytokines such as IL-6 and TNF-α (Ajmone-Cat et al. 2016), and lengthening of the circadian rhythm (McCarthy et al. 2013).
Various lines of animal and human evidence further support the role of aberrant Wnt/GSK3β activity in BD. Transgenic mice that over-express GSK3β develop hyperactive symptoms akin to human mania, whereas haplo-insufficient mice (GSK3+/−) with decreased GSK3β activity exhibit features that replicate chronic lithium treatment. Moreover, induced GSK3β overexpression in mice nullifies the effect of chronic lithium treatment. Importantly, lithium is a well-validated GSK3β inhibitor (Cole 2013).
Patients with BD exhibit decreased levels of β-catenin mRNA and protein in the dorsolateral-prefrontal and temporal regions compared to those with schizophrenia and healthy controls (Pandey et al. 2015). Moreover, several SNPs within the promoter region for GSK3β are associated with an earlier age of onset and sensitivity to lithium therapy (Cole 2013).
Researchers have also demonstrated decreased GSK3β inhibition in the peripheral blood mononuclear cells (PBMCs) of bipolar individuals. Notably, in this small cohort study, a lower magnitude of GSK3β inhibition significantly correlated with the severity of manic/depressive episodes (Polter et al. 2010). More recent evidence has bolstered these findings by demonstrating that treatment with lithium causes an increase in PBMC-GSK3β inhibition, which also correlates with symptomatic improvement (de Sousa et al. 2015a, b).
Apart from lithium, other psychoactive compounds with efficacy in BD also demonstrate GSK3β pathway activity. Conflicting evidence exists regarding the GSK3 activity of anticonvulsant mood stabilizers such as valproic acid and carbamazepine (Muneer 2017). However, second-generation antipsychotics (SGAs), which are becoming increasingly important in the treatment of all phases of BD, have well-documented GSK3β inhibitory properties (Kalinichev and Dawson 2011; Pandey et al. 2015). Biased agonists such as aripiprazole have also been shown to increase the transcription of Wnt-related genes in the β-catenin pathway (de Bartolomeis et al. 2015). Lastly, conventional antidepressants have been shown to interact with several Wnt/GSK3 cellular cascades. GSK3β-mediated alterations in neuronal plasticity occur at the level of genetic transcription and are thus expected to take weeks before subjective improvement in symptoms occurs. This timeline thus concurs with the natural treatment course of SSRI therapies (Pilar-Cúellar et al. 2014).
Given the pervasive involvement of this pathway in a wide range of psychiatric disorders and medication classes, GSK3β inhibition stands as an attractive, albeit illusive therapeutic target. Over the past two decades, AstraZeneca has been at the forefront of GSK3β inhibitor development, with six novel candidates, only one of which progressed to phase II trials. Due to concerns over toxicity, safety margins, as well as various other issues, progress in this area has been slow (Bhat et al. 2018). Building on these efforts, Bhat et al. note that future GSK3 drug development should focus on increasing kinase selectivity as well as using novel conjugated-peptide technology to enhance tissue specificity.
6 Protein Kinase C (PKC) and Diacylglycerol (DAG)
Protein kinase C (PKC) is a family of calcium and phospholipid-dependent enzymes implicated in mood regulation. More specifically, PKC in the brain is present in high levels at presynaptic terminals and thought to play a role in the regulation of neuronal excitability, neurotransmitter release, and neuroplasticity (Zarate and Manji 2009). Conventional PKC (cPKC) isoforms (α, βI, βII, γ) require calcium and diacylglycerol (DAG) for activation, while novel PKC isoforms (δ, ε, η, θ, μ) only require DAG for activation (Zarate and Manji 2009). In CNS, cPKC isoforms are the most common and are highly expressed in several structures classically associated with mood regulation (prefrontal cortex, amygdala, and hippocampus) (Naik et al. 2000). This family of enzymes modulate neuronal transmission at several levels: short term (neurotransmitter/ion flux), intermediate (receptor regulation), and long term (synaptic remodeling, cell proliferation, genetic expression) (Amadio et al. 2006). PKC signaling underlies many of the pathologic mechanisms discussed throughout this chapter: neuronal excitability (Pahl et al. 2014), neurotransmitter release (Zarate et al. 2006), glutamate signaling (Zarate et al. 2003), neuroinflammation (Jun et al. 2014), neuroplasticity (Chu et al. 2014), and mitochondrial dysfunction, especially as it pertains oxidative stress and apoptosis (Nam et al. 2015).
Multiple lines of animal and human evidence support the pervasive involvement of this family of enzymes in BD. PKC inhibition reduces manic-like behaviors and hippocampal cell degeneration in rat sleep deprivation mania models (Abrial et al. 2013). Compared to healthy controls, BD patients demonstrate increased levels of both central (cortical) and peripheral (platelet) PKC activity (Wang and Friedman 1996; Wang et al. 1999). Lastly, a meta-analysis of 8,700 patients with both unipolar and bipolar depression found that suicidality was significantly associated with the genetic locus for PKCε (Saxena et al. 2017).
In that regard, chronic lithium treatment has been shown to decrease PKC levels in platelets of BD patients (Soares et al. 2000). Both lithium and valproic acid inhibit PKC activity in vitro and in vivo (Zarate and Manji 2009; Chen et al. 1994, 2000). Chronic administration of quercetin, a non-specific PKC inhibitor, prevents methylphenidate-induced hyperlocomotion and lipid peroxidation in mice (Kanazawa et al. 2017). Tamoxifen, another potent PKC inhibitor, has demonstrated efficacy in acute manic or mixed episodes of BD as both adjunct and monotherapy (Talaei et al. 2016; Yildiz et al. 2016, 2008; Amrollahi et al. 2011).
7 Neurotrophins
Neurotrophins are cellular growth factors involved in synaptic plasticity, neurogenesis, cell survival, and long-term memory formation (Grande et al. 2010). Within the neurotrophin family, brain-derived neurotrophic factor (BDNF) is the most extensively studied in BD (Fernandes et al. 2011; Rowland et al. 2018). Data from six meta-analyses have consistently demonstrated that BD patients have significantly lower levels of plasma BDNF compared to healthy controls, as do individuals with schizophrenia and unipolar depression (Rowland et al. 2018; Fernandes et al. 2015; Molendijk et al. 2014). Furthermore, BD patients in current manic or depressive episodes both demonstrate reductions in peripheral BDNF levels, unlike their euthymic counterparts (Fernandes et al. 2015; Rowland et al. 2018). The effect size is particularly large in bipolar depression (SMD − 0.86) and moderate in mania (SMD – 0.54) (Rowland et al. 2018).
BDNF plays a significant role in both GSK3β/Wnt and PKC activity (discussed in more detail in their respective sections). Briefly, BDNF transcription can be increased by various GSK3β inhibitors (including lithium) and through GSK3 gene silencing. Moreover, BDNF itself can inhibit GSK3β activity (Machado-Vieira et al. 2009). BDNF also mediates some of the genetic expression associated with synaptic plasticity via PKC signaling (Arevalo and Wu 2006). Beyond acting as a second messenger, PKC itself can also influence the expression of BDNF and other neurotrophins (Xu et al. 2013, 2015). The reciprocity and interdependence involved in both of these pathways underscores the pervasive and complex role that neurotrophins play in modulating a wide array of neuronal signaling mechanisms.
Some studies have suggested an association between polymorphisms in BDNF promoter genes and vulnerability for developing BD (D’Addario et al. 2012). Using a systems model of the human prefrontal transcriptional network, researchers have highlighted the importance of the early growth response gene 3 (EGR3) gene, which was previously shown to be modulated by BDNF (Pfaffenseller et al. 2016). A current proposal suggests a positive feedback loop wherein BDNF signaling dysfunction leads to reduced EGR3 expression, thus impairing neuroplasticity and resilience, increasing the vulnerability to stress, and further lowering BDNF expression (Pfaffenseller et al. 2018). Moreover, using a multisystem analysis of BDNF genes and other loci, researchers were able to identify bipolar patients with a sensitivity of 73% and a specificity of 71% (Munkholm et al. 2019). Building on this success, recent findings indicate that measuring BDNF in conjunction with TNF-α may provide even greater fidelity in distinguishing manic/depressed individuals from euthymic patients (Rowland et al. 2018). All of these studies suggest that BD pathogenesis is highly connected to many BDNF-related pathways. As with the “triple test” in Down syndrome and diagnostic tests for thyroid-related illnesses, BDNF measurements may be of greatest use when combined with other known biomarkers in BD. Given its pervasive influence on neuronal activity, BDNF may also have great potential as future therapeutic target.
Currently, no pharmacological agent used in BD directly targets the neurotrophins; however, antidepressants, lithium, electroconvulsive therapy (ECT), and glutamatergic agents like ketamine and memantine all increase peripheral levels of BDNF in patients with major depressive disorder (MDD) (Molendijk et al. 2014; Duncan and Zarate 2013; Haile et al. 2014; Lu et al. 2012). The pervasive, reciprocal interactions of neurotrophins with many other pathways present significant confounding obstacles for investigators. For now, BDNF may be of greatest utility as biomarker for disease severity and treatment response.
8 Glutamatergic System
Alterations in the glutamatergic system have been extensively implicated in the pathophysiology of BD. Likewise, the glutamate-modulating capability of conventional BD treatments such as lithium, valproate, lamotrigine, and antidepressants is well-documented (Machado-Vieira et al. 2012). Glutamate is the most abundant excitatory neurotransmitter in the brain. It acts in three different cellular compartments – pre/postsynaptic neurons and glia – characterized as the “tripartite glutamatergic synapse.”
Particularly through its action at ionotropic AMPA and NMDA receptors, glutamatergic signaling plays a crucial role in excitatory neurotransmission, synaptic function, neuroplasticity, and neurogenesis. Indeed, AMPA (GluA1 subunit) knockout mice provide a successful model for depression, and NMDA receptor antagonists have repeatedly demonstrated antidepressant efficacy (Papp and Moryl 1994; Chourbaji et al. 2008). Interestingly, Du et al. (2010) showed that the GSK3 inhibitor AR-A014418 regulates AMPA-induced GluR1 and GluR2 internalization via phosphorylation of kinesin light chain 2 (KLC2), the key molecule of the kinesin cargo delivery system (Du et al. 2010). As previously discussed, neurotrophins modulate the activity of GSK3 (Bartzokis 2012). Thus, glutamate seemingly acts as a molecular intermediary between many of the signaling pathways discussed throughout this chapter.
Candidate gene and genome-wide association studies (GWAS) have also implicated glutamate signaling in BD pathophysiology, albeit with some conflicting results. In a recent systematic review, de Sousa et al. found a positive association between BD and glutamate-related genes in 12 of 34 (35%) studies (Nurnberger et al. 2014; de Sousa et al. 2017). Overall, these genetic findings warrant deeper investigation, especially for the glutamatergic genes which have repeatedly demonstrated associations with BD (GRIA3, GRIK2, GRIK4, and GRM7). Moreover, researchers have demonstrated alterations in mRNA expression as well as induction of depressive-like behaviors in genetically altered animal models, further implicating these candidate genes in the disease process (Beneyto et al. 2007; Catches et al. 2012; Cryan et al. 2003; Duric et al. 2013).
Separate genetic analysis has also uncovered a significant association between BD and the glia-astrocyte pathway (Duncan et al. 2014). In addition to being the primary mediators of neuroinflammation, glial cells are integral to the glutamate recycling process. In that regard, investigation into glutamate/glial modulators has substantially increased in recent years. Ketamine, a N-methyl-D-aspartate (NMDA) receptor antagonist, has been placed in the spotlight due to its rapid antidepressant action in both unipolar and bipolar depression (Sanacora et al. 2017). While previous data did not demonstrate effective remission rates in bipolar depression (McCloud et al. 2016), a more recent double-blind, randomized placebo-control study phase 1 trial found that repeated ketamine infusions were effective in treating bipolar depression (Chen et al. 2019). Research suggests that ketamine’s NMDA receptor antagonism increases BDNF-mediated synaptic protein synthesis via downstream glutamate-stimulation of AMPA receptors (Duman et al. 2012). Ketamine has also demonstrated a significant degree of interaction with glia-astrocyte-mediated inflammatory signaling (Miller 2013). Thus, beyond its therapeutic efficacy, ketamine potentially represents a paradigm-shifting convergence of the inflammatory and glutamate hypotheses of depression.
Approved by the FDA for the treatment of amyotrophic lateral sclerosis, riluzole (2-amino-6-trifluoromethoxy benzothiazole), is a glutamatergic modulator with both neuroprotective and anticonvulsant properties. Riluzole inhibits voltage-dependent sodium channels in neurons with subsequent inhibition of glutamate release, enhancing AMPA trafficking and membrane insertion of GluR1 and GluR2 and also increasing glutamate reuptake (Bellingham 2011). While early studies showed promise of riluzole in bipolar depression (Machado-Vieira et al. 2012), a more recent double-blind, placebo-controlled trial failed to show efficacy (Park et al. 2017). Another NMDA agent, memantine, is approved for dementia; it acts as a low-affinity NMDA receptor antagonist (Rammes et al. 2008). Like riluzole, initial clinical trials and case reports generated relatively positive results as an add-on to mood stabilizers in both mania (Koukopoulos et al. 2010; Serra et al. 2013) and bipolar depression (Stevens et al. 2013). However, a recent meta-analysis of randomized, double-blind controlled trials failed to demonstrate efficacy (Zheng et al. 2019). Especially given recent findings in relation to NMDA signaling, targeted modulation of glutamate neurotransmission will likely be an area of great clinical potential in the near future.
9 Dopaminergic System
Dopaminergic neurotransmission and its dysregulation in the development of BD are shown at different levels of evidence: behavioral, biomarker, and pharmacological proof-of-concept studies. Increasing dopamine activity is known to produce mania-like clinical presentations (Cousins et al. 2009). Specifically, amphetamine inhibits dopamine transporter-mediated reuptake and increases dopamine synaptic stimulation in the striatum, nucleus accumbens, and the frontal cortex. Predictably, it induces mood elevation, goal-directed activities, and motor hyperactivity and decreases the need for sleep. Likewise, L-dopa, a dopamine precursor, can induce manic or hypomanic states when used as a treatment for Parkinson’s disease (PD). Homovanillic acid (HVA), a metabolite of dopamine, is decreased in the CSF of untreated individuals with bipolar depression. Conversely, treated and manic subjects have normal or increased HVA (Zarate et al. 2004). A recent meta-analysis of 26 studies supports this claim that decreased HVA is found in those with depressive disorders (Ogawa et al. 2018).
Measurements of in vivo availability of dopamine receptor binding using single-photon emission computed tomography (SPECT) radiotracer [123I] iodobenzamide (IBZM) have generated mixed results. One study demonstrated reduced D1 receptor binding potentials in the frontal cortex when compared to healthy controls, while D2 receptor density was normal in all phases of non-psychotic BD individuals (Gonul et al. 2009). Using SPECT radiotracer [99mTc], a different study found increased dopamine transporter (DAT) availability in euthymic bipolar patients when compared to healthy subjects (Chang et al. 2010). Furthermore, another study used positron emission tomography (PET) and found that unmedicated BD subjects had significantly lower DAT availability and possibly higher dopamine concentrations in the dorsal caudate (Anand et al. 2011). In contrast, a different study found greater DAT density in unipolar and bipolar depressed vs non-depressed subjects (Amsterdam et al. 2012). More studies are needed to elucidate the role of dopamine receptor binding in mania and depression.
As increasing evidence reinforces the role of dopamine in BD pathophysiology, prescriptions of atypical antipsychotics are increasing. One cohort of 343 patients with bipolar depression who received olanzapine monotherapy significantly improved from their symptoms when compared to 171 bipolar depression patients receiving placebo in a randomized, double-blind placebo-controlled trial (Tohen et al. 2012). A separate randomized, double-blind placebo-controlled trial of 802 subjects with acute bipolar depression, which compared two dosages of quetiapine with lithium and placebo, found quetiapine more effective than both (Young et al. 2010). Recently, another randomized, double-blind placebo-controlled trial found cariprazine, a different atypical antipsychotic, to be effective, well-tolerated, and safe in depressive symptoms in adults with bipolar I (Earley et al. 2019). One proposed theory is that the atypical antipsychotics have 5-HT2A antagonism and some D2 receptor antagonism/partial D2 agonism, which balances the dopamine signaling and leads to anti-manic effects (Kato 2019). This could partially explain the aforementioned mixed findings regarding dopamine receptor activity in BD.
Pramipexole, an aminothiazole derivative D2/D3 agonist, approved for use in PD, has been employed in proof-of-concept clinical trials in bipolar depression. Its theoretical utility as an antidepressant is derived in part from its D3 receptor activity, which modulates several neuronal circuits implicated in depressive states (Zarate et al. 2004). It also increases anti-apoptotic Bcl-2 expression (Inden et al. 2009), suggesting an added neuroprotective benefit (Shaltiel et al. 2007). Previously, a cohort of 23 patients were followed, and 60.9% of patients showed sustained remission of a depressive episode (defined as a > 50% on the Montgomery-Asberg Depression Rating Scale score) (Cassano et al. 2004). Using similar criteria, a subsequent meta-analysis showed that pramipexole had a response rate of 52.5%, a long-term response rate of 62.1%, and a long-term remission rate of 39.6% in 504 patients (Tundo et al. 2019). Randomized clinical trials have also demonstrated superiority compared to placebo in major depressive episodes (Tundo et al. 2019). While pramipexole showed beneficial as a therapeutic option for depression in BD patients, the authors suggest having an RCT of a higher power to confirm its benefit (Tundo et al. 2019).
10 Neurohormonal System
Circadian abnormalities have been recently associated with BD (Melo et al. 2017). Rhythm disruption can both precipitate and exacerbate mood episodes (Hirata et al. 2007). It is suggested that causality of this phenomenon is bidirectional, with circadian disruptions also being a consequence of affective disorders themselves (Bechtel 2015). Even in the euthymic state, BD patients have more alterations in their sleeping patterns than healthy controls (Ng et al. 2015). Circadian rhythms are regulated primarily by the secretion of melatonin from the suprachiasmatic nucleus (SCN) and subsequent binding to MT1 and MT2 receptors in the posterior hypothalamus. Normally, melatonin secretion reaches its peak during the night and trough during the day. BD patients characteristically show a delayed onset and lower evening peak of melatonin secretion compared to healthy controls (Robillard et al. 2013; Nurnberger et al. 2000). Mutant mice, deficient in the MT1 receptor encoding gene, display behavioral alterations that resemble some symptoms of depression (Comai et al. 2015).
Corticotropin-releasing hormone (CRH), secreted by the hypothalamus, stimulates the release of adrenocorticotropic hormone (ACTH) from the pituitary gland. ACTH then enables the secretion of cortisol by the adrenal glands. Circulating cortisol exerts a negative feedback effect at multiple levels within the hypothalamic-pituitary-adrenal (HPA) axis. In healthy individuals, cortisol displays the opposite circadian pattern to melatonin: peaking early in the morning and lowest at night. In addition to secreting melatonin, the SCN also modulates cortisol secretion and cognitive performance, both of which are altered in mania and depression (Linkowski et al. 1994). Both hypercortisolemia and a flattening of circadian cortisol variation are seen in depressed individuals (Carroll et al. 1976). Elevated cortisol response to dexamethasone suppression and CRH (DEX/CRH test) at the time of discharge from an inpatient treatment is also predictive of relapse in depressed individuals (Zobel et al. 2001). As with depression, newly diagnosed bipolar patients display elevated baseline cortisol (Coello et al. 2019).
Additionally, changes in CRH secretion may have potential as a future biomarker, as they can be detected before the clinically observable onset of manic or hypomanic symptoms (Daban et al. 2005). Previous research indicates that cortisol secretion is elevated in the manic and the depressed phases of bipolar disorder, suggesting that aberrant stress responsiveness plays a role in both phases of the disease (Cervantes et al. 2001). Higher cortisol concentrations have also been demonstrated in both remitted and non-remitted bipolar patients, implying a persistence of HPA axis abnormalities beyond symptomatic control (Watson et al. 2004). Ellenbogen et al. found that offspring of parents with bipolar disorder have elevated cortisol compared to those with no parental history of mental illness (Ellenbogen et al. 2004). The heritability of basal cortisol secretion level is estimated to be 60% (Bartels et al. 2003). Taken together, this implicates hormonal axis dysfunction as a core mechanism underlying the pathogenesis and transmission of BD. Aberrancies precede, are passed on, and may persist beyond a patient’s detectable symptomatic course.
In addition to hormone secretion, the glucocorticoid receptor (GR) function plays an intricate role in the pathophysiology of mood disorders. Cortisol diffuses through cellular membranes and binds to both GR and mineralocorticoid (MR) intracellular receptors. The human stress response increases glucocorticoid secretion, preferentially causing MR saturation first. GR binding thus becomes the primary mediator of feedback inhibition on the HPA axis (Pariante et al. 2001). Both glucocorticoids and stress have been shown to impair neurogenesis and promote atrophy of dendritic processes in the hippocampus (Kempermann 2002; McEwen 2005). GR antagonists block the detrimental effects of hypercortisolism and increase the expression of GRs, exerting a more powerful negative feedback effect on the HPA axis.
The extensive involvement of the HPA axis in affective disorders makes this system an attractive target for therapeutic interventions. Tricyclic antidepressants increase glucocorticoid receptor protein binding and capacity in vivo. This effect was also seen in rats when submitted to lithium therapy or electroconvulsive therapy. In humans, elevated diurnal cortisol is dampened with chronic lithium prophylaxis (Colla et al. 2009). Thus, it is suggested that part of the overall therapeutic mechanism in the treatment of BD may involve a gradual reinstatement of appropriate glucocorticoid receptor function and some degree of HPA axis normalization.
As follows, several other therapeutic interventions have been attempted, targeting various aspects of HPA/circadian homeostasis. Exogenous melatonin has well-documented hypnotic properties and has been shown to improve sleep disturbances in the context of depression (Satyanarayanan et al. 2018). However, administering melatonin on its own to patients fails to display any antidepressant efficacy. Conversely, agomelatine, a MT1 and MT2 agonist but also a 5-HT2c antagonist, displayed clear antidepressant activity in animal models of depression (Thomas et al. 2016). A single dose of agomelatine can restore sleep architecture in severely depressed individuals. The compound also induces a faster symptomatic improvement in depressed patients than the SSRI sertraline (Kasper and Hamon 2009). This finding was bolstered by a subsequent systematic review which concluded that agomelatine is a viable treatment for depression (Fornaro et al. 2010). With regard to bipolar disorder, an open-label study for agomelatine enrolled 21 patients with bipolar I depression. Patients received 25 mg/day for 6–46 weeks, with 81% of subjects showing substantial improvement (>50% improvement in HAM-D scores) (Calabrese et al. 2007).
Researchers have also investigated the efficacy of the GR antagonist mifepristone (RU-486) in proof-of-concept trials. In one double-blind, placebo-controlled crossover study, patients with psychotic depression experienced rapid improvement of their symptoms following 4 days of mifepristone therapy (Belanoff et al. 2001). Authors replicated this result in a larger study which also found that elevated dosages (>600 mg/day) may be the optimal therapeutic range (Belanoff et al. 2002). Young et al. conducted a mifepristone trial (600 mg/day vs placebo) in 20 patients with bipolar depression. Spatial recognition/memory, verbal fluency, and HAM-D rating scores all significantly improved in the intervention group. Notably, improvements in cognition were inversely correlated with baseline cortisol levels, further implicating an anti-glucocorticoid effect as the therapeutic mechanism (Young et al. 2004). Gallagher et al. conducted a placebo-controlled, 7-day mifepristone trial of 19 individuals with bipolar disorder and 20 with schizophrenia. There was a significant elevation in cortisol secretion directly following mifepristone administration. However, at 21 days post-treatment, cortisol levels decreased significantly, falling below baseline level in both treatment subgroups. Conversely, cortisol levels for both bipolar and schizophrenic patients in the placebo group remained unchanged. This reinforces the notion that GR antagonists cause normalization of the HPA axis through long-term, receptor-mediated negative feedback. More recently, Watson et al. conducted a RDBPCT evaluating a 7-day course of mifepristone (600 mg/day) vs placebo as an adjunct therapy in 60 patients with bipolar depression. Though patients experienced no antidepressant efficacy, spatial working memory showed substantial improvement, which was sustained 7 weeks after cessation of treatment. Consistent with previous findings, the magnitude of cortisol response to mifepristone directly correlated with the magnitude of memory improvement (Watson et al. 2012).
Glucocorticoid synthesis inhibitors such as ketoconazole and metyrapone have also shown some antidepressant efficacy in clinical and preclinical models. In a double-blind, randomized, controlled trial for MDD, metyrapone was superior to placebo as add-on therapy to conventional antidepressants and accelerated the onset of symptomatic relief (Jahn et al. 2004). Gallagher et al. evaluated five trials conducted with ketoconazole in either MDD or BD, finding a significant difference in HAM-D scores favoring treatment (Gallagher et al. 2008). However, the risks associated with long-term use of these agents may limit their applicability in mood disorders. Nevertheless, these proof-of-concept studies show promise for more-targeted approaches in the future.
The neurohormonal modulator, liraglutide, a glucagon-like peptide 1(GLP-1) analog, has already shown promise in preclinical models of Alzheimer’s disease, Parkinson’s disease, and stroke. Weina et al. found that liraglutide successfully decreased behavioral symptoms of depression and anxiety in a corticosterone-induced mouse model of depression. Importantly, these findings were associated with a reduction in ACTH-mediated stress responsiveness. The drug was shown to preserve neuronal plasticity and increase the density of immature neurons in the hippocampus (Weina et al. 2018). Further investigation regarding its clinical efficacy in humans is highly warranted, especially given the strong association between metabolic disease, insulin resistance, and BD.
Non-pharmacologic interventions targeting the neurohormonal/circadian system, including sleep manipulation/deprivation and light therapy, have also been investigated. Total sleep deprivation and partial sleep deprivation during the second half of the night have shown the most antidepressant efficacy (Wirz-Justice et al. 2005). Sleep deprivation, in combination with SSRI, has been proven to accelerate the improvement of depressive symptoms compared to SSRI alone (Benedetti et al. 1997). Light therapy has also shown promise in certain mood disorders, especially seasonal depression. Like sleep deprivation, best results have been demonstrated when used in combination with antidepressants (Lanfumey et al. 2013). Tseng et al. conducted a meta-analysis regarding the use of light therapy and sleep deprivation in patients with bipolar depression. The results of 9 studies, including 489 patients, indicated that adjunct light therapy significantly reduced disease severity in medicated patients (Tseng et al. 2016).
As the primary arbiters of circadian rhythm and stress responses, neurohormones such as cortisol and melatonin play a significant role in the development and transmission of BD. Whether through genetic, epigenetic, or direct signaling mechanisms, circadian and HPA axis dysfunction seems to underlie most mood disorders, making the pathway an attractive target for therapeutic interventions going forward. Successful treatment of BD seems to entail a certain degree of normalization both in GR function and the HPA axis overall. Supporting this hypothesis, therapeutic efficacy, especially in the cognitive domain, is consistently associated with beneficial alterations in cortisol secretion. Currently, however, therapeutic interventions have been mostly limited to proof-of-concept studies and non-pharmacologic modalities, which may not be broadly applicable in real-world clinical settings. Given the significant association between metabolic syndrome and BD, further investigation of hormonal modulators, particularly those which affect insulin signaling, is warranted.
11 Purinergic System and Mania
In 1921, Kraepelin indirectly implicated the purinergic system in the parthenogenesis of BD by suggesting an association between manic symptoms, hyperuricemia, and gout (Ketter 2009). Clinicians have since observed that patients being treated with lithium see improvements not only in their mood disturbances but also in their gout/hyperuricemia (Shorter 2009). This association has subsequently been confirmed by several studies showing elevated uric acid (UA) levels in drug-naïve patients experiencing their first manic episode, as well as nationwide, population-based data indicating an increased risk of gout in patients with BD (Salvadore et al. 2010; Chung et al. 2010). Uric acid modulates a variety of endogenous functions, including sleep, appetite, cognition, memory, motor activity, and social interaction (Machado-Vieira et al. 2002; Lorenzi et al. 2010). Elevated UA levels have been associated with specific manic traits such as impulsivity, irritability, increased drive, disinhibition, and hyperthymia (Machado-Vieira et al. 2002; Lorenzi et al. 2010; Sutin et al. 2014). Manic patients demonstrate increased serum UA compared to those with bipolar depression or MDD (Bartoli et al. 2017b). Higher serum UA is also predictive of bipolar conversion in currently depressed patients (Oliveira et al. 2019). Indeed, hyperuricemia appears to be highly selective for mania in BD (Berardis and De Berardis 2008), whereas low UA levels have been linked to depressive mood scores in BD, independent of current disease phase (Albert et al. 2015; Muti et al. 2015). Reductions in mania are associated with a concurrent decrease in serum uric acid levels, and enhanced urinary excretion of UA has been observed during lithium-induced remission from hypomania (Machado-Vieira et al. 2017a).
Furthermore, plasma uric acid level abnormalities are typically absent during euthymic periods (Berardis and De Berardis 2008). This evidence strongly suggests that purinergic system dysfunction plays an important role, especially early in the development of BD (Machado-Vieira et al. 2008). Given the positive association between peripheral and central uric acid levels (Bowman et al. 2010), UA holds significant potential as a state-dependent biomarker and outcome indicator in BD.
The purine adenosine is decreased in the serum of euthymic bipolar patients when compared to healthy controls, and lower levels confer a higher degree of functional impairment (Gubert et al. 2016). Adenosine receptor agonists characteristically display anti-aggressive, anticonvulsant, and antipsychotic properties, whereas antagonists (caffeine, theophylline) can enhance irritability, anxiety, and insomnia (Lara et al. 2006). This suggests that, beyond acting as surrogate markers for other cellular processes (i.e., nucleic acid turnover), purinergic constituents independently contribute to the overall disease process in BD. Machado-Vieira et al. previously demonstrated the efficacy of allopurinol in treatment-resistant mania associated with hyperuricemia (Machado-Vieira et al. 2001). By inhibiting xanthine oxidase, it is suggested that allopurinol may increase CNS levels of adenosine and other purine metabolites in addition to decreasing UA formation (Marro et al. 2006). Several trials have subsequently demonstrated the efficacy of allopurinol as an adjunct to standard therapy in improving manic symptoms (Machado-Vieira et al. 2002, 2008; Akhondzadeh et al. 2006). Moreover, a 2017 systematic review and meta-analysis of 5 RCTs using adjuvant purine-modulators confirmed their anti-manic efficacy compared to placebo (Bartoli et al. 2017a). Of note, allopurinol can also effectively treat aggressive behavior in patients with dementia, further solidifying the association between UA and the aggression/impulsivity (Lara et al. 2003).
Genetic studies have recently revealed a specific SNP in the P2X7 gene, which encodes a CNS-expressed purine receptor associated with both BD and MDD in animal models (Sperlagh et al. 2012). P2X7 expression is also increased by sleep deprivation and rapid cycling in humans (Backlund et al. 2012). P2X7 receptor-associated neuroinflammation has also been implicated in the parthenogenesis of BD (Masuch et al. 2016). Recently, significant attention has been directed towards developing targeted therapies for P2X7 in BD and MDD, though robust clinical trials have not yet been executed (Bhattacharya et al. 2013; Dodd et al. 2015).
In conclusion, beyond acting as surrogate markers, evidence strongly implicates purinergic system constituents as a priori disease modulators in BD. The diversity of metabolites and downstream interactions associated with this pathway espouse significant potential for future therapeutic and biomarker development.
12 Conclusion
Our evolving understanding of BD weaves an ever-expanding web of conceptual integration. Complexities notwithstanding, several key entities (cortisol, BDNF, PKC, GSK3, calcium, glutamate, and inflammatory cytokines) seem to underlie and connect many of the seemingly disparate concepts discussed in this chapter. Through these elements, we can see how oxidation and mitochondrial function, for example, ultimately affect neurotransmission, plasticity, apoptosis, and even the inflammatory milieu. Despite our limited understanding of the microbiome, we can already appreciate this same dynamic. Small alterations in the gut seem to affect everything from neurotransmitter metabolism, to neuroinflammation, and even the HPA axis. From a therapeutic standpoint, lithium perfectly exemplifies this concept. Its efficacy stems from its ability to modulate so many aspects of this disease from oxidative stress, mitochondrial function, apoptosis, and calcium signaling to inflammation, hormonal activity, glutamate signaling, and even the purinergic system. Likewise, we see how novel therapies like ketamine simultaneously integrate both the glutamate and inflammatory hypotheses of depression through final common pathways. It is no coincidence that emerging biomarkers such as BDNF, TNF-α, UA, and others seem to act as molecular conduits between so many different pathways and systems. Moving forward, clinicians and scientists must build on this ethic: making connections that emphasize a holistic context for every specific discovery, increasing patient screening with objective markers, and implementing multi-modal, tailored approaches to treatment.
References
Abrial E, Etievant A, Bétry C, Scarna H, Lucas G, Haddjeri N, Lambás-Señas L (2013) Protein kinase C regulates mood-related behaviors and adult hippocampal cell proliferation in rats. Prog Neuropsychopharmacol Biol Psychiatry 43:40–48
Ajmone-Cat MA, D'Urso MC, di Blasio G, Brignone MS, De Simone R, Minghetti L (2016) Glycogen synthase kinase 3 is part of the molecular machinery regulating the adaptive response to LPS stimulation in microglial cells. Brain Behav Immun 55:225–235
Akhondzadeh S, Milajerdi MR, Amini H et al (2006) Allopurinol as an adjunct to lithium and haloperidol for treatment of patients with acute mania: a double-blind, randomized, placebo-controlled trial. Bipolar Disord 8:485–489
Albert U et al (2015) Increased uric acid levels in bipolar disorder subjects during different phases of illness. J Affect Disord 173:170–175
Amadio M, Battaini F, Pascale A (2006) The different facets of protein kinases C: old and new players in neuronal signal transduction pathways. Pharmacol Res 54:317–325
Amrollahi Z, Rezaei F, Salehi B, Modabbernia AH, Maroufi A, Esfandiari GR, Naderi M, Ghebleh F, Ahmadi-Abhari SA, Sadeghi M, Tabrizi M, Akhondzadeh S (2011) Double-blind, randomized, placebo-controlled 6-week study on the efficacy and safety of the tamoxifen adjunctive to lithium in acute bipolar mania. J Affect Disord 129(1–3):327–331
Amsterdam JD et al (2012) Greater striatal dopamine transporter density may be associated with major depressive episode. J Affect Disord 141(2–3):425–431
Anand A et al (2011) Striatal dopamine transporter availability in unmedicated bipolar disorder. Bipolar Disord 13(4):406–413
Andreazza AC, Shao L, Wang JF, Young LT (2010) Mitochondrial complex I activity and oxidative damage to mitochondrial proteins in the prefrontal cortex of patients with bipolar disorder. Arch Gen Psychiatry 67:360–368
Arabzadeh S et al (2015) Celecoxib adjunctive therapy for acute bipolar mania: a randomized, double-blind, placebo-controlled trial. Bipolar Disord 17(6):606–614
Arevalo JC, Wu SH (2006) Neurotrophin signaling: many exciting surprises! Cell Mol Life Sci 63:1523–1537
Backlund L et al (2012) P2RX7: expression responds to sleep deprivation and associates with rapid cycling in bipolar disorder type 1. PLoS One 7(8):e43057
Bahls FH, Ozuna J, Ritchie DE (1991) Interactions between calcium channel blockers and the anticonvulsants carbamazepine and phenytoin. Neurology 41(5):740–742
Barbosa IG, Bauer ME, Machado-Vieira R et al (2014) Cytokines in bipolar disorder: paving the way for neuroprogression. Neural Plast 2014:360481
Bartels M et al (2003) Heritability of daytime cortisol levels in children. Behav Genet 33(4):421–433
Bartoli F, Crocamo C et al (2017a) Purinergic system dysfunctions in subjects with bipolar disorder: a comparative cross-sectional study. Compr Psychiatry 73:1–6
Bartoli F, Carrà G, Clerici M (2017b) Purinergic dysfunction in bipolar disorder: Any role for the antioxidant uric acid as a trait and state biomarker? Psychiatry Clin Neurosci 71(6):417
Bartzokis G (2012) Neuroglialpharmacology: myelination as a shared mechanism of action of psychotropic treatments. Neuropharmacology 62(7):2137–2153
Bechtel W (2015) Circadian rhythms and mood disorders: are the phenomena and mechanisms causally related? Front Psych 6:118
Belanoff JK et al (2001) Rapid reversal of psychotic depression using mifepristone. J Clin Psychopharmacol 21(5):516–521
Belanoff JK et al (2002) An open label trial of C-1073 (mifepristone) for psychotic major depression. Biol Psychiatry 52(5):386–392
Bellingham MC (2011) A review of the neural mechanisms of action and clinical efficiency of riluzole in treating amyotrophic lateral sclerosis: what have we learned in the last decade? CNS Neurosci Ther 17(1):4–31
Benedetti F et al (1997) Sleep deprivation hastens the antidepressant action of fluoxetine. Eur Arch Psychiatry Clin Neurosci 247(2):100–103
Beneyto M, Kristiansen LV, Oni-Orisan A, McCullumsmith RE, Meador-Woodruff JH (2007) Abnormal glutamate receptor expression in the medial temporal lobe in schizophrenia and mood disorders. Neuropsychopharmacology 32:1888–1902
Berardis DD, De Berardis D (2008) The role of duloxetine in the treatment of anxiety disorders. Neuropsychiatr Dis Treat 1:929
Berk M, Copolov DL, Dean O et al (2008) N-acetyl cysteine for depressive symptoms in bipolar disorder–a double-blind randomized placebo-controlled trial. Biol Psychiatry 64:468–475
Berk M, Dean OM, Cotton SM et al (2012) Maintenance N-acetyl cysteine treatment for bipolar disorder: a double-blind randomized placebo controlled trial. BMC Med 10:91
Berk M et al (2013) Aspirin: a review of its neurobiological properties and therapeutic potential for mental illness. BMC Med 11(74):2013
Berridge MJ (2014) Calcium signalling and psychiatric disease: bipolar disorder and schizophrenia. Cell Tissue Res 357(2):477–492
Bhat RV, Andersson U, Andersson S, Kneer L, Bauer U, Sundgren-Andersson AK (2018) The conundrum of GSK3 inhibitors: is it the dawn of a new beginning? J Alzheimers Dis 64(1):S547–S554
Bhattacharya A et al (2013) Pharmacological characterization of a novel centrally permeable P2X7 receptor antagonist: JNJ-47965567. Br J Pharmacol 170(3):624–640
Bowman GL et al (2010) Uric acid as a CNS antioxidant. J Alzheimer’s Dis 19(4):1331–1336
Brodie MJ, MacPhee GJ (1986) Carbamazepine neurotoxicity precipitated by diltiazem. Br Med J 292(6529):1170–1171
Brown NC, Andreazza AC, Trevor Young L (2014) An updated meta-analysis of oxidative stress markers in bipolar disorder. Psychiatry Res 218(1–2):61–68
Calabrese JR et al (2007) Agomelatine adjunctive therapy for acute bipolar depression: preliminary open data. Bipolar Disord 9(6):628–635
Capuron L, Neurauter G, Musselman DL et al (2003) Interferon-alpha-induced changes in tryptophan metabolism. Relationship to depression and paroxetine treatment. Biol Psychiatry 54:906–914
Carroll BJ, Curtis GC, Mendels J (1976) Cerebrospinal fluid and plasma free cortisol concentrations in depression. Psychol Med 6(2):235–244
Cassano P et al (2004) Pramipexole in treatment-resistant depression: an extended follow-up. Depress Anxiety 20(3):131–138
Cataldo AM, McPhie DL, Lange NT, Punzell S, Elmiligy S, Ye NZ, Froimowitz MP, Hassinger LC, Menesale EB, Sargent LW, Logan DJ, Carpenter AE, Cohen BM (2010) Abnormalities in mitochondrial structure in cells from patients with bipolar disorder. Am J Pathol 177(2):575–585
Catches JS, Xu J, Contractor A (2012) Genetic ablation of the GluK4 kainate receptor subunit causes anxiolytic and antidepressant-like behavior in mice. Behav Brain Res 228:406–414
Cervantes P et al (2001) Circadian secretion of cortisol in bipolar disorder. J Psychiatry Neurosci 26(5):411–416
Chang TT et al (2010) Higher striatal dopamine transporters in euthymic patients with bipolar disorder: a SPECT study with [Tc] TRODAT-1. Bipolar Disord 12(1):102–106
Chang K-C et al (2015) Estimation of life expectancy and the expected years of life lost among heroin users in the era of opioid substitution treatment (OST) in Taiwan. Drug Alcohol Depend 153:152–158
Chen RW, Chuang DM (1999) Long term lithium treatment suppresses p53 and Bax expression but increases Bcl-2 expression. A prominent role in neuroprotection against excitotoxicity. J Biol Chem 274(10):6039–6042
Chen G, Manji HK, Hawver DB, Wright CB, Potter WZ (1994) Chronic sodium valproate selectively decreases protein kinase C alpha and epsilon in vitro. J Neurochem 63:2361–2364
Chen G, Masana MI, Manji HK (2000) Lithium regulates PKC-mediated intracellular cross-talk and gene expression in the CNS in vivo. Bipolar Disord 2:217–236
Chen M-H et al (2019) Maintenance of antidepressant and antisuicidal effects by D-cycloserine among patients with treatment-resistant depression who responded to low-dose ketamine infusion: a double-blind randomized placebo-control study. Neuropsychopharmacology 44(12):2112–2118
Chourbaji S, Vogt MA, Fumagalli F, Sohr R, Frasca A, Brandwein C et al (2008) AMPA receptor subunit 1 (GluR-A) knockout mice model the glutamate hypothesis of depression. FASEB J 22:3129–3134
Chu Y, Fioravante D, Leitges M, Regehr WG (2014) Calcium-dependent PKC isoforms have specialized roles in short-term synaptic plasticity. Neuron 82:859–871
Chung K-H, Huang C-C, Lin H-C (2010) Increased risk of gout among patients with bipolar disorder: a nationwide population-based study. Psychiatry Res 180(2–3):147–150
Clay HB, Sillivan S, Konradi C (2011) Mitochondrial dysfunction and pathology in bipolar disorder and schizophrenia. Int J Dev Neurosci 29(3):311–324
Coello K et al (2019) Hair cortisol in newly diagnosed bipolar disorder and unaffected first-degree relatives. Psychoneuroendocrinology 99:183–190
Cole AR (2013) Glycogen synthase kinase 3 substrates in mood disorders and schizophrenia. FEBS J 280(21):5213–5227
Colla M et al (2009) Glutamate as a spectroscopic marker of hippocampal structural plasticity is elevated in long-term euthymic bipolar patients on chronic lithium therapy and correlates inversely with diurnal cortisol. Mol Psychiatry 14(7):696–704, 647
Comai S et al (2015) Melancholic-Like behaviors and circadian neurobiological abnormalities in melatonin MT1 receptor knockout mice. Int J Neuropsychopharmacol 18(3):pyu075
Cousins DA, Butts K, Young AH (2009) The role of dopamine in bipolar disorder. Bipolar Disord 11(8):787–806
Craddock N, Sklar P (2013) Genetics of bipolar disorder. Lancet 381(9878):1654–1662
Croarkin PE et al (2015) N-acetylaspartate normalization in bipolar depression after lamotrigine treatment. Bipolar Disord 17(4):450–457
Cryan JF, Kelly PH, Neijt HC, Sansig G, Flor PJ, van Der Putten H (2003) Antidepressant and anxiolytic-like effects in mice lacking the group III metabotropic glutamate receptor mGluR7. Eur J Neurosci 17:2409–2417
D’Addario C et al (2012) Selective DNA Methylation of BDNF Promoter in Bipolar Disorder: Differences Among Patients with BDI and BDII. Neuropsychopharmacology 37(7):1647–1655
Daban C et al (2005) Hypothalamic-pituitary-adrenal axis and bipolar disorder. Psychiatr Clin North Am 28(2):469–480
Dager S, Friedman S, Parow A, Demopulos A, Stoll A, Lyoo I, Dunner D, Renshaw P (2004) Brain metabolic alterations in medication-free patients with bipolar disorder. Arch Gen Psychiatry 61(5):450–458
de Bartolomeis A, Tomasetti C, Iasevoli F (2015) Update on the mechanism of action of aripiprazole: translational insights into antipsychotic strategies beyond dopamine receptor antagonism. CNS Drugs 29(9):773–799
de Sousa RT et al (2014) Oxidative stress in early stage bipolar disorder and the association with response to lithium. J Psychiatr Res 50:36–41
de Sousa RT, Streck EL, Zanetti MV et al (2015a) Lithium increases leukocyte mitochondrial complex I activity in bipolar disorder during depressive episodes. Psychopharmacology (Berl) 232(1):245
de Sousa RT, Zanetti MV, Talib LL, Serpa MH, Chaim TM, Carvalho AF, Brunoni AR, Busatto GF, Gattaz WF, Machado-Vieira R (2015b) Lithium increases platelet serine-9 phosphorylated GSK-3β levels in drug-free bipolar disorder during depressive episodes. J Psychiatr Res 62:78–83
de Sousa RT, Loch AA, Carvalho AF, Brunoni AR, Haddad MR, Henter ID, Zarate CA, Machado-Vieira R (2017) Genetic studies on the tripartite glutamate synapse in the pathophysiology and therapeutics of mood disorders. Neuropsychopharmacology 42(4):787–800
Desplat-Jego S, Johanet C, Escande A, Goetz J, Fabien N, Olsson N et al (2007) Update on anti-Saccharomyces cerevisiae antibodies, anti-nuclear associated anti-neutrophil antibodies and antibodies to exocrine pancreas detected by indirect immunofluorescence as biomarkers in chronic inflammatory bowel diseases: results of a multicenter study. World J Gastroenterol 13(16):2312–2318
Dickerson F, Stallings C, Origoni A, Vaughan C, Khushalani S, Yolken R (2012a) Markers of gluten sensitivity in acute mania: a longitudinal study. Psychiatry Res 196(1):68–71
Dickerson F, Stallings C, Origoni A, Vaughan C, Khushalani S, Yolken R (2012b) Antibodies to the glutamate receptor in mania. Bipolar Disord 14(5):547–553
Dickerson F, Stallings C, Origoni A, Vaughan C, Khushalani S, Yolken R (2013) A combined marker of inflammation in individuals with mania. PLoS One 8(9):e73520
Dickerson F, Severance E, Yolken R (2017) The microbiome, immunity, and schizophrenia and bipolar disorder. Brain Behav Immun 62:46–52
Dodd S, Fernandes BS, Dean OM (2015) Future directions for pharmacotherapies for treatment-resistant bipolar disorder. Curr Neuropharmacol 13(5):656–662
Du J et al (2010) A kinesin signaling complex mediates the ability of GSK-3beta to affect mood-associated behaviors. Proc Natl Acad Sci U S A 107(25):11573–11578
Dubovsky SL et al (1992) Abnormal intracellular calcium ion concentration in platelets and lymphocytes of bipolar patients. Am J Psychiatry 149(1):118–120
Duman RS, Li N, Liu RJ, Duric V, Aghajanian G (2012) Signaling pathways underlying the rapid antidepressant actions of ketamine. Neuropharmacology 62:35–41
Duncan WC Jr, Zarate CA Jr (2013) Ketamine, sleep, and depression: current status and new questions. Curr Psychiatry Rep 15(9):394
Duncan LE, Holmans PA, Lee PH, O'Dushlaine CT, Kirby AW, Smoller JW et al (2014) Pathway analyses implicate glial cells in schizophrenia. PLoS One 9:e89441
Duric V, Banasr M, Stockmeier CA, Simen AA, Newton SS, Overholser JC et al (2013) Altered expression of synapse and glutamate related genes in post-mortem hippocampus of depressed subjects. Int J Neuropsychopharmacol 16:69–82
Earley W et al (2019) Cariprazine treatment of bipolar depression: a randomized double-blind placebo-controlled phase 3 study. Am J Psychiatry 176(6):439–448
Ellenbogen MA, Hodgins S, Walker C-D (2004) High levels of cortisol among adolescent offspring of parents with bipolar disorder: a pilot study. Psychoneuroendocrinology 29(1):99–106
Felger JC, Lotrich FE (2013) Inflammatory cytokines in depression: neurobiological mechanisms and therapeutic implications. Neuroscience 246:199–229
Fernandes BS et al (2011) Brain-derived neurotrophic factor as a state-marker of mood episodes in bipolar disorders: a systematic review and meta-regression analysis. J Psychiatr Res 45(8):995–1004
Fernandes BS et al (2015) Peripheral brain-derived neurotrophic factor (BDNF) as a biomarker in bipolar disorder: a meta-analysis of 52 studies. BMC Med 13:289
Fillman SG, Sinclair D, Fung SJ, Webster MJ, Shannon Weickert C (2014) Markers of inflammation and stress distinguish subsets of individuals with schizophrenia and bipolar disorder. Transl Psychiatry 4:e365
Fornaro M et al (2010) A systematic, updated review on the antidepressant agomelatine focusing on its melatonergic modulation. Curr Neuropharmacol 8(3):287–304
Frye MA et al (2003) Low CSF somatostatin associated with response to nimodipine in patents with affective illness. Biol Psychiatry 53(2):180–183
Gallagher P et al (2008) Antiglucocorticoid treatments for mood disorders. Cochrane Database Syst Rev (1):CD005168
Giannini AJ et al (1984) Antimanic effects of verapamil. Am J Psychiatry 141(12):1602–1603
Giannini AJ et al (2000) Magnesium oxide augmentation of verapamil maintenance therapy in mania. Psychiatry Res 93(1):83–87
Goldstein BI, Kemp DE, Soczynska JK et al (2009) Inflammation and the phenomenology, pathophysiology, comorbidity, and treatment of bipolar disorder: a systematic review of the literature. J Clin Psychiatry 70:1078–1090
Gonul AS, Coburn K, Kula M (2009) Cerebral blood flow, metabolic, receptor, and transporter changes in bipolar disorder: the role of PET and SPECT studies. Int Rev Psychiatry 21(4):323–335
Goodwin FK, Jamison K (2007) Manic-depressive illness, 2nd edn. Oxford University Press, New York
Grande I, Fries GR, Kunz M, Kapczinski F (2010) The role of BDNF as a mediator of neuroplasticity in bipolar disorder. Psychiatry Investig 7(4):243–250
Gubert C et al (2016) Peripheral adenosine levels in euthymic patients with bipolar disorder. Psychiatry Res 246:421–426
Haarman BCM et al (2014a) Relationship between clinical features and inflammation-related monocyte gene expression in bipolar disorder – towards a better understanding of psychoimmunological interactions. Bipolar Disord 16(2):137–150
Haarman BC, Riemersma-Van der Lek RF, de Groot JC et al (2014b) Neuroinflammation in bipolar disorder – A [(11)C]-(R)-PK11195 positron emission tomography study. Brain Behav Immun 40:219–225
Haile CN et al (2014) Plasma brain derived neurotrophic factor (BDNF) and response to ketamine in treatment-resistant depression. Int J Neuropsychopharmacol 17(2):331–336
Harrison PJ (2016) Molecular neurobiological clues to the pathogenesis of bipolar disorder. Curr Opin Neurobiol 36:1–6
Heyes S et al (2015) Genetic disruption of voltage-gated calcium channels in psychiatric and neurological disorders. Prog Neurobiol 134:36–54
Hirata FC et al (2007) Depression in medical school: the influence of morningness-eveningness. Chronobiol Int 24(5):939–946
Hussaini SM, Choi CI, Cho CH, Kim HJ, Jun H, Jang MH (2014) Wnt signaling in neuropsychiatric disorders: ties with adult hippocampal neurogenesis and behavior. Neurosci Biobehav Rev 47:369–383
Inden M et al (2009) Neuroprotective effect of the antiparkinsonian drug pramipexole against nigrostriatal dopaminergic degeneration in rotenone-treated mice. Neurochem Int 55(8):760–767
Jahn H et al (2004) Metyrapone as additive treatment in major depression. Arch Gen Psychiatry 61(12):1235
Janicak PG et al (1998) Verapamil for the treatment of acute mania: a double-blind, placebo-controlled trial. Am J Psychiatry 155(7):972–973
Jun C, Choi Y, Lim SM, Bae S, Hong YS, Kim JE, Lyoo IK (2014) Disturbance of the glutamatergic system in mood disorders. Exp Neurobiol 23:28–35
Kalinichev M, Dawson LA (2011) Evidence for antimanic efficacy of glycogen synthase kinase-3 (GSK3) inhibitors in a strain-specific model of acute mania. Int J Neuropsychopharmacol 14(8):1051–1067
Kanazawa LK, Vecchia DD, Wendler EM, Hocayen PA, Berao PS Jr, de Melo ML, Dos Reis Livero FA, Corso CR, Stipp MC, Acco A, Andreatini R (2017) Effects of acute and chronic quercetin administration on methylphenidate-induced hyperlocomotion and oxidative stress. Life Sci 171:1–8
Kasper S, Hamon M (2009) Beyond the monoaminergic hypothesis: agomelatine, a new antidepressant with an innovative mechanism of action. World J Biol Psychiatry 10(2):117–126
Kato T (2017) Neurobiological basis of bipolar disorder: mitochondrial dysfunction hypothesis and beyond. Schizophr Res 187:62–66
Kato T (2019) Current understanding of bipolar disorder: toward integration of biological basis and treatment strategies. Psychiatry Clin Neurosci 73(9):526–540
Kato T, Stine O, McMahon F, Crowe R (1997) Increased levels of a mitochondrial DNA deletion in the brain of patients with bipolar disorder. Biol Psychiatry 42(10):871–875
Keck PE Jr et al (2000) A review of randomized, controlled clinical trials in acute mania. J Affect Disord 59(1):S31–S37
Kemp DE, Schinagle M, Gao K et al (2014) PPAR-gamma agonism as a modulator of mood: proof-of-concept for pioglitazone in bipolar depression. CNS Drugs 28:571–581
Kempermann G (2002) Regulation of adult hippocampal neurogenesis – implications for novel theories of major depression. Bipolar Disord 4(1):17–33
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE (2005) Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 62:593–602
Ketter TA (2009) Handbook of diagnosis and treatment of bipolar disorders. American Psychiatric Pub, Washington
Kim HJ, Thayer SA (2009) Lithium increases synapse formation between hippocampal neurons by depleting phosphoinositides. Mol Pharmacol 75(5):1021–1030
Klein PS, Melton DA (1996) A molecular mechanism for the effect of lithium on development. Proc Natl Acad Sci U S A 93(16):8455–8459
Koukopoulos A et al (2010) Antimanic and mood-stabilizing effect of memantine as an augmenting agent in treatment-resistant bipolar disorder. Bipolar Disord 12(3):348–349
Kubo H et al (2017) 1H-magnetic resonance spectroscopy study of glutamate-related abnormality in bipolar disorder. J Affect Disord 208:139–144
Lanfumey L, Mongeau R, Hamon M (2013) Biological rhythms and melatonin in mood disorders and their treatments. Pharmacol Ther 138(2):176–184
Lara DR et al (2003) Allopurinol for the treatment of aggressive behaviour in patients with dementia. Int Clin Psychopharmacol 18(1):53–55
Lara DR et al (2006) Involvement of adenosine in the neurobiology of schizophrenia and its therapeutic implications. Prog Neuropsychopharmacol Biol Psychiatry 30(4):617–629
Leboyer M et al (2012) Can bipolar disorder be viewed as a multi-system inflammatory disease? J Affect Disord 141(1):1–10
Lee YT, Hu LY, Shen CC, Huang MW, Tsai SJ, Yang AC et al (2015) Risk of psychiatric disorders following irritable bowel syndrome: a nationwide population-based cohort study. PLoS One 10(7):e0133283
Linkowski P et al (1994) The 24-hour profiles of cortisol, prolactin, and growth hormone secretion in mania. Arch Gen Psychiatry 51(8):616–624
Lorenzi TM et al (2010) Association of serum uric acid levels with emotional and affective temperaments. J Affect Disord 121(1–2):161–164
Louveau A, Smirnov I, Keyes TJ et al (2015) Structural and functional features of central nervous system lymphatic vessels. Nature 523:337–341
Lu R-B et al (2012) Neuroprotective and neurogenesis agent for treating bipolar II disorder: add-on memantine to mood stabilizer works. Med Hypotheses 79(2):280–283
Machado-Vieira R et al (2001) Therapeutic efficacy of allopurinol in mania associated with hyperuricemia. J Clin Psychopharmacol 21(6):621–622
Machado-Vieira R et al (2002) Purinergic dysfunction in mania: an integrative model. Med Hypotheses 58(4):297–304
Machado-Vieira R et al (2007) Oxidative stress parameters in unmedicated and treated bipolar subjects during initial manic episode: a possible role for lithium antioxidant effects. Neurosci Lett 421(1):33–36
Machado-Vieira R et al (2008) A double-blind, randomized, placebo-controlled 4-week study on the efficacy and safety of the purinergic agents allopurinol and dipyridamole adjunctive to lithium in acute bipolar mania. J Clin Psychiatry 69(8):1237–1245
Machado-Vieira R, Manji HK, Zarate CA Jr (2009) The role of lithium in the treatment of bipolar disorder: convergent evidence for neurotrophic effects as a unifying hypothesis. Bipolar Disord:92–109. https://doi.org/10.1111/j.1399-5618.2009.00714.x
Machado-Vieira R et al (2011) The Bcl-2 gene polymorphism rs956572AA increases inositol 1,4,5-trisphosphate receptor-mediated endoplasmic reticulum calcium release in subjects with bipolar disorder. Biol Psychiatry 69(4):344–352
Machado-Vieira R et al (2012) Novel glutamatergic agents for major depressive disorder and bipolar disorder. Pharmacol Biochem Behav 100(4):678–687
Machado-Vieira R, Salem H et al (2017a) Convergent lines of evidence support the role of uric acid levels as a potential biomarker in bipolar disorder. Expert Rev Mol Diagn 17(2):107–108
Machado-Vieira R, Zanetti MV et al (2017b) Increased brain lactate during depressive episodes and reversal effects by lithium monotherapy in drug-naive bipolar disorder. J Clin Psychopharmacol 37(1):40–45
Maes M, Leonard BE, Myint AM et al (2011) The new ‘5-HT’ hypothesis of depression: cell-mediated immune activation induces indoleamine 2,3-dioxygenase, which leads to lower plasma tryptophan and an increased synthesis of detrimental tryptophan catabolites (TRYCATs), both of which contribute to the onset of depression. Prog Neuro-Psychopharmacology Biol Psychiatry 35:702–721
Mallinger AG et al (2008) Verapamil augmentation of lithium treatment improves outcome in mania unresponsive to lithium alone: preliminary findings and a discussion of therapeutic mechanisms. Bipolar Disord 10(8):856–866
Marro PJ, Mishra OP, Delivoria-Papadopoulos M (2006) Effect of allopurinol on brain adenosine levels during hypoxia in newborn piglets. Brain Res 1073-1074:444–450
Masuch A et al (2016) Mechanism of microglia neuroprotection: involvement of P2X7, TNFα, and valproic acid. Glia 64(1):76–89
McCarthy MJ, Wei H, Marnoy Z, Darvish RM, McPhie DL, Cohen BM, Welsh DK (2013) Genetic and clinical factors predict lithium’s effects on PER2 gene expression rhythms in cells from bipolar disorder patients. Transl Psychiatry 3:e318
McCloud TL et al (2016) Ketamine and other glutamate receptor modulators for depression in bipolar disorder in adults. BJ Psych Advances 22(4):215–215
McEwen BS (2005) Glucocorticoids, depression, and mood disorders: structural remodeling in the brain. Metab Clin Exp 54(5). Suppl 1:20–23
Melo MCA et al (2017) Chronotype and circadian rhythm in bipolar disorder: a systematic review. Sleep Med Rev 34:46–58
Mertens J et al (2015) Differential responses to lithium in hyperexcitable neurons from patients with bipolar disorder. Nature 527(7576):95–99
Miller A (2013) Conceptual confluence: the kynurenine pathway as a common target for ketamine and the convergence of the inflammation and glutamate hypotheses of depression. Neuropsychopharmacology 38:1607–1608
Mischoulon D (2009) Update and critique of natural remedies as antidepressant treatments. Obstet Gynecol Clin North Am 36:789–807
Modabbernia A, Taslimi S, Brietzke E et al (2013) Cytokine alterations in bipolar disorder: a meta-analysis of 30 studies. Biol Psychiatry 74:15–25
Molendijk ML et al (2014) Serum BDNF concentrations as peripheral manifestations of depression: evidence from a systematic review and meta-analyses on 179 associations (N=9484). Mol Psychiatry 19(7):791–800
Muneer A (2017) Wnt and GSK3 signaling pathways in bipolar disorder: clinical and therapeutic implications. Clin Psychopharmacol Neurosci 15(2):100–114
Munkholm K, Brauner JV, Kessing LV et al (2013) Cytokines in bipolar disorder vs. healthy control subjects: a systematic review and meta-analysis. J Psychiatr Res 47:1119–1133
Munkholm K et al (2019) A multisystem composite biomarker as a preliminary diagnostic test in bipolar disorder. Acta Psychiatr Scand 139(3):227–236
Muti M et al (2015) Serum uric acid levels and different phases of illness in bipolar I patients treated with lithium. Psychiatry Res 225(3):604–608
Naik MU, Benedikz E, Hernandez I, Libien J, Hrabe J, Valsamis M, Dow-Edwards D, Osman M, Sacktor TC (2000) Distribution of protein kinase Mzeta and the complete protein kinase C isoform family in rat brain. J Comp Neurol 426:243–258
Nam Y, Wie MB, Shin EJ, Nguyen TT, Nah SY, Ko SK, Jeong JH, Jang CG, Kim HC (2015) Ginsenoside Re protects methamphetamine-induced mitochondrial burdens and proapoptosis via genetic inhibition of protein kinase C delta in human neuroblastoma dopaminergic SH-SY5Y cell lines. J Appl Toxicol 35:927–944
Ng TH et al (2015) Sleep-wake disturbance in interepisode bipolar disorder and high-risk individuals: a systematic review and meta-analysis. Sleep Med Rev 20:46–58
Nierenberg AA et al (2013) Mitochondrial modulators for bipolar disorder: a pathophysiologically informed paradigm for new drug development. Aust N Z J Psychiatry 47(1):26–42
Nonaka S, Hough CJ, Chuang DM (1998) Chronic lithium treatment robustly protects neurons in the central nervous system against excitotoxicity by inhibiting N-methyl-D-aspartate receptor-mediated calcium influx. Proc Natl Acad Sci U S A 95(5):2642–2647
Nurnberger JI Jr et al (2000) Melatonin suppression by light in euthymic bipolar and unipolar patients. Arch Gen Psychiatry 57(6):572–579
Nurnberger JI Jr et al (2014) Identification of pathways for bipolar disorder: a meta-analysis. JAMA Psychiat 71(6):657–664
Ogawa S, Tsuchimine S, Kunugi H (2018) Cerebrospinal fluid monoamine metabolite concentrations in depressive disorder: a meta-analysis of historic evidence. J Psychiatr Res 105:137–146
Oliveira PMS et al (2019) Serum uric acid as a predictor of bipolarity in individuals with a major depressive episode. Bipolar Disord 21(3):235–243
Pace TW, Miller AH (2009) Cytokines and glucocorticoid receptor signaling. Relevance to major depression. Ann N Y Acad Sci 1179:86–105
Pahl S, Tapken D, Haering SC, Hollmann M (2014) Trafficking of kainate receptors. Membranes 4:565–595
Pandey GN, Rizavi HS, Tripathi M, Ren X (2015) Region-specific dysregulation of glycogen synthase kinase-3β and β-catenin in the postmortem brains of subjects with bipolar disorder and schizophrenia. Bipolar Disord 17:160–171
Papp M, Moryl E (1994) Antidepressant activity of non-competitive and competitive NMDA receptor antagonists in a chronic mild stress model of depression. Eur J Pharmacol 263:1–7
Pariante CM et al (2001) Antidepressants enhance glucocorticoid receptor function in vitro by modulating the membrane steroid transporters. Br J Pharmacol 134(6):1335–1343
Park LT et al (2017) A double-blind, placebo-controlled, pilot study of riluzole monotherapy for acute bipolar depression. J Clin Psychopharmacol 37(3):355–358
Pazzaglia PJ et al (1998) Nimodipine monotherapy and carbamazepine augmentation in patients with refractory recurrent affective illness. J Clin Psychopharmacol 18(5):404–413
Perugi G, Quaranta G, Belletti S et al (2014) General medical conditions in 347 bipolar disorder patients: clinical correlates of metabolic and autoimmune-allergic diseases. J Affect Disord 107C:95–103
Pfaffenseller B et al (2016) Differential expression of transcriptional regulatory units in the prefrontal cortex of patients with bipolar disorder: potential role of early growth response gene 3. Transl Psychiatry 6(5):e805–e805
Pfaffenseller B et al (2018) Immediate early gene and the brain-derived neurotrophic factor in bipolar disorder. Front Behav Neurosci 12:15
Pilar-Cúellar F, Vidal R, Díaz A, Castro E, dos Anjos S, Vargas V, Romero B, Valdizán EM (2014) Signaling pathways involved in antidepressant-induced cell proliferation and synaptic plasticity. Curr Pharm Des 20(23):3776–3794
Polter A, Beurel E, Yang S, Garner R, Song L, Miller CA, Sweatt JD, McMahon L, Bartolucci AA, Li X, Jope RS (2010) Deficiency in the inhibitory serine-phosphorylation of glycogen synthase kinase-3 increases sensitivity to mood disturbances. Neuropsychopharmacology 35(8):1761–1774
Price WA, James Giannini A (1986) Neurotoxicity caused by lithium-verapamil synergism. J Clin Pharmacol 26(8):717–719
Rammes G, Danysz W, Parsons CG (2008) Pharmacodynamics of memantine: an update. Curr Neuropharmacol 6(1):55–78
Rao JS, Harry GJ, Rapoport SI et al (2010) Increased excitotoxicity and neuroinflammatory markers in postmortem frontal cortex from bipolar disorder patients. Mol Psychiatry 15:384–392
Rizzo LB et al (2013) Immunosenescence is associated with human cytomegalovirus and shortened telomeres in type I bipolar disorder. Bipolar Disord 15(8):832–838
Robillard R et al (2013) Sleep-wake cycle and melatonin rhythms in adolescents and young adults with mood disorders: comparison of unipolar and bipolar phenotypes. Eur Psychiatry 28(7):412–416
Rong Y, Distelhorst CW (2008) Bcl-2 protein family members: versatile regulators of calcium signaling in cell survival and apoptosis. Annu Rev Physiol 70:73–91
Rosenblat JD, McIntyre RS (2015) Are medical comorbid conditions of bipolar disorder due to immune dysfunction? Acta Psychiatr Scand 132(3):180–191
Rosenblat JD, Cha DS, Mansur RB et al (2014) Inflamed moods: a review of the interactions between inflammation and mood disorders. Prog Neuropsychopharmacol Biol Psychiatry 53:23–34
Rosso IM, Crowley DJ, Silveri MM, Rauch SL, Jensen JE (2017) Hippocampus glutamate and N-acetyl aspartate markers of excitotoxic neuronal compromise in posttraumatic stress disorder. Neuropsychopharmacology 42(8):1698–1705
Rowland T, Perry BI, Upthegrove R, Barnes N, Chatterjee J, Gallacher D, Marwaha S (2018) Neurotrophins, cytokines, oxidative stress mediators and mood state in bipolar disorder: systematic review and meta-analyses. Br J Psychiatry 213(3):514–525
Salvadore G et al (2010) Increased uric acid levels in drug-naïve subjects with bipolar disorder during a first manic episode. Prog Neuropsychopharmacol Biol Psychiatry 34(6):819–821
Sanacora G et al (2017) A consensus statement on the use of ketamine in the treatment of mood disorders. JAMA Psychiat 74(4):399–405
Sarris J, Schoendorfer N, Kavanagh DJ (2009) Major depressive disorder and nutritional medicine: a review of monotherapies and adjuvant treatments. Nutr Rev 67:125–131
Sarris J, Mischoulon D, Schweitzer I (2011) Adjunctive nutraceuticals with standard pharmacotherapies in bipolar disorder: a systematic review of clinical trials. Bipolar Disord 13:454–465
Satyanarayanan SK et al (2018) Circadian rhythm and melatonin in the treatment of depression. Curr Pharm Des 24(22):2549–2555
Saxena A, Scaini G, Bavaresco DV et al (2017) Role of protein kinase C in bipolar disorder: a review of the current literature [published correction appears in Mol Neuropsychiatry. 2018 Feb;3(3):180. Valvassoria, Samira S [corrected to Valvassori, Samira S]]. Mol Neuropsychiatry 3(2):108–124
Sequeira A, Martin M, Rollins B, Moon E, Bunney W, Macciardi F, Lupoli S, Smith E, Kelsoe J, Magnan C, van Oven M, Baldi P, Wallace D, Vawter M (2012) Mitochondrial mutations and polymorphisms in psychiatric disorders. Front Genet 3:103
Serra G et al (2013) Antimanic and long-lasting mood stabilizing effect of memantine in bipolar I mood disorder: two case reports. J Clin Psychopharmacol 33(5):715–717
Severance EG, Alaedini A, Yang S, Halling M, Gressitt KL, Stallings CR et al (2012) Gastrointestinal inflammation and associated immune activation in schizophrenia. Schizophr Res 138(1):48–53
Severance EG, Gressitt KL, Yang S, Stallings CR, Origoni AE, Vaughan C et al (2014) Seroreactive marker for inflammatory bowel disease and associations with antibodies to dietary proteins in bipolar disorder. Bipolar Disord 16(3):230–240
Severance EG, Prandovszky E, Castiglione J, Yolken RH (2015) Gastroenterology issues in schizophrenia: why the gut matters. Curr Psychiatry Rep 17(5):27
Shaltiel G, Chen G, Manji HK (2007) Neurotrophic signaling cascades in the pathophysiology and treatment of bipolar disorder. Curr Opin Pharmacol 7(1):22–26
Shorter E (2009) The history of lithium therapy. Bipolar Disord 11(2):4–9
Silverstone PH, Birkett L (2000) Diltiazem as augmentation therapy in patients with treatment-resistant bipolar disorder: a retrospective study. J Psychiatry Neurosci 25(3):276–280
Soares JC et al (2000) Concurrent measures of protein kinase C and phosphoinositides in lithium-treated bipolar patients and healthy individuals: a preliminary study. Psychiatry Res 95(2):109–118
Sperlagh B et al (2012) The role of purinergic signaling in depressive disorders. Neuropsychopharmacol Hung 14(4):231–238
Stertz L, Magalhaes PV, Kapczinski F (2013) Is bipolar disorder an inflammatory condition? The relevance of microglial activation. Curr Opin Psychiatry 26:19–26
Stevens J et al (2013) Bayesian model of Hamilton Depression Rating Score (HDRS) with memantine augmentation in bipolar depression. Br J Clin Pharmacol 75(3):791–798
Sutin AR et al (2014) Impulsivity is associated with uric acid: evidence from humans and mice. Biol Psychiatry 75(1):31–37
Talaei A et al (2016) Tamoxifen: a protein kinase C inhibitor to treat mania: a systematic review and meta-analysis of randomized, placebo-controlled trials. J Clin Psychopharmacol 36(3):272–275
Thomas J, Khanam R, Vohora D (2016) Augmentation of antidepressant effects of venlafaxine by agomelatine in mice are independent of kynurenine pathway. Neurochem Int 99:103–109
Tohen M et al (2012) Randomised, double-blind, placebo-controlled study of olanzapine in patients with bipolar I depression. Br J Psychiatry J Ment Sci 201(5):376–382
Tseng P-T et al (2016) Light therapy in the treatment of patients with bipolar depression: a meta-analytic study. Eur Neuropsychopharmacol 26(6):1037–1047
Tundo A, de Filippis R, De Crescenzo F (2019) Pramipexole in the treatment of unipolar and bipolar depression. A systematic review and meta-analysis. Acta Psychiatr Scand 140(2):116–125
Valvezan AJ, Klein PS (2012) GSK-3 and Wnt signaling in neurogenesis and bipolar disorder. Front Mol Neurosci 5(1):1
Wang HY, Friedman E (1996) Enhanced protein kinase C activity and translocation in bipolar affective disorder brains. Biol Psychiatry 40:568–575
Wang HY, Markowitz P, Levinson D, Undie AS, Friedman E (1999) Increased membrane-associated protein kinase C activity and translocation in blood platelets from bipolar affective disorder patients. J Psychiatr Res 33:171–179
Warsh JJ, Andreopoulos S, Li PP (2004) Role of intracellular calcium signaling in the pathophysiology and pharmacotherapy of bipolar disorder: current status. Clin Neurosci Res 4(3–4):201–213
Watson S et al (2004) Hypothalamic-pituitary-adrenal axis function in patients with bipolar disorder. Br J Psychiatry 184:496–502
Watson S et al (2012) A randomized trial to examine the effect of mifepristone on neuropsychological performance and mood in patients with bipolar depression. Biol Psychiatry 72(11):943–949
Weina H et al (2018) Liraglutide attenuates the depressive- and anxiety-like behaviour in the corticosterone induced depression model via improving hippocampal neural plasticity. Brain Res 1694:55–62
Weston PG (1922) The determination of sodium, potassium, calcium, and magnesium in the blood and spinal fluid of patients suffering from manic depressive insanity. Arch Neurol Psychiatry 8(2):179
Wirz-Justice A et al (2005) Chronotherapeutics (light and wake therapy) in affective disorders. Psychol Med 35(7):939–944
Xu P, Rosen KM, Hedstrom K, Rey O, Guha S, Hart C, Corfas G (2013) Nerve injury induces glial cell line-derived neurotrophic factor (GDNF) expression in Schwann cells through purinergic signaling and the PKC-PKD pathway. Glia 61:1029–1040
Xu H, Czerwinski P, Xia N, Forstermann U, Li H (2015) Downregulation of BDNF expression by PKC and by TNF-alpha in human endothelial cells. Pharmacology 96:1–10
Yildiz A et al (2008) Protein kinase C inhibition in the treatment of mania: a double-blind, placebo-controlled trial of tamoxifen. Arch Gen Psychiatry 65(3):255–263
Yildiz A et al (2016) Antimanic treatment with tamoxifen affects brain chemistry: a double-blind, placebo-controlled proton magnetic resonance spectroscopy study. Biol Psychiatry Cogn Neurosci Neuroimaging 1(2):125–131
Yoshimizu T et al (2015) Functional implications of a psychiatric risk variant within CACNA1C in induced human neurons. Mol Psychiatry 20(2):162–169
Young AH et al (2004) Improvements in neurocognitive function and mood following adjunctive treatment with mifepristone (RU-486) in bipolar disorder. Neuropsychopharmacology 29(8):1538–1545
Young AH et al (2010) A double-blind, placebo-controlled study of quetiapine and lithium monotherapy in adults in the acute phase of bipolar depression (EMBOLDEN I). J Clin Psychiatry 71(2):150–162
Zarate CA Jr, Du J, Quiroz J, Gray NA, Denicoff KD, Singh J, Charney DS, Manji HK (2003) Regulation of cellular plasticity cascades in the pathophysiology and treatment of mood disorders: role of the glutamatergic system. Ann N Y Acad Sci 1003:273–291
Zarate CA Jr et al (2004) Pramipexole for bipolar II depression: a placebo-controlled proof of concept study. Biol Psychiatry 56(1):54–60
Zarate CA Jr, Singh J, Manji HK (2006) Cellular plasticity cascades: targets for the development of novel therapeutics for bipolar disorder. Biol Psychiatry 59:1006–1020
Zarate CA, Manji HK (2009) Protein kinase C inhibitors: rationale for use and potential in the treatment of bipolar disorder. CNS Drugs 23(7):569–582
Zeinoddini A, Sorayani M, Hassanzadeh E et al (2015) Pioglitazone adjunctive therapy for depressive episode of bipolar disorder: a randomized, double-blind, placebo-controlled trial. Depress Anxiety 32:167–173
Zhang J, Terreni L, De Simoni MG et al (2001) Peripheral interleukin-6 administration increases extracellular concentrations of serotonin and the evoked release of serotonin in the rat striatum. Neurochem Int 38:303–308
Zheng W et al (2019) Adjunctive memantine for major mental disorders: a systematic review and meta-analysis of randomized double-blind controlled trials. Schizophr Res 209:12–21
Zobel AW et al (2001) Cortisol response in the combined dexamethasone/CRH test as predictor of relapse in patients with remitted depression. a prospective study. J Psychiatr Res 35(2):83–94
Zuccoli GS et al (2017) The energy metabolism dysfunction in psychiatric disorders postmortem brains: focus on proteomic evidence. Front Neurosci 11:493
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Jones, G.H., Rong, C., Shariq, A.S., Mishra, A., Machado-Vieira, R. (2020). Intracellular Signaling Cascades in Bipolar Disorder. In: Young, A.H., Juruena, M.F. (eds) Bipolar Disorder: From Neuroscience to Treatment. Current Topics in Behavioral Neurosciences, vol 48. Springer, Cham. https://doi.org/10.1007/7854_2020_157
Download citation
DOI: https://doi.org/10.1007/7854_2020_157
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-72142-8
Online ISBN: 978-3-030-72143-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)