Abstract
Background: Use of the ergot-derived dopamine receptor agonists (cabergoline and pergolide) is associated with an increased risk of cardiac valvulopathy. Pergolide was withdrawn from the US market in 2007 because of the risk of valvular heart disease, while the European Medicines Agency (EMA) required a reduction in the maximum daily dosage of cabergoline and pergolide from 6mg/day to 3 mg/day in 2008. In Japan, the package inserts of both drugs were revised in April 2007 to request that physicians conduct periodic ultrasonic cardiography (UCG) examinations for patients taking cabergoline or pergolide. Also, through face-to-face communication with medical representatives of drug companies, physicians were informed that use of cabergoline and pergolide has increased the risk of valvulopathy. However, cabergoline and pergolide have remained in wide use, even following the regulatory actions.
Objective: The objective of this study was to assess the impact of actions, including the package insert revision in April 2007, to encourage periodic UCG.
Methods: Data on monthly claims (January 2005-October 2008) covering 330 000 patients were obtained from a Japanese database vendor. We selected patients ≥40 years of age with Parkinson’s disease. The impact of the regulatory action on the proportion of patients with Parkinson’s disease prescribed cabergoline or pergolide was assessed by segmented regression analysis and by a statistical model of the rates of UCG examination in patients taking/ not taking cabergoline or pergolide before and after the action. We also compared the use of cabergoline and pergolide before and after the action with that of other antiparkinson drugs.
Results: Of 574 patients with Parkinson’s disease, the proportion of patients prescribed cabergoline or pergolide did not decrease but rather tended to increase after the action when analysed by segmented regression analysis (p = 0.13). Similarly, the proportion of the prevalent and incident users of cabergoline or pergolide did not change between two 19-month periods before and after the action. The adjusted rates of UCG examination per personyear before and after the action were both 0.02 in those not prescribed cabergoline or pergolide, but 0.02 before the action and 0.09 after the action in those taking either drug. The excess UCG examination rate of cabergoline or pergolide attributable to the action was 0.08 per person-year (95% CI 0.03, 0.11). While 1 of 49 (2%) patients taking cabergoline or pergolide had a UCG up to 19 months before the action, 9 of 36 (25%) patients taking cabergoline or pergolide had a UCG up to 19 months after the action. Annual sales from 2004 to 2008 were 195, 195, 170, 110 and 75 billion yen, respectively, and the number of valvulopathy events, including incompetence of aortic/mitral/ tricuspid valves and cardiac valve disease, per annual sales from 2004 to 2008 were estimated at 0.23, 0.03, 0.08, 0.25 and 0.19 per billion yen, respectively.
Conclusions: Following the actions in April 2007, no decrease in the use of cabergoline or pergolide occurred, although more patients administered the drug underwent a UCG. However, those undergoing a UCG represented onequarter of the total number prescribed cabergoline or pergolide. To mitigate the risk, additional risk management tools such as patient registration may be needed to secure careful clinical examination (including UCG examination, if necessary) for cardiac function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Parkinson’s disease, which is characterized by movement abnormalities, is one of the most common neurodegenerative disorders.[1] Symptoms of Parkinson’s disease cause disability and reduce quality of life (QOL).[2] The prevalence of Parkinson’s disease in Japan is 36–100 patients per 100000[1,3] and the registered number of patients with Hoehn & Yahr Stage 3 or higher Parkinson’s disease in the National Patients’ Registry as of 2007 is approximately 98 000.[4] Although non-pharmacological interventions are considered in early or uncomplicated Parkinson’s disease patients, when the patient experiences impairment in managing activities of daily living (ADL), most physicians start pharmacological treatment for symptomatic Parkinson’s disease to prevent ADL or QOL from further deteriorating. Levodopa, dopamine receptor agonists, monoamine oxidase isoenzyme type B (MAO-B) inhibitors or anticholinergics may be used as initial therapy.[5,6]
Use of the ergot-derived dopamine receptor agonists, specifically cabergoline or pergolide, is associated with an increased risk of cardiac valvulopathy.[7–12] It is assumed that drug activation of the serotonin 5-HT2B receptor stimulates mitogenesis of cardiac valves, and subsequent valvular heart disease occurs.[13] Effects on 5-HT2b receptors differ between dopamine receptor agonists.[14] Cabergoline and pergolide are known to be potent agonists at 5-HT2B receptors.[15]
Pergolide was withdrawn from the US market in 2007 because of the increased risk of valvular heart disease,[16] while the European Medicines Agency (EMA) required a reduction in the maximum daily dosage of cabergoline and pergolide from 6mg/day to 3mg/day in 2008. [17] In Japan, the ‘standard maintenance daily dose’ of these two drugs was around 3 mg or lower when approved (2–4 mg/day for cabergoline in 1999 and 0.75–1.25 mg/day for pergolide in 1994), and in the labelling change made in April 2007, the following were indicated: (i) “prior to starting cabergoline/pergolide, underlying valvulopathy should be checked by physical examination and ultrasonic cardiography (UCG)”; and (ii) “while the drug is administered, UCG examination should be done within 3–6 months after its initiation and the UCG examination should be repeated at least every 6–12 months thereafter. The drug must be discontinued when the valvular lesion is detected by the UCG and other examinations”.[18] In addition, efforts were made for face-to-face communication by medical representatives of drug companies with physicians in clinics and hospitals to inform them of the risk of valvulopathy associated with the use of these drugs. For cabergoline, in September 2008, the maximum daily dosage was specified as 3 mg/day. Cabergoline and pergolide remained in wide use even following the regulatory actions. For example, annual sales in the fiscal years from 2004 to 2008 were 100, 105, 100, 60 and 40 billion yen for cabergoline and 95, 90, 70, 50 and 35 billion yen for pergolide, respectively.[19,20]
To assess whether the April 2007 actions of revising the package insert following the regulatory actions, and face-to-face communication to request periodic UCG monitoring, had been effective, we compared the use of antiparkinson drugs as well as the frequency of UCG examination in patients with Parkinson’s disease before and after the administrative actions. We also evaluated the impact of the actions by before and after comparisons of the proportion of patients with Parkinson’s disease prescribed cabergoline or pergolide, as well as by the number of spontaneous reports of valvular heart disease associated with the use of these drugs.
Methods
Computerized data of monthly claims (January 2005–October 2008) covering 330000 patients were obtained from a database vendor (Japan Medical Data Center Co. Ltd, Tokyo, Japan).[21] The population covered by the vendor consisted of workers and their family members belonging to one of five health insurance unions operated by five large private firms. The data included encrypted personal identifier, age and sex of the patient, procedures, diagnosis codes according to the International Classification of Diseases, 10th revision (ICD-10), laboratory tests including UCG examinations, and name, dose and number of days of supply of prescribed and/or dispensed drugs. An encrypted personal identifier can be used to link claims data from different hospitals, clinics and pharmacies.
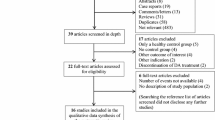
We analysed patients aged ≥40 years of age (as almost all patients with Parkinson’s disease treated with cabergoline or pergolide were 40 years of age or older) using the ICD-10 diagnosis code for Parkinson’s disease (G-20). The effects of the administrative actions (package insert revision and subsequent face-to-face communication) in April 2007 were assessed in two ways. First, the time trend of the proportion of patients with Parkinson’s disease prescribed cabergoline or pergolide was assessed by segmented regression analysis. This method of analysis has been used as a method for statistically modelling interrupted time-series data to draw more formal conclusions about the impact of an intervention on the measure of interest.[22] We plotted the proportion of patients taking and not taking cabergoline or pergolide in each month from 1 January 2005 to 31 October 2008. We investigated changes in the trend (slope) and level (intercept) for the monthly plots of the proportion of patients with Parkinson’s disease prescribed cabergoline or pergolide before (January 2005–March 2007) and after (April 2007–October 2008) the action. In the analysis, we used Proc Autoreg in SAS 9.1 (SAS Institute, Cary, NC, USA).
Furthermore, we counted the number of prevalent and incident users of the following antiparkinson drugs during two 19-month periods before (September 2005–March 2007) and after (April 2007–October 2008) the administrative actions: levodopa alone, levodopa in combination with a dopa decarboxlyase inhibitor (benserazide and carbidopa), dopamine receptor agonists (cabergoline, pergolide, pramipexole, bromocriptine, ropinirole and talipexole), anticholinergic agents (biperiden, trihexyphenidyl, profenamine, piroheptine, metixene and mazaticol), MAO-B inhibitors (selegiline), catechol-O-methyl-transferase (COMT) inhibitors (entacapone) and others (amantadine and droxidopa). The patient was counted as a prevalent user if prescribed each generic antiparkinson drug at least once at any time during the 19-month period before or after the administrative action. The patient was counted as an incident user if prescribed the drug for the first time (at least 8 months after the first claim for the individual patient). Although most patients were observed for two 19-month periods before and after the administrative action, a few were observed only before or after the action, and we estimated the difference of the prevalence and incidence of the use of each antiparkinson drug by Proc GENMOD in SAS 9.1 using generalized estimating equations (GEE) and robust variance estimators.
The UCG examination rates during one of two 19-month periods before (September 2005–March 2007) and after (April 2007–October 2008) the administrative actions in patients taking/not taking cabergoline or pergolide were estimated by the following additive model using Proc GENMOD in SAS 9.1 (equation 1):

where baseline represents the UCG rate before the action without exposure (cabergoline or pergolide) in females under 60 years of age, exposure = 0 during the period when the patient did not use cabergoline or pergolide, action = 0 before 1 April 2007, interaction represents the interaction between exposure and action, old age = 0 if the patient was under 60 years of age and male = 0 if the patient was female. We divided the study period (September 2005–October 2008) into four categories according to whether the period was before or after the administrative action as well as whether or not the patient used cabergoline or pergolide. Only the first UCG examination was counted per period per patient. Where a patient received two or more prescriptions for the drug during the study period, the use of the drug was considered to be continuous if a prescription of the drug was issued within the interval not exceeding 1.4 times the number of days of supply after the preceding prescription. The patient was considered to be drug-exposed during the period starting from the date of the first prescription of cabergoline or pergolide to the date of the last prescription plus the days of supply. Being different from the usual exposure-outcome relationship, the UCG examination can be ‘caused’ by the exposure that follows the examination. We considered the UCG examination to be associated with the use of the drug if conducted during the period of exposure or within 15, 30 and 60 days before the initiation or within 30, 60 and 90 days after discontinuation of the drug. The time ‘at risk’ of UCG examination associated with the use/non-use of the drug for four categories was calculated as the total exposed/non-exposed periods under each of the four categories if the patient had no UCG examination. Otherwise, the time ‘at risk’ was calculated as the exposed/non-exposed period with which the UCG examination was associated plus all the periods under the same category preceding the examination. Because the UCG was counted, at most, four times during the study period for patients who had a UCG examination two or more times, we used GEE and robust variance estimators.
Information on spontaneous reports (number of drug-adverse drug reaction pairs) of valvular heart disease for cabergoline or pergolide from 2006 to 2008 was obtained from the Internet pages of the Japanese Pharmaceuticals and Medical Devices Agency (PMDA).[23] We also calculated the number of spontaneous reports on valvulopathy events per annual sales.
The data provided by a database vendor were anonymized and only the encrypted identifiers were available. According to current ethical standards in Japan, such data are not subject to review by the ethical committee.
Results
The database included 996 patients, of whom 574 were aged ≥40 years with an ICD-10 diagnosis code of Parkinson’s disease. Of these 574, the median age at enrolment was 56 years (range 40–93), 237 (41%) were male and the average follow-up period was 34.1 months. During the study period (January 2005–October 2008), 76 (13%) of 574 patients had one or more UCG examinations, while during two 19-month periods before and after the administrative action (September 2005–October 2008), 62 (11%) of 553 patients with an ICD-10 diagnosis code of Parkinson’s disease had one or more UCG examinations. Of these 62 (including 10 prescribed cabergoline/ pergolide), 7 (1 prescribed cabergoline/pergolide) already had an ICD-10 diagnosis code for valvulopathy, when they first appeared in the database. Also, of the remaining 55 (9), 3 (0) and 1 (1) already had an ICD-10 diagnosis code for ischaemic heart disease and heart failure, respectively, when they first appeared in the database. When the observation period was divided into four categories according to whether the period was before or after the action and whether the period was associated with the exposure to cabergoline or pergolide (the period from 30 days before the patient started either drug until 60 days after the patient stopped the drug), 1 UCG examination was conducted ‘before/ exposed’, 9 were conducted ‘after/exposed’, 32 were conducted ‘before/non-exposed’ and 27 were conducted ‘after/non-exposed’. In the sensitivity analyses where the UCG examination was considered to be associated with the exposure when conducted within 15 or 60 days preceding the exposure period or when conducted within 30 or 90 days after the exposure period, the number of UCG examinations conducted during four categories of time periods remained the same. A total of seven patients with no period exposed to cabergoline or pergolide underwent the UCG both before and after the administrative action; otherwise, the UCG examination was conducted only once per patient.
Table I shows the number and demographics of patients, median (range) daily dose (mg) of cabergoline and pergolide, number of UCG examinations, number of person-years and crude UCG examination rate in four categories of periods subdivided into whether the period was before or after the administrative action and whether or not the patient used cabergoline or pergolide. The crude UCG examination rate in those not taking cabergoline or pergolide before the administrative action (0.05 per person-years) was the same as that after the action (0.05 per person-years). On the other hand, in those taking cabergoline or pergolide, the crude rate after the action (0.26 per person-years) was higher than that before the action (0.03 per person-years). During the period after the administrative action, the crude rate was only 9 (25%) of 36 patients who had a UCG associated with exposure to cabergoline or pergolide.
In figure 1, the monthly plots of the proportion of patients taking cabergoline or pergolide, and the regression line estimated by segmented regression analysis during the period from January 2005 to October 2008 are shown. Although the slope of the regression line before the action was slightly downward (slope = −0.0004/month), it became upward after the action (slope = 0.0006/ month) [p = 0.13]. Immediately after the action, the proportion per year showed a non-significant abrupt drop by −0.0001/month (p = 0.76). In summary, regression analysis revealed no negative impact on the monthly plots of the proportion of patients with Parkinson’s disease prescribed cabergoline or pergolide.
Table II shows the distribution of the prevalent and incident users of antiparkinson drugs in patients with Parkinson’s disease during the two 19-month periods before and after the action. The numbers of patients with no antiparkinson drugs in each period before and after the action were 175 and 170, respectively. Being somewhat different from the monthly plots (figure 1), a nonsignificant decrease of the prevalence and incidence of the use of cabergoline or pergolide was observed after the action. About one-fourth (11/39 for cabergoline and 3/13 for pergolide) and one-fifth (6/26 for cabergoline and 2/10 for pergolide) were new users who started cabergoline or pergolide for the first time before and after the action, respectively. The prevalence and incidence of the use of other antiparkinson drugs were, in general, stable, although the prevalence and incidence of ropinirole and pramipexole increased, while the incidence of biperiden and trihexyphenidyl decreased when compared before and after the action.
Table III shows the rates of UCG examination before and after the action adjusted for age and sex. The adjusted rates of UCG per person-year before and after the action were both 0.02 in females who were younger (<60 years of age) not taking cabergoline or pergolide, but 0.02 before the action and 0.09 after the action in those taking cabergoline or pergolide. The interaction between cabergoline or pergolide and the administrative actions (representing the excess UCG examination rate specifically observed in patients taking cabergoline or pergolide attributable to the impact of the administrative action) was 0.08 per personyear (95% CI 0.03, 0.11).
The annual numbers of valvulopathy events between 2004 and 2008, including incompetence of aortic/mitral/tricuspid valves and cardiac valve disease associated with cabergoline and pergolide use in spontaneous reports, were 44, 6, 14, 28 and 14, respectively. Annual sales from 2004 to 2008 were 195, 195, 170, 110 and 75 billion yen, respectively, and the number of valvulopathy events per annual sales from 2004 to 2008 were estimated as 0.23, 0.03, 0.08, 0.25 and 0.19 per billion yen, respectively.[19,20]
Discussion
Segmented regression analysis revealed that the administrative actions had no impact on the monthly plots of the proportion of patients with Parkinson’s disease prescribed cabergoline or pergolide. Although comparison of the proportion of prevalent and incident users of cabergoline and pergolide during two 19-month periods across the action demonstrated non-significant decrease, the data also indicated that about onefifth of users of those drugs were new users even after the administrative action. This may indicate that the administrative action was not very effective in discouraging physicians to prescribe these drugs for new patients. The impact of regulatory actions such as the boxed warning on the label and the ‘Dear Health Care Professional’ letter has been controversial. For example, Smalley et al.[24] reported that the label change for cisapride was ineffective, whereas Guo et al.[25] concluded that the same action for cisapride had a downward impact on its use. It may be difficult to evaluate the effect of an administrative action solely by the change in the proportion of patients prescribed a specific drug.
In the current study, the impact on the rate of UCG examination may be more important as the UCG examination is more relevant for detection and prevention of valvulopathies in patients taking cabergoline or pergolide. Our results suggest that the increase in the rate of UCG examinations in patients taking cabergoline or pergolide after the action may be attributed to the administrative action itself. Nevertheless, the fraction of patients undergoing UCG examinations was just one-quarter of those taking the drug, and was lower than that expected from the labelling revision in April 2007 requiring UCG examinations to be conducted periodically prior to and during the treatment period for all patients taking cabergoline or pergolide.
There can be some arguments against the requirements in the package insert of cabergoline or pergolide for periodic UCG examinations in all patients. From a clinical viewpoint, careful periodic physical examination may be enough for patients with no signs suggesting cardiac valvulopathies, while the high cost of medical fees for a UCG examination increases the self-pay and can be a burden for patients. Some authors suggested that careful clinical examination may be sensitive enough to suspect the presence of severe valve disease and therefore cost effective over UCG.[26] In addition, as the dose for withdrawn pergolide in US was higher than that in Japan, the risk of valvulopathies may be low, as suggested by Bhattacharyya et al.[13] As in the studies on Japanese patients,[10,11] the daily dose of pergolide in our study was relatively low (table I), although pergolide may have the risk of valvulopathies, even if used at low/usual dose.[10,11,27,28] When taking these uncertainties into account, the labelling change requiring the periodic UCG examination in all patients may not be considered evidence-based.
The annual number of domestic spontaneous reports on valvulopathy events for patients taking cabergoline or pergolide from 2006 to 2008 was approximately constant. As the number of cases in voluntary reporting systems is a function of many factors,[29] such as underreporting, type of event and time, interpretation should be prudent. For example, the increase in number may indicate either of the following scenarios: (i) the physician is more willing to report the events, potentially because the administrative action provoked an interest in the reaction; (ii) old cases so far unrecognized have been diagnosed; or (iii) new cases are still emerging. Nevertheless, the observation that the number of domestic spontaneous reports of valvulopathy remained the same from 2006 to 2008 should be regarded as an alert. Another concern is the observation that the decrease in total sales of cabergoline or pergolide has been modest after the administrative actions. The annual sales of cabergoline or pergolide in Japan in 2007 and 2008 (110 and 75 billion yen, respectively) were about half of those between 2005 and 2006 (195 and 170 billion yen, respectively).[19,20]
This study has several limitations. First, our results might apply to a specific patient population covered by the private healthcare insurance unions for those working in large private firms, although this does not necessarily mean that physicians were special as, under the Japanese healthcare plan, all patients can visit any hospital/ clinic at the same cost irrespective of the type of health insurance. Second, it was not possible to establish the results of the UCG examinations because the personal identifier was encrypted and we could not evaluate the original data. Although the diagnosis code for valvulopathy and other cardiac diseases is available in our data, such a code is often used to ensure reimbursement for the UCG examination and is therefore not reliable. In addition, as we had no data prior to January 2005 it was difficult to control for cardiac conditions at baseline, although some diagnostic codes given when the patient appeared in the database for the first time were available. Third, no data on enrolment and turnover of health insurance status were available for this specific study (although the relevant data will be available from the database vendor in the near future) while new hire and lay-off might affect the longitudinal tracking of patients with Parkinson’s disease. However, the average follow-up period was 34.1 months in 574 patients with Parkinson’s disease during the 46-month period between January 2005 and October 2008, indicating that our study population with Parkinson’s disease was relatively stable. Fourth, we measured the rate of UCG examination in prevalent but not incident users of cabergoline or pergolide, although what was requested in the package insert was periodic UCG examination irrespective of when the patient started the drug. Taking these limitations into account, we also examined the information obtained from other data sources, such as the statistics of annual sales and the number of annual domestic spontaneous reports.
As in the recent study by Zanettini et al.,[30] the risk of valvulopathy may increase in parallel with the duration of exposure to ergots. This finding suggests the need for continuing monitoring of patients, including those who had started cabergoline or pergolide some years ago. At the same time, the requirement of the periodic UCG examination for all the patients does not seem to be evidence-based. It may be worth introducing a scheme to obtain the information that may be useful in determining the most appropriate way of risk minimization, such as patient registration, which may work by itself as an additional risk minimization tool to secure careful clinical examination, including UCG for cardiac function of patients treated with cabergoline or pergolide.
Conclusions
Following the administrative actions in April 2007, no decrease in the use of cabergoline or pergolide occurred, although more patients prescribed cabergoline or pergolide underwent UCG after the action. However, those undergoing UCG examination were only one-quarter of patients taking cabergoline or pergolide. Some scheme may be needed to determine the best way for risk minimization to secure the clinical examination (including UCG examination, if necessary) and prevent deterioration of cardiac function of patients.
References
Muangpaisan W, Hori H, Brayne C. Systematic review of the prevalence and incidence of parkinson’s disease in Asia. J Epidemiol 2009; 19: 281–93
von Campenhausen S, Bornschein B, Wick R, et al. Prevalence and incidence of parkinson’s disease in Europe. Eur Neuropsychopharmacol 2005; 15: 473–90
Morikawa F, Tashiro K, Itoh K, et al. Prevalence of parkinson’s disease in Hokkaido, the northernmost island of Japan. Intern Med 1996; 35: 276–9
MHLW. Statistics of specific diseases [in Japanese; online]. Available from URL: http://www.mhlw.go.jp/toukei/saikin/hw/eisei/08/dl/data_007.pdf [Accessed 2010 Jun 26]
Olanow CW, Watts RL, Koller WC. An algorithm (decision tree) for the management of parkinson’s disease (2001): treatment guideline. Neurology 2001; 56: 1–88
Horstink M, Tolosa E, Bonuccelli U, et al. Review of the therapeutic management of parkinson’s disease. Report of a joint task force of the European Federation of Neurological Societies and the Movement Disorder Society-European Section. Part I: early (uncomplicated) parkinson’s disease. Eur J Neurol 2006; 13: 1170–85
Pritchett AM, Morrison JF, Edwards WD, et al. Valvular heart disease in patients taking pergolide. Mayo Clin Proc 2002; 77: 1280–6
Zanettini R, Antonini A, Gatto G, et al. Valvular heart disease and the use of dopamine agonists for parkinson’s disease. N Engl J Med 2007; 356: 39–46
Corvol JC, Anzouan-Kacou JB, Fauveau E, et al. Heart valve regurgitation, pergolide use, and parkinson disease. Arch Neurol 2007; 64: 1721–6
Yamamoto M, Uesugi T, Nakayama T. Dopamine agonists and cardiac valvulopathy in parkinson disease: a casecontrol study. Neurology 2006; 67: 1225–9
Yamashiro K, Komine-Kobayashi M, Hatano T, et al. The frequency of cardiac valvular regurgitation in Parkinson’s disease. Mov Disord 2008; 23: 935–41
Schade R, Andersohn F, Suissa S, et al. Dopamine agonists and the risk of cardiac-valve regurgitation. N Engl J Med 2007; 356: 29–38
Bhattacharyya S, Schapira AH, Mikhailidis DP, et al. Drug-induced fibrotic valvular heart disease. Lancet 2009; 374: 577–85
Millan MJ, Maiofiss L, Cussac D, et al. Differential actions of antiparkinson agents at multiple classes of monoamin-ergic receptor: I. A multivariate analysis of the binding profiles of 14 drugs at 21 native and cloned human receptor subtypes. J Pharmacol Exp Ther 2002; 303: 791–804
Jähnichen S, Horowski R, Pertz HH. Agonism at 5-HT2B receptors is not a class effect of the ergolines. Eur J Pharmacol 2005; 513: 225–8
US FDA. Withdrawal of parkinson’s treatment: pergolide [online]. Available from URL: http://www.fda.gov/ForConsumers/ConsumerUpdates/ucm048819.htm [Accessed 2010 Jun 26]
EMEA. Questions and answers on the review of ergotderived dopamine agonists [online]. Available from URL: http://www.ema.europa.eu/docs/en_GB/document_library/Referrals_document/Ergot_derived_dopamine_agonists_31/WC500011445.pdf [Accessed 2011 Jan 12]
PMDA. Revision of label [in Japanese; online]. Available from URL: http://www.info.pmda.go.jp/kaitei/kaitei20070419.html#1 [Accessed 2010 Jun 26]
Anonymous. Yakuji handbook 2006 [in Japanese]. Tokyo: Jiho, 2006
Anonymous. Yakuji handbook 2010 [in Japanese]. Tokyo: Jiho, 2010
Kimura S, Sato T, Ikeda S, et al. Development of a database of health insurance claims: standardization of disease classifications and anonymous record linkage. J Epidemiol 2010; 20: 413–9
Wagner AK, Soumerai SB, Zhang F, et al. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther 2002; 27: 299–309
PMDA. On the data of spontaneous reports [in Japanese; online]. Available from URL: http://www.info.pmda.go.jp/fsearchnew/jsp/menu_fukusayou_base.jsp [Accessed 2010 Jun 26]
Smalley W, Shatin D, Wysowski DK, et al. Contraindicated use of cisapride: impact of Food and Drug Administration regulatory action. JAMA 2000; 284: 3036–9
Guo JJ, Curkendall S, Jones JK, et al. Impact of cisapride label changes on codispensing of contraindicated medications. Pharmacoepidemiol Drug Saf 2003; 12: 295–301
Lung B, Gohlke-Bärwolf C, Tornos P, et al. Recommendations on the management of the asymptomatic patient with valvular heart disease. Eur Heart J 2002; 23: 1253–66
Kim JY, Chung EJ, Park SW, et al. Valvular heart disease in parkinson’s disease treated with ergot derivative dopamine agonists. Mov Disord 2006; 213: 1261–4
Waller EA, Kaplan J, Heckman MG. Valvular heart disease in patients taking pergolide. Mayo Clin Proc 2005; 80: 1016–20
Hazell L, Shakir SAW. Under-reporting of adverse drug reactions. Drug Saf 2006; 29: 385–96
Zanettini R, Antonini A, Gatto G, et al. Regression of cardiac valvulopathy related to ergot-derived dopamine agonists. Cardiovasc Ther. Epub 2010 Jun 11
Acknowledgements
No sources of funding were used to prepare this manuscript or conduct this study. The authors have no conflicts of interest to declare that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ooba, N., Yamaguchi, T. & Kubota, K. The Impact in Japan of Regulatory Action on Prescribing of Dopamine Receptor Agonists. Drug-Safety 34, 329–338 (2011). https://doi.org/10.2165/11588230-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11588230-000000000-00000