Abstract
Purpose
Some studies have suggested a potential risk of heart failure in patients with Parkinson’s disease receiving dopamine (DA) agonists. However, the results are conflicting. We used VigiBase®, the World Health Organization (WHO) Global Individual Case Safety Reports (ICSRs) database, to investigate a potential signal strengthening of heart failure with DA agonists in Parkinsonian patients older than 45 years.
Methods
A case/non-case (disproportionality) analysis was performed in Vigibase® using ICSRs registered between 1978 and May 2016. The signal of disproportionality was calculated using reporting odds ratios (ROR). In our study, 154 ICSRs of heart failure occurring in 154 Parkinsonian patients (mean age 69.6 years, 51 % women) treated with DA agonists were included.
Results and conclusion
There was a significant signal between occurrence of heart failure and exposure to pergolide or cabergoline in particular and ergot derivatives in general. In contrast, none signal was found for rotigotine, pramipexole, apomorphine, or ropinirole in particular and non-ergot derivatives in general. The present study underlines the importance to prescribe as DA agonists in Parkinsonian patients only non-ergot derivatives, excluding ergot drugs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several studies have recently discussed a putative association between exposure to some dopamine (DA) agonists and occurrence of heart failure in patients with Parkinson’s disease [1, 2]. According to the different methods used (clinical trials, meta-analyses, or case-control studies) and definition of studied outcomes, results are conflicting. Thus, other approaches are expected.
As evidence remains unclear, we performed a pharmacoepidemiological study using the case/non-case approach to strength a putative signal about heart failure signals with DA agonists. This validated method measures disproportionality of combination between a drug and a particular adverse drug reaction (ADR) in a pharmacovigilance database [3–5]. We used Vigibase®, the World Health Organization (WHO) Global Individual Case Safety Report (ICSR) database.
Methods
Data source
VigiBase® registers ICSRs (ADRs) received on a continuous basis from more than 120 member countries. It is one of the largest and representative databases, developed and maintained by the Uppsala Monitoring Center on behalf of WHO. VigiBase® is a computerized pharmacovigilance system, in which information is recorded in a structured, hierarchical form to allow for easy and flexible retrieval and analysis of the data [6]. By May 2016, over 13 million reports were registered in the database.
Data analysis
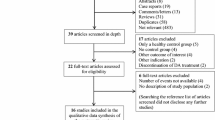
The case/non-case approach measures disproportionality of combination between a drug and a particular ADR in a pharmacovigilance database [3–5]. In the present study, heart failure cases were defined according to the validated Standardized MedDRA (Medical Dictionary for Regulatory Activities for multilingual European DOI Registration Agency) Queries (SMQs) terms “Cardiac failure SMQs”. SMQs are validated, pre-determined sets of MedDRA terms grouped together after extensive review, testing, analysis, and expert discussion [7]. In our analysis, we did not include drug doses, since they are not exhaustively recorded in reports. We included ICSRs whatever the country of origin and only ICSRs with both age and sex known, excluding other ICSRs. We only included ICSRs in patients ≥45 years with idiopathic Parkinson’s disease, excluding, after careful review of all ICSRs, patients with restless leg syndrome, hyperprolactinemia, or other related endocrinological indications of DA agonists. Drug exposition was identified according to Anatomical Therapeutic and Clinical (ATC) classification by the presence in the report of at least one DA agonist (code ATC: N04 BC) defined as “suspected” [8] and whatever the level of causality assessment [9]. DA agonists included were bromocriptine, pergolide and cabergoline (ergot derivatives), rotigotine, piribedil, pramipexole, ropinirole, and apomorphine (non-ergot drugs). Other DA agonists found in Vigibase® (sumanirole, dihydroergotamine, mesulergine, pardoprunox, talipexole, terguride) were not included since they were not marketed or are only used in few countries. Moreover, the number of ICSRs with these six drugs was too small to perform any analysis. Finally, cases included ICSRs with Parkinson’s disease and heart failure plus exposure to the eight DA agonists of interest recorded between 1978 (start of Vigibase®) and the 26th May 2016. Non-cases were defined as all other ICSRs reports (i.e., all other ADR reports with all other drugs) registered between the same period in Vigibase®.
Statistical analysis
For the case/non-case analysis, reporting odds ratios (RORs) were calculated with their 95% confidence interval (95%CI) as crude RORs [4, 5]. The eight DA agonists of interest were subsequently divided into ergot and non-ergot derivatives, as indicated above. All analyses were performed using SAS software, version 9.4 (SAS Institute. Inc., Cary. NC, USA). Statistical significance was defined as a p threshold of 0.05 (Fig. 1).
Results
Among the 5,785,629 ICSRs (with both age and sex known), 16,897 (0.29 %) involved the 8 DA agonists and 154 were registered as heart failure in Parkinsonian patients receiving a DA agonist. Mean age of the 154 patients was 69.6 ± 9.7 (range 48–89) years with 51.3 % women. The total number of DA agonists received by the 154 patients was 159 since 5 patients received 2 DA agonists: 3 were treated with cabergoline + ropinirole, 1 with pergolide + pramipexole, and 1 with bromocriptine + piribedil.
A signal between DA agonist exposure and occurrence of heart failure was found with pergolide [ROR = 4.66 (3.72–5.58), p < 0.0001] or cabergoline [ROR = 3.72 (2.76–5.02), p < 0.0001], but not with bromocriptine [ROR = 0.47 (0.24–0.90)], rotigotine [ROR = 0.37 (0.19–0.72)], piribedil [ROR = 0.37 (0.12–1.16)], pramipexole [ROR = 0.97 (0.75–1.26)], ropinirole [ROR = 0.54 (0.39–0.76)], or apomorphine [ROR = 0.67 (0.37–1.22)].
The disproportionality analysis found also a signal with ergot derivatives in general [ROR = 2.78 (2.33–3.30), p < 0.0001], but not with non-ergot DA agonists [ROR = 0.68 (0.56–0.81)] or DA agonists in general (both ergot and non-ergot) [ROR = 1.15 (1.02–1.31)].
Discussion
The present study investigates in a pharmacovigilance database a putative signal strengthening of heart failure in Parkinsonian patients treated by DA agonists. For this purpose, we used a disproportionality analysis, a methodology never used in this field. In fact, this is the first case of application of the disproportionality analysis to the assessment of ADRs in Parkinson’s disease patients. A signal was found with pergolide or cabergoline (two ergot derivatives) but not with other DA agonists.
Papers investigating this ADR in the literature are very conflicting, and none conclusion can be made from the present literature. The first signal came from clinical trials with pramipexole [10] although a meta-analysis of 27 randomized controlled trials failed to find any signal for non-ergot DA drugs [2]. Data from observational studies are also confusing. First, some associations were described. Mokles observed a statistical association with pramipexole but not with ergot DA agonists in a case-control study nested within a cohort of Parkinson’s disease patients who were new users of dopaminergic (levodopa or DA agonist) drugs [10]. Trifiro found in a multi-country, nested case-control study a risk of cardiac valve regurgitation with ergot DA drugs in Parkinson’s disease but not in hyperprolactinemia [11], thus suggesting the importance of drug dosage, a point that it was not possible to investigate in the present paper. Renoux described in the UK General Practice Research Database (GPRD) an association with the current use of any DA agonist, especially pramipexole or cabergoline after a nested case-control approach [12]. Second, other observational studies failed to find any association. A nested case-control study performed in Taiwan concluded to a non-significant increased risk with DA agonists, including pramipexole, in parkinsonian patients [13]. Finally, a systematic review of observational studies concluded to a strong evidence of cardiac valve regurgitation risk with pergolide or cabergoline and a moderate one of heart failure risk with pramipexole and cabergoline [14]. These confusing conclusions according to the studies and/or the methods used led us to perform the present pharmacoepidemiological study.
In our study, the most interesting result is the difference found according to the chemical structures of DA agonists with a signal for ergot but not for non-ergot drugs. Among the ergot derivatives, a significant result was found for pergolide or cabergoline. No definite conclusion can be made for bromocriptine due to the too small number of ICSRs (n = 9). Among the non-ergot DA agonists, none signal was found for rotigotine, ropinirole, pramipexole, or apomorphine. None conclusion can be draw for piribedil because of too few reported ICSRs (n = 3). It is interesting to compare our conclusions with a recent systematic review of observational studies that concluded to a strong evidence for a high risk of cardiovascular valve regurgitation with pergolide or cabergoline, two ergot DA agonists, and a moderate evidence of heart failure for pramipexole, a non-ergot derivative, or cabergoline [14]. We were unable to confirm for pramipexole. We also add data for rotigotine, a recently marketed drug.
The difference we found between ergot and non-ergot drugs can help to discuss the putative pharmacodynamic mechanisms of this serious ADR. Ergot (but not non-ergot) DA agonists are known to be potent agonists of cardiac 5HT2B receptors, the stimulation of which inducing activation of fibroblasts and then pulmonary arterial hypertension and/or valvular damage, thus leading to heart failure [15–17]. However, our study does not allow excluding other mechanisms to explain these cases of heart failure. It was not the purpose of this study to investigate the mechanism of this ADR but only to discuss a signal strengthening.
The present study has several strengths. First, it was performed in VigiBase®, one of the largest pharmacovigilance data resources, which provides a sufficient statistical power for a disproportionality analysis to highlight signals [18]. The methodology used in the present work is able to detect signals for relatively rare ADRs [3–5]. Second, our work investigates an ADR occurring in the whole world, especially involving different clinical contexts and medical cultures.
However, some mandatory limitations should also be discussed. First, the completeness of the data in the WHO Global ICSR database is not always guaranteed, and we had to deal with some missing data, in particular for indications. Thus, after careful review of the ICSRs, we only selected patients registered with a clear diagnosis of idiopathic Parkinson’s disease. Other patients were excluded. Second, the present work mandatory suffers, like every pharmacovigilance study, from underreporting [19], which does not allow calculating the true incidence of the ADR. However, the magnitude of underreporting does not affect the results in this kind of study [3–5], and it was not the goal of the present study to calculate the true incidence or to describe exhaustively all cases of heart failure occurring with DA agonists but to investigate a putative signal strengthening using a validated method. Finally, it is necessary to underline that, in this kind of study, ROR investigates a risk of ADR spontaneous notification and not, stricto sensu, the risk of heart failure occurrence. Thus, as indicated above, in fact, our study was performed to evaluate a signal strengthening rather than a true risk.
In conclusion, the present study, performed in the context of real world, shows for the first time a clear difference according to the chemical structure of DA agonists, since exposure to ergot DA agonists (and especially pergolide or cabergoline) was associated in Parkinsonian patients to a signal strengthening of heart failure in contrast to non-ergot drugs. From a practical point of view, it underlines the importance to prescribe as DA agonists in Parkinsonian patients only non-ergot DA agonists, excluding ergot derivatives.
References
Perez-Lloret S, Rey MV, Crispo J, Krewski D, Lapeyre-Mestre M, Montastruc JL, Rascol O (2014) Risk of heart failure following treatment with dopamine agonists in Parkinson's disease patients. Expert Opin Drug Saf 13:351–360
De Vecchis R, Cantatrione C, Mazzei D, Baldi C, Di Maio M (2016) Non-ergot dopamine agonists do not increase the risk of heart failure in Parkinson’s disease patients: a meta-analysis of randomized controlled trials. J Clin Med Res 8:449–460
Faillie JL, Montastruc F, Montastruc JL, Pariente A (2016) Pharmacoepidemiology and its input to pharmacovigilance. Therapie 7:211–216
Egberts AC, Meyboom RH, van Puijenbroek EP (2002) Use of measures of disproportionality in pharmacovigilance: three Dutch examples. Drug Saf 25:45–458
Montastruc JL, Sommet A, Bagheri H, Lapeyre-Mestre M (2011) Benefits and strengths of the disproportionality analysis for identification of adverse drug reactions in a pharmacovigilance database. Br J Clin Pharmacol 72:905–908
Bate A, Lindquist M, Edwards IR (2008) The application of knowledge discovery in databases to post-marketing drug safety: example of the WHO database. Fundam Clin Pharmacol 22:127–140
Brown EG, Wood L, Wood S (1999) The medical dictionary for regulatory activities (MedDRA). Drug Saf 20:109–117
Edwards IR, Aronson JK (2000) Adverse drug reactions: definitions, diagnosis, and management. Lancet 356:1255–1259
Miremont-Salamé G, Théophile H, Haramburu F, Bégaud B (2016) Causality assessment in pharmacovigilance: the French method and its successive updates. Therapie 71:179–186
Mokhles MM, Trifirò G, Dieleman JP, Haag MD, van Soest EM, Verhamme KM, Mazzaglia G, Herings R, Cd L, Ross D, Brusselle G, Colao A, Haverkamp W, Schade R, Gv C, Zanettini R, Sturkenboom MC (2012) The risk of new onset heart failure associated with dopamine agonist use in Parkinson’s disease. Pharmacol Res 65:358–364
Trifirò G, Mokhles MM, Dieleman JP, van Soest EM, Verhamme K, Mazzaglia G, Herings R, de Luise C, Ross D, Brusselle G, Colao A, Haverkamp W, Schade R, van Camp G, Zanettini R, Sturkenboom MC (2012) Risk of cardiac valve regurgitation with dopamine agonist use in Parkinson’s disease and hyperprolactinaemia: a multi-country, nested case-control study. Drug Saf 35:159–171
Renoux C, Dell'Aniello S, Brophy JM, Suissa S (2012) Dopamine agonist use and the risk of heart failure. Pharmacoepidemiol Drug Saf 21:34–41
Hsieh PH, Hsiao FY (2013) Risk of heart failure associated with dopamine agonists: a nested case-control study. Drugs Aging 30:739–745
Tran T, Brophy JM, Suissa S, Renoux C (2015) Risks of cardiac valve regurgitation and heart failure associated with ergot- and non-ergot-derived dopamine agonist use in patients with Parkinson’s disease: a systematic review of observational studies. CNS Drugs 29:985–998
Roth BL (2007) Drugs and valvular heart disease. N Engl J Med 356:6–9
Bondon-Guitton E, Prevot G, Didier A, Montastruc JL (2011) Pulmonary arterial hypertension and benfluorex: 5 case reports. Therapie 66:135–138
Weill A, Païta M, Tuppin P, Fagot JP, Neuman A, Simon D, Ricordeau P, Montastruc JL, Allemand H (2010) Benfluorex and valvular heart disease: a cohort study of a million people with diabetes mellitus. Pharmacoepidemiol Drug Saf 19:1256–1262
Lindquist M, Edwards IR (2001) The WHO Programme for International Drug Monitoring, its database, and the technical support of the Uppsala Monitoring Center. J Rheumatol 28:1180–1187
Bégaud B, Martin K, Haramburu F, Moore N (2002) Rates of spontaneous reporting of adverse drug reactions in France. JAMA 288:1588
Acknowledgments
The authors would like to thank the Uppsala Monitoring Centre (UMC) which provided and gave permission to use the data analyzed in the present study. The authors are indebted to the National Pharmacovigilance Centers that contributed data. The opinions and conclusions in this study are not necessarily those of the various centers or of the WHO.
Authors’ contributions
Francois Montastruc, Olivier Rascol, and Jean-Louis Montastruc planned the study and performed analysis and interpretation of the data. Francois Montastruc and Jean-Louis Montastruc wrote the manuscript. Melanie Araujo performed the statistical analysis. Leila Chebane performed acquisition of the data. All authors critically revised the text and approved the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
François Montastruc, Mélanie Linselle, Florence Moulis, Leila Chebane, or Jean-Louis Montastruc declares that they have no conflict of interest. Olivier Rascol who has acted as an advisor for most drug companies developing antiparkinsonian drugs and has received unrestricted scientific grants from GSK, Novartis, Boehringer-Ingelheim, Faust Pharmaceuticals, Eisai, Lundbeck, Servier, TEVA, Eutherapie, and Solvay.
Funding source
The work was performed during the university research time of the authors using the database which is available without fees in the department of the authors. There were no funding sources.
Rights and permissions
About this article
Cite this article
Montastruc, F., Moulis, F., Araujo, M. et al. Ergot and non-ergot dopamine agonists and heart failure in patients with Parkinson’s disease. Eur J Clin Pharmacol 73, 99–103 (2017). https://doi.org/10.1007/s00228-016-2142-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-016-2142-x