Abstract
Background and Objective
Pharmacokinetic drug-drug interactions (DDIs) are one of the major causes of adverse events in pharmacotherapy, and systematic prediction of the clinical relevance of DDIs is an issue of significant clinical importance. In a previous study, total exposure changes of many substrate drugs of cytochrome P450 (CYP) 3A4 caused by coadministration of inhibitor drugs were successfully predicted by using in vivo information. In order to exploit these predictions in daily pharmacotherapy, the clinical significance of the pharmacokinetic changes needs to be carefully evaluated. The aim of the present study was to construct a pharmacokinetic interaction significance classification system (PISCS) in which the clinical significance of DDIs was considered with pharmacokinetic changes in a systematic manner. Furthermore, the classifications proposed by PISCS were compared in a detailed manner with current alert classifications in the product labelling or the summary of product characteristics used in Japan, the US and the UK.
Methods
A matrix table was composed by stratifying two basic parameters of the prediction: the contribution ratio of CYP3A4 to the oral clearance of substrates (CR), and the inhibition ratio of inhibitors (IR). The total exposure increase was estimated for each cell in the table by associating CR and IR values, and the cells were categorized into nine zones according to the magnitude of the exposure increase. Then, correspondences between the DDI significance and the zones were determined for each drug group considering the observed exposure changes and the current classification in the product labelling. Substrate drugs of CYP3A4 selected from three therapeutic groups, i.e. HMG-CoA reductase inhibitors (statins), calcium-channel antagonists/blockers (CCBs) and benzodiazepines (BZPs), were analysed as representative examples. The product labelling descriptions of drugs in Japan, US and UK were obtained from the websites of each regulatory body.
Results
Among 220 combinations of drugs investigated, estimated exposure changes were more than 5-fold for 41 combinations in which ten combinations were not alerted in the product labelling at least in one country; these involved buspirone, nisoldipine and felodipine as substrates, and ketoconazole, voriconazole, telithromycin, clarithromycin and nefazodone as inhibitors. For those drug combinations, the alert classifications were anticipated as potentially inappropriate. In the current product labelling, many intercountry differences were also noted. Considering the relationships between previously observed exposure changes and the current alert classifications, the boundaries between ‘contraindication’ and ‘warning/caution’ were determined as a 7-fold exposure increase for statins and CCBs, and as a 4-fold increase for BZPs. PISCS clearly discriminated these drug combinations in accordance with the determined boundaries. Classifications by PISCS were expected to be valid even for future drugs because the classifications were made by zones, not by designating individual drugs.
Conclusion
The present analysis suggested that many current alert classifications were potentially inappropriate especially for drug combinations where pharmacokinetics had not been evaluated. It is expected that PISCS would contribute to constructing a leak-less alerting system for a broad range of pharmacokinetic DDIs. Further validation of PISCS is required in clinical studies with key drug combinations, and its extension to other CYP and metabolizing enzymes remains to be achieved.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Many patients experience excessive or impaired drug effects because of drug-drug interactions (DDIs)[1] and some drugs have even been withdrawn because of fatal adverse events,[2–5] which may have been potentiated by DDIs. Prediction of DDIs is an issue of clinical significance and has been extensively investigated in the literature by in vitro experiments.[6–10] However, these have met with limited success because of insufficient accuracy and limited applicability when used in clinical settings for dose adjustment.[2] Considering the huge number of drugs used commercially, a complete conception change will be required to allow the prediction of many DDIs occurring in daily pharmacotherapeutic situations.
Recently, a systematic method has been reported for predicting DDI-mediated total drug exposure (or the area under the plasma/serum concentration-time curve [AUC]) changes caused by inhibition or induction of cytochrome P450 (CYP) 3A4 activity.[11,12] CYP3A4 is the most abundant metabolic enzyme in the human liver and intestine and is involved in the metabolism of approximately 50% of currently available therapeutic agents.[2,13–15] CYP3A5 is another important metabolizing enzyme in the human CYP3A family, and it shares similar substrate specificities with CYP3A4.[16–18] Therefore, the contributions of CYP3A5 to most DDIs are difficult to differentiate from those of CYP3A4. Nevertheless, CYP3A5 is not completely equal to CYP3A4, and it has been reported that some inhibitors of CYP3A4 inhibit CYP3A5 significantly less potently than CYP3A4 both in vitro [19–21] and in vivo.[22]
For inhibitory DDIs, the prediction method is based on two parameters obtained from drug exposure changes derived from clinical studies in which drugs were orally coadministered with typical CYP3A4 substrates (i.e. midazolam or simvastatin) or inhibitors (i.e. ketoconazole or itraconazole).[11] Theoretically, these two parameters can be estimated from in vitro experiments. However, in these studies, the source of information was limited to in vivo studies because the accuracy of prediction has not been fully analysed when these parameters are estimated in vitro. Once the two parameters have been calculated, total exposure changes for any oral combination of drugs can be predicted. The accuracy of prediction was satisfactory and the estimated exposure increases were within a range of 0.5- to 2.0-fold of the observed increases in 62 of 65 drug combinations (95%) involving inhibition of CYP3A4.[11]
Considering the broad applicability and precision of the prediction method, it can be regarded as useful in clinical settings. However, for practical application to pharmacotherapy, the clinical significance of DDIs needs to be estimated rather than simple pharmacokinetic changes. Therefore, the aim of the present study was to develop a pharmacokinetic interaction significance classification system (PISCS), which is capable of estimating the clinical significance of DDIs by considering both pharmacokinetic changes and therapeutic aspects. It should be noted that drugs with a broad therapeutic window are less sensitive to clinically significant adverse consequences due to pharmacokinetic DDIs and vice versa. However, the therapeutic window of a drug is often difficult to characterize. Moreover, on occasion, a drug needs to be used when an alternative therapy is unavailable, even though the therapeutic window is narrow and the predicted DDI is significant. Hence, the relationships between pharmacokinetic changes and clinical significance are complicated and not apparent to many clinical personnel. For this reason, having a systematic classification of the clinical significance of DDIs based on pharmacokinetic changes is advantageous. This will aid in constructing a DDI alerting system for various risks associated with numerous pharmacotherapies used in the current market.
In 2006, the US FDA announced a draft guidance titled ‘Drug Interaction Studies — Study Design, Data Analysis, and Implications for Dosing and Labeling’.[23] In this draft guidance, inhibitors and substrates of CYP enzymes were classified according to the magnitude of the drug exposure increase caused by typical coadministered drugs. Although the proposal is effective for classification of new drug candidates, it provides no means for predicting the significance of DDI for a specific drug combination. PISCS has some similarities to the draft guidance in the classification criteria of drugs, but possesses a unique function that allows prediction of clinical significance of DDI.
In many countries, drug prescriptions are legally required to be checked for agreement with the product labelling (or the summary of product characteristics in European countries). The product labelling is developed by pharmaceutical manufacturers under the supervision of regulatory bodies. In the product labelling, a DDI is traditionally classified into one of three categories: contraindication, warning or caution, or nonalerted. In some situations, dose-adjustment recommendations are provided as a useful part of a warning label. The criteria for these alert categories are not always definitive. In this study, the classifications proposed by PISCS were compared with current alert classifications in the product labelling or the summary of product characteristics used in Japan, the US and the UK. We examined whether drug exposure changes predicted by PISCS are in agreement with information provided by the product labelling. Furthermore, the alert classifications were compared in detail among countries for many drug combinations in which a significant exposure increase was anticipated.
In the present study, the target DDIs are limited to pharmacokinetic ones caused mainly by inhibition of CYP3A4, although it is well known that a series of metabolizing enzymes and transporters other than CYP3A4 are involved in pharmacokinetic DDIs. Furthermore, the interactions with some drugs, such as protease inhibitors for treatment of HIV, were excluded because those drugs exhibited a marked potential to induce and inhibit CYP3A4 simultaneously.[24–26] In spite of these limitations, the present study is the first attempt to predict the significance of pharmacokinetic DDIs for many combinations of drugs in a systematic manner.
Methods
Prediction of Drug-Drug Interaction-Mediated Total Exposure Changes
DDI-mediated total drug exposure changes were estimated using the in vivo-based method previously described.[11] Briefly, based on pharmacokinetic considerations, it was hypothesized that total exposure changes are determined by two parameters: the apparent contribution ratio of CYP3A4 to oral clearance of the substrate drug (CRCYP3A4), and the apparent inhibition ratio of CYP3A4 caused by an inhibitor drug (IRCYP3A4).[11] The values of these two parameters were calculated from reported changes in total exposures of substrates produced by inhibitory DDIs with CYP3A4. For any DDI that results in inhibition of CYP3A4, the change in the AUC may be estimated using equation 1:[11]
Equation 1 is compatible with previous pharmacokinetic theories[6,7,10,27–29] as described below. Under assumptions of reversible inhibition and of negligible non-CYP clearance, the following equations (equations 2 and 3) are maintained for CYP3A4 where I, Ki and fm are the concentration of an inhibitor, the inhibition constant and the fraction of metabolism, respectively:
Using these relationships, equation 1 can be rewritten as equation 4, which is frequently presented in the literature of DDI research for competitive and noncompetitive inhibitions:[6,7,10,27–29]
When metabolites of a parent drug also contribute to DDI via inhibition of the CYP enzyme, the IRCYP3A4 is calculated using equation 5:
where I0 and Ki,0 are the concentration and inhibition constant of a given parent drug, I1, I2, I3..., and Ki,1, Ki,2, Ki,3... are those of metabolites, respectively. The drug exposure changes by mechanism-based inhibition were explained mathematically using a degeneration constant (kdeg), an inactivation rate constant (kinact) and inactivator potency (KI).[30,31] Equation 1 becomes equivalent to the equation reported when IRCYP3A4 is related with kdeg and with kinact as in equation 6:
Therefore, equation 1 covers various DDI situations, including reversible (competitive and noncompetitive) and irreversible (mechanism-based) inhibitions, and inhibition by metabolites.
Oral formulations for 13 substrates and 17 inhibitors of CYP3A4 were analysed in this study (tables I and II). In this study, predicted drug exposure increases were restricted to ≤25-fold considering the preciseness of the CR and IR values. Predicted exposure increases were compared with reported exposure increases in humans, which were retrieved from the PubMed database using the keywords ‘CYP3A4’, ‘drug interaction’ and ‘clinical trial’.
Classification of Substrates and Inhibitors of Cytochrome P450 3A4
To demonstrate the applicability of PISCS, substrate drugs of CYP3A4 selected from three therapeutic groups were analysed: HMG-CoA reductase inhibitors (statins), calcium-channel antagonists/blockers (CCBs) and benzodiazepines (BZPs). These groups were selected because many CYP3A4 substrates were included (table I). However, a series of clinically important drugs in these groups were excluded from the analysis because there is no contribution or only a minor contribution of CYP3A4 to their clearances. Although zolpidem is not a BZP, it was included in the BZP group in this analysis because of its therapeutic similarity to BZPs.
In the first step of the analysis, all substrates and inhibitors were stratified into six categories:
-
1.
very selective/strong (VS)
-
2.
selective/strong (S)
-
3.
slightly selective/strong (SS)
-
4.
moderate (M)
-
5.
weak (W)
-
6.
very weak (VW)
corresponding to CRCYP3A4 and IRCYP3A4 values of ≥0.9, 0.8–0.89, 0.7–0.79, 0.5–0.69, 0.3–0.49 and 0.1–0.29, respectively. ‘Very weak’ categories were introduced in a PISCS table for consistency with the prediction of inductive DDIs, which will be described in a future study. For the purpose of estimating significant drug exposure changes caused by inhibition of a single metabolizing enzyme, ‘very weak’ categories would not be informative. Next, a 6 × 6 matrix table was constructed using these categories (figure 1). The estimated average exposure increase in each cell of the matrix was calculated by the double integral of equation 1 as follows (equation 7):
where variables a and b represent boundaries for CR, and variables c and d represent boundaries for IR. S is an area defined by boundaries a, b, c and d. Lis is a polylogarithm function (equation 8):
Pharmacokinetic interaction significance classification system (PISCS) table for inhibitory oral interactions showing categories of contribution ratios (CRs), inhibition ratios (IRs) and zones according to predicted drug exposure increases. Nine zones were placed in the table by grouping the cells with similar estimated increases. Numbers in the cells are the average exposure changes calculated by equation 7. * ‘Very weak’ classifications and zones VIII and IX are not associated with significant exposure changes. See text for details. BZP = benzodiazepine; C = contraindication; CCB = calcium channel antagonist/blocker; N = nonalerted; W/U = warning/caution.
The table was divided into nine zones by grouping the cells of similar estimated average exposure increase. The final decision for grouping was made based on the profiles of the distribution of predicted increases, which were calculated as follows. The distribution of predicted drug exposure increases in each zone was simulated numerically by generating CR and IR values. In each cell in the PISCS table (figure 1), 1600 total exposure predictions were calculated with an arithmetical series of CR and IR values (40 × 40). The distribution of prediction was analysed by making a histogram with Microsoft Office Excel® 2007. Distribution curves were normalized so that the area under the curve was equivalent between zones. In the FDA draft guidance on drug interaction studies,[23] inhibitors and substrates of CYP3A were classified into three (strong, moderate and weak) and two (sensitive and nonsensitive) categories, respectively. Exposure increases of these substrates with coadministration of the inhibitor were simulated, assuming the boundaries of the inhibitors correspond to IR values of 0.87, 0.54 and 0.22, and the boundary for substrates corresponds to CR values of 0.8 and 0.3. The lower boundary of nonsensitive substrates was not specified in the guidance but determined provisionally as a CR value of 0.3, which is equal to the lower boundary of weak substrates. The boundaries for classification of the significance of a given DDI were determined for statins, CCBs and BZPs as representative examples. Theoretically, the boundaries were adjustable with regard to any pharmacological measure, such as the margin of the therapeutic window. In this study, the boundaries were determined in a more pragmatic manner, considering relationships between the observed exposure changes and the current classification of alerts in each product labelling. The boundary between areas corresponding to ‘contraindication’ and ‘warning/caution’ was defined as a total exposure increase of 7-fold for statins and CCBs and 4-fold for BZPs. These values were chosen because observed total exposure increases greater than 7-fold for statins and CCBs and 4-fold for BZPs are categorized as contraindications in many cases in the current product labelling. AUC boundaries between ‘warning/caution’ and ‘nonalerted’ were defined as 2-fold for statins and CCBs, and 1.5-fold for BZPs based on similar consideration. For statins and CCBs, zone I corresponds to contraindication and zones II–V correspond to caution (figure 1). For BZPs, zones I–II and zones III–VI correspond to contraindication and caution, respectively.
Survey of Product Labelling Descriptions of Drugs
The product labelling descriptions of drugs in Japan, the US and the UK were obtained from the website of the Japanese Pharmaceuticals and Medical Device Agency (http://www.pmda.go.jp), the FDA website (http://www.fda.gov) and the UK Electronic Medicines Compendium (http://emc.medicines.org.uk). The websites were accessed in April 2008. These descriptions of DDIs, which were categorized as contraindication, warning or caution, and nonalerted, were compared with predicted changes in AUC values. When an inconsistency existed between the alert classifications of the substrate drug and the inhibitor drug, a higher-level alert was used for analysis. If DDIs were alerted for a group of drugs with example names (e.g. azole antifungals such as ketoconazole and itraconazole), the description was interpreted as limited to the example drugs. Observed total exposure changes for DDIs were obtained from published data.[11]
Results
Implementation of the Pharmacokinetic Interaction Significance Classification System
The substrates and inhibitors of CYP3A4 analysed in this study are listed in tables I and II, respectively. Figure 1 shows the PISCS table in which substrates and inhibitors are stratified into six categories according to the CR and IR values. The table was then divided into nine zones according to the estimated drug exposure increase.
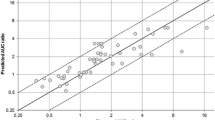
To explore the classification performance of the zones (from I to VII) in the PISCS table, the distributions of total exposure increase were carefully simulated with the arithmetical series of CR and IR values in figure 2a. The zones discriminated the magnitude of exposure increases efficiently. According to our numerical simulation presented in figure 2b, the classifications of CYP3A inhibitors and substrates made by the FDA draft guidance[23] failed to predict exposure increases quantitatively. The magnitudes of the predicted exposure increases overlapped considerably between combinations of sensitive substrate-moderate inhibitor and of nonsensitive substrate-strong inhibitor. The combination of nonsensitive substrate-strong inhibitor also overlapped with the combinations of nonsensitive substrate-moderate inhibitor and sensitive substrate-weak inhibitor.
Distributions of predicted drug exposure increase from classified inhibitors and substrates: (a) prepared according to zones in the pharmacokinetic interaction significance classification system (PISCS) table; (b) prepared according to the classification proposed by the US FDA draft guidance announced in 2006.[23] Distributions of exposure change were calculated using the arithmetical series of contribution ratio (CR) and inhibition ratio (IR) values. In panel (b) it was assumed that the sensitive and nonsensitive substrates correspond to CR ranges of 0.8–1.0 and 0.3–0.8, respectively. Likewise, the strong, moderate and weak inhibitors correspond to IR ranges of 0.87–1.0, 0.55–0.87 and 0.22–0.55, respectively. AUC = area under the plasma/serum concentration-time curve.
Relationship between Predicted Drug Exposure Increases and Alert Classifications
Figure 3 shows the predicted drug exposure increases for 220 DDIs and product labelling alert classifications in Japan, the US and the UK. In general, drug combinations with large predicted exposure increases were associated with high-level alerts in all three countries. However, there was considerable irregularity in all three countries in which the alert classification was at variance with the predicted exposure increase. For example, combinations of nisoldipine and inhibitors of CYP3A4, such as voriconazole, telithromycin, clarithromycin and erythromycin, are not alerted in the UK despite an approximately 5-fold total exposure increase of nisoldipine being estimated for these combinations. On the other hand, a combination of nisoldipine and cimetidine is alerted as a caution but this only raised the plasma exposure of nisoldipine 1.5-fold.[67] Similar irregularities were also found for the alert classifications in Japan and the US (figure 3).
Predicted drug exposure (area under the plasma/serum concentration-time curve [AUC]) increase for oral drug-drug interactions and alert classification according to product labelling in (a) Japan, (b) the US and (c) the UK. Total drug exposure increases were obtained from a previous study.[11] Inhibitors are plotted on the right axis in the order of inhibitory potency: ketoconazole (KET), voriconazole (VOR), itraconazole (ITR), telithromycin (TEL), clarithromycin (CLA), nefazodone (NEF), erythromycin (ERY), diltiazem (DIL), fluconazole (FCZ), verapamil (VER), cimetidine (CIM), ranitidine (RAN), roxithromycin (ROX), fluvoxamine (FLU), azithromycin (AZI), gatifloxacin (GAT) and fluoxetine (FLX). Doses of inhibitors are listed in table II. Substrates are plotted on the left axis in the order of susceptibility to inhibitors: lovastatin (LOV), simvastatin (SIM), buspirone (BUS), nisoldipine (NIS), triazolam (TRI), midazolam (MID), felodipine (FEL), ciclosporin (CIC), nifedipine (NIF), alprazolam (ALP), atorvastatin (ATO), telithromycin (TEL), and zolpidem (ZOL).
Among 220 combinations of various substrates and inhibitors investigated, the drug exposure was anticipated to increase more than 5-fold for 41 combinations in which ten combinations were nonalerted by the product labelling at least in one country; these involved buspirone, nisoldipine and felodipine as substrates, and ketoconazole, voriconazole, telithromycin, clarithromycin and nefazodone as inhibitors (table III). For only one of these combinations, the exposure change had been measured in humans. The number of combinations increased to 30 when a more than 3-fold total exposure increase was considered (table III).
Comparison of Product Labelling Alerts in Japan, the US and the UK
According to the prediction, drug exposures increased by more than 2-fold for 109 of 220 drug combinations. In total, 71.4% of these combinations were associated with alerts and the percentage of alerts was similar among countries (table IV). Clinically documented exposure increases were available for 40.4% (44/109) of these combinations. In all three countries, most combinations in which the observed total exposure increase was greater than 2-fold in humans were associated with product labelling alerts (94.1% in total [table IV]). In contrast, only 56.3% of combinations for which human pharmacokinetics were unavailable were accompanied by product labelling alerts (table IV).
Inconsistencies were also noted among the three countries. Of 109 combinations with a 2-fold or greater predicted total exposure increase, 49.5% of combinations involved drugs unapproved in more than one country. Only 20.2% of combinations had identical alerts in all three countries. Of the remaining 30.3%, 24.8% of combinations had warning/caution alerts in one or two countries.
Analysis of Alerts for HMG-CoA Reductase Inhibitors (Statins), Calcium Channel Antagonists/Blockers and Benzodiazepines
In figure 4, the consistency between drug exposure increases and significance classification of DDIs was compared between the current product labelling and PISCS for CYP3A4 substrate drugs categorized in statins, CCBs and BZPs. It was apparent that PISCS provided more discriminatory alerts. In table V, alert classifications of the current product labelling were compared with proposals by PISCS for azole antifungals. In the present analysis, approximately 50% of classifications by PISCS disagree with the current classifications. For instance, a combination of simvastatin is contraindicated with erythromycin in the UK, with a 6.2-fold increase in the reported AUC of simvastatin.[69] A combination of simvastatin and telithromycin is labelled as a warning in the US, with an 11-fold increase in the reported AUC of simvastatin.[52] On the other hand, PISCS suggested that simvastatin would be classified as a caution and contraindication with erythromycin and telithromycin, respectively.
Comparison of predicted area under the plasma/serum concentration-time curve (AUC) increases between current alert classification of oral drug-drug interaction (DDI) combinations (a) and proposed classification by pharmacokinetic interaction significance classification system (PISCS); (b) for HMG-CoA reductase inhibitors (statins), calcium channel antagonists/blockers (CCBs) and benzodiazepines (BZPs). Predicted AUC increases are presented with box and whisker plots for all possible drug combinations analysed in this study, and the observed AUC increases are presented with solid circles for combinations in which a clinical study has been performed. In the box and whisker plot, the top, the mid-line and the bottom of a box represent the upper quartile, the median, and the lower quartile, respectively. The bars represent the range of the values within 1.5-fold height of the box from the edge of the box. The values beyond this range are plotted individually. SPSS 15.0J for Windows (SPSS Inc., Chicago, IL, USA) was used to draw box and whisker plots. Numerals in parentheses indicate the total number of DDIs in Japan, UK and US, allowing reiteration of the same combination in different countries. C = contraindication; N = nonalerted; W/U = warning/caution.
Discussion
Alerts for DDIs can be classified according to the exposure increases because the pharmacological actions or adverse reactions to drugs that have common pharmacological or toxicological target molecules, such as receptors and enzymes, depend on the degree of occupation of the target molecules.[70–72] Other than total exposure, the maximum plasma concentration (peak exposure) and the time above a certain plasma concentration (such as the minimum inhibitory concentration) have been used as indexes of drug efficacy and toxicity. However, since the correlation between the total exposure and these parameters is generally high, it is not easy to prove the advantages of using these parameters other than the drug total exposure (AUC). Therefore, the total exposure was adopted as a representative index of drug concentrations in this study. Correlation between plasma or serum concentrations of BZPs and the incidence of adverse events, such as postural sway, have been reported.[73] For CCBs and BZPs, the severity of dizziness and other adverse events increases concomitantly with the increase in the blood concentration of the drug after coadministration of inhibitors of CYP3A4.[39,36,74] For statins, rhabdomyolysis has been associated with coadministration of CYP3A4 inhibitors.[75] These pieces of evidence support the development of DDI alerts based on predicted total exposure increases.
For many drug combinations investigated in this study, exposure was anticipated to be markedly elevated according to our prediction, yet nonalerted by the current product labelling. For most of these combinations, pharmacokinetic alternations had not been evaluated in the literature. Therefore, it is meaningful to evaluate their exposure changes in actual clinical studies. Even so, from the therapeutic standpoint, the significance of these clinical studies would not be always high, since some of these combinations include drugs that are rather old and now infrequently prescribed. For example, the alert classification of nisoldipine was at variance with the predicted total exposure increase and was inconsistent among countries (figure 3). This is probably a reflection of both insufficient DDI data and slow updates of the product labelling on nisoldipine. Concerning the disposition of nisoldipine, DDI clinical studies have only been conducted with ketoconazole and cimetidine[36,67] and our analysis suggested it is possible to classify nisoldipine as a very selective substrate of CYP3A4 from these clinical studies. Consequently, exposure changes of nisoldipine were made to be predictable for various combinations. In contrast, it should be emphasized that we could not even determine CR values of the third-generation CCBs such as amlodipine and azelnidipine, which are frequently prescribed in current pharmacotherapy. This is because of lack of appropriate in vivo DDI data on these drugs. Further DDI clinical studies are obviously required with key drug combinations, considering therapeutic needs very carefully.
PISCS would also facilitate safer pharmacotherapy of newer drugs with limited clinical information, such as the effective antifungal agent voriconazole.[76] Although its inhibition of CYP3A4 was reported to be insubstantial in an in vitro experiment as indicated by a 50% inhibitory concentration of 10.5 µmol/L,[77] in vivo data indicated that voriconazole is a strong inhibitor of CYP3A4 because the AUC of coadministered midazolam and sirolimus increased to approximately 10-fold.[53,78] In PISCS, voriconazole is classified as a very strong inhibitor of CYP3A4 comparable with ketoconazole and itraconazole (table II), and it should be prescribed with great care for use concomitantly with very selective or selective substrates of CYP3A4, such as lovastatin, simvastatin, nisoldipine or midazolam (table I). As table V shows, DDIs for voriconazole are possibly underestimated relative to DDIs for other antifungal agents of similar inhibitory activity in the current product labelling. As PISCS is a prediction-based method, it would be possible to simply overestimate the DDI potential of voriconazole, i.e. a false positive. However, caution should be exercised in using voriconazole until a series of clinical studies clearly identifies its in vivo inhibitory potential.
In this study, significant between-country differences were also revealed in DDI alert classifications of the product labelling (figure 3). Theoretically, these differences may reflect intrinsic (genetic) and extrinsic (environmental or cultural) ethnic differences. In the present analysis, however, no clear evidence was found for ethnic differences in drug responses. Rather, these differences may appear to have arisen from the heterogeneity that has resulted historically from approvals that might have been granted over a time range of several decades in each region. It is probable that the description of any product labelling was restricted by proven evidence available at the time of submission and could not refer to hypothetical theories. In the future, however, it seems reasonable to accept that proven evidence for all possible DDIs cannot be collected, as the number of substrate drugs for CYP is in the thousands. Therefore, predictive descriptions may need to be used more explicitly with regard to alerts on DDIs in the product labelling. In addition, achieving international harmonization on the criteria for alerting on DDIs could be very helpful.
Concerning the regulatory aspects of DDI at present, the FDA’s draft guidance on drug interaction studies[23] should have substantial impacts on international drug development and also on the product labelling in the world. One of the new features of the draft guidance was that the inhibitor and substrate drugs of CYP enzymes were categorized by potential of DDIs. In the draft guidance, drugs that increase the AUC of sensitive CYP3A substrates, such as midazolam, by 5-fold or higher, from 2- to 5-fold, and from 1.25- to 2-fold were defined as strong, moderate and weak CYP3A inhibitors, respectively. The basic concept of PISCS is the same as the draft guidance in that the total exposure increase of a concomitantly given selective substrate is the best index for evaluating the inhibitory potential. In fact, increases of midazolam exposure of 1.25-, 2- and 5-fold correspond to IR values of 0.22, 0.54 and 0.87. Regarding the classification of substrates of CYP3A, ‘sensitive substrate’ was defined in the draft guidance as drugs that exhibit total exposure increases of more than 5-fold with coadministration of potent inhibitors. This criterion corresponds to CR values of more than 0.8 in PISCS. In spite of these similarities, the draft guidance provides no means of quantitative prediction for exposure changes caused by a DDI. As simulated in figure 2b, the classifications proposed by the draft guidance would be insufficient to predict the magnitude of drug exposure changes caused by inhibition of CYP enzymes.
Likewise, ‘substrates with narrow therapeutic range’ were exemplified in the draft guidance as drugs that potentially cause serious safety concerns, such as torsades de pointes. This is an important factor to be considered when estimating the significance of DDIs; however, an actual procedure to incorporate the therapeutic range in the alert classification was not documented. Advantages of PISCS would be that the total exposure increases can be quantitatively predicted and, in addition, the alert classification is systematically adjustable, considering the therapeutic range and other requirements. These characteristics may contribute to constructing a leak-less alerting system.
Similar to the FDA guidance, PISCS categorized the substrate and the inhibitor drugs by explanatory names such as ‘selective inhibitor’ rather than using the CR and IR values directly (figure 1). This system would enable alerts to be more descriptive, e.g. “This drug is a selective substrate of CYP3A4 and a moderate inhibitor of CYP2D6” or “This drug is contraindicated with very strong inhibitors of CYP3A4.” It would be impractical to include the names of all relevant generic drugs or therapeutic drug groups in product labelling. An advantage of the proposed system is that such alerts would also be appropriate for future drugs. With the current method, updating the product labelling is slow and often occurs after adverse events have been experienced by patients.[79]
Interindividual variability is an issue that needs great care in any method used for predicting biological events.[80,81] In PISCS, the pharmacokinetic alternations are accounted for primarily in average fold-changes in drug exposure. The significance of any interindividual variability caused by factors such as age, sex, disease state, ethnicity and genetics needs to be considered additionally for the output of the system in some situations. In the PISCS table (figure 1), a given pharmacokinetic change is translated into clinical significance. Conceptually, interindividual variability should be accounted for in this translation. For most drugs, when selecting zones in the PISCS table, a therapeutic window might need to be regarded as narrower than it actually is when considering interindividual variability in pharmacokinetics and/or pharmacodynamics. In addition, clarifying, and if necessary, differentiating target populations of each alert is recommended to reduce potential risks associated with interindividual variability. For example, for BZPs, defining the zones for the elderly population differently from the young would be better because of the higher sensitivity of the elderly for adverse events with these drugs.[82,83]
Finally, current limitations of PISCS should be discussed from the pharmacokinetic viewpoint. Theoretically, PISCS can be applied to DDIs caused by inhibition of any hepatic metabolizing enzymes. However, use of PISCS should be limited to inhibitory DDIs of CYP3A4 at present because prediction for the total exposure changes have been validated only for CYP3A4.[79] The interactions with some drugs, such as protease inhibitors for treatment of HIV, were not predictable with the current method because those drugs exhibited a marked potential to induce and inhibit CYP3A4 simultaneously.[79] Furthermore, the current system cannot manage DDIs caused by inhibition of transporter activity. Ciclosporin is a typical inhibitor of transporters including organic anion transporting polypeptide 1B1(OATP1B1/SLCO1B1), which plays a significant role in the hepatic uptake of several statins.[84] For this reason, ciclosporin as an inhibitor was excluded from the current analysis. It should be noted that ciclosporin increased the exposure of some statins, which could not be explained by inhibition of CYP3A4.[84,85] In the future, to apply PISCS to DDIs caused by alternations in transporter activity, theoretical extensions would be necessary, since drug transport is a reversible process in principle and different from usual irreversible metabolism. Further studies are under way in our laboratory to apply PISCS to metabolizing enzymes other than CYP3A4.
Conclusion
Our analysis of current label classifications and predicted total drug exposure increases for DDIs involving CYP3A4 inhibition revealed current inconsistencies and shows that a comprehensive and quantitative framework for determining criteria for alert classifications would be plausible. The PISCS table was proposed to categorize substrates and inhibitors, and to relate pharmacokinetic changes and clinical significance of DDIs in a systematic manner. Our proposal may facilitate safer and more reliable pharmacotherapy. Further validation of PISCS is necessary from various viewpoints, and extensions to other CYP and metabolizing enzymes remain to be achieved.
References
Pirmohamed M, James S, Meakin S, et al. Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients. BMJ 2004 Jul 3; 329(7456): 15–9
Wienkers LC, Heath TG. Predicting in vivo drug interactions from in vitro drug discovery data. Nat Rev Drug Discov 2005 Oct; 4(10): 825–33
Furberg CD, Pitt B. Withdrawal of cerivastatin from the world market. Curr Control Trials Cardiovasc Med 2001; 2(5): 205–7
Estelle F, Simons R. H1-receptor antagonists: safety issues. Ann Allergy Asthma Immunol 1999 Nov; 83(5): 481–8
Huang SM GF, Rahman A, Frueh F, et al. Application of pharmacogenomics in clinical pharmacology. Toxicol Mech Methods 2006; 16(2): 89–99
Obach RS, Walsky RL, Venkatakrishnan K, et al. The utility of in vitro cytochrome P450 inhibition data in the prediction of drug-drug interactions. J Pharmacol Exp Ther 2006 Jan; 316(1): 336–48
Brown HS, Galetin A, Hallifax D, et al. Prediction of in vivo drug-drug interactions from in vitro data: factors affecting prototypic drug-drug interactions involving CYP2C9, CYP2D6 and CYP3A4. Clin Pharmacokinet 2006; 45(10): 1035–50
Brown HS, Ito K, Galetin A, et al. Prediction of in vivo drug-drug interactions from in vitro data: impact of incorporating parallel pathways of drug elimination and inhibitor absorption rate constant. Br J Clin Pharmacol 2005 Nov; 60(5): 508–18
Ito K, Brown HS, Houston JB. Database analyses for the prediction of in vivo drug-drug interactions from in vitro data. Br J Clin Pharmacol 2004 Apr; 57(4): 473–86
Ito K, Hallifax D, Obach RS, et al. Impact of parallel pathways of drug elimination and multiple cytochrome P450 involvement on drug-drug interactions: CYP2D6 paradigm. Drug Metab Dispos 2005 Jun; 33(6): 837–44
Ohno Y, Hisaka A, Suzuki H. General framework for the quantitative prediction of CYP3A4-mediated oral drug interactions based on the AUC increase by coadministration of standard drugs. Clin Pharmacokinet 2007; 46(8): 681–96
Ohno Y, Hisaka A, Ueno M, et al. General framework for the prediction of oral drug interactions caused by CYP3A4 induction from in vivo information. Clin Pharmacokinet 2008; 47(10): 669–80
Fujita K. Food-drug interactions via human cytochrome P450 3A (CYP3A). Drug Metab Drug Interact 2004; 20(4): 195–217
Guengerich FP. Cytochrome P-450 3A4: regulation and role in drug metabolism. Ann Rev Pharmacol Toxicol 1999; 39: 1–17
Wrighton SA, Stevens JC. The human hepatic cytochromes P450 involved in drug metabolism. Crit Rev Toxicol 1992; 22(1): 1–21
Liu YT, Hao HP, Liu CX, et al. Drugs as CYP3A probes, inducers, and inhibitors. Drug Metab Rev 2007; 39(4): 699–721
Williams JA, Cook J, Hurst SI. A significant drug-metabolizing role for CYP3A5? Drug Metab Dispos 2003 Dec; 31(12): 1526–30
Daly AK. Significance of the minor cytochrome P450 3A isoforms. Clin Pharmacokinet 2006; 45(1): 13–31
McConn 2nd DJ, Lin YS, Allen K, et al. Differences in the inhibition of cytochromes P450 3A4 and 3A5 by metabolite-inhibitor complex-forming drugs. Drug Metab Dispos 2004 Oct; 32(10): 1083–91
Patki KC, Von Moltke LL, Greenblatt DJ. In vitro metabolism of midazolam, triazolam, nifedipine, and testosterone by human liver microsomes and recombinant cytochromes p450: role of CYP3A4 and CYP3A5. Drug Metab Dispos 2003 Jul; 31(7): 938–44
Pearson JT, Wahlstrom JL, Dickmann LJ, et al. Differential time-dependent inactivation of P450 3A4 and P450 3A5 by raloxifene: a key role for C239 in quenching reactive intermediates. Chem Res Toxicol 2007 Dec; 20(12): 1778–86
Isoherranen N, Ludington SR, Givens RC, et al. The influence of CYP3A5 expression on the extent of hepatic CYP3A inhibition is substrate-dependent: an in vitro-in vivo evaluation. Drug Metab Dispos 2008 Jan; 36(1): 146–54
US FDA Center for Drug Evaluation and Research [CDER]. Draft guidance for industry: drug interaction studies — study design, data analysis, and implications for dosing and labelling. Rockville (MD): CDER, 2006 Sep [online]. Available from URL: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM072101.pdf [Accessed 2009 Aug 4]
Mikus G, Schowel V, Drzewinska M, et al. Potent cytochrome P450 2C19 genotype-related interaction between voriconazole and the cytochrome P450 3A4 inhibitor ritonavir. Clin Pharmacol Ther 2006 Aug; 80(2): 126–35
Paine MF, Khalighi M, Fisher JM, et al. Characterization of interintestinal and intraintestinal variations in human CYP3A-dependent metabolism. J Pharmacol Exp Ther 1997 Dec; 283(3): 1552–62
Liu P, Foster G, Gandelman K, et al. Steady-state pharmacokinetic and safety profiles of voriconazole and ritonavir in healthy male subjects. Antimicrob Agents Chemother 2007 Oct; 51(10): 3617–26
Youdim KA, Zayed A, Dickins M, et al. Application of CYP3A4 in vitro data to predict clinical drug-drug interactions: predictions of compounds as objects of interaction. Br J Clin Pharmacol 2008 May; 65(5): 680–92
Houston JB, Galetin A. Methods for predicting in vivo pharmacokinetics using data from in vitro assays. Curr Drug Metab 2008 Nov; 9(9): 940–51
Gibbs JP, Hyland R, Youdim K. Minimizing polymorphic metabolism in drug discovery: evaluation of the utility of in vitro methods for predicting pharmacokinetic consequences associated with CYP2D6 metabolism. Drug Metab Dispos 2006 Sep; 34(9): 1516–22
Venkatakrishnan K, Obach RS, Rostami-Hodjegan A. Mechanism-based inactivation of human cytochrome P450 enzymes: strategies for diagnosis and drug-drug interaction risk assessment. Xenobiotica 2007 Oct–Nov; 37(10–11): 1225–56
Ito K, Iwatsubo T, Kanamitsu S, et al. Prediction of pharmacokinetic alterations caused by drug-drug interactions: metabolic interaction in the liver. Pharmacol Rev 1998 Sep; 50(3): 387–412
Kivisto KT, Kantola T, Neuvonen PJ. Different effects of itraconazole on the pharmacokinetics of fluvastatin and lovastatin. Br J Clin Pharmacol 1998 Jul; 46(1): 49–53
Neuvonen PJ, Jalava KM. Itraconazole drastically increases plasma concentrations of lovastatin and lovastatin acid. Clin Pharmacol Ther 1996 Jul; 60(1): 54–61
Kantola T, Kivisto KT, Neuvonen PJ. Effect of itraconazole on the pharmacokinetics of atorvastatin. Clin Pharmacol Ther 1998 Jul; 64(1): 58–65
Mazzu AL, Lasseter KC, Shamblen EC, et al. Itraconazole alters the pharmacokinetics of atorvastatin to a greater extent than either cerivastatin or pravastatin. Clin Pharmacol Ther 2000 Oct; 68(4): 391–400
Heinig R, Adelmann HG, Ahr G. The effect of ketoconazole on the pharmacokinetics, pharmacodynamics and safety of nisoldipine. Eur J Clin Pharmacol 1999 Mar; 55(1): 57–60
Jalava KM, Olkkola KT, Neuvonen PJ. Itraconazole greatly increases plasma concentrations and effects of felodipine. Clin Pharmacol Ther 1997 Apr; 61(4): 410–5
Tateishi T, Ohashi K, Sudo T, et al. Dose dependent effect of diltiazem on the pharmacokinetics of nifedipine. J Clin Pharmacol 1989 Nov; 29(11): 994–7
Varhe A, Olkkola KT, Neuvonen PJ. Oral triazolam is potentially hazardous to patients receiving systemic antimycotics ketoconazole or itraconazole. Clin Pharmacol Ther 1994 Dec; 56(6 Pt 1): 601–7
Greenblatt DJ, Wright CE, von Moltke LL, et al. Ketoconazole inhibition of triazolam and alprazolam clearance: differential kinetic and dynamic consequences. Clin Pharmacol Ther 1998 Sep; 64(3): 237–47
von Moltke LL, Greenblatt DJ, Harmatz JS, et al. Triazolam biotransformation by human liver microsomes in vitro: effects of metabolic inhibitors and clinical confirmation of a predicted interaction with ketoconazole. J Pharmacol Exp Ther 1996 Feb; 276(2): 370–9
Lam YW, Alfaro CL, Ereshefsky L, et al. Pharmacokinetic and pharmacodynamic interactions of oral midazolam with ketoconazole, fluoxetine, fluvoxamine, and nefazodone. J Clin Pharmacol 2003 Nov; 43(11): 1274–82
Olkkola KT, Backman JT, Neuvonen PJ. Midazolam should be avoided in patients receiving the systemic antimycotics ketoconazole or itraconazole. Clin Pharmacol Ther 1994 May; 55(5): 481–5
Chung E, Nafziger AN, Kazierad DJ, et al. Comparison of midazolam and simvastatin as cytochrome P450 3A probes. Clin Pharmacol Ther 2006 Apr; 79(4): 350–61
Tsunoda SM, Velez RL, von Moltke LL, et al. Differentiation of intestinal and hepatic cytochrome P450 3A activity with use of midazolam as an in vivo probe: effect of ketoconazole. Clin Pharmacol Ther 1999 Nov; 66(5): 461–71
Greenblatt DJ, von Moltke LL, Harmatz JS, et al. Kinetic and dynamic interaction study of zolpidem with ketoconazole, itraconazole, and fluconazole. Clin Pharmacol Ther 1998 Dec; 64(6): 661–71
Kivisto KT, Lamberg TS, Kantola T, et al. Plasma buspirone concentrations are greatly increased by erythromycin and itraconazole. Clin Pharmacol Ther 1997 Sep; 62(3): 348–54
Kivisto KT, Lamberg TS, Neuvonen PJ. Interactions of buspirone with itraconazole and rifampicin: effects on the pharmacokinetics of the active 1-(2-pyrimidinyl)-piperazine metabolite of buspirone. Pharmacol Toxicol 1999 Feb; 84(2): 94–7
Foradori A, Mezzano S, Videla C, et al. Modification of the pharmacokinetics of cyclosporine A and metabolites by the concomitant use of Neoral and diltiazem or ketoconazole in stable adult kidney transplants. Transplant Proc 1998 Aug; 30(5): 1685–7
Butman SM, Wild JC, Nolan PE, et al. Prospective study of the safety and financial benefit of ketoconazole as adjunctive therapy to cyclosporine after heart transplantation. J Heart Lung Transplant 1991 May–Jun; 10(3): 351–8
Gomez DY, Wacher VJ, Tomlanovich SJ, et al. The effects of ketoconazole on the intestinal metabolism and bioavailability of cyclosporine. Clin Pharmacol Ther 1995 Jul; 58(1): 15–9
Sanofi Aventis US LLC. Ketek® (telithromycin tablets): label. Bridgewater (NJ): Sanofi Aventis US LLC, 2007 Feb [online]. Available from URL: http://www.accessdata.fda.gov/drugsatfda_docs/label/2007/021144s012lbl.pdf [Accessed 2009 Aug 4]
Saari TI, Laine K, Leino K, et al. Effect of voriconazole on the pharmacokinetics and pharmacodynamics of intravenous and oral midazolam. Clin Pharmacol Ther 2006 Apr; 79(4): 362–70
Neuvonen PJ, Kantola T, Kivisto KT. Simvastatin but not pravastatin is very susceptible to interaction with the CYP3A4 inhibitor itraconazole. Clin Pharmacol Ther 1998 Mar; 63(3): 332–41
Yeates RA, Laufen H, Zimmermann T. Interaction between midazolam and clarithromycin: comparison with azithromycin. Int J Clin Pharmacol Ther 1996 Sep; 34(9): 400–5
Gorski JC, Jones DR, Haehner-Daniels BD, et al. The contribution of intestinal and hepatic CYP3A to the interaction between midazolam and clarithromycin. Clin Pharmacol Ther 1998 Aug; 64(2): 133–43
Zimmermann T, Yeates RA, Laufen H, et al. Influence of the antibiotics erythromycin and azithromycin on the pharmacokinetics and pharmacodynamics of midazolam. Arzneimittelforschung 1996 Feb; 46(2): 213–7
Olkkola KT, Aranko K, Luurila H, et al. A potentially hazardous interaction between erythromycin and midazolam. Clin Pharmacol Ther 1993 Mar; 53(3): 298–305
Backman JT, Olkkola KT, Aranko K, et al. Dose of midazolam should be reduced during diltiazem and verapamil treatments. Br J Clin Pharmacol 1994 Mar; 37(3): 221–5
Olkkola KT, Ahonen J, Neuvonen PJ. The effects of the systemic antimycotics, itraconazole and fluconazole, on the pharmacokinetics and pharmacodynamics of intravenous and oral midazolam. Anesth Analg 1996 Mar; 82(3): 511–6
Elliott P, Dundee JW, Elwood RJ, et al. The influence of H2 receptor antagonists on the plasma concentrations of midazolam and temazepam. Eur J Anaesthesiol 1984 Sep; 1(3): 245–51
Fee JP, Collier PS, Howard PJ, et al. Cimetidine and ranitidine increase midazolam bioavailability. Clin Pharmacol Ther 1987 Jan; 41(1): 80–4
Elwood RJ, Hildebrand PJ, Dundee JW, et al. Ranitidine influences the uptake of oral midazolam. Br J Clin Pharmacol 1983 Jun; 15(6): 743–5
Backman JT, Aranko K, Himberg JJ, et al. A pharmacokinetic interaction between roxithromycin and midazolam. Eur J Clin Pharmacol 1994; 46(6): 551–5
Backman JT, Olkkola KT, Neuvonen PJ. Azithromycin does not increase plasma concentrations of oral midazolam. Int J Clin Pharmacol Ther 1995 Jun; 33(6): 356–9
Grasela DM, LaCreta FP, Kollia GD, et al. Open-label, nonrandomized study of the effects of gatifloxacin on the pharmacokinetics of midazolam in healthy male volunteers. Pharmacotherapy 2000 Mar; 20(3): 330–5
Van Harten J, van Brummelen P, Lodewijks MT, et al. Pharmacokinetics and hemodynamic effects of nisoldipine and its interaction with cimetidine. Clin Pharmacol Ther 1988 Mar; 43(3): 332–41
Mousa O, Brater DC, Sunblad KJ, et al. The interaction of diltiazem with simvastatin. Clin Pharmacol Ther 2000 Mar; 67(3): 267–74
Kantola T, Kivisto KT, Neuvonen PJ. Erythromycin and verapamil considerably increase serum simvastatin and simvastatin acid concentrations. Clin Pharmacol Ther 1998 Aug; 64(2): 177–82
Ito K, Sawada Y, Sugiyama Y, et al. Linear relationship between GABAA receptor occupancy of muscimol and glucose metabolic response in the conscious mouse brain: clinical implication based on comparison with benzodiazepine receptor agonist. Drug Metab Dispos 1994 Jan–Feb; 22(1): 50–4
Shimada S, Nakajima Y, Yamamoto K, et al. Comparative pharmacodynamics of eight calcium channel blocking agents in Japanese essential hypertensive patients. Biol Pharm Bull 1996 Mar; 19(3): 430–7
Thompson PD, Clarkson P, Karas RH. Statin-associated myopathy. JAMA 2003 Apr 2; 289(13): 1681–90
Robin DW, Hasan SS, Lichtenstein MJ, et al. Dose-related effect of triazolam on postural sway. Clin Pharmacol Ther 1991 May; 49(5): 581–8
Yasui N, Kondo T, Otani K, et al. Effect of itraconazole on the single oral dose pharmacokinetics and pharmacodynamics of alprazolam. Psychopharmacology 1998 Oct; 139(3): 269–73
Bottorff MB. Statin safety and drug interactions: clinical implications. Am J Cardiol 2006 Apr 17; 97(8A): 27–31C
Herbrecht R. Voriconazole: therapeutic review of a new azole antifungal. Expert Rev Anti Infect Ther 2004 Aug; 2(4): 485–97
Niwa T, Shiraga T, Takagi A. Effect of antifungal drugs on cytochrome P450 (CYP) 2C9, CYP2C19, and CYP3A4 activities in human liver microsomes. Biol Pharm Bull 2005 Sep; 28(9): 1805–8
Marty FM, Lowry CM, Cutler CS, et al. Voriconazole and sirolimus coadministration after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 2006 May; 12(5): 552–9
Yoshida N, Yamada A, Mimura Y, et al. Trends in new drug interactions for pharmaceutical products in Japan. Pharmacoepidemiol Drug Saf 2006 Jun; 15(6): 421–7
Vasques LR, Stabellini R, Xue F, et al. XIST repression in the absence of DNMT1 and DNMT3B. DNA Res 2005; 12(5): 373–8
Johnson TN, Rostami-Hodjegan A, Tucker GT. Prediction of the clearance of eleven drugs and associated variability in neonates, infants and children. Clin Pharmacokinet 2006; 45(9): 931–56
Shorr RI, Robin DW. Rational use of benzodiazepines in the elderly. Drugs Aging 1994 Jan; 4(1): 9–20
Petrovic M, Mariman A, Warie H, et al. Is there a rationale for prescription of benzodiazepines in the elderly? Review of the literature. Acta Clin Belg 2003 Jan–Feb; 58(1): 27–36
Neuvonen PJ, Niemi M, Backman JT. Drug interactions with lipid-lowering drugs: mechanisms and clinical relevance. Clin Pharmacol Ther 2006 Dec; 80(6): 565–81
Asberg A. Interactions between cyclosporin and lipid-lowering drugs: implications for organ transplant recipients. Drugs 2003; 63(4): 367–78
Acknowledgements
This study was supported by Health and Labor Sciences Research Grants for Research on Regulatory Science of Pharmaceuticals and Medical Devices from the Ministry of Health, Labor and Welfare, Japan. The authors have no conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hisaka, A., Kusama, M., Ohno, Y. et al. A Proposal for a Pharmacokinetic Interaction Significance Classification System (PISCS) Based on Predicted Drug Exposure Changes and Its Potential Application to Alert Classifications in Product Labelling. Clin Pharmacokinet 48, 653–666 (2009). https://doi.org/10.2165/11317220-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11317220-000000000-00000