Abstract
Introduction
Diffuse malignant peritoneal mesothelioma (DMPM) is a rare malignancy associated with poor outcomes. Recent reports have shown longer survival with radical surgery, usually combined with intraperitoneal chemotherapy. However, surgical interventions in these patients have not been extensively studied at a population level. The objective of this retrospective cohort study is to assess the prevalence of surgical and nonsurgical interventions for DMPM patients, the influence of surgery on survival outcomes, and the associations between demographic and clinical factors with treatments and outcomes.
Methods
This study included adult patients diagnosed with DMPM from 2003 to 2014 and registered in the National Cancer Database (NCDB). The primary outcome was overall survival. Histologically confirmed mesothelioma was defined using International Classification of Diseases (ICD)-3 codes 9050/3, 9051/3, 90523, and 9053/3 and peritoneum as primary affected organ using ICD codes C17-19, C22-24, C26, C42, C48, and C76. Relationships between demographic and clinical variables, surgical treatments, and survival outcomes were evaluated using logistic and Cox modeling and log-rank tests.
Results
A total of 2062 patients were identified, of whom 1055 (51%) did not receive any surgery while 701 (34%) received radical surgery. Patients receiving radical surgery had overall survival of 38.4 months compared with 7.1 months for patients without surgery (p < 0.001) and 41.8 months in patients who received both radical surgery and systemic chemotherapy.
Conclusions
Patients selected for and treated with radical surgery had significantly better overall survival compared with those receiving nonsurgical treatment. Patients newly diagnosed with DMPM should be evaluated for the possibility of receiving radical surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Diffuse malignant peritoneal mesothelioma (DMPM) is a rare primary malignancy of the peritoneum, affecting approximately 200–400 new patients per year in the USA. It accounts for approximately 30% of all mesothelioma tumors and is characterized by progressive accumulation of tumor nodules within the abdominal cavity, leading to nutritional dysfunction, bowel obstruction, malignant ascites, and death.1 Asbestos is the primary risk factor for all mesotheliomas; however, 67% of patients with peritoneal mesothelioma have no reported history of asbestos exposure.2
An important characteristic of peritoneal mesothelioma is that, despite its tendency for diffuse involvement and aggressive progression within the peritoneal cavity, it is rare for DMPM to spread via hematogenous or lymphatic routes or to extend beyond the peritoneal cavity.3,4,5 Despite this characteristic, the disease has been considered universally fatal with a historical survival of 6–12 months.6,7,8,9,10 Chemotherapy-based treatment utilizing pemetrexed in combination with cisplatin has been considered the standard of care, with median survival time of 13.1–24 months and median time to disease progression of 9.5 months.11,12,13 Cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) has been developed in recent years as a treatment option for patients with a variety of peritoneal surface malignancies including DMPM. Multiple studies utilizing CRS and HIPEC have demonstrated median survival of 34–100 months, indicating that surgery may have a very significant impact on survival.14,15,16,17 However, the available studies are primarily single-institution cohort studies from expert HIPEC centers, while prospective clinical trials evaluating the role and impact of surgery are not available.
At a broader, national level, there are very limited data regarding the frequency and impact of surgical treatments on the majority of patients diagnosed with DMPM in the USA. The single published study on this topic is a review of Surveillance, Epidemiology, and End Results (SEER) data, demonstrating that only 56% of patients treated in the USA between 1990 and 2010 received radical surgical therapy.18
Therefore, it appears that surgical treatments may have significant potential but are underutilized for patients with DMPM. It is unknown whether the current trends in utilization of surgical management for DMPM in the USA over the last 10 years have been increasing, correlating with wider acceptance and availability of CRS and HIPEC. There has also been little research identifying which clinical and socioeconomic factors may be associated with surgical interventions in DMPM.
The aim of this study is thus to evaluate the prevalence of all surgical interventions in patients diagnosed with DMPM between 2003 and 2014, the frequency of radical surgery compared with palliative surgical interventions and nonsurgical treatments, the association between clinical and socioeconomic factors and treatments, as well as survival outcomes of patients with DMPM, utilizing data from the National Cancer Database.
Methods
This study is a retrospective cohort study of adult patients diagnosed with DMPM from 2003 to 2014 and registered in the National Cancer Database (NCDB), a clinical oncology database jointly sponsored by the American College of Surgeons and the American Cancer Society. The data are sourced from hospital registry data that are collected in more than 1500 Commission on Cancer (CoC)-accredited facilities. The data represent more than 70% of newly diagnosed cancer cases nationwide.
Patients with histologically confirmed mesothelioma [International Classification of Diseases (ICD)-3 histology codes 9050/3 Mesothelioma malignant, 9051/3 Fibrous mesothelioma, malignant, 9052/3 Epithelioid mesothelioma, malignant, and 9053/3 Mesothelioma biphasic, malignant] and peritoneum as primary affected organ (ICD site codes C17-19, C 22-24, C26, C42, C48, and C76) were included. Cases with pleural or genital tract mesothelioma were excluded. Cystic mesothelioma (ICD-3 code 9055/1) was also excluded. Cases with missing data regarding surgical interventions or survival were excluded. Data related to age, sex, race, histologic subtype, surgical treatment, radiation and systemic treatment, treatment facility type, residential area, residential distance to treatment facility, insurance status, community median household income, community education level, and survival data were analyzed.
Surgical interventions were classified into three categories: (1) no surgery (procedure code 00), (2) minimal or partial surgery, defined as codes describing partial destruction without specimen, excisional biopsy, and partial removal of primary site (procedure codes 10, 13, 20, 21, 22, 23, 25, 26, 30, 51, and 80), and (3) radical surgery, defined as procedures classified as total removal of primary site, debulking surgery, and codes describing en bloc removal or primary site with contiguous organs (procedure codes 40, 50, 60, 61, and 63).
Chemotherapy was classified as no chemotherapy (codes 00, 82, 85, 86, and 87), chemotherapy used (codes 01, 02, and 03), and chemotherapy status unknown.
For surgical patients, the NCDB provides data on the sequence of surgery and “systemic therapy” as a summative variable that includes chemotherapy, immunotherapy, and hormonal therapy. We assumed that the majority of patients who received any form of “systemic therapy” received it in the form of chemotherapy. Therefore, we use the term “chemotherapy” to analyze based on surgery–chemotherapy (“systemic therapy”) sequence. The patients were grouped as follows: no chemotherapy, neoadjuvant chemotherapy before surgery (sequence codes 2 and 4), adjuvant chemotherapy after surgery (sequence code 3), intraoperative therapy during surgery (sequence codes 5 and 6), and status unknown. The patients in the intraoperative therapy group include both those who received other systemic therapy either before or after surgery (sequence code 6) as well as those who only received intraoperative therapy (sequence code 5).
The NCDB does not provide further details regarding the type of “intraoperative” therapy in this variable. However, the authors assume that the majority of these patients received HIPEC.
Descriptive statistics were used to describe the demographic and clinical characteristics, as well as available socioeconomic factors (type of treatment facility, insurance status, household income, and education at community level derived from 2012 US survey data). Primary analyses were designed to address the correlation of the surgical type with overall survival (OS) and identify factors associated with use of radical surgery in this population. OS was defined as time from diagnosis to death due to any cause or last contact, whichever occurred first. Median OS was estimated using the Kaplan–Meier method, with log-rank test to compare the group difference in survival function. Cox proportional hazard model was used to evaluate the relationship between surgical type and OS, with hazard ratio (HR) and 95% confidence interval (CI) for risk of death estimated for limited surgery or radical surgery as compared with no surgery, after adjusting relevant demographic and clinical variables. The surgical type was also further categorized with respect to radical surgery (yes or no), and a multiple logistic regression analysis was performed to identify the demographic, socioeconomic, or clinical characteristics that could significantly affect use of radical surgery. All statistical analyses were carried out using SAS version 9.4 (SAS Institute, Cary, NC), and statistical significance was assessed at α = 0.05. All tests were two-sided.
Results
Patient Characteristics
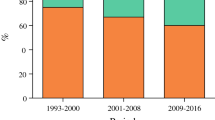
After applying the inclusion and exclusion criteria to the NCDB dataset, a total of 2062 cases were included in the analysis. A majority of patients were male [1149 (55.7%)] and White [1858 (90.1%)], with median age of 63 years. The most commonly reported histological classification was mesothelioma not otherwise specified (NOS) [1055 (51.5%)] followed by epithelioid mesothelioma [841 (40.8%)], while fibrous mesothelioma and biphasic mesothelioma were reported in 78 (3.8%) and 81 (3.9%) cases, respectively. Only 701 (34%) patients received radical surgery, while the majority of patients [1055 (51.2%)] did not receive any surgical intervention. A majority of patients received chemotherapy [1233 (59.8%)]. The clinical and demographic characteristics of the patients are summarized in Table 1. The rate of utilization of radical surgery did not change significantly over the study period.
Factors Associated with Surgical Interventions
Socioeconomic factors as well as type of treatment facility were important factors in determining whether surgery was performed. Patients treated at academic/research cancer programs, those with longer distance from residence to treatment facility, and those with private insurance were more likely to undergo radical surgery. Residential area, patient education level, and household income level did not have a statistically significant correlation with the likelihood of receiving radical surgery. Younger patients and females were more likely to receive radical surgery. Findings regarding demographic, clinical, and socioeconomic factors associated with radical surgery are presented in Table 2.
Long-Term Outcomes
The median overall survival of all patients in the cohort was estimated to be 15.6 months, with survival rates of 56%, 41%, and 33% at 1, 2, and 3 years from diagnosis, respectively. Overall survival was significantly longer in patients who received surgery (38.4 months for radical surgery and 32.4 months for limited surgery) than in those who did not have any surgery (7.1 months) (Fig. 1). Among patients who did not have any surgery, treatment with systemic chemotherapy was associated with improved survival compared with no treatment (11 vs. 3.3 months), but overall survival remained poor in both groups (Fig. 2a). Among patients who did have surgery, treatment with systemic chemotherapy was associated with improved survival as well with an overall survival of 41.8 months for patients who had both surgery and systemic chemotherapy (Fig. 2b). On multivariable analysis, increasing age, female sex, comorbidity score, epithelioid histology type, surgical intervention of any type, and chemotherapy were all found to be associated with improved overall survival (Table 3).
Kaplan–Meier estimate of overall survival among a malignant peritoneal mesothelioma patients treated nonsurgically based on whether they received systemic chemotherapy and b malignant peritoneal mesothelioma patients undergoing radical surgery based on whether they received systemic chemotherapy. Numbers at risk shown below x axis. HR hazard ratio, CI confidence interval
An exploratory analysis evaluating the potential effect of chemotherapy sequence in surgical patients is shown in Fig. 3. Improved survival was particularly evident for patients receiving intraoperative chemotherapy, while no survival benefit was seen with neoadjuvant chemotherapy, though the sample size was limited. The survival was similar for patients who received radical surgery and intraoperative chemotherapy compared with those who received radical surgery and intraoperative therapy with additional systemic therapy (median OS: 66.6 vs. 65.4 months; p = 0.964).
Kaplan–Meier estimate of overall survival among malignant peritoneal mesothelioma surgical patients based on sequence of chemotherapy. No CT no chemotherapy used, Neo-CT chemotherapy used before surgery, Adj-CT chemotherapy used after surgery, Intra-CT chemotherapy used during surgery. Number at risk shown below x axis
Discussion
Diffuse malignant peritoneal mesothelioma (DMPM) has not traditionally been considered a surgical disease.3,4,19 With only approximately 200–400 new cases diagnosed each year in the USA, it is an orphan disease, and a generally nihilistic attitude among physicians prevails. Indeed, the outcomes with the traditional approach of palliative systemic chemotherapy have been disappointing, and the results of this study confirm again that, even in the most recent years, this has not changed compared with historically reported outcomes. The median overall survival of patients treated with systemic chemotherapy in our cohort was only 11 months. The attitude of treating physicians may be impacted by their view of malignant pleural mesothelioma (MPM), for which outcomes have been particularly poor and surgery has also not been consistently utilized. Nelson et al.20 recently published a propensity score matching analysis in which only one-third of the patients were treated surgically. Median survival was extended in the surgery groups, but the difference in survival between patients who received surgery and those who did not was more limited.
Starting in the early 1990s, several centers around the world, spearheaded by efforts at the National Institutes of Health, started to adopt a different treatment strategy for peritoneal mesothelioma that centered on surgery.15,16,17 Several characteristics of DMPM made this treatment strategy a logical choice: although the disease involves the abdominal cavity diffusely, it virtually never spreads hematogenously to the liver or distant organs, and even lymphatic metastases are rare. CRS has evolved as a surgical procedure aimed at resecting visible tumor nodules from the abdominal cavity using a combination of peritoneal stripping and visceral resections.21 This surgical procedure is typically combined with application of HIPEC, based on the fact that microscopic disease is likely to still be present in the abdominal cavity at the end of a cytoreductive procedure and the favorable pharmacologic characteristics of intraperitoneal application and heat for certain chemotherapeutics.22,23 These expert centers have shown that much improved survival outcomes compared with historical controls can be achieved with CRS and HIPEC for DMPM, with median overall survival ranging from 34 to 100 months.
Experience has grown significantly over the years. Yan et al.24 performed a multiinstitutional study that included 405 patients with DMPM and demonstrated median survival of 53 months and 5-year survival of 47%, with the caveat that 79% had epithelial tumors. The most recent systematic review that summarized the outcomes of CRS and HIPEC for DMPM across the world over the last approximately 25 years included 1047 patients.25 While this fairly large number of treated patients and the outcomes reported provide evidence supporting CRS and HIPEC for DMPM, it is less clear that surgery is sufficiently used for DMPM across the USA at the present time and that there has been any significant change in utilization of surgery in recent years.
The study reported herein is the largest regarding treatments administered for patients with DMPM across hospitals in the USA in the modern era (2003–2014). The results demonstrate that surgery had a profound impact on survival, similar to the outcomes reported by expert peritoneal malignancy centers. Patients receiving radical surgery in our cohort had median survival of 38 months compared with 7 months for patients who had no surgery and 41.8 months for patients who received both radical surgery and systemic chemotherapy. However, it appears that surgery remains underutilized, with only about one-third of patients receiving radical surgery and no change in the rate of utilization of radical surgery over the 10-year study period.
The results of this study confirm that a multimodality approach that combines surgery and chemotherapy is associated with the best outcomes. An important aspect of multimodality treatment that combines surgery and chemotherapy is the optimal sequence of these treatments. Expert CRS and HIPEC centers have tried to answer this question, but studies were often limited by small sample size. Some have suggested that neoadjuvant chemotherapy prior to cytoreduction has a detrimental effect.26 Interestingly, the current study also suggests that the outcomes among patients who were treated with both chemotherapy and surgery were worst for patients treated with neoadjuvant chemotherapy (27.9 months) and best for those who were treated with intraoperative chemotherapy (65.9 months). We hypothesize that this latter group of patients most likely represent those treated with CRS and HIPEC who benefited from both the most aggressive surgery as well as HIPEC.
Another interesting aspect of mesothelioma is the impact of gender on the epidemiology and outcomes of mesothelioma (both pleural and peritoneal).27,28 While improved survival outcomes for women have been published in multiple studies, the explanation for this difference remains uncertain. It has been speculated that the hormonal milieu may be a significant factor, as well as possibly earlier diagnosis and improved ability to undergo treatment. In the current study, increased utilization of surgical treatment was observed, which may be another factor that ultimately influences improved survival among women. The reasons why there is a difference in utilization of surgery between sexes cannot be reliably studied using the NCDB dataset. We speculate that the increased use of surgery could be related to frequent involvement of the uterus and ovaries by mesothelioma in women, prompting a different diagnostic approach in females. There is a possible association between infertility and mesothelioma in young women, which again may lead to more aggressive and earlier workup, sometimes including diagnostic laparoscopy allowing for earlier definitive diagnosis and improved assessment of resectability.
There are little data on what factors influence physicians’ decisions regarding treatment choice in peritoneal malignancies such as DMPM. Multiple studies suggest that physicians who do not specialize in treatment of peritoneal malignancies have limited knowledge about the possibility of complete surgical resection, the indications for cytoreductive surgery, and the associated outcomes, which in turn may influence their decisions to pursue only nonsurgical treatments.29,30 The current study could identify some socioeconomic and treatment facility characteristics that were associated with radical surgical treatment, including academic/research program and private insurance.
Considering the rarity of peritoneal mesothelioma, the complexity of the required evaluation and treatments, and in particular the potential strong impact of radical surgical treatment, which appears to be more available in academic cancer programs, strong consideration should be given to the formation of a national network of designated peritoneal mesothelioma treatment centers able to deliver the full spectrum of potential treatments, including radical surgical resection through cytoreductive surgery. This would have the potential to improve access to optimal care for all patients with this rare disease and would facilitate further research. While the NCDB dataset did not allow us to directly evaluate how outcomes of known expert centers in the USA differ from the overall results, we observed that patients who were treated at facilities with the greatest distance from their place of residence had improved outcomes, which potentially captures those patients treated at referral centers.
There are limitations to this study, deriving from the fact that data available through large national databases may have inaccuracies in data collection or classification that cannot be corrected by examining the original patient files. However, the NCDB is likely less prone to these types of errors due to the fact that its primary purpose is not billing or other administrative use, but tracking and quality control of cancer outcomes specifically, and it is based on individual hospitals’ cancer registry information.
Another important limitation in interpreting the results is the fact that peritoneal mesothelioma does not have an accepted staging system and therefore stage of disease could not be incorporated into the analysis. There is no doubt that extent of the disease as well as other patient and clinical factors that we were able to study, such as age, sex, and histological subtype, play an important and independent role in determining the prognosis and survival of patients with mesothelioma, as confirmed in our multivariable analysis. These factors also influence the decision to perform surgery, so that the large survival difference seen between patients who are treated surgically and those who are not in part reflects the inherent difference in prognosis among those two groups of patients. The influence of stage or extent of disease may be somewhat diminished in peritoneal mesothelioma compared with pleural mesothelioma, in which mediastinal invasion, chest wall invasion, and lymph node involvement can be seen and incorporated into staging. In contrast, peritoneal mesothelioma rarely shows retroperitoneal invasion or lymph node extension, and some authors have proposed a staging system that relies in significant part on the intraperitoneal burden of disease.31
The results of this study show that, for those patients who are good candidates for and are selected to receive radical surgery, this is associated with very significant long-term survival, especially when combined with chemotherapy. This means that every patient diagnosed with peritoneal mesothelioma should be evaluated for the possibility of receiving radical surgery. Indeed, the decision of whether or not a patient is an appropriate candidate for radical surgery is likely one of the most important therapeutic decisions when evaluating a patient with newly diagnosed peritoneal mesothelioma and should be done in centers with appropriate experience with surgical treatments of diffuse peritoneal disease. Considering the rarity of DMPM and the difficulties in conducting prospective randomized trials comparing operative and nonoperative treatments, it is unlikely that we will ever have a higher level of evidence supporting surgery versus nonsurgical treatments than a large cohort study such as this one.
This study is the largest to date to report the prevalence of surgical therapy for management of DMPM and the associated outcomes. The results demonstrate that the majority of patients with DMPM are not treated surgically. For those patients who are able to have radical surgery, survival is significantly improved and much better than what is generally discussed as the expected survival after a diagnosis of peritoneal mesothelioma. On the other hand, if patients are not offered or are not candidates for surgery, the outcomes remain very poor and similar to historic results, with median survival of 11 months in our study. The results of this study suggest that every newly diagnosed patient with peritoneal mesothelioma should be evaluated by a multidisciplinary team that includes a surgeon with expertise in peritoneal malignancies, as surgical resection appears to be the intervention with the greatest potential to positively impact survival in appropriately selected patients.
References
Price B, Ware A. Time trend of mesothelioma incidence in the United States and projections of future cases: an update based on SEER data for 1973 through 2005. Crit Rev Toxicol. 2009;39(7):576–88.
Boffetta P. Epidemiology of peritoneal mesothelioma: a review. Ann Oncol. 2007;18(6):985–90.
Bridda A, Padoan I, Mencarelli R, Frego M. Peritoneal mesothelioma: a review. MedGenMed. 2007;9(2):32.
Yan TD, Welch L, Black D, Sugarbaker PH. A systematic review on the efficacy of cytoreductive surgery combined with perioperative intraperitoneal chemotherapy for diffuse malignancy peritoneal mesothelioma. Ann Oncol. 2007;18(5):827–34.
Moertel CG. Peritoneal mesothelioma. Gastroenterology. 1972;63:346–50.
Chua TC, Yan TD, Morris DL. Outcomes of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for peritoneal mesothelioma: the Australian experience. J Surg Oncol. 2009;99(2):109–13.
Turaga KK, Deraco M, Alexander HR. Current management strategies for peritoneal mesothelioma. Int J Hyperthermia. 2017;33(5):579–81.
Mirarabshahii P, Pillai K, Chua TC, Pourgholami MH, Morris DL. Diffuse malignant peritoneal mesothelioma—an update on treatment. Cancer Treat Rev. 2012;38(6):605–12.
Eltabbakh GH, Piver MS, Hempling RE, Recio FO, Intengen ME. Clinical picture, response to therapy, and survival of women with diffuse malignant peritoneal mesothelioma. J Surg Oncol. 1999;70(1):6–12.
Magge D, Zenati MS, Austin F, et al. Malignant peritoneal mesothelioma: prognostic factors and oncologic outcome analysis. Ann Surg Oncol. 2014;21(4):1159–65.
Jänne PA, Wozniak AJ, Belani CP, et al. Open-label study of pemetrexed alone or in combination with cisplatin for the treatment of patients with peritoneal mesothelioma: outcomes of an expanded access program. Clin Lung Cancer. 2005;7(1):40–6.
Lainakis G, Zagouri F, Kastritis E, et al. Systemic chemotherapy with pemetrexed and cisplatin for malignant peritoneal mesothelioma: a single institution experience. Tumori. 2011;97(1):25–9.
Carteni G, Manegold C, Garcia GM, et al. Malignant peritoneal mesothelioma—Results from the International Expanded Access Program using pemetrexed alone or in combination with a platinum agent. Lung Cancer. 2009;64(2):211–8.
Elias D, Bedard V, Bouzid T, et al. Malignant peritoneal mesothelioma: treatment with maximal cytoreductive surgery plus intraperitoneal chemotherapy. Gastroenterol Clin Biol. 2007;31(10):784–8.
Feldman AL, Libutti SK, Pingpank JF, et al. Analysis of factors associated with outcomes in patients with malignant peritoneal mesothelioma undergoing surgical debulking and intraperitoneal chemotherapy. J Clin Oncol. 2003;21(24):4560–67.
Yan TD, Yoo D, Sugarbaker PH. Significance of lymph node metastasis in patients with diffuse malignant peritoneal mesothelioma. Eur J Surg Oncol. 2006;32(9):948–53.
Deraco M, Nonaka D, Baratti D, et al. Prognostic analysis of clinicopathologic factors in 49 patients with diffuse malignant peritoneal mesothelioma treated with cytoreductive surgery and intraperitoneal hyperthermic perfusion. Ann Surg Oncol. 2006;13(2):229–37.
Miura J, Johnston F, Gamblin TC, Turaga KK. Current trends in the management of malignant peritoneal mesothelioma. Ann Surg Oncol. 2014;21(2):3947–53.
Mirabelli D, Roberti S, Gangemi M, et al. Survival of peritoneal malignant mesothelioma in Italy: a population-based study. Int J Cancer. 2009;124(1):194–200.
Nelson D, Rice D, Niu J, et al. Long-term survival outcomes of cancer-directed surgery for malignant pleural mesothelioma: propensity score matching analysis. J Clin Oncol. 2017;35(29):3354–62.
Sugarbaker PH. Peritonectomy procedures. Ann Surg. 1995;221(1):29–42.
Van der Speeten K, Stuart OA, Mahteme H, Sugarbaker PH. A pharmacologic analysis of intraoperative intracavitary cancer chemotherapy with doxorubicin. Cancer Chemother Pharmacol. 2009;63(5):799–805.
Van der Speeten K, Stuart OA, Sugarbaker PH. Pharmacology of perioperative intraperitoneal and intravenous chemotherapy in patients with peritoneal surface malignancy. Surg Oncol Clin N Am. 2012;21(4):577–97.
Yan TD, Deraco M, Baratti D, et al. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for malignant peritoneal mesothelioma: multi-institutional experience. J Clin Oncol. 2009;27(36):6237–42.
Helm JH, Miura JT, Glenn JA, et al. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for malignant peritoneal mesothelioma: a systematic review and meta-analysis. Ann Surg Oncol. 2015;22(5):1686–93.
Kepenekian V, Elias D, Passot G et al. Diffuse malignant peritoneal mesothelioma: Evaluation of systemic chemotherapy with comprehensive treatment through the RENAPE Database. Eur J Cancer 2016; 65:69–79.
Taioli E, Wolf A, Camacho-Rivera, et al. Women with malignant pleural mesothelioma have a threefold better survival rate than men. Ann Thorac Surg 2014; 98:1020–5.
Cao C, Yan TD, Deraco M, et al. The importance of gender in diffuse malignant peritoneal mesothelioma. Ann Oncol. 2012; 23:1494–8.
Bernaiche T, Emery E, Bijelic L. Practice patterns, attitudes, and knowledge among physicians regarding cytoreductive surgery and HIPEC for patients with peritoneal metastases [published online February 23, 2018]. Pleura Peritoneum. 2018. https://doi.org/10.1515/pp-2017-0025.
Spiegle G, Schmocker S, Huang H, et al. Physicians’ awareness of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for colorectal cancer carcinomatosis. Can J Surg. 2013;56(4):237–42.
Yan TD, Deraco M, Elias D, et al. A novel tumor-node-metastasis (TNM) staging system of diffuse malignant peritoneal mesothelioma using outcome analysis of a multi-institutional database. Cancer. 2011;117(9):1855–63.
Acknowledgment
The authors would like to thank Erica Emery, MS, Devon Collins, MPH, and Neul Ha, BS, for their support during the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
No commercial interest and source of any financial or material support.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bijelic, L., Darcy, K., Stodghill, J. et al. Predictors and Outcomes of Surgery in Peritoneal Mesothelioma: an Analysis of 2000 Patients from the National Cancer Database. Ann Surg Oncol 27, 2974–2982 (2020). https://doi.org/10.1245/s10434-019-08138-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-08138-5