Abstract
Background
With the rising cost of healthcare delivery and bundled payments for episodes of care, there has been impetus to minimize hospitalization and increase utilization of outpatient surgery mechanisms. Given the increase in outpatient mastectomy and immediate tissue expander (TE)-based reconstruction and the paucity of data on its comparative safety to inpatient procedures, we sought to understand the risk for early postoperative complications in an outpatient model compared with more traditional inpatient status using the National Surgical Quality Improvement Program database.
Methods
NSQIP data files from 2005 to 2012 were queried to identify patients undergoing immediate TE-based breast reconstruction after mastectomy. Patients were stratified by whether they received outpatient or inpatient care and then propensity score matched based on preoperative baseline characteristics to produce matched cohorts. Multivariate regression analysis was used to determine whether outpatient versus inpatient status conferred differing risk for 30-days complications.
Results
Of the 2014 patients who met criteria, 1:1 propensity matching yielded 634 patients in each of the matched cohorts. Overall complications (5.2 vs. 5.4 %), overall surgical complications (4.3 vs. 3.9 %), overall medical complications (1.3 vs. 2.1 %), and return to the operating room (6.6 vs. 7.3 %) were similar between outpatient and inpatients cohorts (p > .2), respectively. There was a small, but significant increased risk of organ/space SSI in outpatients (1.9 vs. 0.5 %, p = .02) and trend for increased risk for pulmonary embolus (PE) and urinary tract infection (UTI) in inpatients (0.3 vs. 0 %, p = .16; 0.3 vs. 0 %, p = .16).
Conclusions
Our studies suggest that outpatient TE confers similar safety profiles to inpatient TE with regards to 30-day postoperative overall complications, medical and surgical morbidity, and return to the operating room. A slightly increased risk for surgical site infection must be balanced against potential risk for known inpatient-related complications such as UTI and PE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
With the rising cost of healthcare delivery and declining reimbursements, there has been impetus to minimalize hospitalization and increase utilization of outpatient surgery mechanisms. Given these initiatives, outpatient mastectomy has become increasingly common and reconstruction in the outpatient setting has gradually followed since the 1990s.1–3 Although the proportion of outpatients undergoing reconstruction still represents an underutilization relative to inpatient mastectomy with reconstruction, steady gains in outpatient reconstruction have yielded an increase of 9.1 % between 2006 and 2009.4 Because increased outpatient reconstruction can lead to greater cost savings, evolving analysis is necessary to evaluate its safety.2,4,5 Previous efforts in this arena are rare and limited by single-institution sample sizes, inadequate consideration of morbidities, and lack of a comparison group.6,7
Tissue expander (TE) breast reconstruction has become the procedure of choice for postmastectomy reconstruction as it has been shown to produce shorter operation times and rapid recovery and lacks donor site morbidity.8–11 Given this, TE-based reconstruction lends itself well to its use in an outpatient setting. While previous studies showed disparate outcomes of inpatient and outpatient procedures in various surgical settings, it is unknown if outpatient immediate TE-based reconstruction is associated with differing complication profiles when compared with its use in an inpatient setting.12–14 To this end, we have performed the first robust, multi-institutional analysis using the American College of Surgeons National Surgical Quality Improvement Project (NSQIP) employing a propensity-matching strategy to reduce baseline differences in inpatient and outpatient cohorts. The purpose of our study is to assess the safety of outpatient (versus inpatient) immediate TE-based breast reconstruction with a focus on postoperative 30-day complication rates and return to the operating room (return to the OR).
Methods
Institutional Review Board
The Northwestern IRB has deemed this retrospective study of de-identified data exempt from IRB review and approval.
Population
The details of the ACS-NSQIP data collection methods have previously been described in detail and validated.15,16 Data files from 2005 to 2012 were reviewed to collect data on all patients undergoing immediate TE breast reconstruction during that period. All patients of interest were selected from the database based on primary Current Procedural Terminology (CPT) codes 19357. Patients undergoing a reconstructive procedure without concurrent mastectomy were considered to have undergone delayed reconstruction and were excluded. CPT codes used to identify mastectomy included simple mastectomy (19303), skin-sparing mastectomy (19304), modified radical mastectomy (19307), and radical mastectomy (19305 and 19306). Any patient who underwent multiple reconstructive procedures denoted by another or concurrent CPT code of 19340 for implant reconstructions or 19361, 19364, 19367, 19368, and 19369 for autologous reconstruction were excluded. The remaining patients were stratified by whether they received outpatient or inpatient mastectomy with immediate reconstruction as defined by the hospital at which they received the procedure. Traditionally, the inpatient label is given to patients who stayed in the hospital for longer than 23 h. All patients who were male were excluded.
Variables
NSQIP-defined preoperative variables were compared among the respective cohorts. They included demographic variables (e.g., race, age, BMI), lifestyle variables (e.g., smoking, alcohol use), and medical comorbidities (e.g., ASA class, previous sepsis, radiotherapy, chemotherapy, bleeding disorders, steroid use, wound infection, disseminated cancer, previous stroke, previous cardiac surgery, hypertension, chronic obstructive pulmonary disease (COPD), dyspnea, diabetes). Intraoperative characteristics captured included total operative time and total relative value units (RVU).
Primary outcomes were categorized as surgical complications, medical complications, and overall complications. Surgical complications included superficial, deep, or organ-space surgical site infection (SSI) and wound dehiscence. Medical complications included deep venous thrombosis (DVT), pulmonary embolism (PE), unplanned reintubation, ventilator dependence >48 h, progressive renal insufficiency, acute renal failure, coma, stroke, cardiac arrest, myocardial infarction (MI), peripheral nerve injury, pneumonia, urinary tract infection (UTI), blood transfusions, graft/prosthesis/flap failure, and sepsis/septic shock. All variables were used as defined in the NSQIP user guide. Overall complications included all surgical and medical complications. Return to the OR, which was not captured in overall complications, was defined as a planned or unplanned return for a major surgical intervention.
Statistical Analysis
Patients undergoing inpatient and outpatient TE were propensity score matched to reduce differences in 21 baseline characteristics. Nearest-neighbor and computerized greedy matching without replacement in a 1:1 ratio was utilized, the details and advantages of which have been mentioned previously.17–19 In short, propensity score matching allows more accurate assessment of treatment effect by adjusting the differences in patient comorbidities and operative details. When a close match was not available, the case was eliminated. χ 2 tests, for categorical variables, and t test, for continuous variables, were used to identify differences in perioperative variables between inpatient and outpatient cohorts. Significance was defined as p < .05. In addition to inpatient/outpatient status, total RVU and ASA class, perioperative variables with n ≥ 10, and p < .2 as identified in a bivariate screen were included in a binary logistic regression, which determined the risk-adjusted relationship between inpatient/outpatient status and overall, medical, and surgical complications. Again, p < .05 was considered significant. Hosmer–Lemeshow (H–L) and C statistics were calculated to assess model calibration and discriminatory capability, respectively.20,21 All analysis was performed using SPSS version 22 (IBM Corp., Armonk, NY).
Results
Cohort Characteristics
Of the 2014 patients extracted from the 2005 to 2012 NSQIP datasets, 666 underwent outpatient TE reconstruction while 1,348 underwent inpatient TE reconstruction. Very few differences were detected between the cohorts before they were matched (Table 1). With the exception of ASA class 3, 4, 5 (26.6 vs. 16.2 %; p < .001), previous cardiac surgery (0.3 vs. 0.00 %; p = .04), and race (p = .01), all preoperative clinical characteristics and demographics were statistically equivalent. The 746 patients without a match were discarded, leaving 1,268 well-matched patients, of which 634 underwent inpatient TE and 634 underwent outpatient TE. After matching, all pre-existing differences were balanced. Demographic profiles and comorbidity burden were similar between the 2 matched cohorts (Table 1), and no statistically significant differences were detected (p < .05).
Unadjusted rates of postoperative events for both unmatched and matched cohorts are displayed in Table 2. Before matching, all postoperative outcomes were statistically equivalent between the 2 groups with exception of organ space SSI (1.8 vs. 0.6 %; p = .01). After matching, a statistically significant difference in organ space SSIs remained (1.9 vs. 0.5 %; p = .02). Within the matched cohorts, the rate of overall complications in inpatient TE was 5.4 % compared with 5.2 % in outpatient TE (p = .90), the rates of surgical complications in inpatient TE was 3.9 % compared with 4.3 % in outpatient TE (p = .78), the rates of medical complications in inpatient TE was 2.1 % compared with 1.3 % in outpatient TE (p = .27). After matching, inpatient TE had a higher rate of return to the OR than outpatient TE (7.3 vs. 6.6 %), but the difference was neither statistically nor clinically significant (p = .66).
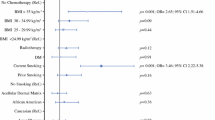
Multivariate Regression Analysis
Multivariate regression analysis was used to determine whether outpatient TE was associated with increased rates of 30-day complications or return to the OR relative to inpatient TE, after establishing matched cohorts and proper risk adjustment. Table 3 displays the results. Outpatient TE does not independently predict significantly increased risk of overall, surgical, and medical complications or return to the OR relative to inpatient TE (p, .919, .732, .275, .627, respectively).
Discussion
The surge in immediate reconstruction rates has been paralleled by a 203 % increase in use of device-based reconstruction and is attributed to many factors.11 Most notably, increasing use of bilateral breast reconstruction has been implicated as a contributing factor.10 A basic query of our NSQIP national data demonstrates a near 50-fold increase from 2008 to 2012 of outpatient mastectomies with TE-based reconstruction (data not shown).
Because the unmatched cohorts of inpatients and outpatients undergoing TE were different, albeit slightly, in terms of ASA class, race, and previous cardiac surgery, we used propensity score matching to reduce these differences, ensuring a strict comparison in which neither inpatients nor outpatients began at a higher risk for experiencing an adverse outcome. After matching, we could not detect a bias toward either surgical setting with regard to minimizing postoperative morbidity. With regard to all 30-day complications and return to the OR, outpatient TE seemed to be at least as safe as inpatient TE in a properly selected group of patients. The surgical complication rate of outpatient TE patients in our study (4.3 %) compares well with the current literature.22 A single-institution study of 29 reconstructions on complications in the outpatient setting demonstrated a 3 % readmission rate and a 24 % overall complication rate.6 That our study had markedly lower rates of 30-day complications after outpatient TE may be explained by our significantly larger sample size. This study also lacked a control group by which to compare complication rates.
After matching, we found that rates of medical complications were higher in inpatient TE relative to outpatient, although the difference was not statistically significant. Medical morbidity such as deep vein thrombosis, pulmonary embolism, and UTI may be biased toward inpatient utilization.23 In our study, of the 3 aforementioned complications, both the incidences of pulmonary embolism, and UTI demonstrated a 0.3 % increase in inpatient relative to outpatient TE. Of note, graft failure, a NSQIP-capture outcome that has been used as a surrogate for implant loss and is regarded as a serious complication of TE’s, was not dissimilar between the 2 cohorts.12
Organ space SSI was the only surgical complication that was increased in outpatient TE. We hypothesize that the increased rate of infection can be explained by a trend toward limiting perioperative antibiotic prophylaxis, an initiative that has been shown to increase infection risk.24 The authors emphasize that upon multivariate analysis, outpatient TE did not independently confer increased risk of surgical complications relative to inpatient. As a whole, our findings suggest that outpatient TE is at least as safe as inpatient TE with respect to 30-day medical morbidity and that more aggressive and longer antibiotic prophylaxis may reduce the disparity in surgical infection risk.
Our study is the first to compare the safety of outpatient and inpatient TE in a multi-institutional national clinical registry. Our findings suggest that across all 30-day complications, TE performed in the outpatient setting is at least as safe as TE performed in the inpatient setting. Moreover, postoperative pain, a well-recognized factor that previously made outpatient reconstruction utilization less feasible, has been reduced with the development of local anesthesia infusion catheters.25,26 A review of the current literature suggests that outpatient pain control methods compare favorably to conventional anesthesia. This provides greater incentive to reduce the length of hospitalization of TE patients and thus reduce hospital costs as our studies suggest that safety and postoperative pain control may not need to play a large role in determining outpatient status.
Our findings must be interpreted in the context of its methodology and limitations. We matched inpatient and outpatient cohorts based on 21 baseline variables to balance pre-existing differences. The resulting bias toward outpatient TE as a safer procedure may be due to not only surgical setting but also any perioperative variables that were not matched, including intraoperative surgical findings that NSQIP does not capture, or patient socioeconomic factors that are not measured. In addition, we did not match the cohorts on the type of mastectomy that was performed (simple, partial with or without axillary lymphadenectomy, radical) because the relative proportions of inpatients and outpatients undergoing all mastectomy modalities were not significantly different. The relatively low proportion of patients who experienced such complications as renal failure, renal insufficiency, and stroke among others may suggest the lack of clinical relevance of certain tracked endpoints. NSQIP was designed for a broad spectrum of surgeries, reflected by the generic rather than surgery-specific outcomes that are captured. Namely, incidence of seroma and hematoma, or any appropriate surrogates, could not be compared between cohorts. A final limitation of the NSQIP database is its designation of inpatient and outpatient status. The inpatient label is commonly given to patients who stayed in the hospital for longer than 23 h regardless of initial determination and does not distinguish between same-day and overnight observation. In addition, some hospitals offer a 47-hour observation that is not recorded as “in-patient” even though patients are spending 1 or 2 nights in the hospital. While the interhospital variability in defining inpatient and outpatient status is a limitation of our study, we have demonstrated that outpatient TE-based reconstruction, which is associated with a shorter mean hospital stay by .77 days, is at least as safe as inpatient (1.06 vs. 1.83 days; p < .0001). An extrapolation of our findings suggests that hospital stays of 1 day may not confer increased risk of 30-days complications relative to longer stays. The ACS-NSQIP only captures the total length of hospital stays in days, as integers, rather than hours. Future interest will be paid to differentiate postoperative safety by hours of hospital stay to achieve more granular conclusions.
In conclusion, we have found that 30-day complication rates following outpatient TE compare well with previously benchmarked rates. Our studies suggest that outpatient TE is at least as safe as inpatient TE with regard to surgical and medical morbidity and return to the OR.
References
Warren JL, Riley GF, Potosky AL, Klabunde CN, Richter E, Ballard-Barbash R. Trends and outcomes of outpatient mastectomy in elderly women. J Natl Cancer Inst. 1998;90:833–40.
Case C, Johantgen M, Steiner C. Outpatient mastectomy: clinical, payer, and geographic influences. Health Serv Res. 2001;36:869–84.
Ferrante, J, Gonzalez E, Pal N, Roetzheim R. The use and outcomes of outpatient mastectomy in Florida. Am J Surg. 2000;179:253–9; discussion 259–60.
Kruper L, Xu XX, Henderson K, Bernstein L, Chen SL. Utilization of mastectomy and reconstruction in the outpatient setting. Ann Surg Oncol. 2013;20:828–35.
Bian J, Krontiras H, Allison H. Outpatient mastectomy and breast reconstructive surgery. Ann Surg Oncol. 2008;15:1032–9.
Simpson SA, Ying BL, Ross LA, et al. Incidence of complications in outpatient mastectomy with immediate reconstruction. J Am Coll Surg. 2007;205:463–7.
Xue DQ, Qian C, Yang L, Wang XF., Risk factors for surgical site infections after breast surgery: a systematic review and meta-analysis. Eur J Surg Oncol. 2012;38:375–81.
Shaikh-Naidu N, Preminger BA, Rogers K, Messina P, Gayle LB. Determinants of aesthetic satisfaction following TRAM and implant breast reconstruction. Ann Plast Surg. 2004;52:465–70; discussion 470.
Gurunluoglu R, Gurunluoglu A, Williams SA, Tebockhorst S. Current trends in breast reconstruction: survey of American Society of Plastic Surgeons 2010. Ann Plast Surg. 2013;70:103–10.
Cema, Y, Albornoz CR, Disa JJ, et al. A paradigm shift in U.S. breast reconstruction: Part 2. The influence of changing mastectomy patterns on reconstructive rate and method. Plast Reconstr Surg. 2013;131:320e–6e.
Albornoz CR, Albornoz CR, Disa JJ, et al. A paradigm shift in U.S. Breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013;131:15–23.
Fischer JP, Nelson JA, Serletti JM, Wu LC. Peri-operative risk factors associated with early tissue expander (TE) loss following immediate breast reconstruction (IBR): a review of 9305 patients from the 2005-2010 ACS-NSQIP datasets. J Plast Reconstr Aesthet Surg. 2013;66:1504–12.
Fischer JP, Wes AM, Tuggle CT 3rd, Serletti JM, Wu LC. Risk analysis of early implant loss after immediate breast reconstruction: a review of 14,585 patients. J Am Coll Surg. 2013;217:983–90.
Peled AW, Stover AC, Foster RD, McGrath MH, Hwang ES. Long-term reconstructive outcomes after expander-implant breast reconstruction with serious infectious or wound-healing complications. Ann Plast Surg. 2012;68:369–73.
Birkmeyer JD, Shahian DM, Dimick JB, et al. Blueprint for a new American College of Surgeons: National Surgical Quality Improvement Program. J Am Coll Surg. 2008;207:777–82.
Ingraham AM, Richards KE, Hall BL, Ko CY. Quality improvement in surgery: the American College of Surgeons National Surgical Quality Improvement Program approach. Adv Surg. 2010;44:251–67.
Austin PC. Some methods of propensity-score matching had superior performance to others: results of an empirical investigation and Monte Carlo simulations. Biom J. 2009;51:171–84.
Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 2011;10:150–61.
Austin PC. A comparison of 12 algorithms for matching on the propensity score. Stat Med. 2014;33:1057–69.
Merkow RP, Bilimoria KY, Hall BL. Interpretation of the C-statistic in the context of ACS-NSQIP models. Ann Surg Oncol. 2011;18 Suppl 3:S295; author reply S296.
Paul P, Pennell ML, Lemeshow S. Standardizing the power of the Hosmer-Lemeshow goodness of fit test in large data sets. Stat Med. 2013;32:67–80.
Washer LL, Gutowski K. Breast implant infections. Infect Dis Clin North Am. 2012;26:111–25.
Khavanin N, Mlodinow A, Kim JY, Ver Halen JP, Antony AK, Samant S. Assessing safety and outcomes in outpatient versus inpatient thyroidectomy using the NSQIP: a propensity score matched analysis of 16,370 patients. Ann Surg Oncol. 2015;22:429–36.
Clayton JL, Bazakas A, Lee CN, Hultman CS, Halvorson EG. Once is not enough: withholding postoperative prophylactic antibiotics in prosthetic breast reconstruction is associated with an increased risk of infection. Plast Reconstr Surg. 2012;130:495–502.
Lu L, Fine NA. The efficacy of continuous local anesthetic infiltration in breast surgery: reduction mammaplasty and reconstruction. Plast Reconstr Surg. 2005;115:1927–34; discussion 1935–6.
Pacik PT, Nelson CE, Werner C. Pain control in augmentation mammaplasty: safety and efficacy of indwelling catheters in 644 consecutive patients. Aesthet Surg J. 2008;28:279–84.
Ethical Approval
De-identified patient information is freely available to all institutional members who comply with the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) Data Use Agreement. The Data Use Agreement implements the protections afforded by the Health Insurance Portability and Accountability Act of 1996 and the ACS-NSQIP Hospital Participation Agreement and conforms to the Declaration of Helsinki.
Disclaimer
The NSQIP and the hospitals participating in the NSQIP are the source of the data used herein; they have not been verified and are not responsible for the statistical validity of the data analysis, or the conclusions derived by the authors of this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Charles Qin and Anuja K Antony are co-first authors.
Rights and permissions
About this article
Cite this article
Qin, C., Antony, A.K., Aggarwal, A. et al. Assessing Outcomes and Safety of Inpatient Versus Outpatient Tissue Expander Immediate Breast Reconstruction. Ann Surg Oncol 22, 3724–3729 (2015). https://doi.org/10.1245/s10434-015-4407-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4407-5