Abstract
Vardenafil hydrochloride is commonly used for the curing of erectile dysfunction. VAR suffers certain limitations: (i) short elimination half-life (4–5 h), (ii) low aqueous solubility (0.11 mg/mL), (iii) susceptibility to extensive first-pass metabolism and drug efflux transporters (p-glycoprotein), and (iv) limited (15%) oral bioavailability. The current study focused on the development of VAR lipomers as promising modified release systems able to enhance oral bioavailability. VAR-lipomers (lipid-polymer complexes) were successfully developed by a modified precipitation technique employing a lipid (polyglyceryl-6-distearate or glyceryl tristearate) and an amphiphilic polymer (Gantrez®). Three VAR:lipid ratios [1:1, 1:2, and 1:3] and three VAR:Gantrez® ratios [4:1, 2:1, and 1:1] were investigated. Solid-state characterization studies involved differential scanning calorimetry (DSC), X-ray diffraction (XRD), and Fourier-transform infrared (FT-IR) spectroscopy. The systems were assessed for particle size, polydispersity index (PDI), zeta-potential, VAR entrapment-efficiency (EE%), morphology, and VAR released % after 2 h (Q2h) and 8 h (Q8h). The best-achieved system (the highest desirability) was promoted for pharmacokinetic studies in fasted rabbits. Statistical analysis of data revealed that L9 system (PGDS, VAR, and Gantrez®; 3:1:1, respectively) had the highest desirability (0.85) with respect to spherical particle size (622.15 nm), PDI (0.11), zeta-potential (−27.90 mV), EE% (62.80%), Q2h (43.45%), and Q8h (77.40%). With respect to Levitra® tablets, the significantly higher relative bioavailability (170%), delayed Tmax, and extended MRT(0–∞) clarified the dual ability of L9 system. Lipomers are emerging systems capable of modifying the rate of VAR release and promoting its oral bioavailability.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
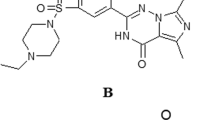
Vardenafil hydrochloride (VAR) is a selective cGMP-specific phosphodiesterase type-5 (PDE5) inhibitor which is commonly used in the curing of erectile dysfunction. VAR induces erection via smooth muscle relaxation and corporeal sinusoids dilatation in the presence of nitric oxide released after sexual arousal (1). Compared to sildenafil, VAR was revealed to be more potent (5–10 times) (1,2). VAR is one of the drugs classified as class II according to BCS (low solubility and high permeability). It possesses short half-life of 4–5 h as well as limited bioavailability (15%) following oral administration. The latter could be correlated to several factors, including; low aqueous solubility (0.11 mg/mL) and hindered intestinal absorption due to high susceptibility to many efflux transporters and first pass metabolism in the liver (CYP3A isozymes) (3,4). So, oral formulations of VAR are assumed to endeavor great challenges.
It is notable that different trials were attempted to overcome VAR’s limitations. In 2012, Sanford developed VAR orodispersible tablets (5). Fahmy aimed to surpass the oral bioavailability and patient compliance by preparing nano-ethosomal transdermal films of VAR (6). Berry et al. prepared VAR nebulizable inhalers to improve the onset of action and avoid the first pass metabolism (7). In our previous work, (8), PAMAM dendrimers of VAR were successfully developed as potential drug release modulators and oral bioavailability enhancers.
In the current work, lipomers (lipid polymer hybrid particles; LPHPs) were explored as another strategy to achieve the same goals for VAR. LPHPs, being mixtures of lipids and polymers, are emerging particulate systems combining the advantages of both components (9). Many studies confirmed the potential of LPHPs as modified-release drug carriers able to enhance the bioavailability, stability, and drug-targeting potential. In fact, these smart systems could maintain therapeutic drug-blood concentrations with minimum side effects (10,11,12).
Lipomers are particulate systems comprising of (i) an ionic polymer core responsible for the ionic complexation with the drug, enabling high entrapment efficiency, and (ii) a lipid coat (a physical barrier) responsible for modifying drug release kinetics via minimizing drug leakage and polymer erosion due to inward diffusion of water. Lipomers can be divided into two main categories: (i) monolithic matrix particles, where polymer-drug complex is homogeneously distributed in the lipid matrix and (ii) core-shell particles, where a lipid coat covers the polymer-drug complex (9). Unlike solid lipid nanoparticles (SLNs) and nanostructured lipid carriers (NLCs) which are mainly used for encapsulating hydrophobic drugs (13), lipomers are capable of entrapping various hydrophilic and hydrophobic drug candidates (9). Compared to liposomes, lipomers show better loading efficiency and stability.
Owing to their safety and non-immunogenicity, lipomers have been used recently in the fields of diagnostic imaging agents (14), vaccines (15), genetic materials (16), chemosensitizers, and anticancer drug-targeting (13,17,18,19). Guhagarkar et al. improved doxorubicin loading in polyethylene sebacate nanoparticles with the help of Gantrez® and use them for hepatic targeting (12). Passive targeting of doxycycline hydrochloride lipomers to the spleen was revealed by Devarajan et al. (20). Lymphatic targeting of orally administered doxorubicin nanocarriers showed a significant role in the field of cancer chemotherapy (10). The intravenous administration of doxycycline hydrochloride lipomers enhanced their reticuloendothelial system uptake (21,22).
In a parallel line, lipomers could enhance the oral bioavailability of VAR. Despite being an amphiphilic polymer, several studies revealed that the absorption of Gantrez®-containing systems is achieved via Peyer’s patches (23,24,25). Interestingly, like other hydrophobic particles (26,27), it could be expected that lipomers bypass the first pass metabolism via their uptake through Peyer’s patches, thereby improving the oral VAR bioavailability. Benival and Devarajan reported the enhancement of the oral bioavailability of doxorubicin via lipomers prepared with Gantrez® and utilizing magnesium acetate as a crosslinking agent (10).
In view of the aforementioned, lipomers were designed using a lipid; polyglyceryl-6-distearate or glyceryl tristearate along with an anionic hydrophilic polymer; Gantrez®. Three VAR:lipid ratios [1:1, 1:2, and 1:3] and three VAR:Gantrez® ratios [4:1, 2:1, and 1:1] were investigated. Based on the in vitro characterization studies, the pharmacokinetic parameters of the best achieved system (having the highest desirability value) were assessed in fasted rabbits; relative to an aqueous suspension of crushed Levitra® tablets.
MATERIALS AND METHODS
Materials
VAR and sildenafil citrate (SIL; internal standard) were kindly provided by Marcyrl Pharmaceutical Industries (Cairo, Egypt) and Evapharm (Giza, Egypt), respectively. Plurol Stearique® WL 1009 (polyglyceryl-6-distearate; PGDS) was donated by Gattefosse (Saint-Priest, France). Gantrez® AN119 (poly-methyl vinyl ether-co-maleic anhydride) was a kind gift from Anshul Agencies (Mumbai, India). Glyceryl tristearate (GTS), tert-butyl methyl ether, acetonitrile (HPLC grade), and formic acid (HPLC grade) were acquired from Sigma-Aldrich® (St. Louis, MO). Magnesium acetate tetrahydrate was procured from Acros Organics (Geel, Belgium). Dibasic sodium phosphate, hydrochloric acid, and acetone were supplied by El-Nasr Pharmaceutical Chemicals Co. (Cairo, Egypt). Semi-permeable membrane tubing was purchased from Spectrum Laboratories Inc., (Spectra Por© M. Wt cut off 12,000–14,000, Rancho Dominguez, CA). Other chemicals (analytical grade) were utilized as received.
Design of VAR Lipomer Systems
Eighteen VAR lipomers comprising (i) PGDS or GTS as a lipid, (ii) Gantrez® as a negatively charged polymer, and (iii) magnesium acetate as a crosslinking agent were successfully prepared using a modified precipitation technique (10,12). The composition of the developed lipomer systems is shown in Table I.
Briefly, the organic phase was prepared by dissolving the lipid along with the polymer in acetone. This organic phase was dropped into a solution of VAR (0.1 mg/mL) in deionized water with magnetic stirring (1000 rpm) at room temperature (25 ± 1 °C). Crosslinking of Gantrez® was achieved via the incorporation of magnesium acetate aqueous solution (0.5% w/v) to the latter dispersion (10,12,22). The dispersion was finally probe sonicated for 5 min (2 s on/2 s off) at 200 V (Cole-Parmer, IL, USA) over an ice bath and left overnight under magnetic stirring (1000 rpm) to allow complete evaporation of the organic solvent (28). The lipomers were concentrated with a rotary evaporator (Heidolph VV 2000, Burladingen, Germany)—working at a speed of 90 rpm and a temperature of 60 °C—so that a final VAR concentration of 1 mg/mL is achieved. The obtained dispersion was re-sonicated for 1 min (as previously noted) to enhance the development of a fine lipomer dispersion.
In vitro Characterization of VAR-lipome Complexes
A representative lipomer system (L9) and its corresponding lipid-free VAR-Gantrez® complex were developed, frozen, and lyophilized for 24 h (−45 °C, 7 × 10−2) mbar (Novalyphe-NL 500 lyophilizer; Savant Instruments; NY, USA). The lyophilized systems passed through the following solid-state investigations.
Fourier-transform Infrared Spectroscopy
FT-IR studies were performed to verify the possible chemical intermolecular interactions between cationic VAR and anionic Gantrez®. The FT-IR spectral analysis of VAR, Gantrez®, VAR-Gantrez® physical mixture, and lipid-free VAR-Gantrez® complex were performed over the spectrum of 4000 to 400 cm−1, as per the potassium bromide disc technique, using Affinity-1 spectrophotometer (Shimadzu, Kyoto, Japan) (29).
Differential Scanning Calorimetry Studies
DSC studies were conducted to assess the possible conversion of the drug into the amorphous state in the investigated lipomer system. DSC thermograms of VAR, Gantrez®, PGDS, magnesium acetate, their physical mixture, and the lipomer system were assessed (DSC-60 Shimadzu, Kyoto, Japan) using indium as reference. The samples (4 mg) were heated from 30 to 300 °C at a constant heating rate (10 °C/min) in hermetically sealed flat aluminum pans; under nitrogen atmosphere flowing at 30 mL/min.
Powder X-ray Diffraction Studies
To confirm the results of the latter studies, PXRD patterns of similar samples to those employed in DSC studies were performed at room temperature (PANalytical X’Pert PRO diffractometer; Almelo, Netherlands) employing nickel-filtered Cu Kα radiation (λ = 1.542 Å, 45 kV, and 35 mA). The results were reported as intensity versus 2θ (2–60°) (30).
In vitro Characterization of VAR-lipomer Dispersions
Particle Size and Zeta Potential Analysis
Dynamic light scattering technology was adopted to measure the mean particle size and polydispersity index (PDI) of the VAR lipomers using Zetasizer Nano ZS at 25 °C (Malvern instruments; Worcestershine, UK). Diluted dispersions (ten times) with deionized water were used to obtain an appropriate scattering intensity. Low PDI values indicate homogenous particle size distribution (31).The electrophoretic mobility of the charged vesicles was observed using a laser doppler anemometer connected to the Zetasizer Nano ZS to determine the zeta potential (ζ) values.
Surface Morphology Examination via Transmission Electron Microscopy
The topographic characteristics of the individual particles in a representative lipomer system (L9) were examined with (TEM) transmission electron microscopy via staining with phosphotungestic acid. A dispersion drop was placed onto copper grids (carbon coated) then a drop of (2%, w/v) phosphotungestic acid solution was added. After the drainage of excess liquid, grids were air-dried and examined under Joel JEM 1230 TEM (Tokyo, Japan) at 80 kV voltage.
Estimation of VAR Entrapment Efficiency Percentages
The EE% of VAR lipomers was calculated by evaluating the unentrapped drug concentration after centrifuging the dispersions at 15,000 rpm (1 h; 4 °C) (Heraeus Megafuge 1.0 R; Hanau, Germany) (10,12,22). Free VAR was assessed spectrophotometrically at a wavelength of 250 nm (32) (Shimadzu UV-1601 PC; Kyoto, Japan) after diluting the clear supernatant.
The EE percentages were calculated using the equation;
In vitro VAR Release Studies
In vitro release studies of an aqueous VAR suspension and VAR lipomers were determined in a type II USP dissolution apparatus (VK 7000, Vankel Industries, Inc., NJ, USA) via the dialysis bag method (29) at 50 rpm. In the first 2 h, 500 ml 0.1 N HCl (pH 1.2) was set as the release media. Then the medium pH was raised to 6.8 by adding 400 ml 0.235 M dibasic sodium phosphate solution (33).
Briefly, aliquot samples of lipomer dispersions were filled and sealed from both sides in semi-permeable membrane tubing (Spectra Por©) and then immersed into the preheated (37 ± 0.5 °C) media. Aliquots of the release media were removed at set time points to plot the drug release patterns; VAR released percentages VS time. To maintain a constant volume, an equal volume of fresh medium was replaced at once (8). The percentage drug released after 2 h (Q2h) and 8 h (Q8h) were assessed.
In vivo Estimation of VAR Pharmacokinetics in Rabbits
Study Design
The in vivo study was performed in accordance with EU Directive 2010/63/EU for animal experiments to compare the pharmacokinetics of VAR after the peroral administration of the test treatment (the best achieved VAR lipomer system; L9) and the reference treatment (crushed Levitra® 20 mg tablets, Bayer HealthCare AG, Germany) in rabbits. Both treatments were administered at 5 mg/kg doses to fasted rabbits following a randomized, parallel, non-blind design. According to Bischoff et al., rabbits can well tolerate VAR doses up to 30 mg/kg (34). The experimental design was accepted (PI–1890) by the Research Ethics Committee at the Faculty of Pharmacy Cairo University, Cairo, Egypt.
Animals
Healthy male New Zealand albino rabbits (1.8–2 kg each) were accommodated under well-defined environmental conditions in separate cages at suitable temperature (25 ± 1 °C), ventilation (15–20 AC/ h), humidity (50%), and light (12 h light/12 h dark cycle). Rabbits were fed standard diets and had free access to water.
Administration of Treatments and Blood Collection
Randomly, the rabbits were allocated to two different groups (5 rabbits each). The first group received an aqueous suspension of crushed Levitra® tablets as the reference treatment (35). Meanwhile, the rabbits in the second group got the test treatment as VAR lipomer dispersion (L9). Both treatments were given via oral gavage.
Blood samples from the cannulated right ear vein were withdrawn at 0 (pre-dose), 0.33, 0.66, 1, 1.5, 2, 4, 6, 9, 12, and 24 h after drug administration and transferred into treated glass tubes (heparinized). Clear plasma samples, derived by centrifugation (Hettich; Germany) at 5000 rpm for 5 min, were transferred to glass tubes and frozen at −20 °C until analysis of the drug.
The preparation (36) and analysis of VAR in rabbit plasma samples via LC-MS/MS (37) was conducted as previously reported in our previous work (8). Briefly, the plasma concentrations of VAR were determined using a triple quadrupole LC-MS/MS mass spectrometer (MDS Sciex, Foster City, CA). Mass analysis was conducted in +ve ion-multiple reaction monitoring mode using an electrospray ionization source (ESI). Sildenafil hydrochloride (SIL) was used as an internal standard. An Agilent column (C18; 50 cm × 4.6 mm) with a particle size of 5 μm (Agilent, USA) was used. A mobile phase consisting of a mixture of acetonitrile: 0.1% formic acid (70%:30%) were was used for peak separation at a flow rate of 1 mL/min. The M/Z ratios were 489.091/151.100 for VAR and 475.194/58.100 for SIL. Under the investigated condition, the retention times of VAR and SIL peaks were 0.76 and 0.79 min, respectively (8).
Pharmacokinetic and Statistical Analysis
The mean plasma concentration-time curves of VAR (± SD) in the rabbit plasma were plotted. A non-compartmental analysis was adopted (38), using WinNonlin® software Ver. 1.5, to estimate the pharmacokinetic parameters; (Cmax, ng/mL) the maximum plasma concentration of VAR, (Tmax, h) the time to reach Cmax, (MRT(0–∞), h) the mean residence time from zero to infinity, (Tel, h) the elimination half-life, AUC(0–24h), (ng.h/mL) the area under the curve from zero to the last sampling point and AUC(0–∞), (ng.h/mL) from zero to infinity. The derived pharmacokinetic parameters (at P value < 0.05) were analyzed via one-way analysis of variance (SPSS 14.0, SPSS Inc., Chicago, USA). The relative bioavailability percentage was estimated from AUC(0–∞) values of both treatments (8).
RESULTS AND DISCUSSION
Development of VAR Lipomers by a Modified Precipitation Technique
VAR lipomers were successfully developed via a modified precipitation technique using different combinations and concentrations of VAR, Gantrez® and lipid (PGDS or GTS). Owing to VAR’s limited aqueous solubility (0.11 mg/mL), a large volume of deionized water was used to dissolve VAR and ensure its complete ionization. Compared to water; acetone has low surface tension (25.20 J/m2 versus 71.98 J/m2). This causes high interfacial turbulence and consequently, facilitates fast diffusion of the organic phase upon dropping into the aqueous phase. This process resulting in; (i) rapid precipitation of the lipid, (ii) hydrolysis of the Gantrez® anhydride groups instantly and simultaneous exposure of the negatively charged carboxylate groups, (iii) formation of ionic VAR-Gantrez® complexes due to the interaction with the protonated amine groups of VAR, and (iv) rapid partitioning and entrapping of VAR-Gantrez® complex into the resulting lipid matrices. A similar mechanism was proposed by Benival & Devarajan to describe the development of doxorubicin hydrochloride lipomers (10). Magnesium acetate was incorporated as a stabilizing agent due to its role in crosslinking Gantrez® (10,12,22,39).
In Vitro Characterization of VAR-lipomer Complexes
Fourier-transform Infrared Spectroscopy
The FT-IR absorption spectra of VAR (a), Gantrez® (b), VAR-Gantrez® physical mixture (c), and lipid-free VAR-Gantrez® complex (d) were scanned to scrutinize the probable intermolecular interactions between cationic VAR and anionic Gantrez® (Fig. 1). As noted and graphed in our previous work (8), the characteristic IR peaks of VAR were C–N (719.45 cm−1), C–O (1156.36 cm−1), –C–H and HC=CH aryl (1332.81 cm−1, 1490.97 cm−1 & 1598.99 cm−1), C=O (1724.36 cm−1), CH2 and C–H (alkyl) (3039.81 cm−1, 2968.45 cm−1& 2937.58 cm−1), and N–H (3398.57 cm−1) (1). The spectral analysis of the IR peaks of Gantrez® revealed the presence of C–O (1095.43 cm−1, 1193.36 cm−1 & 1224.16 cm−1), C=O (1780.46 cm−1 & 1732.16 cm−1) and CH2 and C-H alkyl (2841.15 cm−1, 2748.56 cm−1 & 2619.58 cm−1). The characteristic peaks of VAR and Gantrez® were revealed in the IR spectrum of VAR-Gantrez® physical mixture. On the other hand, the changing in the shape and intensity of some peaks, the vanishing of the peaks corresponding to NH3+ stretching vibrations of VAR at 2449.60 cm−1, 1851.66 cm−1 and 1778.37 cm−1 and the formation of new peaks at 2924.09 cm−1 and 2854.65 cm−1 in the IR spectrum of the VAR-Gantrez® complex could evidence the presence of certain hydrophobic and electrostatic intermolecular interactions between VAR (the protonated amine groups) and Gantrez® (the free carboxyl groups).
Differential Scanning Calorimetry (DSC) Studies
The DSC thermograms of VAR (a), Gantrez® (b), PGDS (c), magnesium acetate (d), their physical mixture (e), and VAR lipomer system (f) are illustrated in Fig. 2A VAR is a typical crystalline material as represented by a sharp endothermic peak at 215 °C (melting point) (1,40). The DSC thermograms of Gantrez®, PGDS and magnesium acetate revealed respective endothermic peaks at 160 °C, 58 °C and 80 °C (melting points). The existence of the specific endothermic peak of VAR in the DSC thermogram of the physical mixture and its disappearance in that of VAR lipomer system could indicate a decrease in drug crystallinity and/or a change into the amorphous state upon complexation with Gantrez®.
Powder X-ray Diffraction Studies
PXRD were considered as complement studies which could support the findings of DSC analysis. In this context, the powder X-ray diffractograms of similar samples were illustrated in Fig. 2B. The drug revealed many sharp, high-intensity peaks at 2θ (6.782, 6.994 & 7.770) confirming its crystalline nature. In fact, the vanishing of these peaks in the diffractogram of the lipomer system stands for the change of VAR into the amorphous or molecular state.
In vitro Characterization of VAR-lipomer Dispersions
Particle Size and Zeta Potential Analysis
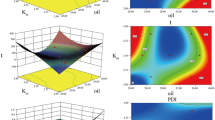
The mean particle size of the developed lipomers ranged from 497.11 nm (L3) to 2873.53 nm (L16) (Table I). The statistical analysis (ANOVA) of data confirmed that the particle size of the developed lipomers is significantly influenced by (i) lipid type (P < 0.0001), (ii) VAR: lipid ratio (P < 0.0001), and (iii) VAR: Gantrez® ratio (P < 0.0001).
Glyceryl tristearate-based lipomers were significantly bigger in size (P < 0.0001) than the corresponding polyglyceryl distearate-based ones. This might be attributed to the addition of more alkyl chains into the domains of the particles leading to size enlargement.
At a fixed VAR: Gantrez® ratio, a direct correlation could be prevailed between the lipid concentration and the particle size. This significant (P < 0.0001) link was held true within each lipid series. Lipomer systems containing the highest lipid content (30 mg) were larger in size than other systems comprising lower lipid contents. Higher mass transfer resistance, due to the increased viscosity of the organic phase, is probably one rationale for the formation of larger particles (22,41). In a parallel line, the higher viscosity of the resulting lipomer dispersion could be another contributing factor since it might decrease the efficiency of sonication and consequently, increase the particle aggregation rate.
At a fixed VAR: lipid ratio, the Gantrez® concentration had significant (P < 0.0001) negative influence on the particle size within each lipid series. These findings were in harmony with those recorded by Benival and Devarajan (10) and Guhagarkar et al. (12). Gantrez® has an amphiphilic nature (surfactant properties). Incorporation of higher Gantrez® ratios might be the reason for the higher emulsification potential. As noted by Tadros and Al-Mahallawi, the utilization of relatively insufficient surfactant concentrations would trigger the aggregation of fine particles to decrease the surface area so that the surfactant concentration can coat the total agglomerate surface (42). The later dispersions would have relatively larger particles and exhibit broad particle size distributions (PDI values > 0.3).
The freshly prepared lipomer dispersions bore negative zeta potential values varying from −16.60 mV (L4) to −27.90 mV (L8 & L9) as presented in Table I. The statistical analysis (ANOVA) of data confirmed that these values are significantly influenced by the lipid type (P = 0.0298). In fact, the VAR: lipid ratio and VAR: Gantrez® ratio showed (P > 0.05) non-significant impacts on the magnitude of the zeta potential values.
Systems having values close to −30 mV are expected to experience good stability and low tendency towards aggregation owing to the strong static repulsion between the particles. A part of these negative charges could be correlated to the carboxylate groups found in stearate-based lipids and Gantrez® which is a copolymer of methyl vinyl ether and maleic anhydride.
Morphological Examination
Transmission electron micrographs of a representative lipomer system (L9) revealed the presence of well-identified, non-aggregated spherical particles having an approximate size of 600–700 nm (Fig. 3). It is worth to note that the observed size range matches well with the Z-average diameter obtained by quasi-elastic light scattering (Table I). As evidenced by zeta potential assessments, repulsion between the negatively charged surfaces could be the reason behind the non-aggregation of the particles (Table I).
Estimation of VAR Entrapment Efficiency Percentages
VAR-EE% denotes for the percentage of the entrapped VAR within the lipomers compared to the initially added amount. As shown in Table I, the mean EE% varied from 51.53% (L3) to 75.30% (L14). ANOVA results confirmed the significant influence of the lipid type, VAR:lipid ratio and VAR:Gantrez® ratio on VAR-EE%.
Glyceryl tristearate-based lipomers showed significantly (P < 0.0001) higher EE% than the corresponding polyglyceryl distearate-based ones. This higher EE% could be referred to the difference in the composition of both lipids, where increasing the number of the alkyl chains in the former systems results in higher lipophilicity and consequently, promotes the entrapment of poorly water-soluble drugs like VAR. In a parallel line, polyglyceryl distearate possesses greater number of hydroxyl groups and this would increase the system polarity and, hence, lowers its ability towards entrapment of VAR (43).
These suggestions were in a close agreement with those presented by Li et al., who observed that poorly water-soluble drugs showed better loading in triglyceride-based systems owing to their reduced polarity (11). On contrary, highly water-soluble drugs were preferentially entrapped in glyceryl monostearate-based lipomers than in glyceryl distearate-or in glyceryl tristearate-based ones since glyceryl monostearate is the most hydrophilic lipid with respect to the investigated ones (22).
A significant improvement (P = 0.0066) in VAR-EE% was observed upon increasing the lipid content in the system; shifting the VAR:lipid ratio from 1:1 to 1:2. These findings could be explained in the light of the increased viscosity of the dispersions and, consequently, the development of larger particles which would have higher ability to entrap more drug. Needless to say, thicker lipid matrices would act as better shields; favoring the incorporation and partitioning of VAR-Gantrez® complexes (9). Non-significant (P > 0.05) changes in VAR-EE% were observed upon shifting the VAR:lipid ratio from 1:2 to 1:3.
Gantrez®, an anionic amphiphilic copolymer, was incorporated to promote VAR entrapment in the lipomers via ionic complexation with the cationic amine groups of VAR. A significant (P < 0.0001) improvement in VAR-EE% was observed upon increasing Gantrez® ratio in the system; shifting the VAR: Gantrez® ratio from 4:1 to 2:1. This could be related to the provision of extra carboxylate groups available for interaction with a fixed number of cationic amine groups. Unexpectedly, a significant decrease in VAR-EE% was noted at VAR:Gantrez® ratio of 1:1. A similar attitude was elaborated by Benival and Devarajan (10). This was related to the negative impact of higher Gantrez® concentrations on particle size to a manner that hinders VAR-EE% (44).
In vitro VAR Release Studies
The in vitro VAR release profiles of PGDS-based lipomer systems (L1-L9) and GTS-based ones (L10-L18), in comparison to an aqueous VAR suspension, are displayed in Fig. 4A, B, respectively. The release profile discriminators; Q2h and Q8h are summarized in Table I.
a In vitro release profiles of VAR aqueous suspension and PGDS-based VAR lipomer systems in 0.1 N HCl (pH 1.2, 2 h) and in phosphate buffer (pH 6.8, 6 h) at 37 ± 0.5 °C (mean ± S.D., n = 3). b In vitro release profiles of VAR aqueous suspension and GTS-based VAR lipomer systems in 0.1 N HCl (pH 1.2, 2 h) and in phosphate buffer (pH 6.8, 6 h) at 37 ± 0.5 °C (mean ± S.D., n = 3)
The release of VAR was almost complete from its aqueous suspension within 5 h; the dialysis membrane did not restrain VAR diffusion (8). On the other hand, more retarded biphasic drug release profiles were attained with VAR LPHPs. They were characterized by a phase of fast drug release (first 2 h) in the acidic medium (pH 1.2), then a phase of slow drug release (until the termination of the release studies) in the simulated intestinal medium (pH 6.8). As noted in our previous work (8), reasonable Q2h (35–40%) and high Qlast (70–80%) were targeted to achieve modified drug release profiles able to effectively initiate and maintain prolonged VAR effect. The release of the un-entrapped and/or the surface adsorbed VAR could be the reason for the initial drug release phase. Moreover, the favorable solubility of VAR in 0.1 N HCl (65 mg/mL) should also be considered (8). On the other hand, the subsequent more prolonged drug release profiles could be related to the liberation of VAR from VAR-Gantrez® complex and subsequent, diffusion via the lipid matrix (45). Comparable results were reported for several drug-loaded lipomers. Doxorubicin lipomers exhibited sustained release profiles owing to the presence of a lipid matrix (10,12). Similarly, the embedding of verapamil hydrochloride-dextran sulfate complex in a lipid matrix delayed the rate of drug diffusion (46). It was suggested that lipid coating delay the rate of drug release via retarding the diffusion of the drug into the dissolution medium (9).
GTS-based lipomers showed significantly slower drug release profiles (Q2h; P = 0.0462 and Q8h; P = 0.0004) than the corresponding PGDS-based ones. GTS (C57H11006; MW:891.48, log P:25.2) has a higher molecular weight and is more lipophilic than PGDS (C45H8809; MW:773.19, log P:14.7) due to inserting longer alky chains. In fact, the positive contribution of the particle size on delaying the rate of drug release of lipomer systems should not be neglected. However, non-significant differences in the drug release profiles (P > 0.05) were noticed by altering VAR: lipid ratio or VAR:Gantrez® ratio.
The differences in Q2h and Q8h could be explained with respect to Gantrez® concentration, and VAR-EE%. As noted earlier, shifting the VAR:Gantrez® ratio from 4:1 to 2:1in PGDS-based lipomers, improved VAR-EE% and consequently, more prolonged drug release profiles were observed. However, a decrease in VAR-EE% was observed at a VAR: Gantrez® ratio of 1:1 and, hence, faster drug release profiles were attained. In harmony with the assumptions of Muller et al., the entrapping of higher drug percentages is expected to slow down the drug release rates (45). In GTS-based lipomers, an inverse correlation was noted between the concentration of Gantrez® and the discriminators of the release profile. Increasing the Gantrez® concentration promotes the generation of more ionic complexes with VAR and hence, more delayed release profiles of VAR were achieved (46).
The best achieved system was derived, via Design-Expert® software, by correlating constraints to both; the dependent responses and the independent variables (lipid type, VAR:lipid ratio and VAR:Gantrez® ratio). The set criteria for the best achieved system were; small particle size, narrow particle size distribution, high zeta potential values, high VAR-EE%, reasonable Q2h and high Q8h. The desirability values were calculated and sorted in a descending order. The highest desirability value (0.85) was attained with one lipomer system (L9) composed of PGDS, VAR and Gantrez® at a respective ratio of 3:1:1. This system was promoted for further pharmacokinetic studies in rabbits.
VAR Pharmacokinetics in Rabbits
The VAR plasma concentrations vs time curves after the oral administration (5 mg/kg doses) of the reference treatment and the test treatment in fasted rabbits are illustrated in Fig. 5. The estimated pharmacokinetic parameters are summarized in Table II.
The statistical significances between the two treatments were detected by comparing their pharmacokinetic parameters. As noted and graphed in our previous work (8), Levitra® tablets were rapidly absorbed with a maximum VAR concentration of 504.80 ± 157.49 ng/mL at a Tmax of 1.5 h (median: 1–2 h). Following the oral administration of lipomers (L9), the mean Cmax (346.74 ± 67.68) ng/mL was attained at a Tmax of 2 h (median: 2–4 h). It is worth to note that VAR plasma concentrations declined in a slower manner than those values of the reference treatment. Significant differences were detected between the mean Cmax values of both treatments (P < 0.01).
The modified release characteristics of L9 system could be concluded from the significant delay (P < 0.01) in the median Tmax (from 1.5 h to 2 h) as well as the significant (P < 0.01) elongation in the MRT(0–∞) (from 5.02 h to 11.37 h) and in the elimination half-life (from 5.95 h to 8.17 h).
Compared to Levitra® tablets, a (P < 0.01) statistically significant improvement in the oral bioavailability of VAR was noted following oral administration of L9 system. The relative bioavailability was 150.80% [comparing the estimated mean AUC(0–24h) values of 1766.91 ng∙h/mL (reference) VS 2664.84 ng∙h/mL (test)] and 170.50% [comparing the mean AUC(0–∞) values of 1846.14 ng∙h/mL (reference) VS 3147.49 ng∙h/mL (test)]. The significant improvement in the relative oral bioavailability of VAR could be correlated to (i) establishing of a drug concentration gradient towards the absorption site (25), and (ii) bypassing the first pass metabolism in the liver via lymphatic uptake through Peyer’s patches (23,24,25).
CONCLUSIONS
VAR lipomers were successfully developed by a modified precipitation technique via the ionic interaction between the cationic drug (VAR) and the anionic polymer (Gantrez®) and the incorporation of this complex in a lipid matrix (PGDS). At an optimum PGDS:VAR:Gantrez® ratio of 3:1:1 (L9 system), the highest system desirability (0.85) was achieved considering the particle size, zeta-potential, PDI, EE%, Q2h and Q8h. Compared to Levitra® tablets, the pharmacokinetic studies in rabbits confirmed the potential of L9 system as a dual platform capable of improving the oral bioavailability and modifying the rate of drug release to initiate and maintain VAR response for a prolonged period.
References
Ashour AE, Motiur Rahman AFM, Kassem MG. Vardenafil dihydrochloride. In: Brittain HG, editor. Profiles of drug substances, excipients and related methodology. San Diego: Academic Press; 2014. p. 515–44.
Keating GM, Scott LJ. Vardenafil: a review of its use in erectile dysfunction. Drugs. 2003;63(23):2673–703.
Choi MK, Song IS. Characterization of efflux transport of the PDE5 inhibitors, vardenafil and sildenafil. J Pharm Pharmacol. 2012;64(8):1074–83.
Moffat AC, Osselton MD, Widdop B. Clarke’s analysis of drugs and poisons. 4th ed. London: The Pharmaceutical Press; 2011.
Sanford M. Vardenafil orodispersible tablet. Drugs. 2012;72(1):87–98.
Fahmy U. Nanoethosomal transdermal delivery of vardenafil for treatment of erectile dysfunction: optimization, characterization, and in vivo evaluation. Drug Des Devel Ther. 2015;9:6129–37.
Berry B, Altman P, Rowe J, Vaisman J. Comparison of pharmacokinetics of vardenafil administered using an ultrasonic nebulizer for inhalation vs a single 10-mg oral tablet. J Sex Med. 2016;13(7):1111–8.
Tawfik MA, Tadros MI, Mohamed MI. Polyamidoamine (PAMAM) dendrimers as potential release modulators and oral bioavailability enhancers of vardenafil hydrochloride. Pharm Dev Technol. 2018;21:1–10.
Wu XY. Strategies for optimizing polymer-lipid hybrid nanoparticle-mediated drug delivery. Expert Opin Drug Deliv. 2016;13(5):609–12.
Benival DM, Devarajan PV. Lipomer of doxorubicin hydrochloride for enhanced oral bioavailability. Int J Pharm. 2012;423(2):554–61.
Li Y, Taulier N, Rauth AM, Wu XY. Screening of lipid carriers and characterization of drug-polymer-lipid interactions for the rational design of polymer-lipid hybrid nanoparticles (PLN). Pharm Res. 2006;23(8):1877–87.
Guhagarkar SA, Gaikwad RV, Samad A, Malshe VC, Devarajan PV. Polyethylene sebacate-doxorubicin nanoparticles for hepatic targeting. Int J Pharm. 2010;401(1–2):113–22.
Wong HL, Bendayan R, Rauth AM, Wu XY. Development of solid lipid nanoparticles containing ionically complexed chemotherapeutic drugs and chemosensitizers. J Pharm Sci. 2004;93(8):1993–2004.
Mieszawska AJ, Gianella A, Cormode DP, Zhao Y, Meijerink A, Langer R, et al. Engineering of lipid-coated PLGA nanoparticles with a tunable payload of diagnostically active nanocrystals for medical imaging. Chem Commun (Camb). 2012;48(47):5835–7.
Moon JJ, Suh H, Polhemus ME, Ockenhouse CF, Yadava A, Irvine DJ. Antigen-displaying lipid-enveloped PLGA nanoparticles as delivery agents for a plasmodium vivax malaria vaccine. PLoS One. 2012;7(2):e31472.
Li J, He Y, Li W, Shen Y, Li Y, Wang Y. A novel polymer-lipid hybrid nanoparticle for efficient nonviral gene delivery. Acta Pharmacol Sin. 2010;31(4):509–14.
Wong HL, Rauth AM, Bendayan R, Manias JL, Ramaswamy M, Liu Z, et al. A new polymer-lipid hybrid nanoparticle system increases cytotoxicity of doxorubicin against multidrug-resistant human breast cancer cells. Pharm Res. 2006;23(7):1574–85.
Wong HL, Rauth AM, Bendayan R, Wu XY. In vivo evaluation of a new polymer-lipid hybrid nanoparticle (PLN) formulation of doxorubicin in a murine solid tumor model. Eur J Pharm Biopharm. 2007;65(3):300–8.
Wong HL, Bendayan R, Rauth AM, Xue HY, Babakhanian K, Wu XY. A mechanistic study of enhanced doxorubicin uptake and retention in multidrug resistant breast cancer cells using a polymer-lipid hybrid nanoparticle system. J Pharmacol Exp Ther. 2006;317(3):1372–81.
Devarajan PV, Jindal AB, Patil RR, Mulla F, Gaikwad RV, Samad A. Particle shape: a new design parameter for passive targeting in splenotropic drug delivery. Int J Pharm. 2010;99(6):2576–81.
Patil RR, Guhagarkar SA, Devarajan PV. Engineered nanocarriers of doxorubicin: a current update. Crit Rev Ther Drug Carrier Syst. 2008;25(1):1–61.
Patil RR, Gaikwad RV, Samad A, Devarajan PV. Role of lipids in enhancing splenic uptake of polymer-lipid (LIPOMER) nanoparticles. J Biomed Nanotechnol. 2008;4(3):359–66.
Salman HH, Gamazo C, De Smidt PC, Russell-Jones G, Irache JM. Evaluation of bioadhesive capacity and immunoadjuvant properties of vitamin B12-Gantrez nanoparticles. Pharm Res. 2008;25(12):2859–68.
Salman HH, Gamazo C, Campanero MA, Irache JM. Salmonella-like bioadhesive nanoparticles. J Control Release. 2005;106:1–2):1–13.
Salman HH, Gamazo C, Campanero MA, Irache JM. Bioadhesive mannosylated nanoparticles for oral drug delivery. J Nanosci Nanotechnol. 2006;6(9–10):3203–9.
Bargoni A, Cavalli R, Zara GP, Fundarò A, Caputo O, Gasco MR. Transmucosal transport of tobramycin incorporated in solid lipid nanoparticles (SLN) after duodenal administration to rats. Part II-tissue distribution. Pharmacol Res. 2001;43(5):497–502.
Eldridge JH, Hammond CJ, Meulbroek JA, Staas JK, Gilley RM, Tice TR. Controlled vaccine release in the gut-associated lymphoid tissues. I. Orally administered biodegradable microspheres target the peyer’s patches. J Control Release. 1990;11(1–3):205–14.
Vandamme TF, Ngombo Mukendi JF. Controlled release of levamisole from poly-(ε-caprolactone) matrices II. Effects of water-soluble polymer and iron powder incorporated into the matrices. Int J Pharm. 1996;132:153–63.
Tayel SA, El-Nabarawi MA, Tadros MI, Abd-Elsalam WH. Duodenum-triggered delivery of pravastatin sodium: II. Design, appraisal and pharmacokinetic assessments of enteric surface-decorated nanocubosomal dispersions. Drug Deliv. 2016;23(9):3266–78.
Abd-Elbary A, Tadros MI, Alaa-Eldin AA. Sucrose stearate-enriched lipid matrix tablets of etodolac: modulation of drug release, diffusional modeling and structure elucidation studies. AAPS PharmSciTech. 2013;14(2):656–68.
Dragicevic-Curic N, Scheglmann D, Albrecht V, Fahr A. Development of different temoporfin-loaded invasomes-novel nanocarriers of temoporfin: characterization, stability and in vitro skin penetration studies. Colloids Surf B Biointerfaces. 2009;70(2):198–206.
Lee HM, Kim CS, Jang YM, Kwon SW, Lee BJ. Separation and structural elucidation of a novel analogue of vardenafil included as an adulterant in a dietary supplement by liquid chromatography-electrospray ionization mass spectrometry, infrared spectroscopy and nuclear magnetic resonance spectroscopy. J Pharm Biomed Anal. 2011;54(3):491–6.
The United States Pharmacopeial Convention. United States Pharmacopeia (USP 36) and National Formulary (NF 31) (Omeprazole delayed release capsules). Rockville, MD; 2013.
Bischoff E, Niewoehner U, Haning H, Es Sayed M, Schenke T, Schlemmer KH. The oral efficacy of vardenafil hydrochloride for inducing penile erection in a conscious rabbit model. J Urol. 2001;165(4):1316–8.
Hosny KM, Aljaeid BM. Sildenafil citrate as oral solid lipid nanoparticles: a novel formula with higher bioavailability and sustained action for treatment of erectile dysfunction. Expert Opin Drug Deliv. 2014;11(7):1015–22.
Lake ST, Altman PM, Vaisman J, Addison RS. Validated LC-MS/MS assay for the quantitative determination of vardenafil in human plasma and its application to a pharmacokinetic study. Biomed Chromatogr. 2010;24(8):846–51.
Johnson RD, Lewis RJ, Angier MK. The LC/MS quantitation of vardenafil (Levitra®) in postmortem biological specimens. Federal Aviation Administration (FAA) Civil Aerospace Medical Institute; technical report documentation no. DOT/FAA/AM-06/17. 2006.
Abd-Elbary A, Tadros MI, Alaa-Eldin AA. Development and in vitro/in vivo evaluation of etodolac controlled porosity osmotic pump tablets. AAPS PharmSciTech. 2011;12(2):485–95.
Layre AM, Couvreur P, Chacun H, Aymes-Chodur C, Ghermani NE, Poupaert J, et al. Busulfan loading into poly (alkyl cyanoacrylate) nanoparticles: physico-chemistry and molecular modeling. J Biomed Mater Res B Appl Biomater. 2006;79((2):254–62.
Sweetman S. Martindale: the complete drug reference. 36th ed. London: Pharmaceutical Press; 2009.
Cachile M, Cazabat AM, Bardon S, Valignat MP, Vandenbrouck F. Spontaneous spreading of surfactant solutions on hydrophilic surfaces. Colloids Surf A Physicochem Eng Asp. 1999;159(1):47–56.
Tadros MI, Al-Mahallawi AM. Long-circulating lipoprotein-mimic nanoparticles for smart intravenous delivery of a practically-insoluble antineoplastic drug: development, preliminary safety evaluations and preclinical pharmacokinetic studies. Int J Pharm. 2015;493(1–2):439–50.
Garanti T, Stasik A, Burrow AJ, Alhnan MA, Wan KW. Anti-glioma activity and the mechanism of cellular uptake of Asiatic acid-loaded solid lipid nanoparticles. Int J Pharm. 2016;500(1–2):305–15.
Liu Y, Pan J, Feng SS. Nanoparticles of lipid monolayer shell and biodegradable polymer core for controlled release of paclitaxel: effects of surfactants on particles size, characteristics and in vitro performance. Int J Pharm. 2010;395(1–2):243–50.
Muller RH, Mader K, Gohla S. Solid lipid nanoparticles (SLN) for controlled drug delivery: a review of the state of the art. Eur J Pharm Biopharm. 2000;50(1):161–77.
Li Y, Wong HL, Shuhendler AJ, Rauth AM, Wu XY. Molecular interactions, internal structure and drug release kinetics of rationally developed polymer-lipid hybrid nanoparticles. J Control Release. 2008;128(1):60–70.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Guest Editor: Sanyog Jain
Rights and permissions
About this article
Cite this article
Tawfik, M.A., Tadros, M.I. & Mohamed, M.I. Lipomers (Lipid-polymer Hybrid Particles) of Vardenafil Hydrochloride: a Promising Dual Platform for Modifying the Drug Release Rate and Enhancing Its Oral Bioavailability. AAPS PharmSciTech 19, 3650–3660 (2018). https://doi.org/10.1208/s12249-018-1191-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12249-018-1191-0