Abstract
Sildenafil (SLD) is employed for the management of erectile dysfunction and pulmonary arterial hypertension. It exhibits meagre water solubility and is available in the form of citrate salt hydrate to improve the solubility. However, it still exhibits moderate solubility, high first-pass metabolism, resulting in very less oral bioavailability. The present study demonstrates the preparation of self-nanoemulsifying drug delivery system for augmenting the oral bioavailability of SLD. Oleic acid and Capmul MCM C8 blend (oil phase), Cremophor® RH40 (surfactant), and Labrafil® M1944 CS (cosurfactant) were selected as main constituents for making liquid preconcentrate based on the solubility and emulsification study. The preconcentrate upon dilution and emulsification showed droplet size 52.03 ± 13.03 nm, PDI 0.143 ± 0.028, and % transmittance was 99.77 ± 1.86% with SLD load of 40 mg/g of formulation. The prepared formulation was further assessed for stability, in vitro release, Caco-2 cell uptake, and in vivo pharmacokinetic performance. SLD-SNEDDS formulation was found to be robust in terms of stability against several folds dilution in the gastrointestinal tract (GIT), freeze–thaw cycles, and had a storage stability of 3 months at 4 °C and 25 °C. SLD-SNEDDS showed ~4.7-fold and ~5-fold increase in time- and concentration-dependent cellular uptake as against SLD cultured with Caco-2 cells. In vivo pharmacokinetic study revealed ~5.8- and ~2.5-fold increase in AUC0-∞ values in case of SLD-SNEDDS as against SLD suspension and SLD citrate solution, respectively.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sildenafil (SLD) is a selective inhibitor of cyclic guanosine monophosphate (cGMP)-specific phosphodiesterase (PDE-5) employed for management of angina pectoris and hypertension [1, 2]. Recently, it is also utilized for management of erectile dysfunction in elderly patients caused due to a variety of reasons. SLD exhibits limited solubility with high log P value and is classified as BCS class II drug [3]. It displays limited absorption, low absolute bioavailability, and a delayed onset of action owing to its low water solubility (∼5–10 mg/L) [4, 5]. As a result, giving the drug in a pre-solubilized form can improve its bioavailability. To improve its solubility, SLD is available in the citrate salt hydrate form for oral use. However, sildenafil citrate (SLD-C) also suffers from extensive first-pass metabolism and has modest solubility (3.5 g/L). It is predominantly eliminated through hepatic metabolism (CYP 3A4), with only 40% oral bioavailability [4, 6]. It shows a comparatively slow onset and brief period of action, with terminal half-life of 3–5 h. Therefore, to maintain drug plasma levels, repeated doses are needed and this leads to various gastrointestinal side effects like burning sensation and dyspepsia [7]. Further, SLD-C exhibits bitter taste, and therefore, film coated tablets with artificial sweeteners are available commercially [8]. Despite the fact that this groundbreaking drug has been in the spotlight for over a decade, comparatively less research on its solubility and pharmacokinetics has been reported. Hence, designing a suitable formulation is a prerequisite to boost the oral bioavailability of SLD by addressing the aforementioned issues.
For BCS class II and class IV drugs, the self-nanoemulsifying drug delivery system (SNEDDS) is an important delivery approach [9,10,11]. SNEDDS has attracted the attention of formulation scientists aiming to augment the oral bioavailability of poorly water-soluble drugs. SNEDDS is an isotropic blend of natural or synthetic oil, surfactants, and cosurfactants that forms a nanoemulsion (globule size range of 100 nm) with gentle agitation provided by the gastrointestinal tract’s digestive motility (GIT). It has a variety of distinct features, including a high solubilization capacity due to the large surface area available for contact between the formulation and the gastrointestinal fluid. It also aids penetration through the GI barrier, inhibits drug precipitation after dilution in the intestine, and protects the drug from chemical and enzymatic breakdown [12, 13]. SNEDDS have shown potential to enhance oral bioavailability of drugs by promoting lymphatic transport, thereby, evading hepatic first-pass metabolism [14,15,16]. SNEDDS have established potential in reducing intra-enterocyte metabolism by cytochrome P450 enzymes [17]. Also, the components employed to prepare SNEDDS (e.g., Cremophor® RH 40) reportedly inhibit the activity of metabolizing enzymes [18]. SNEDDS seems to be most promising as it holds advantages like enhanced physical and/or chemical stability; prospect of delivering them into unit dosage forms, such as soft/hard gelatin or hydroxypropyl methylcellulose capsules (unlike ready-to-use nanoemulsion) which overcomes the palatability-related issues [12]. Further, in case of SNEDDS, the dosage volume can be limited to a maximum of 1 g of prepared liquid preconcentrate that soft gelatin capsule can accommodate [19]. Thus, all these benefits warrant their commercial feasibility and patient compliance.
Considering all these aspects, the present study aims at developing SNEDDS for improving the oral bioavailability and therapeutic potential of SLD. To support our hypothesis, developed SLD-SNEDDS formulation was characterized for their globule shape, PDI, and % transmittance and extensively analyzed using various studies such as stability studies upon dilution in simulated GI fluids, freeze–thaw cycle stability, storage stability, in vitro performance, cellular uptake, and in vivo pharmacokinetic study.
Materials and methods
Materials
Maisine™ 35–1, Peceol™, Capryol™ 90, and Labrafil® M1944 CS were purchased from Gattefosse, France. Captex® 355, Capmul® MCM EP, and Capmul® MCM C8 were acquired from Abitech Corp., USA. Tween® 20 and Tween® 80 were acquired from SDFCL (Baroda, India, 390,007). Propylene Glycol®, PEG-200®, and PEG-400® were procured from Hi-Media, (Mumbai, India). Cremophor® RH40, Cremophor® EL, and sildenafil citrate (SLD-C) were procured from Sigma Aldrich (USA). SLD-C was converted to parent API, SLD using previously reported method (data shown in supplementary data) [20].
Screening of oils
The solubility of SLD in various oils was tested by means of shake flask method. Each vial containing 500 mg of oil had surplus quantity of drug added to it. The liquid was vortexed for 10 min after sealing to achieve a homogeneous mixture. To achieve equilibrium, the mixtures were shaken in a water bath at 50 strokes/min for 72 h at 37 °C. The resulting mixtures were then centrifuged for 10 min at 15,000 rpm. To extract the drug from oil matrix, supernatant was diluted with 0.5 mL ethyl acetate and 2 mL methanol. Mobile phase was used to create final dilutions, which were then evaluated using a validated HPLC method (CBM-20 A pump, SIL-20AC Auto sampler with PDA detector). Waters Symmetry® C18 column (4.6 250 mm, 5 m particle size) was used for chromatographic separation. The HPLC analytical parameters were as follows: mobile phase (ACN: ammonium acetate buffer, pH 7) at 55:45 ratio with a flow rate of 1 mL/min at 240 nm wavelength for SLD.
Screening of surfactant and cosurfactant
Various surfactants were examined for their ability to form emulsion. To obtain an isotropic mixture, a selected oil (combination of oleic acid and Capmul MCM C8) (OAC8) was mixed with an equal amount of several non-ionic surfactants and vortexed for 10 min before heating at 40–45 °C for 5 min. The final emulsion was made by diluting the homogeneous mixtures (200 mg) with 50 mL deionized water. The formed emulsion was left undisturbed for 2 h. Zetasizer (Malvern Instrument, UK) was employed to quantify the size and PDI, and a UV Spectrophotometer (Bio-TEK, USA) was utilized to determine the % transmittance of the emulsion at 638 nm. The % transmittance (T) was calculated using formula,
Similarly, numerous cosurfactants were evaluated for their effect on emulsion forming capacity using the same procedure. Different cosurfactants were tested with a selected oil, and surfactant and their particle size, PDI, and percent transmittance were measured. Various surfactants and cosurfactants were also examined for solubility tests because they have the potential to affect the drug payload in the final SNEDDS formulation.
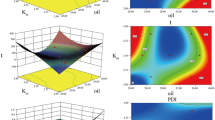
Optimization of liquid SNEDDS formulation through design of experiment (DOE)
Extreme vertices D-optimal mixture design was employed to optimize SNEDDS of SLD. Different dependent variables (droplet size, PDI, and % transmittance) were optimized by varying the fraction of three components (oil, surfactant, cosurfactant) in SNEDDS of SLD deemed as the independent variables. The levels of three independent variables were chosen based on preliminary research conducted before to implementing the experimental design. The response surface methodology of three component system was performed with the constraints 400 ≤ A (OAC8) ≤ 600; 250 ≤ B (Cremophor® RH40) ≤ 500; 50 ≤ C (Labrafil) ≤ 300 of all independent variables. For the optimization investigations, Design Expert® software (Version 9.1, stat-Ease Inc., Minneapolis, MN, USA) was used, and contour plots of all three responses (size, PDI, and % transmittance) were created. For each response, polynomial equations were created. Based on a comparison of numerous statistical metrics such as R2, sequential model sum of squares, lack of fit, and partial sum of square provided by analysis of variance, the appropriate fitting model for each response was selected (ANOVA).
Characterization of SNEDDS
Droplet size, polydispersity index, and ζ potential
The mean droplet size, polydispersity index (PDI), and zeta potential of the resulting nanoemulsion were determined by Zetasizer (Nano ZS, Malvern Instruments, UK). Zeta potential of nanoemulsion was determined both in the presence and absence of SLD to investigate participation of SLD at interface.
Transmission electron microscopy
The morphology of nanoemulsion generated after dilution of SNEDDS was analyzed by TEM [Morgagni, 268D (Fei Electron Optics)] as per previous reports [21]. The detailed procedure is provided in the supplementary information.
Stability studies
Stability in simulated gastric and simulated intestinal fluid
The simulated gastric fluid (SGF) (pH 1.2) and simulated intestinal fluid (SIF) (pH 6.8) were used to examine the stability of the developed SLD-SNEEDS as per previous reports [21]. The detailed procedure is provided in the supplementary information.
Robustness to dilution
The SNEDDS after administration will encounter different degrees of dilution in GIT; therefore, they were assessed for the robustness to dilution at different folds (200- to 800-fold) with SGF (pH 1.2). About 50 mg of SLD-SNEDDS were diluted with SGF at different folds then allowed to attain equilibrium for 2 h and checked for visual change, globule size, and PDI of the nanoemulsion.
Storage stability
Storage stability of SLD-SNEDDS was assessed for 3 months under different temperature conditions for storage. SLD-SNEDDS formulation filled in glass vials was stored at 4 °C and 25 °C for 3 months. After 3 months of storage, the SLD-SNEDDS were examined for the spontaneity of nanoemulsion formation, globule size, and size distribution. Visual change in color and appearance of SNEDDS was also observed.
Freeze-thawing cycle stability
The stability of SLD-SNEDDS at extreme temperatures was tested for brief periods using an optimized formulation that was subjected to freeze-thawing cycles. Three freeze–thaw cycles were performed on the formulation, for e.g., freezing at 0 °C for 24 h and then thawing at 40 °C for 24 h. The particle size and PDI of the formulations were then assessed.
In vitro release, cellular uptake, and in vivo pharmacokinetics
The dialysis bag method employing cellulose membrane (14 kDa, Sigma Aldrich) was employed to assess the in vitro release profile of SLD-SNEDDS as per previous reports [21]. The detailed procedure is provided in the supplementary information. Further, the Caco-2 cell line was used for in vitro cell culture investigations. The Caco-2 cells were acquired from National Centre for Cell Science (NCCS), Pune, India. The cells were cultured and maintained as per our earlier reports [22]. The qualitative and quantitative uptake of the optimized formulation was evaluated using Caco-2 cells as per our previous reports [23, 24]. The detailed procedure for qualitative and quantitative uptake study is provided in the supplementary information. Furthermore, the animal studies were performed on male Sprague Dawley (SD) rats as per previously reported protocol [23, 24]. All the study protocols were duly approved by Institutional Animal Ethics Committee of NIPER, Mohali, India (Approval number: IAEC/17/72) before the start of the study. The detailed procedure is provided in the supplementary information.
Statistical analysis
All the results were expressed as mean ± standard deviation (SD). Graph Pad Prism® (version 5.01) was used to conduct the statistical analysis, which included two-way ANOVA and Bonferroni tests. P < 0.05 was considered as statistically significant difference.
Results
Preparation of SLD-SNEDDS
Selection of oil
The solubility of SLD in numerous oils is shown in Fig. 1A. Oleic acid showed maximum solubility for SLD (131.2 mg/g) followed by Capryol® 90 (32.26 mg/g) and Peceol™ (28.18 mg/g). Thus, for the preparation of SLD-SNEDDS with high drug loading, oleic acid was selected and used for further studies.
Selection of surfactants and cosurfactants
Based on solubility tests, oleic acid was preferred as the oil for SLD. Droplet size, PDI, and % transmittance were used to screen several surfactants and their capacity to emulsify the chosen oil. Practically, oleic acid was not completely emulsified by any of the surfactants. Thus, to improve the emulsification, oleic acid was blended with Capmul MCM C8 (in ratio of 40:60). As shown in Table 1, Cremophor® RH40 had good emulsification ability to emulsify oleic acid and Capmul MCM C8 blend (OAC8). After taking into account the droplet size, PDI, and % transmittance, Cremophor® RH 40 was chosen as the surfactant for OAC8. Further, different cosurfactants were also screened with selected surfactant and oil as shown in Table 2. Cosurfactants are usually employed to increase the spontaneity of nanoemulsion formation. Labrafil M1944CS showed best results among all cosurfactants with suitable droplet size < 100 nm, PDI, and % transmittance. Labrafil M1944CS demonstrated good solubility as well as emulsification ability and was finalized as a cosurfactant and evaluated for further studies.
Optimization of SNEDDS formulation through DOE
The design employed to optimize the final formulation of SLD was extreme vertices mixture design. Three components employed in this study, which were also referred as independent variables, were concentration of oil, surfactant, and cosurfactant. An upper and lower limit of these components was determined from preliminary studies. The droplet size, PDI, and % transmittance were considered as response factors or dependent variables. Tables S1 and S2 show the responses of 16 SLD-SNEDDS batches and their statistical analysis. The responses were fitted into several polynomial models separately, and the model with the highest R2 was chosen as the fitting model. The design constraints were decided on the basis of preliminary study and are depicted in Table 3.
Furthermore, a specific SNEDDS composition was optimized based on desirability criteria. The desirability was to obtain globule size within range of nanoemulsion after dilution of SNEDDS with minimum PDI and maximum % transmittance. A constant amount of SLD 40 mg was added to each composition. The desirability graph was plotted (shown in Fig. 2A), and desirability was found to be 0.935. The SNEDDS containing OAC8 oil, Cremophor® RH 40, and Labrafil M1944CS in the ratio 403:384:213 was chosen as the optimized formulation, depending on the desirability value. Polynomial equations were employed to predict the data of these responses and expected responses were found to be droplet size 52.03 ± 13.03 nm, PDI 0.143 ± 0.028, and % transmittance 99.77 ± 1.86%.
Equations 1, 2, and 3 are polynomial equation for droplet size, PDI, and % transmittance, respectively.
Droplet size | \(=+192.4888*\mathrm{A}-116.960*\mathrm{B}+89.917*\mathrm{C}\) | (1) |
PDI | \(=+2.778*\mathrm{A}+4.541*\mathrm{B}+1.352*\mathrm{C}-12.201*\mathrm{A}*\mathrm{B}-3.424*\mathrm{A}*\mathrm{C}-8.135*\mathrm{B}*\mathrm{C}\) | (2) |
% Transmittance | \(=+5.825*\mathrm{A}-25.473*\mathrm{B}+735.331*\mathrm{C}+420.320*\mathrm{A}*\mathrm{B}-1662.755*\mathrm{A}*\mathrm{C}-1933.395*\mathrm{B}*\mathrm{C}+5653.648*\mathrm{A}*\mathrm{B}*\mathrm{C}\) | (3) |
Characterization of nanoemulsion
Droplet size and zeta potential analysis
The optimized formulation displayed a droplet size of 57.44 ± 6.45 nm with a PDI of 0.130 ± 0.026 and % transmittance was 99.04 ± 0.015%. The zeta potential was found to be −23.4 ± 4.33 mV and − 22.4 ± 5.13 mV in the absence or presence of SLD, respectively.
Transmission electron microscopy (TEM)
Figure 3 demonstrates the morphology of nanoemulsion globules formed after the dilution of SNEDDS. Figure 3 shows that all droplets were spherical in shape and distributed uniformly across the dispersion.
Stability studies
Effect of SGF and SIF
The stability of SLD-SNEDDS in simulated gastrointestinal fluids was assessed depending on size and PDI after 2 h and 6 h, respectively. SLD-SNEDDS had shown insignificant difference (P > 0.05) in the droplet size and PDI value of formed emulsion post dilution with SGF and SIF as depicted in Table 4.
Robustness to dilution
The influence of different folds of dilution (200 to 800 folds) with SGF (pH 1.2) on SLD-SNEDDS size and PDI is depicted in Table 5. The nanoemulsion developed from dilution of SLD-SNEDDS was robust after dilution up to many folds and showed no indication of phase separation or precipitation of drug.
Storage stability
The results of storage stability at 4 °C and 25 °C for 3 months are illustrated in Table 6. The important quality attributes, i.e., particle size and PDI, were not affected in case of SLD-SNEDDS.
Freeze-thawing cycle stability
The quality attributes (droplet size and PDI) achieved after dilution of SNEDDS are shown in Table 7. The important quality attributes, i.e., droplet size and PDI of nanoemulsion obtained following three successive freeze/thaw cycles, were unaltered. Furthermore, during freezing process, no significant signs of solidification, drug precipitation, or phase separation were detected; nevertheless, a modest decline in flowability was observed, which was normal when reinstated to room temperature [23].
In vitro release studies
The in vitro release profile of SLD formulations in simulated GI fluids is depicted in Fig. 4. SLD-SNEDDS formulation initially showed more than 50% of drug release within first 2 h which increased to 75% in next 2 h, i.e., in SIF. After 4 h, SLD-SNEDDS formulation showed sustained drug release with about 85% release in 24 h. In contrast, entire drug was released within 4 h in case of free SLD.
Caco-2 cell culture experiments
Qualitative cell uptake
The CLSM images of Caco-2 cells treated with free Coumarin 6 (C-6) and C-6 loaded SNEDDS for 3 h are shown in Figs. 5A, B. When Caco-2 cells were incubated with C-6 loaded SNEDDS, the fluorescence was significantly higher [Fig. 5B (a)] than when they were incubated with free C-6 [Fig. 5A (a)], indicating that C-6 SNEDDS is efficiently internalized by Caco-2 cells. Furthermore, when incubated with SNEDDS, horizontal series line analysis revealed higher green intensity signals that were overlapped with white line vibrations (due to cellular structures) [Fig. 5B (d and e)]. This indicated that the fluorescence observed could be attributed to the C-6 which was internalized. Further, the overlapping indicated that the fluorescence observed was not because of the residual C-6 in the medium or the well plate [Fig. 5B (d and e)].
Quantitative cell uptake
Figures 6A, B show the time- and concentration-dependent apical cell absorption of SLD and SLD-SNEDDS via Caco-2 cell monolayers. In comparison to free SLD, SLD-SNEDDS had a considerably higher cellular uptake (P < 0.05) in this study. Furthermore, extending the incubation duration from 0.5 to 2 h resulted in an increase in cellular absorption, while increasing the incubation time from 2 to 3 h resulted in no significant change in uptake. After 2 h, the % cell uptake was 15.75% and 74.2% for free SLD and SLD-SNEDDS respectively at concentration 20 µg/mL. In a time-dependent study, SLD-SNEDDS was found to have a ∼ 4.7-fold greater cellular uptake than free SLD. Increasing the concentration of SLD from 10 to 30 µg/mL, on the other hand, resulted in a concentration-dependent increase in cellular uptake. In concentration-dependent study, ∼5-fold increase (at 30 μg/mL) in % SLD cellular uptake from SLD-SNEDDS was observed with respect to free SLD.
In vivo pharmacokinetic study
The mean plasma-concentration versus time profile upon oral administration of the SLD, SLD-C, and SLD-SNEDDS is shown in Fig. 7. The corresponding mean pharmacokinetic parameters are presented in Table 8. It was observed that SLD-SNEDDS showed ~3.4- and ~1.29-fold increment in Cmax as compared to SLD and SLD-C. Furthermore, ~5.8- and ~2.5-fold increase in AUC0-∞ value was observed in case of SLD-SNEDDS as compared to SLD and SLD-C. The half-life of SLD-SNEDDS was 1.46- and 1.29-fold higher than SLD and SLD-C, respectively.
Discussion
The current report deals with the development of SNEDDS for SLD to enhance its oral bioavailability. Initially, the SLD-C was used as a drug to develop its SNEDDS formulation. However, in later stages of experimentation due to the poor solubility in oily components, poor emulsification of selected oil component, and low drug loading (8.70 mg/g) in SNEDDS, SLD-C was converted into its base form and used for further research. The conversion of sildenafil citrate to sildenafil base (SB) was confirmed from IR spectrum of both compounds as shown in Fig. S1. A strong band at 1582 cm−1 in the spectrum of sildenafil citrate is attributed to the symmetric stretching frequency of COOH groups belonging to citrate-ion. It disappears in the spectrum of SB giving rise to a weak band at 1580 cm−1 which may correspond to the overlapped stretching frequency of N–H group. The enlargement of the C–H and N–H stretching vibration bands in the region 2700–3600 cm−1 is usually due to the presence of numerous hydrogen bonds in the citrate complex which are practically absent in sildenafil base. Further, SLD demonstrated higher solubility in various oils, surfactants, and cosurfactants as compared to SLD-C. This higher solubility in vehicles could be a result of lipophilic and semi-crystalline nature of SLD as compared to citrate salt [20, 25]. Oleic acid was selected as an oil phase, as SLD showed higher solubility in oleic acid. Because of the low emulsification of oleic acid by most of the surfactants and cosurfactants, oleic acid was blended with Capmul MCM C8 which had a low solubilizing power for SLD but possessed good emulsion forming ability [26, 27]. Oleic acid was blended with Capmul MCM C8 in a ratio of 40:60. Cremophor® RH 40 was selected as surfactant because it showed the higher emulsification ability than other surfactants [28]. Cosurfactants play an important role to enhance the emulsification ability of surfactants [29]. The droplet size of emulsion formed with Cremophor® RH40 was more than 100 nm and PDI was also more than 0.25. Therefore, to improve the emulsification capability of Cremophor® RH40 and to decrease the droplet size and PDI of the emulsion, Labrafil M1944CS was selected as a cosurfactant. Using Labrafil M1944CS as a cosurfactant for Cremophor® RH40 had a favorable impact on both the droplet size and PDI of the formulation which were reduced to < 100 nm and < 0.150, respectively. The final formulation of SLD-SNEDDS was optimized using Design Expert® software. There were two types of variables known as independent and dependent variables. Here the independent variables were proportion of oil, surfactant, and cosurfactant and dependent variables were droplet size, PDI, and % transmittance of the nanoemulsion. A methodological optimization of various dependent variables was accomplished by changing the percentage of ternary phase components in water which was deemed as independent variable. Final concentration of was optimized by Design Expert®. The final composition of the optimized SNEDDS (OAC8; 403.8 mg, Cremophor® RH40; 383.3 mg, and Labrafil M1944CS; 212.9 mg) when diluted with deionized water portrayed encouraging results in form of nano range droplet size (57.44 ± 6.45 nm), PDI (0.130 ± 0.026), and % transmittance (99.04 ± 0.015). Since SLD showed very good solubility in oleic acid, the drug loading capacity was also improved and the final optimized formula of SLD-SNEDDS contained 40 mg drug per gram of liquid SNEDDS. The optimized formulation was then subjected to reconstitution to finally ensure that the nanoemulsion formed after dilution of SNEDDS has desired droplet size and PDI. The formed nanoemulsion was further characterized for morphology using TEM. The photographs obtained by TEM revealed that all droplets formed after dilution possess were spherical shape and nanometric size and were uniformly dispersed in water, confirming the formation of nanoemulsion after dilution. Following that, the stability of SNEDDS was evaluated in terms of dilution resistance, freeze–thaw stability, and long-term storage stability. When SNEDDS is taken orally, it is subjected to different degrees of dilution in various sections of the GIT. As a result, the resistance of the chosen composition to different degrees of dilution and different pH conditions had to be assessed. The developed SNEDDS formulation was stable and resilient to all dilutions and pH conditions, as shown in Tables 4 and 5. The SNEDDS were also exposed to freeze–thaw cycle study to check whether the final formulation is stable at extreme temperature conditions and that it can withstand extreme temperature variations. The formulation’s freeze–thaw stability was tested using three freeze–thaw cycles, and the appearance, self-emulsifying ability, droplet size, and PDI of the resulting emulsion remained unchanged. Moreover, during storage time, the formulation showed no phase separation or drug precipitation [30]. In vitro drug release study for SLD-SNEDDS and SLD was performed in presence of SGF (pH 1.2), SIF (pH 6.8), and phosphate buffer (pH 7.4) for 24 h using dialysis membrane of 14 kD. The SGF and SIF were used to mimic the physiological conditions. The SNEDDS formulation demonstrated a release of 85% over 24 h while, in case of free drug, almost 100% release took place over period of 4 h. This could be attributed to the fact that SLD is an ampholyte and possesses pH-dependent solubility. However, the sustained release of drug from SNEDDS could be due to the formation of micelles that encapsulate the SLD inside, with subsequent hindrance in SLD release or having larger globule size which could not penetrate the dialysis membrane thus slowing release. Other factors that influence drug release properties include the oil–water partition coefficient, phase volume ratio, dispersed phase droplet size, drug distribution in various phases of the system, potential interaction between excipients and drug, and the rate of drug diffusion in both phases of the system [30, 31].
The Caco-2 cell culture model has long been considered as a gold standard for assessing drug’s transepithelial transport and pre-systemic metabolism. In vitro Caco-2 cell uptake assays were used to assess the developed SNEDDS formulation’s oral transport capability across the GI membrane [30]. CLSM images revealed a much greater qualitative uptake of C-6 nanoemulsion as against free C-6. The validity of these findings was subsequently confirmed using horizontal line series analysis. A concentration- and time-dependent quantitative cellular uptake study was conducted to better understand the SLD’s cellular uptake efficiency through SNEDDS. The time- and concentration-dependent quantitative cellular uptake of SLD-SNEDDS also showed considerable uptake, which was found to be consistent with qualitative uptake studies [30]. In vivo pharmacokinetic study was performed to see if the SNEDDS formulation may augment SLD absorption following oral administration. In vivo pharmacokinetics corroborated the optimistic results of Caco-2 cell uptake experiments, revealing a considerable improvement in bioavailability of SLD-SNEDDS, with a ~5.8- and ~2.5-fold increase in AUC0-∞ value in comparison to SLD and SLD-C, respectively. It can be attributed to the fact that SLD is a BCS class II drug having low water solubility and high first-pass metabolism, and the development of SNEDDS of SLD improved not only its solubility but also tissue permeability. Also, rather than the physicochemical properties of the drug molecules, the features of the nanocarriers influence the pharmacokinetic properties of drugs when delivered in nano formulation. Upon oral administration, SLD loaded SNEDDS instantaneously emulsify in GI tract and result in the formation of drug loaded micellar structures, which overcome the barrier of solubility limited absorption. Further, chylomicrons aid SNEDDS absorption by releasing entrapped drugs into lymph vessels rather than directly emptying into the central compartment, thereby limiting their hepatic first-pass metabolism and, as a result, boosting oral bioavailability [32, 33]. Furthermore, the presence of surfactant and cosurfactants in SNEDDS was linked to increased permeability and augmented absorption through the intestinal wall. Thus, in comparison to SLD suspension and SLD-C, the AUC0-∞, Cmax value, and MRT values showed that SLD-SNEDDS had a superior in vivo pharmacokinetic profile.
Conclusion
The SNEDDS was optimized and developed for oral delivery of SLD in the current study. The resulting formulation had better gastrointestinal and storage stability, as well as increased cellular absorption. In addition, when compared to free SLD and SLD-C, in vivo pharmacokinetic experiments revealed that the proposed formulation had a higher bioavailability. The findings suggest that current SNEDDS formulation could be a good delivery strategy for poorly soluble drugs and drugs with a high pre-systemic metabolism. In addition, this formulation provides significant advantages, which include high industrial adaptability and considerably lower scalability constraints. The conversion of the SNEDDS formulation into solid dosage form could be further line of action to boost the stability of delivery system.
Availability of data and materials
Data will be available on request to authors.
References
Jung S-Y, Seo Y-G, Kim GK, Woo JS, Yong CS, Choi H-G. Comparison of the solubility and pharmacokinetics of sildenafil salts. Arch Pharm Res. 2011;34:451–4. https://doi.org/10.1007/s12272-011-0313-y.
Webb DJ, Freestone S, Allen MJ, Muirhead GJ. Sildenafil citrate and blood-pressure–lowering drugs: results of drug interaction studies with an organic nitrate and a calcium antagonist. Am J Cardiol. 1999;83:21–8. https://doi.org/10.1016/S0002-9149(99)00044-2.
Kim TH, Shin S, Jeong SW, Lee JB, Shin BS. Physiologically relevant in vitro-in vivo correlation (IVIVC) approach for sildenafil with site-dependent dissolution. Pharmaceutics. 2019;11:251. https://doi.org/10.3390/pharmaceutics11060251.
Jung S-Y, Kim D-W, Seo YG, Woo JS, Yong CS, Choi H-G. Development of sildenafil-loaded orally disintegrating tablet with new lactate salt. Drug Dev Ind Pharm. 2012;38:635–41. https://doi.org/10.3109/03639045.2011.621432.
Sanphui P, Tothadi S, Ganguly S, Desiraju GR. Salt and cocrystals of sildenafil with dicarboxylic acids: solubility and pharmacokinetic advantage of the glutarate salt. Mol Pharm. 2013;10:4687–97. https://doi.org/10.1021/mp400516b.
Fraisse A, Butrous G, Taylor MB, Oakes M, Dilleen M, Wessel DL. Intravenous sildenafil for postoperative pulmonary hypertension in children with congenital heart disease. Intensive Care Med. 2011;37:502–9. https://doi.org/10.1007/s00134-010-2065-4.
Wang Y, Chow MSS, Zuo Z. Mechanistic analysis of pH-dependent solubility and trans-membrane permeability of amphoteric compounds: application to sildenafil. Int J Pharm. 2008;352:217–24. https://doi.org/10.1016/j.ijpharm.2007.10.039.
Lee J-H, Choi G, Oh Y-J, Park JW, Choy YB, Park MC, Yoon YJ, Lee HJ, Chang HC, Choy J-H. A nanohybrid system for taste masking of sildenafil. Int J Nanomedicine. 2012;7:1635–49. https://doi.org/10.2147/IJN.S28264.
Ghadi R, Dand N. BCS class IV drugs: highly notorious candidates for formulation development. J Controlled Release. 2017;248:71–95. https://doi.org/10.1016/j.jconrel.2017.01.014.
Elgart A, Cherniakov I, Aldouby Y, Domb AJ, Hoffman A. Improved oral bioavailability of BCS class 2 compounds by self nano-emulsifying drug delivery systems (SNEDDS): the underlying mechanisms for amiodarone and talinolol. Pharm Res. 2013;30:3029–44. https://doi.org/10.1007/s11095-013-1063-y.
Dalal L, Allaf AW, El-Zein H. Formulation and in vitro evaluation of self-nanoemulsifying liquisolid tablets of furosemide. Sci Rep. 2021;11:1315. https://doi.org/10.1038/s41598-020-79940-5.
Date AA, Desai N, Dixit R, Nagarsenker M. Self-nanoemulsifying drug delivery systems: formulation insights, applications and advances. Nanomed. 2010;5:1595–616. https://doi.org/10.2217/nnm.10.126.
Cherniakov I, Domb AJ, Hoffman A. Self-nano-emulsifying drug delivery systems: an update of the biopharmaceutical aspects. Expert Opin Drug Deliv. 2015;12:1121–33. https://doi.org/10.1517/17425247.2015.999038.
Porter CJH, Trevaskis NL, Charman WN. Lipids and lipid-based formulations: optimizing the oral delivery of lipophilic drugs. Nat Rev Drug Discov. 2007;6:231–48. https://doi.org/10.1038/nrd2197.
Singh B, Khurana L, Bandyopadhyay S, Kapil R, Katare OOP. Development of optimized self-nano-emulsifying drug delivery systems (SNEDDS) of carvedilol with enhanced bioavailability potential. Drug Deliv. 2011;18:599–612. https://doi.org/10.3109/10717544.2011.604686.
Franco V, Gershkovich P, Perucca E, Bialer M. The interplay between liver first-pass effect and lymphatic absorption of cannabidiol and its implications for cannabidiol oral formulations. Clin Pharmacokinet. 2020;59:1493–500. https://doi.org/10.1007/s40262-020-00931-w.
Singh G, Pai RS. Trans-resveratrol self-nano-emulsifying drug delivery system (SNEDDS) with enhanced bioavailability potential: optimization, pharmacokinetics and in situ single pass intestinal perfusion (SPIP) studies. Drug Deliv. 2015;22:522–30. https://doi.org/10.3109/10717544.2014.885616.
Chen M-L. Lipid excipients and delivery systems for pharmaceutical development: a regulatory perspective. Adv Drug Deliv Rev. 2008;60:768–77. https://doi.org/10.1016/j.addr.2007.09.010.
Constantinides PP. Lipid microemulsions for improving drug dissolution and oral absorption: physical and biopharmaceutical aspects. Pharm Res. 1995;12:1561–72. https://doi.org/10.1023/A:1016268311867.
Melnikov P, Corbi PP, Cuin A, Cavicchioli M, Guimarães WR. Physicochemical properties of sildenafil citrate (Viagra) and sildenafil base. J Pharm Sci. 2003;92:2140–3. https://doi.org/10.1002/jps.10469.
Jain S, Garg T, Kushwah V, Thanki K, Agrawal AK, Dora CP. α-Tocopherol as functional excipient for resveratrol and coenzyme Q10-loaded SNEDDS for improved bioavailability and prophylaxis of breast cancer. J Drug Target. 2017;25:554–65. https://doi.org/10.1080/1061186X.2017.1298603.
Bapat P, Ghadi R, Chaudhari D, Katiyar SS, Jain S. Tocophersolan stabilized lipid nanocapsules with high drug loading to improve the permeability and oral bioavailability of curcumin. Int J Pharm. 2019;560:219–27. https://doi.org/10.1016/j.ijpharm.2019.02.013.
Rege MD, Ghadi R, Katiyar SS, Kushwah V, Jain S. Exploring an interesting dual functionality of anacardic acid for efficient paclitaxel delivery in breast cancer therapy. Nanomed. 2019;14:57–75. https://doi.org/10.2217/nnm-2018-0138.
Jain S, Deore SV, Ghadi R, Chaudhari D, Kuche K, Katiyar SS. Tumor microenvironment responsive VEGF-antibody functionalized pH sensitive liposomes of docetaxel for augmented breast cancer therapy. Mater Sci Eng C. 2021;121:111832. https://doi.org/10.1016/j.msec.2020.111832.
Elshafeey AH, Bendas ER, Mohamed OH. Intranasal microemulsion of sildenafil citrate: in vitro evaluation and in vivo pharmacokinetic study in rabbits. AAPS PharmSciTech. 2009;10:361–7. https://doi.org/10.1208/s12249-009-9213-6.
Taha EI, Al-Saidan S, Samy AM, Khan MA. Preparation and in vitro characterization of self-nanoemulsified drug delivery system (SNEDDS) of all-trans-retinol acetate. Int J Pharm. 2004;285:109–19. https://doi.org/10.1016/j.ijpharm.2004.03.034.
Balakumar K, Raghavan CV, Selvan NT, Rahman SMH. Self emulsifying drug delivery system: optimization and its prototype for various compositions of oils, surfactants and co-surfactants. J Pharm Res. 2013;6:510–4. https://doi.org/10.1016/j.jopr.2013.04.031.
Thomas N, Holm R, Müllertz A, Rades T. In vitro and in vivo performance of novel supersaturated self-nanoemulsifying drug delivery systems (super-SNEDDS). J Controlled Release. 2012;160:25–32. https://doi.org/10.1016/j.jconrel.2012.02.027.
Kassem AA, Mohsen AM, Ahmed RS, Essam TM. Self-nanoemulsifying drug delivery system (SNEDDS) with enhanced solubilization of nystatin for treatment of oral candidiasis: design, optimization, in vitro and in vivo evaluation. J Mol Liq. 2016;218:219–32. https://doi.org/10.1016/j.molliq.2016.02.081.
Jain S, Jain AK, Pohekar M, Thanki K. Novel self-emulsifying formulation of quercetin for improved in vivo antioxidant potential: implications for drug-induced cardiotoxicity and nephrotoxicity. Free Radic Biol Med. 2013;65:117–30. https://doi.org/10.1016/j.freeradbiomed.2013.05.041.
Elnaggar YSR, El-Massik MA, Abdallah OY. Self-nanoemulsifying drug delivery systems of tamoxifen citrate: design and optimization. Int J Pharm. 2009;380:133–41. https://doi.org/10.1016/j.ijpharm.2009.07.015.
Khoo S-M, Shackleford DM, Porter CJH, Edwards GA, Charman WN. Intestinal lymphatic transport of halofantrine occurs after oral administration of a unit-dose lipid-based formulation to fasted dogs. Pharm Res. 2003;20:1460–5. https://doi.org/10.1023/A:1025718513246.
Porter CJH, Charman WN. Intestinal lymphatic drug transport: an update. Adv Drug Deliv Rev. 2001;50:61–80. https://doi.org/10.1016/S0169-409X(01)00151-X.
Acknowledgements
Authors would like to acknowledge Director, NIPER S.A.S. Nagar, for providing necessary facilities and infrastructure. Authors are also thankful to Mr. Rahul Mahajan, NIPER, S.A.S. Nagar, for his technical assistance.
Author information
Authors and Affiliations
Contributions
SJ and NK conceived this research and designed experiments; SJ, BN, RG, and TD participated in designing and interpretation of the data; NK and BN performed experiments and analysis; and RG and RS wrote the paper and participated in the revisions of it. DC and SK significantly contributed in performing the in vitro and in vivo studies. (SJ: Sanyog Jain; NK: Narinder Kumar; RS: Reena Sharma; RG: Rohan Ghadi; TD: Tushar Date; BN: Bhargavi Nallamothu; DC: Dasharath Chaudhari; SK: Sameer S. Katiyar).
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The animal study protocols were duly approved by Institutional Animal Ethics Committee of NIPER, Mohali, India (Approval number: IAEC/17/72) before the start of the study.
Consent for publication
All authors have read and approved the submitted manuscript.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jain, S., Kumar, N., Sharma, R. et al. Self-nanoemulsifying formulation for oral delivery of sildenafil: effect on physicochemical attributes and in vivo pharmacokinetics. Drug Deliv. and Transl. Res. 13, 839–851 (2023). https://doi.org/10.1007/s13346-022-01247-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-022-01247-x