Abstract
In vitro Andersen cascade impactor-sized mass (ISM) and aerodynamic fine particle mass (FPM) <5 μm for tiotropium and salmeterol combined in a novel inhalation powder formulation containing 7.5 μg tiotropium/25 μg salmeterol (TSHH) were similar (within ±15%) to reference products containing 18 μg of tiotropium (Spiriva® HandiHaler®) (TioHH) and 50 μg of salmeterol (Serevent® Diskus®) (SalD). The pharmacokinetics (PK), pharmacodynamics, safety, and tolerability of the novel fixed-dose TSHH formulation administered once daily was compared with the single-agent therapies TioHH (once daily [qd]) and SalD (twice daily [bid]) and with the jointly administered combination of TioHH (qd) plus SalD (bid) in a randomized, 22-week, open-label, four-way crossover study in 50 patients with chronic obstructive pulmonary disease (COPD). For tiotropium, TSHH and TioHH were bioequivalent based on mean steady-state plasma area under the plasma concentration–time curves (AUC), while the urinary excretion amount was higher for TSHH and not bioequivalent to TioHH. Tiotropium peak plasma concentrations at steady state (C max,ss) were 40% higher with TSHH. For salmeterol, substantial differences were observed in plasma AUCs and Cmax,ss. No significant differences in 8-h forced expiratory volume in 1 s or forced vital capacity were detected for the TSHH (qd) against the combination of TioHH (qd) with SalD (bid). Maintenance therapy with tiotropium plus salmeterol as TSHH or as the jointly administered reference products is superior to either agent alone, safe, and well tolerated in COPD patients. In vitro results were not predictive of clinical PK findings for both tiotropium and salmeterol for the TSHH dry powder inhaler product.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is characterized by airflow limitation that is not fully reversible (1). This limitation is usually progressive with accumulating restrictions to patients’ physical activity, which can become disabling upon even modest physical exertion. Inhaled bronchodilators are central to COPD management, for both the prevention and relief of symptoms, primarily breathlessness, and to improve patients’ functional ability.
The long-acting muscarinic antagonist (LAMA) tiotropium (Spiriva® HandiHaler® [HH]) is an established, once-daily inhaled therapy for the maintenance treatment of COPD (2,3). Similarly, the long-acting β2-adrenergic agonist (LABA) salmeterol (Serevent® Diskus®) is well established in the treatment of COPD, providing significant increases in lung function for 12 h and longer. As a single-agent therapy, salmeterol requires twice-daily dosing in order to achieve and maintain adequate bronchodilation over a 24-h period (4).
Combining bronchodilators of different pharmacologic classes improves spirometric efficacy compared to single-agent therapy; therefore, a muscarinic antagonist and β2-adrenergic agonist are frequently co-prescribed and, together, produce greater and more sustained improvements in forced expiratory volume in 1 s (FEV1) than either drug alone (5).
COPD is characterized by dyspnea on exertion, mainly during the daytime waking hours. Contributing to the dyspnea are circadian changes in lung function resulting from increased sympathetic activity during the day and parasympathetic activity during the night (6). A therapeutic objective would be to provide optimal airway patency during the more physically active periods of the day and maintain this through the night. It was hypothesized that, despite the differences in dosing frequency, a once-daily combination of these two agents may provide the desired bronchodilation during daytime (due to the additive bronchodilator effects of both the anticholinergic and adrenergic components) and sustain the bronchodilation during the less-active nighttime (due to the prolonged 24-h bronchodilator activity of the anticholinergic component tiotropium) (7).
A new, unit dose, capsule-based, dry powder inhaler (DPI) and formulation combining tiotropium and salmeterol was developed, possessing in vitro aerodynamic fine particle size characteristics for each drug substance that matched the established single-agent products. A clinical study in COPD patients was undertaken to compare the pharmacokinetics (PK), pharmacodynamics (PD), and safety of the new formulation to the single-agent therapies in their marketed formulations and approved daily-dose regimens, as well as to the combination of the single-marketed agents. The pharmaceutical and clinical study data sets were jointly examined for potential in vitro/in vivo relationships and predictive correlations, to bring additional evidence into the ongoing debate on the extent to which in vitro testing can be relied upon exclusively as a surrogate for assessing bioequivalence of orally inhaled, locally acting drug products (8–10).
MATERIALS AND METHODS
Description of Dry Powder Inhalers
Tiotropium (Spiriva® HandiHaler®) (TioHH) is a single-unit, gelatin capsule-based system. Each capsule contains 5.5 mg of powder formulation consisting of 18 μg of micronized tiotropium (as bromide monohydrate, 22.5 μg) with lactose monohydrate as carrier, which is inhaled using the HandiHaler® (HH) device. HH is classified as a high-resistance device (4-kPa pressure drop at 39 L/min). Under standardized conditions (US Pharmacopeia [USP] <601>), an average of 10.4 μg of tiotropium is delivered per capsule. The SalD inhaler consists of a strip of 60 blisters; each 12.5-mg blister contains a powder blend composed of micronized salmeterol 50 μg (as salmeterol xinafoate) with lactose monohydrate as carrier. The reported (11) Diskus® airflow resistance is ≤2.6 kPa when tested at 60 L/min.
The delivery system for the new 7.5 μg tiotropium/25 μg salmeterol (TSHH) was based on the HH design and operating principle. Instead of a gelatin-based capsule, an interlocking two-piece capsule fabricated from polyethylene (PE) was used. The capsule contained 10 mg of powder formulation combining 7.5 μg of micronized tiotropium (as bromide monohydrate, 9.4 μg) and 25 μg of micronized salmeterol (as xinafoate, 36.3 μg), with lactose monohydrate as carrier. Owing to the different total mass and center of mass of the powder-filled PE capsule, slight dimensional adjustments to the HH airflow pathway were introduced, in order to maintain critical capsule vibration characteristics and an airflow resistance of 4 kPa at 39 L/min.
Aerodynamic Particle Size Distribution
Emitted dose (ED) aerodynamic particle size distributions (APSD) were characterized using an Andersen cascade impactor (ACI; USP <601>, Apparatus 3). For TioHH and TSHH, an airflow rate of 39 L/min was used. The samples of SalD obtained for the study required 70 L/min to achieve the reported pressure drop. Separately, APSD of SalD was also measured at 39 L/min. Impaction plates were pre-coated with an ethanolic glycerol/Brij 35 mixture (5:3 w/w) to prevent re-entrainment of impacted particles. Each TioHH and TSHH test consisted of powder from six capsules aerosolized into the ACI using a vacuum pump to draw the required flow rate through the apparatus. For each salmeterol determination, three doses were discharged into the impactor. Tiotropium and salmeterol were quantitatively recovered from the induction port (throat), pre-separator, and cascade impactor stages and analyzed by high-performance liquid chromatography (gradient HPLC with dual wavelength detection). For the TioHH and TSHH configurations, residual drug amounts in the capsule and device were also quantitated. To facilitate comparison with previously published work (11), impactor-stage groupings were constructed as follows: throat + pre-separator + stage 0 (T_P_S0), stages 1 and 2 (S1_2), stages 3 and 4 (S3_4), stage 5 (S5), and stages 6 and 7 plus filter (S6_7_F). The emitted dose per capsule was estimated from the total quantity of active pharmaceutical ingredient recovered from the throat, pre-separator, and all stages of the cascade impactor. The impactor-sized mass (ISM) per capsule was determined from the individual quantities of active pharmaceutical ingredient recovered from stage 1 to filter at 39 L/min or stage -1 to filter for 70 L/min. Mass median aerodynamic diameter (MMAD), geometric standard deviation (GSD), and aerodynamic fine particle masses (FPM) <5 μm and <3 μm were estimated from log-probability plots of cumulative percentage of mass less than stated aerodynamic diameter vs. aerodynamic diameter. The effective cutoff diameters (ECD) were calculated according to equation 1 in reference (12) for the two flow rates investigated.
Clinical Study Design
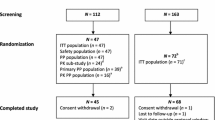
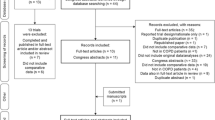
The clinical investigation was a 22-week, multicenter, randomized, active-controlled, open-label, four-way crossover trial in COPD patients. Following an initial screening visit, patients entered a 2-week run-in period, during which any medications containing tiotropium or salmeterol were excluded, to ensure clinical stability (i.e., no exacerbations). Qualifying patients were then randomized into the 16-week, open-label, crossover treatment portion of the study, in which they received each of the four treatments (Table I) for 4 weeks in a randomized sequence. There was no washout period when switching from one treatment to the next in order to reduce protocol complexity. Carryover effects, if present, would have dissipated by the fourth treatment week even considering the long half-life (5–6 days) of tiotropium. One to 3 days prior to the end of each of the 4-week treatment periods, patients returned for electrocardiogram (ECG) monitoring that commenced just before the administration of that morning’s dose of study medication and lasted for the subsequent 8 h. On the final day of each 4-week treatment period, each patient returned to the clinical site for the administration of that morning’s dose of study medication. Pre- and 8-h post-dosing blood and urine sampling along with pulmonary function testing (PFT) and vital sign measurements were performed during this visit. After completion of all treatment administrations, there was a 4-week follow-up period included in the protocol solely for monitoring any post-treatment adverse events. The study design is outlined diagrammatically in Supplemental 1.
Subjects
Male and female subjects with a COPD diagnosis and meeting the following criteria were enrolled: relatively stable airway obstruction with a post-bronchodilator (salbutamol) FEV1 <80% of predicted normal, and post-bronchodilator FEV1 <70% of post-bronchodilator forced vital capacity (FVC) at the initial visit according to Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria (1); and current or ex-smokers aged ≥40 years with a smoking history of ≥10 pack-years. Patients had to be able to perform technically acceptable pulmonary function tests during the study period and demonstrate ability to inhale medication in a competent manner from the HandiHaler® and Diskus® devices.
Exclusion criteria included history of asthma, eosinophil count ≥600/mm3, a respiratory disorder in addition to COPD (e.g., bronchiectasis or cystic fibrosis) or significant comorbidity that might affect lung function, regular oxygen use (and unable to abstain from the use of oxygen therapy), a history of a respiratory infection or COPD exacerbation in the 4 weeks prior to the screening visit or during the run-in period, and previous lung resection.
The study was carried out in accordance with the principles of the Declaration of Helsinki (version, October 1996) and the International Conference on Harmonization Good Clinical Practice Guidelines. The study protocol (sponsor code 1184.24, clinicaltrials.gov NCT00673478), subject information, and informed consent forms were reviewed and approved by an independent ethics committee. Written informed consent was obtained from each subject prior to the performance of any study-specific procedures.
A total of 58 patients were screened for participation in this trial; 50 met the inclusion criteria. Of these, two patients discontinued prematurely due to an adverse event and one for logistical reasons. For the 48 remaining subjects, one discontinued the tiotropium single-agent therapy (TioHH) period due to incorrect dosing of the study medication, but continued in the study. Data from this patient for all other treatment periods were included in the final evaluation set (full analysis set). Demographics and baseline disease characteristics for the patients completing the study are presented in Supplemental 2.
Pharmacokinetics
Blood samples were collected before drug administration (−5 min) and then 2, 5, 7, 10, 15, 20, 40, 50, 60, and 70 min and 2, 4, 6, and 8 h after administration, by means of an indwelling venous catheter. Plasma aliquots were kept frozen until analysis.
Urine samples were collected before drug administration and during the intervals 0–2, 2–4, and 4–8 h after drug administration. The volume of urine for the sample interval was determined gravimetrically. Urine aliquots were acidified with citric acid and kept frozen until analysis.
Tiotropium and salmeterol concentrations were determined by validated assays using HPLC coupled to tandem mass spectrometry. The lower limits of quantitation (LOQ) were 2.50 pg/mL for tiotropium and 5.0 pg/mL for salmeterol.
Plasma PK parameters for tiotropium and salmeterol (Table II) were derived from concentration–time data by non-compartmental analysis using WinNonlin software (Professional Edition, version 1.5; Scientific Consulting Inc., Cary, NC, USA). Area under the plasma concentration–time curves (AUC) was calculated using “Linear up-Logarithmic down” option in WinNonLin.
Pharmacodynamics
After a qualifying pre-bronchodilator spirometric test, severity of COPD according to GOLD was assessed 45 min following inhalation of four puffs of salbutamol (100 μg/puff). After completion of the run-in period, study baseline FEV1 and FVC were determined before inhalation of the first dose of study medication. Serial spirometry was conducted at the end of each treatment period including readings 10 min prior to and 30 min and 1, 2, 3, 4, 6, 8 h after dosing. Testing on any PFT measurement day started between 07:00 a.m. and 10:00 a.m., with 30-min maximum difference from the corresponding start time at the randomization visit. Measurements were performed according to American Thoracic Society criteria (13); the highest values of FEV1 and FVC from three technically adequate measurements were retained.
For time-points where both PK blood sampling and PFT were scheduled to occur, blood sampling was always performed first.
Safety
Blood pressure was measured 10 min prior to drug administration and 10, 20, and 40 min and 1, 2, 3, 4, 6, and 8 h post-dosing. Twelve-lead ECGs were recorded 10 min prior to drug administration and 2, 5, 7, 10, 20, and 40 min and 1, 2, 4, and 8 h post-dosing.
Statistics
Plasma concentration values were log-transformed prior to statistical analysis using a linear model analysis of variance, incorporating terms for treatment, period, sequence, and subject within sequence. The effect “subject within sequence” was considered as random and the other effects as fixed. The difference between the expected means for log(test)-log(reference) was estimated by the difference in the corresponding least-square means (point estimate), and two-sided 90% confidence intervals (CIs) based on the t distribution were computed. These quantities were then back-transformed to the original scale to give the point estimator (geometric mean) and interval estimates for the median intra-/intersubject ratio between the response for test and reference treatments. Variance estimates from previously conducted studies were used to estimate the number of subjects necessary to sufficiently power the study to provide a 90% CI for the treatment ratios with a coverage probability of 95%. As the spirometric efficacy parameters were considered secondary in this study, an analysis of covariance (with terms for center, patients within center, baseline, treatment, and period) was considered appropriate. The adjusted mean values, treatment contrasts (difference), and 95% CIs were calculated.
RESULTS
Aerodynamic Particle Size Distribution
Tiotropium
Content and delivery information for tiotropium for TioHH and TSHH is shown in Table I and stage-grouped ACI results in Fig. 1. The TSHH system displays significantly less retention in the device and much lower deposition in grouping T_P_S0 compared to the reference product. As a consequence, the amount of tiotropium contained in each TSHH capsule was reduced to achieve the same ISM and FPM <5 μm amounts as the reference TioHH. While there were no appreciable differences in ISM, FPM <5 μm, or MMAD between TioHH or TSHH, FPM <3 μm was higher by about 40% for TSHH.
Salmeterol
Content and delivery information for salmeterol for the reference SalD and the TSHH combination is shown in Table I. Cascade impactor results are shown in Fig. 2 plotted as a function of particle dimension to permit comparison across the different flow rates. The TSHH system displays a threefold lower deposition in the inlet/throat/pre-separator cluster compared to the reference product; this also drove a reduction in the amount of salmeterol needed to match SalD ISM and FPM <5 μm. Device residual was not measured for the reference SalD since only 6% of the initial content went unrecovered from the ACI. The size distribution profiles for SalD and TSHH are well matched. The distribution profiles for both devices using 39 L/min are compared in Fig. 3, where it can be similarly observed that the large particle fraction represented by deposition in the grouping T_P_S0 is substantially greater for SalD compared to TSHH. While the stage 3 amounts are approximately equal at the lower flow rate, a comparison across the group S1_2 and group S4_5 data as well as ISM and FPM (Table I) suggests that a greater inhalable mass of salmeterol is available from the TSHH powder.
Comparison of aerodynamic particle size profiles for the salmeterol treatments. SalD was tested at 70 L/min. TSHH was tested at 39 L/min. Individual points represent the pooled average of 12 capsules for TSHH and 9 actuations for SalD. Impactor-sized mass and fine particle mass results are overlapping data points. I/T/P inlet + throat + pre-separator, ISM impactor-sized mass, FPM fine particle mass <5 μm
Pharmacokinetics
Tiotropium
Average plasma level profiles are presented in Fig. 4 and average urinary excretion amounts in Fig. 5. A summary of the PK parameters for tiotropium is provided in Table II. The systemic exposure in terms of C max,ss, area under the plasma concentration–time curve over the interval 0-8 h after inhalation at steady state (AUC0–8,ss,), and the amount of tiotropium eliminated in urine incrementally over the interval 0–8 h after inhalation at steady state (Ae0–8,ss) was comparable for the two reference treatments TioHH and TioHH + SalD. However, TSHH resulted in a higher systemic exposure (approximately 12% higher AUC0–8,ss, 23% higher Ae0–8,ss, and 45% higher C max,ss values) compared to the reference TioHH. Likewise, the test formulation TSHH produced greater systemic exposure (approximately 19% higher AUC0–8,ss, 28% higher Ae0–8,ss, and 38% higher C max,ss) values of tiotropium compared to the reference TioHH + SalD. The tiotropium t max,ss values were similar for the three treatments.
The results of the statistical evaluation of relative bioavailability of tiotropium are in Table III. The AUC0–8,ss values for TSHH and TioHH were not markedly different and met criteria for bioequivalence. In contrast, the AUC0–8,ss value for TSHH was significantly higher than that for TioHH + SalD, with a geometric mean ratio of 117.6. For C max,ss, a significant difference between TSHH and both TioHH treatments was found. For Ae0–8,ss, a significant difference between TSHH vs. both the reference treatments TioHH and TioHH + SalD was found.
Salmeterol
Geometric mean salmeterol plasma concentration–time profiles for TSHH, single-agent therapy SalD, and jointly administered combination therapy TioHH + SalD are shown in Fig. 6. A summary of the PK parameters for salmeterol is provided in Table II. The systemic exposure in terms of C max,ss and AUC0–8,ss of salmeterol from the two SalD treatments was essentially replicated. However, TSHH administration resulted in a totally different systemic exposure profile of salmeterol (approximately 29% higher C max,ss and 57% lower AUC0–8,ss values) compared to TioHH + SalD. Similarly, TSHH led to approximately 18.5% higher C max,ss and 54.1% lower AUC0–8,ss values compared to the reference SalD. The median t max,ss was about 5 min for TSHH in comparison to 50–60 min for the reference administrations.
The results of the statistical evaluation of relative bioavailability of salmeterol are provided in Table III. TSHH was not bioequivalent to the comparators SalD and TioHH + SalD, with significantly lower AUC0–8,ss. Despite lower AUC values, TSHH yielded significantly higher C max,ss values compared to the reference treatments.
Pharmacodynamics
The 8-h time-course profiles for the spirometric parameters are illustrated in Fig. 7. Mean responses for FEV1 and FVC results (AUC0–8 h, trough, and peak) by treatment are shown in Supplemental 3 along with response comparisons for TSHH vs. the other three treatments.
Following the 4-week treatment period, once-daily TSHH provided a significantly greater FEV1 response compared with the individual single-agent therapies TioHH and SalD. No clinically relevant (<0.02 L) (14) or statistically significant differences were found between TSHH and TioHH + SalD.
There was also a significantly greater FVC response with TSHH compared to the single-agent therapies TioHH and SalD. In terms of trough FVC, TSHH was superior to salmeterol (0.182 L, p < 0.0001), while compared to tiotropium, no relevant difference was found (0.065 L, p = 0.14). No relevant differences (<0.04 L, p > 0.46) were found between TSHH and TioHH + SalD.
Safety Results
No clinically significant differences between any of the four treatment regimens were observed. Roughly 25% of the subjects showed an increase in systolic (>25 mmHg above baseline) or diastolic (>90 mmHg and an increase of >10 mmHg above baseline) blood pressure, which was comparable across all treatment periods. Changes in mean heart rate post-dosing were small and comparable between the four treatments. For QT interval corrected by the Fridericia formula (QTcF), small differences were observed between the three salmeterol-containing treatments (Supplemental 4). For the QTcF comparisons, TioHH was used as a surrogate placebo since tiotropium does not produce an effect here (15). The maximum difference in QTcF for TSHH was seen 10 min post-inhalation and was slightly higher compared to the two salmeterol reference treatments. For single-agent therapy with SalD, the maximum difference in QTcF of 3.92 ms was found 40 min post-inhalation, while for TioHH + SalD, the maximum difference was seen 1 h post-inhalation. The mean increases observed in QTcF are <5 ms for all three salmeterol-containing treatments with the upper bound of the two-sided 90% CI <10 ms, meaning that these increases are below the threshold level of concern, as described in the International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use Harmonized Tripartite Guideline (ICH E14) (16).
DISCUSSION
Guidelines on pharmacotherapy of COPD recommend combining two long-acting bronchodilators with different pharmacological mechanisms in patients who require both classes of drugs for optimal control of their disease and to improve treatment compliance. It has been previously shown that a once-daily combination of tiotropium and salmeterol provides superior bronchodilator effects which were not only restricted to the relevant period of daily activities but were also observed during the nighttime (7). The present study reinforces those earlier findings and clearly demonstrates that with the TSHH combination formulation, a reduction in the total systemic exposure of salmeterol could be achieved thereby opening the potential for reducing LABA-related adverse events. Assessing a true clinical benefit, however, would require longer-term studies including clinical outcomes such as lung function improvement, symptom control, exacerbation rates, and health status.
In Vitro Evaluation
The HandiHaler® is a well-established and accepted high-resistance DPI administration device. Drug delivery shows little flow rate dependency, even at 20 L/min. It is efficient in converting the energy of the inhaled airstream into useful work for deagglomeration and aerosolization of the drug/carrier content (17,18). Despite these advantages, the current Spiriva® HH system exhibits appreciable retention of tiotropium on the inner surface of the gelatin capsule, a consequence of non-specific adhesion coupled with the large ratio of capsule surface area to drug mass. An interaction between micronized tiotropium and the lactose carrier leads to a further loss of inhalable tiotropium, evidenced by the amount retained in the T_P_S0 portion of the APSD.
Using the basic concept of the HH, a modified version of the system was developed for TSHH. A size #3 capsule fabricated from PE was substituted for the gelatin size #3 capsule that altered the adhesion interaction and significantly reduced the amount of unemitted powder. The dimensions of the HH capsule chamber were adjusted to accommodate the lighter PE capsule containing 10-mg total powder (altered center of mass) to maximize vibrational dynamics while preserving the 4-kPa flow resistance at a flow rate of 39 L/min. Quality adjustments in the lactose carrier also reduced the interaction effects, leading to a decrease in the non-inhalable large particle fraction. The goal of matching the tiotropium in vitro ISM and FPM with minimal change to the APSD profile was realized using a nominal dose of 7.5 μg that resulted in a dose delivery of 6.5 μg, compared to 18 and 10.4 μg, respectively, for the marketed TioHH.
For salmeterol, the non-inhalable large particle fraction was considerably lower for TSHH vs. SalD, which also required adjustment in drug content to achieve ISM and FPM that matched the reference. With the exception of this large particle fraction, there were no differences in the APSD profiles between the two articles when tested at their standardized flow rates.
A comparison of salmeterol APSD results for TSHH and SalD at 39 L/min (Fig. 3) showed a similar pattern with a substantial (nearly fourfold) reduction in the non-inhalable large particle fraction and near equivalence in ISM. FPMs were within 15% of each other but subtle differences in deposition for S1 + S2, S4, and S5 could be detected, with the suggestion of a slightly finer aerodynamic distribution for salmeterol from the TSHH.
Pharmacokinetic Evaluation
Tiotropium has some interesting features that were exploited in the present PK evaluations. Despite its high aqueous solubility in excess of 25 mg/mL, as a quaternary ammonium compound (log P of −2.28), it is negligibly absorbed (19) from the human gastrointestinal (GI) tract. In the oral Biopharmaceutics Classification System (BCS) nomenclature, it would be categorized as a high-solubility, low-permeability substance. Thus, any inhaled tiotropium detected in the systemic circulation is likely to have come from transport of dissolved material through pulmonary membranes. Additionally, tiotropium is largely unmetabolized and excreted predominantly as parent drug in the urine (19).
The PK profile for tiotropium delivered from TioHH in this study agrees with other published results (20). Absorption after inhalation was rapid with an average t max of 5 min. The tiotropium PK profile (AUC0–8,ss, C max,ss, t max,ss) was unaltered by the concomitant administration of salmeterol via SalD. This evidence eliminates a PK interaction as the reason for the different profile exhibited by tiotropium with TSHH. For the test formulation TSHH, plasma AUC0–8,ss demonstrated bioequivalence to the respective references TioHH and TioHH + SalD. For tiotropium administered as TSHH, t max was similarly rapid, at about 5 min. The approximately 40% higher C max,ss for TSHH was not anticipated based on the <15% difference in ISM or FPM <5 μm Andersen cascade impactor results. FPM <3 μm was therefore added as a further metric.
To compensate for the very low concentrations of drug present in plasma, parallel determination of tiotropium urinary excretion was included to improve the reliability of bioequivalence assessments. The necessity of doing this was confirmed when examining plasma AUC0–8,ss results, which gave mixed statistical outcomes for TSHH vs. its tiotropium comparators. As expected, TioHH and TioHH + SalD AUC0–8,ss were shown to be equivalent. Confusingly, for AUC0–8,ss, TSHH and TioHH were found to be equivalent (ratio point estimate 1.12) whereas TSHH vs. TioHH + SalD (ratio point estimate 1.17) were not equivalent due to a failure to meet confidence interval criteria. Thus, urinary data were relied upon to resolve the discrepancy. Cumulative urinary excretion amounts confirmed the plasma-derived equivalence between the reference comparators. For TSHH, the trend toward slightly higher absorption suggested by plasma data was clearly demonstrated with 22–26% more tiotropium found in the urine vs. the comparators, confirming non-equivalence to either tiotropium reference. The addition of urinary excretion measurements and subsequent statistical analysis contributed definitively to the overall bioequivalence assessment in this study and should be considered as necessary in any tiotropium bioequivalence evaluation.
The reason for the higher absorption of tiotropium from TSHH cannot be entirely explained from the present study data. While FPM <3 μm was approximately 40% greater for TSHH, it was the only parameter difference compatible with the higher AUC and C max. The lack of any parallel behavior in ISM, FPM <5 μm, and MMAD leads to the suspicion that the FPM <3 μm finding is anomalous. We maintain that the well-known limitations in the in vitro test system especially the inability to accurately mimic in vivo inhalation dynamics and lung deposition are the primary causes for the poor in vitro/ in vivo correlation (IVIVC) exhibited.
Salmeterol xinafoate, in contrast to tiotropium, possesses only moderate to low aqueous solubility at 60 μg/mL (21) with a log P of 4.2 (22) and, in the BCS paradigm, represents a low-solubility, high-permeability substance. After oral administration, salmeterol undergoes significant metabolism with only minor urinary excretion of the parent drug. Significant absorption attributed to material impacting the oropharynx and upper airways that was subsequently swallowed has also been described (23).
Identical PK profiles for salmeterol administered via SalD alone and as TioHH + SalD were observed, demonstrating well-controlled, within- and between-subject variability throughout the study and eliminating a PK interaction as the reason for the different profile exhibited by salmeterol with TSHH. For all three salmeterol treatments, the first appearance of salmeterol in the systemic circulation occurred within 10 min, suggesting rapid dissolution and transport across pulmonary membranes for some portion of the emitted dose. The overall profile for TSHH was distinctly different with a rapidly attained peak plasma level that quickly declined and remained below that of SalD from 30-min post-dosing onward. Secondary absorption of salmeterol from TSHH appeared to be absent, suggesting that oropharyngeal deposition was minimal, which is consistent with the lower large particle fraction seen in the in vitro APSD profile. The plasma AUC0–8,ss was 40% lower for TSHH because of the absence of this secondary absorption phase. A charcoal block was not used in this study so an independent estimate of purely pulmonary absorption could not be made. Secondary absorption of salmeterol is largely thought to be the result of oral input after mouth- and upper airway-impacted material has been cleared and swallowed. However, modeling by Weber and Hochhaus (24) suggests that protracted pulmonary absorption limited by dissolution kinetics can also be a contributor in the case of low-solubility substances. This highlights the need to include an oral absorption inhibitor as part of any inhalation bioequivalence comparisons where secondary GI absorption is known to occur.
Pharmacodynamic Evaluation
FEV1 and FVC profiles showed differential lung function responses and clear time dependencies over the 8-h measurement period. Differences in the magnitude of response between tiotropium alone via TioHH and salmeterol alone via SalD were apparent, a function of both intrinsic pharmacology and inhaled dose. Maximal response after the administration of both tiotropium/salmeterol combinations was greater than either single agent, consistent with previous reports (7). The hypothesis that salmeterol administration could be reduced to just once daily in combination with tiotropium was proven through the comparison of trough FEV1 and FVC values. There was no significant difference at trough FEV1 despite the fact that 24 h had elapsed since the last salmeterol dosing with TSHH vs. 12 h in the TioHH + SalD treatment group. The overall PFT time profile for both tiotropium/salmeterol combinations remained indistinguishable throughout the 8-h active measurement period.
Safety Evaluation
Based on the observations made in the present study, therapy with once-daily TSHH during a 4-week treatment period was shown to be safe and well tolerated compared to 4 weeks of treatment with each of the single agents or with jointly administered combination therapy of TioHH plus SalD. The safety parameters of blood pressure and heart rate did not reveal any relevant treatment differences; analysis of the standard laboratory tests did not reveal any relevant findings. In terms of QTcF, small differences were observed between the three salmeterol-containing treatments vs. the surrogate placebo. None of the differences exceeded the threshold level of concern as described in the ICH E14 guideline (16). The time at which the maximal effect on QTcF occurred aligned closely with the salmeterol t max, confirming once again the discrimination capability of PK for mapping systemic safety and insuring equivalence between inhalation drug products.
Overall
This study presents another example of the general inability of the current in vitro inhalation product test platforms to demonstrate a reliable level A IVIVC (25). For oral dosage forms, establishing a level A IVIVC is a prerequisite for dispensing with PK or PD studies, i.e., granting of a biowaiver. Therefore, any regulatory pathway leading to approval of an inhalation dosage product on the basis of in vitro data alone using current pharmacopoeial test platforms is scientifically unsupported at this time. PK was again shown to be highly discriminating with respect to safety inferences and remains an important BE feature. FEV1 and FVC outcomes were similar for the new combination formulation and the jointly administered single-agent products where in vitro ISM and FPM had been matched. This suggests that qualitative (i.e., level B) IVIVCs might exist in some cases.
CONCLUSIONS
In the present study, both tiotropium and salmeterol in vitro results using currently defined pharmacopoeial test conditions were not predictive of PK outcomes. The study offered no new evidence or validation that systemic PK could serve as a reliable surrogate and eliminate the need for measurement of airway pharmacologic effect; PD data remain critical in bioequivalence assessments for locally acting orally inhaled drug products. The study results also show that simultaneous measurement of tiotropium in plasma and urine should be included in any comparative PK protocol and that plasma AUC and urinary Ae-derived BE conclusions must agree with each other. The surprising PK results for salmeterol reaffirm that when any low-solubility active pharmaceutical ingredient with meaningful secondary oral absorption is being evaluated, protocols should include administration with and without an oral absorption inhibitor, to clearly separate immediate and dissolution-limited direct pulmonary absorption from any secondary GI component.
References
Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001;163(5):1256–76. doi:10.1164/ajrccm.163.5.2101039.
Gross NJ. Tiotropium bromide. Chest. 2004;126(6):1946–53. doi:10.1378/chest.126.6.1946.
Vincken W. Bronchodilator treatment of stable COPD: long-acting anticholinergics. Eur Respir Rev. 2005;14:23–32. doi:10.1183/09058180.05.00009403.
Jarvis B, Markham A. Inhaled salmeterol: a review of its efficacy in chronic obstructive pulmonary disease. Drugs Aging. 2001;18(6):441–72.
Tashkin DP, Ferguson GT. Combination bronchodilator therapy in the management of chronic obstructive pulmonary disease. Respir Res. 2013;14:49. doi:10.1186/1465-9921-14-49.
Postma DS, Keyzer JJ, Koeter GH, Sluiter HJ, De Vries K. Influence of the parasympathetic and sympathetic nervous system on nocturnal bronchial obstruction. Clin Sci (Lond). 1985;69(3):251–8.
van Noord JA, Aumann JL, Janssens E, Smeets JJ, Zaagsma J, Mueller A, et al. Combining tiotropium and salmeterol in COPD: effects on airflow obstruction and symptoms. Respir Med. 2010;104(7):995–1004. doi:10.1016/j.rmed.2010.02.017.
Adams WP, Ahrens RC, Chen ML, Christopher D, Chowdhury BA, Conner DP, et al. Demonstrating bioequivalence of locally acting orally inhaled drug products (OIPs): workshop summary report. J Aerosol Med Pulm Drug Deliv. 2010;23(1):1–29. doi:10.1089/jamp.2009.0803.
Evans C, Cipolla D, Chesworth T, Agurell E, Ahrens R, Conner D, et al. Equivalence considerations for orally inhaled products for local action-ISAM/IPAC-RS European Workshop report. J Aerosol Med Pulm Drug Deliv. 2012;25(3):117–39. doi:10.1089/jamp.2011.0968.
O’Connor D, Adams WP, Chen ML, Daley-Yates P, Davis J, Derendorf H, et al. Role of pharmacokinetics in establishing bioequivalence for orally inhaled drug products: workshop summary report. J Aerosol Med Pulm Drug Deliv. 2011;24(3):119–35. doi:10.1089/jamp.2011.0878.
Daley-Yates PT, Mehta R, Chan RH, Despa SX, Louey MD. Pharmacokinetics and pharmacodynamics of fluticasone propionate and salmeterol delivered as a combination dry powder from a capsule-based inhaler and a multidose inhaler in asthma and COPD patients. J Aerosol Med Pulm Drug Deliv. 2014;27(4):279–89. doi:10.1089/jamp.2013.1040.
General Chapters. <601> Aerosols, nasal sprays, metered-dose inhalers, and dry powder inhalers. In: US Pharmacopeia: National Formulary, editor. 2013 USP 36-NF 31. Rockville, MD: US Pharmacopeia (USP); 2012.
American Thoracic Society. Standardization of Spirometry, 1994 Update. Am J Respir Crit Care Med. 1995;152(3):1107–36. doi:10.1164/ajrccm.152.3.7663792.
Jones PW, Beeh KM, Chapman KR, Decramer M, Mahler DA, Wedzicha JA. Minimal clinically important differences in pharmacological trials. Am J Respir Crit Care Med. 2014;189(3):250–5. doi:10.1164/rccm.201310-1863PP.
Koenen-Bergmann M, Ring A, Ritzhaupt A, Platz J, Germeyer S. Some properties of different analyses in "Thorough QT studies" compared using a QT study of tiotropium. Deutsche Gesellschaft für Medizinische Informatik, Biometrie und Epidemiologie e V (gmds) 2006. 2006. http://www.egms.de/static/de/meetings/gmds2006/06gmds167.shtml. Accessed 29 September 2014.
International Conference on Harmonisation (ICH) of Technical Requirements for Registration of Pharmaceuticals for Human Use. Harmonized tripartite guideline ICH E14. The clinical evaluation of QT/QTc interval prolongation and proarrhythmic potential for non-antiarrhythmic drugs. ICH website. 2005. http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E14/E14_Guideline.pdf. Accessed 29 September 2014.
Shur J, Lee S, Adams W, Lionberger R, Tibbatts J, Price R. Effect of device design on the in vitro performance and comparability for capsule-based dry powder inhalers. AAPS J. 2012;14(4):667–76. doi:10.1208/s12248-012-9379-9.
Wachtel H, Ertunc O, Koksoy C, Delgado A. Aerodynamic optimization of Handihaler and Respimat: the roles of computational fluid dynamics and flow visualization. In: Dalby R, Byron P, Suman J, Farr S, Young P, editors. Respiratory drug delivery. River Grove: Davis Healthcare International Publishing; 2008.
Price D, Sharma A, Cerasoli F. Biochemical properties, pharmacokinetics and pharmacological response of tiotropium in chronic obstructive pulmonary disease patients. Expert Opin Drug Metab Toxicol. 2009;5(4):417–24. doi:10.1517/17425250902828337.
Hohlfeld JM, Sharma A, van Noord JA, Cornelissen PJ, Derom E, Towse L, et al. Pharmacokinetics and pharmacodynamics of tiotropium solution and tiotropium powder in chronic obstructive pulmonary disease. J Clin Pharmacol. 2014;54(4):405–14. doi:10.1002/jcph.215.
Jouyban-Gharamaleki A, York P, Hanna M, Clark BJ. Solubility prediction of salmeterol xinafoate in water–dioxane mixtures. Int J Pharm. 2001;216(1-2):33–41.
National Library of Medicine. Salmeterol. TOXnet HSDB database. 2005. http://toxnet.nlm.nih.gov/cgi-bin/sis/search/a?dbs+hsdb:@term+@DOCNO+7315. Accessed 23 September 2014.
Cazzola M, Testi R, Matera MG. Clinical pharmacokinetics of salmeterol. Clin Pharmacokinet. 2002;41(1):19–30. doi:10.2165/00003088-200241010-00003.
Weber B, Hochhaus G. A pharmacokinetic simulation tool for inhaled corticosteroids. AAPS J. 2013;15(1):159–71. doi:10.1208/s12248-012-9420-z.
Byron PR, Hindle M, Lange CF, Longest PW, McRobbie D, Oldham MJ, et al. In vivo-in vitro correlations: predicting pulmonary drug deposition from pharmaceutical aerosols. J Aerosol Med Pulm Drug Deliv. 2010;23 Suppl 2:S59–69. doi:10.1089/jamp.2010.0846.
Acknowledgments
The authors acknowledge the important contributions of Stefan Leiner to the development of this manuscript.
Disclosure Statement
Stephen Horhota, Cynthia Verkleij, Loek Bour, Ashish Sharma, Michael Trunk, and Piet Cornelissen are employees of Boehringer Ingelheim. Dr. Jan van Noord was the principal investigator for this study that was funded by Boehringer Ingelheim.
Author information
Authors and Affiliations
Corresponding author
Additional information
Guest Editors: Lawrence Yu, Sau L. Lee, Guenther Hochhaus, Lana Lyapustina, Martin Oliver, and Craig Davies-Cutting
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Supplemental 1
Outline of the clinical trial protocol (GIF 227 kb)
Supplemental 2
(DOC 46 kb)
Supplemental 3
(DOC 47 kb)
Supplemental 4
(DOC 33 kb)
Rights and permissions
About this article
Cite this article
Horhota, S.T., van Noord, J.A., Verkleij, C.B. et al. In Vitro, Pharmacokinetic, Pharmacodynamic, and Safety Comparisons of Single and Combined Administration of Tiotropium and Salmeterol in COPD Patients Using Different Dry Powder Inhalers. AAPS J 17, 871–880 (2015). https://doi.org/10.1208/s12248-015-9751-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12248-015-9751-7