Abstract
Background
Current evidence on chronic conditions favors promotion of health behaviors as a mean to positively impact health outcomes. In Parkinson’s disease, performing health behaviors is indicated as a means to fight the long-lasting burden of the disease. Understanding actual engagement in health behaviors and patient activation and their association to function and health-related quality of life is therefore important. Our objectives were, among people with Parkinson’s disease: (1) to characterize health behaviors including utilization of rehabilitative treatments, physical activity, and patient activation levels, and (2) to test the associations between these health behaviors and health outcomes.
Methods
A cross-sectional study of 88 people with Parkinson’s disease (age 66.84 ± 8.8) was conducted. Participants answered questionnaires measuring health behaviors including utilization of health professions treatments, physical activity, patient activation, and health outcomes consisting of function and health-related quality of life. Linear regression models were conducted to test associations between measured health behaviors, function and health-related quality of life.
Results
Participants rarely engage in rehabilitative treatments, but showed high levels of patient activation. Controlled by demographics and disease severity, physical activity and patient activation were associated with function (b = 0.41, p < .001; b = 0.2, p = .02, respectively) and physical activity but not patient activation, which was associated with health-related quality of life (b = 0.19, p = .03). There was also interaction effects of physical activity and non-motor symptoms, and physical activity and motor symptoms on health-related quality of life (b = 0.19, p = .02 and b = − 0.22, p = .01, respectively).
Conclusions
In respect to their potential health-related benefits for people with Parkinson’s disease, health professionals’ treatments are underutilized. Findings supported the importance of health behaviors for maintaining function and health-related quality of life among people with Parkinson’s disease. They also show a differential contribution of motor and non-motor symptoms to the association between physical activity and quality of life. It is suggested that policy makers encourage opportunities for physical activity tailored for people with Parkinson’s disease and adopt a proactive stance towards enhancing awareness and use of rehabilitation services.
Trial registration NCT05211700, ClinicalTrials.gov ID: NCT05211700 first release 12/30/2021, https://classic.clinicaltrials.gov/ct2/show/NCT05211700
Similar content being viewed by others
Introduction
Parkinson’s disease (PD) is an incurable, chronic, progressive neurodegenerative disorder that affects motor, cognitive, and autonomic functions [1, 2]. The number of patients living with PD (PwP) is poised for growth due to aging of the world’s population [3]. Because the life expectancy of PwP is only slightly shorter than that of the general population [4, 5], PwP foresees managing symptoms for an extended duration, including severe disability and its associated medical complexities [6,7,8]. Given the increasing impact of PD on the economy, healthcare systems, and patients themselves, there’s a pressing need to facilitate strategies that can be widely used in diverse PwP populations. The current evidence on chronic conditions favors promotion of health behaviors [9,10,11] as a means of positively impacting health outcomes.
At the individual level, health behaviors refer to any activity the patient performs to get well (e.g., receiving treatment from medical providers, lifestyle adjustments) and to the individual’s beliefs and perceptions related to health maintenance, restoration, and improvement [12]. In PD, non-pharmacological treatment approaches focus on everyday life functioning (e.g., gait, falls, activities of daily living, speech) and their underlying impaired body functions (e.g., balance, dexterity). Therefore, utilization of multidisciplinary rehabilitative treatments, which should include physical therapy, occupational therapy, speech and language pathology and psychology, is recommended [13, 14]. Several systematic reviews and meta-analyses published in recent years concluded that rehabilitative treatments such as physical therapy have significant effects on motor symptoms and function, including balance, gait, risk of falls, and freezing of gait [15,16,17]. Reports of physical therapy insurance claims, however, range from 14 to 60% in different countries [18].
In addition, physical activity plays a major role in the non-pharmacological treatment of PwP, and its effects are widely discussed in the context of brain plasticity, cognitive function, motor symptoms and physical capacity [19,20,21,22]. Long-term engagement in physical activity, is therfore an important lifestyle-related health behavior.
The concept of patient activation captures the mental aspects of health behaviors: people’s knowledge, skills, and confidence in managing their health. Higher patient-activation levels indicate higher readiness to adopt behaviors that maintain or improve health. Compared with people with low levels of activation, people with high activation levels are more likely to adopt health behaviors such as maintaining physical activity [23]; Thus, they are more likely to experience better health outcomes [24, 25].
Previous studies reported the effect of structured health profession interventions or physical activity on different health domains in PwP, and showed the positive role these activities play in maintaining health outcomes [26,27,28,29,30]. These studies do not, however, represent actual health behaviors performed by PwP in real life (i.e., without structured intervention). Our goal in the current study was to measure health behaviors related to PD effectively performed by PwP in real life, and to test the relationship between these behaviors and health outcomes. More specifically, our objectives were, among PwP living in the community: (1) to characterize self-reported utilization of rehabilitative treatments, self-reported engagement in physical activity, and patient activation levels; (2) to test the possible associations between these aspects of health behaviors and health outcomes, including function and health-related quality of life (HRQoL).
We hypothesized that greater utilization of rehabilitative treatment, greater engagement in physical activity and higher patient activation will be associated with better function and HRQoL.
Methods
Study design: a cross-sectional study with a convenience sampling.
Study sample
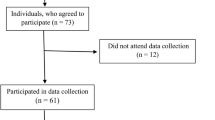
A total of 88 PwP were recruited from the Movement Disorders Institute, Department of Neurology, Rambam Health Care Campus. Patients were included in the study if they had been diagnosed with PD and were not experiencing severe cognitive decline. The Ethics Committees of the University of Haifa and the Rambam Health Care Campus approved the study. All participants provided written informed consent.
Procedure
Patients arriving for a routine visit at the Movement Disorders Institute were screened for eligibility by the treating neurologist. Eligible patients were given a short explanation of the study procedures and invited to participate in a one-hour session consisting of answering questionnaires and assessments, described below, conducted by a trained research assistant. Data about the disease and pharmacological treatment were retrieved from electronic medical records.
Study variables
Information on participants’ age, gender, years of education, and disease duration and disease severity was collected. To assess disease severity, we used the following variables, which are disease-specific indicators of the severity of PD, but each reflects a different aspect of the disease (motor symptoms, non-motor symptoms, and dopamine consumption): (1) the Unified Parkinson’s disease rating scale revised by the Movement disorders society (MDS-UPDRS), motor part score, to assess severity of motor signs of PD [34]; (2) the Non-Motor Symptoms Questionnaire score (NMSQ) [35], to assess severity of non-motor signs of PD; and (3) the Levodopa Equivalent Daily Dose (LEDD) [36], which provides an artificial summary of the total daily anti-Parkinsonian medications a patient is receiving [36, 37].
Health behaviors included utilization of rehabilitative treatments and physical activity level. Participants were asked to report whether and how frequently they utilize physical therapy, occupational therapy, and speech and language pathology treatments. The International Physical Activity Questionnaire–Short version (IPAQ-Short) [31] was used to assess physical activity. The IPAQ is a commonly used, self-report questionnaire of time spent in four categories of physical activity (i.e., vigorous, moderate, walking, and sitting) during the last seven days. Scores are interpreted as total physical activity in metabolic equivalent units (METS) in the last 7 days [31].
Patients’ activation was assessed with the Patient’s Activation Measure (PAM-13®, Insignia Health) [32]. The PAM-13 is a self-report, validated, licensed tool to measure a patient’s knowledge, skills, and confidence for self-management [32]. We used a validated, licensed Hebrew version of the PAM-13 supplied by Insignia Health (https://www.insigniahealth.com/products/pam-survey), which holds the copyrights to the questionnaire. The PAM-13 consists of 13 items, to which participants rate their agreement on a 4-point Likert scale. The score is transformed into a continuous 0–100 scale according to a licensed conversion table (Insignia Health) [33]. A patient’s overall score captures the extent to which they feel engaged and confident in managing their health conditions, with higher scores indicating stronger activation [32]. Based on their PAM-13 score, patients are divided into four ordinal levels of activation. Level 1 represents patients who tend to be passive and feel overwhelmed managing their own health, while level 4 represents patients who have the attitude, knowledge and skills that are important for engagement in health behaviors.
Health outcomes were evaluated across two domains: function, and HRQoL. Function was assessed with (1) the Frenchay Activities Index (FAI) [38], and (2) the 10 Meter Walk Test (10-MWT) for comfortable walking speed. Walking speed correlates with functional mobility and physical function in PwP and other populations [39,40,41]. Frenchay index and gait speed were standardized to mean 0 and SD 1 and then averaged to produce the dependent variable of functioning.
HRQoL was assessed using the PD Questionnaire–39 (PDQ-39) [42]. The questionnaire items measure frequency of experiencing difficulties across eight dimensions of daily living. The HRQoL construct was developed using two indicator variables: the emotions and cognition subscales of the PDQ-39. The theory-based selection of these specific subscales was further strengthened by factor analysis. We conducted a factor analysis using a Varimax rotation method that confirmed that all PDQ subscales constitute a single construct; Therefore, only the two subscales with the highest loadings were used: the PDQ Emotions and Cognition scales (0.82 and 0.80 respectively).
Statistical analysis
Descriptive statistics were calculated to describe the study sample and to characterize utilization of rehabilitative treatments, physical activity, and patient activation levels. Nominal and ordinal variables are presented using frequency indices. Continuous variables are presented as mean ± standard deviation (SD) or as median and a range between quartiles 1 and 3, depending on the distribution of the variable.
For the walking-speed variable, a missing value for one participant was corrected using the mean of all participants.
Linear regression models were used to evaluate if health behaviors (physical activity and patient activation) were associated with functioning and HRQoL, controlling for demographics and disease severity. We used an iterative approach to developed our final model. First, we tested a model that included only demographic variables (sex, age, disease duration, years of education, social support (MSPSS score), co-morbidities (Charlson Index) and living with another person (indicating support at home); Second, we entered variables related to disease severity (NMSQ, MDS-UPDRS and LEDD); Third, we entered health behaviors (IPAQ and PAM), then we entered interactions between health behaviors and disease severity variables. Finally, a final reduced model was tested omitting non-significant variables. Variables included in the final model were selected using the backward method.
The level of statistical significance was determined to be p < 0.05 for all analyses. Analyses were performed using SAS version 9.4.
Results
A total of 90 PwP were recruited, of whom 88 (58 men, 30 women, mean age 66.84 ± 8.8, mean Hoehn & Yahr stage 2.5 ± 0.8) had complete data and were included in the analyses. The majority of participants (84.1%) resided with someone else at home, suggesting they had family or caregiver support at home. Additionally, approximately one-third (33.3%) received assistance from social security, signifying a certain degree of limitation in their Activities of Daily Living (ADLs).
Table 1 presents sample demographics and disease-related characteristics.
Descriptive statistics of the measured variables
Table 2 presents descriptive statistics of disease severity, health behaviors, function, and HRQoL.
Utilization of rehabilitative treatment was as follows: 14.8% (n = 13) attended physical therapy; 2.3% (n = 2), occupational therapy; 5.7% (n = 5), hydrotherapy; 2.3% (n = 2), speech and language pathology; and 2.3% (n = 2), psychology. Since utilization of healthcare services was almost negligible, this variable was not included in the regression analysis.
Overall, 8% of the participants were assigned PAM Level 1 (PAM ≤ 47), 10.2% were assigned PAM Level 2 (47 < PAM ≤ 55), 43.2% were assigned PAM Level 3 (55 < PAM ≤ 67), and 38.6% were assigned PAM Level 4 (PAM > 67).
Correlations between study variables
A preliminary Pearson correlation analysis of the research variables (see Additional file 1) revealed significant correlations between the variables, ranging from r = 0.22 to r = 0.70. These results confirmed the relevance of the selected variables for the model.
Multiple regression analyses for function
In the final iteration, multiple linear regression was used to test if IPAQ, PAM and MDS-UPDRS were significantly associated with function. A summary of each iteration model is presented in Table 3 and the complete results of the final model are presented in Table 4.
The overall regression was statistically significant (R2adj = 0.51, F(3, 83) = 31.23, p < 0.001). IPAQ and PAM were found to be significantly associated with function (b = 0.41, p < 0.001; b = 0.2, p = 0.02 respectively). Disease severity, indicated by MDS-UPDRS, was also found to be significantly associated with function (b = − 0.4, p < 0.0001).
Multiple regression analyses for HRQoL
In the final iteration, multiple linear regression was used to test if age, NMSQ, MDS-UPDRS, IPAQ, NMSQ × IPAQ, and MDS-UPDRS × IPAQ were significantly associated with HRQoL. A summary of each iteration model is presented in Table 5 and the complete results of the final model are presented in Table 6.
The overall regression was statistically significant (R2ad = 0.52, F(6, 81) = 16.98, p < 0.001). IPAQ was found to be significantly associated with HRQoL (b = 0.19, p = 0.03). Disease severity as indicated by the NMSQ but not MDS-UPDRS was significantly associated with HRQoL (b = − 0.57, p < 0.001). Age was significantly associated with HRQoL (b = 0.19, p = 0.02). The interactions NMSQ × IPAQ and MDS-UPDRS × IPAQ were also significantly associated with HRQoL (b = 0.19, p = 0.02; b = − 0.23, p = 0.01, respectively).
The interactions effects found showed that the strength of the association between IPAQ and HRQoL is a function of the NMSQ or MDS-UPDRS scores. It also showed that the direction of the interactions is opposite such that the association between IPAQ and HRQoL is stronger among people with higher NMSQ scores (i.e., more non-motor symptoms; Fig. 1A), while the association is stronger among people with lower MDS-UPDRS scores (i.e., fewer motor symptoms) (Fig. 1B).
A Two-way interaction effect NMSQ*IPAQ on HRQoL (NMSQ levels are represented as mean (solid line), + 1SD (dashed line) and -1SD (spaced dashed line) slopes). IPAQ, International Physical Activity Questionnaire; NMSQ, Non-Motor Symptoms Questionnaire; HRQoL, Health-related quality of life; SD, standard deviation and B Two-way interaction effect MDS-UPDRS*IPAQ on HRQoL (MDS-UPDRS levels are represented as mean (solid line), + 1SD (dashed line) and -1SD (spaced dashed line) slopes). IPAQ, International Physical Activity Questionnaire; HRQoL, Health-related quality of life; MDS-UPDRS, Movement Disorders Society Unified Parkinson’s disease rating scale; SD, standard deviation
Discussion
This study provides information on PwPs’ self-reported engagement in PD-related health behaviors. We found that many patients do not utilize rehabilitative treatments. For example, only 14.8% of PwP in our study utilized physical therapy. This is in the lower range of rates previously reported in other countries, which ranged for physical therapy from 14% in the United States to 60% in the Netherlands [18, 43,44,45]. Among the services on which participants reported, physical therapy had the highest utilization rate, while hydrotherapy, occupational therapy, and speech and language pathology had substantially lower rates. Our findings may be explained by barriers at the individuals and healthcare-system levels that impede PwPs’ utilization of these services, such as patients’ or physicians’ low awareness of the benefits of rehabilitation treatments, low availability and accessibility of rehabilitation services [46], and possibly low health insurance literacy [47]. Furthermore, at the healthcare-system level, there is a notable absence of practical framework for the delivery of rehabilitative treatments in progressive chronic disease such as PD.
The IPAQ Research Committee [48] suggests a cutoff value of 600 MET-min/week to distinguish between people engaged in light and moderate levels of physical activity and 3000 MET-min/week to distinguish between people engaged in moderate and vigorous levels of activity. Accordingly, our sample was engaged in physical activity at a moderate level (mean ± SD score = 1876.74 ± 2127.04 MET-min/week). This is similar to the level of physical activity previously reported in PwP in an Australian cohort (1823.6 ± 1693.6 MET-min/week) [49].
Average PAM scores and distributions across PAM levels were similar to those reported for other chronic diseases, such as cancer, diabetes mellitus, and asthma [49]. For example, Hibbard et al. [50] reported a mean PAM score of 64.2 in these populations, in comparison to 67.3 in our study. Most of our participants were at level 3 or 4, indicating high levels of patient activation. It is possible that this finding is biased by the fact that our participants were recruited from a Movement Disorder Institute and thus were already relatively active in managing their care and might have knowledge about their disease. The discrepancy between the moderate-high level of activation and the very low engagement in rehabilitative treatments reveals heterogeneity across the dimensions of health behaviors. Specifically, it shows that a person may have the knowledge, skills, and confident to self-manage their disease, yet fail to take actual steps to engage in health behavior actions. Thus, these findings underscore that the construct of health behaviors in PD is complex and requires multidimensional assessment.
The study results show associations between health behaviors (including physical activity and patient activation) and function. These behaviors, in combination with motor symptom severity, explain approximately 50% of the variance in function. Findings also show that physical activity (but not patient activation) and its interactions with motor and the non-motor symptoms of PD are associated with HRQoL. In combination with age and non-motor symptoms, physical activity explains approximately 50% of the variance in HRQoL. This structure of relationships was not previously demonstrated.
Higher levels of physical activity have been associated with higher function and quality of life in other chronic diseases [51,52,53], and specifically in PD [30, 54]. Our results highlight the role of disease severity in the association between physical activity and HRQoL. Physical activity has a greater contribution to HRQoL in patients with more non-motor symptoms relative to those with fewer non-motor symptoms. In contrast to the effects of motor symptoms, the presence of non-motor symptoms does not seem to limit the potential of physical activity to improve HRQoL. The clinical implications of this finding supports the importance of engaging in physical activity even for patients with advanced non-motor symptoms. However, greater severity of motor symptoms may diminish the positive effect of physical activity on HRQoL. The interaction effect of severity may be unique to PD, as the disease is characterized by a very wide spectrum of debilitating symptoms across many body systems.
Specific novel insights gained in our study refer to the role of patient activation. Prior literature on chronic diseases associated higher patient activation with reduced disease-related symptoms, and with higher HRQoL and function [23, 55, 56]. To the best of our knowledge, this is the first study to report an association between patient activation and function in PwP. In a recent study [57], PwP with higher levels of patient activation were less susceptible to the negative impact of COVID-19-imposed social distancing [57]. The finding of the current study joins these findings and suggests that patient activation has a positive impact on function in PwP. Patient activation was not associated with HRQoL. The measurement of patient activation mainly relates to patients’ readiness to take action and, to a lesser degree, to aspects of patients’ emotional coping. This may explain why PAM was associated with function but not with HRQoL.
Policy implications: this study draws the attention to health behaviors of PwP. Our findings emphasize the connection between physical activity and patient engagement and function. This highlights the need for policymakers to make physical activity opportunities more available and accessible for PwP within the healthcare system. This trend aligns with the growing recognition of physical activity as a key aspect of managing various chronic conditions. Furthermore, our study reveals that rehabilitative healthcare services are being underutilized by PwP, despite the known benefits these services offer for health and quality of life. To increase the utilization of rehabilitative treatments, there is a need to address not only aspects related to patients but also healthcare policy. Healthcare organizations could adopt a proactive approach by providing educational materials on the benefits of rehabilitative care, encouraging general practitioners to refer PwP to such services, and actively engaging PwP in specialized programs like exercise groups within community clinics. Informative brochures about the benefits of rehabilitative care and information about what the patient needs to do in bureaucratic matters to receive treatment could be distributed to patients by general practitioners, neurologists, allied health professionals, or through patient organizations (such as the Israel Parkinson Association). The value of knowledge and information for treatment utilization and adherence was supported in research among PwP [58, 59]. As to encouraging general practitioners to refer PwP to rehabilitative treatments, we suggest that the utilization of these services may be considered a quality indicator of the treatment of PwP. This is aligned with current guidelines and improve utilization rates. Health maintenance organizations (HMOs) should enhance opportunities for engaging in rehabilitative activities. This necessitates establishing specific services like group training and multidisciplinary rehabilitation within the community.
Our study has several limitations. Participants’ cognitive status was informally evaluated by the treating neurologist. Utilization of rehabilitative treatments was not included in the analysis due to very low rates of utilization. Level of physical activity relied on responses to a self-report questionnaire (IPAQ). Future research may use objective measures such as activity monitors. In addition, previous physical activity was not documented. Future research could encompass long-term physical activity to gain a more thorough understanding of how it relates to function and HRQoL.
Conclusions
The results of this study showed underutilization of an important domain of health behaviors that have potential benefits for PwP, i.e., treatments by health professionals. The associations found support the hypothesis that health behaviors are important for maintaining function and HRQoL in PwP. They also reveal that motor and non-motor symptoms have a differential contribution to the association between physical activity and quality of life.
Practice implications
Our study has clinical implications. Patients and physicians should be made aware of the scientific evidence supporting the positive impacts of rehabilitative treatments on disease severity, function, and HRQoL in PwP, in order utilization. In addition, our findings support facilitation of patient activation as a tool to promote HRQoL and maintain function, through the development and implementation of support programs that provide access to knowledge and training in self-management skills.
Availability of data and materials
The data analyzed during the current study are available at: https://zenodo.org/deposit/5931646
Abbreviations
- PD:
-
Parkinson’s disease
- PwP:
-
People living with PD
- HRQoL:
-
Health-related quality of life
- MDS-UPDRS:
-
Unified Parkinson’s disease rating scale
- NMSQ:
-
Non-motor symptoms questionnaire score
- LEDD:
-
Levodopa equivalent daily dose
- IPAQ-Short:
-
International physical activity questionnaire–short version
- PAM-13:
-
Patient’s activation measure
- FAI:
-
Frenchay activities index
- 10-MWT:
-
10 meter walk test
- PDQ-39:
-
PD questionnaire–39
- SD:
-
Standard deviation
- MSPSS score:
-
Multidimensional scale of perceived social support
References
DeMaagd G, Philip A. Parkinson’s disease and its management: part 1: disease entity, risk factors, pathophysiology, clinical presentation, and diagnosis. PT. 2015;40:504.
Poewe W, Seppi K, Tanner C, Halliday GM, Brundin P, Volkmann J, et al. Parkinson disease. Nat Rev Dis Prim. 2017;3:1–53.
Dorsey ER, Bloem BR. The Parkinson pandemic—a call to action. JAMA Neurol. 2018;75:9–10.
Zhang Y, Wang C, Wang Y, Xiao Q, Liu J, Ma J, et al. Parkinsonism and related disorders mortality from Parkinson’s disease in China: findings from a ten-year follow up study in Shanghai. Park Relat Disord. 2018;55:75–80.
Ishihara LS, Cheesbrough A, Brayne C, Schrag A. Estimated life expectancy of Parkinson’s patients compared with the UK population. J Neurol Neurosurg Psychiatry. 2007;78:1304–9.
Schrag A, Hommel ALAJ, Lorenzl S, Meissner WG, Odin P, Coelho M, et al. The late stage of Parkinson’s –results of a large multinational study on motor and non-motor complications. Park Relat Disord. 2020;75:91–6.
Hommel ALAJ, Meinders MJ, Lorenzl S, Dodel R, Coelho M, Ferreira JJ, et al. The prevalence and determinants of neuropsychiatric symptoms in late-stage Parkinsonism. Mov Disord Clin Pract. 2020;75:91–6.
Lee MA, Prentice WM, Hildreth AJ, Walker RW. Measuring symptom load in Idiopathic Parkinson’s disease. Park Relat Disord. 2007;13:284–9.
Grady PA, Gough LL. Self-management: a comprehensive approach to management of chronic conditions. Am J public Health. 2014;104:e25-31.
Nolte E, Knai C, Saltman RB, World Health Organization. Assessing chronic disease management in European health systems. Concepts and approaches. 2014.
Brady TJ, Sacks JJ, Terrillion AJ, Colligan EM. Operationalizing surveillance of chronic management support. Prev Chronic Dis. 2018;15:1–15.
Gochman DS. Health behavior research, Definitions and diversity. In: Handbook of health behavior research I: personal and social determinants. 1997;1:3–20.
Bloem BR, de Vries NM, Ebersbach G. Nonpharmacological treatments for patients with Parkinson’s disease. Mov Disord. 2015;30:1504–20.
Radder DLM, Nonnekes J, Van Nimwegen M, Eggers C, Abbruzzese G, Alves G, et al. Recommendations for the organization of multidisciplinary clinical care teams in Parkinson’s disease. J Parkinsons Dis. 2020;10:1087–98.
Cosentino C, Baccini M, Putzolu M, Ristori D, Avanzino L, Pelosin E. Effectiveness of physiotherapy on freezing of gait in Parkinson’s disease: a systematic review and meta-analyses. Mov Disord. 2020;35:523–36.
Radder DLM, Silva L, de Lima A, Domingos J, Keus SHJ, van Nimwegen M, Bloem BR, et al. Physiotherapy in Parkinson’s disease: a meta-analysis of present treatment modalities. Neurorehabil Neural Repair. 2020;34:871–80.
Mak MK, Wong-Yu IS, Shen X, Chung CL. Long-term effects of exercise and physical therapy in people with Parkinson disease. Nat Rev Neurol. 2017;13:689–703.
Seo HG, Park SJ, Seo J, Byun SJ, Oh BM. Rehabilitation therapy utilization in patients with Parkinson’s disease in Korea. Parkinsons Dis. 2018.
Hirsch MA, van Wegen EEH, Newman MA, Heyn PC. Exercise-induced increase in brain-derived neurotrophic factor in human Parkinson’s disease: a systematic review and meta-analysis. Transl Neurodegener. 2018;7:1–2.
Ahlskog JE. Aerobic exercise: evidence for a direct brain effect to slow Parkinson disease progression. In: Mayo clinic proceedings 2018; 93: 360–372. Elsevier.
Da Silva FC, Iop RDR, De Oliveira LC, Boll AM, De Alvarenga JGS, Filho PJBG, et al. Effects of physical exercise programs on cognitive function in Parkinson’s disease patients: a systematic review of randomized controlled trials of the last 10 years. PLoS ONE. 2018;13: e0193113.
Uhrbrand A, Stenager E, Pedersen MS, Dalgas U. Parkinson’s disease and intensive exercise therapy—A systematic review and meta-analysis of randomized controlled trials. J Neurol Sci. 2015;353:9–19.
Mosen DM, Schmittdiel J, Hibbard J, Sobel D, Remmers C, Bellows J. Is Patient activation associated with outcomes of care for adults with chronic conditions? J Ambul Care Manage. 2007;30:21–9.
Greene J, Hibbard JH. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J Gen Intern Med. 2012;27:520–6.
Greene J, Hibbard JH, Sacks R, Overton V, Parrotta CD. When patient activation levels change, health outcomes and costs change. Too Health Aff. 2015;34:431–7.
Tomlinson CL, Patel S, Meek C, Herd CP, Clarke CE, Stowe R, et al. Physiotherapy versus placebo or no intervention in Parkinson’s disease. Cochrane Database Syst Rev. 2013(9).
Sturkenboom IH, Graff MJ, Hendriks JC, Veenhuizen Y, Munneke M, Bloem BR, et al. Efficacy of occupational therapy for patients with Parkinson’s disease: a randomised controlled trial. Lancet Neurol. 2014;13:557–66.
Herd CP, Tomlinson CL, Deane KH, Brady MC, Smith CH, Sackley CM, et al. Speech and language therapy versus placebo or no intervention for speech problems in Parkinson’s disease. Cochrane Database Syst Rev. 2001(2).
Radder DL, Sturkenboom IH, Van Nimwegen M, Keus SH, Bloem BR, De Vries NM. Physical therapy and occupational therapy in Parkinson’s disease. Int J Neurosci. 2017;127:930–43.
Lauzé M, Daneault JF, Duval C. The effects of physical activity in Parkinson’s disease: a review. J Park Dis. 2016;6:685–98.
Hagströmer M, Oja P, Sjöström M. The international physical activity questionnaire (IPAQ): a study of concurrent and construct validity the international physical activity questionnaire (IPAQ): a study of concurrent and construct validity. Public Health Nutr. 2006;9:755–62.
Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the patient activation measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39:1005–26.
Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005;40:1918–30.
Zitser J, Peretz C, Ber David A, Shabtai H, Ezra A, Kestenbaum M, et al. Validation of the hebrew version of the movement disorder society—unified Parkinson’s disease rating scale. Park Relat Disord. 2017;45:7–12.
Chaudhuri KR, Martinez-Martin P, Schapira AHV, Stocchi F, Sethi K, Odin P, et al. International multicenter pilot study of the first comprehensive self-completed nonmotor symptoms questionnaire for Parkinson’s disease: the NMSQuest study. Mov Disord. 2006;21:916–23.
Tomlinson CL, Stowe R, Patel S, Rick C, Gray R, Clarke CE. Systematic review of levodopa dose equivalency reporting in Parkinson ‘s disease. Mov Disord. 2010;25:2649–53.
Julien C, Hache G, Dulac M, Dubrou C, Castelnovo G, Giordana C, et al. The clinical meaning of levodopa equivalent daily dose in Parkinson’s disease. Fundam Clin Pharmacol. 2021;35:620–30.
Holbrook M, Skilbeck CE. An activities index for use with stroke patients. Age Ageing. 1983;12:166–70.
Paker N, Bugdayci D, Goksenoglu G, Demircioğlu DT, Kesiktas N, Ince N. Gait speed and related factors in parkinson’s disease. J Phys Ther Sci. 2015;27:3675–9.
Paltamaa J, Sarasoja T, Leskinen E, Wikström J, Mälkiä E. Measures of physical functioning predict self-reported performance in self-care, mobility, and domestic life in ambulatory persons with multiple sclerosis. Arch Phys Med Rehabil. 2007;88:1649–57.
Kim HJ, Park I, Lee HJ, Lee O. The reliability and validity of gait speed with different walking pace and distances against general health, physical function, and chronic disease in aged adults. J Exerc Nutr Biochem. 2016;20:46.
Jenkinson C, Fitzpatrick RAY, Peto VIV, Greenhall R. The Parkinson’s disease questionnaire (PDQ-39): development and validation of a Parkinson’s disease summary index score. Age Ageing. 1997;26:353–7.
Gal O, Srp M, Konvalinkova R, Hoskovcova M, Capek V, Roth J, et al. Physiotherapy in Parkinson’s disease: building ParkinsonNet in Czechia. Parkinsons Dis. 2017;2017:22.
Keus SH, Bloem BR, Verbaan D, De Jonge PA, Hofman M, Van Hilten BJ, et al. Physiotherapy in Parkinson’s disease: utilisation and patient satisfaction. J Neurol. 2004;251:680–7.
Fullard ME, Thibault DP, Hill A, Fox J, Bhatti DE, Burack MA, et al. Utilization of rehabilitation therapy services in Parkinson disease in the United States. Neurology. 2017;89:1162–9.
Cavaglion A, Duvdevani M, Siegelman NA, Kizony R, Yogev-Seligmann G. Occupational therapy for people with Parkinson’s disease in Israel: a SWOT analysis. Scand J Occup Ther. 2022.
Yagi BF, Luster JE, Scherer AM, Farron MR, Smith JE, Tipirneni R. Association of health insurance literacy with health care utilization: a systematic review. J Gen Intern Me. 2022.
IPAQ Research Committee. Guidelines for data processing and analysis of the international physical activity questionnaire (IPAQ)—short and long forms. http://www.ipaq.ki.se/scoring.pdf. 2005.
Lubomski M, Davis RL, Sue CM. Depression in Parkinson’s disease: perspectives from an Australian cohort. J Affect Disord. 2020;277:1038–44.
Hibbard JH, Cunningham PJ. How engaged are consumers in their health and health care, and why does it matter? Washington, DC: Center for Studying Health System Change; 2008.
Béland M, Lavoie KL, Briand S, White UJ, Gemme C, Bacon SL. Aerobic exercise alleviates depressive symptoms in patients with a major non-communicable chronic disease: a systematic review and meta-analysis. Br J Sports Med. 2020;54:272–8.
Cai H, Li G, Hua S, Liu Y, Chen L. Effect of exercise on cognitive function in chronic disease patients: a meta-analysis and systematic review of randomized controlled trials. Clin Interv Aging. 2017;12:773.
Pasanen T, Tolvanen S, Heinonen A, Kujala UM. Exercise therapy for functional capacity in chronic diseases: an overview of meta-analyses of randomised controlled trials. Br J Sports Med. 2017;51:1459–65.
Lauzé M, Daneault JF, Duval C. The effects of physical activity in Parkinson’s disease: a review. J Parkinsons Dis. 2016;6(4):685–98.
Kukla M, Salyers MP, Lysaker PH. Levels of patient activation among adults with schizophrenia: associations with hope, symptoms, medication adherence, and recovery attitudes. J Nerv Ment Dis. 2013;201:339–44.
Sacks RM, Greene J, Hibbard J, Overton V, Parrotta CD. Does patient activation predict the course of type 2 diabetes? A longitudinal study. Patient Educ Couns. 2017;100:1268–75.
Yogev-Seligmann G, Kafri M. COVID-19 social distancing: Negative effects on people with Parkinson disease and their associations with confidence for self-management. BMC Neurol. 2021;21:1–8.
Mendorf S, Witte OW, Grosskreutz J, Zipprich HM, Prell T. What predicts different kinds of nonadherent behavior in elderly people with Parkinson’s disease? Front Med. 2020;7:103.
Ellis T, Boudreau JK, DeAngelis TR, Brown LE, Cavanaugh JT, Earhart GM, et al. Barriers to exercise in people with Parkinson disease. Phys Ther. 2013;1(93):628–36.
Acknowledgements
We are grateful to the study participants for their generous time when participating in this study.
Funding
This work was supported by Faculty of Social Welfare & Health Sciences, University of Haifa and Rambam Health Care Campus under Grant 10/12-83 and by internal grant from the Center for Research and Study of Aging, Faculty of Social Welfare & Health Sciences, University of Haifa.
Author information
Authors and Affiliations
Contributions
GYS and MK conceived the study design. IS, MN, and RH recruited subjects and MD performed the measurements. IS and IE were responsible for project administration. MK, GYS and MD analyzed the data and drafted the manuscript with inputs from all co-authors. IS, MN and RF contributed to the critical revision of the manuscript. GYS, MK and IS supervised the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All participants provided informed consent. The study was approved by the ethical Ethics Committee of the Faculty of Social Welfare & Health Sciences, University of Haifa (approval number 471/18) and complied with the Declaration of Helsinki, and was also approved by the Helsinki committee of Rambam Health Care Campus (Application number 0067-19-RMB).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Correlations between study variables.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Duvdevani, M., Yogev-Seligmann, G., Schlesinger, I. et al. Association of health behaviors with function and health-related quality of life among patients with Parkinson’s disease. Isr J Health Policy Res 13, 2 (2024). https://doi.org/10.1186/s13584-023-00588-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13584-023-00588-3