Abstract
Background
To investigate whether modifiable predictors (depressive symptoms, impairment in behavior and mood, balance impairments, and knee extensor muscle strength) are determinants of the physical activity level in Parkinson’s disease.
Materials and methods
A cross-sectional study with individuals diagnosed with idiopathic Parkinson’s disease. Regression analysis of the data was used to investigate whether depressive symptoms, impairments in behavior and mood, balance impairments, or dominant knee extensor muscle strength are predictors of physical activity levels in Parkinson’s disease.
Results
A total of 50 individuals with mild to moderate Parkinson’s disease participated in this study, with a mean age of 67 ± 8 years and 68% male. Balance impairments explained 29% of the variation in the physical activity levels. The explained variance increased to 34% when depressive symptoms were included in the model.
Conclusion
Among the predictor variables investigated in our study, only balance impairments and depressive symptoms explained the variance in physical activity levels in individuals with Parkinson’s disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Individuals with Parkinson’s disease have motor and non-motor symptoms which can cause disabilities which in turn affect their physical activity levels (PAL) [1]. PAL is defined as any body movement generated by skeletal muscles resulting in energy expenditure [2, 3]. The main recognized motor symptoms referred to as cardinal signs of Parkinson’s disease are resting tremor, bradykinesia, rigidity, and postural instability [4]. In addition, individuals with Parkinson’s disease usually present depressive symptoms, impairment in behavior and mood, balance impairments, and lower limb muscle weakness [5,6,7,8]. Although muscle weakness is not a primary sign of Parkinson’s disease, weakness is observed in several muscle groups [6]. However, it is not known what the influence of these variables is on the physical activity levels of these individuals.
Previous studies have shown that regular physical activity is an effective way of controlling the motor symptoms of the disease and depressive symptoms and improves the functionality of individuals [9, 10]. Furthermore, it is known that physical activity has a neuroprotective effect and can reduce vulnerability to dopamine aggressors and promote neuroplasticity [11]. Thus, staying active is of paramount importance to minimize the functional impairments of Parkinson’s disease and delay its evolution [10,11,12].
Some studies have already evaluated potential determinants of physical activity in Parkinson’s disease and have suggested that maintaining high physical activity levels would be associated with age, gender, income, social support, education, lower bradykinesia, and higher severity of the disease, among other non-modifiable variables [13,14,15,16]. However, there are few studies in the literature investigating modifiable variables as predictors of physical activity practice in Parkinson’s disease [6, 8] which can be addressed in rehabilitation programs.
In order to contribute to formulating new intervention strategies, we seek to understand the influence of modifiable predictors on the physical activity level in individuals with Parkinson’s disease. Considering that a portion of these remain poorly explained [13, 15], the present study aimed to investigate whether modifiable predictors (depressive symptoms, impairment in behavior and mood, balance impairments, and knee extensor muscle strength) are determinants of the physical activity level in Parkinson’s disease.
Design and methods
Study design and ethical considerations
This is a cross-sectional study approved by the Ethics Committee of the Faculdade Ciências Médicas de Minas Gerais (CAAE:10047219.2.0000.5134), with individuals diagnosed with idiopathic Parkinson’s disease, from April 2019 to January 2020. All participants signed an informed consent form.
Participants
Participants in this study were individuals diagnosed with idiopathic Parkinson’s disease, recruited by phone from a previous research contact database. Individuals were contacted at their home. As inclusion criteria, the individuals were to be older than 50 years and able to walk independently. Individuals who had other neurological diseases or who did not obtain an adequate score on the Mini Mental State Examination according to pre-established cut-off points in the literature (13 for individuals with illiteracy, 18 for those with elementary and middle education, and 26 for those with high education) [17] considering the years of schooling were excluded.
The sample size of at least 50 participants was based upon the formula proposed by Dohoo, Martin, and Stryhn [18], sample size = (n + 1)*10, where n = number of independent variables. Thus, four independent variables were included in the multiple regression model for this calculation.
Procedures
Sociodemographic and clinical data were collected in an interview format through a questionnaire developed by the research team. All tests and questionnaires designed to collect the variable of interest and predictors present adequate measurement properties. The questionnaires used in our study were applied individually in order to avoid potential conflicts and external influences.
The dependent variable (physical activity level) was assessed with the Human Activity Profile (HAP), which is a questionnaire consisting of 94 items of routine activities with different functional levels, sorted in order of increasing energy costs. We considered the adjusted score activity (AAS) with cut-offs defined for stratification of individuals as inactive (< 53), moderately active (53 to 74), and active (> 74) [19, 20].
The following four potential predictors were included: depressive symptoms, behavioral and mood, balance impairments, and dominant knee extensor muscle strength.
Depressive symptoms were investigated by the Patient Health Questionnaire-9 (PHQ-9), a questionnaire consisting of 9 items used to screen for symptoms such as depressed mood, anhedonia, change in appetite, and feeling of guilt. The regularity of these symptoms in the past 2 weeks was assessed on a scale of 0 to 3 corresponding to the answers “not once,” “several days,” “more than half the days,” and “almost every day”, respectively, where a score equal to or greater than 10 indicates the presence of depressive symptoms [21].
The assessment of the behavior and mood was performed by subpart I of Unified Parkinson’s Disease Rating Scale (UPDRS), which includes cognitive behavioral disorders, neuropsychiatric disorders (caused by dementia or drug toxicity), presence of depression, and reduction in motivation [22]. It consists of 4 items with a score ranging from 0 to 4, which 0 being the least compromised and 4 being the highest [23].
The assessment of balance impairments was performed with the MiniBESTest, which is a quick test application containing 14 items scored ranging from 0 to 2 and involves evaluating four areas of dynamic balance: anticipatory postural adjustments, reactive postural control, sensory orientation, and gait dynamics [24]. The application time varies between 10 and 15 min [25].
The muscle strength of the dominant knee extensor was measured in mmHg and was performed by researchers trained on the Modified Sphygmomanometer Test (MST). The cuff was inflated to 100 mmHg to remove all possible folds and then deflated to 20 mmHg, resulting in a measuring range of 20–304 mmHg [26]. The individuals and instruments were positioned according to previous recommendations [27]. Two measures were taken, one for familiarization and the other for measuring strength. Standardized verbal stimuli were given during the test to sustain a maximum isometric contraction against the device for 5 s and instructed to not perform the valsalva maneuver [26, 27].
Blood pressure, heart rate, and oxygen saturation of the individuals were continually monitored during tests.
Statistical analysis
Descriptive statistics, tests for normality (Kolmogorov-Smirnov), and equality of variances (Levene) were calculated for all outcomes. Stepwise multiple regression analysis was performed to identify which of the independent variables would significantly predict physical activity. Variable entry for the regression was set at 0.05, and removal was set at 0.10. The data were evaluated prior to performing regression to determine if they fulfill all requirements for regression analyses, such as linearity, homoscedasticity, independence, and normality of the residuals, as well as multicollinearity and outliers. All analyses were carried out with the SPSS software (version 17.0) with a significance level of 5%.
Results
From a list of 112 individuals, 51 (46%) of potential participants were excluded due to death (n = 3), incorrect contact information (n = 15), and refusals (n = 21). The most frequent reasons for refusal were disinterest (n = 5) and unavailability (n = 16). Of the 73 individuals who agreed to participate, 12 did not attend even with prior confirmation, and 11 were excluded for not reaching the cut-off score on the Mini Mental State Examination. A final sample of 50 individuals remained in the study, as shown in Fig. 1.
The mean age was 67 ± 8.0 years, with a predominance of 68% male. In addition, 90% of the individuals reported physical activity practice and/or rehabilitation at least once a week, and 63% reported having some fear of falling. The adjusted activity score of the Human Activity Profile test revealed that 26% of the individuals were considered active, 52% moderately active, and 22% inactive. The sociodemographic and clinical characteristics of the sample are described in Table 1.
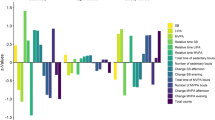
Regression analysis revealed that deficits in balance explain 29% of the variation of the physical activity level assessed by the adjusted activity score of the Human Activity Profile. The explained variance increased to 34% when depressive symptoms were included in the model. These results indicate that individuals with Parkinson’s disease who had balance impairments and depressive symptoms have a lower physical activity level.
Knee extensor muscle strength and behavior and mood impairment did not enter the model and did not significantly correlate with the physical activity level. Table 2 presents the regression analysis results.
Discussion
Balance impairments explained 29% of the physical activity level of individuals with Parkinson’s disease in our study, and this variance increased to 34% when added to depressive symptoms. These results indicate that individuals who present better balance and had lower levels of depressive symptoms were less likely to present lower physical activity levels.
A study carried out with a sample of characteristics similar to ours found no difference in the balance between active and inactive individuals [28]. In contrast, the findings of our study relate balance impairments to individuals with lower physical activity levels. In addition, about 35 to 75% of individuals with Parkinson’s disease have balance deficits with consequent fear of falling [29, 30], which was shown in a previous study to be a major barrier to adherence to exercise [8]. Data from a meta-analysis reinforced the evidence that the practice of exercise and motor training have a positive effect on balance and should therefore be included in rehabilitation programs as a strategy to reduce physical inactivity [31].
The literature supports that non-motor symptoms such as depression affect 44 to 52% of all individuals with Parkinson’s disease, and this is considered a risk factor for the development of a less active lifestyle [1]. The presence of depressive symptoms in our study explained 5% of the variation in the physical activity level of these individuals. In a recent systematic review which investigated the effects of physical activity on depressive symptoms and quality of life, a reduction was found in depression scores and in the incidence of various non-motor symptoms in active groups [32]. Also, a previous study found a relationship of depression, cognition, and quality of life in individuals with Parkinson’s disease [33]. On the other hand, evidence points out that balance and aerobic exercises have effective results which minimize worsening of depressive symptoms in Parkinson’s disease [34]. Therefore, a multiprofessional intervention can effectively contribute to changing the lifestyle of these individuals.
Although more than 70% of the activities described in HAP mainly involve lower limbs, dominant knee extensor strength could not predict physical activity. This finding may be explained by the fact that our sample obtained an average strength equal to 75% of the predicted value for age and gender considering healthy individuals [27]. Thus, muscle strength and maintenance of basic motor functions are essential for independence in Parkinson’s disease [7, 35]. Moreover, previous studies reinforce that strength training is a complementary approach of paramount importance in rehabilitation which provides benefits to other deficits related to Parkinson’s disease, such as balance [36, 37].
As far as we know, this study is the first to propose impairment in behavior and mood as variables which could influence the physical activity level in Parkinson’s disease. However, these variables did not present statistically significant values to enter the regression model. In any case, it is well known that impairments in behavior and mood, such as apathy and anxiety, are common symptoms in Parkinson’s disease and are dissociable from depression [38]. The literature suggests that non-motor symptoms in advanced cases are associated with disability and decreased quality of life [39]. Findings also suggest that individuals who have cognitive changes are more affected by impairment in behavior and mood [40]. Considering that our sample was predominantly composed of individuals with a mean of 2.5 on the Hoehn and Yahr and with preserved cognition, this may have influenced our results. Bearing in mind that there are few studies which have investigated the relationship between impairment in behavior and mood with the physical activity level in individuals with Parkinson’s disease [32, 41, 42], further studies are necessary.
The present study is not without limitations. One such limitation is related to the recruitment process, which was based upon a convenience sample. Also, although the sample size was sufficient according to the sample size calculation, it could be considered a small sample. All the implemented tests have valid and reliable measurement properties for older adults and individuals with Parkinson’s disease [19,20,21, 23, 24, 27]. The findings regarding muscle strength of the dominant knee extensor strength may have been limited due to the sample profile of this study. This is because most of the individuals reported that they were already inserted in rehabilitation programs and/or performing some physical activity, which may justify the absence of weakness of the mentioned muscle group [7, 27]. Furthermore, these changes reinforce that impairment in behavior and mood and muscle strength, as well as other variables related to Parkinson’s disease, should be investigated in future studies in order to determine their possible influence on the physical activity level.
It was reported that age, gender, marital status, disease severity, walking speed, and lower limb bradykinesia predict and explain a relevant percentage of the variance of physical activity level in individuals with Parkinson’s disease [13, 15, 16]. However, it is understood that age, gender, and marital status are variables which cannot be modified. Our study found modifiable variables such as balance impairments and depressive symptoms which explained a 34% variance in the physical activity level in individuals with Parkinson’s disease and can therefore be used as multiprofessional therapeutic intervention strategies. Based on this, the depressive symptoms should not be neglected, but evaluated with caution for rehabilitation. Balance also needs to be approached and included in rehabilitation programs so that better physical activity levels can be promoted in individuals and reduce their fear of falling.
Conclusion
Among the possible predictive variables investigated in our study, balance impairments and depressive symptoms explained the variance in the physical activity level in individuals with Parkinson’s disease. The other variables of impairment in behavior and mood and muscle strength of the dominant knee extensor did not present significant values in our sample, indicating the need for further studies.
Data availability
Not applicable.
References
Bhalsing KS, Abbas MM, Tan L (2018) Role of physical activity in Parkinson’s disease. Ann Indian Acad Neurol 21(4):242–249. https://doi.org/10.4103/aian.AIAN_169_18
Caspersen CJ, Powell KE, Christenson GM (1985) Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep 100(2):126–131
Bouça-Machado R, Rosário A, Caldeira D, Castro Caldas A, Guerreiro D, Venturelli M, Tinazzi M, Schena F, J. Ferreira J (2019) Physical activity, exercise, and physiotherapy in Parkinson’s disease: defining the concepts. Mov Disord Clin Pract 7(1):7–15. https://doi.org/10.1002/mdc3.12849
Shulman JM, Jager PL, Feany MB (2011) Parkinson’s disease: genetics and pathogenesis. Annu Rev Pathol. 6:193–222. https://doi.org/10.1146/annurev-pathol-011110-130242
Smulders K, Esselink RA, De Swart BJ et al (2014) Postural inflexibility in PD: does it affect compensatory stepping? Gait Posture. 39(2):700–706. https://doi.org/10.1016/j.gaitpost.2013.10.003
Caetano MJD, Lord SR, Allen NE, Song J, Paul SS, Canning CG, Menant JCC (2019) Executive functioning, muscle power and reactive balance are major contributors to gait adaptability in people with Parkinson’s disease. Front Aging Neurosci. 11:154. https://doi.org/10.3389/fnagi.2019.00154
Cano-de-la-Cuerda R, Pérez-de-Heredia M, Miangolarra-Page JC, Muñoz-Hellín E, Fernández-de-las-Peñas C (2010) Is there muscular weakness in Parkinson’s disease? Am J Phys Med Rehabil. 89(1):70–76. https://doi.org/10.1097/PHM.0b013e3181a9ed9b
Ellis T, Boudreau JK, DeAngelis TR et al (2013) Barriers to exercise in people with Parkinson’s disease. Phys Ther. 93(5):628–636. https://doi.org/10.2522/ptj.20120279
Van der Kolk NM, King LA (2013) Effects of exercise on mobility in people with Parkinson’s disease. Mov Disord Clin Pract 28(11):1587–1596. https://doi.org/10.1002/mds.25658
Lauhue SC, Comella CL, Tanner CM (2016) The best medicine? The influence of physical activity and inactivity on Parkinson’s disease. Mov Disord Clin Pract. 31(10):1444–1454. https://doi.org/10.1002/mds.26728
Hou L, Chen W, Liu X, Qiao D, Zhou FM (2017) Exercise-induced neuroprotection of the nigrostriatal dopamine system in Parkinson’s disease. Front Aging Neurosci. 9:358. https://doi.org/10.3389/fnagi.2017.00358
Palasz E, Niewiadomski W, Gąsiorowska A et al (2019) Exercise-induced neuroprotection and recovery of motor function in animal models of Parkinson’s disease. Front Neurol. 10:1143. https://doi.org/10.3389/fneur.2019.01143
Van NM, Speelman AD, Overeem S et al (2013) Physical inactivity in Parkinson’s disease. J Neurol. 258(2):2214–2221. https://doi.org/10.1007/s00415-011-6097-7
Ellis T, Cavanaugh JT, Earhart GM, Ford MP, Foreman KB, Fredman L, Boudreau JK, Dibble LE (2011) Factors associated with exercise behavior in people with Parkinson’s disease. Phys Ther. 91:1838–1848. https://doi.org/10.2522/ptj.20100390
Lana RC, Araújo LN, Cardoso F et al (2016) Main determinants of physical activity levels in individuals with Parkinson’s disease. ArqNeuropsiquiatr 74(2):112–116. https://doi.org/10.1590/0004-282X20160009
Andrew Z, Laura E, Alyssa S, et al (2019) Determinants of exercise behaviour in persons with Parkinson’s disease. Disabil Rehabil 1464–5165. https://doi.org/10.1080/09638288.2019.1638975
Bertolucci PHF, Brucki SMD, Campacci S et al (1994) The Mini-Mental State Examination in a general population: impact of schooling. ArqNeuropsiquiatr. 52:1–7
Dohoo IR, Martin W, Stryhn H (2003) Veterinary epidemiologic research. University of Edward Island, Charlottetown
Davidson H, Morton N (2007) A systematic review of the Human Activity Profile. Clin Rehabil. 21(2):151–162. https://doi.org/10.1177/0269215506069475
Souza AC, Magalhães LDC, Teixeira-Salmela LF (2006) Cross-cultural adaptation and analysis of the psychometric properties in the Brazilian version of the Human Activity Profile. Rep Publ Health. 22(12):2623–2636. https://doi.org/10.1590/S0102-311X2006001200012
Chagas MH, Tumas V, Rodrigues GR et al (2013) Validation and internal consistency of Patient Health Questionnaire-9 for major depression in Parkinson’s disease. Age Ageing 42(5):645–649. https://doi.org/10.1093/ageing/aft065
Fahn S, Elton R, Marsden CD et al (1987) The UPDRS development committee. Unified Parkinson’ disease rating scale. NPJ Parkinson's Dis. 2:153–163
Martignoni E, Franchignoni F, Pasetti C, Ferriero G, Picco D (2003) Psychometric properties of the unified Parkinson’s disease rating scale and of the short Parkinson’s evaluation scale. Neurol. Sci. 24(3):190–191. https://doi.org/10.1007/s10072-003-0124-0
Maia AC, Rodrigues-de-Paula F, Magalhães LC et al (2013) Cross-cultural adaptation and analysis of the psychometric properties of the Balance Evaluation Systems Test and MiniBESTest in the elderly and individuals with Parkinson’s disease: application of the Rasch model. Braz J Phys Ther 17(3):195–217. https://doi.org/10.1590/S1413-35552012005000085
Keus S, Munneke M, Graziano M, et al (2014) European physiotherapy guideline for Parkinson’s disease, 1st edition. The Netherlands
Souza LAC, Martins JC, Teixeira-Salmela LF et al (2013) Evaluation of muscular strength with the modified sphygmomanometer test: a review of the literature. Fisioter Mov 26(2):437–452. https://doi.org/10.1590/S0103-51502013000200021
Benfica PD, Aguiar LT, Brito SA et al (2018) Reference values for muscle strength: a systematic review with a descriptive meta-analysis. Braz J Phys Ther 22(5):355–369. https://doi.org/10.1016/j.bjpt.2018.02.006
Santos PCR, Morais LC, Simieli L et al (2016) Comparison of balance and functional mobility among active and inactive patients with Parkinson’s disease. Rev Bras AtivFísSaúde 21(6):534–541. https://doi.org/10.12820/rbafs.v.21n6p534-541
Nilsson MH, Hariz GM, Iwarsson S, Hagell P (2012) Walking ability is a major contributor to fear of falling in people with Parkinson's disease: implications for rehabilitation. Park Dis. 2012:713236. https://doi.org/10.1155/2012/713236
Lindholm B, Hagell P, Hansson O, Nilsson MH (2014) Factors associated with fear of falling in people with Parkinson’s disease. BMC Neurol. 14(19):1–7. https://doi.org/10.1186/1471-2377-14-19
Allen NE, Sherrington C, Paul SS, Canning CG (2011) Balance and falls in Parkinson’s disease: a meta-analysis of the effect of exercise and motor training. Mov Disord Clin Pract. 26(9):1605–1615. https://doi.org/10.1002/mds.23790
Wu PL, Lee M, Huang TT (2017) Effectiveness of physical activity on patients with depression and Parkinson’s disease: a systematic review. PLoS One. 12(7):1–14. https://doi.org/10.1371/journal.pone.0181515
van Uem JMT, Cerff B, Kampmeyer M, Prinzen J, Zuidema M, Hobert MA, Gräber S, Berg D, Maetzler W, Liepelt-Scarfone I (2018) The association between objectively measured physical activity, depression, cognition, and health-related quality of life in Parkinson’s disease. Parkinsonism Relat Disord. 48:74–81. https://doi.org/10.1016/j.parkreldis.2017.12.023
Cruickshank TM, Reyes AR, Ziman MR (2015) A systematic review and meta-analysis of strength training in individuals with multiple sclerosis or Parkinson’s disease. Medicine. 94(4):411. https://doi.org/10.1097/MD.0000000000000411
Altmann LJP, Stegemöller E, Hazamy AA, Wilson JP, Bowers D, Okun MS, Hass CJ (2016) Aerobic exercise improves mood, cognition, and language function in Parkinson’s disease: results of a controlled study. J Int Neuropsychol Soc. 22(9):878–889. https://doi.org/10.1017/S135561771600076X
Cherup NP, Buskard ANL, Strand KL et al (2019) Power vs strength training to improve muscular strength, power, balance and functional movement in individuals diagnosed with Parkinson’s disease. Exp Gerontol 128:110740. https://doi.org/10.1016/j.exger.2019.110740
Ramazzina I, Bernazzoli B, Costantino C (2017) Systematic review on strength training in Parkinson’s disease: an unsolved question. Clin Interv Aging. 12:619–628. https://doi.org/10.2147/CIA.S131903
Kirsch-Darrow L, Fernandez HH, Marsiske M et al (2006) Dissociating apathy and depression in. Park Dis Neurol 67(1):33–38. https://doi.org/10.1212/01.wnl.0000230572.07791.22
Martinez-Martin P, Rodriguez-Blazquez C, Kurtis MM et al (2011) The impact of non-motor symptoms on the health-related quality of life of patients with Parkinson’s disease. Mov Disord Clin Pract 26(3):399–406. https://doi.org/10.1002/mds.23462
Jones JD, Mangal P, Lafo J, Okun MS, Bowers D (2016) Mood differences among Parkinson’s disease Patients with mild cognitive impairment. J Neuropsy Clin Neurosci. 28(3):211–216. https://doi.org/10.1176/appi.neuropsych.15090221
Todorova A, Jenner P, Ray CK (2014) Non-motor Parkinson’s: integral to motor Parkinson’s, yet often neglected. Pract Neurol. 14(5):310–322. https://doi.org/10.1136/practneurol-2013-000741
Amara AW, Memon AA (2018) Effects of exercise on non-motor symptoms in Parkinson’s disease. Clin Ther. 40(1):8–15. https://doi.org/10.1016/j.clinthera.2017.11.004
Acknowledgments
We appreciate the support of the Research and Extension Sector of the Faculdade Ciências Médicas de Minas Gerais and to all the participants who contributed to the realization of this study.
Funding
This study was supported by the Institutional Funding Agency PROBIC (Programa Institucional de Bolsas da Faculdade Ciências Médicas de Minas Gerais).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Jéssica Soares Feliciano, Samara Maria Alves Rodrigues, Raquel de Carvalho Lana, and Janaine Cunha Polese. The first draft of the manuscript was written by Jéssica Soares Feliciano and Samara Maria Alves Rodrigues. The authors Raquel de Carvalho Lana and Janaine Cunha Polese commented on previous versions of the manuscript. The authors are responsible for the content and writing of this article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethics approval
This study was approved by the ethics and Institutional Research Committee on April 4, 2019 (CAAE: 10047219.2.0000.5134).
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Patients signed informed consent regarding publishing their data.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Feliciano, J.S., Rodrigues, S.M.A., de Carvalho Lana, R. et al. Predictors of physical activity levels in individuals with Parkinson’s disease: a cross-sectional study. Neurol Sci 42, 1499–1505 (2021). https://doi.org/10.1007/s10072-020-04701-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-020-04701-1