Abstract
Background
Hereditary spherocytosis (HS, MIM#612641) is one of the most common hereditary hemolytic disorders. This study aimed to confirm a novel variant’s pathogenicity and reveal a patient’s genetic etiology.
Methods
The clinical data of a patient with HS who underwent genetic sequencing at the Children’s Hospital of Chongqing Medical University were reviewed retrospectively. In silico prediction and in vitro minigene splicing reporter system were then conducted on the detected variant to analyze its intramolecular impact. A summary of the literature related to HS due to SPTB gene variants was also presented.
Results
A novel variant (c.301–2 A > G) in the SPTB gene (NM_001024858.4) was identified in the proband. Using Sanger sequencing, we conclusively confirmed that the inheritance of the variant could not be traced to the biological parents. The in vitro minigene assay revealed three different transcripts derived from the c.301–2 A > G variant: r.301_474del, r.301_306delCCAAAG, and r.301-1_301-57ins. Through a literature review, patients with HS who had been genotypically validated were summarized and the SPTB gene variant profile was mapped.
Conclusion
We identified a splicing variant of the SPTB gene, thus confirming its aberrant translation. The novel variant was the probable genetic etiology of the proband with HS. Our findings expanded the variant spectrum of the SPTB gene, thus improving the understanding of the associated hereditary hemolytic disorders from a clinical and molecular perspective and contributing to the foundation of genetic counseling and diagnosis.
Similar content being viewed by others
Introduction
Hereditary spherocytosis (HS, MIM#612641) is a red blood cell (RBC) membrane disorder caused by gene variants. It is one of the most common nonimmune congenital hemolytic anemia, with typical manifestations of yellow discoloration of the sclera and skin, anemia, and hepatosplenomegaly [1]. It is well documented globally that HS is a highly prevalent form of hereditary anemia among individuals of Northern European and Northern American descent, with an incidence rate of approximately 1 in 5,000 to 1 in 2,000 [2]. A few sporadic cases of HS have also been reported in mainland China; however, there is a lack of precise incidence rate data. This may be attributed to the difficulties in diagnosing HS in clinical practice. Ideally, HS diagnosis should be combined with laboratory test results; however, laboratory test results can be easily affected, and have a chance of resulting in false-positive or false-negative errors [3]. An increase in spherocytes in a blood smear is an important indicator of HS, but it is not a unique feature of the disease and is only used to screen for typical cases [4]. As next-generation sequencing (NGS) continues to advance, molecular detection of HS-related genes is currently considered the new diagnostic standard [5]. A positive result from genetic sequencing can be regarded as a diagnostic basis for HS [6].
As humanity is gradually entering the era of genomic medicine, an increasing number of pathogenic variant sites associated with HS are being detected. However, most of these variants are likely pathogenic or variants of uncertain significance, thus making the interpretation and prediction of pathogenicity for such variant sites challenging for clinicians as well as researchers [7]. Therefore, it is crucial to conduct in-depth research on the clinical significance of unknown variants and further expand the HS pathogenic gene variant database for disease prevention, which would be particularly helpful for genetic counseling and screening of asymptomatic family members [8].
In this study, we recruited a Han Chinese patient who displayed typical manifestations of HS and his family. A novel splicing variant, c.301–2 A > G, was identified in the SPTB gene through gene sequencing. To further verify the function of the detected variant, we performed an in vitro minigene assay, which enabled us to assess its impact on splicing patterns and confirm its pathogenicity. Furthermore, the variant spectrum of the SPTB gene was mapped based on the results of literature searches.
Materials and methods
Participants and ethical approval
In this study, we recruited a Han Chinese family with clinically suspected HS. The proband in the enrolled pedigree exhibited symptoms of anemia; however, the parents were healthy. Data was collected through face-to-face interviews and medical record abstractions.
The study protocol was approved by the Ethics Review Committee of the Children’s Hospital of Chongqing Medical University and was conducted in accordance with the Declaration of Helsinki declaration. Data analysis and blood sample collection were conducted after written informed consent was obtained from the participants.
NGS, paternity testing and Sanger sequencing
A sequencing panel of 700 pathogenic genes associated with hematological genetic diseases and immunodeficiency disorders was used for genetic testing. The gene panel targeted all exons and flanking intronic regions of five HS-associated genes: SPTA1, SPTB, ANK1, SLC4A1, and EPB42. Genomic DNA (gDNA) was extracted from the peripheral blood of all the family members using the QIAamp DNA Blood Mini Kit (Qiagen, China). DNA concentration was measured using NanoDrop 2000 (Thermo Fisher Scientific, USA). Standard Illumina libraries were constructed using qualified gDNA with Invitrogen Collibri DNA Library Prep Kit (Thermo Fisher Scientific, USA). Polymerase chain reaction (PCR) was used to amplify the target genes, and the amplified products were sequenced using the Illumina HiSeq X Ten platform. (Illumina, USA). The average sequencing depth was greater than 150X (greater than 20X coverage across 96% of targeted regions). The data obtained were in FASTQ file format and were used to identify variant sites associated with the patient’s clinical phenotype. Human genome hg19 version GRCh37 was used for data analysis. Further annotation and analysis of the detected variants were performed according to previously published methods [9, 10]. Quality control metrics for WES raw reads are presented in Supplementary Table 1. Paternity was verified using Somalier (version 0.2.18), following the methodology established in previous studies [11]. Sanger sequencing was performed to validate variants that were predicted to be deleterious by functional prediction tools. Detailed information on the variants detected in the proband across the five genes associated with HS is presented in Supplementary Table 4.
Splicing prediction
Three in silico prediction tools, SpliceAI (https://spliceailookup.broadinstitute.org/), Human Splicing Finder Pro version 4.3.3 (HSF, https://www.genomnis.com/access-hsf), and RDDC RNA Splicer (https://rddc.tsinghua-gd.org/) were used to evaluate the effects of variants on splicing.
Minigene approach
The minigene approach has gained broad acceptance as a tool for validating the impact of variants on gene splicing [12, 13]. The wild-type (WT) and mutant-type SPTB (c.301–2 A > G) minigene plasmid were constructed separately. The amplicons were cloned into pMini-Cop-GFP vector at the BamHI/XhoI restriction enzyme sites respectively and then transformed into TOP10 chemically competent Escherichia coli. The WT sequence of the exon containing the variant and approximately 150 bp flanking intronic sequences were amplified. The pMini-Cop-GFP-WT-SPTB plasmid was used as a template to construct the mutant plasmid via in vitro site-directed mutagenesis. The gene sequences were verified using Sanger sequencing. Detailed information on the plasmids is available in the Supplementary Material 1.
Human Embryonic Kidney (HEK) 293T cells were cultured in Dulbecco’s modified eagle medium containing 10% fetal bovine serum in a 5% CO2 atmosphere at 37 °C in a sterile incubator (Thermo Fisher Scientific, USA). The cell density was adjusted to 5 × 105 using the Automated Cell Counter IM1200 (Countstar, Shanghai, China), and the cells were seeded in 10 cm culture dishes. The WT and mutant plasmids were transfected separately into HEK 293T cells using Lipofectamine 2000 (Thermo Fisher Scientific Co., Ltd.). After 48 h, total RNA was extracted from the cells using TRIzol Reagent (Kangwei Century Biotechnology Co., Ltd., China), followed by reverse transcription into cDNA using the RT Master Mix for qPCR II (MedChemExpress, USA). Subsequently, reverse transcription PCR experiments were conducted to analyze the impact of the variant on mRNA splicing. PCR conditions are described in Supplementary Material 1. The effects were assessed using agarose gel electrophoresis and Sanger sequencing.
Summary of the literature search
To delineate the gene variant spectrum, we conducted a comprehensive literature search in the PubMed database using the keywords “SPTB gene” and “hereditary spherocytosis” spanning from the inception of the database to the present. All relevant publications on SPTB gene variants were meticulously collected. Detailed data, including genotype, ethnicity, and other pertinent information of recorded cases, were compiled into a well-organized tabular format. The mapping of variant sites within the SPTB gene was performed based on the literature analysis to better demonstrate the specific locations and frequencies of the identified variants.
Results
Case presentation
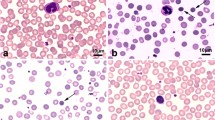
The proband (II-1, Fig. 1A) was a 7-year-old boy with suspected HS who was referred to our hospital. The boy presented with recurring pallor, occasional jaundice, and dark urine. There was no parental consanguinity and no history of congenital anomalies or recurrent miscarriages.Clinical laboratory examinations were performed. Routine blood tests showed an RBC count of 3.68 × 10^12/L (reference values 4.30–5.70 × 10^12/L), a hemoglobin concentration of 102 g/L (reference values 120–158 g/L), an erythrocyte distribution width of 19.6% (reference values < 15.0%), and a reticulocyte ratio of 8% (reference values 0.5%~1.5% ). Biochemical tests indicated an elevation in total and indirect bilirubin levels, which exceeded the normal range. Nevertheless, the remaining indicators were mainly within the expected parameters. Direct and indirect antiglobulin test results were negative. From osmotic fragility tests, the patient’s erythrocytes exhibited more inferior resistance toward osmotic pressure as compared to that reported in healthy control subjects. The patient’s RBCs started to induce hemolysis when the salt solution concentration was 0.56%. In addition, the RBCs were completely hemolyzed at a salt solution concentration of 0.24%. In the eosin-5′-maleimide binding test, the patient showed a 31.39% reduction in mean fluorescence intensity (biological reference interval < 16%). Examination of the peripheral blood smear showed that the RBCs were unequal in size, small RBCs were predominant, and spherical RBCs accounted for approximately 1.7%. Bone marrow cytology showed active cell proliferation, with erythroid predominance. Furthermore, an abdominal ultrasound revealed that the spleen was located approximately 3.4 cm below the left costal margin, approximately 11.3 cm in length and 3.4 cm in thickness.
Novel variant of the SPTB gene
Based on the clinical phenotypes of hemolytic disorders, the c.301–2 A > G variant detected by NGS was suspected to be a disease-associated variant in the SPTB gene. The gene was known to cause HS and was identified as a potential causative gene in the proband. A cosegregation analysis showed that the c.301–2 A > G variant carried by the proband was likely de novo and was not inherited from the parents (Fig. 1B). Based on the genomic relatedness data generated by Somalier, we can conclude that the proband exhibits a parent-child relationship with both parental samples. Detailed data are available in Supplementary Table 2. In addition, buccal sampling confirmed that the c.301–2 A > G variant was not a somatic variant. Phylogenetic analysis indicated that c.301–2 A > G site was highly conserved in multiple species (Fig. 1C).
Genetic variant in the HS family. The figure shows the genetic segregation of variants and the details of the SPTB variants. (A) Family pedigree. Circles represent female family members, and squares represent males. Filled symbols designate the proband. (B) Sanger sequencing showed that the c.301–2 A > G variant carried by the proband was likely de novo and was not inherited from the parents. (C) Multiple sequence alignment in the c.301-2 site variant of SPTB among different species, indicating that this variant was highly conserved. Conserved nucleotide is marked in red boxes
In silico analysis of the SPTB variant c.301–2 A > G
In this case, the c.301–2 A > G (NM_001024858.4) variant in the SPTB gene was classified as a “pathogenic” variation relating to very strong pathogenicity evidence (PVS1_moderate) + strong pathogenicity evidence (PS2) + moderate pathogenicity evidence (PM2) according to the American Society of Medical Genetics and Genomics guidelines (https://doi.org/10.1038/gim.2015.30) and recommendations put forth by the Clinical Genome Resource (ClinGen) Sequence Variant Interpretation (SVI) Working Group [14]. This variant was not reported in the 1000 Genomes Project, dbSNP, or ExAC databases. To confirm the splicing variant in the SPTB gene, we used three online bioinformatics tools—Splice AI, HSF, and RDDC RNA Splicer—for in silico analysis. The aim was to predict the potential impact of the c.301–2 A > G variant on mRNA splicing of the SPTB gene. According to Splice AI analysis, the c.301–2 A > G variant was predicted to cause acceptor loss with a score of 0.89 and a maximum prediction distance of 50 bp in our study. HSF analysis revealed that the WT acceptor site was disrupted following the variant, likely affecting splicing. The online RDDC RNA Splicer predicted two possible abnormal splice patterns: splice pattern 1, a 6 bp deletion and a new acceptor, and splice pattern 2, exon skipping resulting in the loss of 58 codons without premature termination. This may be due to exon 3, which contains 174 bp (Fig. 2).
Assessment of c.301–2 A > G in the SPTB gene by minigene splicing assay
To investigate the impact of the c.301–2 A > G variant on normal splicing, we reconstructed mutant and WT minigene plasmids using the pMini-Cop-GFP vector (Fig. 3A). Following agarose gel electrophoresis, we observed that the WT plasmid produced the expected 489-bp transcript. The mutant-type plasmid yielded three distinct PCR bands at 315 bp, 483 bp, and 546 bp (Fig. 3B). Figure 3C shows a schematic of our study’s abnormal alternative splicing event. Splicing sequences were confirmed by Sanger sequencing (Fig. 3D). Three novel transcript variants were detected, designated as NM_001024858: c.301_474del, NM_001024858: c.301_306delCCAAAG, and NM_001024858: c.301-1_301-57ins. These variants were predicted to form truncated proteins: p.Pro101_Gln158del, p.Lys102_Pro103del, and p.Lys102LeufsTer3. The protein sequences are shown in Supplementary Material 2.
In vitro minigene assay of the c.301–2 A > G variant. (A) Plasmid construction flow chart. The WT minigene (pMini-Cop GFP-WT) contains exons 2–4 and full-length intron 2 and intron 3 of the SPTB gene. (B) Agarose gel electrophoresis of the RT-PCR fragments from HEK 293 T cells. Original pictures of the amplified bands from the gel are available in Supplementary Material 3. (C) The schematic representation of the different transcripts. (D) Sanger sequencing of the RT- PCR products. WT, wild-type; MT, mutant-type
Literature review and variant features of the SPTB gene
Following an extensive literature search, 193 patients carrying mutant sites in the SPTB gene were included. Articles with a lack of clinical information or without genetic tests results were excluded. Figure 4 shows the gene variant map based on the literature reports. Of these, 77 variant sites were classified as de novo, and 116 variant sites were classified as hereditary. The pattern of variants in SPTB gene-associated mutants was complex and diverse. Within these variations, the top three most abundant variant types were nonsense (n = 87), frameshift (n = 56), and missense variants (n = 27). The variant positions were scattered throughout the gene; however, a relatively higher number of variations were observed in exons 13 (n = 27), 15 (n = 21), and 23 (n = 6). Of the 193 patients, 94 (43 male and 51 female) displayed their gender. Their ages ranged from 10 h to a maximum of 70 years. Detailed matching information are available in Supplementary Table 3.
Pie diagram and Lollipop chart illustrating the distribution of variants reported in the literature. (A) Distribution of de novo variants. (B) Distribution of inherited variant. (C) Lollipop chart of all variants. Variant diagram circles are colored with respect to the corresponding variant types. De novo: build up from nothing; CNV: copy number variation
Discussion
In this study, we identified a new pathogenic variant, c.301–2 A > G, in the SPTB gene of a Han Chinese family with HS. As this variant is absent from the literature and existing databases, it can be inferred that it is a completely novel variant. Using a minigene assay, we demonstrated abnormal splicing of the SPTB gene due to the variant. In addition, we constructed variant profiles of the SPTB gene variants that have been previously reported in the literature.
Variants in genes encoding RBC membrane proteins constitute one element of the pathogenesis of HS. The genes primarily associated with HS include SPTA1, SPTB, ANK1, SLC4A1, and EPB42 [15], and the variants of these genes vary between countries [16]. Among European and American populations, the ANK1 gene variant is the most prevalent, accounting for approximately 50% of all HS cases. In China, patients with HS commonly have variants in the SPTB and ANK1 genes [17]. In addition, the proportion of HS cases attributable to SPTB gene variants varies across populations. SPTB gene variants account for 15–30% of HS cases in Northern European populations, whereas heterozygous variants in the SPTB gene account for 25% of HS cases in Northern American populations [18, 19]. In China, the proportion of HS patients caused by SPTB gene variants is 37.8% [20]. In the last decade, the development and application of NGS in the genetic diagnosis of congenital hereditary diseases have resulted in the detection of thousands of variants with uncertain clinical significance [21]. Due to the potential for inaccurate variant interpretation that could mislead researchers and result in incorrect diagnoses, it is important to precisely classify these variants based on predictive and functional evidence [22].
Herein, we reported a novel SPTB gene variant, further expanding the spectrum of SPTB variants in patients with HS. Previous studies have demonstrated that the SPTB gene is located on chromosome 14q23.3 and spans 38 exons [18]. The gene is involved in encoding a protein called the spectrin beta chain, which consists of 2,137 amino acids, and is important for maintaining the structure and stability of the RBCs [17]. According to current literature, many of the documented SPTB gene variants are nonsense variants or frameshift variants. Nonsense variants introduce premature stop codons, while frameshift variants alter the reading frame and often lead to premature stop codons. Both types of variants can result in truncated proteins or trigger nonsense-mediated decay, potentially leading to an inability to produce a functional protein [23]. In addition, aberrant splicing events can introduce premature termination codons (PTCs) in the reading frame, leading to premature truncation of protein synthesis [24]. These findings were consistent with those reported in our study. Minigene experiments demonstrated that the mutant plasmid co-transcribes three aberrant mRNA isoforms, resulting in truncated protein synthesis. Nonsense-mediated RNA degradation (NMD) is a widely conserved mRNA surveillance mechanism in eukaryotic cells, which targets transcripts with PTCs [25]. In this study, the variant detected three aberrant transcripts on agarose gel electrophoresis, indicating that the variant may have escaped NMD surveillance. While further experiments at the protein level are necessary to fully elucidate the function of the splice-site variant, our current findings suggest that it likely results in the loss of the normal transcript from one allele in affected patients, with the other allele appearing to remain normal. However, additional research is needed to confirm these preliminary observations. This heterozygous state is consistent with the autosomal dominant inheritance pattern observed in hereditary spherocytosis caused by SPTB variants.
At present, HS diagnosis is based on clinical manifestations, family history, and peripheral blood smear results. However, a study that investigated 94 HS pedigrees revealed that de novo variants accounted for approximately 23.4% of the cases, indicating that family history may not always be the primary diagnostic criterion for this condition [15], which is consistent with the results of our literature review. The systematic review of the literature revealed that a total of 193 HS cases were caused by variants in the SPTB gene. Children with no family history of HS, who exhibit no apparent clinical symptoms, and who experience hemolysis only during episodes of infection or stress are at a significantly increased risk of being either clinically misdiagnosed or missed entirely [26]. Although the proband in our study had no family history of HS, an accurate diagnosis was possible by integrating clinical data and genetic testing results, which proved the high reliability of targeted sequencing using NGS. Moreover, this method is both rapid and accurate, thus making it highly effective in comprehensively analyzing genetic variations that underlie this condition [27]. Based on these aforementioned reasons, genetic testing plays a crucial role in HS diagnosis.
Conclusion
Genetic sequencing can help establish a definitive diagnosis for HS. In this study, we successfully established a genetic diagnosis for a case of HS using NGS. Our in silico and in vitro studies provided strong evidence supporting the pathogenicity of the novel variant (c.301–2 A > G). The findings of our study offer specific insights into the effects of a novel splice-site variant in the SPTB gene, furthering our understanding of the genetic underpinnings of hereditary spherocytosis (HS) and expanding the known spectrum of variants associated with the SPTB gene. We underscored the significance of systematic molecular testing and in-depth pedigree investigation in complex cases. Nonetheless, further studies exploring in-depth the pathogenesis and mechanism of SPTB-related HS are warranted.
Data availability
The data analyzed in the current study are available in the GenBank database. The gene ID of SPTB used in the current study is 6710. The cDNA sequence number is NM_00102485, and the gDNA sequence number is NG_016202.2.
Abbreviations
- HS:
-
Hereditary spherocytosis
- NGS:
-
Next-generation sequencing
- VUS:
-
Variants of uncertain significance
- gDNA:
-
Genomic DNA
- PCR:
-
Polymerase chain reaction
- WT:
-
Wild-type
- HEK:
-
Human Embryonic Kidney
- NMD:
-
Nonsense-mediated RNA degradation
- RBC:
-
Red blood cell
- HSF:
-
Human Splicing Finder
- PTC:
-
Premature termination codon
References
Gallagher PG. Difficulty in diagnosis of Hereditary Spherocytosis in the Neonate. Pediatrics, 2021. 148(3).
Wang C, et al. A systematic review of hereditary spherocytosis reported in Chinese biomedical journals from 1978 to 2013 and estimation of the prevalence of the disease using a disease model. Intractable Rare Dis Res. 2015;4(2):76–81.
Agarwal AM. Ankyrin mutations in Hereditary Spherocytosis. Acta Haematol. 2019;141(2):63–4.
van Asten I, et al. Hereditary spherocytosis without pronounced spherocytes on the peripheral blood smear. Int J Lab Hematol. 2023;45(1):6–8.
Russo R, et al. Multi-gene panel testing improves diagnosis and management of patients with hereditary anemias. Am J Hematol. 2018;93(5):672–82.
King MJ, et al. ICSH guidelines for the laboratory diagnosis of nonimmune hereditary red cell membrane disorders. Int J Lab Hematol. 2015;37(3):304–25.
Carraro M, et al. Performance of in silico tools for the evaluation of p16INK4a (CDKN2A) variants in CAGI. Hum Mutat. 2017;38(9):1042–50.
Wang Y, et al. De novo variations of ANK1 gene caused hereditary spherocytosis in two Chinese children by affecting pre-mRNA splicing. BMC Pediatr. 2023;23(1):23.
Zhang K, et al. A synonymous mutation in PI4KA impacts the transcription and translation process of gene expression. Front Immunol. 2022;13:987666.
Che F, et al. Identification of two novel variants of the BCL11B gene in two Chinese pedigrees associated with neurodevelopmental disorders. Front Mol Neurosci. 2022;15:927357.
Pedersen BS, et al. Somalier: rapid relatedness estimation for cancer and germline studies using efficient genome sketches. Genome Med. 2020;12(1):62.
Du M, et al. Identification of a novel CACNA1F mutation in a Chinese family with CORDX3. Mol Genet Genomic Med. 2022;10(11):e2060.
Xu W, et al. A novel homozygous TUB mutation associated with autosomal recessive retinitis pigmentosa in a consanguineous Chinese family. BMC Med Genomics. 2023;16(1):9.
Walker LC, et al. Using the ACMG/AMP framework to capture evidence related to predicted and observed impact on splicing: recommendations from the ClinGen SVI Splicing Subgroup. Am J Hum Genet. 2023;110(7):1046–67.
Wang WJ, et al. Identification of variants in 94 Chinese patients with hereditary spherocytosis by next-generation sequencing. Clin Genet. 2023;103(1):67–78.
Han N, et al. Hereditary spherocytosis complicated by intrahepatic cholestasis: two case reports. Ann Transl Med. 2022;10(22):1255.
Wang R, et al. Exome sequencing confirms molecular diagnoses in 38 Chinese families with hereditary spherocytosis. Sci China Life Sci. 2018;61(8):947–53.
Jang W, et al. Hereditary spherocytosis caused by copy number variation in SPTB gene identified through targeted next-generation sequencing. Int J Hematol. 2019;110(2):250–4.
Bassères DS, et al. beta-spectrin S(Ta) Bárbara: a novel frameshift mutation in hereditary spherocytosis associated with detectable levels of mRNA and a germ cell line mosaicism. Br J Haematol. 2001;115(2):347–53.
Christensen RD, Yaish HM, Gallagher PG. A pediatrician’s practical guide to diagnosing and treating hereditary spherocytosis in neonates. Pediatrics. 2015;135(6):1107–14.
Zhang K, et al. Molecular genetic testing and diagnosis strategies for dystrophinopathies in the era of next generation sequencing. Clin Chim Acta. 2019;491:66–73.
Zhang X, et al. Functional analysis of variants in DMD exon/intron 10 predicted to affect splicing. J Hum Genet. 2022;67(8):495–501.
Li S, et al. A novel SPTB mutation causes hereditary spherocytosis via loss-of-function of β-spectrin. Ann Hematol. 2022;101(4):731–8.
Wang D, et al. Mutational characteristics of causative genes in Chinese Hereditary Spherocytosis patients: a report on fourteen cases and a review of the literature. Front Pharmacol. 2021;12:644352.
Schweingruber C, et al. Nonsense-mediated mRNA decay - mechanisms of substrate mRNA recognition and degradation in mammalian cells. Biochim Biophys Acta. 2013;1829(6–7):612–23.
Shih YH, et al. A large family of hereditary spherocytosis and a rare case of hereditary elliptocytosis with a novel SPTA1 mutation underdiagnosed in Taiwan: a case report and literature review. Med (Baltim). 2023;102(4):e32708.
Wang X, et al. Genetic and clinical characteristics of patients with Hereditary Spherocytosis in Hubei Province of China. Front Genet. 2020;11:953.
Acknowledgements
We express our gratitude for the contribution made by the patients, their families, pediatricians, and investigators. We thank Mengxue Gao for his guidance and assistance in bringing forth the figures. We thank Bullet Edits Limited for the linguistic editing and proofreading of the manuscript.
Funding
This work was supported by Public Welfare Project for Rare Blood Disorders in the field of Hematology in China (xyxthjb-2023-006).
Author information
Authors and Affiliations
Contributions
WY wrote the initial draft. WY, LT, and WW conceived and designed the study. XL, ZYJ, and XY collected and analyzed the data of the family. JCX, HL, and LT contributed to the interpretation of the results. YJ supervised the research project. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was reviewed and approved by the Medical Ethics Committee of the Children’s Hospital of Chongqing Medical University with the approval file number 2021.457. All methods were performed in accordance with the Declaration of Helsinki.
Consent for publication
Written informed consent was obtained from the patient’s legal guardians (parents) prior to the investigation for the publication of any potentially identifiable images or data included in this article.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, Y., Liu, T., Jia, C. et al. A novel variant in the SPTB gene underlying hereditary spherocytosis and a literature review of previous variants. BMC Med Genomics 17, 206 (2024). https://doi.org/10.1186/s12920-024-01973-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12920-024-01973-w