Abstract
The aim of the study was to evaluate psychophysiological predictors of the quality of monotonous activity performance against the background of partial sleep deprivation. Fourteen subjects aged 18–22 years with partial sleep deprivation participated in the experiments. Each subject participated in four experimental sessions with a computer driving simulator: 1—without sleep deprivation, 2—with sleep deprivation, 3—with sleep deprivation and periodic exposure to a massage vibration seat cover, 4—with sleep deprivation and periodic spraying of peppermint oil from an aroma diffuser. Periodically, the subject was required to respond to two types of stimuli. Driving simulator data, 19-channel electroencephalogram (EEG), electrocardiogram (ECG) and videotape of the subject's face were recorded. Subjects took questionnaires for drowsiness and general well-being, and their reaction time was also tested before the experiment. A statistically significant increase in eye closure percentage and heart rate variability spectral features were detected before the driving errors. High-stress levels and chronic sleep deprivation were detected in the subjects. Against this background, peppermint oil and massage vibration seat cover had no statistically significant effect on the number of errors. The values of physiological indices before errors indicate different causes of errors in experiments. Neither peppermint oil or massage vibration sit cover were effective in preventing errors in case of high stress and chronic sleep deprivation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The problem of accidents on the roads is obviously rising with the growth of automobile traffic. Thus, according to the World Health Organization [1], about 1.3 million people die in road accidents every year, and 20–50 million are injured, and the human factor is responsible for about 90% of accidents. Falling asleep accounts for 20–25% of crashes with severe consequences, and another 20% of crashes may be due to distraction by cell phones [2, 3]. In megacities, where automobile traffic is mostly concentrated, residents suffer from light and noise pollution, high-stress levels and sleep deprivation [4]. Sleep deprivation (less than 6 h of nighttime sleep before driving) increases the risk of falling asleep at the wheel by 2.6 times, and less than four hours of sleep increases the risk of falling asleep at the wheel by 15 times [5].
Recently, with the development of artificial intelligence, more and more high-tech car models are entering the market. A number of studies [6, 7] have shown that attention in semi-automated vehicles decreases faster, while drowsiness occurs within 20–30 min.
A survey of the literature [8] shows that various approaches can be used to improve the quality of monotonous activities and attention levels, including the use of vibration-massage seat covers [9], or the spraying of essential oils, particularly peppermint [10].
The aim of our study was to evaluate psychophysiological predictors of the quality of monotonous activity performance.
The objectives of the study were to verify whether periodic exposure to a massage vibration seat cover or peppermint oil could reduce errors number during driving, as well as to investigate the possibility of predicting the subject's performance by previous testing for sensorimotor reaction time, sleep time the night before the experiment and self-estimated well-being.
2 Methods
2.1 Subjects
Fourteen subjects aged 18–22 years without neurologic diseases participated in the experiments. The subjects were medical students with a high study load and chronic sleep deprivation. Sleep deprivation was monitored using Condor Instruments actigraphs [11]. Each subject took part in four experimental sessions, the interval between sessions ranged from 3 days to 3 weeks.
2.2 Experiments
Before the experiments 2–4 subjects were asked to have additional sleep deprivation (4 h of sleep the night before the experiment). Each subject participated in the experimental series in the following particular order:
-
1.
No sleep deprivation—driving for 15 min.
-
2.
Sleep deprivation: driving for 90 мин.
-
3.
Sleep deprivation and massage seat cover: driving for 90 min, massage seat coat activation each 10 min
-
4.
Sleep deprivation and peppermint oil: driving for 90 min, peppermint oil spraying each 10 min.
The experiments were conducted during the daytime, from 13 to 16 h, in a darkened soundproofed room equipped with air conditioning, at a temperature of 23 °C. Before each driving session in the computer driving simulator, subjects completed the Wellbeing-Activity-Mood (WAN) questionnaire and Epworth sleep scale. Subjects' reaction times to simple visual stimuli and to visual stimuli with incorrect audial cues were tested on the UPDK-MK hardware-software complex [12]. During the experiment, EEG according to the standard scheme 10–20, as well as ECG were recorded with a sampling frequency of 1000 Hz using the hardware-software complex NeoRecNVX36 [13]. The subject during the experiment was sitting in a chair with a headrest at a comfortable distance from the monitor, handling tasks in the computer driving simulator by means of the game steering wheel and pedals.
A video camera with a sampling frequency of 60 Hz was attached to the monitor in the subject's room to track the subject's head position and facial expression. Data from the driving simulator were recorded at a 6 Hz frequency.
Car simulator was developed by authors. The image in the simulation was a stylized first-person view of a four-lane road divided by dashed markings. In the absence of stimuli, the "car" did not require steering and moved in the center of the second right lane at a speed of 60 km/h. The following events (9 events of each type in one experimental session) could occur during the movement:
-
1.
Gradual reddening of the lane on which the subject was traveling for ten seconds. The required response was to move off into any neighboring lane; after ten seconds, return to his/her lane and continue driving.
-
2.
Appearance at a fixed distance in front of the car (30 m) of a fixed obstacle in the form of a stylized figure of a pedestrian. The required reaction is to press the brake pedal as quickly as possible and stop in front of the pedestrian.
The time between events varied randomly from 3 to 7 min, with an average of 5 min. The sequence of events at the beginning of each experimental session was set randomly.
2.3 Data processing
Video images of the subject's face were processed frame by frame in the Python Anaconda computing environment using the OpenCV library [14] for Python and the team's own software. The face in each frame was brought to a frontal perspective and standardized height, after which the average distance between the lower and upper eyelids of both eyes was calculated.
Electroencephalogram. EEG artifacts throughout the experiment were manually marked by the examiner to exclude from further processing processing was performed in the Python Anaconda computing environment using the mne library [15] and software of the team's own development. Most related to the attention and sleep functions spectral frequency domains: theta (4–7 Hz), alpha (8–13 Hz) and beta (14–30 Hz) and their ratios were tested [16] by means of the mne method mne.time_frequency.tfr_array_morlet, using single-trial Morlet wavelet spectral power and the 1-s long window.
Electrocardiogram. ECG markup was performed semi-automatically, followed by visual inspection by an expert. The spectral index of heart rate variability was calculated in Python Anaconda using the method described in [17].
3 Results
3.1 Subjects’ sleep before the experiment
Before the experiment without sleep deprivation, the average sleep time of the subjects amounted to 394.5 ± 94.88 min (from 4 to 8 h), which is significantly less than the normal sleep duration of an adult human and indicates chronic deprivation. In experiments with sleep deprivation, these values were: 246.9 ± 16.7 min (no stimulation), 247.8 ± 20.35 min (massage seat cover), 242.5 ± 14.6 min (peppermint oil).
3.2 Subjective rates of wellbeing, activity, mood and sleepiness
Subjects filled wellbeing-activity-mood (WAM) questionnaire [18] before and after each experiment. All three scales were strongly correlated: wellbeing-mood correlation was equal to r = 0.76 (p < 0.001) before the experiment and r = 0.77 (p < 0.001) after it. Activity-wellbeing correlation was strongly negative: r = − 0.74, p < 0.001 before the experiment and r = − 0.89, p < 0.001 after the experiment.
Subjective assessment of sleepiness did not correlate significantly with actual sleep time the night before. However, correlations of this parameter with WAM questionnaire scales were found: with activity (r = 0.28, p < 0.05) before the experiment and all assessments after the experiment (well-being r = − 0.38, p < 0.01, activity r = 0.33, p < 0.05, mood r = − 0.40, p < 0.01).
Subjective assessment of sleepiness according to Epworth's sleepiness scale [19] in the control experiment without sleep deprivation score was 4.3 ± 1.42, in the experiment with deprivation and without exposure—5.23 ± 2.09; in the experiment with vibration cape—5.29 ± 1.94; in the experiment with peppermint oil—4.93 ± 1.59.
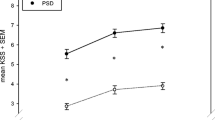
To test the experimental session effects on participants, we subtracted scale meanings before the experiment from the ones after it (thus, negative rates show decrease of each parameter). From the Table 1 and Fig. 1 we can see that changes were not big, but Activity dynamics was different for the experiments with massage stimulation and peppermint oil compared to the no-stimulation experiment.
For each type of exposure, changes in the scales "wellbeing", "activity", and "mood" are presented: the values after the experiment were subtracted from the values before the experiment. Experiment type: 0—no stimulation, control experiment without sleep deprivation; 1—no stimulation, experiment with sleep deprivation; 2—vibration seat cover, experiment with sleep deprivation; 3 – experiment with the peppermint oil and sleep deprivation. No statistically significant differences were found
3.3 Reaction times before the experiment and errors in the car simulator driving session
Before the beginning of each experiment, subjects were tested on a simple and complex sensorimotor response on the UPDK-MK device.
Neither reaction time nor the number of errors on average changed from experiment to experiment, and sleep deprivation also had no effect on the performance of these tests (Table 2) compared to experiments without sleep deprivation. Reaction time showed an inverse correlation with the Activity scale of the WAM questionnaire (r = − 0.33, p < 0.05—with activity before the experiment, r = − 0.39, p < 0.01—with activity after the experiment) and a direct correlation with the mood index after the experiment (r = 0.44, p < 0.01). No significant relationship with sleep time was found for this parameter.
The number of errors made in the simulator did not change significantly from experiment to experiment (1.91 ± 1.93 in the experiment without exposure, 2.50 ± 2.03 in the experiments with massage seat cover and with peppermint oil).
Reaction times to the two types of obstacles in the car simulator driving session showed opposite trends. The response to a smoothly occurring obstacle (road reddening) was fastest for the no-stimulation experiment, slowed in the massage seat cover experiment, and was maximal in the peppermint oil experiment. In the case of stopping in front of a suddenly appearing pedestrian, the stopping distance was longer in the experiments with both types of stimulation, and in the experiment without stimulation it was minimal (Table 3). These reaction parameters did not correlate significantly with each other.
Only the average reaction time to a smoothly appearing obstacle correlated with the number of errors made during the experiment (r = 0.78, p < 0.001), and the significant correlation was maintained when analyzing experiments with different types of influence separately (without stimulation—r = 0.65, p < 0.05; massage seat cover—r = 0.79, p < 0.01; peppermint oil—r = 0.90, p < 0.001).
We could assume that it was the test subject's inability to respond adequately even to an obstacle that did not appear quickly reflected the increased level of sleepiness or distraction from the task that accompanied the errors.
3.4 Heart rate variability (HRV) spectral index
HRV spectral index [20] reflects slow changes in the balance of sympathetic and parasympathetic nervous system activity. This parameter requires data collection for at least one minute to assess but provides an estimate of the overall tone of the nervous system. In all experiments, including the control one without sleep deprivation there was a slight increase in this parameter during the of the experiment (comparison of HRV at the beginning of the experiment and over the entire driving time, analysis of variance with repeated measures, F(1,37) = 16.71, p < 0.001).
For all experiments, an extremely pronounced and significant increase of this parameter was observed during the minute before the error was made (comparison of the index during the work and before the error, analysis of variance with repeated measurements, F(1,36) = 54.67, p < 0.001), indicating a significant activation of the sympathetic nervous system (see Table 4 for index values). Differences in HRV spectral index between the period before the error and the whole work time were greatest in experiment 1 (8.17 ± 6.54) and almost equal in the massage seat cover experiment (6.30 ± 6.89) and peppermint oil (6.37 ± 4.09) experiment, although difference from the no-stimulation experiment was not statistically significant.
3.5 Eye closure index (PERCLOS)
For all experiments, including the control one, no significant change in the eye closure index (PERCLOS) [21] was found, when comparing the index in the first two minutes of work and for the whole duration of the experiment, and in all experiments with sleep deprivation there was a significant increase in this parameter before making an error, while the type of exposure had no significant effect on the level of eye closure (repeated-measures analysis of variance, F(1,36 = 71.36, p < 0.001), on average during the experiment this index was 0.12 and before making an error—0.65 (Table 5). A number of subjects had their eyes closed before committing the error (PERCLOS = 1), and a high level of eye closure index was more frequent in experiments with exposure than without, although the mean values across experiments did not show significant differences. This parameter is important to distinguish between errors made due to inattention and due to falling asleep, as it may remain unchanged when distraction is involved. In the case of the conducted experiments, a significant part of the errors was due to drowsiness and falling asleep.
3.6 EEG spectral indices
Before the beginning of each experiment, a standard two-minute test was performed to compare the power of the alpha rhythm with eyes open and closed. Of the 20 subjects, 5 had a flattened alpha rhythm or virtually no changes in alpha rhytm even with their eyes closed. This EEG feature is considered a variant of normal, but it is usually noted that it is quite rare. This variant should be taken into account in EEG analysis, because in such people the alpha rhythm associated with relaxation and sleepiness may also be weakly expressed and the indices based on it may be uninformative, while it is been used as a drowsiness indicator or even drowsiness golden standard in some studies (Fig. 2).
Power spectral analysis of EEG rhythms at electrode P3 in the alpha test before the experiment. Horizontal axis—EEG rhythm frequency, Hz. Vertical axis—power of EEG rhythm, µV. Dashed line—open eyes, solid line—closed eyes. Right image—subject with a pronounced alpha activity. Left image—subject with the “flat” alpha activity
To compare EEG parameters, we used theta, alpha, and beta ranges, which are the most informative for the situation of operator work and falling asleep [16]. Expressed activity in the theta range should signal falling asleep, and activity increase in the alpha range—a relaxed or drowsy state. The following band spectral power ratios were selected: alpha to theta, alpha to beta, and theta to beta. The alpha/beta index is used to contrast drowsiness (alpha) and active wakefulness (beta) brain activities. Since these ratios showed no significant differences in subjects with a flattened alpha sample, their data were also included in the analysis.
These coefficients were compared during the first two minutes in the simulator, for the entire running time, and 15 s before the error was made.
Alpha/beta index increased during the experiment compared to the beginning regardless of exposure or the presence of sleep deprivation, and before the error, the index was highest in the no-stimulation experiment and was not significantly different from the baseline indices in both experiments with stimulation (repeated-measures analysis of variance, contrast start of work/all work F(1,52) = 24.4, p < 0.0001; stimulation type factor for the index before the error F(2,39) = 4.7, p = 0.01) (Fig. 3).
Increased alpha rhythm accompanies increased sleepiness, relaxation and distraction from the task, and the increase in alpha/theta and alpha/beta indices from the beginning of work to the average for the whole time of work reflects these processes. For the alpha/theta index, the difference 1st 10 min and the whole time of the experience was also very pronounced, and it was maximal in the control experiment without sleep deprivation, although an increase in the index during work was observed in all experiments (repeated-measures analysis of variance, contrast beginning of work/all work F(1,52) = 35.1, p < 0.0001, interaction of experience factors and contrast beginning of work/all work F(3,52) = 3.0, p = 0.04). The alpha/theta index was not differed significantly from the indices at other times (see Fig. 4).
The theta/beta index changed least during the driving simulator, the drop in the index was significant overall, but less pronounced in the sleep deprivation experiments than in the control experiment where the index was highest (repeated measures analysis of variance, contrast start of work/all work F(1,52) = 4.8, p = 0.03). The index increased before errors in the experiment without and with the stimulation using the massage seat cover and decreased in the experiments with peppermint oil stimulation, but all these changes were not significant (Fig. 5).
When analyzing correlations between different EEG indices, the most pronounced relationships were within the alpha/beta and theta/beta indices, where all of them were positively and significantly correlated. The alpha/beta and theta/beta indices were almost linearly related at the beginning of the experiment and throughout the experiment. Apparently, the beta rhythm was more stable within one experiment and characterized the general state of the subject on a particular day (Table 6).
4 Discussion
According to the combination of different behavioral assessments, psychophysiological parameters of psychological testing and physiological parameters during the driving sessions, it is possible assess the state of the study participants. High parameters of subjective activity were obtained in combination with poor well-being and lowered mood, which could mark constant stress and stress way of activation. The correlation of self-rated well-being, activity, and mood parameters, as well as sleep data before the experience without sleep deprivation (mean 6.5 h) suggest chronic sleep deprivation in addition to acute sleep deprivation in the main series of experiments.
The amount of sleep did not correspond to the subjectively perceived sleepiness but was reflected in activity and in all subjective assessments of self-state after the experimental sessions. Differences between of real amount sleep time at night, the level of subjective sleepiness and well-being also marks chronic sleep deprivation and stress. Such a state leads to increased fatigue, inability to correctly assess one's own performance and increased risks in driving [22]. For these reasons, many measures, such as the number of errors in pre-session testing, are not significantly differ in the control experiment and in the sleep deprivation experiments.
Additional sleep deprivation did not affect the performance in psychomotor tests on the UPDC complex, but the level of errors was high enough already in the control experiment without sleep deprivation. Thus, the complex could not serve to distinguish between conditions of acute and chronic sleep deprivation, because they were both risky for real driving. Also, the reaction data obtained did not correlate with the performance in the car simulator.
Within the experiment, the average reaction time to a slowly appearing obstacle (road reddening) correlated with the total number of errors in the driving simulator.
Activity in the low frequency (LF) spectral range of HRV is associated with the sympathetic nervous system (SNS), but it is also influenced by the parasympathetic nervous system (PNS). High frequency (HF) activity is only influenced by the parasympathetic nervous system. To account for this, the HF/HF ratio, or HRV spectral index is used. The transition from wakefulness to sleep is accompanied by a decrease in SNS activity and an increase in PNS activity [21]. A sharp decrease in this index is interpreted as a sign of approaching sleep. In the study [23], the decrease in HRV spectral index occurred within 10 min preceding falling asleep, but the picture was somewhat different for subjects suffering from obstructive sleep apnea. Sometimes a drop in HRV spectral index occurs even after the establishment of the first stage of sleep as determined by the electroencephalogram. However, if a person actively struggles to fall asleep, he/she has increased activity of the sympathetic nervous system, which was observed in the case of our study.
The HRV spectral index showed additional activation of the SNS during the course of the work compared to the beginning of the experience, reflecting the predominance of sympathetic nervous system (SNS) activity over the parasympathetic and the stressful effect of the experience on the subjects. Significant additional increases in this index were observed before committing an error, particularly in the no-exposure experiment, which also had the lowest eye closure index among the sleep deprivation experiments. These trends may indicate differences in the causes of errors made in experiments with and without stimulation. We hypothesize that both massage seat cover and peppermint oil could reduce stress within subjects within the experiment, but due to their chronic sleep deprivation relaxing effect of stimulation causes them to fall asleep just after the stress reduction.
According to the difference in the theta/beta index in the presence and absence of acute sleep deprivation and its decrease during work and its changes during the short-term period (15 s before the error), we assume that it did not reflect possible falling asleep (accompanied by amplification of the theta rhythm in the first stage of sleep). Theta rhythms in the anterior and medial regions in wakefulness are associated with processes of attention maintenance, orientation, task concentration, and cognitive control [24, 25]. In our experimental design, this index most likely reflected exactly the decrease in the level of vigilance and control against the background of sleep deprivation and monotonous task performance and either unsuccessful activation of attention before making a mistake or changes in theta activity before falling asleep, which gave the opposite change in the index compared to the background decrease.
For the experiments without stimulation, more pronounced sympathetic activation, a pronounced alpha rhythm of the EEG, and a relatively low PERCLOS level before making errors indicated that many of them were made due to inattention, as a result of distraction from the task. For the experiments with massage seat cover or peppermint oil, the eye closure index was higher before the error, though changes in EEG alpha/beta and HRV index were not significant. To summarize, it may suggest a transition to drowsiness where the alpha rhythm begins to fade, the theta rhythm generalizes and signals the beginning of the transition to sleep, and sympathetic activation becomes insufficient to keep the subject awake. There may be two reasons for this: either the exposures to the vibration and peppermint oil were perceived as relaxing and subjects moved more easily from distraction to sleep, or subjects reduced self-control over wakefulness levels, relying on external cues for activation. However, exposure was not tailored to the timing of falling asleep, and reduced control could also led to more frequent falling asleep.
Despite the differences in psychophysiological parameters, in all conditions the total number of errors, regardless of their causes, remained approximately the same. Taking into account the stability of test results before the experiments, we suggest that the initial state in all three experiments for all subjects was close, and apparently it provoked similarity in numbers of periods of reduced level of wakefulness during the driving sessions. But without stimulation, the reduced level of alertness often led to distractions from the task, and exposure indirectly provoked an additional attention decrease and sleepiness.
We could conclude that errors and driving risks have several causes and therefore one could not use some universal psychophysiological index to control attention level, drowsiness and activation simultaneously. Instead, a combination of different indices looks much more promising.
5 Conclusions
-
1.
According to the results of questionnaires and test performance, the subjects were in a state of chronic sleep deprivation and chronic stress for all experiments.
-
2.
In the sample of subjects involved, no statistically significant differences could be found between the experiments after partial sleep deprivation without additional stimulation, with the use of a massage vibration seat cover on the chair every 10 min and with periodical spraying of peppermint oil every 10 min.
-
3.
PERCLOS and HRV spectral index showed a significant statistically significant increase before errors, but there was a large variation of values, which, in our opinion, may be due to some errors were caused by distraction from the task by one's own thoughts rather than by falling asleep.
-
4.
The values of physiological indices before errors indicate different causes of errors in the experiments without stimulation and in the ones with stimulation with massage seat cover or peppermint oil every 10 min.
Data availability
The datasets analyzed during the current study are available from the corresponding author upon reasonable request.
References
WHO, Road traffic injuries (2021). https://www.who.int/news-room/fact-sheets/detail/road-traffic-injuries. Accessed 22 Aug 2023
A. Morgan, F.L. Mannering, The effects of road-surface conditions, age, and gender on driver-injury severities. Accid. Anal. Prev. 43(5), 1852–1863 (2011). https://doi.org/10.1016/j.aap.2011.04.024
J. Weng, Q. Meng, Effects of environment, vehicle and driver characteristics on risky driving behavior at work zones. Saf. Sci. 50(4), 1034–1042 (2012). https://doi.org/10.1016/j.ssci.2011.12.005
Research: mean sleep time in Russia was found to be 6.83 hours, RBC. Trends (2021). http://trends.rbc.ru/trends/social/6128ba189a79477d3d16f1f7. Accessed 22 Aug 2023.
B.C. Tefft, Acute sleep deprivation and culpable motor vehicle crash involvement. Sleep 1(41), 10 (2018). https://doi.org/10.1093/sleep/zsy144
O.N. Tkachenko, V.B. Dorokhov, V.V. Dementienko, E.O. Gandina, G.N. Arseniev, A.O. Taranov, D.R. Bakirova, D.S. Sveshnikov, Comparison of the effectiveness of performance in a driving simulator in manual and semi-automatic modes: behavioral and physiological analysis. Social’no-ecologicheskie technologii. 1, 62–80 (2022). https://doi.org/10.31862/2500-2961-2022-12-1-62-80
T. Vogelpohl, M. Kühn, T. Hummel, M. Vollrath, Asleep at the automated wheel—sleepiness and fatigue during highly automated driving. Accid. Anal. Prev.. Anal. Prev. 126, 70–84 (2018). https://doi.org/10.1016/j.aap.2018.03.013
O.N. Tkachenko, V.B. Dorokhov, V.V. Dementienko, Psychophysiological aspects of maintaining optimal driver attention levels during partially automated driving. Social’no-ecologicheskie technologii. 10(4), 482–509 (2020). https://doi.org/10.31862/2500-2961-2020-10-4-482-509
A. Telpaz, B. Rhindress, I. Zelman, O. Tsimhoni, Haptic seat for automated driving, in Proceedings of the 7th International Conference on Automotive User Interfaces and Interactive Vehicular Applications (2015). https://doi.org/10.1145/2799250.2799267
M. Mahachandra, E.D. Garnaby, The effectiveness of in-vehicle peppermint fragrance to maintain car driver’s alertness. Proc. Manuf. 4, 471–477 (2015). https://doi.org/10.1016/j.promfg.2015.11.064
Condor instruments actigraphs. https://condorinst.com/en/. Accessed 22 Aug 2023
UPDK-MK complex of testing test operators functional state. https://neurocom.ru/products/professional-systems/updk-mk/. Accessed 22 Aug 2023
EEG caps MSCCap. https://mks.ru/. Accessed 22 Aug 2023
Open-CV computer vision package for Python. https://pypi.org/project/opencv-python/. Accessed 22 Aug 2023
URL: MNE tool for Python. https://mne.tools/stable/overview/cite.html. Accessed 22 Aug 2023
I. Stancin, M. Cifrek, A. Jovic, A review of EEG signal features and their application in driver drowsiness detection systems. Sensors 21, 3786 (2021). https://doi.org/10.3390/s21113786
K. Fujiwara, E. Abe, K. Kamata, C. Nakayama, Y. Suzuki, T. Yamakawa, T. Hiraoka, M. Kano, Y. Sumi, F. Masuda, M. Matsuo, H. Kadotan, Heart rate variability-based driver drowsiness detection and its validation with EEG. IEEE Trans. Biomed. Eng. 66(6), 1769–1778 (2019). https://doi.org/10.1109/tbme.2018.2879346
V.A. Doskin, N.A. Lavrent’eva, M.P. Miroshnikov, V.B. Sharaj, Test of differential functional state diagnostics. Voprosy Psihol 6, 141–145 (1973)
Epworth Sleepiness Scale. https://epworthsleepinessscale.com/about-the-ess/. Accessed 22 Aug 2023
PERCLOS, A valid psychophysiological measure of alertness as assessed by psychomotor vigilance corporate creator(s): United States. Federal Motor Carrier Safety Administration. Technology Division (1998). https://doi.org/10.21949/1502740
J. Vicente, P. Laguna, A. Bartra, R. Bailon, Drowsiness detection using heart rate variability. Med. Biol. Eng. Comput.Comput. 54(6), 927–937 (2016). https://doi.org/10.1007/s11517-015-1448-7
N.B. Powell, J.K. Chau, Sleepy driving. Med. Clin. N. Am. 94(3), 531–540 (2010). https://doi.org/10.1016/j.mcna.2010.02.002
Z. Shiner, S. Akselrod, Y. Dagan, A. Baharav, Autonomic changes during wake-sleep transition: a heart rate variability based approach. Auton. Neurosci. 130(1–2), 17–27 (2006)
L.I. Aftanas, S.A. Golocheikine, Human anterior and frontal midline theta and lower alpha reflect emotionally positive state and internalized attention: high-resolution EEG investigation of meditation. Neurosci. Lett. 310(1), 57–60 (2001). https://doi.org/10.1016/s0304-3940(01)02094-8
J.F. Cavanagh, M.J. Frank, Frontal theta as a mechanism for cognitive control. Trends Cogn. Sci. 18(8), 414–421 (2014). https://doi.org/10.1016/j.tics.2014.04.012
Acknowledgements
Authors express their appreciation to the employees of the Medical Institute of RUDN University for their help with the experimental series arrangement.
Funding
VBD, VVD, AOT, GNA, and ONT were funded by the Russian Science Foundation (Grant # 19-29-06071). The article was prepared in full within the state assignment of the Ministry of Education and Science of the Russian Federation for 2021–2023 # AAAA-A17-117092040004-0.
Author information
Authors and Affiliations
Contributions
Conceptualization ONT, VBD, and VVD; funding acquisition ONT, AOT, VBD, and VVD; data curation ONT, VVD, EOG, AOT, GNA, and ANP, resources DSS, BZV and VBD; project administration ONT, VVD, DSS, and VBD; supervision VVD and VBD; software GNA, ONT, AOT, and VVD; investigation DSS, VBD, ANP, and ONT; methodology VVD, VBD, and ONT; artefact scoring: AOT, EOG, and ONT; data preprocessing and analysis: ANP and ONT; validation ANP and ONT; visualization ANP and ONT; writing—review and editing VBD, DSS, ONT, VVD, EOG, GNA, AOT, ANP, BZV and DSS.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests. The funders had no role in the design of the study, the collection, analyses, or interpretation of data, the writing of the manuscript, and the decision to publish the results.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tkachenko, O.N., Dorokhov, V.B., Dementienko, V.V. et al. Assessment and prevention of inattention and sleepiness during monotonous operator activity with underlying sleep deprivation. Eur. Phys. J. Spec. Top. 233, 647–658 (2024). https://doi.org/10.1140/epjs/s11734-024-01088-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1140/epjs/s11734-024-01088-4