Abstract
In this paper, we compare four methods of extracting the sequence of intervals between heartbeats from the photoplethysmogram signal to estimate the total percentage of phase synchronization of autonomic regulation circuits of blood circulation that are designed to operate in real time. In the analysis of the experimental ensemble of records of healthy subjects, the optimal parameters for the used approaches were selected. We compared cardiointervalograms obtained from photoplethysmogram signals with cardiointervalograms isolated from simultaneously recorded electrocardiogram signals during the analysis of phase synchronization between the phases of the extracted signals in the low-frequency range (0.04–0.15 Hz), which reflects the element activity of autonomic control of blood circulation. The operability of the approaches used in the analysis of the total percentage of phase synchronization of the autonomic regulation circuits of the cardiovascular system based on the photoplethysmogram signal for groups of healthy people and patients during COVID-19 was demonstrated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
The human body is a complex non-linear system of high dimension. The regulation of the operation of its elements is ensured by the coordinated operation of many circuits of nervous and humoral regulation. Flexible adjustment of the operation of the cardiovascular system to the current needs of the body is provided by both humoral factors and dual innervation from the sympathetic and parasympathetic branches of the autonomic nervous system with the participation of various oscillatory processes that reflect the activity of autonomic regulation subsystems that actively interact with each other [1].
To control the state of the body, it is possible and important to quantify the characteristics of the individual and collective dynamics of the subsystems of nervous regulation by analyzing the low-frequency spectral components in the signals of the cardiovascular system [2–4].
Synchronization of 0.1-Hz oscillations in the heart rhythm and peripheral circulation is an important physiological feature of the human body, allowing it to adapt and self-regulate [5]. The degree of this synchronization indicates the functional state of the cardiovascular system (CVS): in patients, the contours of autonomic regulation of the heart rate and arterial tone demonstrate rarer epochs of synchronization compared to healthy people, which may indicate a partial functional uncoupling of the mechanisms of autonomic regulation of blood circulation [6].
Previously, a new indicator for estimating the synchronization degree of 0.1-Hz oscillations, which is focused on the analysis of non-stationary signals of a biological nature, namely, the total percentage of phase synchronization S, was proposed [7]. Using the developed index, new fundamental information about the internal structure and features of the interaction of autonomic regulation of human CVS [3, 8] was obtained, and its practical importance for solving the problems of diagnosing and personalized therapy of circulatory pathologies was shown [4, 9, 10].
For the mass introduction of the analysis of the total percentage of phase synchronization, it is necessary to develop hardware–software systems and methods that allow analyzing CVS signals in real time. In our previous studies, several results were obtained in this direction [11–13]. An important step in the creation of compact, mass-produced, and ergonomic diagnostic devices is the transition from the synchronization analysis based on a pair of simultaneously recorded signals: an electrocardiogram (ECG) and a photoplethysmogram (PPG) to an estimate of S based on univariant PPG. Earlier, we showed the fundamental possibility of this [14]. However, systematic studies comparing various methods for extracting information about the dynamics of the heart rate from PPG and choosing the values of free parameters of such approaches were not carried out.
In this paper, the approach we proposed earlier is compared with three new methods. In the comparison of cardiointervalograms isolated from ECG and PPG recorded in healthy subjects and patients suffering from COVID-19, the parameters of the methods were refined, and the choice was made in favor of the most sensitive one.
1 DATA AND METHODS
Experimentally obtained simultaneous ECG recordings (standard lead I) and PPG (distal phalanx of the ring finger of the left hand) of healthy volunteers without detected CVS pathologies (13 men of 21.2 ± 3.1 years old, 12 women of 20.9 ± 2.2 years old) and patients with COVID-19 who are on inpatient treatment, do not need oxygen support, and without identified pulmonary complications (12 men of 49.4 ± 11.6 years old, 9 women of 51.0 ± 12.5 years old) were considered. All records were registered by an EEGA-21/26 Medic Encephalan-131-03 certified electroencephalograph analyzer. The sampling rate was 250 Hz per channel, the bandwidth of the analog path was 0.016–70 Hz. The recording duration was 120 min. For analysis, 5-min sections of the recordings that did not contain artifacts and arrhythmia sections were selected.
The methods considered here are ultimately focused on the analysis of contour phase synchronization of the autonomic regulation of heart rate and blood pressure using the proposed earlier method based on the calculation of the total percentage of phase synchronization S. This method was proposed in [7] and involves the use of simultaneously recorded PPG and ECG signals. From the ECG signal, a sequence of time intervals between successive heart contractions (RR intervals, cardiointervalogram) is isolated. For this, the spline interpolation procedure (recommended in the methodological study [2]), which results in an equidistant time series of RR intervals with a sampling frequency of 5 Hz, is used. This signal and the PPG signal are filtered in the so-called LF-range (0.04–0.15 Hz) using a band-pass filter for extracting components associated with the operation of the circuits of sympathetic regulation of the heart rate (HR) and blood pressure, respectively [2]. The filtered PPG sample rate is downsampled to 5 Hz using decimation. Using the Hilbert transform, time series of instantaneous phases are extracted from the received signals, and their difference is calculated. In accordance with [15], the section of the instantaneous phase difference signal is identified as the section of phase synchronization if the phase difference remains close to a constant. The change in value is tracked using a linear approximation in a sliding window using the least squares method. If the slope of the approximating line (meaning the detuning of the instantaneous oscillation frequencies) remains less than the specified threshold value, then the segment is identified as synchronous. As a result, quantitative index S, the total percentage of phase synchronization, is calculated as the sum of the durations of all identified synchronization sections related to the total length of the implementation and expressed as a percentage.
Previously [16], the fundamental possibility of estimating S from a univariant PPG signal was shown while information about the sequence of intervals between heartbeats was also extracted from this signal. Based on small statistics, it was shown that the sequence of local PPG minima in the cardiocycle interval could be used as an analogue of RR intervals. In this case, the results of the synchronization analysis using a pair of ECG and PPG signals and using only the latter showed differences in S estimates up to 10.5%. This is explained by the fact that the ECG R-peak (corresponding to the moment of contraction of the heart ventricles) traditionally used to identify the CVS moment in healthy volunteers is a short high-amplitude pulse that is weakly subject to noise and distortion of the measuring path. On the contrary, the PPG signal due to its physiological nature and technical features registration has a smooth shape and is much more prone to noise and distortion. Besides, the known results indicate the presence of a number of physiological factors that introduce errors in extracting information about heart contractions from PPG [17]. In this paper, four methods for extracting a sequence of intervals between heartbeats from PPG (hereinafter, referred to as PP intervals) are compared with the choice of free parameter values of the methods and comparison of the obtained signals of PP intervals with RR intervals extracted from simultaneously recorded ECG signals.
A natural way to deal with interference and noise in the measuring channel when identifying PP intervals is narrow-band PPG filtering (Fig. 1a) near the main heart rate (~1 Hz in healthy volunteers). Here, we compare cases of identifying PP-intervals as intervals between local maxima (method 1) or minima (method 2) of this signal. As can be seen in Fig. 1a, narrow-band filtration significantly distorts the phases and amplitudes of the spectral components of the PPG signal, which can obviously affect the accuracy of the operation of such methods for selecting PP intervals. Therefore, two other methods were taken for comparison. For their implementation, narrow-band filtering near the main heart rate was a preliminary step necessary to determine the position of the current cardiocycle. Within the cardiocycle identified in this way, local maxima (method 3) or minima (method 4) of the PPG signal (see Fig. 1a) filtered in a relatively wide band (wider than when using methods 1 and 2, but narrower than the bandwidth of the analog path to eliminate low-frequency trends and high-frequency interference).
Stages of PP-interval selection by methods 1–4: (a) detection of the distance between PPG extrema (dashed line—an original PPG signal (band of 0.016–70 Hz), thin line—PPG filtered by a narrow-band filter (band of 0.8–1.8 Hz), thick line—a line signal filtered by a broadband filter (band 0.6–6.0 Hz); local extrema for PPG filtered in a narrow band (methods 1 and 2 are indicated by dark and light triangles, respectively) and a wide band (methods 3 and 4 are indicated by dark and light circles, respectively); (b) differences of instantaneous phases of PP- and RR-intervals in the LF-range determined by methods 1–4; (c) RR- and PP-intervals identified by method 1 for subject no. 1; and (d) RR- and PP-intervals for subject no. 1 filtered in the LF range.
To limit the band of PPG signals in the implementation of the four listed methods, filters with a rectangular amplitude–frequency characteristic were used.
To select the parameters of the compared methods for the optimal values of the cutoff frequencies, which ensure the best correspondence between the signals of the RR- and PP-intervals in the LF range, these parameters were enumerated with the maximization of the value of the phase coherence coefficient (PCC) [18] between the instantaneous phases of the 5-min segments of the corresponding RR- and PP intervals (see Fig. 1c) in this range (see Fig. 1d). This index reaches 1.0 with full phase coherence of the signals (the distribution of the folded phase difference is a δ-peak) and 0.0 in the absence of phase coherence (uniform distribution of the phase difference).
2 RESULTS
At the first stage, the parameters for the proposed methods for the selection of PP-intervals were selected (Fig. 2). The performed analysis made it possible to choose the optimal filtering bands for the four compared methods, which provided the highest probability of observing the ensemble of high phase coherence of RR- and PP-intervals in the LF range. Method 1: 0.8–1.8 Hz; method 2: 0.8–1.8 Hz; method 3: 0.8–1.8 Hz for narrow-band and 0.8–4 Hz for wide-band filters; method 4: 0.6–1.8 Hz and 0.6–6.0 Hz, respectively.
Probability Р to meet in the sample a PCC value higher than 0.95 for bandwidth settings according to methods 1–4. Cutoff frequencies were enumerated: (a) lower and (b) upper limit of the narrow-band filter, (c) lower and (d) upper limit of the wide-band filter. Sections of a multidimensional surface are presented in the parameter space for the parameter vector that provides the maximal PCC values in this section.
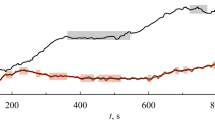
Figure 3 shows the PCC values calculated from experimental implementations of healthy volunteers at the selected filter bandwidths. PCC is 0.83 ± 0.20 (mean ± standard deviation) for method 1; 0.84 ± 0.20 for method 2; 0.84 ± 0.21 for method 3; and 0.79 ± 0.26 for method 4.
The operability of the methods used to identify PP-intervals was compared in the course of calculating the total percentage of phase synchronization S of various categories of subjects using a pair of ECG and PPG signals or SRR, or using a univariant PPG signal or SPP. The absolute values of the difference of these values are shown in Fig. 4a. The difference values averaged over the ensemble are: 7.34 ± 9.69 for method 1, 7.05 ± 7.43 for method 2, 7.69 ± 7.84 for method 3, and 5.83 ± 6.34 for method 4. The distribution functions of these quantities are shown in Figs. 4b. As can be seen, the best fit to the reference method is provided by method 4 while the worst is provided by method 3.
Comparison of the results of estimating the total percentage of phase synchronization of healthy volunteers for the reference method based on the analysis of a pair of ECG and PPG signals SRR and used methods 1–4 SPP: (a) absolute values of difference in S estimates for all healthy volunteers, (b) the distribution function of the difference module of estimates.
The parameters of the compared methods for identifying PP-intervals were selected during the analysis of the records of healthy volunteers. The possibilities of the approach in the analysis of patients were estimated when analyzing an ensemble of records of patients with COVID-19 since it was previously shown in [19] that in this category of patients, the S value is significantly reduced relative to the group of healthy volunteers.
The results of the analysis of patients are presented in Fig. 5a. The ensemble mean differences are 6.28 ± 7.50, 5.32 ± 7.61, 5.34 ± 5.79, and 5.75 ± 4.29 for methods 1–4, respectively. The distribution functions of these quantities are shown in Figs. 5b. It can be seen that the best fit to the reference method is provided by method 2 while the worst fit is provided by method 1.
Comparison of the results of estimating the total percentage of phase synchronization in patients with COVID-19 for the reference method based on the analysis of a pair of ECG and PPG signals SRR and used methods 1–4 SPP: (a) absolute values of the difference in S estimates for all healthy volunteers, and (b) the function distribution of the difference module of estimates.
3 DISCUSSION
The performed analysis shows a qualitative agreement between the results of the analysis of groups of volunteers (healthy and patients suffering from COVID-19) while the filter parameters of the compared methods were selected during the analysis of only a sample of healthy subjects. This allows us to count on the efficiency of the approaches used in the analysis of various groups of subjects.
Comparison of the results of the analysis indicates a better correspondence to the reference approach of the univariant PPG synchronization analysis method using the PP-interval selection method 4. This method demonstrates satisfactory compliance with the reference method. The advantages of this method over the other three can be explained by the fact that the narrow-band filtering used in techniques 1 and 2 significantly distorts the phase response of the signal, although it provides a better signal-to-noise ratio. The use of method 4 for estimating S by a univariant PPG signal can potentially be implemented based on mass portable small-sized ergonomic hardware–software diagnostic systems for screening the psychophysical state of the subjects. The synchronization analysis based on a univariant PPG signal may have advantages over the method based on the analysis of a pair of ECG and PPG signals in the analysis of data from patients suffering from arrhythmias and cardiological pathologies that distort the ECG shape.
In this study, signal segments that obviously did not contain artifacts and arrhythmias were analyzed. However, when implementing monitoring diagnostic systems in the future, the issue of identifying, correcting, and/or excluding from the analysis sections of records containing artifacts is an important issue that requires separate consideration and solution. The presence of arrhythmias in patients is also a criterion for excluding such patients from the analysis of the total percentage of phase synchronization.
CONCLUSIONS
In the paper, we show the possibility of analyzing the phase synchronization of autonomic circulatory control circuits based on univariant PPG signals from healthy volunteers and patients suffering from COVID-19.
The previously proposed and proven reference approach, which uses ECG and PPG signals for synchronization analysis, and four methods based on the selection of PP intervals from a univariant PPG signal were compared. Parameters (passbands of the pass filters) for the compared methods were chosen to provide the best fit to the reference approach. When identifying PP intervals, the performed study allows recommending making a choice in favor of method 4, which involves preliminary PPG filtering in the 0.6–1.8 Hz band to clarify the position of the cardiocycle and, then, finding the local PPG minimum within the identified cardiocycle using the PPG signal filtered in the 0.6–6.0 Hz band.
REFERENCES
R. Shmidt and G. Tevs, Human Physiology (Springer-Verlag, Berlin, 1983; Mir, Moscow, 2005), Vol. 2.
R. M. Baevskii, G. G. Ivanov, L.V. Chireikin, et al. Vestn. Aritmolog. 24, 65 (2001).
A. R. Kiselev, S. A. Mironov, A. S. Karavaev, et al., Physiol. Meas. 37, 580 (2016).
A. R. Kiselev, V. I. Gridnev, M. D. Prokhorov, et al., Ann. Noninvas. Electrocard. 17 (3), 204 (2012).
C. Schäfer, M.G. Rosenblum, J. Kurths, and H.‑H. Abel, Nature 392 (6673), 239 (1998).
V. I. Ponomarenko, M. D. Prokhorov, A. S. Karavaev, et al., Eur. Phys. J. Spec. Top. 222 (10), 2687 (2013).
A. S. Karavaev, M. D. Prokhorov, V. I. Ponomarenko, et al., Chaos 19, 033112 (2009).
A. S. Karavaev, Yu. M. Ishbulatov, V. I. Ponomarenko, et al., Fiziolog. Chelov. 43, 70 (2017).
A. R. Kiselev, V. I. Gridnev, A. S. Karavaev, et al., Arterial. Gipertenz. 17, 354 (2011).
A. R. Kiselev, A. S. Karavaev, V. I. Gridnev, et al. Saratov. Nauch.-Med. Zh. 6, 061 (2010).
D. D. Kul’minskii, A. V. Kurbako, V. V. Skazkina, et al., Izv. Saratov. Univ., Nov. Ser., Ser. Fizika. 21, 58 (2021).
A. V. Kurbako, E. I. Borovkova, A. R. Kiselev, et al., Izv. Saratov. Univ. Nov. Ser., Ser. Fizika. 21, 213 (2021).
A. V. Kurbako, D. D. Kul’minskii, E. I. Borovkova, et al., Izv. Vyssh. Uchebn. Zaved., Prikl. Nelin. Din. 29, 892 (2021).
D. D. Kul’minskii, O. V. Astakhov, A. R. Kiselev, and A. S. Karavaev, in Proc. VIII All-Russian Conf. Young Scientists “Nanophotonics, Nanoelectronics and Nonlinear Physics”, Saratov, 2013 (Saratov. Gos. Univ., Saratov, 2013), p. 139.
M. G. Rosenblum, A. S. Pikovsky, J. Kurths, et al., Neuro-Informatics and Neural Modelling. Handbook of Biological Phys., Vol. 4. Eds. by F. Moss, S. Gielen (Elsevier, Amsterdam, 2001), p. 269.
E. I. Borovkova, A. S. Karavaev, A. R. Kiselev, et al., Ann. Aritmolog. 11 (2), 84 (2014).
Y. Imai, A, I. Aihara, T. Ohkubo, et al., Am. J. Hypertension 10 (11), 1281 (1997).
F. Mormann, K. Lehnertz, P. David, and C. E. Elger, Physica D: Nonlin. Phenomena 144 (3-4), 358 (2000).
V. V. Skazkina, N. S. Krasikova, E. I. Borovkova, et al., Russian Open Med. J. 10 (3), e0307 (2021).
Funding
This work was supported by the Russian Foundation for Basic Research, projects nos. 20-02-00702 and 20-38-90067, as well as by the state task of the Institute of Radioengineering and Electronics, Saratov Branch, Russian Academy of Sciences.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.
COMPLIANCE WITH ETHICAL STANDARDS
The design of the experiment was approved by the ethics committee at the Saratov State Medical University.
Additional information
Translated by A. Ivanov
Rights and permissions
About this article
Cite this article
Kurbako, A.V., Skazkina, V.V., Borovkova, E.I. et al. Method for Cardiointervalogram Selection from a Photoplethysmogram Signal for Estimating the Total Percentage of Phase Synchronization of Contours of Autonomic Circulation Regulation. J. Commun. Technol. Electron. 67, 1243–1249 (2022). https://doi.org/10.1134/S1064226922100084
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S1064226922100084