Abstract
Objectives
To analyse and compare the efficacy of different interventions for myopia prevention and control in children.
Methods
We searched CNKI, VIP, Wan-Fang, CBM, Chinese Clinical Registry, PubMed, The Cochrane Library, Web of Science, Embase and ClinicalTrials.gov from inception to July 2022. We selected randomized controlled trials (RCTs) that included interventions to slow myopia progression in children. The main outcomes included mean annual change in axial length (AL) (millimetres/year) and in refraction (R) (dioptres/year).
Results
A total of 80 RCTs (27103 eyes) were included. In comparison with control, orthokeratology (AL, −0.36 [−0.53, −0.20], P < 0.05; R, 0.56 [0.34, 0.77], P < 0.05), 1%Atropine (AL, −0.39 [−0.65, −0.13], P < 0.05; R, 0.54 [0.31, 0.77], P < 0.05), 0.01%Atropine + orthokeratology (AL, −0.47 [−0.80, −0.14], P < 0.05; R, 0.81 [0.43, 1.20], P < 0.05) could significantly slow the progression of myopia; in addition, progressive multi-focal spectacle lenses (PMSL) (0.42, [0.06, 0.79], P < 0.05), bifocal soft contact lenses (0.40, [0.03, 0.77], P < 0.05), 0.5%Atropine (0.67 [0.25, 1.10], P < 0.05), 0.1%Atropine (0.42 [0.15, 0.71], P < 0.05), 0.05%Atropine (0.57 [0.28, 0.86], P < 0.05), 0.01%Atropine (0.33 [0.15, 0.52], P < 0.05), 1%Atropine + bifocal spectacle lenses (BSL) (1.30 [0.54, 2.00], P < 0.05), 1%Atropine + PMSL (0.66 [0.23, 1.10], P < 0.05), 0.01%Atropine + single vision spectacle lenses (SVSL) (0.70 [0.23, 1.10], P < 0.05), 0.01%Atropine + orthokeratology (0.81 [0.43, 1.20], P < 0.05), BSL + Massage (0.85 [0.22, 1.50], P < 0.05), SVSL + Red light (0.59 [0.06, 0.79], P < 0.05) showed significant slowing effect on the increase in R.
Conclusions
This network meta-analysis suggests that the combined measures were most effective in AL and R, followed by Atropine.
Similar content being viewed by others
Introduction
Myopia is a disease affecting nearly a quarter of the world’s population, and the prevalence of myopia is expected to double by 2050 [1]. In addition to decreased visual function due to optical defocus, myopia is associated with an increased risk of irreversible blindness, such as myopic macular degeneration [2], retinal detachment [3], and glaucoma [4]. Moreover, myopia has a substantial financial burden. For example, the spending on spectacles and contact lenses in the United States is up to $2 billion annually [5].
In many East and Southeast Asian countries [6], there is a tendency for early-onset myopia in childhood under educational pressure, with over half of school-age chiledren affected. The myopia rate is about 80% by the end of school [6,7,8,9]. Early-onset myopia often leads to faster progression and a longer duration of myopia [10]. Thus early-onset myopia increases the risk of high myopia and sight-threatening complications in later life. Therefore, it is important to delay myopia progression in childhood.
It can be seen that the widespread prevalence and incidence of myopia are increasing, resulting in the increase of occurrence of related diseases affecting vision and the decline of accompanying quality of life, as well as the increase of huge cost incurred to correct myopia, which has made myopia a major public health problem [1].
At present, there is no effective way to prevent the occurrence of myopia. The main methods to control myopia include spectacles [11,12,13,14,15], contact lenses [16,17,18], outdoor activities [19], pharmaceutical [20] and low-level red light [21] mainly. These studies were based on clinical observations, myopic animal models, or both [22,23,24,25]. Trials of such interventions provided a substantial evidence base. However, most studies are of a single intervention versus control, lacking direct head-to-head comparisons. There are many inconsistencies among trials studying a certain intervention. Conventional meta-analyses enable comparisons between two interventions only, do not enable comparisons between multiple treatments, and most meta-analyses give statistical advice only on the efficacy of a single intervention. In clinic, two or more combined measures are often combined to treat myopia, especially myopia progressing rapidly. Previously, the additive effect of combined intervention in preventing and controlling myopia has been proposed; however, its conclusion still needs to be supported by a large amount of evidence. Therefore, this network meta-analysis directly or indirectly compared the efficacy of 37 interventions, including combined interventions, and ranked them to provide more comprehensive and reliable evidence-based medical recommendations for preventing and controlling myopia in children.
Methods
Literature search
A systematically electronic literature search was conducted using the databases of PubMed, Cochrane Library, Web of Science and EMBASE and ClinicalTrials.gov in English and the CNKI (http://www-cnki-net-s.vpn.uestc.edu.cn:8118/), Wan-Fang (http://www-wanfangdata-com-cn-s.vpn.uestc.edu.cn:8118/index.html), VIP (http://qikan.cqvip.com/), Chinese Biomedical Literature Service System (http://www.sinomed.ac.cn/index.jsp) and Chinese Clinical Registry in Chinese (up to July 2022). The search strategy is presented in the Supplement (eMethod 1 in the Supplement).
To identify relevant studies, we also examined reference lists from clinical trials, meta-analyses, and systematic review reports.
Inclusion criteria
(1) Subjects aged 6 to 18 years old. (2) The language of the literature is limited to Chinese and English. (3) Interventions to delay the progression of myopia in children. (4) Outcomes: mean annual change in axial length and spherical equivalent. (5) The follow-up time is at least 1 year, and the longest follow-up years are taken for those greater than 1 year. (6) randomized controlled trials (RCTs).
Literature screening and data extraction
(1) The retrieved literatures were imported into Endnote software, and the repeated literatures were deleted after checking, and then the unqualified literatures were deleted by two investigators according to the above proposed inclusion criteria by reading the titles and abstracts. (2) For the remaining literatures, the full texts were read in detail by two investigators, and the literatures that full texts could not be obtained, the follow-up time was less than 1 year, the subjects’ age was <6 or >18 years old, the study content or intervention measures did not meet, the data was incomplete, questionable or repeated were deleted. (3) two investigators extracted relevant data, mainly including: author, publication year, follow-up time, country, interventions, sample size, gender ratio, age, baseline and endpoint, change value and number of lost to follow-up. The data were integrated and cross-checked after extraction. Any disagreement was resolved by a joint reevaluation of the article by a third reviewer (CQ). The judgement result of the third reviewer is the final result.
Literature quality evaluation method
The quality of the included RCTs was assessed using the Cochrane Collaboration’s risk-of-bias method and the modified Jadad scale, respectively, including a description of the method of randomization, allocation concealment, blinding, completeness of data, selective reporting of results, and other sources of bias. The Cochrane Collaboration’s risk-of-bias tool rated each item area as having a ‘low’, ‘high’, or ‘unclear’ bias risk; a modified Jadad scale total score of 4–7 was assigned to high-quality studies and 1–3 to low-quality studies. The literature screening and methodological quality evaluation were independently completed and checked by two investigators. Disagreements during the screening process were resolved through negotiation, and if there were differences, they were decided by the tutor (a third party).
Statistical methods
Data analyses were performed using Review Manager (version 5.3; Cochrane Collaboration), STATA (version 17.0; StataCorp), and R software (version 4.2.1; SAS Institute, Inc). Inconsistency tests were used to analyse global inconsistency between direct and indirect evidence, with P > 0.05 considered no inconsistency, and a consistency model was fitted, whereas an inconsistency model was fitted. Local inconsistency tests for direct and indirect comparisons were performed using the node splitting method, and P > 0.05 was considered no local inconsistency. The heterogeneity test was analysed using the prediction intervals, and the heterogeneity was insignificant if the results of the fixed effect model and the random effect models were consistent. Measurement data were presented as weighted mean difference (WMD) and its 95% confidence interval (CI). In statistics, P < 0.05 indicates a significant difference and vice versa. Intervention efficacy was ranked according to the surface under the cumulative ranking area (SUCRA), with a larger area under the curve indicating better intervention efficacy.
Publication bias was assessed using funnel plots when more than 10 included articles, and publication bias was assessed by visual inspection of the symmetry of the distribution of each point on funnel plots.
Results
Literature results
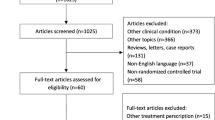
Database searches yielded 4122 potentially relevant entries. After removing duplicated publications by Endnote X9, 3063 articles remained. Among the remaining articles that qualified for the title and abstract review, 2530 were excluded because of their apparent irrelevance. After reading the full text, 80 pieces of literature were finally included, with a total of 27,103 eyes (Fig. 1).
Basic characteristics and methodological quality assessment of included studies
The basic information of the included literature is shown in the Supplement (eTable 1 in the Supplement), and all were RCTs.
The Jadad score of each study is more than or equal to 3 points, with 11 studies having 7 points, 15 studies having 6 points, 20 studies having 5 points, 12 studies having 4 points, and 22 studies having 3 points. All the studies with 3 points were unable to achieve double-blind due to the different physical properties of the interventions. Altogether, the overall quality of the included articles is acceptable.
Cochrane Risk Bias Assessment is shown in the Supplement (eFig. 1 in the Supplement).
Network meta-analysis results
Evidence network
Based on direct comparison data, relationships were formed between all interventions. Each vertex of the relationship diagram represents different interventions, the vertex size represents the sample size included in each intervention, the line between the vertices indicates the direct comparison between the two interventions, and the width of the line is proportional to the number of studies of each pair of interventions. There is direct or indirect evidence between different interventions, and the basic conditions for performing network meta-analysis are met (Fig. 2).
Notes: A is for axial length and B is for refraction. 1 = control; 2 = Bifocal spectacle lenses (BSL); 3 = Blue-violet light filtering spectacle lenses (BVLFSL); 4 = Defocus incorporated multiple segments spectacle lenses (DIMSSL); 5 = Progressive addition spectacle lenses (PASL); 6 = Prismatic bifocal spectacle lenses (PBSL); 7 = Peripheral defocus modifying spectacle lenses (PDMSL); 8 = Progressive multi-focal spectacle lenses (PMSL); 9 = Spectacle lenses with highly aspherical lenslets (SLHAL); 10 = Spectacle lenses with slightly aspherical lenslets (SLSAL); 11 = Undercorrected single vision spectacle lenses (USVSL); 12 = Bifocal soft contact lenses (BSCL); 13 = Defocus incorporated soft contact lenses (DISCL); 14 = Extended depth of focus soft contact lenses (EDOFSCL); 15 = Orthokeratology (OK); 16 = Progressive addition soft contact lenses (PASCL); 17 = Progressive multi-focal soft contact lenses (PMSCL); 18 = Rigid gas permeable contact lens (RGP); 19 = Positive spherical aberration soft contact lenses (+SASCL); 20 = 1%Atropine (Atr); 21 = 0.5%Atr; 22 = 0.1%Atr; 23 = 0.05%Atr; 24 = 0.025%Atr; 25 = 0.02%Atr; 26 = 0.01%Atr; 27 = Compound tropicamide eye drops (CTED); 28 = Pirenzepine (Pir); 29 = More outdoor activities (MOA); 30 = 1%Atr + BSL; 31 = 1%Atr + PMSL; 32 = 1%Atr + Racanisodamine; 33 = 0.01%Atr + SVSL; 34 = 0.01%Atr + OK; 35 = BSL + M; 36 = SVSL + OK; 37 = SVSL + Red light (RL).
Consistency test
Inconsistency model test results for axial length and refraction showed P > 0.05, indicating that the global inconsistency was insignificant. Thus, a consistency model can be used to fit.
The node splitting method was used to test for local inconsistency for the two outcomes of axial length and refraction separately (eTable 2 in the Supplement). The results of axial length showed no inconsistency between any two interventions (P > 0.05). The refraction results showed local inconsistency between “control vs 0.5%Atropine” (P < 0.05), “control vs 1%Atropine + Racanisodamine” (P < 0.05), “control vs 0.01%Atropine + single vision spectacle lenses” (P < 0.05) and “1%Atropine vs 1%Atropine + Racanisodamine” (P < 0.05) and no local inconsistency between any two remaining interventions (P > 0.05).
Heterogeneity test
Any two interventions of axial length and refraction were analysed by fixed effect model and random effect model, respectively, and the results showed that the two models had consistent results, suggesting that the heterogeneity of the included studies was insignificant (eTable 3 in the Supplement).
Axial length
Seventy-one studies reported axial length changes, totalling 35 interventions. Network meta-analysis results showed that except for progressive addition spectacle lenses, axial length growth after treatment by other interventions was less than control. Among them, three interventions such as orthokeratology (−0.36 [−0.53, −0.20], P < 0.05), 1%Atropine (−0.39 [−0.65, −0.13], P < 0.05) and 0.01%Atropine + orthokeratology (−0.47 [−0.80, −0.14], P < 0.05) were statistically significant from control (Fig. 3A). Network meta-analysis results of axial length changes are presented in the Supplement (eTable 4 in the Supplement).
Notes: A is for axial length and B is for refraction. 1 = control; 2 = Bifocal spectacle lenses (BSL); 3 = Blue-violet light filtering spectacle lenses (BVLFSL); 4 = Defocus incorporated multiple segments spectacle lenses (DIMSSL); 5 = Progressive addition spectacle lenses (PASL); 6 = Prismatic bifocal spectacle lenses (PBSL); 7 = Peripheral defocus modifying spectacle lenses (PDMSL); 8 = Progressive multi-focal spectacle lenses (PMSL); 9 = Spectacle lenses with highly aspherical lenslets (SLHAL); 10 = Spectacle lenses with slightly aspherical lenslets (SLSAL); 11 = Undercorrected single vision spectacle lenses (USVSL); 12 = Bifocal soft contact lenses (BSCL); 13 = Defocus incorporated soft contact lenses (DISCL); 14 = Extended depth of focus soft contact lenses (EDOFSCL); 15 = Orthokeratology (OK); 16 = Progressive addition soft contact lenses (PASCL); 17 = Progressive multi-focal soft contact lenses (PMSCL); 18 = Rigid gas permeable contact lens (RGP); 19 = Positive spherical aberration soft contact lenses (+SASCL); 20 = 1%Atropine (Atr); 21 = 0.5%Atr; 22 = 0.1%Atr; 23 = 0.05%Atr; 24 = 0.025%Atr; 25 = 0.02%Atr; 26 = 0.01%Atr; 27 = Compound tropicamide eye drops (CTED); 28 = Pirenzepine (Pir); 29 = More outdoor activities (MOA); 30 = 1%Atr + BSL; 31 = 1%Atr+PMSL; 32 = 1%Atr + Racanisodamine; 33 = 0.01%Atr + SVSL; 34 = 0.01%Atr + OK; 35 = BSL + M; 36 = SVSL + OK; 37 = SVSL + Red light (RL).
For slowing axial progression, the cumulative probability ranking results for each intervention showed that the top ten were: 1%Atropine + bifocal spectacle lenses (84.8%) >0.01%Atropine + orthokeratology (80.9%) > 1%Atropine (76.0%) >0.01%Atropine + single vision spectacle lenses (73.9%) > orthokeratology (73.0%) >1%Atropine + progressive multi-focal spectacle lenses (68.2%) >0.5%Atropine (67.8%) >0.1%Atropine (65.8%) >0.05%Atropine (64.7%) >1%Atropine + Racanisodamine (64.0%), suggesting 1%Atropine + bifocal spectacle lenses may be the most effective measure to delay axial growth (Fig. 4A).
Notes: A is for axial length and B is for refraction. Atr, Atropine; BSCL, bifocal soft contact lenses; BSL, bifocal spectacle lenses; BVLFSL, blue-violet light filtering spectacle lenses; CTED, compound tropicamide eye drops; DIMSSL, defocus incorporated multiple segments spectacle lenses; DISCL, defocus incorporated soft contact lenses; EDOFSCL, extended depth of focus soft contact lenses; M, Massage; MOA, more outdoor activities; OK, orthokeratology; PASCL, progressive addition soft contact lenses; PASL, progressive addition spectacle lenses; PBSL, prismatic bifocal spectacle lenses; PDMSL, peripheral defocus modifying spectacle lenses; Pir, pirenzepine; PMSCL, progressive multi-focal soft contact lenses; PMSL, progressive multi-focal spectacle lenses; Rac, Racanisodamine; RGP, rigid gas permeable contact lenses; RL, red light; SLHAL, spectacle lenses with highly aspherical lenslets; SLSAL, spectacle lenses with slightly aspherical lenslets; SVSL, single vision spectacle lenses; USVSL, undercorrected single vision spectacle lenses; +SASCL, positive spherical aberration soft contact lenses.
Spherical equivalent
Sixty-seven studies reported refractive changes, totalling 36 interventions. The results of network meta-analysis showed that except for bifocal spectacle lenses, blue-violet light filtering spectacle lenses, undercorrected single vision spectacle lenses, compound tropicamide eye drops, and 1%Atropine + Racanisodamine, the progress of refraction after treating by other interventions was less than control; among them fourteen interventions such as progressive multi-focal spectacle lenses (0.42 [0.06, 0.79], P < 0.05), bifocal soft contact lenses (0.40 [0.03, 0.77], P < 0.05), orthokeratology (0.56 [0.34, 0.77], P < 0.05), 1%Atropine (0.54 [0.31, 0.77], P < 0.05), 0.5%Atropine (0.67 [0.25, 1.10], P < 0.05), 0.1%Atropine (0.42 [0.15, 0.71], P < 0.05), 0.05%Atropine (0.57 [0.28, 0.86], P < 0.05), 0.01%Atropine (0.33 [0.15, 0.52], P < 0.05), 1%Atropine + bifocal spectacle lenses (1.3 [0.54, 2.00], P < 0.05), 1%Atropine + progressive multi-focal spectacle lenses (0.66 [0.23, 1.10], P < 0.05), 0.01%Atropine + single vision spectacle lenses (0.70 [0.23, 1.10], P < 0.05), 0.01%Atropine + orthokeratology (0.81 [0.43, 1.20], P < 0.05), bifocal spectacle lenses + Massage (0.85 [0.22, 1.50], P < 0.05), single vision spectacle lenses + Red light (0.59 [0.06, 1.10], P < 0.05) were statistically significant from control (Fig. 3B). Network meta-analysis results of refraction changes are presented in the Supplement (eTable 4 in the Supplement).
For slowing refraction progression, the cumulative probability ranking results for each intervention showed that the top ten were: 1%Atropine + bifocal spectacle lenses (96.8%) >0.01%Atropine + orthokeratology (88.6%) > bifocal spectacle lenses + Massage (87.0%) >0.01%Atropine + single vision spectacle lenses (81.5%) >0.5%Atropine (80.6%) >1%Atropine + progressive multi-focal spectacle lenses (79.6%) >0.05%Atropine (74.7%) > orthokeratology (73.7%) > single vision spectacle lenses + Red light (73.2%) > 1%Atropine (71.9%), suggesting that 1%Atropine + bifocal spectacle lenses may be the most effective measure to slow refraction progress (Fig. 4B).
Cluster analysis for ranking of two outcomes
Cluster analysis of the cumulative probabilities of 34 common interventions showed that all interventions fell into 6 categories, with decreasing effectiveness in delaying myopia progression from top right to bottom left; there were a total of 11 interventions in the top right category, of which 5 (45.45%) were combination interventions and 4 (36.36%) were Atropine. This result suggested that combination interventions may most effectively delay myopia progression (Fig. 5).
Note: Atr, atropine; BSCL, bifocal soft contact lenses; BSL, bifocal spectacle lenses; BVLFSL, blue-violet light filtering spectacle lenses; CTED, compound tropicamide eye drops; DIMSSL, defocus incorporated multiple segments spectacle lenses; DISCL, defocus incorporated soft contact lenses; EDOFSCL, extended depth of focus soft contact lenses; MOA, more outdoor activities; OK, orthokeratology; PASCL, progressive addition soft contact lenses; PASL, progressive addition spectacle lenses; PBSL, prismatic bifocal spectacle lenses; PDMSL, peripheral defocus modifying spectacle lenses; Pir, pirenzepine; PMSCL, progressive multi-focal soft contact lenses; PMSL, progressive multi-focal spectacle lenses; Rac, racanisodamine; RGP, rigid gas permeable contact lenses; RL, red light; SLHAL, spectacle lenses with highly aspherical lenslets; SLSAL, spectacle lenses with slightly aspherical lenslets; SVSL, single vision spectacle lenses; +SASCL, positive spherical aberration soft contact lenses.
Publication bias
From the funnel plot of axial length and refraction, it can be found that each point is scattered and asymmetrical incompletely, suggesting that there may be some publication bias. Some scattered points are distributed at the bottom of the funnel plot of each study indicator, indicating a small sample effect (eFig. 2 in the Supplement).
Discussion
Our study is a network meta-analysis to investigate the efficacy of different interventions in slowing myopia progression in children. In addition, this study updates and extends previous evidence-based reviews to some extent. Adding more high-quality clinical trials into this network meta-analysis could provide some clinical recommendations on myopia prevention and control.
The main findings of this study are as follows:
-
1.
In general, the efficacy in slowing myopia progression was in the order of combined measures [21, 26,27,28,29] > Atropine [30,31,32,33,34,35,36,37,38,39,40] >orthokeratology [16, 41,42,43,44] > spectacles [11,12,13,14, 45,46,47,48,49,50,51,52,53,54] or contact lenses [5, 55,56,57,58,59,60,61,62,63] > other single measures [64,65,66].
-
2.
Compared with control, orthokeratology [16, 41, 44] (P < 0.05), 1%Atropine [67] (P < 0.05), 0.01%Atropine + orthokeratology [26,27,28, 68] (P < 0.05) could significantly slow the progression of myopia.
-
3.
In the comparison of different groups of interventions, most of the combination interventions were more effective than other types of interventions, with 1%Atropine + bifocal spectacle lenses [69] and 0.01%Atropine + orthokeratology [26,27,28, 68] being significantly more effective than progressive addition spectacle lenses [11, 47] for myopia prevention and control (P < 0.05; P < 0.05). In spectacles groups, undercorrected single vision spectacle lenses [54] was less effective in slowing the increase in refraction than the other interventions. In contact lenses, the orthokeratology was significantly more effective than progressive addition spectacle lenses in delaying myopia progression (P < 0.05) and significantly more effective than bifocal spectacle lenses (P < 0.05), blue-violet light filtering spectacle lenses (P < 0.05), peripheral defocus modifying spectacle lenses (P < 0.05), progressive addition spectacle lenses (P < 0.05), undercorrected single vision spectacle lenses (P < 0.05), compound tropicamide eye drops (P < 0.05), more outdoor activities (P < 0.05) and 1%Atropine + Racanisodamine (P < 0.05) in delaying refraction progression. In addition, different concentrations of Atropine showed good effects in slowing myopia progression, second only to combination interventions; compound tropicamide eye drops and Pirenzepine were less effective than most of the interventions.
The main strengths of our current network meta-analysis are as follows: firstly, the included studies and the resulting sample size are very large; secondly, many combination interventions contribute to the analysis of the additive effects of two interventions; thirdly, although some interventions have been compared in multiple studies, others have only been performed in one trial or have never been performed. Thus, the network meta-analysis allowed us to validate prior empirical evidence for direct comparisons and provide evidence for comparisons without direct empirical evidence.
There have been few studies on the prevention and control of myopia by multi-focal glasses in recent years, and the conclusions are usually relatively conservative. Most of the subjects are patients with non-simple myopia. Cheng’s study showed that bifocal lenses modestly slowed myopia progression in children with a high rate of myopia progression after 24 months [12]. Fulk’s study suggested that children with myopic esotropia using bifocal glasses rather than single vision glasses appear to somewhat slow myopic progression [70]. From our findings, bifocal glasses have a limited role in myopia prevention and control.
Orthokeratology slows the progression of myopia by providing reasonable mechanical compression of the central corneal region, which flattens the corneal curvature while reducing hyperopic defocus in the peripheral retina. Many studies have shown that orthokeratology significantly slows myopia progression and has become one of the main means of myopia prevention and control. However, orthokeratology is not widespread because of various possible issues, such as the cost, difficulty in regularly going to the hospital for rechecking, intolerable and the risk of corneal infection [71]. Some specially designed soft contact lenses may become a means of myopia prevention and control because they can produce additional myopic defocus on the retina. Our results suggested that specially designed contact lenses are more effective than corresponding spectacles for myopia prevention and control. Because relatively few studies were included, this conclusion still needs to be supported by evidence with larger sample sizes.
As a non-selective M cholinergic receptor antagonist, Atropine has been the first-line drug for myopia prevention and control. Many previous studies have shown that the myopia prevention and control effect of Atropine and its side effects (photophobia, blurred vision, glare) are concentration-dependent; the higher the concentration, the better the effect, and the greater the side effects. Our results did not show a statistically significant concentration dependency, but this suggested that low concentrations of Atropine may be a better choice if the effects are similar.
So far, the mechanism of more outdoor activities slowing myopia progression is not well understood. However, many studies have shown that outdoor activity time of more than 2 h per day can effectively delay the occurrence and progression of myopia [64,65,66]. Unexpectedly, our study suggested that more outdoor activities played a weak role in myopia prevention and control.
The greatest feature of this study is the inclusion of multiple combination interventions, and the results showed that almost all combination interventions were significantly more effective than others. Thus, in clinic, flexible use of two or more interventions for myopia prevention and control is of great interest.
Low-level red light gradually attracts scientists’ interest because of its good effect and operability [21]. The results of a multicentre, randomized, parallel-group, single-blind clinical trial evaluating the efficacy of repeated low-level red light in the treatment of myopia in children showed that after 12 months of intervention, the axial length and spherical equivalent of the single vision spectacle lenses group increased 0.26 mm (95% CI, 0.20~0.31 mm) and - 0.59 D (95% CI, −0.72 to −0.46 D) respectively than the red light group. However, the red light only showed moderate efficacy for myopia in our study. The network meta-analysis showed that single vision spectacle lenses + red light was more effective than bifocal spectacle lenses (P < 0.05) and control (P < 0.05) only in slowing refraction progression.
Limitations
This network meta-analysis has some inherent limitations and should be emphasized. (1) We only focus on the difference in concentration of Atropine but ignore the frequency and time of administration; (2) due to the physical properties of the interventions, double-blind cannot be achieved in many studies; therefore, all the studies with 3 points which were unable to achieve double-blind due to the different physical properties of the interventions were included; (3) due to the lack of safety data in the included literature, we cannot provide information on the safety of different treatment; (4) the range of subjects included is wide, and the potential bias caused by race/ethnicity, parental myopia and environmental factors (such as near work time and outdoor time) was not discussed; (5) the compliance to treatment was not assessed specifically in the risk of bias tool. Clinical decision-making for any intervention requires information about efficacy, short-term/long-term benefits, and risk of side effects, so it is important to perform additional tests on the safety of these interventions.
Conclusions
Despite these limitations, our network meta-analysis provides valuable evidence-based guidelines for analysing the effectiveness of myopia prevention and control measures. (1) Combined measures can not only reduce the side effects of a single intervention but also produce greater effective sizes, which is worth recommending; (2) in addition, Atropine (1%, 0.5%, 0.1%, 0.05%, 0.01%) and orthokeratology are also effective in myopia prevention and control; (3) progressive addition spectacle lenses, undercorrected single vision spectacle lenses, compound tropicamide eye drops are ineffective in children; (4) low-level red light had a role in myopia control, but a more evidence-based rationale is still needed to support it.
Summary
What was known before
-
At present, there are many ways for myopia prevention and control, but it is impossible to compare the effectiveness between every two interventions directly and indirectly.
-
The additive effect of combined intervention in preventing and controlling myopia has been proposed; however, its conclusion still needs to be supported by a large amount of evidence.
What this study adds
-
The combined measures were most effective, followed by Atropine, and the least effective were progressive addition spectacle lenses, undercorrected single vision spectacle lenses, compound tropicamide eye drops, and Pirenzepine.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article [and/or] its supplementary materials.
References
Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123:1036–42.
Vongphanit J, Mitchell P, Wang JJ. Prevalence and progression of myopic retinopathy in an older population. Ophthalmology. 2002;109:704–11.
Eye Disease Case-Control Study Group. Risk factors for idiopathic rhegmatogenous retinal detachment. The Eye Disease Case-Control Study Group. Am J Epidemiol. 1993;137:749–57.
Mitchell P, Hourihan F, Sandbach J, Wang JJ. The relationship between glaucoma and myopia: the Blue Mountains Eye Study. Ophthalmology. 1999;106:2010–5.
Katz J, Schein OD, Levy B, Cruiscullo T, Saw SM, Rajan U, et al. A randomized trial of rigid gas permeable contact lenses to reduce progression of children’s myopia. Am J Ophthalmol. 2003;136:82–90.
Ma Y, Qu X, Zhu X, Xu X, Zhu J, Sankaridurg P, et al. Age-specific prevalence of visual impairment and refractive error in children aged 3-10 years in Shanghai, China. Invest Ophthalmol Vis Sci. 2016;57:6188–96.
Lin LL, Shih YF, Hsiao CK, Chen CJ. Prevalence of myopia in Taiwanese schoolchildren: 1983 to 2000. Ann Acad Med Singap. 2004;33:27–33.
Wu PC, Huang HM, Yu HJ, Fang PC, Chen CT. Epidemiology of myopia. Asia Pac J Ophthalmol (Phila). 2016;5:386–93.
Saw SM, Tong L, Chua WH, Chia KS, Koh D, Tan DT, et al. Incidence and progression of myopia in Singaporean school children. Invest Ophthalmol Vis Sci. 2005;46:51–7.
Baird PN, Saw SM, Lanca C, Guggenheim JA, Smith Iii EL, Zhou X, et al. Myopia. Nat Rev Dis Primers. 2020;6:99.
Gwiazda J, Hyman L, Hussein M, Everett D, Norton TT, Kurtz D, et al. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Invest Ophthalmol Vis Sci. 2003;44:1492–1500.
Cheng D, Schmid KL, Woo GC, Drobe B. Randomized trial of effect of bifocal and prismatic bifocal spectacles on myopic progression: two-year results. Arch Ophthalmol. 2010;128:12–9.
Hasebe S, Ohtsuki H, Nonaka T, Nakatsuka C, Miyata M, Hamasaki I, et al. Effect of progressive addition lenses on myopia progression in Japanese children: a prospective, randomized, double-masked, crossover trial. Invest Ophthalmol Vis Sci. 2008;49:2781–9.
Berntsen DA, Sinnott LT, Mutti DO, Zadnik K. A randomized trial using progressive addition lenses to evaluate theories of myopia progression in children with a high lag of accommodation. Invest Ophthalmol Vis Sci. 2012;53:640–9.
Walline JJ, Lindsley K, Vedula SS, Cotter SA, Mutti DO, Twelker JD. Interventions to slow progression of myopia in children. Cochrane Database Syst Rev. 2011:Cd004916.
Cho P, Cheung SW. Retardation of myopia in Orthokeratology (ROMIO) study: a 2-year randomized clinical trial. Invest Ophthalmol Vis Sci. 2012;53:7077–85.
Sun Y, Xu F, Zhang T, Liu M, Wang D, Chen Y, et al. Orthokeratology to control myopia progression: a meta-analysis. PLoS One. 2015;10:e0124535.
Kang P, McAlinden C, Wildsoet CF. Effects of multifocal soft contact lenses used to slow myopia progression on quality of vision in young adults. Acta Ophthalmol. 2017;95:e43–e53.
Xiong S, Sankaridurg P, Naduvilath T, Zang J, Zou H, Zhu J, et al. Time spent in outdoor activities in relation to myopia prevention and control: a meta-analysis and systematic review. Acta Ophthalmol. 2017;95:551–66.
Saw SM. A synopsis of the prevalence rates and environmental risk factors for myopia. Clin Exp Optom. 2003;86:289–94.
Jiang Y, Zhu Z, Tan X, Kong X, Zhong H, Zhang J, et al. Effect of repeated low-level red-light therapy for myopia control in children: a multicenter randomized controlled trial. Ophthalmology. 2021;129:509–19.
Smith EL 3rd, Kee CS, Ramamirtham R, Qiao-Grider Y, Hung LF. Peripheral vision can influence eye growth and refractive development in infant monkeys. Invest Ophthalmol Vis Sci. 2005;46:3965–72.
Gwiazda J, Thorn F, Bauer J, Held R. Myopic children show insufficient accommodative response to blur. Invest Ophthalmol Vis Sci. 1993;34:690–4.
McBrien NA, Moghaddam HO, Reeder AP. Atropine reduces experimental myopia and eye enlargement via a nonaccommodative mechanism. Invest Ophthalmol Vis Sci. 1993;34:205–15.
Rose KA, Morgan IG, Ip J, Kifley A, Huynh S, Smith W, et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008;115:1279–85.
Kinoshita N, Konno Y, Hamada N, Kanda Y, Shimmura-Tomita M, Kaburaki T, et al. Efficacy of combined orthokeratology and 0.01% atropine solution for slowing axial elongation in children with myopia: a 2-year randomised trial. Sci Rep. 2020;10:12750.
Tan Q, Ng AL, Choy BN, Cheng GP, Woo VC, Cho P. One-year results of 0.01% atropine with orthokeratology (AOK) study: a randomised clinical trial. Ophthalmic Physiol Opt. 2020;40:557–66.
Zhao Q, Hao Q. Clinical efficacy of 0.01% atropine in retarding the progression of myopia in children. Int Ophthalmol. 2021;41:1011–7.
Charm J, Cho P. High myopia–partial reduction ortho-k: a 2-year randomized study. Optom Vis Sci. 2013;90:530–9.
Chua WH, Balakrishnan V, Chan YH, Tong L, Ling Y, Quah BL, et al. Atropine for the treatment of childhood myopia. Ophthalmology. 2006;113:2285–91.
Fan DSP, Lam DSC, Chan CKM, Fan AH, Cheung EYY, Rao SK. Topical atropine in retarding myopic progression and axial length growth in children with moderate to severe myopia: a pilot study. Jpn J Ophthalmol. 2007;51:27–33.
Zhu Q, Tang Y, Guo L, Tighe S, Zhou Y, Zhang X, et al. Efficacy and safety of 1% atropine on retardation of moderate myopia progression in chinese school children. Int J Med Sci. 2020;17:176–81.
Wang YR, Bian HL, Wang Q. Atropine 0.5% eyedrops for the treatment of children with low myopia: A randomized controlled trial. Medicine (Baltimore). 2017;96:e7371.
Chia A, Chua WH, Cheung YB, Wong WL, Lingham A, Fong A, et al. Atropine for the treatment of childhood myopia: safety and efficacy of 0.5%, 0.1%, and 0.01% doses (Atropine for the Treatment of Myopia 2). Ophthalmology. 2012;119:347–54.
Li FF, Kam KW, Zhang Y, Tang SM, Young AL, Chen LJ, et al. Differential effects on ocular biometrics by 0.05%, 0.025%, and 0.01% atropine: low-concentration atropine for myopia progression study. Ophthalmology. 2020;127:1603–11.
Fu A, Stapleton F, Wei L, Wang W, Zhao B, Watt K, et al. Effect of low-dose atropine on myopia progression, pupil diameter and accommodative amplitude: low-dose atropine and myopia progression. Br J Ophthalmol. 2020;104:1535–41.
Chaurasia S, Negi S, Kumar A, Raj S, Kaushik S, Optom RKM, et al. Efficacy of 0.01% low dose atropine and its correlation with various factors in myopia control in the Indian population. Sci Rep. 2022;12:7113.
Jethani J. Efficacy of low-concentration atropine (0.01%) eye drops for prevention of axial myopic progression in premyopes. Indian J Ophthalmol. 2021;70:238–40.
Moriche-Carretero M, Revilla-Amores R, Diaz-Valle D, Morales-Fernández L, Gomez-de-Liaño R. Myopia progression and axial elongation in Spanish children: efficacy of atropine 0.01% eye-drops. J Fr Ophtalmol. 2021;44:1499–504.
Wei S, Li SM, An W, Du J, Liang X, Sun Y, et al. Safety and efficacy of low-dose atropine eyedrops for the treatment of myopia progression in Chinese children: a randomized clinical trial. JAMA ophthalmology. 2020;138:1178–84.
Ruiz-Pomeda A, Pérez-Sánchez B, Valls I, Prieto-Garrido FL, Gutiérrez-Ortega R, Villa-Collar C. MiSight Assessment Study Spain (MASS). A 2-year randomized clinical trial. Graefes Arch Clin Exp Ophthalmol. 2018;256:1011–21.
Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, Gutierrez-Ortega R. Myopia control with orthokeratology contact lenses in Spain: refractive and biometric changes. Invest Ophthalmol Vis Sci. 2012;53:5060–5.
Tang WT, Li JQ, Zhou LS, Yu Q. Effect of orthokeratology on relative peripheral refraction in adolescent myopia. International eye science. 2021;21:734–7.
Walline JJ, Jones LA, Sinnott LT. Corneal reshaping and myopia progression. Br J Ophthalmol. 2009;93:1181–5.
Zhao HL, Jiang J, Yu J, Xu HM. Role of short-wavelength filtering lenses in delaying myopia progression and amelioration of asthenopia in juveniles. Int J Ophthalmol. 2017;10:1261–7.
Lam CSY, Tang WC, Tse DY, Lee RPK, Chun RKM, Hasegawa K, et al. Defocus Incorporated Multiple Segments (DIMS) spectacle lenses slow myopia progression: a 2-year randomised clinical trial. Br J Ophthalmol. 2020;104:363–8.
Hasebe S, Jun J, Varnas SR. Myopia control with positively aspherized progressive addition lenses: a 2-year, multicenter, randomized, controlled trial. Invest Ophthalmol Vis Sci. 2014;55:7177–88.
Leung JTM, Brown B. Progression of myopia in Hong Kong Chinese schoolchildren is slowed by wearing progressive lenses. Optom Vis Sci. 1999;76:346–54.
Gwiazda JE. Progressive-addition lenses versus single-vision lenses for slowing progression of myopia in children with high accommodative lag and near esophoria. Invest Ophthalmol Vis Sci. 2011;52:2749–57.
Edwards MH, Li RW, Lam CS, Lew JK, Yu BS. The Hong Kong progressive lens myopia control study: study design and main findings. Invest Ophthalmol Vis Sci. 2002;43:2852–8.
Zhu X, Wang D, Li N, Zhao F. Effects of customized progressive addition lenses vs. single vision lenses on myopia progression in children with esophoria: a randomized clinical trial. Journal of ophthalmology. 2022;2022:9972761.
Huang JO, Wei XH. Effect of peripheral vision control technology in the development of juvenile myopia. International eye science. 2015;15:378–80.
Bao J, Huang Y, Li X, Yang A, Zhou F, Wu J, et al. Spectacle lenses with aspherical lenslets for myopia control vs single-vision spectacle lenses: a randomized clinical trial. JAMA ophthalmology. 2022;140:472–8.
Adler D, Millodot M. The possible effect of undercorrection on myopic progression in children. Clinical and Experimental Optometry. 2006;89:315–21.
Aller TA, Liu M, Wildsoet CF. Myopia control with bifocal contact lenses: a randomized clinical trial. Optom Vis Sci. 2016;93:344–52.
Sankaridurg P, Bakaraju RC, Naduvilath T, Chen X, Weng R, Tilia D, et al. Myopia control with novel central and peripheral plus contact lenses and extended depth of focus contact lenses: 2 year results from a randomised clinical trial. Ophthalmic Physiol Opt. 2019;39:294–307.
Chamberlain P, Peixoto-de-Matos SC, Logan NS, Ngo C, Jones D, Young G. A 3-year randomized clinical trial of misight lenses for myopia control. Optom Vis Sci. 2019;96:556–67.
Shen EP, Chu HS, Cheng HC, Tsai TH. Center-for-near extended-depth-of-focus soft contact lens for myopia control in children: 1-year results of a randomized controlled trial. Ophthalmol Ther. 2022;11:1577–88.
Fujikado T, Ninomiya S, Kobayashi T, Suzaki A, Nakada M, Nishida K. Effect of low-addition soft contact lenses with decentered optical design on myopia progression in children: a pilot study. Clin Ophthalmol. 2014;8:1947–56.
Walline JJ, Walker MK, Mutti DO, Jones-Jordan LA, Sinnott LT, Giannoni AG, et al. Effect of high add power, medium add power, or single-vision contact lenses on myopia progression in children: The BLINK randomized clinical trial. JAMA. 2020;324:571–80.
Walline JJ, Greiner KL, McVey ME, Jones-Jordan LA. Multifocal contact lens myopia control. Optom Vis Sci. 2013;90:1207–14.
Walline JJ, Jones LA, Mutti DO, Zadnik K. A randomized trial of the effects of rigid contact lenses on myopia progression. Arch Ophthalmol. 2004;122:1760–6.
Cheng X, Xu J, Chehab K, Exford J, Brennan N. Soft contact lenses with positive spherical aberration for myopia control. Optom Vis Sci. 2016;93:353–66.
He M, Xiang F, Zeng Y, Mai J, Chen Q, Zhang J, et al. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA. 2015;314:1142–8.
He X, Sankaridurg P, Wang J, Chen J, Naduvilath T, He M, et al. Time outdoors in reducing myopia: a school-based cluster randomized trial with objective monitoring of outdoor time and light intensity. Ophthalmology. 2022;129:1245–54.
Wu PC, Chen CT, Lin KK, Sun CC, Kuo CN, Huang HM, et al. Myopia prevention and outdoor light intensity in a school-based cluster randomized trial. Ophthalmology. 2018;125:1239–50.
Gong Q, Liu L. Therapeutic effect of atropine 1% in children with low myopia. J AAPOS. 2016;20:379.
Tan Q, Ng AL, Cheng GP, Woo VC, Cho P. Combined 0.01% atropine with orthokeratology in childhood myopia control (AOK) study: A 2-year randomized clinical trial. Cont Lens Anterior Eye. 2022;46:101723.
Zhang H, Chen M. Curative effects and mechanisms of atropine with a long term use on myopia in children (in Chinese) [J]. Recent Adv. Ophthalmol. 2009;29:851–4.
Fulk GW, Cyert LA, Parker DE. A randomized trial of the effect of single-vision vs. bifocal lenses on myopia progression in children with esophoria. Optom Vis Sci. 2000;77:395–401.
Kam KW, Yung W, Li GKH, Chen LJ, Young AL. Infectious keratitis and orthokeratology lens use: a systematic review. Infection. 2017;45:727–35.
Funding
This work was supported by the Natural Science Foundation of China under Grant [No. 82171026].
Author information
Authors and Affiliations
Contributions
GZ and JJ extracted data from published studies and analysed the results. GZ retrieved, ranked documents and drafted the manuscript. CQ provided oversight for the extraction and analysis and identified the accuracy of results and discussion presented in the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
An ethics statement is not applicable because this study is based exclusively on published literature.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, G., Jiang, J. & Qu, C. Myopia prevention and control in children: a systematic review and network meta-analysis. Eye 37, 3461–3469 (2023). https://doi.org/10.1038/s41433-023-02534-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02534-8
- Springer Nature Limited