Abstract
Purpose
Myopia is a prevalent condition among Asians. Orthokeratology lens has gained popularity as a method of myopia control. This systematic review is to summarize the clinical profile of infectious keratitis in association with orthokeratology lens wear.
Methods
We searched in the PubMed and EMBASE for articles adopting the search strategy “(orthokeratology lens OR orthokeratology) AND (bacterial eye infection OR keratitis OR cornea ulcer OR microbial keratitis OR bacterial keratitis)”, from the start date of the databases to August 23, 2016. Articles reporting infectious keratitis in orthokeratology lens users with data of individual cases were considered eligible for this systematic review. We recorded the outcome measures including method of diagnosis, etiological agents, duration and mode of treatment and treatment outcomes.
Results
Our literature search yielded 172 papers. After removing duplicated and irrelevant reports, we included 29 articles for data analysis, involving 173 eyes. Among all reported cases, the mean age at presentation was 15.4 ± 6.2 years, with a female preponderance (male-to-female ratio 1:1.7). Positive microbiological cultures were reported in 69.4% of cases, with Pseudomonas aeruginosa and Acanthamoeba being the most common etiological agents. The mean duration of hospitalization was 7.7 ± 6.7 days. Mean LogMAR visual acuity at presentation was 1.17 ± 0.78, increased to 0.33 ± 0.41 at final visit (p < 0.001).
Conclusions
Despite early intervention and treatment, the majority of infections resulted in the formation of corneal scars and almost 10% of eyes needed surgical treatment. Timely awareness and treatment of keratitis should be emphasized to the users.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myopia is a prevalent ocular disorder globally, especially in Asia, where the prevalence was up to 90% among young adults [1]. Axial elongation of the globe is a major mechanism of myopia development in children [2]. Over the past several decades, different strategies towards prevention or control of myopic progression have been proposed, including topical atropine eye drops [3], increased outdoor activity [4], and orthokeratology lenses use. The atropine for treatment of myopia (ATOM) study has established the efficacy of atropine eye drops in retarding myopic progression over 5 years, during which atropine was found to be safe and not associated with serious adverse effect. However, a rebound phenomenon was observed with higher concentration of atropine [5]. Increased outdoor activities have been found to reduce the incidence of myopia over a 3-year-period in a cluster randomized controlled trial conducted in Guangzhou, China [6].
Orthokeratology adopts reverse geometry rigid gas-permeable contact lenses to alter the corneal shape and hence refractive power. The effect is transient; therefore, the users need to wear the orthokeratology lenses during night time while asleep, so that they can avoid wearing glasses during daytime. Although studies have reported the effect of orthokeratology in slowing axial elongation, level I evidence showing long-term efficacy of orthokeratology in reducing myopia progression is lacking [7]. Studies on orthokeratology lens were either limited by the relative short follow-up to study myopia which develops over years [8] or small sample sizes. Besides, other factors that may influence myopic progression were often not possible to be controlled in these small numbers of subjects such as genetic factors, parental myopia and gene-environmental interactions [8]. One of the non-randomized clinical studies by Santodomingo-Rubido et al., examined refractive outcomes of 14 orthokeratology lens wearers with more than 6 years of follow-up. They reported a trend toward a reduction in the rate of axial elongation in the orthokeratology group when compared to the sixteen controls. However, the authors also reported that no significant relationships could be found between the change in axial length at 7 years in comparison to baseline, alongside the mean spherical equivalent refractive error for either orthokeratology or control groups [9]. The actual efficacy of orthokeratology in reducing myopia progression remained an implication rooted on an apparently slower axial elongation. On the other hand, the safety profile of orthokeratology should raise concern. The compressive forces of the reverse geometry rigid lenses may disrupt the corneal epithelium and extended overnight wear may potentiate infectious keratitis [10]. So far, a number of case reports and case series have reported infectious keratitis associated with orthokeratology lens use, but the clinical profiles and microbial spectra were variable across studies. We thus conducted a systematic review to summarize the clinical profile of infectious keratitis associated with orthokeratology lens use.
Materials and methods
Search strategy
We searched in PubMed and EMBASE for studies that evaluated infectious keratitis associated with orthokeratology lens wear. In PubMed, we used the following search terms “(orthokeratology OR orthokeratology lens) AND (keratitis OR microbial OR bacterial OR fungal OR herpetic OR corneal ulcer OR complications OR infective OR infection OR eye infection)” and yielded 97 titles. In EMBASE, we used the search terms “Orthokeratology lens/or orthokeratology” AND “Bacterial eye infection/or keratitis/or cornea ulcer/or microbial keratitis” from the period of 1980–2017 and 75 titles were identified. We did not apply any language restrictions in our search. Official translation of articles published originally in another language was obtained from the publisher or original journal website. We performed the final search in all databases on August 23, 2016.
Inclusion and exclusion criteria
Two reviewers independently assessed the titles and abstracts to identify articles that fulfilled the inclusion criteria: (1) clinical studies; (2) studies that included human subjects; and (3) studies that assessed infectious keratitis or infections associated with orthokeratology lens wear. Any discrepancies were solved by discussion with a third reviewer. We excluded studies that only discussed either infectious keratitis or orthokeratology lens separately, or studies that do not provide sufficient data for analysis. We also reviewed the references of articles to identify any relevant studies that were not identified in the initial literature search.
Data extraction
Two reviewers independently performed data extraction, and then combined for crosscheck of data accuracy. Duplicated data of any identical patients reported in more than one article were eliminated. We used a customized form to record the authors of study, year of publication, country of publication, sample size, mean age of subjects, gender, duration of orthokeratology lens wear and pre-morbid visual function in logarithm of minimal angle resolution (LogMAR) visual acuity and intraocular pressure where reported. Snellen visual acuity was converted to LogMAR units. Counting finger was equivalent to 2.0 LogMAR units and hand motion was 3.0. Visual acuity of light perception or less was excluded from calculating the geometric mean. In studies where only the mean value was reported, it was assumed that all subjects bore the same mean value in calculation of the standard deviation. Information regarding the infectious episodes, including the method of diagnosis, ancillary investigations such as confocal microscopy and corneal biopsy, mode and duration of treatment, complications and outcomes was extracted for analyses. Unclear or insufficient data were discarded from statistical analyses where appropriate.
Statistical analysis
After detailed assessment of the data from all the included studies, we found that no single parameter is eligible for meta-analysis. Therefore, in this systematic review, we reported the mean, median, range and standard deviations for descriptive statistics where appropriate. We adopted the Chi-square test to assess the association between categorical variables, and Mann–Whitney U test to compare pre-morbid and final geometric mean LogMAR visual acuity. A two-tailed p value of <0.05 is considered statistically significant.
Results
We identified a total of 172 studies from our literature search in the two databases. After removing 55 duplicates, we assessed 117 titles and abstracts and excluded 55 records that were not eligible according to our inclusion criteria. We then retrieved 72 articles for full text review but excluded 32 studies which only discussed either orthokeratology or infectious keratitis, and another 11 studies where there were no sufficient data of individual case. We finally included 29 studies into the systematic review. Figure 1 shows the flow of our study inclusion. Most studies have been individually referenced in the rest of this article, except a few [11,12,13].
Characteristics of the included studies
The characteristics of the 29 included studies, involving a total of 173 eyes of 166 subjects, are shown in Table 1. These studies were published between years 2002–2014. Among them, 18 were case series and 11 were case reports. No level I evidence or any randomized controlled trial or comparative trial was identified from our literature search. Eighteen of the 29 studies were conducted in the Asian populations, with the majority from Taiwan (n = 6) and Hong Kong (n = 5), followed by South Korea (n = 3), China (n = 2), Japan (n = 1) and Singapore (n = 1). Among the other 11 studies, four were from North America, three from Australia, two from Europe, and two from Israel.
Demographics
The majority of patients with orthokeratology-related infectious keratitis were female, with a male to female ratio of 1:1.7. There were 59 male and 99 female subjects, and the gender of 8 subjects was not reported [28]. The mean age of subjects at diagnosis was 15.4 ± 6.2 years (median 14.0; range 8–60 years). Figure 2 shows the age and sex distribution of patients. The mean duration of orthokeratology lens wear before onset of disease was 19.4 ± 15.5 months (median 15.5 months; range 5 days–156 months). The majority of patients had unilateral disease, except for seven patients who had bilateral involvement, of which six were under age 18 years. Among these seven patients, three were reported in Korea [14,15,16], three were from Taiwan [17,18,19] and one from the United States [20]. The mean pre-morbid spherical equivalent was −3.81 ± 1.56 diopters (D) (median −4.0D; range −8.75 to −1.25D.) The indication for orthokeratology lens wear was not specified in the majority of cases. The reported indications were myopia control (n = 41), myopia correction (n = 7) and myopia reduction (n = 3), respectively.
Risk of orthokeratology lens associated infectious keratitis
Only one included article discussed the risk of infectious keratitis among orthokeratology lens wearers. The study was a post-marketing surveillance of the Paragon Corneal Refractive Therapy where 1317 orthokeratology lens wearers (640 adults and 677 children) were surveyed and only two episodes of infectious keratitis were reported.
Diagnosis of infectious keratitis
Cultures were obtained from corneal epithelium in the majority of patients, followed by cultures of the offending contact lens, the storage solution or the storage case. Overall the positivity of microbiological cultures (from any specimen) was 69.4% (120/173 eyes). Corneal scrapings were reported to be performed in 116 eyes. Among them, 91 corneal specimens (78.4%) were positive and 25 (21.6%) were negative. Besides Gram staining, inverted phase contrast microscopy was performed in one study [14] and axenization and molecular techniques were utilized to identify acanthamoeba strains in another [16]. Cultures of the contact lens were reported in 40 cases (23.1%), of which 20 (50.0%) showed positive finding of one or more micro-organisms. Cultures of the contact lens storage solution were reported in 61 cases (35.3%), of which 20 (32.8%) yielded positive findings.
The remaining 53 patients had pan-negative microbiological cultures from corneal specimen, contact lens, storage solution or the storage case. These cases were either treated empirically or further investigated with confocal microscopy.
Ancillary investigations
In vivo confocal microscopy (IVCM) was reported to be positive in six cases [21,22,23,24]. No negative confocal microscopy was reported. All of them identified the presence of acanthamoeba cysts. Four cases had negative cultures for Acanthamoeba using non-nutrient agar plates, and the diagnosis of Acanthamoebic keratitis relied solely on confocal microscopy [21,22,23]. Reassessment by IVCM in 1 year after medical and crosslinking treatment was reported in one study [7].
In the study of Wilhelmus et al., corneal biopsy was performed in the diagnosis of acanthaemobic keratitis in a 16-year-old girl in addition to positive corneal scrapings and contact lens cultures, both of which yielded Acanthamoeba species. Confocal microscopy was, however, not reported [20].
Microbiology
The most commonly identified agent was Pseudomonas aeruginosa (36.4%), followed by Acanthamoeba species (32.4%) and coagulase negative staphylococcus (6.9%). Two cases of fungal infections (1.2%) were identified. Among all reported cases with positive microbiology, ten eyes were polymicrobial [10, 17, 25,26,27]. Nine of the ten eyes had Pseudomonas aeruginosa infection and co-infection by other organism(s). These organisms included staphylococci, Flavobacterium species, Serratia, Xanthomonas, Pseudomonas putida, Burkholderia cepacia and Klebsiella species. The remaining patient had both acanthamoeba and coagulase negative staphylococci identified. Figure 3 shows the frequency distribution of micro-organisms identified in positive cornea/contact lens/contact lens case/contact lens solution cultures and/or confocal microscopy.
Clinical course
The mean duration of hospitalization was 7.7 ± 6.7 days (range 3–15.3 days) in three studies [25, 28], and the mean duration of disease from onset to remission was 96.7 ± 67.8 days (range 2.5–223 days). The mean duration of antimicrobial treatment was 4.5 ± 5.4 months (range 2.5 days–20 months).
Treatment
Medical treatment
Topical antimicrobial agents were cornerstone to regimen, supplemented with subconjunctival, oral or intravenous injections in selected cases. Regarding bacterial infection, topical monotherapy or combination therapy was both adopted (monotherapy no. of studies: 10; combination: 13). Monotherapy with fluoroquinolone was reported in six studies, followed by aminoglycoside in 2, cephalosporin in 1 and aminoglycoside in 1 [17,18,19, 21, 25, 27, 29,30,31]. Combination therapy was reported in 13 studies, involving different combinations of the four groups of antibiotics named above [14, 17,18,19, 24,25,26,27,28, 32,33,34]. Intravenous cephalosporin was reported in three studies [26, 34, 35], whilst subconjunctival cephalosporin or aminoglycoside was reported in two studies [16, 35].
For acanthamoebic infections, combination therapy was more commonly adopted than monotherapy. Monotherapy with polyhexamethylene biguanide (PHMB) was reported in two studies only [14, 32], whereas in the remaining 13 studies combination therapy involving different combinations of PHMB, Brolene, chlorhexidine, neomycin and amidine [15,16,17, 19,20,21,22,23,24,25, 34, 36, 38]. PHMB was the most common anti-amoebic agent of choice, reported in 11 out of 15 studies reporting acanthamoebic keratitis. Adjunctive oral itraconazole was adopted in three studies [16, 20, 23]. There was no report of subconjunctival or intravenous injection for acanthamoebic keratitis.
Surgical treatment
Surgical treatments were reported in four studies [20,21,22, 34]. One patient required insertion of Ahmed valve shunt for refractory secondary glaucoma [22]. Wilhelmus reviewed the literature and identified 17 patients who suffered from acanthaemobic keratitis associated with orthokeratology; 11 of these eyes underwent corneal transplantation as part of the treatment [20]. Yepes et al. reported that a 41-year-old Canadian who was diagnosed with acanthamoebic keratitis had elective combined cataract surgery and corneal transplant for dense corneal scarring and secondary cataract; however, no surgical outcome was reported [34].
Arance-Gil et al. diagnosed a case of acanthamoebic keratitis using confocal microscopy with pan-negative cultures [21]. The patient’s condition progressed despite undergoing 1 year of intensive combination anti-amoebic therapy and standard corneal cross-linking was performed at one year for ulceration and recurrent uveitis. Despite improvements in signs and symptoms following crosslinking, the patient underwent further amniotic membrane implantation for deficient corneal re-epithelialization at 2 months later. Eventually the patient developed corneal melting and secondary glaucoma and, therefore, underwent a glaucoma filtration surgery combined with cataract extraction and penetrating keratoplasty at 20 months after the onset of infection.
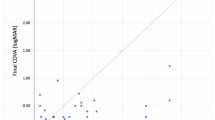
Visual outcome and complications
The geometric mean LogMAR visual acuity at presentation was 1.17 ± 0.78, and at final visit 0.33 ± 0.41 (p < 0.001). The most common complication was the formation of corneal scars with and without irregular astigmatism. Thirteen eyes warranted a corneal transplantation either as lamellar or full-thickness replacement. This is followed by two cases of cataracts and two cases of glaucoma. There was no report of corneal perforation or endophthalmitis.
Discussion
In this systematic review, we summarized the clinical profiles of orthokeratology-related infectious keratitis. Most of the patients were under the age of 18 years. The mean duration between the starting of orthokeratology lens wear and the onset of keratitis was 19.4 months, inferring that the majority of patients were not beginners of contact lens use. Nevertheless, it is noteworthy that about half of the infections have occurred within the first two years. Therefore, patient education, including correct usage, symptoms and signs of keratitis, and the need of early attendance to ophthalmology clinics should be emphasized to fresh users of orthokeratology lenses.
As all included studies were case series or case reports, our review could not establish the incidence of infectious keratitis associated with orthokeratology lens use. In a nationwide survey performed in Singapore, among 953 complications reported to be associated with contact lens wear, there were 244 cases of infective keratitis which was the commonest complication [37]. The surveillance study by Bullimore et al. is indeed the only source of information regarding the absolute risk of infectious keratitis. In this study, the overall incidence was estimated to be 7.7 in 10,000 per year of orthokeratology lens wear. However, this study was observational in nature and deemed susceptible to significant participation and reporting bias. Only 86 out of 200 orthokeratology lens practitioners contacted replied to the survey. Among the 50 events reported, the diagnosis of definite microbial keratitis was dependent on a voting system formed by the investigator panel instead of the attending clinician/contact lens practitioner. Subjects who presented to alternative practitioner who were not included or did not respond to the survey would have been missed.
Like any other infection, microbiological culture of the infected specimen was of utmost importance in confirming the diagnosis and guiding subsequent antimicrobial treatment. Corneal scraping was performed in majority of eyes but still one in five cultures had failed to identify any organism. Nevertheless, corneal scraping yielded the highest positivity results than specimens from contact lens, solution or their cases. One limitation of any microbiological culture was the difficulty in differentiating genuine offending microorganism versus contamination. Due to proximity of cornea and the eyelids, the identification of skin flora in microbiological culture might not always indicate genuine infection by skin flora. Hence, the utilization of IVCM remains crucial in arriving at the final diagnosis.
Clinical practice for treating infectious keratitis may vary among practitioners and institutions. Patients may be managed as outpatients or inpatients at the discretion and experience of the treating clinicians. Hence, the mean duration of hospitalization may not bear significance to individual practitioner. However, the mean duration of hospitalization of one week might be noteworthy for the authority as the cost of hospitalization needs to be taken into account. The cost of medications especially non-formulary items or non-commercially available items such as anti-amoebic agents like PHMB, or anti-fungal agents requires special preparations by individual pharmacies. The often prolonged recommended treatment duration, especially for fungal and amoebic infection, further adds to the costs of these illnesses.
Although clinical history may provide clues to clinicians regarding the offending micro-organisms, it was known that overlapping clinical findings of microbial keratitis caused by various agents might not be easily distinguishable by slit-lamp examination alone. Fortified broad-spectrum antibiotic eyedrops were often used as the empirical treatment for suspected bacterial keratitis before the results of microbiological cultures are available. A combination of two agents with coverage of the different bacterial spectrum was often adopted. The initial response of the keratitis to such treatment would provide further clues to clinicians regarding the causative agents of the microbial keratitis.
Like other contact lens keratitis, pseudomonas and acanthamoeba are the commonest micro-organisms involved in orthokeratology lens-related keratitis, as these organisms are known to adhere to surfaces of the rigid gas-permeable contact lenses. Reduced oxygen transmission and redistribution of the corneal epithelium as a result of the compressive forces of the reverse geometry lenses may predispose the eye to disruption in the epithelial barrier and subsequently infection [27].
Among included studies, majority arise from Asian populations such as Hong Kong, Taiwan and Singapore, and only two patients from Europe were included. This might be related to the high prevalence of myopia in Asia and, hence, the demand for myopia control. However, a rise in popularity of Orthokeratology lens across Europe in recent years was reported.
Corneal scars are the top complication following infectious keratitis in our review, followed by two eyes with cataract and two eyes with glaucoma among reported cases. Despite the apparently small number, one has to take into account that both cataract and glaucoma are chronic conditions and may continue to develop with time. The formation of peripheral anterior synechiae was not reported in the studies, which, however, might be related to subsequent development of glaucoma. The intraocular pressure was not reported or mentioned in the majority of studies and hence could not be analyzed.
Overall 12 eyes (6.9%) underwent corneal transplantation for corneal scar, and 1 eye was scheduled for combined corneal transplant and cataract extraction. One cataract surgery (0.6%) and two glaucoma procedures (1.2%) were performed among the 173 eyes. The rate of keratoplasty identified in our systematic review was lower than the series from Por et al., who reported an outbreak of 42 patients with acanthamoebic keratitis and 15 of whom required corneal transplantations. This was likely due to the heterogeneity of the offending organisms included in our review [38]. In the Netherlands, Hoddenbach et al. reported that more than 20% of eyes with contact lens-associated microbial keratitis had required corneal transplantation either as elective or emergency as a result of perforation. Furthermore, 19 keratoplasties were scheduled in their series due to substantial loss of vision as a result of scarring. Similar to our review, their series contained a variety of micro-organisms; however, almost 90% of their patients wore soft contact lenses which were known to carry a higher risk of microbial keratitis than rigid lenses [39]. Noureddin et al. recently reviewed their retrospective data on pediatric infectious keratitis and 3 of 16 patients required either penetrating or deep anterior lamellar keratoplasty as part of visual rehabilitation. In their series, only a third of these included children had prior contact lens wear and the rest had other risk factors including three patients with Stevens–Johnson syndrome [40].
The figures in our review represent the severity of infectious keratitis as a complication of orthokeratology, and as many of these subjects were young, the long-term outcome of these operations could not be addressed through this systematic review.
This systematic review was limited by its retrospective nature and variation in individual clinical practices between institutions and practitioner. The nature of some included studies utilized survey to derive the diagnosis of microbial keratitis may introduce information bias in disease ascertainment. The wide spectrum of microbiological agents and range of treatment duration and modalities may limit the meaning of the final visual acuity. Also, the majority of the patients are Asians with only two studies from Europe included in our study. This may affect generalization of our results. But the rate of surgical intervention required should raise concerns among eye care professionals.
In summary, this systemic review summarized the clinical profile of infectious keratitis associated with orthokeratology lens use, with Pseudomonas aeruginosa and Acanthamoeba being the most commonly identified offending agents. The majority of these infections resulted in the formation of corneal scars and almost 10% of eyes needed surgical treatment. Proper use of the orthokeratology lens, early awareness of corneal infection with timely clinical attendance should be emphasized to the patients.
References
Goh WS, Lam CS. Changes in refractive trends and optical components of Hong Kong Chinese aged 19–39 years. Ophthalmic Physiol Opt. 1994;14:378–82.
Fledelius HC. Ophthalmic changes from age of 10 to 18 years. A longitudinal study of sequels to low birth weight. III. Ultrasound oculometry and keratometry of anterior eye segment. Acta Ophthalmol. 1982;60:393–402.
Chua WH, Balakrishnan V, Chan YH, et al. Atropine for the treatment of childhood myopia. Ophthalmology. 2006;113:2285–91.
Rose KA, Morgan IG, Ip J, et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008;115:1279–85.
Chia A, Chua WH, Tan D. Effect of topical atropine on astigmatism. Br J Ophthalmol. 2009;93:799–802.
He M, Xiang F, Zeng Y, et al. Effect of time spent outdoors at School on the development of myopia among children in China: a randomized clinical trial. JAMA. 2015;314:1142–8.
Cho P, Cheung SW. Retardation of myopia in Orthokeratology (ROMIO) study: a 2-year randomized clinical trial. Invest Ophthalmol Vis Sci. 2012;53:7077–85.
He M, Du Y, Liu Q, et al. Effects of orthokeratology on the progression of low to moderate myopia in Chinese children. BMC Ophthalmol. 2016;16:126.
Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, et al. Long-term efficacy of orthokeratology contact lens wear in controlling the progression of childhood myopia. Curr Eye Res. 2016;. doi:10.1080/02713683.2016.1221979.
Young A. Orthokeratology lens-related corneal ulcers in children a case series. Ophthalmology. 2004;111:590–5.
Hsiao CH, Yeung L, Ma DH, et al. Pediatric microbial keratitis in Taiwanese children: a review of hospital cases. Arch Ophthalmol. 2007;125:603–9.
Watt KG, Boneham GC, Swarbrick HA. Microbial keratitis in orthokeratology: the Australian experience. Clin Exp Optom. 2007;90:182–9.
Young AL, Leung KS, Tsim N, et al. Risk factors, microbiological profile, and treatment outcomes of pediatric microbial keratitis in a tertiary care hospital in Hong Kong. Am J Ophthalmol. 2013;156:1040–4.
Kim EC, Kim MS. Bilateral Acanthamoeba keratitis after orthokeratology. Cornea. 2010;29:680–2.
Lee J-E, Hahn TW, Oum BS, et al. Acanthamoeba keratitis related to orthokeratology. Int Ophthalmol. 2007;27:45–9.
Lee SJ, Jeong HJ, Lee JE, et al. Molecular characterization of Acanthamoeba isolated from amebic keratitis related to orthokeratology lens overnight wear. Korean J Parasitol. 2006;44:313–20.
Hsiao CH, Lin HC, Chen YF, et al. Infectious keratitis related to overnight orthokeratology. Cornea. 2005;24:783–8.
Hsiao CH, Yeh LK, Chao AN, et al. Pseudomonas aeruginosa corneal ulcer related to overnight orthokeratology. Chang Gung Med J. 2004;27:182–7.
Tseng CH, Fong CF, Chen WL, et al. Overnight orthokeratology-associated microbial keratitis. Cornea. 2005;24:778–82.
Wilhelmus KR. Acanthamoeba keratitis during orthokeratology. Cornea. 2005;24:864–6.
Arance-Gil A, Gutierrez-Ortega AR, Villa-Collar C, et al. Corneal cross-linking for Acanthamoeba keratitis in an orthokeratology patient after swimming in contaminated water. Cont Lens Anterior Eye. 2014;37:224–7.
Robertson DM, McCulley JP, Cavanagh HD. Severe acanthamoeba keratitis after overnight orthokeratology. Eye Contact Lens. 2007;33:121–3.
Sun X, Zhao H, Deng S, et al. Infectious keratitis related to orthokeratology. Ophthalmic Physiol Opt. 2006;26:133–6.
Tran T, Samarawickrama C, Petsoglou C, et al. Recent cluster of childhood microbial keratitis due to orthokeratology. Clin Exp Ophthalmol. 2014;42:793–4.
Chan TC, Li EY, Wong VW, et al. Orthokeratology-associated infectious keratitis in a tertiary care eye hospital in Hong Kong. Am J Ophthalmol. 2014;158:1130–5.
Shehadeh-Masha’our R, Segev F, Barequet IS, et al. Orthokeratology associated microbial keratitis. Eur J Ophthalmol. 2009;19:133–6.
Young AL, Leung AT, Cheung EY, et al. Orthokeratology lens-related Pseudomonas aeruginosa infectious keratitis. Cornea. 2003;22:265–6.
Chee EWL, Li L, Tan D. Orthokeratology-related infectious keratitis: a case series. Eye Contact Lens. 2007;33:261–3.
Lang J, Rah MJ. Adverse corneal events associated with corneal reshaping: a case series. Eye Contact Lens. 2004;30:231–3.
Lau LI, Wu CC, Lee SM, et al. Pseudomonas corneal ulcer related to overnight orthokeratology. Cornea. 2003;22:262–4.
Poole TR, Frangouli O, Ionides AC. Microbial keratitis following orthokeratology. Eye. 2003;17:440–1.
Hutchinson K, Apel A. Infectious keratitis in orthokeratology. Clin Exp Ophthalmol. 2002;30:49–51.
Priel A, Grinbaum A, Barequet IS. Severe Pseudomonas aeruginosa keratitis shortly after initiation of corneal refractive therapy. Eye Contact Lens. 2006;32:1–2.
Yepes N, Lee SB, Hill V, et al. Infectious keratitis after overnight orthokeratology in Canada. Cornea. 2005;24:857–60.
Araki-Sasaki K, Nishi I, Yonemura N, et al. Characteristics of Pseudomonas corneal infection related to orthokeratology. Cornea. 2005;24:861–3.
Wong VWY, Chi SCC, Lam DSC. Good visual outcome after prompt treatment of Acanthamoeba keratitis associated with overnight orthokeratology lens wear. Eye Contact Lens. 2007;33:329–31.
Teo L, Lim L, Tan DTH, et al. A survey of contact lens complications in Singapore. Eye Contact Lens. 2011;37:16–9.
Por YM, Mehta JS, Chua JLL, et al. Acanthamoeba keratitis associated with contact lens wear in Singapore. Am J Ophthalmol. 2009;148:7–12.
Hoddenbach JG, Boekhoorn SS, Wubbels R, et al. Clinical presentation and morbidity of contact lens-associated microbial keratitis: a retrospective study. Graefe’s Arch Clin Exp Ophthalmol. 2013;252:299–306.
Noureddin GS, Sasaki S, Butler AL, et al. Paediatric infectious keratitis at tertiary referral centres in Vancouver, Canada. Br J Ophthalmol. 2016;100:1714–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Kam, K.W., Yung, W., Li, G.K.H. et al. Infectious keratitis and orthokeratology lens use: a systematic review. Infection 45, 727–735 (2017). https://doi.org/10.1007/s15010-017-1023-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-017-1023-2