Abstract
Several studies have reported an association between CMV reactivation and a decreased incidence of relapse for AML after adult donor allogeneic hematopoietic cell transplantation (HCT). Limited data, however, are available on the impact of CMV reactivation on relapse after cord blood (CB) stem cell transplantation. The unique combination of higher incidence of CMV reactivation in the seropositive recipient and lower incidence of graft versus host disease (GvHD) in CB HCT permits a valuable design to analyze the impact of CMV reactivation. Data from 1684 patients transplanted with CB between 2003 and 2010 for AML and ALL were analyzed. The median time to CMV reactivation was 34 days (range: 2–287). CMV reactivation and positive CMV serology were associated with increased non-relapse mortality (NRM) among both AML and ALL CB recipients (reactivation, AML: relative risk (RR) 1.41 (1.07–1.85); ALL: 1.60 (1.14–2.23); Serology, AML: RR 1.39 (1.05–1.85), ALL: RR 1.61 (1.18–2.19)). For patients with ALL, but not those with AML, this yielded inferior overall survival (P<0.005). Risk of relapse was not influenced by CMV reactivation or positive CMV serostatus for either disease.
Similar content being viewed by others
Introduction
Since the early years of transplant, a positive CMV serology in the recipient and CMV reactivation have been associated with inferior outcomes after hematopoietic cell transplantation (HCT), reflecting an increase in non-relapse mortality (NRM).1 However, the development and adoption of effective monitoring of CMV either by PCR or pp65 antigenemia (pp65-AG) in the blood, and the use of preemptive antiviral therapy in the late 1990s/early 2000, has had a favorable impact on reducing the incidence of CMV disease and resulted in a decline in CMV-associated mortality.2
Recently, some studies have reported an association of positive CMV serology or early (before day 100) CMV reactivation with decreased incidence of relapse after HCT.3, 4, 5, 6, 7, 8 This protective effect against relapse appears restricted to AML, and, in some single-center studies, is associated with an improvement in overall survival (OS).3, 4, 5, 8 One hypothesis is that CMV reactivation results in expansion of natural killer (NK) cells with a mature phenotype (CD56dim, NKG2C+ and CD57+) that produce INFγ.9 Mature NK cell expansion is hypothesized to enhance antitumor responses, providing a biological rationale for reduced relapse occurring after CMV reactivation. T cells may be also involved as some γδ T cells recognize CMV peptides that are cross-reactive against leukemia cells.10 Consistent with this hypothesis, use of antithymocyte globulin or alemtuzumab (serotherapy) has been reported to abrogate the benefit of CMV reactivation on relapse.11, 12, 13, 14, 15 Published literature is conflicting, as several studies have failed to show a favorable association between CMV serology or reactivation and leukemia relapse or survival.4, 5, 7, 8, 14, 16, 17, 18
None of these prior studies focused on the impact of CMV-recipient serostatus or CMV reactivation in cord blood (CB) recipients. It is critical to look at CMV reactivation outcomes in CB HCT, specifically as CB HCT is unique. CB T cells are naive and there is no transfer of protective memory T cells;19 therefore, CB is considered inherently seronegative and CB transplant is associated with a high incidence of CMV reactivation in the seropositive recipient. CB HCT also tends to be associated with less acute and chronic GvHD, given the degree of mismatch, yet a powerful GvL effect remains.20, 21, 22
Given the disparity in the medical literature for the influence of CMV on leukemia relapse, and lack of sufficient CB data, the primary aim of this study was to use the large multi-institutional database of the Center for International Blood and Marrow Transplant Research (CIBMTR) to more completely analyze the impact of CB-recipient serostatus and early CMV reactivation primarily on leukemia relapse; secondary outcomes included the impact on OS, and NRM, in the era of preemptive therapy.
Patients and methods
Data source
The CIBMTR is a working group of more than 500 transplant centers worldwide that provide detailed patient, disease, transplant characteristics and outcomes of consecutive transplantations. Data are collected at the Statistical Center at the Medical College of Wisconsin or at the Data-Coordinating Center of the National Marrow Donor Program, where computerized checks for discrepancies, physicians' review of submitted data and on-site audits of participating centers ensure data quality. The CIBMTR collects both Transplant Essential Data and Comprehensive Report Form data before transplantation, 100 days (D100) and 6 months after transplantation, and annually thereafter. All subjects whose data were included in this study provided institutional review board-approved consent to participate in the CIBMTR Research Database and have their data included in observational research studies. The Institutional Review Boards of the Medical College of Wisconsin and the National Marrow Donor Program approved this study.
Data collection and criteria for selection
All patients reported to the CIBMTR, and receiving first CB HCT between 2003 and 2010, for AML and ALL using any conditioning regimen, were included. Patients with only former National Marrow Donor Program forms were excluded, given lack of data on CMV reactivation (n=298). Patients from centers with less than 30% completeness of follow-up index were also excluded (n=64). Other exclusion criteria were as follows: no signed informed consent (n=35), lack of day 100 follow-up forms capturing CMV reactivation data (n=70), CMV serostatus match missing and death before transplantation (n=4). A total of 1684 CB recipients with AML and ALL are included in this analysis. The database was locked on 31 August 2013. The completeness index was very good, 99% at 1 year and 97% at 5 years of follow-up.
Data regarding CMV reactivation, surveillance and treatment
The CIMBTR day 100 follow-up forms collect information on the date of onset of CMV reactivation and the site where CMV was identified. No information is collected regarding diagnostic method, level of virus detected or on therapy provided.
Study design and statistical analysis
Patients with AML (n=925) and ALL (n=759) were analyzed separately. For univariate outcomes and the initial multivariable analysis, patients were categorized as D−/R+ or D−/R−, as CB is considered inherently CMV-seronegative. A second multivariable analysis was performed based on the presence or absence of CMV reactivation post transplant as a time-dependent covariate. Patients receiving single (n=944) and double (n=740) cord were analyzed together as randomized trials demonstrate no difference in transplant outcomes of relapse and survival with single versus double cord transplant.23
Variables included time to CMV reactivation, CMV (D/R) serology, recipient age, gender, race, Karnofsky score at HCT, time from diagnosis to HCT, disease risk category based on ASBMT RFI 2014 classification,24 year of transplant (2003–2006 versus 2007–2010), conditioning intensity, use of total body irradiation, use of serotherapy, GvHD prophylaxis regimen and development of acute and/or chronic GvHD post transplant. For multivariable analyses, the main effect variable was either D/R CMV serology (D–/R– as reference versus D–/R+) or CMV reactivation as a time-dependent covariate (yes versus no). Additional variables analyzed in the models included age (⩽10 years versus 10–30 versus >30 years), disease risk category, conditioning intensity, serotherapy (Yes versus No), GvHD prophylaxis (Tacrolimus/Cyclosporine+Methotrexate±Others versus Tacrolimus/Cyclosporine+Others versus Others) and acute GvHD (aGvHD) occurring before CMV reactivation as a time-dependent covariate.
Patient, disease and transplant-related factors were compared between groups using the Pearson X2-test for discrete variables and the Kruskal–Wallis test for continuous variables. Probabilities of disease-free survival (DFS) and OS were calculated using the Kaplan–Meier estimator. Values for other end points were generated using cumulative incidence estimates to account for competing risks. OS was defined as the time to death from any cause with surviving patients censored at time of last follow-up. DFS was defined as the time to relapse or death from any cause. NRM was defined as death without evidence of disease with relapse as a competing risk. Relapse was recurrence/progression of acute leukemia with death as the competing risk. For aGvHD grades II–IV and chronic GvHD (cGvHD) of any severity, death was the competing risk and patients were censored at time of relapse. In both multivariable analyses of CMV serology and CMV reactivation, the proportional hazard assumption was examined. If violated, it was included as a time-dependent covariate. A stepwise selection procedure was used. Interactions between the main effect and significant covariates were examined. A P-value <0.05 was considered significant. SAS v9.3 (Cary, NC, USA) was used for statistical analysis.
Results
Distribution of CMV serology and CMV reactivation
Table 1 provides basic information on the patients included in the analysis. A total of 1011 CB recipients were CMV-serostatus-positive, with 606 (66%) in the AML cohort and 405 (53%) in the ALL cohort reflecting the older median age for patients with AML [(ALL, median 12 (<1–68) years versus AML, 28 (<1–79) years; P<0.001). The median time to CMV reactivation for the entire cohort was 34 days (range, 2–287) after HCT. It was similar for the AML cohort regardless of the D/R serostatus; however, for ALL patients, the 4% of D−/R− who developed reactivation occurred significantly later after transplant. Nearly all CMV reactivations occurred in the first 3 months after transplant.
Relapse
For patients with AML, relapse by 1 year occurred in 27% (95% confidence interval (CI), 23–31%) of seropositive recipients and 26% (95% CI, 21–31%) of seronegative recipients (P 0.77; Table 2 and Figure 1a). Relapse at 1 year was slightly lower in patients with ALL, but there was no effect of recipient CMV serostatus (D−/R+, 20% (95% CI, 16–24%); D−/R−, 18% (95% CI, 14–22%), P=0.49; Table 2 and Figure 1b).
In multivariable analysis adjusted for other known risk factors for relapse, CMV-seropositive recipients with AML had a higher risk of relapse (RR 1.39, P=0.022) compared with seronegative recipients (Table 3). For ALL patients, the risk of relapse was slightly higher for the CMV-seropositive recipients, albeit not statistically significantly (Table 4). CMV reactivation as a time-dependent event did not favorably have an impact on relapse for patients with either AML or ALL [(AML: RR 0.8 (95% CI, 0.62–1.04), P=0.097; ALL: RR 1.01 (95% CI, 0.70–1.46), P=0.95). As expected, AML and ALL patients with high-risk disease or recipients of reduced intensity conditioning had a higher risk of relapse. ALL patients developing acute GvHD were less likely to have disease relapse (RR of 0.7 (95% CI, 0.52–0.94), P<0.02).
GvHD
Acute GvHD grades II–IV by day 100 were similar regardless of disease indication for transplant or CMV-recipient serostatus (AML D−/R+: 43% (95% CI, 39–47%); AML D−/R−: 40% (95% CI, 34–45%); ALL D−/R+: 39% (95% CI, 34–44%); ALL D−/R−: 40% (95% CI, 35–45%)). cGvHD by 3 years did not differ (AML D−/R+: 30% (95% CI, 26–33%); AML D−/R−: 34% (95% CI, 28– 39%); ALL D−/R+: 31% (95% CI, 27–36%); ALL D−/R−: 35% (95% CI, 30–40%)).
In multivariable analysis, positive CMV serology had no impact on the incidence of aGvHD or cGvHD in AML or ALL. CMV reactivation occurring before the onset of aGvHD demonstrated a slightly increased but not statistically different risk of aGvHD (AML: RR 1.31 (95% CI, 0.96–1.79), P=0.083; ALL: RR 1.38 (95% CI, 0.96–1.98), P=0.084). CMV reactivation had no impact on the development of cGvHD when adjusted for other factors.
Other factors having an impact on development of aGvHD grades II–IV included the use of serotherapy for either disease; although for patients with AML, this effect became attenuated after 1 month post transplant (Table 3). There was also a decreased risk of aGvHD for patients with AML receiving a reduced intensity conditioning regimen, but this only occurred in the first month from transplant. As expected, cGvHD was decreased in patients receiving serotherapy, regardless of underlying malignancy (Table 3). In addition, for patients with ALL, older age and prior aGvHD increased the risk for development of cGvHD (Table 4).
Non-relapse mortality
Recipient CMV serology and CMV reactivation were both associated with increased NRM. In univariate analysis, patients with AML who were D−/R+ had an increased risk of NRM at 1 and 3 years compared with D−/R− pairs (1 year, D−/R+: 26% (95% CI, 23–30%) versus D−/R−: 18% (95% CI, 14–22%), P=0.003; Table 2 and Figure 2a). This was similar in patients with ALL as well (Table 2 and Figure 2b). This effect remained significant for both AML and ALL when adjusted for other factors in multivariable analysis (Table 3 and Table 4). Similarly, CMV reactivation increased NRM in multivariable analysis such that patients with AML had a 1.4-fold greater risk (95% CI, 1.07–1.85; P <0.02) and those with ALL were about 1.6 times as likely to die of NRM (95% CI, 1.14–2.23; P>0.007).
For patients with AML, older age was also associated with increased NRM. For ALL, increased age, use of serotherapy and the development of aGvHD were all associated with increased NRM.
Survival
As shown in Table 2, both DFS and OS were inferior for patients with acute leukemia who were CMV seropositive (Figure 3a, b). When adjusting for other factors, this effect was no longer significant in AML patients (Table 3). However, for ALL patients, CMV-seropositive recipients had a higher risk of death from any cause (Table 4). Use of serotherapy had an adverse impact on DFS. For ALL patients not receiving serotherapy, DFS was similar to CMV-seronegative recipients; however, the use of serotherapy was associated with significantly inferior DFS in CMV-seropositive recipients.
When adjusting for CMV reactivation, there was no impact on DFS or OS for patients with AML (DFS, RR 1.05 (95% CI, 0.87–1.27), P=0.61; OS: RR 1.07 (95% CI, 0.88–1.30), P=0.48); however, patients with ALL and a CMV reactivation had inferior DFS (RR 1.31 (95% CI, 1.02–1.67), P=0.03) and higher risk of death (RR 1.44 (95% CI, 1.12–1.84), P<0.005).
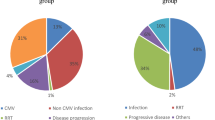
Regardless of type of acute leukemia, patients with more advanced disease and older age had a higher risk of death and impaired DFS. For patients with ALL, patients receiving reduced intensity conditioning had inferior DFS and OS. Specific causes of death for all patients by the D/R serostatus are shown in Table 5.
Discussion
Several studies have examined the impact of CMV reactivation specifically in AML after HCT. However, none of these studies examined outcomes in the CB setting. This CIBMTR analysis of 1684 patients was specifically designed to look at the influence of CMV serology and early CMV reactivation on relapse and survival following CB HCT for either AML or ALL. Our data suggest that CMV reactivation does not prevent relapse of AML or ALL in patients receiving CB HCT. Furthermore, our study highlights a persistent negative impact for CB recipients who are CMV seropositive and for patients experiencing CMV reactivation after CB HCT.
The lack of benefit of CMV seropositivity and CMV reactivation seen in our analysis contrasts with other studies that have described a protective effect for positive CMV serology or CMV reactivation in preventing AML relapse.4, 5, 7, 8, 17, 25 However, other studies have reported a lack of benefit from positive CMV serology and a negative effect of early CMV reactivation with regards to the risk of leukemia relapse.18, 26 A recent analysis from the European Blood and Marrow Transplant Group demonstrated a higher risk of leukemia relapse and poorer OS associated with positive CMV serology.17, 27
CMV reactivation and positive CMV serology (D−/R+ versus D−/R−) increased NRM in our cohort. Similar to the European Blood and Marrow Transplant Group study, we found that CMV-seropositive recipients were more likely to have infection reported as a primary cause of death compared with CMV-seronegative CB recipients (R+, 21%; R−, 14%). Notably, there was a roughly similar increase in recurrence/persistent disease as the primary cause of death in CMV-seronegative recipients (R+, 37%; R−, 48%). Despite these findings, there was no protection from relapse seen in either univariate or multivariable analysis. Since an indirect effect of CMV serology on the risk of infections with other pathogens has been reported, it is possible that any small decrease in relapse risk is counterbalanced by an increase in fatal infections.28
For patients with ALL who received either ATG or alemtuzumab serotherapy, CMV reactivation and a positive CMV-recipient serology was detrimental to LFS. Influence of serotherapy on LFS may be explained by the higher likelihood of CMV reactivation in these patients.12 CMV-positive serology (P=0.0007) and CMV reactivation (P=0.0042) had a negative impact on OS in ALL. This negative impact in ALL is not surprising, given the negative impact on both NRM and LFS in ALL CB recipients. Notably, CMV status (positive serology or CMV reactivation) had no impact on LFS or OS in AML. It is interesting that, despite its negative impact on NRM, the CMV status did not have a negative impact on OS in AML CB. The differences in outcomes between AML and ALL cannot be solely attributed to disease category as non-disease-related factors, such as age and prior chemotherapy, may have had a role as well. Within the ALL group, predominantly younger patients, recipient CMV seropositivity was a stronger predictor of NRM compared with AML patients, which may account for the lack of impact of the CMV status on LFS and OS for AML patients.
Although multicenter registry studies such as ours have the advantage of a large sample size, the caveat is the lack of detailed information. Data with regards to the viral monitoring test used to diagnose CMV reactivation, frequency of testing or preemptive versus prophylactic policies applied by each center were not available. In addition, information regarding antiviral therapy itself, trigger for initiation, timing of initiation and total duration of treatment for CMV reactivation were not captured. Moreover, CMV reactivation may be under-reported in multicenter registry studies. This is likely explained by a trend for reporting to registries only CMV reactivations that are considered to have a clinical importance because of their level or duration. The lack of detailed data may introduce bias diluting the effect of CMV serostatus and CMV reactivation; however, the large number of patients and centers should counteract this bias somewhat.
The implications of our CB study showing the persistent negative impact of the CMV serostatus and reactivation on NRM, despite the existence of effective antiviral pharmacotherapy, are far-reaching. Although antiviral pharmacotherapy, diligent surveillance and early preemptive antiviral therapy have significantly reduced the progression to CMV disease and mortality observed before this era, there remains significant limitations to current therapy including myelosuppression (ganciclovir) and electrolyte imbalances/renal impairment (foscarnet). Our data justify the need for development of novel antiviral drugs, with superior efficacy and toxicity profiles.29, 30 For example, a prophylactic rather than preemptive approach may lead to superior outcomes in CB stem cell transplants. Some centers have reported using IV ganciclovir during conditioning regimen (days −8 to −2) and high-dose valacyclovir prophylaxis (2 gm every 8 h) in the post-transplant setting in their CMV-seropositive CB recipients. An alternative approach to antiviral pharmacotherapy, especially in CB HCT, is adoptive cellular immunotherapy for CMV and other viral diseases.31, 32 Adoptive cellular immunotherapy, after having amassed an excellent record for efficacy and safety, is advancing from therapy of refractory disease to prophylaxis. Boosting immune reconstitution and antiviral immunity post (CB) HCT rather than focusing on pharmacotherapy has the potential to be cost effective.33, 34, 35 Regardless of the approach, our data confirm that there is a great scope for further improving the management of CMV after CB HCT.
In conclusion, in this only multicenter data set of CB recipients, CMV reactivation is associated with decreased DFS and OS in ALL but not in AML. Positive recipient CMV serology and CMV reactivation continue to contribute to increased NRM even in the era of preemptive treatment. If CMV reactivation has an effect on decreasing AML relapse, our study suggests that the benefit is small and likely balanced by the increased NRM, particularly in the setting of CB HCT.
References
Winston DJ, Gale RP . Prevention and treatment of cytomegalovirus infection and disease after bone marrow transplantation in the 1990s. Bone Marrow Transplant 1991; 8: 7–11.
Ljungman P, Hakki M, Boeckh M . Cytomegalovirus in hematopoietic stem cell transplant recipients. Hematol Oncol Clin North Am 2011; 25: 151–169.
Behrendt CE, Rosenthal J, Bolotin E, Nakamura R, Zaia J, Forman SJ . Donor and recipient CMV serostatus and outcome of pediatric allogeneic HSCT for acute leukemia in the era of CMV-preemptive therapy. Biol Blood Marrow Transplant 2009; 15: 54–60.
Elmaagacli AH, Steckel NK, Koldehoff M, Hegerfeldt Y, Trenschel R, Ditschkowski M et al. Early human cytomegalovirus replication after transplantation is associated with a decreased relapse risk: evidence for a putative virus-versus-leukemia effect in acute myeloid leukemia patients. Blood 2011; 118: 1402–1412.
Green ML, Leisenring WM, Xie H, Walter RB, Mielcarek M, Sandmaier BM et al. CMV reactivation after allogeneic HCT and relapse risk: evidence for early protection in acute myeloid leukemia. Blood 2013; 122: 1316–1324.
Ito S, Pophali P, Co W, Koklanaris EK, Superata J, Fahle GA et al. CMV reactivation is associated with a lower incidence of relapse after allo-SCT for CML. Bone Marrow Transplant 2013; 48: 1313–1316.
Jang JE, Kim SJ, Cheong JW, Hyun SY, Kim YD, Kim YR et al. Early CMV replication and subsequent chronic GVHD have a significant anti-leukemic effect after allogeneic HSCT in acute myeloid leukemia. Ann Hematol 2014; 94: 275–282.
Manjappa S, Bhamidipati PK, Stokerl-Goldstein KE, DiPersio JF, Uy GL, Westervelt P et al. Protective effect of cytomegalovirus reactivation on relapse after allogeneic hematopoietic cell transplantation in acute myeloid leukemia patients is influenced by conditioning regimen. Biol Blood Marrow Transplant 2014; 20: 46–52.
Foley B, Cooley S, Verneris MR, Pitt M, Curtsinger J, Luo X et al. Cytomegalovirus reactivation after allogeneic transplantation promotes a lasting increase in educated NKG2C+ natural killer cells with potent function. Blood 2012; 119: 2665–2674.
Scheper W, van Dorp S, Kersting S, Pietersma F, Lindemans C, Hol S et al. gammadeltaT cells elicited by CMV reactivation after allo-SCT cross-recognize CMV and leukemia. Leukemia 2013; 27: 1328–1338.
Nakamura R, Battiwalla M, Solomon S, Follmann D, Chakrabarti S, Cortez K et al. Persisting posttransplantation cytomegalovirus antigenemia correlates with poor lymphocyte proliferation to cytomegalovirus antigen and predicts for increased late relapse and treatment failure. Biol Blood Marrow Transplant 2004; 10: 49–57.
Soiffer RJ, Lerademacher J, Ho V, Kan F, Artz A, Champlin RE et al. Impact of immune modulation with anti-T-cell antibodies on the outcome of reduced-intensity allogeneic hematopoietic stem cell transplantation for hematologic malignancies. Blood 2011; 117: 6963–6970.
Admiraal R, van Kesteren C, Jol-van der Zijde CM, Lankester AC, Bierings MB, Egberts TCG et al. Association between anti-thymocyte globulin exposure and CD4+ immune reconstitution in paediatric haemopoietic cell transplantation: a multicentre, retrospective pharmacodynamic cohort analysis. Lancet Haematol 2015; 2: e194–e203.
Thomson KJ, Mackinnon S, Peggs KS . CMV-specific cellular therapy for acute myeloid leukemia? Blood 2012; 119: 1088–1090 author reply 1090-1081.
Sellar RS, Arce Vargas F, Henry JY, Verfuerth S, Charrot S, Beaton B et al. CMV promotes recipient T-cell immunity following reduced intensity T-cell depleted HSCT significantly modulating chimerism status. Blood 2014; 125: 731–739.
Jeljeli M, Guerin-El Khourouj V, Porcher R, Fahd M, Leveille S, Yakouben K et al. Relationship between cytomegalovirus (CMV) reactivation, CMV-driven immunity, overall immune recovery and graft-versus-leukaemia effect in children. Br J Haematol 2014; 166: 229–239.
Ljungman P, Brand R, Hoek J, de la Camara R, Cordonnier C, Einsele H et al. Donor cytomegalovirus status influences the outcome of allogeneic stem cell transplant: a study by the European group for blood and marrow transplantation. Clin Infect Dis 2014; 59: 473–481.
Travi G, Pergam SA, Xie H, Boeckh MJ . Donor CMV serostatus not predictive of relapse in D-/R- pediatric HCT. Biol Blood Marrow Transplant 2009; 15: 758–760.
McGoldrick SM, Bleakley ME, Guerrero A, Turtle CJ, Yamamoto TN, Pereira SE et al. Cytomegalovirus-specific T cells are primed early after cord blood transplant but fail to control virus in vivo. Blood 2013; 121: 2796–2803.
Eapen M, Rubinstein P, Zhang MJ, Stevens C, Kurtzberg J, Scaradavou A et al. Outcomes of transplantation of unrelated donor umbilical cord blood and bone marrow in children with acute leukaemia: a comparison study. Lancet 2007; 369: 1947–1954.
Kumar P, Defor TE, Brunstein C, Barker JN, Wagner JE, Weisdorf DJ et al. Allogeneic hematopoietic stem cell transplantation in adult acute lymphocytic leukemia: impact of donor source on survival. Biol Blood Marrow Transplant 2008; 14: 1394–1400.
Willemze R, Rodrigues CA, Labopin M, Sanz G, Michel G, Socie G et al. KIR-ligand incompatibility in the graft-versus-host direction improves outcomes after umbilical cord blood transplantation for acute leukemia. Leukemia 2009; 23: 492–500.
Wagner JE, Eapen M, Carter S, Wang Y, Schultz KR, Wall DA et al. One-unit versus two-unit cord-blood transplantation for hematologic cancers. N Engl J Med 2014; 371: 1685–1694.
Armand P, Kim HT, Logan BR, Wang Z, Alyea EP, Kalaycio ME et al. Validation and refinement of the Disease Risk Index for allogeneic stem cell transplantation. Blood 2014; 123: 3664–3671.
Lonnqvist B, Ringden O, Ljungman P, Wahren B, Gahrton G . Reduced risk of recurrent leukaemia in bone marrow transplant recipients after cytomegalovirus infection. Br J Haematol 1986; 63: 671–679.
Cantoni N, Hirsch HH, Khanna N, Gerull S, Buser A, Bucher C et al. Evidence for a bidirectional relationship between cytomegalovirus replication and acute graft-versus-host disease. Biol Blood Marrow Transplant 2010; 16: 1309–1314.
Schmidt-Hieber M, Labopin M, Beelen D, Volin L, Ehninger G, Finke J et al. CMV serostatus still has an important prognostic impact in de novo acute leukemia patients after allogeneic stem cell transplantation: a report from the Acute Leukemia Working Party of EBMT. Blood 2013; 122: 3359–3364.
Nichols WG, Corey L, Gooley T, Davis C, Boeckh M . High risk of death due to bacterial and fungal infection among cytomegalovirus (CMV)-seronegative recipients of stem cell transplants from seropositive donors: evidence for indirect effects of primary CMV infection. J Infect Dis 2002; 185: 273–282.
Ariza-Heredia EJ, Nesher L, Chemaly RF . Cytomegalovirus diseases after hematopoietic stem cell transplantation: a mini-review. Cancer Lett 2014; 342: 1–8.
Marty FM, Winston DJ, Rowley SD, Vance E, Papanicolaou GA, Mullane KM et al. CMX001 to prevent cytomegalovirus disease in hematopoietic-cell transplantation. N Engl J Med 2013; 369: 1227–1236.
Blyth E, Clancy L, Simms R, Ma CK, Burgess J, Deo S et al. Donor-derived CMV-specific T cells reduce the requirement for CMV-directed pharmacotherapy after allogeneic stem cell transplantation. Blood 2013; 121: 3745–3758.
Leen AM, Bollard CM, Mendizabal AM, Shpall EJ, Szabolcs P, Antin JH et al. Multicenter study of banked third-party virus-specific T cells to treat severe viral infections after hematopoietic stem cell transplantation. Blood 2013; 121: 5113–5123.
Gea-Banacloche JC . Antiviral cell therapy: is this the future? Blood 2013; 121: 5108–5109.
Heslop HE . Pharmacotherapy versus T lymphocytes for CMV. Blood 2013; 121: 3544–3545.
Jain NA, Lu K, Ito S, Muranski P, Hourigan CS, Haggerty J et al. The clinical and financial burden of pre-emptive management of cytomegalovirus disease after allogeneic stem cell transplantation-implications for preventative treatment approaches. Cytotherapy 2014; 16: 927–933.
Acknowledgements
The CIBMTR is supported by Public Health Service Grant/Cooperative Agreement 5U24-CA076518 from the National Cancer Institute (NCI), the National Heart, Lung and Blood Institute (NHLBI) and the National Institute of Allergy and Infectious Diseases (NIAID); a Grant/Cooperative Agreement 5U10HL069294 from NHLBI and NCI; a contract HHSH250201200016C with Health Resources and Services Administration (HRSA/DHHS); two Grants N00014-13-1-0039 and N00014-14-1-0028 from the Office of Naval Research; and grants from Alexion; *Amgen Inc.; Anonymous donation to the Medical College of Wisconsin; Be the Match Foundation; *Bristol Myers Squibb Oncology; *Celgene Corporation; *Chimerix Inc.; Fred Hutchinson Cancer Research Center; Gamida Cell Ltd.; Genentech Inc.; Genzyme Corporation; *Gilead Sciences Inc.; Health Research Inc. Roswell Park Cancer Institute; HistoGenetics Inc.; Incyte Corporation; *Jazz Pharmaceuticals Inc.; Jeff Gordon Children’s Foundation; The Leukemia & Lymphoma Society; The Medical College of Wisconsin; Merck & Co Inc.; Mesoblast; *Millennium: The Takeda Oncology Co.; *Miltenyi Biotec Inc.; National Marrow Donor Program; Neovii Biotech NA Inc.; Novartis Pharmaceuticals Corporation; Onyx Pharmaceuticals; Optum Healthcare Solutions Inc.; Otsuka America Pharmaceutical Inc.; Otsuka Pharmaceutical Co, Ltd.—Japan; Oxford Immunotec; Perkin Elmer Inc.; Pharmacyclics; *Sanofi US; Seattle Genetics; Sigma-Tau Pharmaceuticals; *Spectrum Pharmaceuticals Inc.; St. Baldrick’s Foundation; *Sunesis Pharmaceuticals Inc.; Swedish Orphan Biovitrum Inc.; Telomere Diagnostics Inc.; TerumoBCT; Therakos Inc.; University of Minnesota; and *Wellpoint Inc. Corporate Members have been denoted by the ‘*’ symbol.
Disclaimer
The views expressed in this article do not reflect the official policy or position of the National Institute of Health, the Department of the Navy, the Department of Defense, Health Resources and Services Administration (HRSA) or any other agency of the US Government.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ramanathan, M., Teira, P., Battiwalla, M. et al. Impact of early CMV reactivation in cord blood stem cell recipients in the current era. Bone Marrow Transplant 51, 1113–1120 (2016). https://doi.org/10.1038/bmt.2016.89
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2016.89
- Springer Nature Limited
This article is cited by
-
CMV Infection Post Allogeneic Hematopoietic Stem Cell Transplantation in a Resource Limited Country
Indian Journal of Hematology and Blood Transfusion (2023)
-
Reduced leukemia relapse through cytomegalovirus reactivation in killer cell immunoglobulin-like receptor-ligand-mismatched cord blood transplantation
Bone Marrow Transplantation (2021)
-
Effects of HLA mismatch on cytomegalovirus reactivation in cord blood transplantation
Bone Marrow Transplantation (2019)
-
Intrabone transplant provides full stemness of cord blood stem cells with fast hematopoietic recovery and low GVHD rate: results from a prospective study
Bone Marrow Transplantation (2019)
-
Cytomegalovirus infection is associated with AML relapse after allo-HSCT: a meta-analysis of observational studies
Annals of Hematology (2019)