Abstract
To gain insight into the natural history of cytomegalovirus (CMV) infection following unrelated cord blood transplantation (UCBT) in seropositive patients, we analyzed the data of 349 seropositive patients who received UCBT in Korea between 2000 and 2011. CMV reactivation occurred in 49 % (171/349) of the CMV-seropositive transplant recipients at a median of 31 days post UCBT. One hundred sixty-four out of 171 patients (96 %) received preemptive therapy. The median duration of CMV reactivation was 29 days. In multivariate analysis, weight >22 kg, use of total body irradiation, use of pre-transplant antithymocyte globulin, graft-versus-host disease (GVHD) prophylaxis with mycophenolate mofetil, and presence of grade II–IV acute GVHD were independent predictors of CMV reactivation. CMV reactivation did not impact transplantation-related mortality (TRM), leukemia relapse, or survival. CMV disease was diagnosed in 62 patients (17.8 %) at a median 55 days after UCBT. Longer duration of CMV reactivation was the only risk factor for progression to CMV disease (p = 0.01). CMV disease resulted in higher TRM (56.0 vs. 31.4 %, p < 0.01) and lower survival (36.1 vs. 55.1 %, p = 0.02).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Posttransplantation cytomegalovirus (CMV) infection is associated with recipient pre-transplantation CMV status [1]. Unlike peripheral blood (PB) or bone marrow (BM) transplantation, where CMV can be reactivated from either the donor or recipient, pathogenic issues of CMV after cord blood (CB) transplantation (CBT) occur almost exclusively from reactivation of endogenous virus in the host [2]. This is because CMV infection in newborns is rare, and infected CB units are not generally banked or used clinically [1].
CB grafts are naïve and their functional recovery may be impaired, more permissive of viral reactivation and less able to control viral replication [3, 4]. Host damage of CMV can lead to life-threatening invasive disease, particularly in high-risk seropositive recipients [5]. Several studies have indicated that CMV-seropositive patients are at a substantial disadvantage after hematopoietic stem cell transplantation (HSCT) [6, 7], but the use of different prevention methods and the inclusion of low-risk seronegative recipients limit comparisons [8, 9]. The increased mortality and morbidity of CMV-seropositive recipients is probably due to both direct and indirect effects of CMV reactivation as well as toxic effects of antiviral agents used for prophylaxis or treatment of CMV infection.
To date, little is known about CMV reactivation in unrelated cord blood transplantation (UCBT) recipients in high prevalence CMV populations such as Korea, where over 90 % of HSCT patients are CMV-seropositive before transplantation [10]. To gain insight of CMV reactivation following UCBT in seropositive patients, we analyzed the clinical features of CMV reactivation and its impact on CBT-associated outcomes.
Materials and methods
Patients
The data of 381 Korean recipients of UCBT between 2000 and 2011 were collected. Three hundred forty-nine of these patients (91.6 %) were CMV-seropositive. In this study, we reviewed the clinical data of these 349 seropositive patients who received UCBT in 19 medical centers in Korea. Details of the CBT in the various institutions were registered in the Korean Cord Blood Transplantation Registry, and the data were verified by comparing the reports with the primary data sources. This study was approved by the Institutional Review Board of Hanyang University Medical Center. Informed consent was obtained from the patients and/or guardians before CBT.
CMV prophylaxis
The selection of CMV prophylaxis strategies was at the discretion of each center. The dose and duration of antiviral prophylaxis was also influenced by the patient herpes simplex and varicella zoster virus serostatus. The majority (n = 295, 84.5 %) of patients received antiviral prophylaxis with acyclovir (ACV). Frequently used ACV infusion schedules were as follows: (1) 600 mg/m2 every 12 h (n = 143), (2) 500 mg/m2 every 8 h (n = 107), or (3) 250 mg/m2 every 8 h for 4 weeks or 100 days after UCBT (n = 45).
Definitions
CMV reactivation was defined as either CMV antigenemia (≥1 CMV pp65 positive cells / 50,000) or DNAemia (≥500 copies by quantitative polymerase chain reaction (PCR)) [11]. CMV disease was defined as end-organ disease, such as pneumonia, gastrointestinal disease, hepatitis, etc., with a documented CMV etiology [11, 12]. After clearance of CMV for >30 days, any subsequent episode of CMV reactivation was considered a recurrence [11]. Preemptive therapy was initiated immediately after CMV reactivation was detected. The surveillance schedule and antiviral agent were chosen at the discretion of each center.
Most of the patients underwent once- or twice-weekly screening for CMV reactivation by PCR and/or antigenemia testing for the first month, then every 1–4 weeks until the end of treatment with immunosuppressive agents or the resolution of graft-versus-host disease (GVHD). In Korea, CMV PCR has been routinely used for CMV infection screening before neutrophil engraftment since 2005. In this study, 127 out of 349 patients underwent UCBT before 2005 and 104 patients underwent CMV antigenemia assay only. Since 2005, CMV surveillance analysis has generally been performed by a combination of PCR and/or antigenemia assay. CMV surveillance analysis was performed by PCR before neutrophil engraftment; after engraftment, it was performed by antigenemia assay and/or PCR.
Neutrophil engraftment was defined as the first of three consecutive days with an absolute neutrophil count >0.5 × 109/L. Reduced-intensity conditioning (RIC) was defined according to the published criteria [13]. Pre-engraftment syndrome (PES) was defined as unexplained fever >38.3 °C not associated with documented infection and/or unexplained erythematous skin rash resembling that of acute GVHD, with either the fever or the rash occurring before or at the time of neutrophil recovery [14]. Acute and chronic GVHD was diagnosed and graded according to the previously published criteria [15, 16]. Overall survival (OS) was defined as the time between the date of transplantation and the date of death from any cause or, for survivors, the date of last follow-up. Transplantation-related mortality (TRM) was defined as any death not the result of relapse, progression, or persistence of the underlying disease.
Statistical methods
Categorical variables were compared using the chi-square test, and continuous variables using the Mann-Whitney U test. The cumulative incidences of neutrophil engraftment, GVHD, relapse, and TRM were calculated and compared by Gray’s method. For neutrophil engraftment, the competing risks were autologous recovery, infusion of a backup graft, or death. GF and death were the competing events for GVHD, whereas relapse was the competing event for TRM. OS was the time between day 0 of CB infusion and death due to any cause, and living patients were censored at last follow-up. Survival was calculated by the Kaplan-Meier method, and differences in survival rates as a function of CMV infection were determined using the log-rank test. A Cox proportional hazard model was used to identify the independent effects of potential predictors of CMV reactivation and disease, treating acute GVHD as a time-dependent covariate. Factors significant at the 0.1 level in univariate analysis were considered for multivariate analyses using backwards elimination. Two-sided p values less than 0.05 were considered significant. All analyses were conducted with SPSS version 18.0 software and R version 2.10.1
Results
The characteristics of patients and transplants are listed in Table 1. Median follow-up after UCBT was 27.2 months (range, 1.0–149.6 months). The median numbers of total nucleated cells (TNCs) and CD34+ cells were 5.02 × 107/kg (range, 0.27–104.40) and 2.04 × 105/kg (range, 0.08–61.62), respectively. Approximately 46 % of patients received cord blood units with ≥2 HLA mismatches.
Clinical features of CMV reactivation
Of the 349 CMV-seropositive transplant recipients, CMV reactivation occurred in 171 patients (49.0 %) at a median of 31 days post UCBT (range, 3–163 days). The median duration of CMV positivity was 29 days (range, 4–246 days). CMV reactivation before neutrophil engraftment occurred in 16 patients (4.6 %). Recurrent CMV reactivation was seen in 71 patients (20.3 %). A total of 271 patients were followed up for more than 100 days after CBT. Of these, 29 patients (10.7 %) experienced CMV reactivation more than 100 days after CBT, including 24 in whom reactivation had already occurred once before. CMV reactivation was diagnosed on the basis of detecting pp65 antigen in 150 patients and from the results of PCR in 21 patients. Of the 171 patients experiencing CMV reactivation, 162 (94.7 %) received preemptive therapy using gangiclovir (GCV, n = 152) or foscarnet (n = 10).
Risk factors for CMV reactivation
A number of variables were studied to identify possible risk factors for CMV reactivation (Table 2). They were age, gender, body weight, disease risk, HLA match status, use of pre-transplant ATG, preparative regimen, type of GVHD prophylaxis, infused cell doses including TNCs, CD3+ cells, and CD34+ cells, achievement of engraftment, time to engraftment, presence of PES, presence of grade II–IV acute GVHD, and type of treatment for acute GVHD. In univariate analysis, the significant risk factors identified were age >6.9 years, weight >22 kg, use of total body irradiation (TBI), pre-transplant ATG, GVHD prophylaxis with mycophenolate mofetil (MMF), presence of PES, and grade II–IV acute GVHD. In multivariate analysis, weight >22 kg, TBI, pre-transplant ATG, GVHD prophylaxis with MMF, and presence of grade II–IV acute GVHD remained independent predictors of CMV reactivation.
Impact of CMV reactivation on transplantation-related outcomes
Engraftment data were available for 168 out of the 171 patients with CMV reactivation. Neutrophil engraftment occurred in 153 of these 168 patients, and the median time to engraftment was 18 days (range, 7–58 days). The cumulative incidence of neutrophil engraftment at 60 days after UCBT was significantly higher in patients experiencing CMV reactivation than in those not experiencing reactivation (90.6 vs. 77.0 %, p < 0.01) (Fig. 1a). However, when we analyzed the engraftment results of each CMV reactivation diagnostic method separately, there was no significant difference in the cumulative incidence of neutrophil engraftment between patients with CMV reactivation defined by PCR and those without CMV reactivation (90.3 vs. 77.0 %, p = 0.62), while patients with CMV reactivation defined by pp65 antigenemia had a significantly higher engraftment rate compared to patients without CMV reactivation (91.6 vs. 77.0 %, p < 0.01) (Fig. 1b).
The cumulative incidence of grade II–IV acute GVHD at day 100 were 57.3 % in patients experiencing CMV reactivation and 29.5 % in patients not experiencing reactivation (p < 0.01) (Fig. 2a), and the cumulative incidence of chronic GVHD by 1 year after UCBT was 27.4 % in patients with CMV reactivation and 11.7 % in patients without (p < 0.01) (Fig. 2b).
The cumulative incidences of leukemia relapse did not differ significantly between patients with CMV reactivation and patients without (27.2 vs. 23.3 %, p = 0.99) nor did OS at 3 year after UCBT (54.6 vs. 49.9 %; p = 0.15). The cumulative incidences of TRM at 1 year after transplantation in patients with and without CMV reactivation were 39.3 and 32.3 %, respectively (p = 0.07).
The number of CMV reactivations (1 vs. 2 or more) was not predictive of RFS, TRM, or OS.
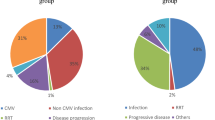
CMV disease
CMV disease was diagnosed in 62 (17.8 %) of the 349 CMV-seropositive transplant recipients at a median of 55 days after UCBT (range, 20–403): pneumonitis in 37 patients, enterocolitis in 12 patients, retinitis in 10 patients, hepatitis in 2 patients, and encephalitis in 1 patient. The median interval between CMV reactivation and disease was 31 days (range, 0–376 days). In seven patients (11.3 %), CMV disease was not preceded by surveillance detection of CMV infection.
Initial treatment for the 62 patients consisted of GCV (n = 45, 72.6 %), foscarnet (n = 11, 17.7 %), and others (n = 6, 9.7 %). Seventeen patients (27.4 %) did not respond to their initial treatment and received a second course of therapy: GCV → foscarnet in 14 patients, foscarnet → cidofovir in 2 patient, and CMV immunoglobulin (Megalotect®) → cidofovir in 1 patient. Of the 17 patients who received second line antiviral treatment, only 5 patients cleared the CMV disease.
To identify possible risk factors for CMV disease in patients with reactivated CMV, we employed the same variables used to predict the risk of CMV reactivation. In addition, we included the following variables: first day of CMV reactivation after UCBT, neutropenia at detection of CMV reactivation, empiric antiviral agent used to manage CMV reactivation, and duration of CMV reactivation. Longer duration of CMV reactivation was the only risk factor for progression from CMV reactivation to CMV disease (HR, 1.69; 98 % CI, 1.01–2.74; p = 0.01). The mean duration of CMV reactivation was 49.9 days in patients who developed CMV disease and 34.6 days in patients who did not.
There was no significant difference in the cumulative incidences of neutrophil engraftment (p = 0.16) between patients with CMV disease and those without, or in the cumulative incidences of leukemia relapse (22.9 vs. 27.8 %, p = 0.19). OS at 3 years after UCBT among patients who had CMV disease was significantly lower than among those without CMV disease (36.1 vs. 55.1 %, p < 0.01) (Fig. 3a), while the cumulative incidence of TRM at 1 year after transplantation was significantly higher (56.0 vs. 31.4 %, p < 0.01) (Fig. 3b). Interestingly, the time of CMV disease occurrence had statistical power to predict TRM; thus, patients who died due to transplantation-related complications were diagnosed with CMV disease earlier than those who did not (median, 68 days in TRM+ patients vs. median 113 days in TRM− patients, p = 0.05).
Discussion
In the present study, CMV reactivation occurred in 49 % of patients and recurrent CMV reactivation was seen in approximately 20 %. In subgroup analyses focusing on seropositive patients, although the numbers of patients were small, the incidence of CMV reactivation after UCBT ranged from 51 to 77 % [2, 17, 18].
Our findings suggest that the likelihood of CMV reactivation in seropositive patients is increased in the following conditions: first, by factors interfering with T cell depleting agents such as ATG. Previous studies have found an association between T cell immune reconstitution and CMV infection [5, 19–21]. ATG may damage recipient-derived anti-CMV immune cells, which may be important because CB recipients cannot acquire anti-CMV immunity from the donor stem cells [22]. Second, by grade II–IV acute GVHD: we observed that this was associated with a higher incidence of CMV reactivation, confirming the results of previous studies [9, 23, 24]. Also, steroid therapy for acute GVHD may have impeded the recovery of anti-CMV cytotoxic T lymphocytes (of the 179 patients with grade II–IV acute GVHD, 151 received steroid [data are not shown]) [25]. Third, it is affected by the use of TBI as previously reported [26, 27]. Preparative regimens including TBI may damage recipient-derived anti-CMV immune cells resulting in CMV reactivation. Fourth, it is increased by greater body weight. Beck et al. [2] found a trend toward increased CMV reactivation with age in multivariate analysis, with patients 18 years and older having a relative risk of CMV reactivation of 1.5. In our study, both age and weight were significant risk factors for CMV reactivation in univariate analysis. However, in multivariate analysis, age was not an independent risk factor. Finally, the use of MMF as GVHD prophylaxis was associated with an increased risk of CMV reactivation, consistent with data published by Hambach et al. [28]. MMF potently inhibits both T and B lymphocyte proliferation, thus impairing both cellular and humoral immunity directed toward CMV [29]. Separately, MMF may directly or indirectly influence viral replication by altering cytokine profiles or affecting the downregulation of adhesion molecules induced by CMV [30].
In our study, patients experiencing CMV reactivation had a higher neutrophil engraftment rate than those not experiencing CMV reactivation. When we analyzed the engraftment results of each CMV reactivation diagnostic method separately, there was no significant difference in the neutrophil engraftment rate between patients with CMV reactivation defined by PCR and those without CMV reactivation, while patients with CMV reactivation defined by pp65 antigenemia methods had a significantly higher engraftment rate compared to patients without CMV reactivation. These findings suggest that the higher engraftment rate observed in patients with CMV reactivation is not a valid result, but, rather, the consequence of selection bias due to the fact that the CMV detection method relies on CMV antigenemia, which identifies the pp65 protein of CMV in PB leukocytes. Taking into consideration only PCR-based diagnosis of CMV, neutrophil engraftment was not influenced by CMV reactivation. However, because there were only a few patients who were diagnosed by PCR, further studies are warranted to clarify the impact of CMV reactivation on engraftment.
We found that CMV reactivation was associated with a higher incidence of acute or chronic GVHD, as previously reported [26]. In our study, CMV reactivation did not alter TRM, leukemia relapse, or survival. However, we found lower OS and higher TRM among patients experiencing CMV disease. Furthermore, patients in whom CMV disease was diagnosed early suffered higher TRM. Therefore, predictive factors for CMV disease developing from CMV reactivation need to be identified, along with effective preemptive strategies against CMV.
In our study, the incidence of CMV disease after UCBT was 17.8 % in CMV seropositive recipients, which is slightly above the previously published rates of 1.0–13.8 % [2, 17, 23]. However, differences in preparative regimens, methods of CMV prevention, and patient characteristics limit comparisons. The duration of CMV reactivation was the only risk factor, and we identified for progression from CMV reactivation to CMV disease. Our findings indicate a need for intensive anti-CMV strategies to shorten the duration of CMV reactivation and so improve the outcomes of CMV disease. Recently, Milano et al. [31] reported that the use of intensive CMV prevention strategies using GCV reduced CMV reactivation and disease. Therefore, the addition of GCV before transplantation could contribute to lower rates of CMV disease. Foscarnet is as effective as GCV for preemptive treatment of CMV reactivation [32]. However, there is a paucity of information on the use of foscarnet for prophylaxis of CMV, although preliminary data showed that it was effective in some patients at high risk of CMV reactivation. Shereck et al. [33] reported that alternate day GCV/foscarnet was well tolerated and was 100 % effective in preventing CMV disease. As stated above, intensive intervention could be an effective strategy for preventing CMV disease.
In conclusion, CMV reactivation had little demonstrable impact on UCBT outcomes, whereas the development of CMV disease led to inferior outcomes. The high incidence of progression to CMV disease despite preemptive treatment underlines the need for newer strategies for CMV seropositive recipients. Since we could not identify patients at high risk of developing CMV disease at the time of UCBT, and the duration of CMV reactivation was the only risk factor for developing the disease, further studies are needed to determine the best management strategy for long-lasting CMV infections.
References
Albano MS, Taylor P, Pass RF, Scaradavou A, Ciubotariu R, Carrier C, Dobrila L, Rubinstein P, Stevens CE (2006) Umbilical cord blood transplantation and cytomegalovirus: posttransplantation infection and donor screening. Blood 108:4275–4282
Beck JC, Wagner JE, DeFor TE, Brunstein CG, Schleiss MR, Young JA, Weisdorf DH, Cooley S, Miller JS, Verneris MR (2010) Impact of cytomegalovirus (CMV) reactivation after umbilical cord blood transplantation. Biol Blood Marrow Transplant 16:215–222
D'Arena G, Musto P, Cascavilla N, Di Giorgio G, Fusilli S, Zendoli F, Carotenuto M (1998) Flow cytometric characterization of human umbilical cord blood lymphocytes: immunophenotypic features. Haematologica 83:197–203
Komanduri KV, St John LS, de Lima M, McMannis J, Rosinski S, McNiece I, Bryan SG, Kaur I, Martin S, Wieder ED, Worth L, Cooper LJ, Petropoulos D, Molldrem JJ, Champlin RE, Shpall EJ (2007) Delayed immune reconstitution after cord blood transplantation is characterized by impaired thymopoiesis and late memory T-cell skewing. Blood 110:4543–4551
Boeckh M, Nichols WG, Papanicolaou G, Rubin R, Wingard JR, Zaia J (2003) Cytomegalovirus in hematopoietic stem cell transplant recipients: current status, known challenges, and future strategies. Biol Blood Marrow Transplant 9:543–558
Broers AE, van Der Holt R, van Esser JW, Gratama JW, Henzen-Logmans S, Kuenen-Boumeester V, Lowenberg B, Cornelissen JJ (2000) Increased transplant-related morbidity and mortality in CMV-seropositive patients despite highly effective prevention of CMV disease after allogeneic T-cell-depleted stem cell transplantation. Blood 95:2240–2245
Ljungman P, Hakki M, Boeckh M (2010) Cytomegalovirus in hematopoietic stem cell transplant recipients. Infect Dis Clin N Am 24:319–337
Walker CM, van Burik JA, De For TE, Weisdorf DJ (2007) Cytomegalovirus infection after allogeneic transplantation: comparison of cord blood with peripheral blood and marrow graft sources. Biol Blood Marrow Transplant 13:1106–1115
George B, Kerridge I, Gilroy N, Huang G, Hertzberg M, Gottlieb D, Bradstock K (2010) Fludarabine-based reduced intensity conditioning transplants have a higher incidence of cytomegalovirus reactivation compared with myeloablative transplants. Bone Marrow Transplant 45:849–855
Yoo KH, Lee SH, Sung KW, Koo HH, Chung NG, Cho B, Kim HK, Kang HJ, Shin HY, Ahn HS, Baek HJ, Han DK, Kook H, Hwang TJ, Kim SY, Lee YH, Hah JO, Im HJ, Seo JJ, Park SK, Jung HJ, Park JE, Lim YJ, Park SS, Lim YT, Yoo ES, Ryu KH, Park HJ, Park BK (2011) Current status of pediatric umbilical cord blood transplantation in Korea: a multicenter retrospective analysis of 236 cases. Am J Hematol 86:12–17
Ljungman P, Griffiths P, Paya C (2002) Definitions of cytomegalovirus infection and disease in transplant recipients. Clin Infect Dis 34:1094–1097
Frangoul H, Wang L, Harrell FE Jr, Ho R, Domm J (2009) Preengraftment syndrome after unrelated cord blood transplant is a strong predictor of acute and chronic graft-versus-host disease. Biol Blood Marrow Transplant : J Am Soc Blood Marrow Transplant 15:1485–1488
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, Apperley J, Slavin S, Pasquini M, Sandmaier BM, Barrett J, Blaise D, Lowski R, Horowitz M (2009) Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transplant 15:1628–1633
Patel KJ, Rice RD, Hawke R, Abboud M, Heller G, Scaradavou A, Young JW, Barker JN (2010) Pre-engraftment syndrome after double-unit cord blood transplantation: a distinct syndrome not associated with acute graft-versus-host disease. Biol Blood Marrow Transplant 16:435–440
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, Thomas ED (1995) 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transplant 15:825–828
Vigorito AC, Campregher PV, Storer BE, Carpenter PA, Moravec CK, Kiem HP, Fero ML, Warren EH, Lee SJ, Appelbaum FR, Martin PJ, Flowers ME (2009) Evaluation of NIH consensus criteria for classification of late acute and chronic GVHD. Blood 114:702–708
Tomonari A, Takahashi S, Ooi J, Tsukada N, Konuma T, Kato S, Kasahara S, Iseki T, Yamaguchi T, Tojo A, Asano S (2008) Impact of cytomegalovirus serostatus on outcome of unrelated cord blood transplantation for adults: a single-institute experience in Japan. Eur J Haematol 80:251–257
Mikulska M, Raiola AM, Bruzzi P, Varaldo R, Annunziata S, Lamparelli T, Frassoni F, Tedone E, Galano B, Bacigalupo A, Viscoli C (2012) CMV infection after transplant from cord blood compared to other alternative donors: the importance of donor-negative CMV serostatus. Biol Blood Marrow Transplant 18:92–99
Buyck HC, Prentice HG, Griffiths PD, Emery VC (2010) The risk of early and late CMV DNAemia associated with Campath use in stem cell transplant recipients. Bone Marrow Transplant 45:1212–1219
Pinana JL, Martino R, Barba P, Margall N, Roig MC, Valcarcel D, Sierra J, Rabella N (2010) Cytomegalovirus infection and disease after reduced intensity conditioning allogeneic stem cell transplantation: single-centre experience. Bone Marrow Transplant 45:534–542
Barron MA, Gao D, Springer KL, Patterson JA, Brunvand MW, McSweeney PA, Zeng C, Baron AE, Weinberg A (2009) Relationship of reconstituted adaptive and innate cytomegalovirus (CMV)-specific immune responses with CMV viremia in hematopoietic stem cell transplant recipients. Clin Infect Dis 49:1777–1783
Yi ES, Kim YJ (2012) Cytomegalovirus infection according to cell source after hematopoietic cell transplantation in pediatric patients. Yonsei Med J 53:393–400
Montesinos P, Sanz J, Cantero S, Lorenzo I, Martin G, Saavedra S, Palau J, Romero M, Montava A, Senent L, Martinez J, Jarque I, Salavert M, Cordoba J, Gomez L, Weiss S, Moscardo F, de la Rubia J, Larrea L, Sanz MA, Sanz GF (2009) Incidence, risk factors, and outcome of cytomegalovirus infection and disease in patients receiving prophylaxis with oral valganciclovir or intravenous ganciclovir after umbilical cord blood transplantation. Biol Blood Marrow Transplant 15:730–740
Al-Hajjar S, Al Seraihi A, Al Muhsen S, Ayas M, Al Jumaah S, Al Jefri A, Shoukri M, El Solh H (2011) Cytomegalovirus infections in unrelated cord blood transplantation in pediatric patients: incidence, risk factors, and outcomes. Hematol/Oncol Stem Cell Ther 4:67–72
Ozdemir E, St John LS, Gillespie G, Rowland-Jones S, Champlin RE, Molldrem JJ, Komanduri KV (2002) Cytomegalovirus reactivation following allogeneic stem cell transplantation is associated with the presence of dysfunctional antigen-specific CD8+ T cells. Blood 100:3690–3697
Matsumura T, Narimatsu H, Kami M, Yuji K, Kusumi E, Hori A, Murashige N, Tanaka Y, Masuoka K, Wake A, Miyakoshi S, Kanda Y, Taniguchi S (2007) Cytomegalovirus infections following umbilical cord blood transplantation using reduced intensity conditioning regimens for adult patients. Biol Blood Marrow Transplant 13:577–583
Kullberg-Lindh C, Mellgren K, Friman V, Fasth A, Ascher H, Nilsson S, Lindh M (2011) Opportunistic virus DNA levels after pediatric stem cell transplantation: serostatus matching, anti-thymocyte globulin, and total body irradiation are additive risk factors. Transpl Infect Dis 13:122–130
Hambach L, Stadler M, Dammann E, Ganser A, Hertenstein B (2002) Increased risk of complicated CMV infection with the use of mycophenolate mofetil in allogeneic stem cell transplantation. Bone Marrow Transplant 29:903–906
Lipsky JJ (1996) Mycophenolate mofetil. Lancet 348:1357–1359
Heemann U, Azuma H, Hamar P, Schmid C, Tilney N, Philipp T (1996) Mycophenolate mofetil inhibits lymphocyte binding and the upregulation of adhesion molecules in acute rejection of rat kidney allografts. Transpl Immunol 4:64–67
Milano F, Pergam SA, Xie H, Leisenring WM, Gutman JA, Riffkin I, Chow V, Boeckh MJ, Delaney C (2011) Intensive strategy to prevent CMV disease in seropositive umbilical cord blood transplant recipients. Blood 118:5689–5696
Bacigalupo A, Boyd A, Slipper J, Curtis J, Clissold S (2012) Foscarnet in the management of cytomegalovirus infections in hematopoietic stem cell transplant patients. Expert Rev Anti-Infect Ther 10:1249–1264
Shereck EB, Cooney E, van de Ven C, Della-Lotta P, Cairo MS (2007) A pilot phase II study of alternate day ganciclovir and foscarnet in preventing cytomegalovirus (CMV) infections in at-risk pediatric and adolescent allogeneic stem cell transplant recipients. Pediatr Blood Cancer 49:306–312
Acknowledgments
This study was supported by a grant of Kyowa Hakko Kirin Korea Co., Ltd., 2011.
Conflict of interest
The authors declare no conflicts of interest.
Authors’ contributions
M. Park designed the study, performed the analysis, and wrote the paper; Y.H. Lee designed the study, performed the research, and reviewed the manuscript; S.H. Lee, K.H. Yoo, K.W. Sung, H.H. Koo, H.J. Kang, K.D. Park, H.Y. Shin, H.S. Ahn, N.G. Chung, B. Cho, H.K. Kim, K.N. Koh, H.J. Im, J.J. Seo, H.J. Baek, H. Kook, T.J. Hwang, J.M. Lee, J.O. Hah, Y.J. Lim, J.E. Park, C.J. Lyu, Y.T. Lim, S.Y. Chong, and D. Oh contributed to the analysis of data.
Participating centers
This study was conducted at the following institutions: College of Medicine, Chungbuk National University, Cheongju; Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul; Hanyang University Medical Center, Hanyang University College of Medicine, Seoul; Cancer Research Institute, Seoul National University College of Medicine, Seoul; Seoul St. Mary’s Hospital, The Catholic University of Korea, Seoul; Asan Medical Center Children’s Hospital, University of Ulsan College of Medicine, Seoul; Chonnam National University Hwasun Hospital, Chonnam National University Medical School, Gwangju; Yeungnam University College of Medicine, Daegu; Chungnam National University College of Medicine, Daejon; Ajou University School of Medicine, Suwon; CHA Bundang Medical Center, CHA University, Seongnam; Mokdong Hospital, Ehwa women’s University College of Medicine, Seoul; Yonsei University College of Medicine, Seoul; Gyeongsang National University School of Medicine, Jinju; Pusan National University, School of Medicine, Pusan; National Cancer Center, Goyang; Konkuk University College of Medicine, Seoul; Gachon University Gil Hospital, Gachon University School of Medicine, Incheon; Daegu Fatima Hospital, Daegu, Korea.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Park, M., Lee, Y.H., Lee, S.H. et al. Cytomegalovirus infection in seropositive unrelated cord blood recipients: a study of 349 Korean patients. Ann Hematol 94, 481–489 (2015). https://doi.org/10.1007/s00277-014-2222-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-014-2222-x