Abstract
Human herpesvirus-6 (HHV-6) encephalitis following allogeneic hematopoietic cell transplantation is a serious and often fatal complication accompanying reactivation of HHV-6B. Incidence varies among studies, but is reportedly 0–11.6% after bone marrow or PBSC transplantation and 4.9–21.4% after umbilical cord blood transplantation, typically around 2–6 weeks post transplant. Symptoms are characterized by memory loss, loss of consciousness and seizures. Magnetic resonance imaging (MRI) typically shows bilateral signal abnormalities in the limbic system. This complication is considered to represent acute encephalitis caused by direct virally induced damage to the central nervous system, but our understanding of the etiologies and pathogenesis is still limited. The mortality rate attributable to this pathology remains high, and survivors are often left with serious sequelae such as impaired memory and epilepsy. Despite the poor prognosis, no validated treatments or preventative measures have been established. Establishment of preventative strategies represents an important challenge. This article reviews the current knowledge of the clinical features, incidence, pathogenesis and treatment of HHV-6 encephalitis, and discusses issues needing clarification in the future to overcome this serious complication.
Similar content being viewed by others
Introduction
Reactivation of human herpesvirus-6 (HHV-6) is common after allogeneic hematopoietic cell transplantation (allo-HCT),1, 2, 3, 4, 5 and is sporadically associated with the development of HHV-6 encephalitis.1, 3, 4, 5, 6, 7, 8 The first case of HHV-6 encephalitis after allo-HCT was described in 1994 by Drobyski et al.9 Since then, a significant amount of information regarding the incidence, risk factors, therapy and outcomes has been reported. Over the past decade, HHV-6 encephalitis has become well known as a significant complication of allo-HCT. However, several important questions have not been clarified. We know HHV-6 causes HHV-6 encephalitis, but we do not know how; we know what drugs may work in vitro, but we do not know how to apply them in vivo; we know that systemic HHV-6 reactivation sporadically accompanies encephalitis, but we do not know the mechanisms dividing symptomatic reactivation from asymptomatic.
In this article, we review the current understanding of HHV-6 encephalitis, and discuss the future directions needed to overcome this feared transplant complication.
Disease associations: we do not know the precise disease association of HHV-6 with allo-HCT
HHV-6 is a member of the Roseolovirus genus in the Betaherpesvirinae subfamily. HHV-6 comprises two closely related species, HHV-6A and -6B.10 HHV-6B is a ubiquitous virus that infects virtually all children by 2 years of age11 and is a causative agent for exanthema subitum. Less is known about the epidemiology and clinical significance of HHV-6A. Most HHV-6 infections in allo-HCT recipients are due to reactivation of HHV-6B.1, 12
Reactivation of HHV-6 is usually asymptomatic, leading some to question its role as a pathogen. Because of the relatively high frequency of HHV-6 reactivation and existence of many causes for central nervous system (CNS) dysfunction after allo-HCT, establishing a causal relationship between HHV-6 reactivation and encephalitis is difficult.13 However, accumulated data have shown that HHV-6 sporadically causes encephalitis in allo-HCT recipients. Wang et al.14 detected HHV-6 DNA in cerebrospinal fluid specimens from 5 of 22 cases (23%) with CNS symptoms and in cerebrospinal fluid specimens from 1 of 107 controls (0.9%). Zerr and Ogata15 showed that a causal association between HHV-6 and encephalitis can be demonstrated by application of the Bradford Hill criteria for strength of association, as a list of the criteria necessary to provide epidemiological evidence for causality, including consistency, specificity, temporality, biological gradient, plausibility, coherence, analogy and experimental evidence.16, 17 (See Zerr and Ogata15 regarding how HHV-6 meets these criteria.)
CNS dysfunction attributable to HHV-6 may not necessarily appear as encephalitis. A well-designed, prospective study18 demonstrated an independent association between HHV-6 reactivation and subsequent delirium. HHV-6 reactivation was also associated with subsequent neurocognitive declines. In that study, no typical imaging abnormalities associated with HHV-6 encephalitis were confirmed in any of the 9 patients who underwent brain magnetic resonance imaging (MRI).18
HHV-6 may also cause bone marrow suppression or graft failure.1, 2, 6, 19, 20, 21 Many clinical reports have described possible associations between HHV-6 infection and other post-transplant complications, including pneumonitis,22, 23 gastroenterocolitis,2, 24 GVHD25, 26 and cytomegalovirus infection.25 However, these associations have not been consistently demonstrated and causality remains uncertain.
Chromosomally integrated HHV-6 (ciHHV-6): we know a few individuals have ciHHV-6, but we do not know its pathogenicity
HHV-6 is the only human herpesvirus known to integrate into the germline.27 The complete HHV-6 genome becomes integrated into the telomere of every chromosome and is vertically transmitted.27 This condition, ciHHV-6, is considered to be present in ∼1% of the populations of the United States and United Kingdom.28, 29 Although ciHHV-6 can be induced to a state of viral replication both in vitro27 and in vivo,30, 31 whether the integrated virus can reactivate and cause disease in the setting of allo-HCT is unknown. To date, only one case of a patient with ciHHV-6A and HHV-6A reactivation as a possible cause of HHV-6 encephalitis in the setting of allo-HCT has been reported.32 Individuals with ciHHV-6 always show abnormally high copy numbers of HHV-6 DNA in whole blood, and cerebrospinal PCR testing for HHV-6 may also become positive in patients with cerebrospinal fluid pleocytosis.27, 33 As described below, blood HHV-6 DNA levels usually appear high in patients with HHV-6 encephalitis and the demonstration of positive HHV-6 DNA in cerebrospinal fluid is an important condition for diagnosis. As a result, ciHHV-6 should be carefully excluded before HHV-6 encephalitis is diagnosed. The possibility of ciHHV-6 should be considered when high viral DNA loads persist in blood despite an absence of clinical symptoms. In situations where a donor has ciHHV-6, the blood HHV-6 DNA load in the recipient will increase with engraftment.34 Quantitative PCR results for HHV-6 are usually >106 copies/mL of whole blood.27 Conversely, where a recipient has ciHHV-6, blood HHV-6 DNA in the recipient may appear high both before and immediately after HCT. PCR testing of hair follicles or nails for HHV-6 DNA can confirm ciHHV-6 status in recipients.35
Clinical presentation and diagnosis: we know clinical features of typical HHV-6 encephalitis, but do not know the variability of its presentation
HHV-6 encephalitis typically develops ∼2–6 weeks after allo-HCT,3, 4, 5, 36, 37 and symptoms often include delirium, amnesia, confusion, ataxia and seizure. The most typical initial symptom is memory loss with subsequent progression to confusion and loss of consciousness.3, 36, 37 Overt seizures, including generalized seizures and partial seizures, develop in 40–70% of patients.36, 37, 38 HHV-6 encephalitis may accompany syndrome of inappropriate antidiuretic hormone.38, 39, 40
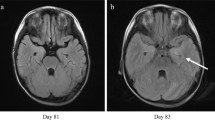
HHV-6 encephalitis typically shows an MRI signature of hyperintense lesions on T2-weighted, fluid-attenuated inversion recovery imaging and diffusion-weighted imaging of bilateral medial temporal lobes, primarily affecting the hippocampus and amygdala (Figure 1).3, 7, 36, 37, 38, 41, 42 Some investigators have termed this finding ‘post-transplant acute limbic encephalitis (PALE)38, 40, 42, 43, 44 and HHV-6 PALE has been diagnosed when the patient has detectable HHV-6 DNA in cerebrospinal fluid in the context of acute-onset altered mental status, amnesia, seizures or other evidence of medial temporal lobe disease involving the limbic system and no other identifiable etiology.38, 42 A recent retrospective study45 showed, however, not all cases of HHV-6-associated CNS dysfunction meet the criteria for PALE. HHV-6 may also cause myelitis that presents with systemic pruritus and severe pain in the extremities.46, 47, 48 They indicate that HHV-6 should be considered as a possible cause of CNS dysfunction, even if the clinical presentation is atypical for HHV-6 encephalitis.
Magnetic resonance imaging (MRI) of the brain for 8 patients who developed HHV-6 encephalitis at Oita University Hospital or Oita Prefectural Hospital. (a–c) T2-weighted imaging. (d–h) T2-weighted fluid-attenuated inversion recovery imaging. Arrows indicate signal hyperintensities in the region of the hippocampus. MRI was performed at 20 days (a), 10 days (b), 5 days (c), 0 days (d), 7 days (e), 3 days (f), 0 days (g) and 6 days (h) after onset of neurological symptoms. Images in (a, b, d) were taken from Ogata et al.,3 image in (c) was taken from Ogata et al.7 and images in (f–h) were taken from Ogata et al.41
How should we diagnose HHV-6 encephalitis? The gold-standard technique to detect causative infectious agents in encephalitis is a study of brain biopsy material,49 but this is not possible in most HCT recipients. The results of retrospective studies14, 38 and many case reports36 have suggested the importance of demonstrating HHV-6 DNA in cerebrospinal fluid, and several guidelines recommend cerebrospinal PCR testing for the diagnosis of HHV-6 encephalitis.50, 51, 52, 53 Criteria frequently used in the literature to define HHV-6 encephalitis include: the presence of neurological symptoms (altered mental status, altered level of consciousness, amnesia, seizures and change in personality and behavior); positive PCR results for HHV-6 in cerebrospinal fluid (ciHHV-6 should be excluded); and the absence of other identified etiologies of CNS dysfunction.5, 15, 37, 44, 45, 54 This criterion may enable physicians to diagnose HHV-6 encephalitis effectively and efficiently. False-positive results for HHV-6 DNA in cerebrospinal fluid may occur,50, 52, 55 and hence positive results must be interpreted carefully in conjunction with clinical symptoms and negative results for other etiologies.
HHV-6 reactivation and HHV-6 encephalitis: we know HHV-6 reactivation is common after allo-HCT, but do not know the factors diving symptomatic reactivation from asymptomatic
With allo-HCT, reactivation of HHV-6 is observed in 30–70% of patients at 2–4 weeks after transplantation.1, 2, 3, 4, 5, 6 The duration of displaying positive HHV-6 DNA in plasma is only 1–2 weeks in most cases.3, 5, 7, 8 HHV-6B accounts for most reactivation events.1, 12 Risk factors for displaying HHV-6 reactivation are HLA mismatch,3, 4 steroid treatment,1, 3 transplants from unrelated donors2, 3 and umbilical cord blood transplantation (UCBT).4, 5
HHV-6 encephalitis develops concomitant to peak blood HHV-6 DNA.3, 5, 7, 8 Some studies in which blood levels of HHV-6 DNA have been monitored have shown a correlation between HHV-6 reactivation and the development of HHV-6 encephalitis,1, 3, 4, 5, 6, 7, 8, 56 but others have failed to demonstrate such associations.2, 57, 58 The reasons for these divergent results may be because of the low incidence of HHV-6 encephalitis even in patients with HHV-6 reactivation. For example, Hentrich et al.2 reported encephalitis developing in 1 of 99 patients not infected with HHV-6, and 3 of 129 patients infected with HHV-6. Betts et al.57 reported that rates of CNS dysfunction were similar in HHV-6 viremia-positive and -negative patients in their prospective study, including 82 patients. A recently published prospective multicenter study5 evaluating plasma HHV-6 DNA twice a week after transplantation showed incidences of HHV-6 encephalitis of 0%, 8.1% and 16% among patients with peak plasma HHV-6 DNA <104 copies/mL, ⩾104 copies/mL and ⩾105 copies/mL, respectively. For identifying HHV-6 encephalitis, plasma HHV-6 DNA ⩾104 copies/mL offered 100% sensitivity and 64.6% specificity, whereas plasma HHV-6 DNA ⩾105 copies/mL offered 57.1% sensitivity and 90.6% specificity.5 A large retrospective study42 reported that the sensitivity and specificity of plasma HHV-6 DNA ⩾105 copies/mL were 71% and 94%, respectively, for identifying HHV-6 encephalitis. These studies suggest that higher levels of HHV-6 reactivation are associated with an increased risk of developing HHV-6 encephalitis. However, they also showed that even when the HHV-6 DNA plasma level was high, most patients still did not develop HHV-6 encephalitis.5, 42
Incidence and risk factors: we know UCBT is a risk factor of HHV-6 encephalitis, but do not know the true incidence and other risk factors
Reported incidences of HHV-6 encephalitis in allo-HCT recipients have ranged from 0.95 to 11.6% (Table 1).3, 4, 5, 8, 42, 44, 45, 47, 54, 55, 59, 60, 61, 62 Many factors will affect the reported incidence, including the proportion of stem cell sources in the analyzed population, study design, definitions of HHV-6 encephalitis, selection of immunosuppressants and efforts toward diagnosis.
Clearly, UCBT represents a strong risk factor for HHV-6 encephalitis (Table 1). Among previous reports, a systematic review and meta-analysis of 19 papers,62 a large-scale single-center retrospective study analyzing 1344 patients42 and a prospective multicenter study monitoring HHV-6 reactivations5 all showed a similar incidence, with 7.9–9.9% among UCBT recipients and 0.5–1.2% among bone marrow or PBSC transplant recipients developing HHV-6 encephalitis. The high incidence of HHV-6 encephalitis among UCBT recipients may be associated with the lack of memory T cells against HHV-6 in the cord blood that are certainly present in stem cells sourced from adult donors. However, use of antithymocyte globulin as part of the conditioning regimen rather decreases the frequency of HHV-6 reactivation.5 Furthermore, HHV-6 encephalitis is quite rare in primary or acquired immunodeficiencies.63 They suggest that development of HHV-6 encephalitis does not simply depend on impaired T-cell function.
The inflammatory milieu early after allo-HCT may be associated with the development of HHV-6 encephalitis. Mori et al.47 reported that all of 13 patients with HHV-6 encephalitis/myelitis presented with pre-engraftment syndrome before the onset of encephalitis. A large-scale retrospective study42 demonstrated acute GVHD as a significant risk factor with an adjusted hazard ratio of 7.5 (P<0.001) for subsequent development of HHV-6 encephalitis. Among patients with high-level HHV-6 reactivation, GVHD and engraftment syndrome represented significant risk factors for subsequent development of HHV-6 encephalitis.8 Classically, activating cytokines were thought to cause reactivation of herpesviruses. Several drugs, including hydrocortisone, or some antibiotics are associated with HHV-6 reactivation.27 Apoptosis of lymphocytes triggers the lytic replication of HHV-6.64 The cellular receptor for HHV-6B entry is CD134 that is present on activated T lymphocytes.65 They suggest that immune reactions such as GVHD or treatment against the reactions may enhance HHV-6 replication and accelerate the development of HHV-6 encephalitis. Evaluation of the direction of the causative association between immune reaction and HHV-6 encephalitis will be important, because it may not only elucidate the pathogenic processes but also lead to the development of prophylactic approaches. Better prevention of GVHD and related inflammatory condition early after transplant may reduce the incidence of HHV-6 encephalitis.
Other risk factors for HHV-6 encephalitis include steroid treatment,3 second UCBT,47 use of alemtuzumab59 and male sex.45, 66 The significance of these factors remains unconfirmed.
It is important to note that the incidence of HHV-6 encephalitis can be underestimated if HHV-6 encephalitis cannot be diagnosed adequately. A prospective multicenter study performing monitoring of HHV-6 reactivation5 suggested that many patients may not be given a diagnosis of HHV-6 encephalitis when lumbar puncture is not performed.
Pathogenesis: we do not know how HHV-6 contributes to CNS disease pathology
To date, no evidence of productive HHV-6B infection has been obtained for neural stem cells, astrocytes and oligodendrocytes,67, 68, 69 suggesting that CNS reactivation depends on systemic HHV-6 reactivation. Autopsy studies of patients who died with HHV-6 encephalitis have shown the hippocampus has strong reactivity against HHV-6,9, 70 and HHV-6 has displayed tropism for astrocytes in the hippocampus.70 HHV-6B will directly cause neuronal damage based on the finding that HHV-6B localizes to pathologically damaged regions.
Nevertheless, other mechanisms may contribute to the pathology of HHV-6 encephalitis. An in vitro study showed HHV-6-induced dysregulation of glutamate uptake in HHV-6-infected astrocytes.71 Such mechanisms may be responsible for the occurrence of seizures. Brain MRI commonly shows bilaterally symmetrical findings in the region of the limbic system (Figure 1), suggesting the existence of systemic processes. HHV-6 PALE bears a clinical resemblance to paraneoplastic limbic encephalitis, a subacute illness associated with paraneoplastic autoantibodies. Not only high-level HHV-6 reactivation, but also a hypercytokinemic state preceding HHV-6 reactivation is associated with progression to HHV-6 encephalitis.8 Furthermore, HHV-6-negative PALE has been described.38 Such findings suggest the existence of multiple pathogenic mechanisms, including autoimmunity, autoantibodies or hypercytokinemic state, underlying the CNS manifestations of HHV-6 encephalitis.
Outcomes: we do not know much about the mortality rate and long-term outcomes
A review of reported cases by Zerr36 revealed that 11 of the 44 patients (25%) died of encephalitis, 14% showed improvement but died because of various problems, 18% were left with lingering neurological compromise and 43% appeared to make a full recovery. A multicenter survey in Japan37 reported that 2 of 23 patients died from encephalitis, whereas 21 patients recovered. However, 10 of these 21 patients showed after-effects of short-term memory impairment. A single-center retrospective study42 showed that 5 of 19 patients (26%) died of encephalitis and 9 patients (47%) survived with residual fatigue and memory impairment. Sakai et al.60 reported that four of five surviving patients were unable to return to society because of neuropsychological disorders. In that report, prominent hippocampal atrophy in the late phase was demonstrated on MRI. These data indicate a high mortality rate for HHV-6 encephalitis, and even among survivors, many patients are left with neurological compromise. Frequently reported sequelae include memory impairment and temporal lobe epilepsy.36, 37 The variability of reported outcomes may be because of small cohorts of cases. A larger cohort study is needed to reveal more precisely the mortality rates and long-term outcomes of HHV-6 encephalitis.
Treatment: we know what agents are active in vitro, but do not know how to use them for patients with HHV-6 encephalitis
The International Herpes Management Forum,50 European Conference of Infections in Leukaemia,51 Clinical Practice Guideline by the Infectious Disease Society of America52 and the Japan Society for Hematopoietic Cell Transplantation72 all recommend foscarnet (PFA) or ganciclovir (GCV) as first-line therapies for HHV-6 encephalitis. However, no controlled trial to evaluate the clinical efficacy of these antiviral agents against HHV-6 encephalitis has been carried out and no validated treatments have been established.
How should we treat HHV-6 encephalitis based on currently available data? Because neurological symptoms progress rapidly in patients who develop HHV-6 encephalitis,3, 38, 41, 42 antiviral therapy should be started as soon as possible. Delayed initiation of antiviral therapy will give the HHV-6 time to expand in the brain. Studies of in vitro efficacy73, 74, 75, 76 have identified PFA as showing the highest selectivity among anti-HHV-6 compounds, and PFA is therefore considered the preferred treatment option for HHV-6 encephalitis. Combination therapy with PFA and GCV50, 51 may be more effective than monotherapy, but the benefits and additional risks have yet to be assessed. In vitro susceptibility testing73, 75 for isolated HHV-6 may be a reliable method for selecting antivirals, but the process is both time consuming and labor intensive.
For the treatment of HHV-6 encephalitis, the dose of PFA should not be reduced except in response to renal dysfunction. An in vitro study showed that 40–107 μM of PFA completely suppresses HHV-6 replication.73, 76 The maximum drug concentration in blood from patients receiving 180 mg/kg/day PFA ranged from 560 to 580 μM. Raffi et al.77 reported that the median ratio of the concentration in cerebrospinal fluid to that in plasma was 0.27. These observations suggest that the PFA concentration in cerebrospinal fluid theoretically achieves the therapeutic range in patients who receive 180 mg/kg/day of PFA. Actually, a clinical study of prophylactic PFA therapy showed that low-dose PFA (50 mg/kg/day) appeared insufficient, but PFA at 180 mg/kg/day was sufficient to suppress HHV-6 replication in cerebrospinal fluid.41 If creatinine clearance is >1.4 mL/min/kg, then 180 mg/kg/day of PFA should be used when treating HHV-6 encephalitis. Evidence to guide the optimal duration of therapy is sorely lacking. However, many clinicians would plan for at least 3 weeks of antiviral therapy.15
Many other compounds that are active against cytomegalovirus, including brincidofovir (CMX-001),78, 79 CMV423,80 methylenecyclopropane analogs81 and artesunate82 have also been reported to inhibit HHV-6 in vitro. Administration of brincidofovir at a single dose of 2 mg/kg led to maximum plasma concentrations of 350 ng/mL83 that sufficiently exceeds the half-maximum effective concentration of HHV-6B strain79 without adverse events including changes in hematological or renal functions.83 A case report showed artesunate was effective and safe for treating HHV-6B myocarditis.84 Clinical trials will be required to assess the potential values of these drugs in the treatment of HHV-6-related diseases.
Recent progress of HHV-6-specific T-cell therapy is encouraging.85, 86, 87 Adoptive transfer of anti-HHV-6 T cells may effectively reduce the clinical manifestations of HHV-6 encephalitis or prevent HHV-6 diseases in the future.
Prevention: we do not know measures for preventing HHV-6 encephalitis
Because the efficacy of antiviral treatment appears insufficient if HHV-6 encephalitis has already developed, the establishment of methods for prediction or prevention is expected.7, 18, 47, 60, 88, 89
Can monitoring of HHV-6 reactivation predict the development of HHV-6 encephalitis? HHV-6 encephalitis develops concomitant to displaying high levels of plasma HHV-6 DNA.3, 5, 7, 8 Plasma HHV-6 DNA loads, however, can elevate from undetectable to very high level within a few days in patients with HHV-6 encephalitis.3, 5, 7 Monitoring of HHV-6 DNA may be useful to assume HHV-6 encephalitis in patients who present with CNS dysfunction,5 but cannot predict the development of HHV-6 encephalitis in most cases. Actually, trials of plasma HHV-6 DNA-guided preemptive approaches have proven inadequate in preventing the development of HHV-6 encephalitis because of the dynamic kinetics of plasma HHV-6 DNA.7, 90
Prophylactic administration of anti-HHV-6 antivirals will suppress HHV-6 replication and may effectively prevent the development of HHV-6 encephalitis. However, the toxicity of currently applicable antivirals limits the practical application for prophylaxis. Prophylaxis using GCV in the early phase of transplantation may compromise engraftment, and PFA is associated with renal toxicity. Furthermore, no available data have yet demonstrated any significant efficacy of prophylactic antiviral therapy in preventing HHV-6 encephalitis among allo-HCT recipients. A study evaluating the effects of prophylactic PFA showed that 50 mg/kg/day of PFA for 10 days was safe, but failed to effectively suppress HHV-6 reactivation and could not prevent HHV-6 encephalitis.41
To establish effective measures for preventing HHV-6 encephalitis, we are now conducting a clinical study of prophylactic PFA (90 mg/kg) for longer periods in UCBT recipients. The results of this study are encouraging because they may indicate the effect of currently available agents for high-risk patients, but we also consider that toxicity of PFA limits the practical application of prophylaxis to the wider HCT recipient population. Many other new compounds including brincidofovir,78, 79 methylenecyclopropane analogs81 or artesunate82 may be available in the future for preventing HHV-6 encephalitis. A phase 2 trial showed that brincidofovir effectively prevented cytomegalovirus diseases without myelosuppression and nephrotoxicity in allo-HCT recipients.91 Diarrhea was the most common adverse event.91 Clinical trials will be required to assess the safety and efficacy of new agents to suppress HHV-6 reactivation and prevent HHV-6 encephalitis.
Future needs
-
1
To ascertain the true incidence and outcome. A large-scale prospective study or large cohort study may reveal the clinical significance of HHV-6 encephalitis more clearly. We are now conducting an epidemiological study using the Japanese national registry data.
-
2
To understand the pathophysiology. Analysis of inflammatory status in blood and cerebrospinal fluid (cytokines, chemokines and other biomarkers), antineuronal antibodies, biomarkers for blood–brain barrier injury and detailed autopsy study (HHV-6 status) may foster a better understanding of the pathophysiology
-
3
To determine optimal treatment. A randomized controlled study to evaluate the effect of antivirals against HHV-6 encephalitis may be difficult to achieve, because HHV-6 encephalitis is relatively rare and progresses rapidly. Collection of large-scale data about treatment (dose, start timing and duration of antiviral treatment such as GCV and PFA) and outcomes in patients with HHV-6 encephalitis will be useful to guide current treatment strategies.
-
4
To improve treatment. Effects of other compounds, particularly brincidofovir, are encouraging. Immunotherapy may effectively improve the outcomes of HHV-6 encephalitis. Clinical studies are needed to confirm the efficacies and toxicities of any new therapies.
-
5
To establish effective prophylaxis. The incidence of HHV-6 encephalitis according to risk factors (such as UCBT, GVHD or others) should be analyzed to determine who should receive prophylaxis. Clinical studies evaluating the safety and efficacy of prophylactic treatments using either currently available agents such as PFA or new compounds are needed. Furthermore, whether better control of GVHD or inflammatory conditions may reduce the incidence of HHV-6 encephalitis should be confirmed.
References
Zerr DM, Corey L, Kim HW, Huang ML, Nguy L, Boeckh M . Clinical outcomes of human herpesvirus 6 reactivation after hematopoietic stem cell transplantation. Clin Infect Dis 2005; 40: 932–940.
Hentrich M, Oruzio D, Jager G, Schlemmer M, Schleuning M, Schiel X et al. Impact of human herpesvirus-6 after haematopoietic stem cell transplantation. Br J Haematol 2005; 128: 66–72.
Ogata M, Kikuchi H, Satou T, Kawano R, Ikewaki J, Kohno K et al. Human herpesvirus 6 DNA in plasma after allogeneic stem cell transplantation: incidence and clinical significance. J Infect Dis 2006; 193: 68–79.
Yamane A, Mori T, Suzuki S, Mihara A, Yamazaki R, Aisa Y et al. Risk factors for developing human herpesvirus 6 (HHV-6) reactivation after allogeneic hematopoietic stem cell transplantation and its association with central nervous system disorders. Biol Blood Marrow Transplant 2007; 13: 100–106.
Ogata M, Satou T, Kadota J, Saito N, Yoshida T, Okumura H et al. Human herpesvirus 6 (HHV-6) reactivation and HHV-6 encephalitis after allogeneic hematopoietic cell transplantation: a multicenter, prospective study. Clin Infect Dis 2013; 57: 671–681.
Ljungman P, Wang FZ, Clark DA, Emery VC, Remberger M, Ringden O et al. High levels of human herpesvirus 6 DNA in peripheral blood leucocytes are correlated to platelet engraftment and disease in allogeneic stem cell transplant patients. Br J Haematol 2000; 111: 774–781.
Ogata M, Satou T, Kawano R, Goto K, Ikewaki J, Kohno K et al. Plasma HHV-6 viral load-guided preemptive therapy against HHV-6 encephalopathy after allogeneic stem cell transplantation: a prospective evaluation. Bone Marrow Transplant 2008; 41: 279–285.
Ogata M, Satou T, Kawano R, Takakura S, Goto K, Ikewaki J et al. Correlations of HHV-6 viral load and plasma IL-6 concentration with HHV-6 encephalitis in allogeneic stem cell transplant recipients. Bone Marrow Transplant 2010; 45: 129–136.
Drobyski WR, Knox KK, Majewski D, Carrigan DR . Brief report: fatal encephalitis due to variant B human herpesvirus-6 infection in a bone marrow-transplant recipient. N Engl J Med 1994; 330: 1356–1360.
Adams MJ, Carstens EB . Ratification vote on taxonomic proposals to the International Committee on Taxonomy of Viruses. Arch Virol 2012; 157: 1411–1422.
Zerr DM, Meier AS, Selke SS, Frenkel LM, Huang ML, Wald A et al. A population-based study of primary human herpesvirus 6 infection. N Engl J Med 2005; 352: 768–776.
Reddy S, Manna P . Quantitative detection and differentiation of human herpesvirus 6 subtypes in bone marrow transplant patients by using a single real-time polymerase chain reaction assay. Biol Blood Marrow Transplant 2005; 11: 530–541.
Kadakia MP, Rybka WB, Stewart JA, Patton JL, Stamey FR, Elsawy M et al. Human herpesvirus 6: infection and disease following autologous and allogeneic bone marrow transplantation. Blood 1996; 87: 5341–5354.
Wang FZ, Linde A, Hagglund H, Testa M, Locasciulli A, Ljungman P . Human herpesvirus 6 DNA in cerebrospinal fluid specimens from allogeneic bone marrow transplant patients: does it have clinical significance? Clin Infect Dis 1999; 28: 562–568.
Zerr DM, Ogata M . HHV-6A and HHV-6B in recipients of hematopoietic cell transplantation. In: Flamand L, Lautenschlager I, Krueger G, Ablashi D (eds). Human Herpesviruses HHV-6A, HHV-6B & HHV-7. Diagnosis and Clinical Management 3rd edn. Elsevier: Kidlington, Oxford, UK, 2014 pp 217–234.
Hill AB . The environment and disease: association or causation? Proc R Soc Med 1965; 58: 295–300.
Weed DL . On the use of causal criteria. Int J Epidemiol 1997; 26: 1137–1141.
Zerr DM, Fann JR, Breiger D, Boeckh M, Adler AL, Xie H et al. HHV-6 reactivation and its effect on delirium and cognitive functioning in hematopoietic cell transplantation recipients. Blood 2011; 117: 5243–5249.
Johnston RE, Geretti AM, Prentice HG, Clark AD, Wheeler AC, Potter M et al. HHV-6-related secondary graft failure following allogeneic bone marrow transplantation. Br J Haematol 1999; 105: 1041–1043.
Lagadinou ED, Marangos M, Liga M, Panos G, Tzouvara E, Dimitroulia E et al. Human herpesvirus 6-related pure red cell aplasia, secondary graft failure, and clinical severe immune suppression after allogeneic hematopoietic cell transplantation successfully treated with foscarnet. Transpl Infect Dis 2010; 12: 437–440.
Le Bourgeois A, Labopin M, Guillaume T, Delaunay J, Foucher Y, Tessoulin B et al. Human herpesvirus 6 reactivation before engraftment is strongly predictive of graft failure after double umbilical cord blood allogeneic stem cell transplantation in adults. Exp Hematol 2014; 42: 945–954.
Cone RW, Hackman RC, Huang ML, Bowden RA, Meyers JD, Metcalf M et al. Human herpesvirus 6 in lung tissue from patients with pneumonitis after bone marrow transplantation. N Engl J Med 1993; 329: 156–161.
Nakayama T, Okada F, Ando Y, Honda K, Ogata M, Goto K et al. A case of pneumonitis and encephalitis associated with human herpesvirus 6 (HHV-6) infection after bone marrow transplantation. Br J Radiol 2010; 83: e255–e258.
Amo K, Tanaka-Taya K, Inagi R, Miyagawa H, Miyoshi H, Okusu I et al. Human herpesvirus 6B infection of the large intestine of patients with diarrhea. Clin Infect Dis 2003; 36: 120–123.
Zerr DM, Boeckh M, Delaney C, Martin PJ, Xie H, Adler AL et al. HHV-6 reactivation and associated sequelae after hematopoietic cell transplantation. Biol Blood Marrow Transplant 2012; 18: 1700–1708.
Dulery R, Salleron J, Dewilde A, Rossignol J, Boyle EM, Gay J et al. Early human herpesvirus type 6 reactivation after allogeneic stem cell transplantation: a large-scale clinical study. Biol Blood Marrow Transplant 2012; 18: 1080–1089.
Pellett PE, Ablashi DV, Ambros PF, Agut H, Caserta MT, Descamps V et al. Chromosomally integrated human herpesvirus 6: questions and answers. Rev Med Virol 2012; 22: 144–155.
Leong HN, Tuke PW, Tedder RS, Khanom AB, Eglin RP, Atkinson CE et al. The prevalence of chromosomally integrated human herpesvirus 6 genomes in the blood of UK blood donors. J Med Virol 2007; 79: 45–51.
Hall CB, Caserta MT, Schnabel K, Shelley LM, Marino AS, Carnahan JA et al. Chromosomal integration of human herpesvirus 6 is the major mode of congenital human herpesvirus 6 infection. Pediatrics 2008; 122: 513–520.
Gravel A, Hall CB, Flamand L . Sequence analysis of transplacentally acquired human herpesvirus 6 DNA is consistent with transmission of a chromosomally integrated reactivated virus. J Infect Dis 2013; 207: 1585–1589.
Endo A, Watanabe K, Ohye T, Suzuki K, Matsubara T, Shimizu N et al. Molecular and virological evidence of viral activation from chromosomally integrated human herpesvirus 6A in a patient with X-linked severe combined immunodeficiency. Clin Infect Dis 2014; 59: 545–548.
Hill JA, Sedlak RH, Zerr DM, Huang ML, Yeung C, Myerson D et al. Prevalence of chromosomally integrated human herpesvirus 6 in patients with human herpesvirus 6-central nervous system dysfunction. Biol Blood Marrow Transplant 2015; 21: 371–373.
Lee SO, Brown RA, Razonable RR . Chromosomally integrated human herpesvirus-6 in transplant recipients. Transpl Infect Dis 2012; 14: 346–354.
Clark DA, Nacheva EP, Leong HN, Brazma D, Li YT, Tsao EH et al. Transmission of integrated human herpesvirus 6 through stem cell transplantation: implications for laboratory diagnosis. J Infect Dis 2006; 193: 912–916.
Ward KN, Leong HN, Nacheva EP, Howard J, Atkinson CE, Davies NW et al. Human herpesvirus 6 chromosomal integration in immunocompetent patients results in high levels of viral DNA in blood, sera, and hair follicles. J Clin Microbiol 2006; 44: 1571–1574.
Zerr DM . Human herpesvirus 6 and central nervous system disease in hematopoietic cell transplantation. J Clin Virol 2006; 37: S52–S56.
Muta T, Fukuda T, Harada M . Human herpesvirus-6 encephalitis in hematopoietic SCT recipients in Japan: a retrospective multicenter study. Bone Marrow Transplant 2009; 43: 583–585.
Seeley WW, Marty FM, Holmes TM, Upchurch K, Soiffer RJ, Antin JH et al. Post-transplant acute limbic encephalitis: clinical features and relationship to HHV6. Neurology 2007; 69: 156–165.
Toriumi N, Kobayashi R, Yoshida M, Iguchi A, Sarashina T, Okubo H et al. Risk factors for human herpesvirus 6 reactivation and its relationship with syndrome of inappropriate antidiuretic hormone secretion after stem cell transplantation in pediatric patients. J Pediatr Hematol Oncol 2014; 36: 379–383.
Kawaguchi T, Takeuchi M, Kawajiri C, Abe D, Nagao Y, Yamazaki A et al. Severe hyponatremia caused by syndrome of inappropriate secretion of antidiuretic hormone developed as initial manifestation of human herpesvirus-6-associated acute limbic encephalitis after unrelated bone marrow transplantation. Transpl Infect Dis 2013; 15: E54–E57.
Ogata M, Satou T, Inoue Y, Takano K, Ikebe T, Ando T et al. Foscarnet against human herpesvirus (HHV)-6 reactivation after allo-SCT: breakthrough HHV-6 encephalitis following antiviral prophylaxis. Bone Marrow Transplant 2013; 48: 257–264.
Hill JA, Koo S, Guzman Suarez BB, Ho VT, Cutler C, Koreth J et al. Cord-blood hematopoietic stem cell transplant confers an increased risk for human herpesvirus-6-associated acute limbic encephalitis: a cohort analysis. Biol Blood Marrow Transplant 2012; 18: 1638–1648.
Howell KB, Tiedemann K, Haeusler G, Mackay MT, Kornberg AJ, Freeman JL et al. Symptomatic generalized epilepsy after HHV6 posttransplant acute limbic encephalitis in children. Epilepsia 2012; 53: e122–e126.
Cheng FW, Lee V, Leung WK, Chan PK, Leung TF, Shing MK et al. HHV-6 encephalitis in pediatric unrelated umbilical cord transplantation: a role for ganciclovir prophylaxis? Pediatr Transplant 2010; 14: 483–487.
Bhanushali MJ, Kranick SM, Freeman AF, Cuellar-Rodriguez JM, Battiwalla M, Gea-Banacloche JC et al. Human herpes 6 virus encephalitis complicating allogeneic hematopoietic stem cell transplantation. Neurology 2013; 80: 1494–1500.
Mori T, Mihara A, Yamazaki R, Shimizu T, Aisa Y, Suzuki S et al. Myelitis associated with human herpes virus 6 (HHV-6) after allogeneic cord blood transplantation. Scand J Infect Dis 2007; 39: 276–278.
Mori Y, Miyamoto T, Nagafuji K, Kamezaki K, Yamamoto A, Saito N et al. High incidence of human herpes virus 6-associated encephalitis/myelitis following a second unrelated cord blood transplantation. Biol Blood Marrow Transplant 2010; 16: 1596–1602.
Aoki K, Arima H, Kato A, Hashimoto H, Tabata S, Matsushita A et al. Human herpes virus 6-associated myelitis following allogeneic bone marrow transplantation. Ann Hematol 2012; 91: 1663–1665.
Granerod J, Cunningham R, Zuckerman M, Mutton K, Davies NW, Walsh AL et al. Causality in acute encephalitis: defining aetiologies. Epidemiol Infect 2010; 138: 783–800.
Dewhurst S . Human herpesvirus type 6 and human herpesvirus type 7 infections of the central nervous system. Herpes 2004; 11: 105a–111a.
Ljungman P, de la Camara R, Cordonnier C, Einsele H, Engelhard D, Reusser P et al. Management of CMV, HHV-6, HHV-7 and Kaposi-sarcoma herpesvirus (HHV-8) infections in patients with hematological malignancies and after SCT. Bone Marrow Transplant 2008; 42: 227–240.
Tunkel AR, Glaser CA, Bloch KC, Sejvar JJ, Marra CM, Roos KL et al. The management of encephalitis: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis 2008; 47: 303–327.
Tomblyn M, Chiller T, Einsele H, Gress R, Sepkowitz K, Storek J et al. Guidelines for preventing infectious complications among hematopoietic cell transplantation recipients: a global perspective. Biol Blood Marrow Transplant 2009; 15: 1143–1238.
Fujimaki K, Mori T, Kida A, Tanaka M, Kawai N, Matsushima T et al. Human herpesvirus 6 meningoencephalitis in allogeneic hematopoietic stem cell transplant recipients. Int J Hematol 2006; 84: 432–437.
Hill JA, Boeckh MJ, Sedlak RH, Jerome KR, Zerr DM . Human herpesvirus 6 can be detected in cerebrospinal fluid without associated symptoms after allogeneic hematopoietic cell transplantation. J Clin Virol 2014; 61: 289–292.
Olson AL, Dahi PB, Zheng J, Devlin SM, Lubin M, Gonzales AM et al. Frequent human herpesvirus-6 viremia but low incidence of encephalitis in double-unit cord blood recipients transplanted without antithymocyte globulin. Biol Blood Marrow Transplant 2014; 20: 787–793.
Betts BC, Young JA, Ustun C, Cao Q, Weisdorf DJ . Human herpesvirus 6 infection after hematopoietic cell transplantation: is routine surveillance necessary? Biol Blood Marrow Transplant 2011; 17: 1562–1568.
Jeulin H, Agrinier N, Guery M, Salmon A, Clement L, Bordigoni P et al. Human herpesvirus 6 infection after allogeneic stem cell transplantation: incidence, outcome, and factors associated with HHV-6 reactivation. Transplantation 2013; 95: 1292–1298.
Vu T, Carrum G, Hutton G, Heslop HE, Brenner MK, Kamble R . Human herpesvirus-6 encephalitis following allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant 2007; 39: 705–709.
Sakai R, Kanamori H, Motohashi K, Yamamoto W, Matsuura S, Fujita A et al. Long-term outcome of human herpesvirus-6 encephalitis after allogeneic stem cell transplantation. Biol Blood Marrow Transplant 2011; 17: 1389–1394.
Shimazu Y, Kondo T, Ishikawa T, Yamashita K, Takaori-Kondo A . Human herpesvirus-6 encephalitis during hematopoietic stem cell transplantation leads to poor prognosis. Transpl Infect Dis 2013; 15: 195–201.
Scheurer ME, Pritchett JC, Amirian ES, Zemke NR, Lusso P, Ljungman P . HHV-6 encephalitis in umbilical cord blood transplantation: a systematic review and meta-analysis. Bone Marrow Transplant 2013; 48: 574–580.
Quereda C, Corral I, Laguna F, Valencia ME, Tenorio A, Echeverria JE et al. Diagnostic utility of a multiplex herpesvirus PCR assay performed with cerebrospinal fluid from human immunodeficiency virus-infected patients with neurological disorders. J Clin Microbiol 2000; 38: 3061–3067.
Prasad A, Remick J, Zeichner SL . Activation of human herpesvirus replication by apoptosis. J Virol 2013; 87: 10641–10650.
Tang H, Serada S, Kawabata A, Ota M, Hayashi E, Naka T et al. CD134 is a cellular receptor specific for human herpesvirus-6B entry. Proc Natl Acad Sci USA 2013; 110: 9096–9099.
Gewurz BE, Marty FM, Baden LR, Katz JT . Human herpesvirus 6 encephalitis. Curr Infect Dis Rep 2008; 10: 292–299.
Donati D, Martinelli E, Cassiani-Ingoni R, Ahlqvist J, Hou J, Major EO et al. Variant-specific tropism of human herpesvirus 6 in human astrocytes. J Virol 2005; 79: 9439–9448.
Ahlqvist J, Fotheringham J, Akhyani N, Yao K, Fogdell-Hahn A, Jacobson S . Differential tropism of human herpesvirus 6 (HHV-6) variants and induction of latency by HHV-6A in oligodendrocytes. J Neurovirol 2005; 11: 384–394.
De Filippis L, Foglieni C, Silva S, Vescovi A, Lusso P, Malnati MS . Differentiated human neural stem cells: a new ex vivo model to study HHV-6 infection of the central nervous system. J Clin Virol 2006; 37: S27–S32.
Fotheringham J, Akhyani N, Vortmeyer A, Donati D, Williams E, Oh U et al. Detection of active human herpesvirus-6 infection in the brain: correlation with polymerase chain reaction detection in cerebrospinal fluid. J Infect Dis 2007; 195: 450–454.
Fotheringham J, Williams EL, Akhyani N, Jacobson S . Human herpesvirus 6 (HHV-6) induces dysregulation of glutamate uptake and transporter expression in astrocytes. J Neuroimmune Pharmacol 2008; 3: 105–116.
The Japan Society for Hematopoietic Cell Transplantation (JSHCT) Monograph. 2012; 34 (Japanese). http://www.jshct.com/guideline/pdf/kansenkanri.pdf.
Manichanh C, Grenot P, Gautheret-Dejean A, Debre P, Huraux JM, Agut H . Susceptibility of human herpesvirus 6 to antiviral compounds by flow cytometry analysis. Cytometry 2000; 40: 135–140.
Akesson-Johansson A, Harmenberg J, Wahren B, Linde A . Inhibition of human herpesvirus 6 replication by 9-[4-hydroxy-2-(hydroxymethyl)butyl]guanine (2HM-HBG) and other antiviral compounds. Antimicrob Agents Chemother 1990; 34: 2417–2419.
De Clercq E, Naesens L, De Bolle L, Schols D, Zhang Y, Neyts J . Antiviral agents active against human herpesviruses HHV-6, HHV-7 and HHV-8. Rev Med Virol 2001; 11: 381–395.
Yoshida M, Yamada M, Tsukazaki T, Chatterjee S, Lakeman FD, Nii S et al. Comparison of antiviral compounds against human herpesvirus 6 and 7. Antiviral Res 1998; 40: 73–84.
Raffi F, Taburet AM, Ghaleh B, Huart A, Singlas E . Penetration of foscarnet into cerebrospinal fluid of AIDS patients. Antimicrob Agents Chemother 1993; 37: 1777–1780.
Williams-Aziz SL, Hartline CB, Harden EA, Daily SL, Prichard MN, Kushner NL et al. Comparative activities of lipid esters of cidofovir and cyclic cidofovir against replication of herpesviruses in vitro. Antimicrob Agents Chemother 2005; 49: 3724–3733.
Bonnafous P, Bogaert S, Godet AN, Agut H . HDP-CDV as an alternative for treatment of human herpesvirus-6 infections. J Clin Virol 2013; 56: 175–176.
De Bolle L, Andrei G, Snoeck R, Zhang Y, Van Lommel A, Otto M et al. Potent, selective and cell-mediated inhibition of human herpesvirus 6 at an early stage of viral replication by the non-nucleoside compound CMV423. Biochem Pharmacol 2004; 67: 325–336.
Prichard MN, Williams JD, Komazin-Meredith G, Khan AR, Price NB, Jefferson GM et al. Synthesis and antiviral activities of methylenecyclopropane analogs with 6-alkoxy and 6-alkylthio substitutions that exhibit broad-spectrum antiviral activity against human herpesviruses. Antimicrob Agents Chemother 2013; 57: 3518–3527.
Milbradt J, Auerochs S, Korn K, Marschall M . Sensitivity of human herpesvirus 6 and other human herpesviruses to the broad-spectrum antiinfective drug artesunate. J Clin Virol 2009; 46: 24–28.
Painter W, Robertson A, Trost LC, Godkin S, Lampert B, Painter G . First pharmacokinetic and safety study in humans of the novel lipid antiviral conjugate CMX001, a broad-spectrum oral drug active against double-stranded DNA viruses. Antimicrob Agents Chemother 2012; 56: 2726–2734.
Hakacova N, Klingel K, Kandolf R, Engdahl E, Fogdell-Hahn A, Higgins T . First therapeutic use of Artesunate in treatment of human herpesvirus 6B myocarditis in a child. J Clin Virol 2013; 57: 157–160.
Papadopoulou A, Gerdemann U, Katari UL, Tzannou I, Liu H, Martinez C et al. Activity of broad-spectrum T cells as treatment for AdV, EBV, CMV, BKV, and HHV6 infections after HSCT. Sci Transl Med 2014; 6: 242ra283.
Tischer S, Priesner C, Heuft HG, Goudeva L, Mende W, Barthold M et al. Rapid generation of clinical-grade antiviral T cells: selection of suitable T-cell donors and GMP-compliant manufacturing of antiviral T cells. J Transl Med 2014; 12: 336.
Becerra A, Gibson L, Stern LJ, Calvo-Calle JM . Immune response to HHV-6 and implications for immunotherapy. Curr Opin Virol 2014; 9: 154–161.
Caserta MT, Dewhurst S . Dazed and confused by HHV-6. Blood 2011; 117: 5016–5018.
Ward KN . Child and adult forms of human herpesvirus 6 encephalitis: looking back, looking forward. Curr Opin Neurol 2014; 27: 349–355.
Ishiyama K, Katagiri T, Hoshino T, Yoshida T, Yamaguchi M, Nakao S . Preemptive therapy of human herpesvirus-6 encephalitis with foscarnet sodium for high-risk patients after hematopoietic SCT. Bone Marrow Transplant 2011; 46: 863–869.
Marty FM, Winston DJ, Rowley SD, Vance E, Papanicolaou GA, Mullane KM et al. CMX001 to prevent cytomegalovirus disease in hematopoietic-cell transplantation. N Engl J Med 2013; 369: 1227–1236.
Acknowledgements
This work was supported by Health Labour Science Research grant (Grant Number H26-kakushintekigan-ippan-140).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ogata, M., Fukuda, T. & Teshima, T. Human herpesvirus-6 encephalitis after allogeneic hematopoietic cell transplantation: What we do and do not know. Bone Marrow Transplant 50, 1030–1036 (2015). https://doi.org/10.1038/bmt.2015.76
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2015.76
- Springer Nature Limited
This article is cited by
-
Risk factors and long-term outcomes for human herpesvirus 6 encephalitis in the early period after allogeneic stem cell transplantation
Bone Marrow Transplantation (2024)
-
The preceding hyponatremia is a useful hallmark for the diagnosis of HHV-6 encephalitis after allogeneic hematopoietic stem cell transplantation
Bone Marrow Transplantation (2023)
-
Human seminal virome: a panel based on recent literature
Basic and Clinical Andrology (2022)
-
Differentiating central nervous system infection from disease infiltration in hematological malignancy
Scientific Reports (2022)
-
Clinical and microbiological characteristics of bacterial meningitis in umbilical cord blood transplantation recipients
International Journal of Hematology (2022)