Abstract
Relapse is the major cause of treatment failure after allogeneic hematopoietic cell transplantation (alloHCT) for acute leukemia and myelodysplastic syndrome (MDS). Wilms' tumor Ag (WT1) is overexpressed in the majority of acute leukemia and MDS patients and has been proposed as a universal diagnostic marker for detection of impending relapse. Comprehensive studies have shown that WT1 transcript levels have predictive value in acute leukemia patients in CR after chemotherapy. However, the focus of this study is the period after alloHCT for predicting relapse onset. We analyzed the accumulation of WT1 mRNA transcripts in PB of 82 leukemia and MDS patients and defined specific molecular ratios for relapse prediction. The extensively validated WT1/c-ABL ratio was used to normalize increases in WT1 transcript levels. The observed lead time of crossing or exceeding set WT1 levels is presented along with linear interpolation to estimate the calculated day the WT1 thresholds were crossed. The WT1/c-ABL transcript ratio of 50 or above yielded 100% specificity and 75% sensitivity reliably predicting future relapse with an observed average of 29.4 days (s.d.=19.8) and a calculated average of 63 days (s.d.=29.3) lead time before morphologic confirmation. A lower ratio of 20 or above gave lower specificity, but higher sensitivity (84.8% and 87.5%, respectively) identified more patients who relapsed, at earlier times, providing an earlier warning with actual average lead time of 49.1 days (s.d.=30.8) and calculated average of 78 days (s.d.=28.8). WT1 transcript levels serve as a diagnostic relapse test with greater sensitivity than the morphologic approach used in the clinic as a readout.
Similar content being viewed by others
Introduction
Allogeneic hematopoietic cell transplantation (alloHCT) is the intensive but optimal therapy for higher risk acute types of leukemia (AML, ALL, CML in accelerated phase (AP) or blast crisis (BC)) and myelodysplastic syndrome (MDS) patients. However, relapse is still a frequent cause of treatment failure, although intervention before overt relapse may be beneficial.1, 2, 3, 4 Approximately 35–45% of alloHCT recipients will relapse within 5 years with their original malignancy.5 Technologic advances produced sensitive methods for early recognition of hematologic malignancy relapse. The highest sensitivity is achievable by PCR-based assays detecting recurrent molecular aberrations such as fusion transcripts and mutations. However, not all leukemia and MDS patients have aberrations detectable by PCR, limiting the applicability of such monitoring to only some patient subgroups. In contrast, non-mutated WT1 is overexpressed (5–10 times above background levels) in ⩾86% of patients with AML, MDS and ALL6, 7, 8, 9, 10 and could serve as a universal diagnostic marker for detection of leukemic blasts, despite heterogeneity in the etiology of these diseases. Since 1990, several groups have associated WT1 expression and its elevation with progression and relapse of hematologic malignancies.2,8,10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25 While existing literature established the relevance of WT1 for identifying future relapse,2,8,10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25 the WT1 test has not yet been validated as a relapse definition across relevant hematologic malignancies.
In a prospective study, we longitudinally evaluated the accumulation of WT1 mRNA transcripts in PB of alloHCT recipients to establish levels of WT1 transcripts (WT1 ratios) that will accurately predict the onset of relapse and to estimate a time interval from molecular (quantitative PCR of WT1) to hematologic (morphology of blasts) relapse.
Materials and methods
Study subjects
This study was conducted under City of Hope IRB-approved protocol no. 09050. Patients gave written informed consent, in accordance with the Declaration of Helsinki, for laboratory-based studies on PB samples obtained prospectively after alloHCT monthly for 6 months, and then alternating between 1 or 2 months until day 780. Patients over 18 years of age with confirmed diagnosis of MDS, AML, ALL and CML undergoing alloHCT at City of Hope after reaching CR (MDS with ⩽20% blasts, AML or ALL in morphologic remission (first or subsequent remission) or CML in chronic phase) were eligible for the study and were enrolled prospectively. Confirmed diagnosis of hematologic relapse, monitored prospectively, was defined as a study end point. Thus, patients who relapsed became ineligible to continue participation in the study.
Cells, RNA purification and cDNA synthesis
PBMCs and BM mononuclear cells were purified by Ficoll-Hypaque density gradient centrifugation from 10 to 40 ml PB or BM. Subsequently, total RNA was isolated from 3 to 5 million PBMCs or BM mononuclear cells using RNeasy (Qiagen, Valencia, CA, USA). cDNA was made from 500 ng of total RNA using the RevertAid First Strand cDNA Synthesis Kit (Fermentas Inc., Glen Burnie, MD, USA). RNA quality was measured by NanoVue (GE Healthcare, Little Chalfont, Buckinghamshire, UK) and its purity was based on its 260/280 ratio.
Quantitative real-time PCR analysis
WT1 transcript levels in PBMCs and BM mononuclear cells were measured in a batch using SYBR Green quantitative real-time PCR (qRT-PCR) on the ABI7300 instrument (Applied Biosystems, Carlsbad, CA, USA). c-ABL gene transcript was used as a recommended internal control.13,21,26 Absolute quantification of the transcript copy number was achieved for WT1 and c-ABL genes from the corresponding standard curves enabled by WT1 and c-ABL control genes cloned into plasmids. Plasmid dilutions were generated to span the anticipated transcript copy range (101–106 copies). For WT110 and c-ABL,26 published sequences were used to generate 89 and 96 bp products, respectively. Results were expressed as a ratio of WT1/c-ABL transcript copy numbers normalized by 104 (WT1 ratio: WT1/c-ABLx104).7,27,28 RNA from control positive cell line K562 served as a positive control. Results showing a >1 cycle deviation from the threshold cycle number (Ct) between duplicate wells were repeated. If the ratio was inconsistent or if two wells were dissimilar, sample testing was repeated. If ratios were still inconsistent or dissimilar after repeat, the data point(s) were excluded from the analyses. Samples containing <1000 copies of c-ABL were considered degraded and new cDNA was generated. Results were not released to the treating physicians and did not influence their clinical practice.
Statistical analysis
WT1 mRNA transcript levels of consented patients with at least two PB draws after alloHCT were analyzed. We evaluated longitudinal changes in transcript levels to establish WT1 thresholds that would be likely to indicate impending relapse. We identified patients having WT1 ratios exceeding these thresholds and then determined the sensitivity, specificity, negative predictive value (NPV) and positive predictive value (PPV) of subsequent relapse. Exact 95% binomial confidence intervals (CIs) were calculated for sensitivities and specificities. Means and s.d.'s for lead time were calculated based on the earliest observed post-alloHCT day on which the patient’s WT1 ratio was greater than or equal to the threshold. To estimate the day on which the patient’s WT1 ratio was equal to the threshold, we used linear interpolation. In other words, we calculated the line between the last measure before crossing the threshold and the first measure greater than the threshold and estimated the day that the threshold was crossed. Cox proportional hazard regression models were used to examine the predictors of time to relapse (days) by univariate and multivariate analysis tools. The predictors included crossing the WT1 ratio of 20 (time dependent, dichotomous: whether or not each WT1 ratio exceeded the 20 ratio), age at transplant (above or below median), patient gender, patient/donor sex match (male/female, others), donor age (above or below median), disease type (AML, ALL/CML, MDS), donor type (related, matched unrelated), stem cell source (BM, PB, cord blood), pre-alloHCT CMV serostatus (negative, positive), donor pre-alloHCT CMV serostatus (negative, positive), disease risk status at transplantation (low, high), conditioning regimen (full intensity, reduced intensity), injected cell dose, acute GVHD grade (none or grade 1, grades 2–4), log-transformed pre-alloHCT WT1 ratio and CMV reactivation within 3 months (yes, no). Crossing the WT1 ratio of 50 (time dependent, dichotomous: whether or not each WT1 measure exceeded the 50 threshold) was not considered as a variable in the survival analyses because of its 100% specificity (i.e., patients who did not relapse never had WT1 ratio ⩾50). The multivariate analysis used stepwise regression on the variables that were significant in the univariate analyses. In a secondary analysis, we examined WT1 ratio and the interaction of the WT1 ratio with risk in a Cox proportional hazards model as predictors of time to relapse. We also examined a Cox proportional hazards model with post-alloHCT WT1 ratio and log-transformed pre-alloHCT WT1 ratio as predictors of time to relapse. To test the reliability of the WT1 ratio using PB, we analyzed the association of post-alloHCT WT1 transcript levels measured on PB and BM using a repeated-measures regression model. We also analyzed the association of the PB post-alloHCT WT1 ratio with bcr/abl using a repeated-measures regression model. The bcr/abl data were only available in the subset of Ph+ ALL and CML patients. As we could not derive a correlation coefficient from the output of the repeated-measures model, we converted the PB and BM WT1 ratios and bcr/abl measurements into z-scores and used this standardized coefficient as a proxy for the correlation coefficient. Exact binomial 95% CIs were calculated using StatXact 7. SAS version 9.3 (SAS Institute, Cary, NC, USA) was used to perform all other statistical analyses. The statistical significance level was set at α=0.05. R 3.0.1 was used to generate the figures.
Results
The WT1 transcript ratio level as a highly specific predictor of relapse
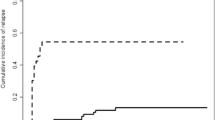
We measured the rate of change of WT1 ratio levels (WT1 assay) as a means to assess molecular relapse and a predictor of clinical relapse. WT1 transcript ratio levels were measured longitudinally in 82 AML, ALL, MDS and CML patients after alloHCT. The median follow-up was 295.5 days (range 57–785). Patient demographic and transplantation characteristics, alloHCT outcomes and the number of samples obtained per patient are summarized in Table 1. Fifty patients were considered as low risk for disease (AML CR1, n=25; ALL CR1, n=18; MDS RA or RARS, n=6; or CML CP1, n=1), whereas the remaining 32 patients were at high risk for disease (AML CR2/3, n=14; ALL CR2/3, n=6; MDS RAEB or RAEBT, n=10; or CML CP2, n=2). Cytogenetic risks for each disease are also detailed in Table 1. As expected in the transplant cohort, many had intermediate- or high-risk cytogenetics. Among 18 AML patients with normal cytogenetics, Flt3 mutation status was available in nine patients (five positive, four negative). The longitudinal patterns of WT1 ratio levels after alloHCT for patients who did not relapse (n=66) are depicted in Figure 1. A reference line was generated and fit to the data retrospectively at the WT1 ratio of 50, because it is the minimum WT1 ratio level that none of the non-relapsed patients exceeded. This level defines maximum specificity of 100% (95% binomial exact CI: 94.5–100) and can be considered a highly specific threshold level for relapse prediction. Figure 2 shows the WT1 ratios vs time for the 16 relapsed patients increased longitudinally. As opposed to Figure 1, which shows all patients in one plot, Figure 2 has individual panels for each patient so that each patient trend could be separately assessed. A reference line is drawn at WT1 ratio equal to 50 (towards the bottom of the plot) to quantitate how many relapsed patients had WT1 ratios that exceeded this highly specific threshold. Within each panel, the relapse day (number of days after alloHCT) and the patient’s last two WT1 ratio measurements and the number of days before relapse in which they were taken (R-day) are provided. For example, in the case of patient 1, R-74 means 74 days before relapse on day 747 after alloHCT. Four patients (patients 13–16 in Figure 2) never had a WT1 ratio exceeding 50, whereas the remaining 12 patients (12/16) had WT1 levels that exceeded the ratio of 50, providing a sensitivity of 75% for this ratio level (95% binomial exact CI: 48–93). The PPV and the NPV performance parameters for the WT1 ratio of 50 were 100% and 94.4%, respectively. The average number of days between the earliest observed time of crossing the WT1 ratio threshold of 50 to relapse for 12 patients depicted in Figure 2 was 29.4 (s.d.=19.8). Using the linear interpolation method, the average estimated day of crossing the WT1 ratio of 50 threshold was 63 days (s.d.=29.3). Thus, the WT1 ratio of 50 is a specific threshold for detection of impending hematologic relapse after alloHCT with an estimated 63 days before diagnosis of morphologic relapse.
WT1 levels in non-relapsed acute leukemia and MDS patients after alloHCT. WT1 transcript levels were measured by qRT-PCR in 82 patients and expressed as a ratio of WT1/c-ABL transcript copy numbers normalized by 104 (WT1 ratio). Patients without relapse did not cross the WT1 ratio of 50 illustrated by the horizontal solid line (66/66, 100% specificity).
Time course of WT1 transcript expression levels in acute leukemia and MDS patients (N=16) with relapse after alloHCT. WT1 transcript levels measured by qRT-PCR and expressed as ratios (as in Figure 1) are shown for relapsed patients after alloHCT. Disease diagnosis of each patient is indicated in each individual panel. WT1 ratios crossed the level of 50 (horizontal solid line) and began to increase exponentially in 12 of 16 patients (12/16, 75% sensitivity). The relapse day and the patient’s last two WT1 ratio measurements and the day before relapse in which they were taken are provided (R-day). The y-axis WT1 ratio range for this plot is much larger than that for Figure 1 to accommodate the high levels of WT1 ratios these relapsed patients reached.
Varying WT1 ratio thresholds for relapse prediction
Using the WT1 ratio of 50 as a threshold for detection of impending relapse yielded 100% specificity (all non-relapsed patients never had WT1 levels reaching this threshold) and 75% sensitivity (three-quarters of patients who relapsed had reached WT1 levels exceeding this threshold). We further assessed lower WT1 ratios to increase sensitivity and capture more patients with impending relapse while only minimally reducing specificity. Table 2 shows numbers of relapsed and non-relapsed patients with varying WT1 levels, together with sensitivity, specificity, PPV and NPV. Means and s.d.'s of the calculated time to relapse from the patient’s earliest time of having a WT1 level equal to the given threshold are also shown. The thresholds of 40 and 30 decrease the specificity but do not increase sensitivity. Sensitivity increased to 87.5% using a WT1 ratio threshold of 20, whereas the specificity decreased to 84.8% as expected because of slightly increased number of false positives. Although, using a threshold of 10, the sensitivity becomes >90%, and the specificity is reduced to ~56.1%. Thus, the lower WT1 ratio threshold of 20 provides an improved sensitivity and specificity combination for relapse prediction and longer duration before morphologic relapse. Specifically, the observed time of patients’ earliest WT1 ratio exceeding the threshold of 20 and the onset of relapse increased to 49.1 days (s.d.=30.8). Using the linear interpolation method, patients crossed the WT1 ratio threshold of 20 by an average of 78 days (s.d.=28.8) before relapse diagnosis. Consequently, using a lower WT1 ratio threshold of 20 will improve the sensitivity and specificity combination and increase the time to relapse interval, without having excessive false positives.
Approaches to reduce false-positive cases
Using a lower WT1 ratio threshold (20 vs 50) increases sensitivity of detecting patients with impending relapse. However, as a negative consequence, the PPV decreases, thereby increasing the number of false-positive patients who never relapse. The highly specific WT1 ratio threshold of 50 had a PPV of 100% (no false positives detected) and the WT1 ratio threshold of 20 resulted in a decreased PPV of 58.3% with 10 false-positive patients. The absolute number of patients falsely identified as likely to relapse will be dependent on the cohort demographics. The proportion of patients with positive test results for the WT1 threshold of 20 that are going to have a disease relapse (PPV) may improve if we target the test to the patients clinically at higher risk of developing relapse. We evaluated the high-risk group (defined as AML and ALL in CR2/3, CML in CP2 or AP and MDS RAEB or RAEBT; see Table 1) and found that the PPV of the WT1 ratio of 20 improved to 69.2% in the high-risk patients (Table 3) compared with 58.3% for the entire cohort (Table 2). The sensitivity and specificity of the WT1 ratio of 20 for high-risk patients is comparable to those of the whole cohort using the ratio of 20. Additionally, the average time to relapse interval is longer for high-risk patients (58.1 days, s.d.=34.9; Table 3) than for the entire cohort (49.1 days, s.d.=30.8; Table 2). Thus, the lower WT1 ratio of 20 appears to be more valuable for this specific subgroup of patients with a higher prevalence of relapsed disease (11 relapsed patients in the high-risk group vs 5 in the low-risk group), which reduces the number of false-positive cases improving the PPV.
Subgroup analyses of each disease category
We also assessed the sensitivity and specificity of the WT1 ratio for disease type (AML, ALL/CML, MDS). First, there was no significant association between each disease category and relapse (χ2 P=0.3409) or time to relapse (Cox proportional hazards model P=0.3177). Consistent with the analysis of the entire cohort, sensitivity and specificity was found to be optimized using the WT1 ratio of 20 for each disease category. Crossing the WT1 ratio of 20 was associated with the sensitivities of 90% for AML, 66.7% for ALL/CML and 100% for MDS. Specificities were 86.2% for AML, 83.3% for ALL/CML and 84.6% for MDS. The average time of crossing the WT1 ratio of 20 to the onset of relapse was 50.8 days (s.d.=31.6 days) in AML, 51.5 days (s.d.=19.1 days) in ALL/CML and 42.3 days (s.d.=43.6 days) in MDS. Thus, compared with the results of the entire cohort (Table 2), the WT1 ratio provided a better sensitivity in AML and MDS patients, whereas better specificity was found for AML patients.
Model of relapse prediction using consecutive pairs of WT1 measurements
To improve the PPV rate without sacrificing sensitivity and specificity, we evaluated WT1 ratio thresholds using multiple measurements as opposed to just one WT1 ratio measurement using patient data shown in Figure 2. We evaluated patients’ consecutive pairs of measurements (immediately following each other by date of acquisition) by identifying increases in WT1 ratio levels from consecutive samples and identified patients whose WT1 ratio levels had a sum greater than or equal to a threshold of 30. With this method, the PPV of detecting impending relapse increases to 73.7% with five false-positive patients. This is an improvement over the 10 false positives found when using the single measurement WT1 ratio threshold of 20. With this method, sensitivity remained at 87.5% with 14 of the 16 patients shown in Figure 2 having two consecutive WT1 ratio measurements that totaled >30. For the 14 patients, the average time to relapse from the day when the patient’s second WT1 measurement totaled 30 was 41.8 days (s.d.=27.1).
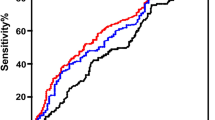
WT1 expression as a significant and independent predictor of time to relapse
We used Cox proportional hazard regression models to identify risk factors predicting time to relapse in a survival analysis. Potential predictors of time to relapse were first examined individually in univariate Cox regression models. Table 4 lists the predictors that were found to be significant in the univariate Cox models (see Materials and methods section for the complete list of variables analyzed). Crossing the WT1 ratio of 20 (hazard ratio (HR)=58.16, P<0.0001), having high disease risk at transplantation (HR=3.27 P=0.0232) or receiving alloHCT from donors with age above the median age of 34 (HR=5.124, P=0.0109) were found to significantly increase hazard or decrease time to relapse in the univariate analysis. We used stepwise regression analysis to find that crossing the WT1 ratio of 20 was the only predictor independent of other variables significantly associated with decreased time to relapse (HR=58.16, P<0.0001; Table 4).
Our secondary analysis examines WT1 ratio, risk and the interaction of the WT1 ratio and risk as predictors of time to relapse. The interaction of the WT1 ratio and risk was significant (P=0.0141), indicating that the WT1 ratio has a different effect on time to relapse in each risk group. The HR in the high-risk group is NS, indicating that the WT1 ratio does not have an effect on time to relapse (HR=1.428, P=0.7417); however, the hazard ratio in the low-risk group is significant (HR: 1.007; P=0.0005). In another Cox model with WT1 ratio and log-transformed pre-alloHCT WT1 ratio as predictors of time to relapse, only the WT1 ratio was significant, but the log-transformed pre-alloHCT WT1 ratio was NS (data not shown).
Relationship of transcript levels of WT1 in PB and BM and association with bcr/abl
To further characterize the performance of WT1 expression as a minimal residual disease (MRD) marker, we studied the association of WT1 expression levels in PB and BM specimens. There were a total of 107 time points where both PB and BM samples were available in 61 subjects. We observed a strong positive association between PB and BM WT1 expression levels using the repeated-measures regression model (standardized coefficient=0.9311, P<0.0001). In addition, we examined the association of WT1 with the clinically available bcr/abl transcript levels of the 15 Ph+ ALL and CML patients (75 time points). There was a strong positive association between WT1 and bcr/abl positivity (standardized coefficient=0.6799, P<0.0001). These results emphasize the reliability and validity of measurement of WT1 transcripts for MRD monitoring and relapse prediction.
Discussion
Our prospective study expands on earlier observations evaluating WT1 as a marker for relapse detection in leukemia and MDS patients.2,4,7,11,12,18,20,22,23,29, 30, 31, 32, 33, 34, 35, 36, 37 In contrast to previous studies, all of the enrolled patients were adults (no pediatric patients) undergoing alloHCT after achieving CR. Our approach combines biologic measurement with statistical analytic tools to define quantitatively predictive thresholds for the onset of relapse based on a large and uniform cohort of patients. Assessment of predictive value of WT1 mRNA transcript quantitation was based on sequential measurements by qRT-PCR, an established method.38 An additional advantage to our approach is the sole use of patient PB specimens for measurements rather than relying on the more difficult to obtain BM biopsy specimen used in many previous studies.2,4,18,20,22,24,29,35, 36, 37,39,40
The long-term prognosis for patients with acute leukemia and MDS who relapse after alloHCT is very poor, with median survival of ⩽6 months, with only 25% having longer survival.41 The usefulness of our approach is its capacity to reliably predict a 29-day (or a 63-day interval estimated by interpolation) interval of relapse detection from crossing the WT1 ratio of 50, a relatively low ratio. While our methods provide an estimation of risk, given the relation between disease burden and outcome, achieving a 63-day lead time before morphologic relapse has potential clinical benefits as treatment regimens can be implemented or altered, such as immunotherapeutics targeting WT142,43 while the tumor burden is low.44, 45, 46
The conventional relapse definition is based on BM having >5% blasts on morphologic exam. This approach has major limitations as follows: (1) it is not quantitative; (2) it is incapable of detecting or predicting impending relapse; (3) and it is dependent on BM sampling requiring patients to undergo invasive procedures that have greater risk compared with PB draws. Our study, similar to others published in the past decade, relied on less-invasive PB sampling to obtain quantitative PCR data for longitudinal analysis of WT1 transcripts.7,16,17,23,25,31, 32, 33, 34,47,48 Based on a comparison of the timing of conventional morphologic tests that only alert retrospectively if relapse has already occurred, the WT1 test offers superior prediction of relapse, because of its ability to uncover an earlier step in the 'evolution' of relapse.
We acknowledge that there are published reports on the association of WT1 and future relapse. However, many studies have not developed a predictive model for relapse using statistical algorithms,10,25,33, 34, 35, 36, 37,47, 48, 49 use incomplete longitudinal data or have limited clinical relevance because of BM sampling or selection of patients from inhomogeneous cohorts (in terms of therapy, remission status before alloHCT and age).2, 3, 4,31 While an early study derived a 40-day post-transplant prediction window, the underlying data that were used to generate the longitudinal analysis were incomplete and specificity was not calculated.2 Other studies used either cross-sectional or longitudinal measurements to analyze a few representative patients to derive a prediction window that is not well validated for clinical translation.20,22
Several studies have been informative and bolster our initiative, without duplication. A representative example was a study using diverse patient subgroups with acute leukemia that derived a rough estimation of prediction intervals based on a small cohort of relapses, with a minority of patients receiving allo- or autotransplant dependent on age at presentation.16 However, as the data measurements were not at comparable intervals for all patients, extracting a uniform predictive algorithm was not the objective as it was in our study. An exhaustive longitudinal study of AML patients having CR without transplant showed that WT1 transcript levels could be used as a predictive test, yet PB was far less sensitive than BM as a cell source for measurement.32 The comprehensive study sponsored by a European-wide consortium was optimally conducted, and also focused on chemotherapy-treated patients who did not receive alloHCT.7 Interestingly, our proposed WT1 ratio level of 50 as an important threshold is consistent with this large European study.7 The conclusion from all of this work is that a framework exists for using WT1 for diagnosing MRD or confirming relapse, but its use as a prognostic tool has not been fully developed. Our prospective post-HCT cohort study is a valuable addition that could be further refined and generalized for all acute leukemia patients who are at high risk of relapse, despite receiving an alloHCT.50
Our data demonstrated that when the WT1 test is at a ratio of 50, it can serve as a clinically relevant reference value imparting a clear biologic meaning as a biomarker identifying all patients who crossed this ratio as being at risk for impending relapse (PPV=100%). However, it failed to identify 25% of patients who relapsed without crossing this ratio (75% sensitivity). Our investigation seeking a stronger sensitivity level and thus a less stringent lower ratio aimed to enhance the value of the WT1 test by broadening the patient population whose relapse could be better predicted than by the highly specific WT1 ratio of 50. Even with a risk of false positives (15% for the WT1 ratio of 20), an increased sensitivity because of the identification of additional patients with impending relapse may be valuable, especially if less toxic therapies (i.e., histone deacetylase inhibitors, hypomethylating agents, proteasome inhibitors, monoclonal antibodies, bispecific antibodies) were an option to reduce risk of future relapse.51,52 Lower ratios also lead to an earlier detection of relapse, when the disease burden is minimal and therapeutic options are most effective.44, 45, 46
In summary, because of its greater sensitivity the WT1 molecular assay is an alternative to the conventional morphologic approach of enumerating blasts. Ours is the first prospective study of WT1 transcript kinetics in alloHCT recipients that establishes an observed time interval between molecular and hematologic relapse based on longitudinal analysis of data from patient blood specimens. The recognition that a WT1 measurement above a highly specific ratio is an unambiguous indicator of relapse enables the implementation of early interventional therapies. It can also guide mechanistically oriented early-phase clinical research, as it provides an earlier definition of patient clinical status. The objective is to apply WT1 transcript measurements as a diagnostic biomarker for detection of relapse in the highest risk individuals—acute leukemia and MDS patients undergoing alloHCT. Our study design could be easily replicated at other centers to confirm that WT1 is a clinically useful biomarker of relapse after alloHCT that will guide treatment decisions for such patients.
References
Bader P, Klingebiel T, Schaudt A, Theurer-Mainka U, Handgretinger R, Lang P et al. Prevention of relapse in pediatric patients with acute leukemias and MDS after allogeneic SCT by early immunotherapy initiated on the basis of increasing mixed chimerism: a single center experience of 12 children. Leukemia 1999; 13: 2079–2086.
Ogawa H, Tamaki H, Ikegame K, Soma T, Kawakami M, Tsuboi A et al. The usefulness of monitoring WT1 gene transcripts for the prediction and management of relapse following allogeneic stem cell transplantation in acute type leukemia. Blood 2003; 101: 1698–1704.
Zhao XS, Jin S, Zhu HH, Xu LP, Liu DH, Chen H et al. Wilms' tumor gene 1 expression: an independent acute leukemia prognostic indicator following allogeneic hematopoietic SCT. Bone Marrow Transplant 2012; 47: 499–507.
Pozzi S, Geroldi S, Tedone E, Luchetti S, Grasso R, Colombo N et al. Leukaemia relapse after allogeneic transplants for acute myeloid leukaemia: predictive role of WT1 expression. Br J Haematol 2013; 160: 503–509.
Pasquini MC, Wang D Current use and outcome of hematopoietic stem cell transplantation: CIBMTR summary slides. 2012 Available at: http://www.cibmtr.org.
Kern W, Schoch C, Haferlach T, Schnittger S Monitoring of minimal residual disease in acute myeloid leukemia. Crit Rev Oncol Hematol 2005; 56: 283–309.
Cilloni D, Renneville A, Hermitte F, Hills RK, Daly S, Jovanovic JV et al. Real-time quantitative polymerase chain reaction detection of minimal residual disease by standardized WT1 assay to enhance risk stratification in acute myeloid leukemia: a European LeukemiaNet study. J Clin Oncol 2009; 27: 5195–5201.
Cilloni D, Saglio G WT1 as a universal marker for minimal residual disease detection and quantification in myeloid leukemias and in myelodysplastic syndrome. Acta Haematol 2004; 112: 79–84.
Keilholz U, Menssen HD, Gaiger A, Menke A, Oji Y, Oka Y et al. Wilms' tumour gene 1 (WT1) in human neoplasia. Leukemia 2005; 19: 1318–1323.
Ostergaard M, Olesen LH, Hasle H, Kjeldsen E, Hokland P WT1 gene expression: an excellent tool for monitoring minimal residual disease in 70% of acute myeloid leukaemia patients—results from a single-centre study. Br J Haematol 2004; 125: 590–600.
Yan CH, Liu DH, Liu KY, Xu LP, Liu YR, Chen H et al. Risk stratification-directed donor lymphocyte infusion could reduce relapse of standard-risk acute leukemia patients after allogeneic hematopoietic stem cell transplantation. Blood 2012; 119: 3256–3262.
Hourigan CS, Karp JE Minimal residual disease in acute myeloid leukaemia. Nat Rev Clin,. Oncol 2013; 10: 460–471.
Cilloni D, Gottardi E, De Micheli D, Serra A, Volpe G, Messa F et al. Quantitative assessment of WT1 expression by real time quantitative PCR may be a useful tool for monitoring minimal residual disease in acute leukemia patients. Leukemia 2002; 16: 2115–2121.
Inoue K, Sugiyama H, Ogawa H, Nakagawa M, Yamagami T, Miwa H et al. WT1 as a new prognostic factor and a new marker for the detection of minimal residual disease in acute leukemia. Blood 1994; 84: 3071–3079.
Tamaki H, Ogawa H, Ohyashiki K, Ohyashiki JH, Iwama H, Inoue K et al. The Wilms' tumor gene WT1 is a good marker for diagnosis of disease progression of myelodysplastic syndromes. Leukemia 1999; 13: 393–399.
Garg M, Moore H, Tobal K, Liu Yin JA Prognostic significance of quantitative analysis of WT1 gene transcripts by competitive reverse transcription polymerase chain reaction in acute leukaemia. Br J Haematol 2003; 123: 49–59.
Inoue K, Ogawa H, Yamagami T, Soma T, Tani Y, Tatekawa T et al. Long-term follow-up of minimal residual disease in leukemia patients by monitoring WT1 (Wilms tumor gene) expression levels. Blood 1996; 88: 2267–2278.
Lapillonne H, Renneville A, Auvrignon A, Flamant C, Blaise A, Perot C et al. High WT1 expression after induction therapy predicts high risk of relapse and death in pediatric acute myeloid leukemia. J Clin Oncol 2006; 24: 1507–1515.
Trka J, Kalinova M, Hrusak O, Zuna J, Krejci O, Madzo J et al. Real-time quantitative PCR detection of WT1 gene expression in children with AML: prognostic significance, correlation with disease status and residual disease detection by flow cytometry. Leukemia 2002; 16: 1381–1389.
Weisser M, Kern W, Rauhut S, Schoch C, Hiddemann W, Haferlach T et al. Prognostic impact of RT-PCR-based quantification of WT1 gene expression during MRD monitoring of acute myeloid leukemia. Leukemia 2005; 19: 1416–1423.
Candoni A, Tiribelli M, Toffoletti E, Cilloni D, Chiarvesio A, Michelutti A et al. Quantitative assessment of WT1 gene expression after allogeneic stem cell transplantation is a useful tool for monitoring minimal residual disease in acute myeloid leukemia. Eur J Haematol 2009; 82: 61–68.
Candoni A, Toffoletti E, Gallina R, Simeone E, Chiozzotto M, Volpetti S et al. Monitoring of minimal residual disease by quantitative WT1 gene expression following reduced intensity conditioning allogeneic stem cell transplantation in acute myeloid leukemia. Clin Transplant 2011; 25: 308–316.
Miyawaki S, Hatsumi N, Tamaki T, Naoe T, Ozawa K, Kitamura K et al. Prognostic potential of detection of WT1 mRNA level in peripheral blood in adult acute myeloid leukemia. Leuk Lymphoma 2010; 51: 1855–1861.
Bergmann L, Miething C, Maurer U, Brieger J, Karakas T, Weidmann E et al. High levels of Wilms' tumor gene (wt1) mRNA in acute myeloid leukemias are associated with a worse long-term outcome. Blood 1997; 90: 1217–1225.
Gray JX, McMillen L, Mollee P, Paul S, Lane S, Bird R et al. WT1 expression as a marker of minimal residual disease predicts outcome in acute myeloid leukemia when measured post-consolidation. Leuk Res 2012; 36: 453–458.
Beillard E, Pallisgaard N, van dV V, Bi W, Dee R, van der SE et al. Evaluation of candidate control genes for diagnosis and residual disease detection in leukemic patients using 'real-time' quantitative reverse-transcriptase polymerase chain reaction (RQ-PCR) - a Europe against cancer program. Leukemia 2003; 17: 2474–2486.
Kroger N, Bacher U, Bader P, Bottcher S, Borowitz MJ, Dreger P et al. NCI First International Workshop on the Biology, Prevention, and Treatment of Relapse after Allogeneic Hematopoietic Stem Cell Transplantation: report from the Committee on Disease-Specific Methods and Strategies for Monitoring Relapse following Allogeneic Stem Cell Transplantation. Part I: methods, acute leukemias, and myelodysplastic syndromes. Biol Blood Marrow Transplant 2010; 16: 1187–1211.
Willasch AM, Gruhn B, Coliva T, Kalinova M, Schneider G, Kreyenberg H et al. Standardization of WT1 mRNA quantitation for minimal residual disease monitoring in childhood AML and implications of WT1 gene mutations: a European multicenter study. Leukemia 2009; 23: 1472–1479.
Qin YZ, Zhu HH, Liu YR, Wang YZ, Shi HX, Lai YY et al. PRAME and WT1 transcripts constitute a good molecular marker combination for monitoring minimal residual disease in myelodysplastic syndromes. Leuk Lymphoma 2013; 54: 1442–1449.
Rossi G, Minervini MM, Carella AM, de Waure C, di Nardo F, Melillo L et al. Comparison between multiparameter flow cytometry and WT1-RNA quantification in monitoring minimal residual disease in acute myeloid leukemia without specific molecular targets. Leuk Res 2012; 36: 401–406.
Lange T, Hubmann M, Burkhardt R, Franke GN, Cross M, Scholz M et al. Monitoring of WT1 expression in PB and CD34(+) donor chimerism of BM predicts early relapse in AML and MDS patients after hematopoietic cell transplantation with reduced-intensity conditioning. Leukemia 2011; 25: 498–505.
Ommen HB, Nyvold CG, Braendstrup K, Andersen BL, Ommen IB, Hasle H et al. Relapse prediction in acute myeloid leukaemia patients in complete remission using WT1 as a molecular marker: development of a mathematical model to predict time from molecular to clinical relapse and define optimal sampling intervals. Br J Haematol 2008; 141: 782–791.
Yamauchi T, Negoro E, Lee S, Takai M, Matsuda Y, Takagi K et al. Detectable Wilms' tumor-1 transcription at treatment completion is associated with poor prognosis of acute myeloid leukemia: a single institution's experience. Anticancer Res 2013; 33: 3335–3340.
Polak J, Hajkova H, Haskovec C, Cechova H, Marinov I, Mikulenkova D et al. Quantitative monitoring of WT1 expression in peripheral blood before and after allogeneic stem cell transplantation for acute myeloid leukemia—a useful tool for early detection of minimal residual disease. Neoplasma 2013; 60: 74–82.
Zhao XS, Yan CH, Liu DH, Xu LP, Liu YR, Liu KY et al. Combined use of WT1 and flow cytometry monitoring can promote sensitivity of predicting relapse after allogeneic HSCT without affecting specificity. Ann Hematol 2013; 92: 1111–1119.
Yoon JH, Kim HJ, Shin SH, Yahng SA, Lee SE, Cho BS et al. BAALC and WT1 expressions from diagnosis to hematopoietic stem cell transplantation: consecutive monitoring in adult patients with core-binding-factor-positive AML. Eur J Haematol 2013; 91: 112–121.
Nomdedeu JF, Hoyos M, Carricondo M, Bussaglia E, Estivill C, Esteve J et al. Bone marrow WT1 levels at diagnosis, post-induction and post-intensification in adult de novo AML. Leukemia 2013; 27: 2157–2164.
Cilloni D, Gottardi E, Messa F, Fava M, Scaravaglio P, Bertini M et al. Significant correlation between the degree of WT1 expression and the International Prognostic Scoring System Score in patients with myelodysplastic syndromes. J Clin Oncol 2003; 21: 1988–1995.
Rossi G, Carella AM, Minervini MM, Savino L, Fontana A, Pellegrini F et al. Minimal residual disease after allogeneic stem cell transplant: a comparison among multiparametric flow cytometry, Wilms tumor 1 expression and chimerism status (complete chimerism versus low level mixed chimerism) in acute leukemia. Leuk Lymphoma 2013; 54: 2660–2666.
Gu W, Hu S, Chen Z, Qiu G, Cen J, He B et al. High expression of WT1 gene in acute myeloid leukemias with more predominant WT1+17AA isoforms at relapse. Leuk Res 2010; 34: 46–49.
Pollyea DA, Artz AS, Stock W, Daugherty C, Godley L, Odenike OM et al. Outcomes of patients with AML and MDS who relapse or progress after reduced intensity allogeneic hematopoietic cell transplantation. Bone Marrow Transplant 2007; 40: 1027–1032.
Chapuis AG, Ragnarsson GB, Nguyen HN, Chaney CN, Pufnock JS, Schmitt TM et al. Transferred WT1-reactive CD8+ T cells can mediate antileukemic activity and persist in post-transplant patients. Sci Transl Med 2013; 5: 174ra27.
Van Tendeloo VF, van d V, Van Driessche A, Cools N, Anguille S, Ladell K et al. Induction of complete and molecular remissions in acute myeloid leukemia by Wilms' tumor 1 antigen-targeted dendritic cell vaccination. Proc Natl Acad Sci USA 2010; 107: 13824–13829.
Pollyea DA, Kohrt HE, Gallegos L, Figueroa ME, Abdel-Wahab O, Zhang B et al. Safety, efficacy and biological predictors of response to sequential azacitidine and lenalidomide for elderly patients with acute myeloid leukemia. Leukemia 2012; 26: 893–901.
Porter DL, Alyea EP, Antin JH, DeLima M, Estey E, Falkenburg JH et al. NCI First International Workshop on the Biology, Prevention, and Treatment of Relapse after Allogeneic Hematopoietic Stem Cell Transplantation: Report from the Committee on Treatment of Relapse after Allogeneic Hematopoietic Stem Cell Transplantation. Biol Blood Marrow Transplant 2010; 16: 1467–1503.
Schmid C, Labopin M, Nagler A, Bornhauser M, Finke J, Fassas A et al. Donor lymphocyte infusion in the treatment of first hematological relapse after allogeneic stem-cell transplantation in adults with acute myeloid leukemia: a retrospective risk factors analysis and comparison with other strategies by the EBMT Acute Leukemia Working Party. J Clin Oncol 2007; 25: 4938–4945.
Andersson C, Li X, Lorenz F, Golovleva I, Wahlin A, Li A Reduction in WT1 gene expression during early treatment predicts the outcome in patients with acute myeloid leukemia. Diagn Mol Pathol 2012; 21: 225–233.
Kwon M, Martinez-Laperche C, Infante M, Carretero F, Balsalobre P, Serrano D et al. Evaluation of minimal residual disease by real-time quantitative PCR of Wilms' tumor 1 expression in patients with acute myelogenous leukemia after allogeneic stem cell transplantation: correlation with flow cytometry and chimerism. Biol Blood Marrow Transplant 2012; 18: 1235–1242.
Cilloni D, Messa F, Arruga F, Defilippi I, Gottardi E, Fava M et al. Early prediction of treatment outcome in acute myeloid leukemia by measurement of WT1 transcript levels in peripheral blood samples collected after chemotherapy. Haematologica 2008; 93: 921–924.
Polak J, Hajkova H, Maalaufova-Soukupova J, Markova J, Salek C, Schwarz J et al. Estimation of molecular upper remission limit for monitoring minimal residual disease in peripheral blood of acute myeloid leukemia patients by WT1 expression. Exp Ther Med 2012; 3: 129–133.
de Lima M, Giralt S, Thall PF, de Padua SL, Jones RB, Komanduri K et al. Maintenance therapy with low-dose azacitidine after allogeneic hematopoietic stem cell transplantation for recurrent acute myelogenous leukemia or myelodysplastic syndrome: a dose and schedule finding study. Cancer 2010; 116: 5420–5431.
Topp MS, Gokbuget N, Zugmaier G, Degenhard E, Goebeler ME, Klinger M et al. Long-term follow-up of hematologic relapse-free survival in a phase 2 study of blinatumomab in patients with MRD in B-lineage ALL. Blood 2012; 120: 5185–5187.
Slovak ML, Kopecky KJ, Cassileth PA, Harrington DH, Theil KS, Mohamed A et al. Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Easter Cooperative Oncology Group study. Blood 2000; 96: 4075–4083.
Wetzler M, Dodge RK, Mrozek K, Carroll AJ, Tantravahi R, Block AW et al. Prospective karyotype analysis in adult acute lymphoblastic leukemia: the cancer and leukemia Group B experience. Blood 1999; 93: 3983–3993.
Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood 1997; 89: 2079–2088.
Acknowledgements
We thank the staff of the Department of Hematology and Hematopoietic Cell Transplant for their unwavering support of the program. The dedication of the hematology nurse coordinators and staff in facilitating the study, assisting the patients with informed consent and collecting the blood specimens is greatly appreciated. We are most grateful to the patients who participated in the study. This work was partially supported by the Tim Nesvig Lymphoma Fellowship and Research Fund (RN and DJD) and by the ThinkCure Foundation (RN and DJD), and PHS Grants CA077544 (DJD) and CA030206 to DJD and SJF. The City of Hope Cancer Center is supported by CA33572. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Israyelyan, A., Goldstein, L., Tsai, W. et al. Real-time assessment of relapse risk based on the WT1 marker in acute leukemia and myelodysplastic syndrome patients after hematopoietic cell transplantation. Bone Marrow Transplant 50, 26–33 (2015). https://doi.org/10.1038/bmt.2014.209
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2014.209
- Springer Nature Limited
This article is cited by
-
WT1 and TP53 as valuable diagnostic biomarkers for relapse after hematopoietic stem cell transplantation in acute myeloid leukemia
Molecular Biology Reports (2024)
-
WT1-guided pre-emptive therapy after allogeneic hematopoietic stem cell transplantation in patients with acute myeloid leukemia
International Journal of Hematology (2024)
-
Possible prognostic impact of WT1 mRNA expression at day + 30 after haploidentical peripheral blood stem cell transplantation with posttransplant cyclophosphamide for patients with myeloid neoplasm: a multicenter study from the Okayama Hematological Study Group
International Journal of Hematology (2022)
-
Quantitative chimerism in CD3-negative mononuclear cells predicts prognosis in acute myeloid leukemia patients after hematopoietic stem cell transplantation
Leukemia (2020)
-
A phase I study of selinexor in combination with high-dose cytarabine and mitoxantrone for remission induction in patients with acute myeloid leukemia
Journal of Hematology & Oncology (2018)