Abstract
The biologic effects of visible light, particularly blue light, on the skin at doses and irradiances representative of sunlight have been established. Recent research studies investigated the effects of blue light (BL) from electronic screen devices; however, it is unclear if the evidence can be generalized to real life. The aim of this systematic review was to evaluate available evidence regarding clinical effects of BL emitted from electronic devices on human skin using the framework established by the Office of Health Assessment and Translation (OHAT). A systematic literature search was conducted by two librarians in Ovid MEDLINE, Embase.com, and Web of Science for relevant articles published from 1946 to March 2022. In vitro and in vivo studies that investigated the effects of BL from electronic devices on skin were included. From the 87 articles gathered from database searches and 1 article identified from citation search, only 9 met the inclusion criteria (6 in vitro and 3 in vivo studies). Human and animal literature with the highest level of evidence ratings were considered with mechanistic data to form one of five human hazard identifications for each outcome category using the OHAT protocol: (1) known, (2) presumed, (3) suspected, (4) not classifiable, or (5) not identified to be a hazard to humans. Literature-based evidence integration did not identify exposure to BL from electronic devices as a hazard to skin pigmentation, redness, yellowness, or melasma exacerbation. Exposure to BL from electronic devices was not classified as a skin photoaging hazard. Low confidence in representative exposure characterization drove high OHAT risk-of-bias ratings for the majority of included studies. While these conclusions hold true for the limited existing data, a larger number of future studies with high-confidence evidence are needed to verify and strengthen hazard identification conclusions.
Graphic Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
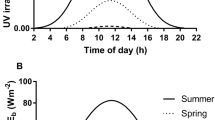
The visible light (VL; 400 to 700 nm) portion of the solar spectrum can induce long-lasting skin pigmentation in dark skin types (Fitzpatrick skin types [FSTs] IV–VI) and erythema in light skin types (FSTs I–III) through the production of free radicals [1,2,3]. Additionally, certain pathologies such as melasma, post-inflammatory hyperpigmentation, and photodermatoses are exacerbated by VL exposure [4]. Of note, the effects of VL are determined by its intensity and wavelength. Shorter wavelengths of visible light, particularly wavelengths close to ultraviolet A (blue-violet 415 nm), were shown to dose-dependently generate free radicals and stimulate skin pigmentation under irradiation conditions similar to natural sun exposure [5, 6]. While sunlight is the primary source of blue light (BL) at ground level, low-intensity BL (with irradiance approximately 1000 times lower than that of the corresponding natural sunlight) can be generated by other sources, including screens of electronic devices [7]. In addition to producing a lower intensity BL than the sun, dominant BL wavelengths emitted by most electronic devices do not contain the shorter and more energetic 415 nm wavelength [7,8,9].
With the increased exposure to electronic screens in recent years, there is a growing interest in the effects of their low-intensity BL emissions on the skin. This is supported by frequent features in the media and many photoprotection products claiming defense against BL [10,11,12,13]. As such, recent publications discuss the results regarding the impact of BL emitted from electronic devices on the skin [7,8,9, 14,15,16,17,18,19]. Of note, due to unavailability of validated and standardized phototesting guidelines against VL and BL, study protocols and exposures varied greatly. This makes it challenging to interpret the results into clinical significance. The objective of this systematic review was to comprehensively evaluate the literature investigating the effects of BL from electronic devices on the skin in vivo and in vitro and determine the level of evidence for a hazardous effect on humans by closely following the framework established by the Office of Health Assessment and Translation (OHAT).
2 Methods
2.1 Focused question and protocol registration
This focused question was: “Does BL emitted from electronic devices have clinical effects on human skin?” This review was registered with the Prospective Register of Systematic Reviews (PROSPERO) and followed the Preferred Reporting Items for Systematic Reviews (PRISMA) guidelines.
2.2 Search strategy
Ovid MEDLINE, Embase.com, and Web of Science databases were searched by two independent librarians from 1946 to March 10, 2022. Individual search strings used for each database is included in Supplemental Fig. 1. Reference lists of relevant articles were hand searched for additional articles.
2.3 Eligibility criteria
This review included studies in English that evaluated exposure to BL emitted from electronic device screens or aimed to simulate such an exposure. We included in vitro studies on human or animal cell lines and in vivo studies on human or animal skin. Articles were included if the measurement of biological and clinical outcomes related to skin pigmentation, skin redness, skin yellowness, or skin photoaging occurred following exposure to the light source. We excluded abstract only papers, opinion/communication, narrative reviews, systematic reviews, and meta-analyses.
2.4 Article selection & data extraction
Based on eligibility criteria, titles and abstracts of all articles were screened and full-text review of eligible texts were subsequently performed. Two authors (MC and JP) independently reviewed all the records and extracted data from included studies. Consensus was determined by a third author (IK).
The following relevant information was collected from eligible studies: (1) publication details (first author, year, country, funding sources, and possible and reported conflicts of interest), (2) study design, (3) qualities of test and control samples/substrates (number, conditions, source, eligibility criteria), (4) aims, (5) primary and ancillary endpoints, (5) assessment methods, and (6) lowest level of exposure for outcomes. Light source parameters were extracted based on the recommendations for reporting methods in phototesting studies and included: (1) light source type, (2) exposure waveband (nm), (3) filter, (4) calibration method, (5) distance between light source and sample/substrate, (6) irradiation time, (7) number of exposures and frequency, (8) individual and cumulative doses (J/cm2), and (9) irradiance [20]. Covidence, a web-based platform for systematic review management, was used to organize the articles and data extraction.
2.5 Risk of bias assessment and evidence integration
The Office of Health Assessment and Translation (OHAT) framework for determination of potential hazardous health effects from exposure to environmental substances was used to integrate the evidence obtained from the systematic review process into conclusions. The sequence of OHAT steps followed after data extraction from studies included in the systematic review were: (1) critically assess individual studies for risk of bias (all included studies), (2) synthesize confidence in the results of included studies (in vivo: human and animal), (3) translate the confidence ratings into levels of evidence (in vivo: human and animal), and (4) develop hazard identification conclusions (all included studies) [21]. Inclusion of studies in each step was according to OHAT recommended guidelines. Evidence from human and animal studies were assessed separately and integrated in the last step [22]. Methodology for each of the four OHAT-specific steps is discussed below:
-
(1)
Risk of bias assessment: individual studies
All included studies were separated by study design and independently assessed for risk of bias by two authors (MC and JP) with consensus formed by a third author (IK). Applicable OHAT risk of bias questions relevant to the design of each study were rated on a four-point scale: definitely low risk (++), probably low risk (+), not reported/probably high risk (-), and definitely high risk (–) [21,22,23]. Following this, a three-tier approach was used to determine individual study quality based on the risk of bias question ratings with emphasis on project-specific key study elements, which for this review were regarding confidence in exposure characterization, outcome assessment, and consideration of important confounding variables. Tier grading criteria are described in Supplemental Table 1. Optimally, Tier 3 studies, which have a high concern of bias on key elements, should be excluded from further analysis; however, considering the limited number of relevant studies all available in vivo data was considered for analysis in the next step [22].
-
(2)
Forming confidence ratings in bodies of evidence
Following the OHAT framework to determine the confidence in the bodies of evidence, an initial confidence rating of high (++++), moderate (+++), low (++), or very low (+) was assigned to each outcome evaluated in the included human and animal studies based on the number of the following study design features: controlled exposure, exposure prior to outcome, individual outcome data, and use of comparison group. Then, this initial confidence rating was downgraded one level for each factor weakening confidence (risk of bias, unexplained inconsistency, indirectness, lack of applicability, imprecision, and publication bias) and upgraded one level each for each factor strengthening confidence (large magnitude of effect, dose response, consistency across dissimilar evidence streams, and consideration of residual confounders). Resulting evidence with a very low confidence rating (+) was not considered for the next step [21, 22].
-
(3)
Translation into evidence of health effects
The resulting confidence ratings from each body of evidence from the previous step were translated into corresponding evidence ratings for each health effect. Studies showing evidence of a health effect were given an evidence rating of high, moderate, or low based on their respective confidence level in the body of evidence. For studies showing no health effect, the level of evidence was translated into evidence of no health effect (high confidence in body evidence) or inadequate evidence (moderate and low confidence in body of evidence). Outcomes from the previous step were first assessed separately before similar outcomes were considered together to determine the overall confidence in the association between exposure and the health effect [21].
-
(4)
Develop hazard identification
In the last step, one of five hazard identification conclusions (known, presumed, suspected, not classifiable, not identified) for health effects to humans is developed. Hazard identification is formed by integrating the level of evidence for health effects in human and animal studies determined in the prior step, which then can be upgraded or downgraded depending on the strength of relevant mechanistic in vitro data [21, 22].
2.6 Statistical analysis
The analyses of this study involved implementation of the OHAT framework on the data extracted from the included articles to evaluate evidence for potential hazardous health effects of BL from electronic device screens on human skin. Use of statistical tests was not applicable.
3 Results
3.1 Included studies
A total of 87 studies were identified from databases and processed according to the PRISMA statement (Fig. 1). After de-duplication, 54 articles were screened by title and abstract, which identified 28 studies that did not meet eligibility criteria. Full-text review of 26 articles excluded 18 studies for the following reasons: abstract only (n = 12), review paper (n = 2), inapplicable aim (n = 1), inapplicable substrate (n = 1), communication (n = 1), and retracted paper (n = 1). A total of one record was identified by citation search, assessed for eligibility, and included in the review. Thus, a grand total of nine studies from both database and citation searches were included for data extraction, qualitative analysis, risk assessment, and hazard identification conclusions.
3.2 General study features
General study qualities that were extracted from the included studies are summarized in Supplemental Table 2.
Of the nine included articles, six conducted in vitro studies and three conducted in vivo human studies. There were zero in vivo animal studies. Eight studies (89%) were non-randomized experimental studies while one (11%) was randomized. Studies were conducted in the USA, France, Korea, Spain, Italy, and Monaco and published between 2018 and 2021.
The six in vitro studies performed experiments on multiple sample types, with some studies using more than one form. Studies used human-derived fibroblasts (n = 5), human-derived keratinocytes (n = 2), murine-derived melanocytes (n = 2), and skin explants (n = 1). The three in vivo studies performed experiments on the skin located on the back (n = 2) and the face (n = 1) of female adults with FST III–IV. Within the six vitro studies, primary biologic endpoints included reactive oxygen species (ROS), DNA damage, mitochondrial damage, cellular viability, cytoskeleton damage, and hyperpigmentation. The three in vivo studies had primary biologic endpoints of hyperpigmentation, redness, yellowness, erythema, and photoaging. Outcomes were measured using the L*a*b* values, individual typography angle (ITA), minimum persistent pigment darkening dose (MPPD), melanin index, modified melasma area and severity (mMASI) score, erythema index, transparency, skin hydration, and elasticity.
3.3 Blue light irradiation parameters
Light source parameters and irradiation procedures varied among the nine included studies and are summarized in Supplemental Table 3. To study the effects of BL, seven (77.8%) studies used light-emitting diode (LED) lights, one used filtered light from a xenon solar simulator, and one used multiple electronic devices. Seven (77.8%) studies exclusively studied wavelengths only within the BL spectrum with peaks ranging within 415–490 nm. Two (22.2%) studies investigated BL effects by using broad-spectrum sources including wavelengths beyond BL, as one used the VL and infrared spectrum (420 to 1072 nm) and one used blue, green, and red wavelengths (450 nm, 525 nm, and 625 nm). Calibration method was reported in four (44.4%) studies, where a photometer, spectroradiometer, optical power meter, and power meter intensities were used. Irradiance of BL was reported in four (44.4%) studies and could be calculated from reported parameters in three (33.3%) studies, which ranged from 0.207 to 112 mW/cm2. Eight (88.9%) studies had one exposure and one (12.5%) study had five exposures over 5 days. Single and multiple exposures led to cumulative BL doses that ranged from 0.7452 to 1597 J/cm2 with some corresponding to BL only and some to BL within the broadband source. The distance between light source and sample/substrate was reported in four (44.4%) studies, in which two studies placed the light source directly below the cell culture plate, one study placed the light source 1 cm from the cell plate, and one study placed the subject 20 cm away from the light source. The duration of exposure was reported in four (44.4%) studies and ranged from 15 min to 3 h.
3.4 Relevant outcomes
Hazardous human health effects of BL emitted from electronic devices were depicted in all six in vitro studies and two of three in vivo studies. Specific outcomes examined in included studies are summarized below and in Supplemental Table 4.
-
(1)
Outcomes evaluated by in vitro studies
Increased production of ROS was the first effect observed with the lowest dose of BL, which was 0.7452 J/cm2 from an Apple iPad that emitted a total VL + infrared (IR) dose of 3.06 J/cm2 [8]. Increased ROS production was measured in three studies using dihydrorhodamine-123 (DHR-123) flow cytometry (n = 1), 2',7'-dichlorodihydrofluorescein diacetate (H2-DCFDA) oxidation (n = 1), and dihydrofluorescein diacetate (DHFDA) fluorescent microscopy (n = 1) [8, 14, 18]. Increased DNA damage was found by three studies: one study found increased olive tail moment (OTM) distributions, increased cyclobutane–pyrimidine dimers (CPD) lesions, slower time-dependent repair, and increased number of micronucleated cells, one study found increased 8-dihydroxy-2'-deoxyguanosine (8-OHdG) production, and one study found increased light-modulated transcripts from human genome microarray-based gene expression analysis [9, 14, 15]. Five studies evaluated the effects on cell viability. One study did not find significant changes in apoptosis and necrosis using FlowCellect Annexin Red Kit flow cytometry [8]. Decreased cellular viability was found in four studies using 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl-2H-tetrazolium bromide (MTT) assays (n = 4), adenosine 5-triphosphate (ATP) levels (n = 1), and population doubling times (n = 1) [9, 14, 18, 19]. Increased mitochondrial effects were found in three studies by using mitochondrial network length (n = 1), irregular morphology (n = 3), and membrane potential hyperpolarization (n = 2) [9, 18, 19]. Disorganized cytoskeletal effects were determined with F-actin organization and cell spreading image analysis in one study [9]. Increased degradation of extracellular matrix mRNA and protein components were assessed in two studies from increased expression of matrix metalloproteinase-1 (n = 1), matrix metalloproteinase-12 (n = 1) and down-regulation of pro-collagen type 1 (n = 1) and collagen type 1 (n = 1) [9, 14]. Hyperpigmentation was assessed in one study by measuring increased darkening of extracellular and intracellular pigments [19]. Two studies evaluated signal transduction outcomes, as one found increased activation of p38 melanogenic signaling pathway and one study found increased activation of mitogen-activated protein kinase p38 phosphorylation and increased opsin-3 expression [18, 19].
-
(2)
Outcomes evaluated by in vivo studies
All three in vivo studies evaluated the effects of BL from electronic devices on FST III–IV female adult skin, among these was one study on subjects with melasma. One study had irradiance information available, while irradiance was not reported (NR) and could not be calculated from given parameters for the parts of the other two studies included in this review. All three studies evaluated skin pigmentation effects. One study did not find a significant change in skin pigmentation as assessed by delta L* or delta ITA in melasma patients with a BL dose of 0.865 J/cm2 BL administered at an irradiance of 0.48 mW/cm2 [7]. Both of the other two studies found significant pigmentary changes: one found changes in L* and melanin index with the effect induced at 447 J/cm2 (irradiance NR) [16] and the other obtained changes in melanin index and three-point visual examination score with a BL dose of 135 J/cm2 (irradiance NR) [17].
Two studies assessed skin redness and yellowness by measuring delta a* and delta b*, where one study observed 958 J/cm2 and 1597 J/cm2 as the lowest doses to exert a significantly increased delta a* and delta b*, respectively (irradiance NR) [16]. The other study did not find a significant change in delta a* or delta b* with a BL dose of 0.864 J/cm2 using 0.48 mW/cm2 irradiance [7]. One study measured the erythema index, which had a significant increase at a 447 J/cm2 BL dose (irradiance NR) [16]. One study measured disease activity of melasma using the change in mMASI, where no significant effect was observed using a single BL dose of 0.865 J/cm2 or cumulative 5-day BL dose of 4.43 J/cm2 performed at an irradiance of 0.48 mW/cm2 [7]. One study measured the skin photoaging qualities of transparency, hydration, and elasticity and an increase in all photoaging parameters was found at the lowest BL dose of 446 J/cm2 (irradiance NR) [16].
3.5 Quality assessment and hazard identification conclusions
-
(1)
Bias assessment of individual studies
Figure 2 shows individual study ratings for each risk-of-bias question that applied to its study design according to the OHAT tool. Across all study types, one (11.1%) study was rated as Tier 1, indicating the lowest risk of bias. Four studies (44.4%) were rated as Tier 2 and four (44.4%) studies were rated as Tier 3. Out of the three in vivo studies, there was one (33.3%) Tier 1 study, which had a “definitely low” risk of bias in all applicable domains, and two (66.6%) Tier 3 studies. Nonetheless, Tier 3 evidence was considered for further analysis due to a limited number of included in vivo studies. Zero (0%) in vitro studies had a “definitely low” or “probably low” risk of bias in all applicable domains.
-
(2)
Confidence in the bodies of evidence
Three human studies, which included two Tier 3 studies, were considered in the body of evidence confidence rating for each health outcome. No animal studies were considered, as none were found in included articles. Mechanistic in vitro studies were not included in this step, per OHAT handbook [22]. Table 1 shows the final confidence levels in the body of evidence for the four main clinical outcomes: skin pigmentation (high confidence, ++++), skin redness and yellowness (high confidence, ++++), melasma exacerbation (high confidence, ++++), and skin photoaging (low confidence, ++). Supplemental Table 5 contains further details involved in determination of these confidence ratings and factors that upgraded or downgraded the confidence of each outcome by one level for each factor. All studies had an initial confidence rating of high (++++).
-
(3)
Health effects
Health effects are summarized in Table 1 and detailed in Supplemental Table 5. The evidence with high-level confidence showed BL from electronic devices did not have a health effect on skin pigmentation, skin redness, skin yellowness, and melasma exacerbation. Evidence with low-level confidence showed that BL from electronic devices did have a photoaging health effect.
-
(4)
Hazard identification
Final hazard identification conclusions are summarized in Table 1. BL from electronic devices was not identified as a hazard to human skin pigmentation, skin redness, skin yellowness, or melasma exacerbation, as high-level evidence did not find these health effects. BL was not classifiable as a hazard to human skin photoaging due to associated evidence having low-level confidence. In vitro data did not provide strong evidence to support upgrading the hazard identification conclusion for skin photoaging.
3.6 Discussion
Based on the current literature, BL from electronic devices was not determined a hazard to human skin pigmentation, redness, yellowness, or melasma activity and was not classifiable as a hazard to human skin photoaging. Apart from photoaging, which was based on Tier 3 evidence, these conclusions were determined from studies with the highest level of evidence.
The level of confidence in studies was primarily affected by irradiation exposure parameters and choice of tested substrate, which varied significantly among the included studies. Findings representative or suggestive of negative health effects were found frequently among bodies of evidence that received a low confidence rating. This was primarily influenced by low confidence in exposure characterization in the OHAT risk-of-bias ratings. Electronic devices emit BL at a very low irradiance, approximately 30 µW/cm2 [7]. However, most of the included studies used irradiances two to three orders of magnitude greater [7, 9]. The findings, as such, should be interpreted with caution. These studies may have utilized high irradiances to recreate long-term exposure in a shortened amount of time [24]. With VL phototesting still being a relatively new area of study, standard guidelines for testing are not yet in place. Therefore, until appropriate testing ranges are established, irradiation parameters in study protocols must be deliberatively chosen to mimic irradiation levels of actual electronic devices as closely as possible to obtain clinically relevant results.
Outcomes indicative of negative health effects were found among all included in vitro studies. However, findings of in vitro studies are not intended to identify a disease phenotype. Rather, they are meant to detect cellular, biochemical, and molecular processes or early biomarkers [22]. For this reason, mechanistic data from in vitro studies is integrated in the last OHAT step, rather than during determination of confidence in the body of evidence for each health effect outcome [22]. Additionally, in vitro studies may be more sensitive to interventions, such as irradiation, as structural integrity, barrier function, and physiologic repair mechanisms are not maintained [25]. In vitro studies also cannot account for FST, which is an important factor to consider, as VL primarily exerts clinical changes on FST IV–VI skin [1].
Findings of this study suggest the established effects on skin by BL from sunlight are not induced by the low-intensity BL from electronic devices [1, 3, 5, 26]. As such, based on available evidence, we do not consider it necessary to use sunscreen protective against blue light while using electronic devices indoors in a room without sunlight from a window. Clinicians and consumers should be aware of the clinically unsupported claims of skin photodamage induced by BL from electronic devices. This information can be used to guide patients on the environmental conditions that require photoprotection, lifestyle practices, and purchase of evidence-based skin care products.
3.7 Conclusion
Using the OHAT approach for systematic review and integration of the current evidence, BL from electronic devices was not identified as a hazard to human skin pigmentation, redness, yellowness, and exacerbation of melasma. BL from electronic devices was not classifiable as a hazard to human photoaging. A larger number of future studies with minimal bias and exposure levels representative of electronic devices is warranted to verify and strengthen these hazard identification conclusions.
References
Mahmoud, B. H., Ruvolo, E., Hexsel, C. L., Liu, Y., Owen, M. R., Kollias, N., Lim, H. W., & Hamzavi, I. H. (2010). Impact of long-wavelength uva and visible light on melanocompetent skin. The Journal of Investigative Dermatology, 130(8), 2092–2097. https://doi.org/10.1038/jid.2010.95
Liebel, F., Kaur, S., Ruvolo, E., Kollias, N., & Southall, M. D. (2012). Irradiation of skin with visible light induces reactive oxygen species and matrix-degrading enzymes. The Journal of Investigative Dermatology, 132(7), 1901–1907. https://doi.org/10.1038/jid.2011.476
Kohli, I., Zubair, R., Lyons, A. B., Nahhas, A. F., Braunberger, T. L., Mokhtari, M., Ruvolo, E., Lim, H. W., & Hamzavi, I. H. (2019). Impact of long-wavelength ultraviolet al and visible light on light-skinned individuals. Photochemistry and Photobiology, 95(6), 1285–1287. https://doi.org/10.1111/php.13143
Austin, E., Geisler, A. N., Nguyen, J., Kohli, I., Hamzavi, I., Lim, H. W., & Jagdeo, J. (2021). Visible light. Part i: Properties and cutaneous effects of visible light. Journal of the American Academy of Dermatology, 84(5), 1219–1231. https://doi.org/10.1016/j.jaad.2021.02.048
Duteil, L., Cardot-Leccia, N., Queille-Roussel, C., Maubert, Y., Harmelin, Y., Boukari, F., Ambrosetti, D., Lacour, J. P., & Passeron, T. (2014). Differences in visible light-induced pigmentation according to wavelengths: a clinical and histological study in comparison with uvb exposure. Pigment Cell & Melanoma Research, 27(5), 822–826. https://doi.org/10.1111/pcmr.12273
Vandersee, S., Beyer, M., Lademann, J., & Darvin, M. E. (2015). Blue-violet light irradiation dose dependently decreases carotenoids in human skin, which indicates the generation of free radicals. Oxidative Medicine and Cellular Longevity, 2015, 579675. https://doi.org/10.1155/2015/579675
Duteil, L., Queille-Roussel, C., Lacour, J. P., Montaudié, H., & Passeron, T. (2020). Short-term exposure to blue light emitted by electronic devices does not worsen melasma. Journal of the American Academy of Dermatology, 83(3), 913–914. https://doi.org/10.1016/j.jaad.2019.12.047
Austin, E., Huang, A., Adar, T., Wang, E., & Jagdeo, J. (2018). Electronic device generated light increases reactive oxygen species in human fibroblasts. Lasers in Surgery and Medicine. https://doi.org/10.1002/lsm.22794
Rascalou, A., Lamartine, J., Poydenot, P., Demarne, F., & Bechetoille, N. (2018). Mitochondrial damage and cytoskeleton reorganization in human dermal fibroblasts exposed to artificial visible light similar to screen-emitted light. Journal of Dermatological Science. https://doi.org/10.1016/j.jdermsci.2018.04.018
Intner, K. (2020). The best products to protect your skin from blue light damage. Harper’s BAZAAR. https://www.harpersbazaar.com/beauty/skin-care/g32253448/best-blue-light-skin-protectors/
Anello, C. (2020). Do we need blue-light-specific skin care? New York Magazine. https://nymag.com/strategist/article/blue-light-skin-care.html
Nazish, N. (2021). Everything dermatologists want you to know about blue light protection skincare. Forbes. https://www.forbes.com/sites/nomanazish/2021/01/23/everything-dermatologists-want-you-to-know-about-blue-light-protection-skincare/?sh=186172bd7e8a
Mazkenzie, M., Prinzivalli L., Stables, P. (2020). How your phone’s blue light could be damaging your skin, according to dermatologists. Allure. https://www.allure.com/story/blue-light-phone-skin-effects
Avola, R., Graziano, A. C. E., Pannuzzo, G., Bonina, F., & Cardile, V. (2019). Hydroxytyrosol from olive fruits prevents blue-light-induced damage in human keratinocytes and fibroblasts. Journal of Cellular Physiology, 234(6), 9065–9076. https://doi.org/10.1002/jcp.27584
Chamayou-Robert, C., DiGiorgio, C., Brack, O., & Doucet, O. (2022). Blue light induces DNA damage in normal human skin keratinocytes. Photodermatology, Photoimmunology and Photomedicine, 38(1), 69–75. https://doi.org/10.1111/phpp.12718
Jo, H. L., Jung, Y., Kim, Y. K., Kim, N., Cho, E., Han, J., Hwang, Y. K., Suh, B. F., & Kim, E. (2021). Efficacy of ethyl ascorbyl ether-containing cosmetic cream on blue light-induced skin changes. Journal of Cosmetic Dermatology. https://doi.org/10.1111/jocd.14232
Jo, H. L., Jung, Y., Suh, B. F., Cho, E., Kim, K., & Kim, E. (2020). Clinical evaluation method for blue light (456 nm) protection of skin. Journal of Cosmetic Dermatology, 19(9), 2438–2443. https://doi.org/10.1111/jocd.13508
Lorrio, S., Rodríguez-Luna, A., Delgado-Wicke, P., Mascaraque, M., Gallego, M., Pérez-Davó, A., González, S., & Juarranz, Á. (2020). Protective effect of the aqueous extract of deschampsia antarctica (edafence(®)) on skin cells against blue light emitted from digital devices. International Journal of Molecular Sciences. https://doi.org/10.3390/ijms21030988
Portillo, M., Mataix, M., Alonso-Juarranz, M., Lorrio, S., Villalba, M., Rodríguez-Luna, A., & González, S. (2021). The aqueous extract of polypodium leucotomos (fernblock(®)) regulates opsin 3 and prevents photooxidation of melanin precursors on skin cells exposed to blue light emitted from digital devices. Antioxidants (Basel). https://doi.org/10.3390/antiox10030400
Tisack, A., Pourang, A., Kohli, I., Lim, H. W., & Hamzavi, I. H. (2022). Recommendations for reporting methods in phototesting studies. Photochemistry and Photobiology, 98(1), 130–131. https://doi.org/10.1111/php.13493
Rooney, A. A., Boyles, A. L., Wolfe, M. S., Bucher, J. R., & Thayer, K. A. (2014). Systematic review and evidence integration for literature-based environmental health science assessments. Environmental Health Perspectives, 122(7), 711–718. https://doi.org/10.1289/ehp.1307972
Handbook for conducting a literature-based health assessment using ohat approach for systematic review and evidence integration. (2019). National Institute of Environmental Health Sciences Retrieved from https://ntp.niehs.nih.gov/ntp/ohat/pubs/handbookdraftmarch2019.pdf
Rooney, A. (2015). Extending a risk-of-bias approach to address in vitro studies. National Toxicology Program Retrieved from https://ofmpub.epa.gov/eims/eimscomm.getfile?p_download_id=526750
Kohli, I., Lim, H. W., & Hamzavi, I. H. (2020). Caution regarding testing for long wavelength ultraviolet al and visible light effects on human skin in vivo. Photodermatology, Photoimmunology and Photomedicine, 36(1), 58–60. https://doi.org/10.1111/phpp.12487
Fitoussi, R., Faure, M. O., Beauchef, G., & Achard, S. (2022). Human skin responses to environmental pollutants: A review of current scientific models. Environmental Pollution, 306, 119316. https://doi.org/10.1016/j.envpol.2022.119316
Passeron, T. (2019). The key question of irradiance when it comes to the effects of visible light in the skin. Journal of Dermatological Science, 93(1), 69–70. https://doi.org/10.1016/j.jdermsci.2018.11.011
Acknowledgements
We would like to acknowledge the Dermatology Foundation for the salary support through the Research Career Development Award.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors do not report any relevant conflicts of interest for this publication.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ceresnie, M.S., Patel, J., Lim, H.W. et al. The cutaneous effects of blue light from electronic devices: a systematic review with health hazard identification. Photochem Photobiol Sci 22, 457–464 (2023). https://doi.org/10.1007/s43630-022-00318-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43630-022-00318-9